Effect of Abutment Type and Tightening Sequence on Torque Maintenance Capacity after Mechanical Cycling in Splinted Implant-Supported Restorations
Abstract
:1. Introduction
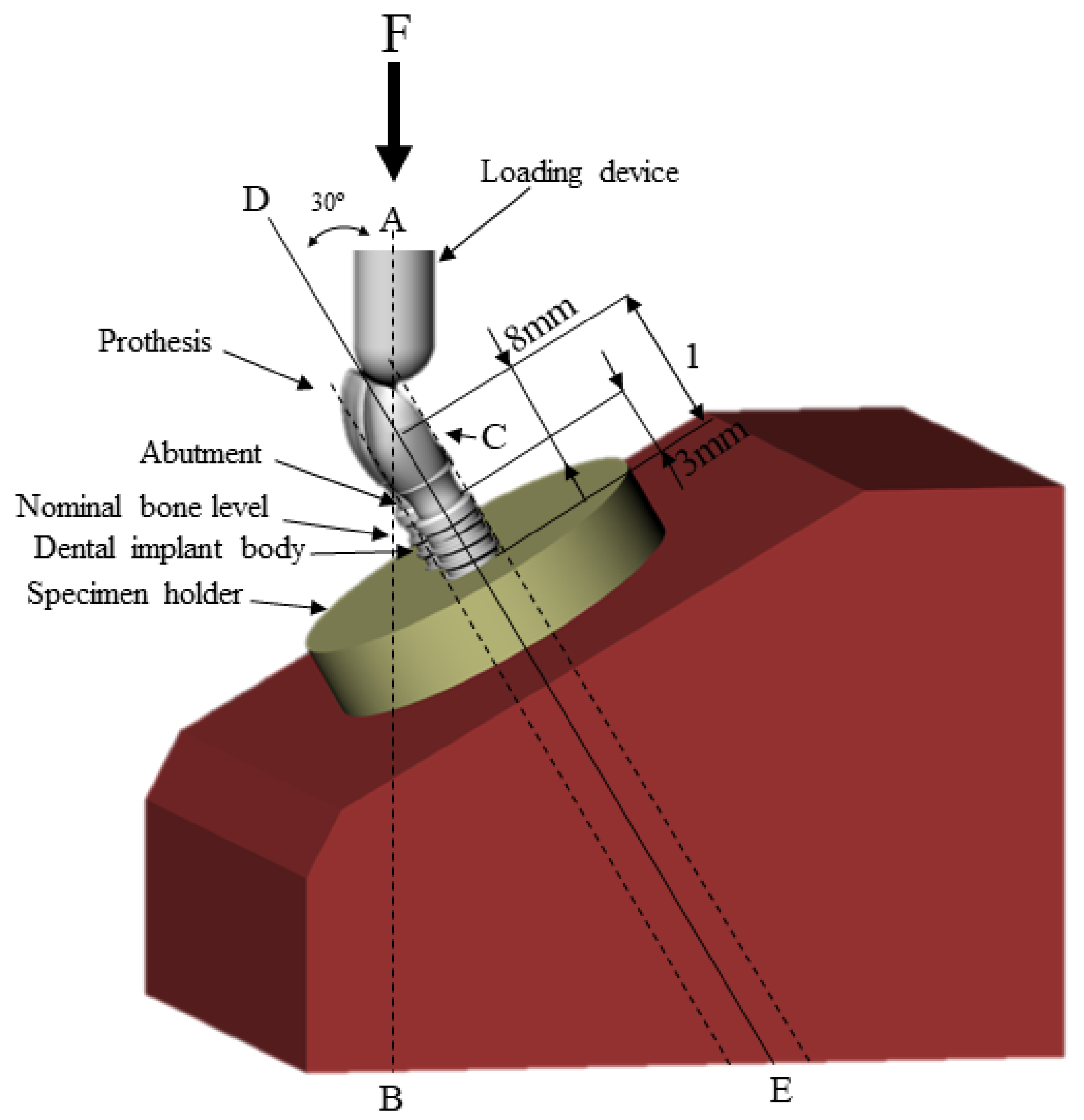
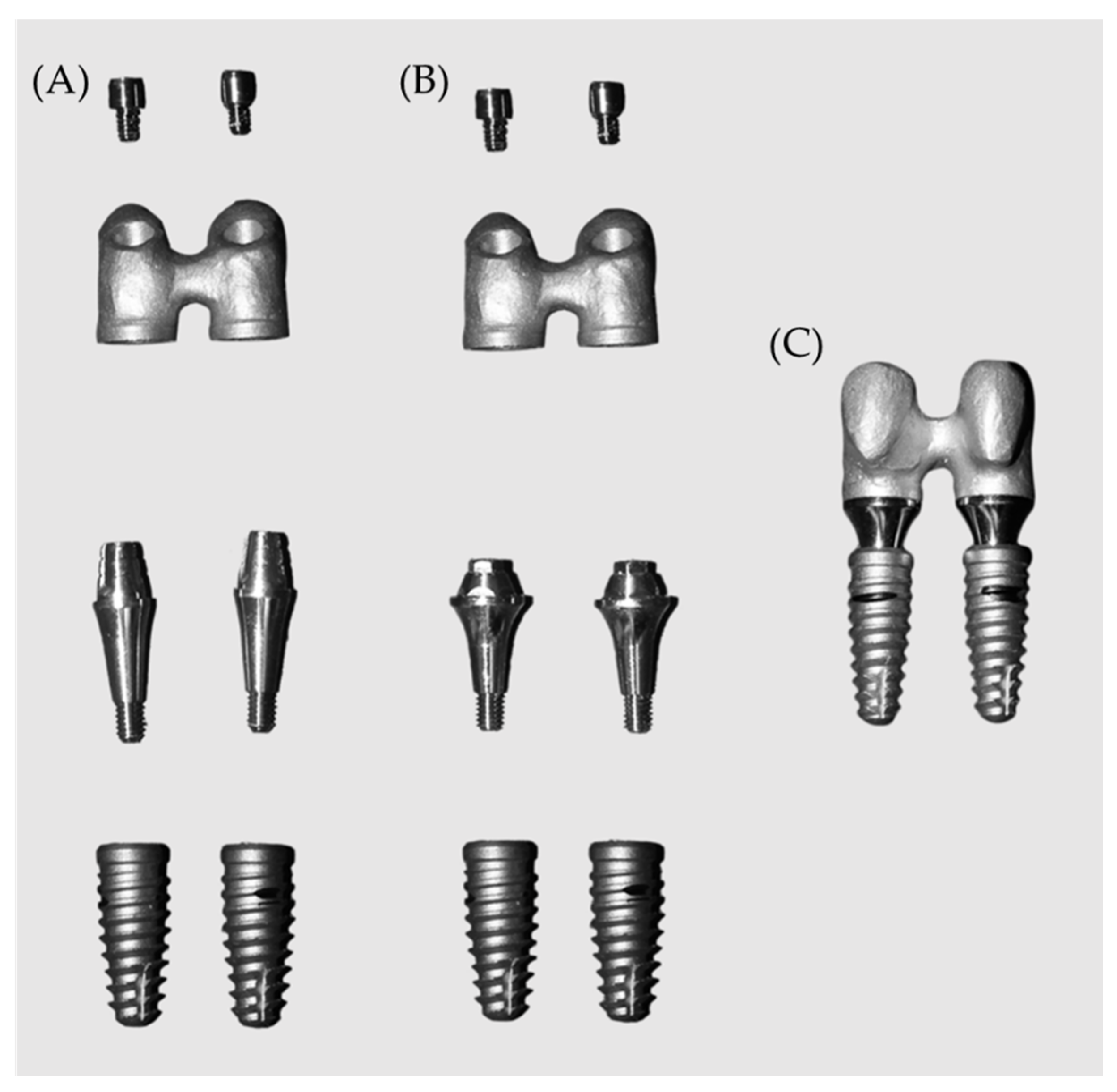
2. Materials and Methods
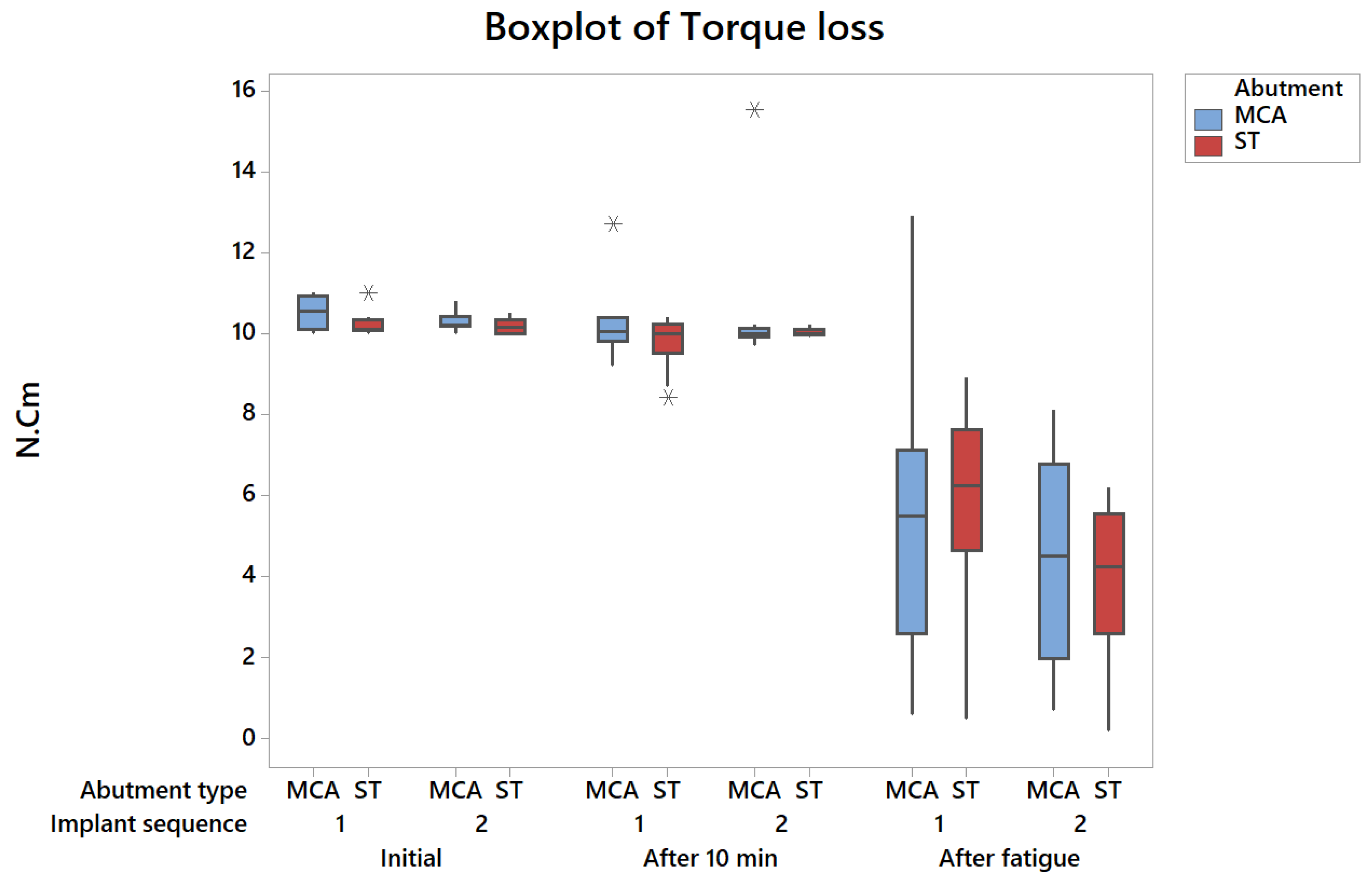
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Silveira, M.; Campaner, L.; Bottino, M.; Nishioka, R.; Borges, A.; Tribst, J.P. Influence of the dental implant number and load direction on stress distribution in a 3-unit implant-supported fixed dental prosthesis. Dent. Med. Probl. 2021, 58, 69–74. [Google Scholar] [CrossRef]
- Tribst, J.; Piva, A.D.; da Silva-Concílio, L.; Ausiello, P.; Kalman, L. Influence of Implant-Abutment Contact Surfaces and Prosthetic Screw Tightening on the Stress Concentration, Fatigue Life and Microgap Formation: A Finite Element Analysis. Oral 2021, 1, 88–101. [Google Scholar] [CrossRef]
- Bernardes, S.R.; Mattos, M.D.G.C.D.; Hobkirk, J.; Ribeiro, R.F. Loss of preload in screwed implant joints as a function of time and tightening/untightening sequences. Int. J. Oral Maxillofac. Implant. 2014, 29, 89–96. [Google Scholar] [CrossRef] [Green Version]
- Adolfi, D.; Tribst, J.; Borges, A.; Bottino, M.A. Torque Maintenance Capacity, Vertical Misfit, Load to Failure, and Stress Concentration of Zirconia Restorations Cemented or Notched to Titanium Bases. Int. J. Oral Maxillofac. Implant. 2020, 35, 357–365. [Google Scholar] [CrossRef]
- Tonin, B.S.H.; He, Y.; Ye, N.; Chew, H.P.; Fok, A. Effects of tightening torque on screw stress and formation of implant-abutment mi-crogaps: A finite element analysis. J. Prosthet. Dent. 2021. [Google Scholar] [CrossRef]
- De Carvalho, B.A.C.; Vedovatto, E.; De Carvalho, P.S.P.; Mazaro, J.V.Q.; Falcón-Antenucci, R.M. Effect of Mechanical Cycling on Screw Torque in External Hexagon Implants with and without Platform Switching. Braz. Dent. J. 2015, 26, 284–287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gehrke, S.A.; Pereira, F.D.A. Changes in the Abutment-Implant Interface in Morse Taper Implant Connections After Mechanical Cycling: A Pilot Study. Int. J. Oral Maxillofac. Implant. 2014, 29, 791–797. [Google Scholar] [CrossRef] [Green Version]
- Martins, C.M.; Ramos, E.V.; Kreve, S.; De Carvalho, G.A.P.; Franco, A.B.G.; De Macedo, L.G.S.; Silva, A.D.M.; Dias, S.C. Reverse torque evaluation in indexed and nonindexed abutments of Morse Taper implants in a mechanical fatigue test. Dent. Res. J. 2019, 16, 110–116. [Google Scholar] [CrossRef]
- Schmitt, C.M.; Nogueira-Filho, G.; Tenenbaum, H.C.; Lai, J.Y.; Brito, C.; Döring, H.; Nonhoff, J. Performance of conical abutment (Morse Taper) connection implants: A systematic review: Performance of Conical Implant-Abutment Connection Systems. J. Biomed. Mater. Res. A 2014, 102, 552–574. [Google Scholar] [CrossRef]
- Mishra, S.K.; Chowdhary, R.; Kumari, S. Microleakage at the Different Implant Abutment Interface: A Systematic Review. J. Clin. Diagn. Res. 2017, 11, ZE10–ZE15. [Google Scholar] [CrossRef]
- Thomé, G.; Torres Gomes, A.F.; de Moura, M.B.; Felippi, C.; Trojan, L.C. Evaluation of the mechanical reliability of different im-plant-abutment connections for single crowns according to the ISO 14801 fatigue test protocol. Int. J. Oral Maxillofac. Implant. 2021, 36, 47–54. [Google Scholar] [CrossRef]
- Varvara, G.; Sinjari, B.; Caputi, S.; Scarano, A.; Piattelli, M. The Relationship Between Time of Re-Tightening and Preload Loss of Abutment Screws for Two Different Implant Designs: An In-Vitro Study. J. Oral Implant. 2019, 46, 13–17. [Google Scholar] [CrossRef]
- Winkler, S.; Ring, K.; Ring, J.D.; Boberick, K.G. Implant Screw Mechanics and the Settling Effect: An Overview. J. Oral Implant. 2003, 29, 242–245. [Google Scholar] [CrossRef]
- Sakaguchi, R.L.; Borgersen, S.E. Nonlinear contact analysis of preload in dental implant screws. Int. J. Oral Maxillofac. Implant. 1995, 10, 295–302. [Google Scholar]
- Xu, Y.; Li, W.; Su, M. Clinical Assessment of Preload Maintenance in the Abutment Screws of Single Posterior Implants After 1 Month of Use. Int. J. Oral Maxillofac. Implant. 2021, 36, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.-S.; Han, J.-S.; Lim, Y.-J. Settling of abutments into implants and changes in removal torque in five different implant-abutment connections. Part 1: Cyclic loading. Int. J. Oral Maxillofac. Implant. 2014, 29, 1079–1084. [Google Scholar] [CrossRef] [Green Version]
- Huang, Y.; Wang, J. Mechanism of and factors associated with the loosening of the implant abutment screw: A review. J. Esthet. Restor. Dent. 2019, 31, 338–345. [Google Scholar] [CrossRef] [PubMed]
- Spazzin, A.O.; Henrique, G.E.P.; de Arruda Nóbilo, M.A.; Consani, R.L.X.; Correr-Sobrinho, L.; Mesquita, M.F. Effect of retorque on loos-ening torque of prosthetic screws under two levels of fit of implant-supported dentures. Braz. Dent. J. 2010, 21, 12–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silva, T.S.D.O.; Alencar, S.M.M.; Valente, V.D.S.; de Moura, C.D.V.S. Effect of internal hexagonal index on removal torque and tensile removal force of different Morse taper connection abutments. J. Prosthet. Dent. 2017, 117, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.; Melo, R.; Borges, A.; Souza, R.; Bottino, M.A. Mechanical Behavior of Different Micro Conical Abutments in Fixed Prosthesis. Int. J. Oral Maxillofac. Implant. 2018, 33, 1199–1205. [Google Scholar] [CrossRef]
- Gomes, A.; Tiossi, R.; Faria, A.C.L.; Rodrigues, R.C.S.; Ribeiro, R.F. Torque loss under mechanical cycling of long-span zirconia and titanium-cemented and screw-retained implant-supported CAD/CAM frameworks. Clin. Oral Implant. Res. 2013, 25, 1395–1402. [Google Scholar] [CrossRef] [PubMed]
- Pardal-Peláez, B.; Montero, J. Preload loss of abutment screws after dynamic fatigue in single implant-supported restorations. A systematic review. J. Clin. Exp. Dent. 2017, 9, e1355–e1361. [Google Scholar] [CrossRef] [PubMed]
- Theoharidou, A.; Petridis, H.P.; Tzannas, K.; Garefis, P. Abutment screw loosening in single-implant restorations: A systematic review. Int. J. Oral Maxillofac. Implant. 2008, 23, 681–690. [Google Scholar]
- Tribst, J.P.M.; Rodrigues, V.A.; Borges, A.L.S.; de Lima, D.R.; Nishioka, R.S. Validation of a Simplified Implant-Retained Cantilever Fixed Prosthesis. Implant. Dent. 2018, 27, 49–55. [Google Scholar] [CrossRef] [PubMed]
| Initial Torque | DF | SQ | MS | F Value | p-Value |
|---|---|---|---|---|---|
| Implant sequence | 1 | 0.19600 | 0.19600 | 2.28 | 0.140 |
| Abutment type | 1 | 0.36100 | 0.36100 | 4.19 | 0.068 |
| Implant sequence*abutment type | 1 | 0.08100 | 0.08100 | 0.94 | 0.338 |
| Error | 36 | 3.09800 | 0.08606 | ||
| Total | 39 | 3.73600 |
| After 10 min | DF | SQ | MS | F Value | p-Value |
|---|---|---|---|---|---|
| Implant sequence | 1 | 0.7023 | 0.70225 | 0.64 | 0.431 |
| Abutment type | 1 | 2.2563 | 2.25625 | 2.04 | 0.162 |
| Implant sequence*abutment type | 1 | 0.0123 | 0.01225 | 0.01 | 0.917 |
| Error | 36 | 39.7890 | 1.10525 | ||
| Total | 39 | 42.7598 |
| Torque after Fatigue | DF | SQ | MS | F Value | p-Value |
|---|---|---|---|---|---|
| Implant sequence | 1 | 27.556 | 27.5560 | 3.72 | 0.062 |
| Abutment type | 1 | 0.036 | 0.0360 | 0.00 | 0.945 |
| Implant sequence*abutment type | 1 | 1.369 | 1.3690 | 0.19 | 0.670 |
| Error | 36 | 266.378 | 7.3994 | ||
| Total | 39 | 295.339 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakano, L.J.N.; Gomes, L.C.L.; de Queiroz, T.S.; Paes-Junior, T.J.d.A. Effect of Abutment Type and Tightening Sequence on Torque Maintenance Capacity after Mechanical Cycling in Splinted Implant-Supported Restorations. Oral 2021, 1, 300-306. https://doi.org/10.3390/oral1040029
Nakano LJN, Gomes LCL, de Queiroz TS, Paes-Junior TJdA. Effect of Abutment Type and Tightening Sequence on Torque Maintenance Capacity after Mechanical Cycling in Splinted Implant-Supported Restorations. Oral. 2021; 1(4):300-306. https://doi.org/10.3390/oral1040029
Chicago/Turabian StyleNakano, Leonardo Jiro Nomura, Laís Carolina Landim Gomes, Talita Suelen de Queiroz, and Tarcisio José de Arruda Paes-Junior. 2021. "Effect of Abutment Type and Tightening Sequence on Torque Maintenance Capacity after Mechanical Cycling in Splinted Implant-Supported Restorations" Oral 1, no. 4: 300-306. https://doi.org/10.3390/oral1040029
APA StyleNakano, L. J. N., Gomes, L. C. L., de Queiroz, T. S., & Paes-Junior, T. J. d. A. (2021). Effect of Abutment Type and Tightening Sequence on Torque Maintenance Capacity after Mechanical Cycling in Splinted Implant-Supported Restorations. Oral, 1(4), 300-306. https://doi.org/10.3390/oral1040029





