1. Introduction
Plantar heel pain involving the plantar fascia (plantar fasciitis, plantar fasciosis) is one of the most common overuse foot injuries in the general population, affecting both active and sedentary individuals [
1]. With respect to the prevalence in active individuals, a prospective study of lower extremity injuries in runners found that plantar heel pain was the most common injury, affecting 31.3% of runners over the five-year study period [
2]. Further, a systematic review of running-related musculoskeletal injuries reported plantar heel pain as the third most common injury after medial tibial stress syndrome and Achilles tendinopathy [
3]. In addition to the high prevalence, plantar heel pain is also associated with significant economic and personal burden. In the United States, 65% of patients with plantar heel pain seek medical attention multiple times [
4], and the average annual treatment cost associated with plantar heel pain is USD 284 million [
5]. Moreover, studies have shown that plantar heel pain is associated with diminished foot-specific health and overall health-related quality of life [
6]. To reduce the negative impacts associated with plantar heel pain, it is crucial to identify and address the pathoetiological factors associated with the injury.
In general, it is accepted that the mechanical overload of the plantar fascia during gait and/or long periods of weightbearing leads to microtrauma and subsequent degeneration [
7]. During gait, the plantar fascia contributes as a passive stabilizer to control foot pronation in the early stance and to facilitate foot supination in the mid-late stance [
8,
9,
10,
11,
12,
13,
14]. Prior to initial contact, the plantar fascia is preloaded to facilitate control of the foot pronation that occurs following initial contact [
12]. During the early stance phase, tension in the plantar fascia effectively secures the cuboid within the confines of the calcaneus, thereby establishing stability within the midtarsal complex of the foot (calcaneocuboid locking mechanism) [
8,
11]. As the foot enters into midstance and the orientation of the midtarsal shafts shifts from a horizontal to vertical alignment, the plantar fascia assumes a tie-rod role, effectively distributing compressive loads across the tarsal and metatarsal bones and enhancing stability within the central midfoot structures (truss mechanism) [
8]. Finally, during the terminal phase of the gait, tension in the plantar fascia activates the windlass mechanism, which facilitates foot supination [
8,
13]. While the function of the plantar fascia during gait is well established, the effect of plantar heel pain on foot function during running gait is currently poorly understood. The current clinical belief is that the repetitive straining of the plantar fascia during running causes progressive chronic degeneration that is eventually experienced as heel pain [
15]. In addition to producing pain, degeneration [
7,
16] is also likely to cause changes to the mechanical properties of the plantar fascia and compromised function during running gait. The compromised function during gait may contribute to the development and/or persistence of the plantar heel pain. To date, only two studies have investigated the effect of plantar heel pain on foot function during running gait [
17,
18]. Pazhooman et al. [
17] reported differences in the stance phase range of motion in runners with plantar heel pain, consistent with a decreased ability to control foot pronation in the early–mid stance and contribute to foot supination in the mid-late stance. Wiegand et al. [
18] reported significant differences between runners with plantar heel pain and runners that had recovered from plantar heel pain, but not between runners with plantar heel pain and uninjured runners.
In addition to changes in the kinematics at individual joints, the coupling between adjacent joints has also been theorized to be important to normal lower extremity function during gait. Changes in the normal/typical coupling between adjacent joints are believed to cause the abnormal loading of the bones and soft tissues in and around the affected joints, which may lead to initial injury and/or injury persistence [
19]. Thus, abnormal joint coupling between adjacent joints of the foot may be a cause of repetitive strain, leading to plantar heel pain and/or may contribute to the persistence of plantar heel pain. The only study conducted to date found that individuals with plantar heel pain demonstrated significantly fewer frontal plane anti-phase movements between the rearfoot and medial forefoot during walking gait than uninjured participants [
20]. While this study has further improved the understanding of the effect of plantar heel pain on foot function during walking gait, the results may not be generalizable to running gait [
21]. Furthermore, this study investigated discrete variables at predetermined instances/periods during gait. While discrete analyses are important, they may not capture other relevant changes throughout the stance phase. Statistical parametric mapping (SPM) is an approach that enables the examination of joint kinematics across an entire time series [
22].
To date, the effect of plantar heel pain on foot joint coupling during running gait has not been investigated using curve analysis techniques. Therefore, the purpose of this study was to employ SPM methodology to investigate foot joint coupling during running gait in runners with and without plantar heel pain. We hypothesized that the degenerative changes in the plantar fascia that occur with plantar heel pain would change the foot joint coupling angles of individuals with plantar heel pain during the stance phase of running gait.
2. Materials and Methods
A total of 13 uninjured runners (7 m, 6 f) (uninjured) and 13 runners with plantar heel pain associated with the pathology of plantar fascia (PHP) (6 m, 7 f) participated in the study. All runners were between the ages of 18 and 45 years old, and all were informed of the study procedures and provided written consent approved by the Institutional Review Board. The PHP runners had common clinical symptoms of plantar heel pain associated with pathology of the plantar fascia for a minimum of six weeks, were consistently running at least 10 miles per week at the time of this study [
23], and had a body mass index (BMI) of <30 kg/m
2 [
24]. The clinical symptoms indicative of plantar heel pain consisted of point tenderness localized to the medial calcaneal tubercle, the medial region of the proximal segment of the plantar fascia, or along the length of the plantar fascia [
25]. In addition, runners must have reported plantar heel pain during the first few steps of weight-bearing, following prolonged periods of inactivity that gradually diminished throughout the day with normal walking [
26,
27,
28]. The presence of plantar heel pain due to pathology of the plantar fascia was confirmed, and other potential sources of heel pain (e.g., heel pad syndrome, tibialis posterior tendinopathy) were ruled out during a brief screening exam performed by an allied health professional. Runners in the uninjured group did not have an history of plantar heel pain and were age (±5 y), sex, and mileage (10–20, 20–30, 30+ miles per week)-matched with the PHP runners. Exclusion criteria for all participants were as follows: current lower extremity injury, besides plantar heel pain in the PHP group; pregnancy; a history of lower extremity surgery on the injured side; inflammatory or connective tissue disease; diagnosed foot deformity (e.g., hallux valgus); a systemic neurologic disorder that would predispose an individual to heel pain and/or muscle weakness; and diabetic neuropathy [
29].
To determine if the current investigation would have sufficient power to detect significant differences between groups, a power analysis using data from the Wiegand et al. [
18] study that investigated the effect of plantar heel pain on foot function during running was used. Results of the power analysis (G Power 3.1) indicated that a sample size of 26 participants (13 participants per group) would be sufficient to identify a large effect size (Cohen d = 0.9), at an alpha level of 0.05, and a power 0.8.
Foot kinematics were quantified using a seven-segment foot model that defines six foot segments and a shank segment (
Figure 1) [
30]. The multi-segment foot model is fully described in our previous studies [
17,
30]. Following the application of the retroreflective markers associated with the foot model, a static trial was performed to identify additional anatomical landmarks relative to the appropriate technical marker cluster. Participants then completed 10 successful running trials at 4.0 m/s (±10%) along a runway wearing the same style sandals (Maui and Sons, Pacific Palisades, CA, USA) [
31]. The sandals were selected because they enabled the placement of markers directly on the participant’s skin and allowed participants to utilize their preferred foot strike pattern during running. Running gait speed was monitored using an opto-electronic timing device. A successful trial was defined as a trial within the fixed speed range where initial contact and toe off occurred on the force plate. Three-dimensional (3D) marker positions were captured at 200 Hz with a 10-camera Eagle system (Motion Analysis Inc, Santa Rosa, CA, USA). The stance phase initial contact and toe-off events (10 N threshold) were identified by a force plate (Advanced Mechanical Technology, Inc., Watertown, MA, USA) sampling at 1000 Hz mounted near the center of the runway.
Following the static trial and running trials, 3D marker positions were reconstructed using Cortex software (v. 5.3, Motion Analysis Inc, Santa Rosa, CA, USA). A custom-written software program (MATLAB v. 7.6.0, The MathWorks Inc., Natick, MA, USA) was then used to low-pass filter (4th order zero-lag Butterworth filter) the kinematic (12 Hz cutoff) and force plate (50 Hz cutoff) data and perform rigid body transformation procedures. Joint angles computed during the static trial were used as offset angles for the gait trials. For the running trials, the first five trials with no obvious erroneous marker displacement were selected for the stance phase coupling analysis. Stance phase joint coupling angles between adjacent functional articulations of interest (
Table 1) were calculated using the vector coding method proposed by Heiderscheit et al. [
32] (Equation (1)).
where θ
i is the joint coupling angle between 0° and 360°, i is the ith frame of the stance phase, and x and y are the angular positions of the proximal and distal functional articulation, respectively. The angle calculated is the orientation to the right horizontal of the resultant vector between two adjacent data points of the proximal functional articulation (e.g., the shank for the rearfoot complex) and two adjacent data points of the distal segment (e.g., the calcaneus for the rearfoot complex) during the stance phase [
32]. The coupling angles were interpreted as defined by Hamill et al. [
33].
0° or 180° indicates rotation primarily of the proximal joint with the distal joint fixed.
90° or 270° indicates rotation primarily of the distal joint with the proximal joint fixed.
45° or 225° reflects equal relative rotation of joints in the same direction.
135° or 315° indicates equal relative rotation of the two joints in opposite directions.
Finally, the spm1d package for one-dimensional SPM was used in MATLAB to investigate the joint coupling time series using circular statistics. To assess the normality of the data, all the comparisons were completed using the parametric (spm1d.stats.ttest2) and nonparametric (spm1d.stats.nonparam) scripts. If the parametric and nonparametric results did not differ qualitatively, the assumption of normality was considered reasonable, and the results of the parametric t-test were used. The independent variable in each test was the group (PHP, uninjured). The dependent variables were the joint couples of interest during stances. Significance for all statistical tests was defined as α = 0.05.
3. Results
Descriptive data are presented in
Table 2. A previously published statistical analysis of the descriptive data for this cohort of participants reported no significant age, BMI, or running speed group differences [
17]. A rearfoot strike pattern was the preferred strike pattern of all the runners. The strike pattern was observed during the gait trials and was confirmed following the trials by the presence of rearfoot complex plantar flexion in the weight acceptance period following initial contact.
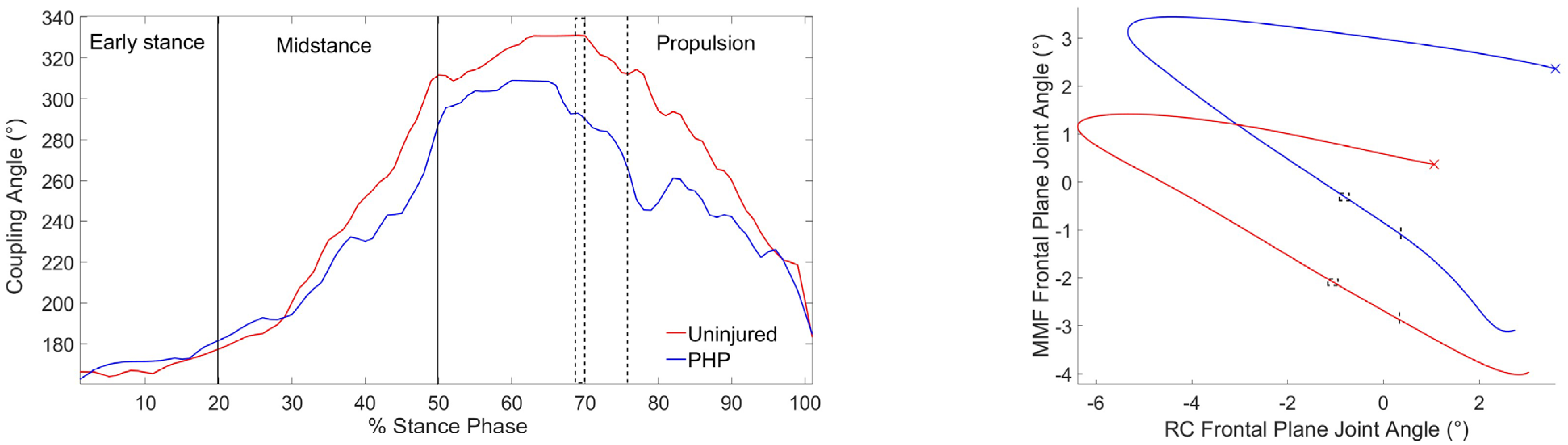
None of parametric and nonparametric SPM results differed qualitatively, so the parametric t-test was selected for all the comparisons. The SPM analyses between runners with and without plantar heel pain revealed a significant difference in RC
Fron-MMF
Fron joint coupling between the PHP and uninjured groups from 69 to 70% (mean difference = 39.41°,
p = 0.042, 95% CI [36.2°, 42.6°]) stance phase and at 76% (mean difference = 47.89°,
p = 0.049, 95% CI [44.7°, 51.1°]) of the running gait stance phase (
Figure 2). During 69–70% stance, the mean coupling angles of the PHP and uninjured groups were 291.6 ± 1.94° and 331.0 ± 1.9°, respectively. At 76% stance, the coupling angles of the PHP and uninjured groups were 264.2° and 312.1°, respectively. The results of the SPM analyses that were not statistically significant can be found in the
Supplementary Materials (Figures S1–S11).
4. Discussion
The purpose of the current study was to use SPM methodology to investigate foot joint coupling during the stance phase of running gait in runners with and without plantar heel pain. Our hypothesis that the foot coupling angles would be different in runners with plantar heel pain compared to uninjured runners during running was supported for the rearfoot complex frontal plane and medial midfoot frontal plane coupling angle between 69 and 70% stance phase and at 76% stance. Both differences occurred during the propulsion subphase (50–100%) of the running stance, when the foot should be transitioning to a more supinated position.
From 69 to 70% stance, the mean coupling angle of the PHP group was 291.6 ± 1.94°, which is between “relative equal rotation of the two joints in opposite directions (315°)” and “rotation primarily of the distal joint with the proximal joint fixed (270°)”, indicating the rearfoot complex and medial midfoot were rotating in opposite directions with the medial midfoot rotating more than the rearfoot complex. The angle–angle plot in
Figure 2 indicates the rearfoot complex was in an everted position and inverting, while the medial midfoot was in an inverted position and everting. During the same period, the mean coupling angle of the uninjured group was 331.0 ± 1.9°, which is between “rotation primarily of the proximal joint with the distal joint fixed (0°)” and “relative equal rotation of the two joints in opposite directions (315°)”, indicating that the rearfoot complex and medial midfoot were rotating in opposite directions, but with the rearfoot complex rotating more than the medial midfoot. The angle–angle plot in
Figure 2 indicates the rearfoot complex was in an everted position and inverting, while the medial midfoot was in an everted position and everting.
At 76% stance, the PHP group coupling angle of 264.2° is very close to “rotation primarily of the distal joint with the proximal joint fixed (270°)”, indicating the medial midfoot was the primary joint rotating and the rearfoot was relatively fixed. Finally, the coupling angle of the uninjured groups at 76% stance of 312.1° is very close to “equal relative motion of the two joints in opposite directions (315°)”, indicating the near equal relative rotation of the rearfoot and medial midfoot in opposite directions. The difference in the rearfoot complex and medial midfoot frontal plane coupling occurred during the propulsion phase of the running stance phase, when the foot should be transitioning to a more supinated position. The greater midfoot eversion rotation relative to rearfoot inversion rotation in the PHP group could be an indicator of insufficient supination due to the degenerative changes in the plantar fascia.
Because this is the first study to utilize SPM to examine foot joint coupling in this population during running, the results cannot be directly compared to previous plantar heel pain gait studies. The only previous studies investigating the effect of plantar heel pain on running gait included a discrete analysis of the stance phase range of motion using the same cohort of runners as the current study [
17], and the study by Wiegand et al. [
18]. In the Pazhooman et al. [
17] study, the runners with PHP demonstrated increased lateral midfoot eversion ROM during the early stance, which may be consistent with a decreased ability to control foot pronation in the early–mid stance. Interestingly, the difference identified between the groups using SPM to investigate coupling between adjacent joints was also in the frontal plane; however, it did not involve the lateral midfoot and occurred in the propulsion phase vs. early stance. These differences suggest that discrete single-joint ROM analysis and SPM analysis may detect different characteristics of plantar heel pain. A strength of SPM analysis is that it can detect significant differences anywhere in the time series versus at predetermined events (e.g., peaks) or within predetermined periods (e.g., early stance). Wiegand et al. [
18] did not report any significant differences in sagittal or frontal plane forefoot, midfoot, or ankle peak angles or ROM during stances between runners with plantar heel pain and uninjured runners. In addition to the difference in the statistical analysis techniques utilized, the inclusion criteria (symptoms within the past two weeks vs. for a minimum of six weeks), footwear (participant’s personal running shoe vs. standardized sandal), and marker placement (on participant’s running shoe vs. on participant’s skin) may have contributed to the inconsistent results between the studies.
The only previous study to investigate joint coupling in individuals with plantar heel pain was a discrete analysis that reported a greater number of anti-phase movements between the rearfoot complex and medial forefoot joints in the frontal plane in uninjured individuals compared to individuals with PHP during the stance phase of walking gait [
20]. The results of the Chang et al. [
20] study and those of the current study cannot be compared due to difference in the study methodologies (discrete vs. continuous, walking gait vs. running gait). With respect to gait type, it is possible that PHP may affect foot function differently during walking compared to running due to the increased forces and/or decreased time during stances for the foot to accomplish its various functions during running. The likelihood that the results of the effect on running may not be generalizable to walking, and vice-versa, is supported by a previous study that investigated the effect of medial tibial stress syndrome (MTSS) on foot function during walking and running [
34]. This study found that the effect of MTSS on hindfoot and forefoot motion, compared to an uninjured group, differed between walking and running gait.
Before drawing conclusions regarding this study, several limitations should be considered. First, to minimize variability due to running speed, all runners ran at a fixed speed (4 m/s ± 10%). Although the running speed range is common for healthy adults, it may not have represented every runner’s preferred speed, which could influence their foot kinematics. Second, to accommodate multi-segment foot marker placement and eliminate variability that could have been caused by differing footwear, all participants wore the same style sandal (Maui and Sons, Pacific Palisades, CA, USA). As a result, the foot kinematics in the sandal may not be generalizable to the foot coupling kinematics that occur in traditional running shoes. It will be important for future studies to investigate if varying degrees of footwear support (e.g., minimalist vs. motion control) influence foot coupling during running gait in patients with PHP. Third, this study only included young adults, limiting the generalizability of the findings to other age groups. Fourth, all the runners in the current study were rearfoot strikers. Thus, the results may not be generalizable to runners with forefoot strike patterns [
35,
36]. Fifth, to have sufficient statistical power for the SPM analyses, the current analysis combined male and female runners in the PHP and uninjured groups. However, recent studies have identified sex differences in foot kinematics in both healthy [
37] and injured [
17,
38] individuals. Thus, it will be important for future studies to explore a potential interaction between sex and group (uninjured vs. PHP) on foot joint coupling during running gait. Sixth, the current study was sufficiently powered to identify large effect sizes but may not have been able to identify moderate effect sizes, which may also be clinically relevant. Lastly, the current study was a retrospective study; therefore, whether the observed differences in foot function are a cause or a consequence of plantar heel pain cannot be determined.