Mechanical Properties of Direct Composite Resins and CAD/CAM Composite Blocks
Abstract
1. Introduction
2. Materials and Methods
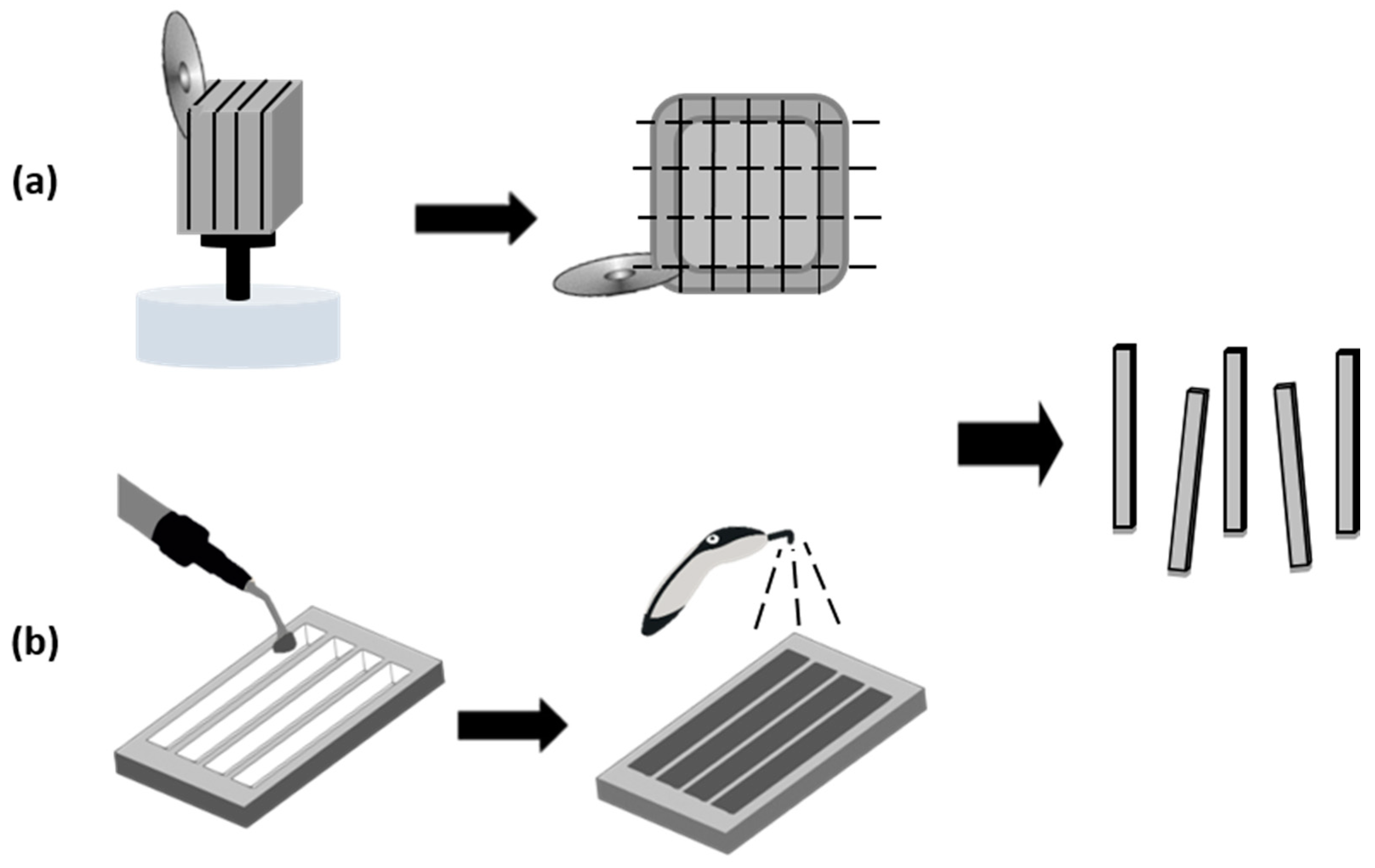
2.1. Sample Preparation
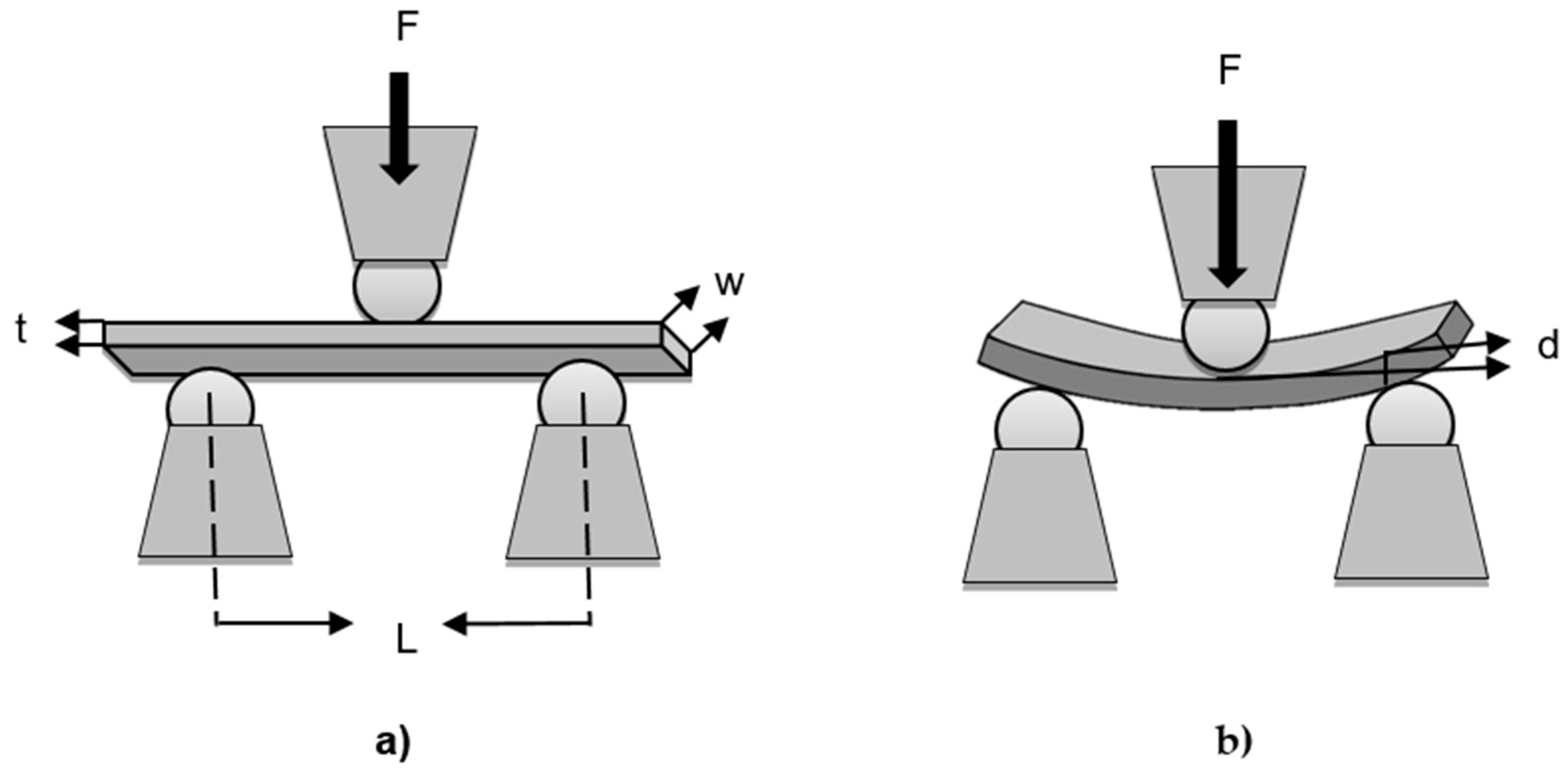
2.2. Three-Point Bending Flexural Test
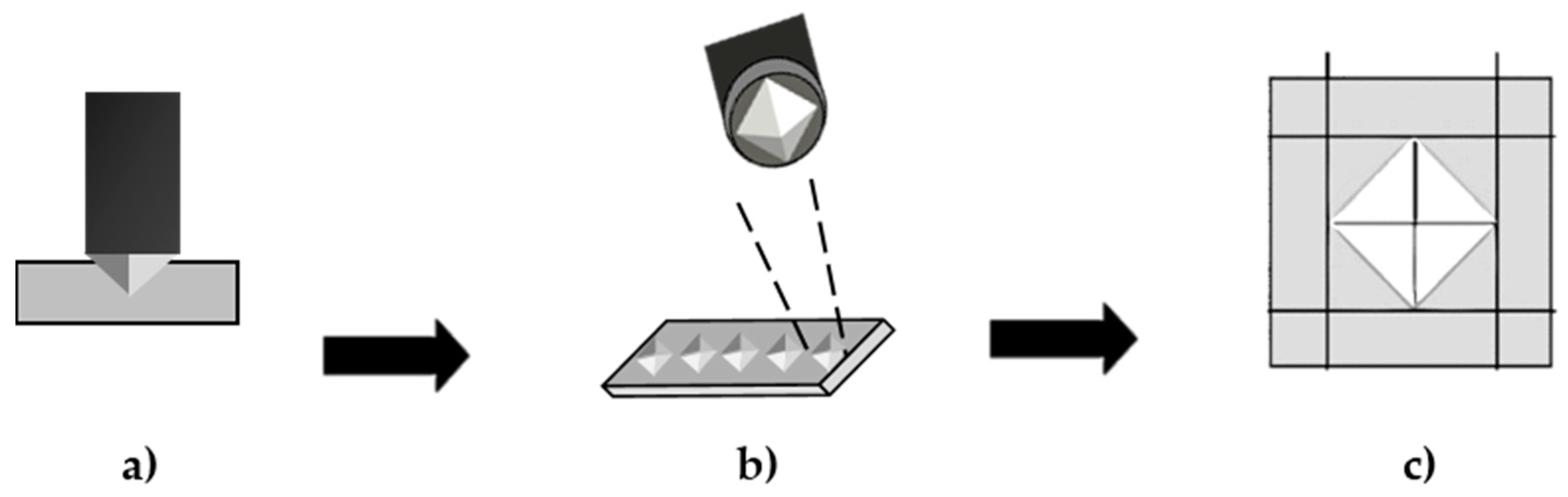
2.3. Vickers Microhardness Measurement
2.4. Statistical Analysis
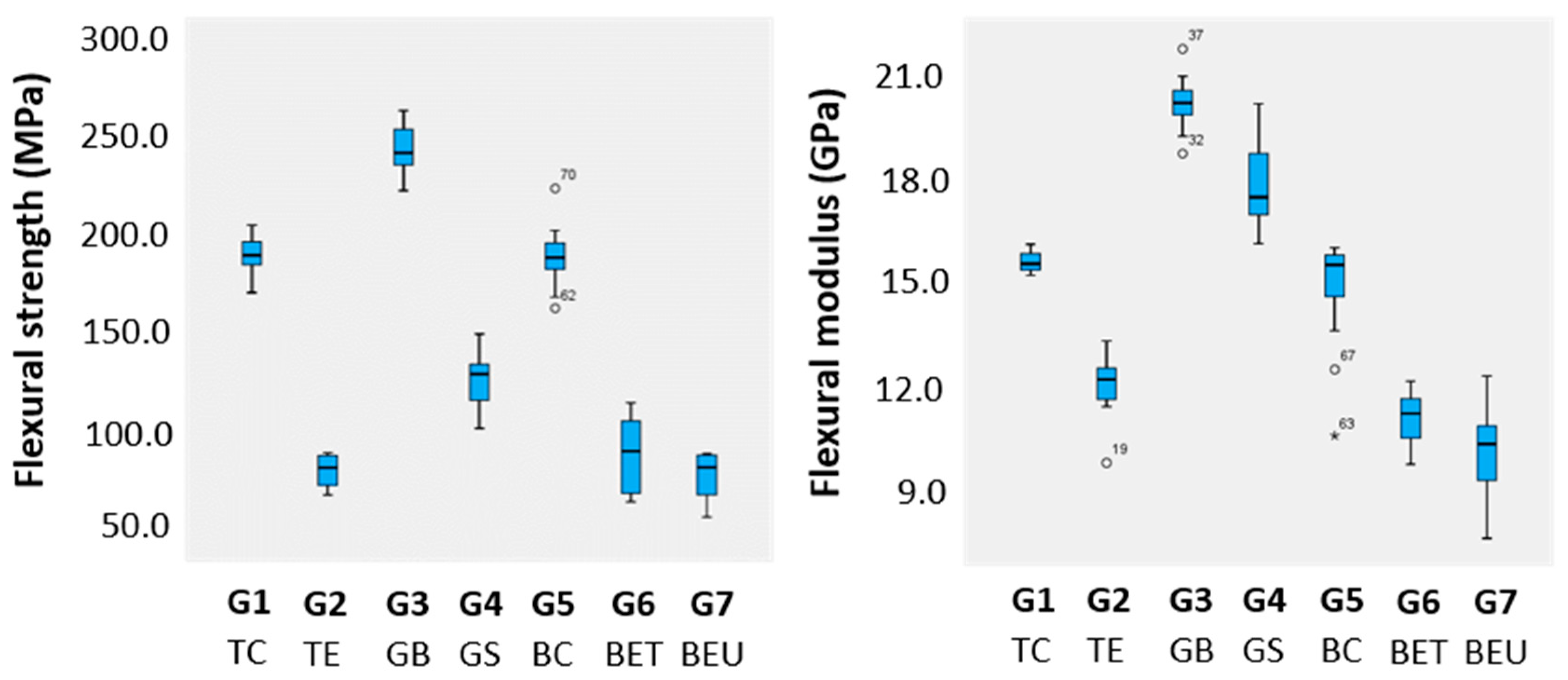
3. Results
4. Discussion
5. Conclusions
- The mean flexural strength of the RCBs (BC, GB, and TC) was significantly higher than all direct composite resins tested (BET, BEU, GS, and TEC).
- The mean flexural modulus of the RCBs (BC, GB, TC) and the direct composite resin GS was significantly higher than the other direct composite resin tested (BET, BED, and TEC).
- The mean microhardness of the RCBs (BC, GB, TC) and the direct resin GS was significantly higher than the other direct composite resin tested (BET, BED, and TEC).
- The RCB and the direct resin composite evaluated in this study with better mechanical properties were Grandio blocs and GrandioSO, respectively.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, L.; D’Alpino, P.H.; Lopes, L.G.; Pereira, J.C. Mechanical properties of dental restorative materials: Relative contribution of laboratory tests. J. Appl. Oral Sci. 2003, 11, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Oouchi, H.; Takamizawa, T.; Tamura, T.; Ishii, R.; Tsujimoto, A.; Miyazaki, M.; Kitahara, N. Flexural properties and wear behavior of computer-aided design/computer-aided manufacturing resin blocks. Dent. Mater. J. 2021, 40, 979–985. [Google Scholar] [CrossRef] [PubMed]
- Okada, R.; Asakura, M.; Ando, A.; Kumano, H.; Ban, S.; Kawai, T.; Takebe, J. Fracture strength testing of crowns made of CAD/CAM composite resins. J. Prosthodont. Res. 2018, 62, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Ilie, N.; Hilton, T.J.; Heintze, S.D.; Hickel, R.; Watts, D.C.; Silikas, N.; Stansbury, J.W.; Cadenaro, M.; Ferracane, J.L. Academy of Dental Materials guidance-Resin composites: Part I-Mechanical properties. Dent. Mater. 2017, 33, 880–894. [Google Scholar] [CrossRef]
- Egilmez, F.; Ergun, G.; Cekic-Nagas, I.; Vallittu, P.K.; Lassila, L.V.J. Does artificial aging affect mechanical properties of CAD/CAM composite materials. J. Prosthodont. Res. 2018, 62, 65–74. [Google Scholar] [CrossRef]
- Zhi, L.; Bortolotto, T.; Krejci, I. Comparative in vitro wear resistance of CAD/CAM composite resin and ceramic materials. J. Prosthet. Dent. 2016, 115, 199–202. [Google Scholar] [CrossRef] [PubMed]
- Mainjot, A.K.; Dupont, N.M.; Oudkerk, J.C.; Dewael, T.Y.; Sadoun, M.J. From Artisanal to CAD-CAM Blocks: State of the Art of Indirect Composites. J. Dent. Res. 2016, 95, 487–495. [Google Scholar] [CrossRef] [PubMed]
- Papathanasiou, I.; Kamposiora, P.; Dimitriadis, K.; Papavasiliou, G.; Zinelis, S. In vitro evaluation of CAD/CAM composite materials. J. Dent. 2023, 136, 104623. [Google Scholar] [CrossRef]
- Dirxen, C.; Blunck, U.; Preissner, S. Clinical performance of a new biomimetic double network material. Open Dent. J. 2013, 7, 118–122. [Google Scholar] [CrossRef]
- Lim, K.; Yap, A.U.; Agarwalla, S.V.; Tan, K.B.; Rosa, V. Reliability, failure probability, and strength of resin-based materials for CAD/CAM restorations. J. Appl. Oral Sci. 2016, 24, 447–452. [Google Scholar] [CrossRef]
- Alamoush, R.A.; Sung, R.; Satterthwaite, J.D.; Silikas, N. The effect of different storage media on the monomer elution and hardness of CAD/CAM composite blocks. Dent. Mater. 2021, 37, 1202–1213. [Google Scholar] [CrossRef]
- Peumans, M.; Valjakova, E.B.; De Munck, J.; Mishevska, C.B.; Van Meerbeek, B. Bonding Effectiveness of Luting Composites to Different CAD/CAM Materials. J. Adhes. Dent. 2016, 18, 289–302. [Google Scholar] [PubMed]
- Porto, T.; Roperto, R.; Akkus, A.; Akkus, O.; Porto-Neto, S.; Teich, S.; Lang, L.; Campos, E. Mechanical properties and DIC analyses of CAD/CAM materials. J. Clin. Exp. Dent. 2016, 8, e512–e516. [Google Scholar] [CrossRef] [PubMed]
- Tunac, A.T.; Celik, E.U.; Yasa, B. Two-year performance of CAD/CAM fabricated resin composite inlay restorations: A randomized controlled clinical trial. J. Esthet. Restor. Dent. 2019, 31, 627–638. [Google Scholar] [CrossRef] [PubMed]
- Rocha Gomes Torres, C.; Caroline Moreira Andrade, A.; Valente Pinho Mafetano, A.P.; Stabile de Abreu, F.; de Souza Andrade, D.; Cintra Mailart, M.; Aun de Barros Lima Rocha Campello de Souza, M.L.; Guimarães Alarça Nunes, L.; Ariel Rodrigues de Araújo, C.; Di Nicoló, R.; et al. Computer-aided design and computer-aided manufacturer indirect versus direct composite restorations: A randomized clinical trial. J. Esthet. Restor. Dent. 2022, 34, 776–788. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Ilie, N.; Hickel, R.; Reis, A.; Loguercio, A.; Rousson, V. Laboratory mechanical parameters of composite resins and their relation to fractures and wear in clinical trials-A systematic review. Dent. Mater. 2017, 33, e101–e114. [Google Scholar] [CrossRef] [PubMed]
- ISO-6872:2023; Dentistry—Ceramic Materials. International Organization for Standardization: Geneva, Switzerland, 2023.
- ASTM C1327-15; Standard Test Method for Vickers Indentation Hardness of Advanced Ceramics. ASTM International: West Conshohocken, PA, USA, 2015.
- Silva, E.A.; Simionato, A.A.; Faria, A.C.L.; Bonfante, E.A.; Rodrigues, R.C.S.; Ribeiro, R.F. Mechanical Properties, Wear Resistance, and Reliability of Two CAD-CAM Resin Matrix Ceramics. Medicina 2023, 59, 128. [Google Scholar] [CrossRef] [PubMed]
- Thomaidis, S.; Kakaboura, A.; Mueller, W.D.; Zinelis, S. Mechanical properties of contemporary composite resins and their interrelations. Dent. Mater. 2013, 29, e132–e141. [Google Scholar] [CrossRef]
- Mandikos, M.N.; McGivney, G.P.; Davis, E.; Bush, P.J.; Carter, J.M. A comparison of the wear resistance and hardness of indirect composite resins. J. Prosthet. Dent. 2001, 85, 386–395. [Google Scholar] [CrossRef]
- ISO 4049:2019; Dentistry—Polymer-Based Restorative Materials. International Organization for Standardization: Geneva, Switzerland, 2019.
- Lawson, N.C.; Bansal, R.; Burgess, J.O. Wear, strength, modulus and hardness of CAD/CAM restorative materials. Dent. Mater. 2016, 32, e275–e283. [Google Scholar] [CrossRef]
- Alamoush, R.A.; Silikas, N.; Salim, N.A.; Al-Nasrawi, S.; Satterthwaite, J.D. Effect of the Composition of CAD/CAM Composite Blocks on Mechanical Properties. Biomed. Res. Int. 2018, 2018, 4893143. [Google Scholar] [CrossRef] [PubMed]
- Awada, A.; Nathanson, D. Mechanical properties of resin-ceramic CAD/CAM restorative materials. J. Prosthet. Dent. 2015, 114, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues Junior, S.A.; Zanchi, C.H.; Carvalho, R.V.; Demarco, F.F. Flexural strength and modulus of elasticity of different types of resin-based composites. Braz. Oral Res. 2007, 21, 16–21. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Liebermann, A.; Eichberger, M.; Güth, J.F. Evaluation of mechanical and optical behavior of current esthetic dental restorative CAD/CAM composites. J. Mech. Behav. Biomed. Mater. 2015, 55, 1–11. [Google Scholar] [CrossRef]
- Sonmez, N.; Gultekin, P.; Turp, V.; Akgungor, G.; Sen, D.; Mijiritsky, E. Evaluation of five CAD/CAM materials by microstructural characterization and mechanical tests: A comparative in vitro study. BMC Oral Health 2018, 18, 5. [Google Scholar] [CrossRef] [PubMed]
- Askeland, D.R.; Fulay, P.P.; Wright, W.J. The Science and Engineering of Materials, 5th ed.; Cengage Learning: Stamford, CT, USA, 2010. [Google Scholar]
- Gutiérrez-Salazar, M.; Reyes-Gasga, J. Microhardness and Chemical Composition of Human Tooth. Mater. Res. 2003, 6, 367–373. [Google Scholar] [CrossRef]
- Goujat, A.; Abouelleil, H.; Colon, P.; Jeannin, C.; Pradelle, N.; Seux, D.; Grosgogeat, B. Mechanical properties and internal fit of 4 CAD-CAM block materials. J. Prosthet. Dent. 2018, 119, 384–389. [Google Scholar] [CrossRef]
- Sabbagh, J.; Ryelandt, L.; Bachérius, L.; Biebuyck, J.J.; Vreven, J.; Lambrechts, P.; Leloup, G. Characterization of the inorganic fraction of resin composites. J. Oral Rehabil. 2004, 31, 1090–1101. [Google Scholar] [CrossRef]
- Ionescu, A.C.; Hahnel, S.; König, A.; Brambilla, E. Resin composite blocks for dental CAD/CAM applications reduce biofilm formation in vitro. Dent. Mater. 2020, 36, 603–616. [Google Scholar] [CrossRef]
- Lohbauer, U.; Belli, R.; Ferracane, J.L. Factors involved in mechanical fatigue degradation of dental resin composites. J. Dent. Res. 2013, 92, 584–591. [Google Scholar] [CrossRef]
- Alamoush, R.A.; Salim, N.A.; Silikas, N.; Satterthwaite, J.D. Long-term hydrolytic stability of CAD/CAM composite blocks. Eur. J. Oral Sci. 2022, 130, e12834. [Google Scholar] [CrossRef] [PubMed]
- Faria, A.C.; Benassi, U.M.; Rodrigues, R.C.; Ribeiro, R.F.; Mattos Mda, G. Analysis of the relationship between the surface hardness and wear resistance of indirect composites used as veneer materials. Braz. Dent. J. 2007, 18, 60–64. [Google Scholar] [CrossRef] [PubMed]
- Hussain, B.; Thieu, M.K.L.; Johnsen, G.F.; Reseland, J.E.; Haugen, H.J. Can CAD/CAM resin blocks be considered as substitute for conventional resins? Dent. Mater. 2017, 33, 1362–1370. [Google Scholar] [CrossRef] [PubMed]
- da Veiga, A.M.; Cunha, A.C.; Ferreira, D.M.; da Silva Fidalgo, T.K.; Chianca, T.K.; Reis, K.R.; Maia, L.C. Longevity of direct and indirect resin composite restorations in permanent posterior teeth: A systematic review and meta-analysis. J. Dent. 2016, 54, 1–12. [Google Scholar] [CrossRef] [PubMed]
| Experimental Group | Type of Material | Composition | LOT | Brand | |
|---|---|---|---|---|---|
| G1 | TC | Block: Tetric® CAD MT A2/C14 | Bis-GMA, Bis-EMA, TEGDMA, UDMA, barium aluminum silicate glass, and silicon dioxide fillers (71 wt. %/51 vol-%) | X51323 | Ivoclar Vivadent, Ellwangen, Germany |
| G2 | TE | Composite resin: Tetric EvoCeram® A1 | Bis-GMA, urethane dimethacrylate, thoxylated Bis-EMA, barium glass filler, ytterbiumtrifluoride, mixed oxide, and prepolymers (75–76 wt. %/53–55 vol-%) | X31979 | |
| G3 | GB | Block: Grandio® blocs 14L A2 LT | Nanohybrid fillers, UDMA+DMA (86 wt. %/NR) | 1821398 | VOCO GmbH, Cuxhaven, Germany |
| G4 | GS | Composite resin: Grandio® SO A2 | Bis-GMA, Bis-EMA, TEGDMA, functionalized silicon dioxide nanoparticles, and glass ceramic filler (89 wt. %/NR) | 1847313 | |
| G5 | BC | Block: Brilliant Crios® CAD/CAM A2 LT 14 | Cross-linked methacrylates (Bis-GMA, BIS-EMA, TEGDMA), barium glass and silica particles (71 wt. %/51.5 vol-%) | J27358 | Coltene/Whaledent, Langenau, Germany |
| G6 | BET | Composite resin: Brilliant EverGlowTM Translucent | Bis-GMA, TEGDMA, Bis-EMA, prepolymerized particles containing glass and nano-silica, aggregated and non-aggregated colloidal silica, and barium glass (71 wt. %/64 vol-%) | I80057 | |
| G7 | BEU | Composite resin: Brilliant EverGlowTM Universal Shade A2/B2 | I36341 | ||
| Flexural Strength (MPa) | Flexural Modulus (GPa) | Vickers Microhardness (HV) | ||||
|---|---|---|---|---|---|---|
| mean ± std. deviation | 95% Confidence Interval for Mean | mean ± std. deviation | 95% Confidence Interval for Mean | mean ± std. deviation | 95% Confidence Interval for Mean | |
| lower bound/upper bound | lower bound/upper bound | lower bound/upper bound | ||||
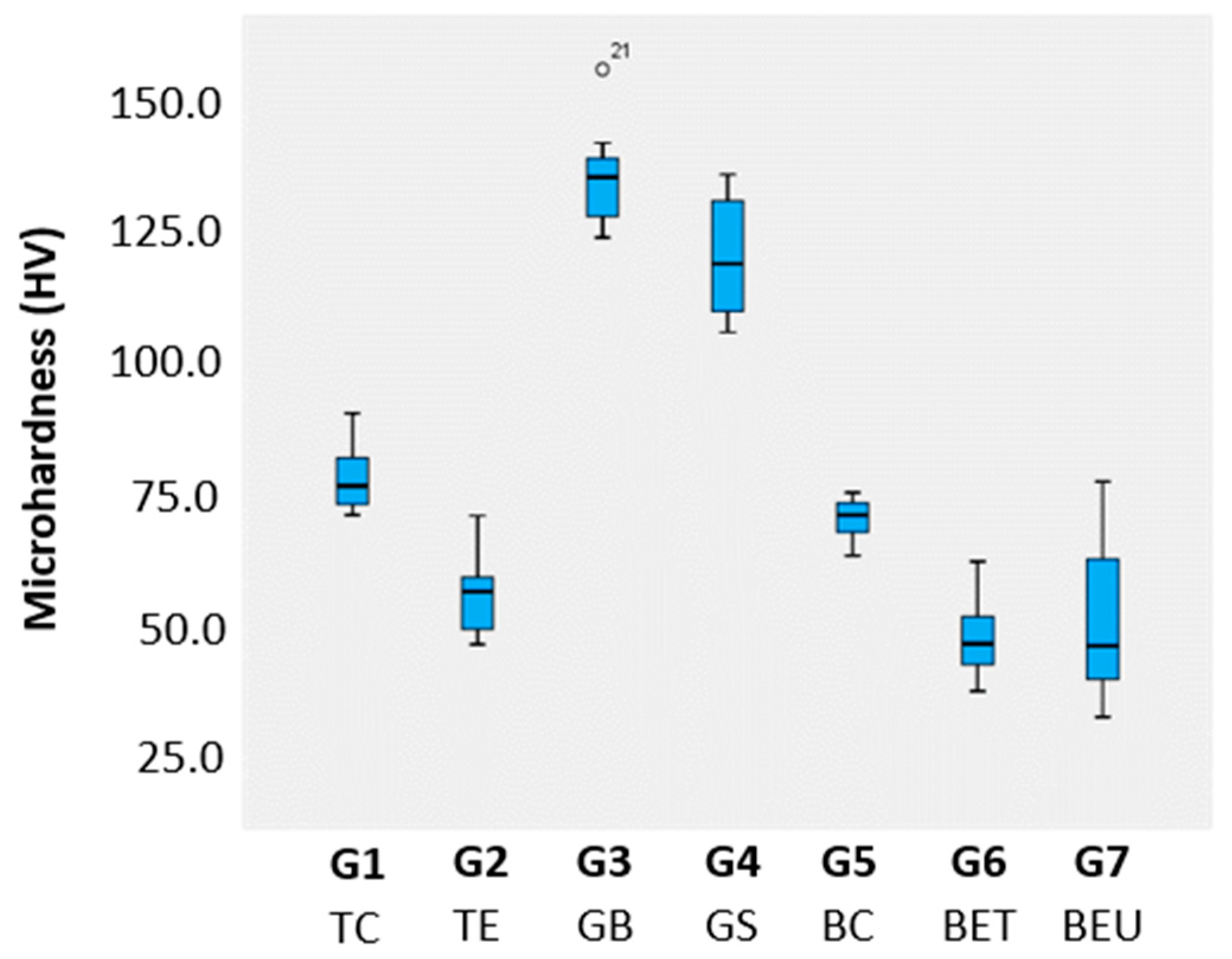
| G1 | 192.4 ± 9.8 a | 187.0/197.9 | 15.8 ± 0.3 a | 15.7/16.0 | 79.3 ± 6.3 a | 74.8/83.8 |
| G2 | 84.1 ± 7.6 b | 78.6/89.6 | 12.3 ± 0.9 b | 11.6/13.0 | 57.2 ± 7.1 b | 52.1/62.3 |
| G3 | 246.5 ± 12.5 c | 239.6/253.4 | 20.3 ± 0.7 c | 19.9/20.7 | 136.2 ± 9.6 c | 129.0/143.1 |
| G4 | 129.6 ± 13.2 d | 122.3/137.0 | 18.0 ± 1.3 d | 17.3/18.7 | 121.2 ± 11.0 c | 113.4/129.0 |
| G5 | 192.8 ± 14.5 a | 184.8/200.9 | 15.1 ± 1.5 a | 14.3/16.0 | 71.7 ± 3.7 a | 69.0/72.3 |
| G6 | 92.5 ± 18.7 b | 79.2/105.9 | 11.4 ± 0.8 b | 10.8/11.9 | 49.9 ± 7.2 b | 44.2/54.5 |
| G7 | 81.1 ± 12.2 b | 72.3/89.8 | 10.6 ± 1.4 b | 9.6/11.6 | 50.9 ± 14.5 b | 40.6/61.3 |
| p * | <0.001 | <0.001 | <0.001 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramos, J.C.; Marinho, A.; Messias, A.; Almeida, G.; Vinagre, A.; Dias, R. Mechanical Properties of Direct Composite Resins and CAD/CAM Composite Blocks. Oral 2024, 4, 206-216. https://doi.org/10.3390/oral4020017
Ramos JC, Marinho A, Messias A, Almeida G, Vinagre A, Dias R. Mechanical Properties of Direct Composite Resins and CAD/CAM Composite Blocks. Oral. 2024; 4(2):206-216. https://doi.org/10.3390/oral4020017
Chicago/Turabian StyleRamos, João Carlos, Alfredo Marinho, Ana Messias, Gabriela Almeida, Alexandra Vinagre, and Ricardo Dias. 2024. "Mechanical Properties of Direct Composite Resins and CAD/CAM Composite Blocks" Oral 4, no. 2: 206-216. https://doi.org/10.3390/oral4020017
APA StyleRamos, J. C., Marinho, A., Messias, A., Almeida, G., Vinagre, A., & Dias, R. (2024). Mechanical Properties of Direct Composite Resins and CAD/CAM Composite Blocks. Oral, 4(2), 206-216. https://doi.org/10.3390/oral4020017









