Comprehensive Management of Odontogenic Myxofibroma in the Mandible: A Four-Year Follow-Up Case Report with a Review of Differential Diagnosis and Treatment Approaches
Abstract
1. Introduction
2. Case Report
2.1. Examination
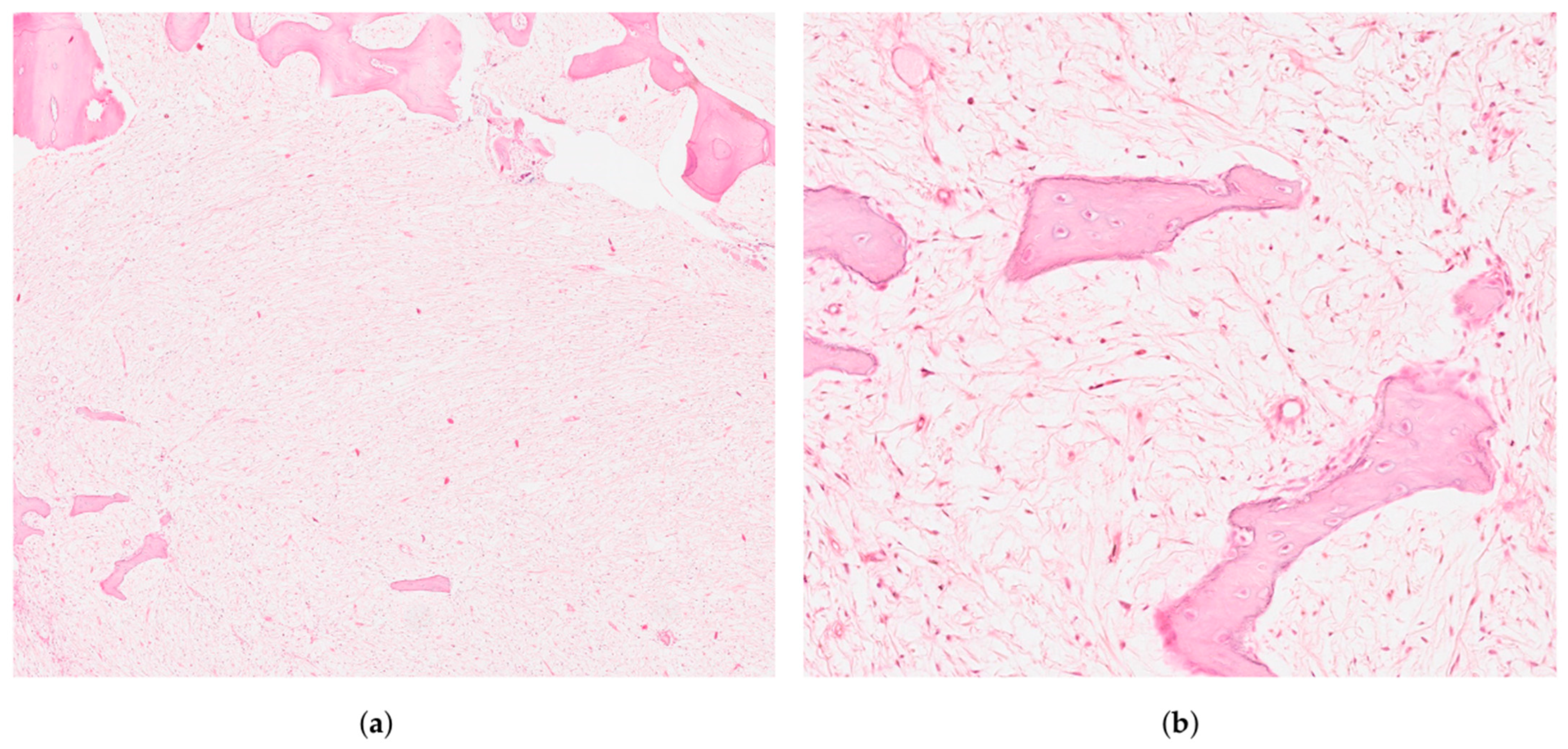
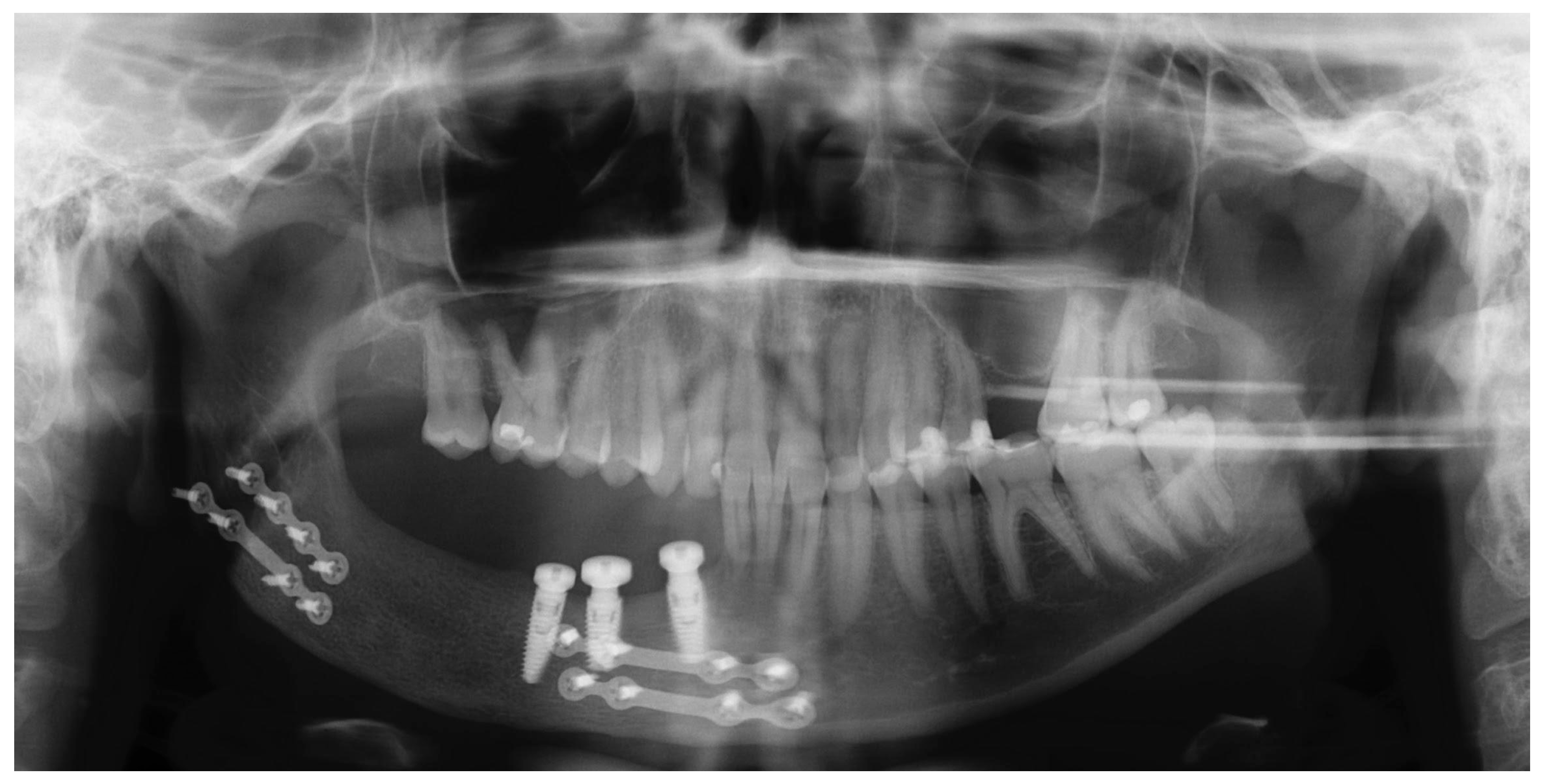
2.2. Treatment Procedures and Histopathological Results
2.3. Postoperative Care
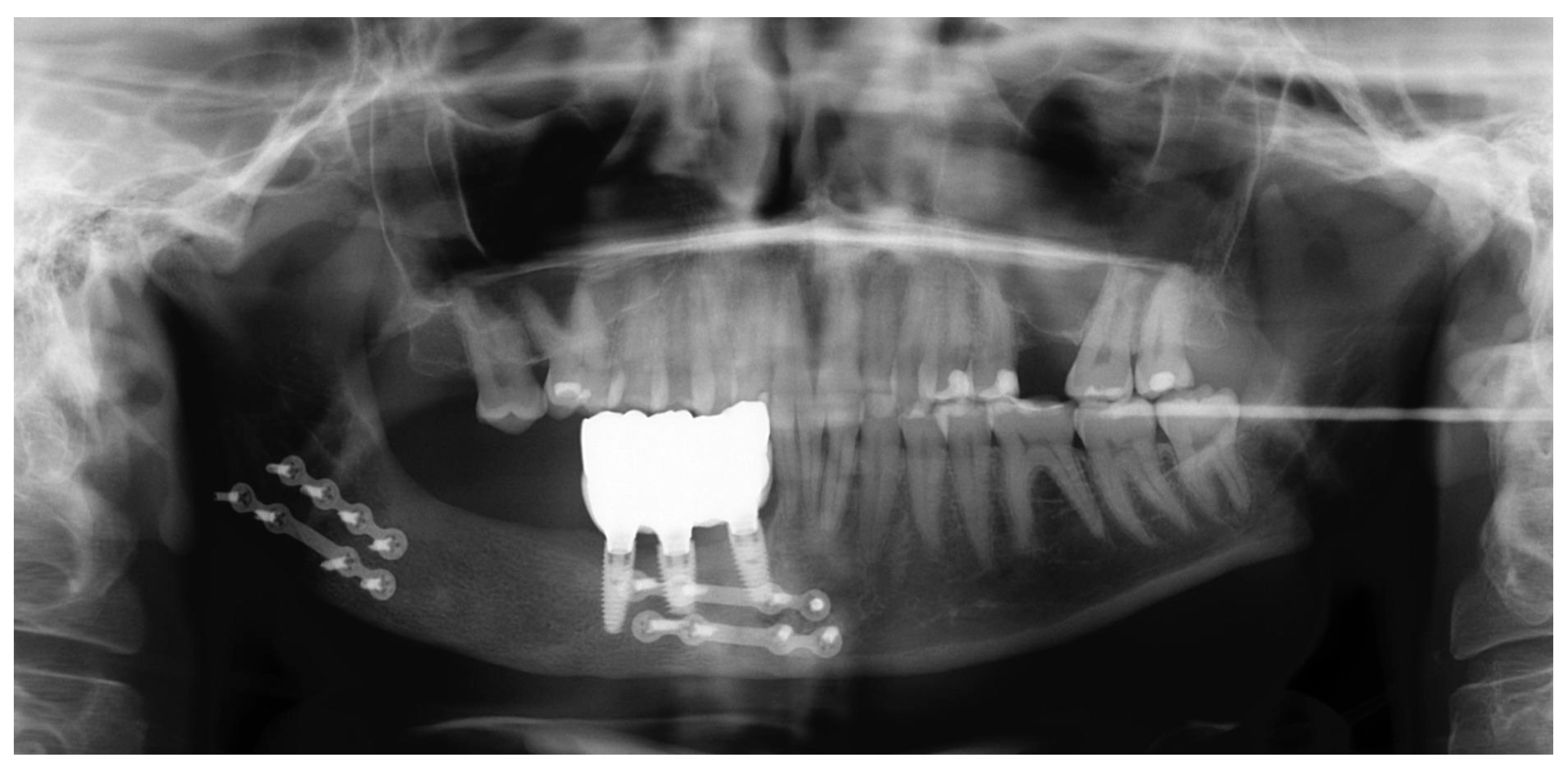
2.4. Follow-Ups
3. Discussion
3.1. Diagnostic Features with Differential Diagnoses
- Ameloblastoma: Features islands of odontogenic epithelium resembling the enamel organ.
- Chondromyxoid fibroma: Comprises lobules of chondroid and myxoid tissue with spindle cells, commonly affecting long bones.
- Osteosarcoma: Defined by the production of malignant osteoid by atypical osteoblasts and a characteristic “sunburst” radiographic pattern [11].
3.2. Management Methods
3.2.1. Conservative Treatment
3.2.2. Radical Surgical Resection
3.2.3. Reconstruction and Graft Considerations
3.3. Outcomes and Recurrence Prevention
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Asnani, P.; Ali, S.; Odedra, S.; Pillai, J.; Jayasheel, N.; Jadeja, R. A comprehensive analysis of odontogenic tumors according to recent WHO (2022) classification: An institution-based retrospective study. J. Oral Maxillofac. Pathol. 2024, 28, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Simon, E.N.; Merkx, M.A.; Vuhahula, E.; Ngassapa, D.; Stoelinga, P.J.W. Odontogenic myxoma: A clinicopathological study of 33 cases. Int. J. Oral Maxillofac. Surg. 2004, 33, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Thitiyuk, C.; Patchanee, S.; Chaiprakit, N. Odontogenic Myxofibroma: A Case Report. J. Int. Dent. Med. Res. 2022, 15, 820–823. [Google Scholar]
- Ghimire, B.; Miya, N.; Rajbhandari, R.; Verma, L. Segmental resection with primary reconstruction using patient- specific implant for odontogenic fibromyxoma: An illustrative rare case from Nepal. Int. J. Surg. Case Rep. 2024, 121, 109972. [Google Scholar] [CrossRef] [PubMed]
- Infante-Cossío, P.; Martínez-de-Fuentes, R.; García-Perla-García, A.; Jiménez-Castellanos, E.; Gómez-Izquierdo, L. Myxofibroma of the maxilla: Reconstruction with iliac crest graft and dental implants after tumor resection. Med. Oral Patol. Oral Cir. Bucal 2011, 16, e532–e536. [Google Scholar] [CrossRef] [PubMed]
- Çelebioğlu Genç, B.G.; Orhan, K. Odontogenic fibromyxoma: A case report in myasthenia gravis patient and review of the literature. Int. J. Surg. Case Rep. 2022, 96, 107306. [Google Scholar] [CrossRef] [PubMed]
- Meleti, M.; Giovannacci, I.; Corradi, D.; Manfredi, M.; Merigo, E.; Bonanini, M.; Vescovi, P. Odontogenic myxofibroma: A concise review of the literature with emphasis on the surgical approach. Med. Oral Patol. Oral Cir. Bucal 2015, 20, e1–e6. [Google Scholar] [CrossRef] [PubMed]
- Leiser, Y.; Abu-El-Naaj, I.; Peled, M. Odontogenic myxoma—A case series and review of the surgical management. J. Cranio-Maxillofac. Surg. 2009, 37, 206–209. [Google Scholar] [CrossRef] [PubMed]
- Chiapasco, M.; Colletti, G.; Romeo, E.; Zaniboni, M.; Brusati, R. Long-term results of mandibular reconstruction with autogenous bone grafts and oral implants after tumor resection. Clin. Oral Implant. Res. 2008, 19, 1074–1080. [Google Scholar] [CrossRef] [PubMed]
- Górka, T.; Stypułkowska, J. Peculiarities of oral cancers in Poland: A review of the literature. Arch. Euromedica 2024, 4, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Barnes, L.; Eveson, J.W.; Reichart, P.; Sidransky, D. (Eds.) Pathology and Genetics of Head and Neck Tumours, Proceeding of the Reflects the Views of a Working Group That Convened for an Editorial and Consensus Conference in Lyon, France, 16–19 July 2003; Reprinted; IARC Press: Lyon, France, 2007. [Google Scholar]
- Sweeney, J.; Laverick, S. Odontogenic Myxofibroma—A Rare Case Report. Int. J. Med. Case Rep. 2020, 5, 1–3. [Google Scholar]
- Poudel, P.; Bajracharya, B.; Bhattacharyya, S.; Bajracharya, D.; Singh, S.; Pokhrel, P.; Desar, B. Odontogenic myxofibroma—Report of a rare entity. J. Pathol. Nepal. 2016, 6, 1043–1045. [Google Scholar] [CrossRef]
- Lo Muzio, L.; Nocini, P.; Favia, G.; Procaccini, M.; Mignogna, M.D. Odontogenic myxoma of the jaws: A clinical, radiologic, immuno-histochemical, and ultrastructural study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1996, 82, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Pogrel, M.A.; Podlesh, S.; Anthony, J.P.; Alexander, J. A comparison of vascularized and nonvascularized bone grafts for reconstruction of mandibular continuity defects. J. Oral Maxillofac. Surg. 1997, 55, 1200–1206. [Google Scholar] [CrossRef] [PubMed]
- González García, R.; Rodríguez Campo, F.J.; Naval Gías, L.; Muñoz Guerra, M.F.; Sastre Pérez, J.; Díaz González, F.J. Mandibular odontogenic myxoma. Reconstructive considerations by means of the vascularized fibular free flap. Med. Oral Patol. Oral Cir. Bucal 2006, 11, 531–535. [Google Scholar]
- Khayat, S.; Urmeneta, Á.S.; Moure, B.G.; Fernández Acosta, D.; Benito Anguita, M.; López López, A.; Verdaguer Martín, J.J.; Navarro Cuéllar, I.; Falahat, F.; Navarro Cuéllar, C. Reconstruction of Segmental Mandibular Defects with Double-Barrel Fibula Flap and Osseo-Integrated Implants: A Systematic Review. J. Clin. Med. 2024, 13, 3547. [Google Scholar] [CrossRef] [PubMed]
- Garajei, A.; Kheradmand, A.A.; Miri, S.R.; Emami, A. A retrospective study on mandibular reconstruction using iliac crest free flap. Ann. Med. Surg. 2021, 66, 102354. [Google Scholar] [CrossRef] [PubMed]
- Darwich, K.; Ismail, M.B.; Al-Mozaiek, M.Y.A.S.; Alhelwani, A. Reconstruction of mandible using a computer-designed 3D-printed patient-specific titanium implant: A case report. Oral Maxillofac. Surg. 2021, 25, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Reddy, G.S.P.; Kumar, B.S.; Muppa, R.; Regonda, S.K.; TVS, H.K. Odontogenic Fibromyxoma of Maxilla: A Rare Case Report. Case Rep. Dent. 2013, 345479, 2013. [Google Scholar]








| Aspect | Details | References |
|---|---|---|
| Radiographic | “Soap-bubble”, “ground-glass” or “tennis racquet strings” patterns complicating the diagnosis | [4,12,14] |
| Histology and Odontogenic Epithelium | Spindle and stellate-shaped cells in a myxoid stroma with prominent collagen fibres. Possible remnants of odontogenic epithelium, aiding differentiation from odontogenic myxoma | [4,13,14] |
| Recurrence Potential | High due to local invasion into cancellous bone and absence of encapsulation | [2,14] |
| Feature | Odontogenic Myxofibroma (OMF) | Ameloblastoma | Chondromyxoid Fibroma | Low-Grade Myxofibrosarcoma | Osteosarcoma |
|---|---|---|---|---|---|
| ICD-O Code | 9262/0 (odontogenic myxoma) | 9310/0 (benign ameloblastoma) | 9240/0 (benign chondromyxoid fibroma) | 8830/3 (myxofibrosarcoma, malignant) | 9180/3 (malignant osteosarcoma) |
| Age Group | 20s to 40s | 30s to 60s | Adolescents and young adults | Middle-aged to older adults | Adolescents and young adults |
| Gender Predilection | Slight female predominance | Equal distribution | Slight male predominance | Slight male predominance | Slight male predominance |
| Common Location | Mandible | Mandible | Long bones; rare in jaws | Extremities; rare in jaws | Metaphysis of long bones; jaw involvement rare |
| Clinical Presentation | Painless swelling, facial asymmetry | Painless swelling, possible ulceration | Localised pain, swelling | Slow-growing mass, may be painless | Painful swelling, rapid growth |
| Radiographic Appearance | Multilocular radiolucency with “soap-bubble” or “honeycomb” pattern | Multilocular radiolucency, “soap-bubble” appearance | Eccentric, radiolucent lesion with cortical expansion | Ill-defined margins, may show soft tissue mass | Mixed radiolucent–radiopaque lesion, “sunburst” pattern |
| Histopathology | Spindle and stellate cells in myxoid stroma with collagen fibres | Islands of odontogenic epithelium resembling enamel organ | Lobules of chondroid and myxoid tissue with spindle cells | Spindle-shaped cells in myxoid matrix, mild atypia | Malignant osteoid production by atypical osteoblasts |
| Treatment Approach | Surgical resection with clear margins; recurrence possible with conservative treatment | Surgical resection; high recurrence rate if not completely excised | Curettage or resection; recurrence possible | Wide surgical excision; may require adjuvant therapy | Neoadjuvant chemotherapy followed by surgical resection; poor prognosis if untreated |
| Reconstruction Method | Advantages | Limitations |
|---|---|---|
| Free vascularised fibula graft (FVFG) [16] |
|
|
| Double-Barrel Fibula Flap (DBFF) [17] |
|
|
| Iliac crest free flap [18] |
|
|
| Patient-specific implants (PSIs) [19] |
|
|
| Treatment Approach | Details | References |
|---|---|---|
| Conservative Management | Smaller lesions: Curettage and simple enucleation, possibly with peripheral osteotomy. | [2,14] |
| Radical Resection | Larger lesions: Segmental resection with 1.5–2 cm osseous margins to minimise recurrence. | [4,15,16] |
| Reconstruction | Primary mandibular reconstruction with iliac crest bone graft. | [18] |
| Graft Considerations | Adequate periosteum coverage to promote vascularisation and reduce resorption. | [9] |
| Dental Rehabilitation | Dental implants and implant-supported prostheses reduce graft resorption and improve outcomes. | [9,18] |
| Timing for Implants | Delay between the bone graft and implant placement: 4–6 months to ensure graft consolidation and stability. | [9,18] |
| Reference | Age/Gender | Localisation | Treatment | Follow-Up | Recurrence |
|---|---|---|---|---|---|
| Current case | 35/F | Posterior segment of the mandible | Resection | 4 years | No |
| Thitiyuk et al. [3] | 50/M | Anterior segment of the mandible | Enucleation and curettage | 1 year | Not reported |
| Sweeney et al. [12] | 59/F | Posterior segment of the maxilla | Enucleation | Not reported | Not reported |
| Çelebioğlu et al. [6] | 29/F | Anterior region of the mandible | Enucleation | 3 years | No |
| Poudel et al. [13] | 53/F | Posterior segment of the mandible | Resection | Not reported | Not reported |
| Siva Prasad Reddy et al. [20] | 12/F | Left maxilla | Curettage and enucleation | Not reported | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wójcik, J.; Yefanova, L.; Nijakowski, K.; Bednarek-Rajewska, K.; Osmola, K.; Okła, M. Comprehensive Management of Odontogenic Myxofibroma in the Mandible: A Four-Year Follow-Up Case Report with a Review of Differential Diagnosis and Treatment Approaches. Oral 2025, 5, 39. https://doi.org/10.3390/oral5020039
Wójcik J, Yefanova L, Nijakowski K, Bednarek-Rajewska K, Osmola K, Okła M. Comprehensive Management of Odontogenic Myxofibroma in the Mandible: A Four-Year Follow-Up Case Report with a Review of Differential Diagnosis and Treatment Approaches. Oral. 2025; 5(2):39. https://doi.org/10.3390/oral5020039
Chicago/Turabian StyleWójcik, Joanna, Liliia Yefanova, Kacper Nijakowski, Katarzyna Bednarek-Rajewska, Krzysztof Osmola, and Maciej Okła. 2025. "Comprehensive Management of Odontogenic Myxofibroma in the Mandible: A Four-Year Follow-Up Case Report with a Review of Differential Diagnosis and Treatment Approaches" Oral 5, no. 2: 39. https://doi.org/10.3390/oral5020039
APA StyleWójcik, J., Yefanova, L., Nijakowski, K., Bednarek-Rajewska, K., Osmola, K., & Okła, M. (2025). Comprehensive Management of Odontogenic Myxofibroma in the Mandible: A Four-Year Follow-Up Case Report with a Review of Differential Diagnosis and Treatment Approaches. Oral, 5(2), 39. https://doi.org/10.3390/oral5020039







