Unexpected Hyperglycemia? Check the Pen and Needle! An Opportunity to Prevent Injection Technique Errors and Find Causes and Possible Solutions
Abstract
1. Premises
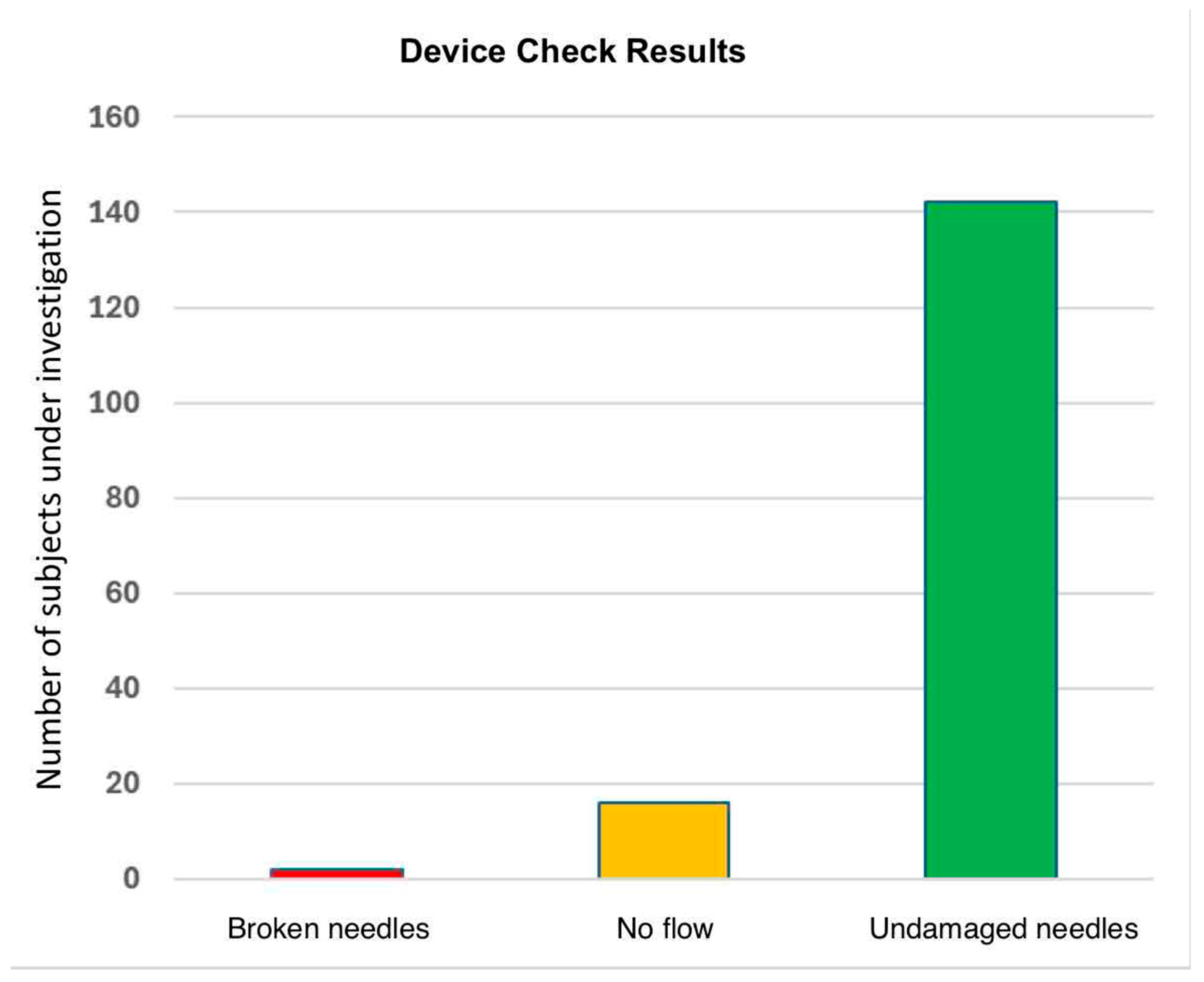
2. Clinical Case
3. Comments
4. Epicrisis
Case Considerations and an Overview
5. Errors
6. Nurses
7. Physicians
8. Pharmacists
9. Injection Technique Training and Clinical Outcomes
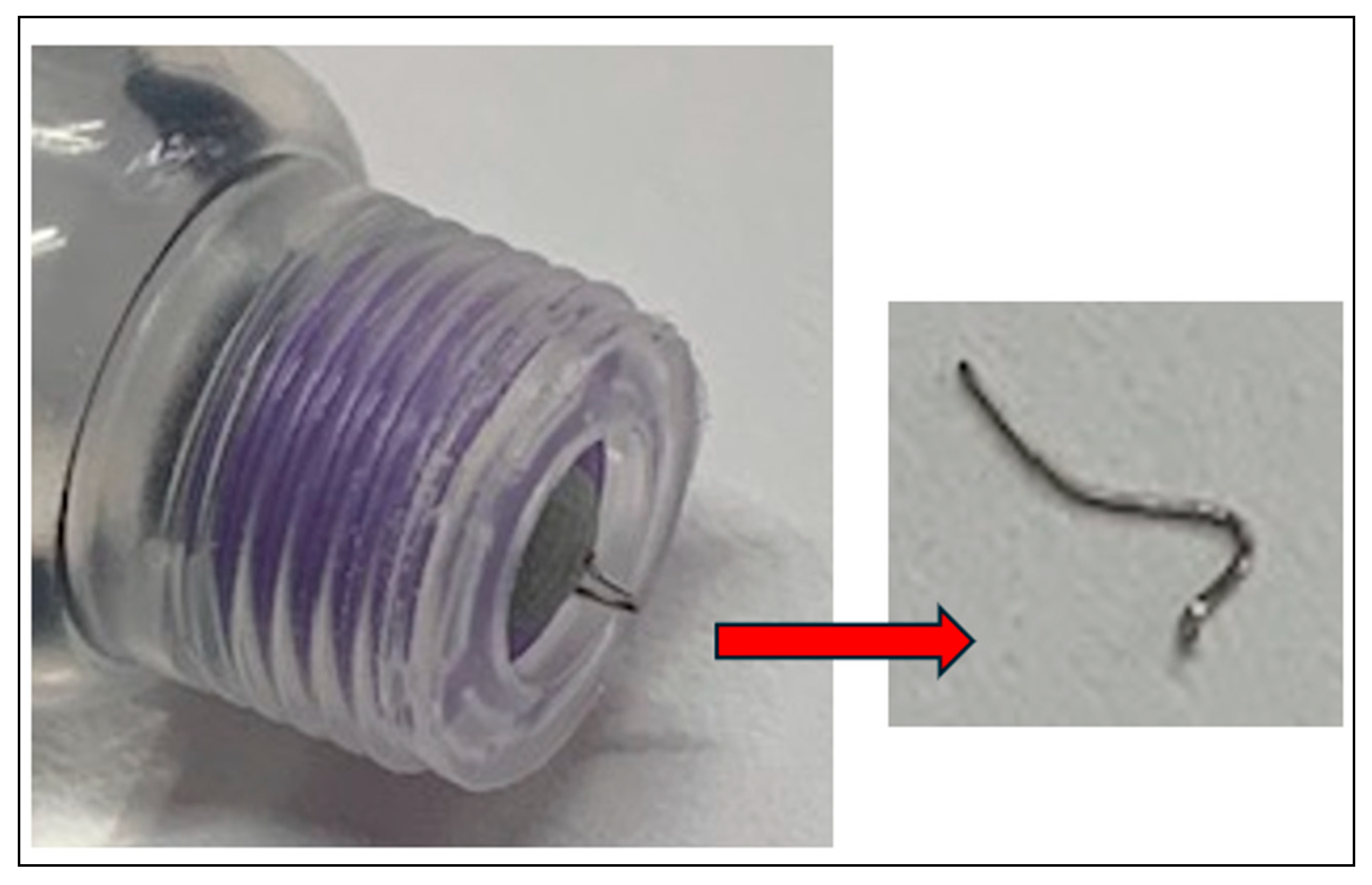
10. Needle Reuse
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADA | American Diabetes Association |
| BMI | body mass index |
| CG | control group |
| CGM | continuous glucose monitoring |
| FITTER | Forum for Injection Technique and Therapy Expert Recommendations |
| FI HCPs | healthcare providers |
| IG | intervention group |
| IM | intramuscular |
| LH | lipohypertrophy |
| TDD | daily insulin dose |
| PwD | people with diabetes |
References
- Gentile, S.; Guarino, G.; Della Corte, T.; Marino, G.; Fusco, A.; Corigliano, G.; Colarusso, S.; Piscopo, M.; Improta, M.R.; Corigliano, M.; et al. AMD-OSDI Study Group on Injection Techniques and Nefrocenter Research & Nyx Start-up Study Group. Insulin-Induced Skin Lipohypertrophy in Type 2 Diabetes: A Multicenter Regional Survey in Southern Italy. Diabetes Ther. 2020, 11, 2001–2017. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Frid, A.H.; Kreugel, G.; Grassi, G.; Halimi, S.; Hicks, D.; Hirsch, L.J.; Smith, M.J.; Wellhoener, R.; Bode, B.W.; Hirsch, I.B.; et al. New Insulin Delivery Recommendations. Mayo Clin. Proc. 2016, 91, 1231–1255. [Google Scholar] [CrossRef] [PubMed]
- Frid, A.H.; Hirsch, L.J.; Menchior, A.R.; Morel, D.R.; Strauss, K.W. Worldwide Injection Technique Questionnaire Study: Population Parameters and Injection Practices. Mayo Clin. Proc. 2016, 91, 1212–1223. [Google Scholar] [CrossRef] [PubMed]
- Mader, J.K.; Fornengo, R.; Hassoun, A.; Heinemann, L.; Kulzer, B.; Monica, M.; Nguyen, T.; Sieber, J.; Renard, E.; Reznik, Y.; et al. Relationship Between Lipohypertrophy, Glycemic Control, and Insulin Dosing: A Systematic Meta-Analysis. Diabetes Technol. Ther. 2024, 26, 351–362. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gentile, S.; Guarino, G.; Della Corte, T.; Marino, G.; Satta, E.; Pasquarella, M.; Romano, C.; Alfrone, C.; Strollo, F. On behalf of the AMD-OSDI Study Group on Injection Technique, and Nefrocenter Research and Nyx Start-Up Study Group. Role of Structured Education in Reducing Lipodystrophy and its Metabolic Complications in Insulin-Treated People with Type 2 Diabetes: A Randomized Multicenter Case-Control Study. Diabetes Ther. 2021, 12, 1379–1398. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gentile, S.; Guarino, G.; Della Corte, T.; Marino, G.; Satta, E.; Pasquarella, M.; Romano, C.; Alfrone, C.; Giordano, L.; Loiacono, F.; et al. on behalf of the AMD-OSDI Study Group on Injection Technique; Nefrocenter Research and Nyx Start-Up Study Group. The Durability of an Intensive, Structured Education-Based Rehabilitation Protocol for Best Insulin Injection Practice: The ISTERP-2 Study. Diabetes Ther. 2021, 12, 2557–2569. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- American Diabetes Association Professional Practice Committee. 9. Pharmacologic approaches to glycemic treatment: Standards of Medical Care in Diabetes—2022. Diabetes Care 2022, 45 (Suppl. S1), S125–S143. [Google Scholar]
- Aronson, R. The role of comfort and discomfort in insulin therapy. Diabetes Technol. Ther. 2012, 14, 741–747. [Google Scholar] [CrossRef]
- Wei, E.T.; Koh, E.; Kelly, M.S.; Wright, L.A.; Tylee, T.S. Patient errors in use of injectable antidiabetic medications: A need for improved clinic-based education. J. Am. Pharm. Assoc. 2020, 60, e76–e80. [Google Scholar] [CrossRef] [PubMed]
- Qiao, Y.J.; Xin-Yuan, Y.; Xu, R.L.; Song, X.Y.; Ye, S.; Zhen, P.; Zhou, S.H.; Zhang, H.Q. Effect of a reused insulin needle remaining in a patient’s body. J. Diabetes Investig. 2023, 14, 821–823. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Briatore, L. Insulin: Where, how, how much?, or: The most bizarre ways to (not) inject insulin. Il G. AMD 2015, 18, 197–199. Available online: https://aemmedi.it/files/Congressi/amd_2015/poster/P134.pdf (accessed on 15 March 2025).
- Pozzuoli, G.M.; Laudato, M.; Barone, M.; Crisci, F.; Pozzuoli, B. Errors in insulin treatment management and risk of lipohypertrophy. Acta Diabetol. 2018, 55, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Saltiel-Berzin, R.; Cypress, M.; Gibney, M. Translating the research in insulin injection technique: Implications for practice. Diabetes Educ. 2012, 38, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Truong, T.H.; Nguyen, T.T.; Armor, B.L.; Farley, J.R. Errors in the Administration Technique of Insulin Pen Devices: A Result of Insufficient Education. Diabetes Ther. 2017, 8, 221–226. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Değer, T.B.; Çakmak, H.S.G.; Erdoğan, B.C.; Değer, M.Ö. Effect of Insulin Pen Training Using the Teach-Back Method on Diabetes Self-Management, Quality of Life, and HbA1c Levels in Older Patients with Type 2 Diabetes: A Quasi-Experimental Study. Healthcare 2024, 12, 1854. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wu, X.; Zhao, F.; Zhang, M.; Yuan, L.; Zheng, Y.; Huang, J.; Li, Y.; Li, C. Insulin Injection Knowledge, Attitudes, and Practices of Nurses in China: A Cross-Sectional Nationwide Study. Diabetes Ther. 2021, 12, 2451–2469. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liao, Y.; Liu, X.; Huang, J.; Chen, Q.; Li, N.; Zhou, P. Insulin injection knowledge, attitude and behaviour of nurses: A cross-sectional study in Guangdong Province. Nurs. Open 2023, 10, 3754–3765. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Guo, L.; Zhang, Q.; Xue, Y.; Ran, X.; Chen, L.; Jiang, S.; Liu, D.; Ji, Q.; Liu, J. A Nationwide Cross-sectional Survey of Knowledge and Practices of Diabetes Drug Injection Techniques of Patients, Nurses, and Physicians: The China IT Improve Study. Mayo Clin. Proc. 2023, 98, 1482–1500. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, L.J.; Strauss, K.W. The injection technique factor: What you Don’t know or teach can make a difference. Clin. Diabetes 2019, 37, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Spollett, G.; Edelman, S.V.; Mehner, P.; Walter, C.; Penfornis, A. Improvement of insulin injection technique: Examination of current issues and recommendations. Diabetes Educ. 2016, 42, 379–394. [Google Scholar] [CrossRef]
- Gentile, S.; Strollo, F.; Guarino, G.; Brancario, C.; Corigliano, M.; Cozzolino, G.; Improta, M.; Fasolino, A.; Lamberti, C.; Lapice, M.; et al. Why are so huge differences reported in the occurrence rate of skin lipohypertrophy? Does it depend on method defects or on lack of interest? Diabetes Metab. Syndr. 2019, 13, 682–686. [Google Scholar] [CrossRef] [PubMed]
- Trief, P.M.; Cibula, D.; Rodriguez, E.; Akel, B.; Weinstock, R.S. Incorrect insulin administration: A problem that warrants attention. Clin. Diabetes 2016, 34, 25–33. [Google Scholar] [CrossRef]
- Institute for Safe Medication Practices. Severe Hyperglycemia in Patients Incorrectly Using Insulin Pens at Home. Available online: www.ismp.org/alerts/severe-hyperglycemia-patients-incorrectlyusing-insulin-pens-home. (accessed on 10 September 2018).
- Kalra, S.; Mithal, A.; Sahay, R.; John, M.; Unnikrishnan, A.G.; Saboo, B.; Ghosh, S.; Sanyal, D.; Hirsch, L.J.; Gupta, V.; et al. Indian Injection Technique Study: Injecting Complications, Education, and the Health Care Professional. Diabetes Ther. 2017, 8, 659–672. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shen, M.; Shi, Y.; Zheng, S.; Fan, H.; Xu, J.; Yang, T. A Systematic Survey of Physicians’ Insights into Lipohypertrophy. Front. Public Health 2021, 9, 738179. [Google Scholar] [CrossRef]
- Luo, D.; Shi, Y.; Zhu, M.; Wang, H.; Yan, D.; Yu, J.; Ji, J.; Liu, X.; Fan, B.; Xu, Y.; et al. Subclinical lipohypertrophy–Easily ignored complications of insulin therapy. J. Diabetes Complicat. 2021, 35, 107806. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.H. Hospital Management; People’s Health Publishing House: Beijing, China, 1990. [Google Scholar]
- Zhang, W.; Deng, Z.; Evans, R.; Xiang, F.; Ye, Q.; Zeng, R. Social media landscape of the tertiary referral hospitals in China: Observational descriptive study. J. Med. Internet Res. 2018, 20, e249. [Google Scholar] [CrossRef]
- Frid, A.H.; Hirsch, L.J.; Menchior, A.R.; Morel, D.R.; Strauss, K.W. Worldwide injection technique questionnaire study: Injecting complications and the role of the professional. Mayo Clin. Proc. 2016, 91, 1224–1230. [Google Scholar] [CrossRef]
- Orabone, A.W.; Do, V.; Cohen, E. Pharmacist-Managed Diabetes Programs: Improving Treatment Adherence and Patient Outcomes. Diabetes Metab. Syndr. Obes. 2022, 15, 1911–1923. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- CDC. Cost-Effectiveness of Diabetes Interventions. 2021. Available online: https://www.cdc.gov/chronicdisease/programs-impact/pop/diabetes.htm#:~:text=The%20High%20Cost%20of%20Diabeteshronic%20condition%20in%20our%20nation.&text=%241%20out%20of%20every%20%244aring%20for%20people%20with%20diabetes.&text=%24237%20billion%E2%80%A1(c)%20is,(c)%20on%20reduced%20productivity (accessed on 15 March 2025).
- Wang, J.; Pei, Y.; Yu, F.; Kang, Z.; Zheng, Y. Understandings, Attitudes, and Barriers About Diabetes Care: Analysis of Factors Influencing Community Pharmacists in China. Diabetes Metab. Syndr. Obes. 2021, 14, 1999–2009. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Woodhouse, A.G.; Orvin, C.; Rich, C.; Crosby, J.; Keedy, C.A. Diabetes outcomes before and during telehealth advancements surrounding COVID-19. J. Am. Pharm. Assoc. 2022, 62, 214–217. [Google Scholar] [CrossRef]
- Fantasia, K.L.; Stockman, M.-C.; Ju, Z.; Ortega, P.; Crable, E.L.; Drainoni, M.-L.; Walkey, A.J.; Bergstrom, M.; O’BRien, K.; Steenkamp, D. Professional continuous glucose monitoring and endocrinology eConsult for adults with type 2 diabetes in primary care: Results of a clinical pilot program. J. Clin. Transl. Endocrinol. 2021, 24, 100254. [Google Scholar] [CrossRef]
- Ulrich, H.; Bowen, M. The clinical utility of professional continuous glucose monitoring by pharmacists for patients with type 2 diabetes. J. Am. Pharm. Assoc. 2003, 2021, e76–e82. [Google Scholar] [CrossRef]
- Shah, M.; Norwood, C.A.; Farias, S.; Ibrahim, S.; Chong, P.H.; Fogelfeld, L. Diabetes transitional care from inpatient to outpatient setting: Pharmacist discharge counseling. J. Pharm. Pract. 2013, 26, 120–124. [Google Scholar] [CrossRef]
- Abdelaziz, T.A.; Abdulraheem, M.A.; Badi, S.A.; Badawi, M.I.; Saeed, A.O.; Elobied, M.A.; Ahmed, M.H. Knowledge, attitude and practice of Sudanese pharmacist with regard to management of diabetes during Ramadan: A cross-sectional survey. Diabetes Metab. Syndr. 2019, 13, 122–126. [Google Scholar] [CrossRef]
- Risøy, A.J.; Kjome, R.L.S.; Svensberg, K.; Råheim, M.; Sølvik, U.Ø. Pharmacists’ experience of a diabetes risk-assessment service and analytical quality control in community pharmacies—A focus-group study. Res. Soc. Adm. Pharm. 2021, 17, 1259–1266. [Google Scholar] [CrossRef]
- Katangwe, T.; Family, H.; Sokhi, J.; Al-Jabr, H.; Kirkdale, C.L.; Twigg, M.J.; Torpey, K. The community pharmacy setting for diabetes prevention: Views and perceptions of stakeholders. PLoS ONE 2019, 14, e0219686. [Google Scholar] [CrossRef]
- Smith, M.; Clapham, L.; Strauss, K. UK lipohypertrophy intervention study. Diabetes Res. Clin. Pract. 2017, 126, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Campinos, C.; Le Floch, J.P.; Petit, C.; Penfornis, A.; Winiszewski, P.; Bordier, L.; Lepage, M.; Fermon, C.; Louis, J.; Almain, C.; et al. An effective intervention for diabetic lipohypertrophy: Results of a randomised, controlled, prospective, multicentre study in France. Diabetes Technol. Ther. 2017, 19, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Misnikova, I.V.; Gubkina, V.A.; Lakeeva, T.S.; Dreval, A.V. A randomized controlled trial to assess the impact of proper insulin injection technique training on glycemic control. Diabetes Ther. 2017, 8, 1309–1318. [Google Scholar] [CrossRef]
- Gentile, S.; Guarino, G.; Della Corte, T.; Marino, G.; Satta, E.; Pasquarella, M.; Romano, C.; Alfrone, C.; Giordano, L.; Loiacono, F.; et al. The Economic Burden of Insulin Injection-Induced Lipohypertophy. Role of Education: The ISTERP-3 Study. Adv. Ther. 2022, 39, 2192–2207, Erratum in Adv. Ther. 2022, 39, 3058. https://doi.org/10.1007/s12325-022-02147-9. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- De Coninck, C.; Frid, A.; Gaspar, R.; Hicks, D.; Hirsch, L.; Kreugel, G.; Liersch, J.; Letondeur, C.; Sauvanet, J.-P.; Tubiana, N.; et al. Results and analysis of the 2008–2009 Insulin Injection Technique Questionnaire survey. J. Diabetes 2010, 2, 168–179. [Google Scholar] [CrossRef]
- Vardar, B.; Kızılcı, S. Incidence of lipohypertrophy in diabetic patients and a study of influencing factors. Diabetes Res. Clin. Pract. 2007, 77, 231–236. [Google Scholar] [CrossRef]
- Saez-de Ibarra, L.; Gallego, F. Factors related to lipohypertrophy in insulin-treated diabetic patients; role of educational intervention. Pract. Diabetol. Int. 1998, 15, 9–11. [Google Scholar] [CrossRef]
- Strauss, K.; De Gols, H.; Hannet, I.; Partanen, T.; Frid, A. A pan-European epidemiologic study of insulin injection technique in patients with diabetes. Pract. Diabetol. Int. 2002, 19, 71–76. [Google Scholar] [CrossRef]
- Misnikova, I.; Dreval, A.; Gubkina, V.; Rusanova, E. The risk of repeated use of insulin pen needles in patients with diabetes mellitus. J. Diabetol. 2011, 1, 2. [Google Scholar] [CrossRef]
- Puder, J.J.; Atar, M.; Muller, B.; Pavan, M.; Keller, U. Using insulin pen needles up to five times does not affect needle tip shape nor increase pain intensity. Diabetes Res. Clin. Pract. 2005, 67, 119–123. [Google Scholar] [CrossRef]
- Schuler, G.; Pelz, K.; Kerp, L. Is the reuse of needles for insulin injection systems associated with a higher risk of cutaneous complications? Diabetes Res. Clin. Pract. 1992, 16, 209–212. [Google Scholar] [CrossRef]
- Thomas, D.R.; Fischer, R.G.; Nicholas, W.C.; Beghe, C.; Hatten, K.W.; Thomas, J.N. Disposable insulin syringe reuse and aseptic practices in diabetic patients. J. Gen. Intern. Med. 1989, 4, 97–100. [Google Scholar] [CrossRef]
- Klonoff, D.C.; Berard, L.; Franco, D.R.; Gentile, S.; Gomez, O.V.; Hussein, Z.; Jain, A.B.; Kalra, S.; Anhalt, H.; Mader, J.K.; et al. Advance Insulin Injection Technique and Education with FITTER Forward Expert Recommendations. Mayo Clin. Proc. 2024. submitted. [Google Scholar] [CrossRef]
- Zabaleta-Del-Olmo, E.; Vlacho, B.; Jodar-Fernández, L.; Urpí-Fernández, A.-M.; Lumillo-Gutiérrez, I.; Agudo-Ugena, J.; Morros-Pedrós, R.; Violán, C. Safety of the reuse of needles for subcutaneous insulin injection: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2016, 60, 121–132. [Google Scholar] [CrossRef]
- Chowdhury, S.; Chakraborty, P.P. Errors of insulin therapy: Real-life experiences from developing world. J. Fam. Med. Prim. Care 2017, 6, 724–729. [Google Scholar] [CrossRef]
- Kamrul-Hasan, A.; Paul, A.K.; Amin, M.N.; Gaffar, M.B.J.; Asaduzzaman, M.; Saifuddin, M.; Mustari, M.; Alam, M.J.; Shahid, M.M.; Nahid-Ul-Haque, K.M.; et al. Insulin injection practice and injection complications—Results from the Bangladesh insulin injection technique survey. Eur. Endocrinol. 2020, 16, 41–48. [Google Scholar] [CrossRef]
- Vaag, A.; Handberg, A.; Lauritzen, M.; Henriksen, J.E.; Pedersen, K.D.; Beck-Nielsen, H. Variation in absorption of NPH insulin due to intramuscular injection. Diabetes Care 1990, 13, 74–76. [Google Scholar] [CrossRef] [PubMed]
- Blanco, M.; Hernández, M.; Strauss, K.; Amaya, M. Prevalence and risk factors of lipohypertrophy in insulin-injecting patients with diabetes. Diabetes Metab. 2013, 39, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Grassi, G.; Scuntero, P.; Trepiccioni, R.; Marubbi, F.; Strauss, K. Optimizing insulin injection technique and its effect on blood glucose control. J. Clin. Transl. Endocrinol. 2014, 1, 145–150. [Google Scholar] [CrossRef]
- Ji, L.; Sun, Z.; Li, Q.; Qin, G.; Wei, Z.; Liu, J.; Chandran, A.B.; Hirsch, L.J. Lipohypertrophy in China: Prevalence, risk factors, insulin consumption and clinical impact. Diab Technol. Ther. 2017, 19, 61–67. [Google Scholar] [CrossRef]
- Gentile, S.; Ceriello, A.; Strollo, F. Insulin shot dependent lipodystrophy: Evidence, uncertainties and current terminology overlaps. J. Diabetes Metab. Disord. Control 2016, 3, 53–55. [Google Scholar]
- Conwell, L.S.; Pope, E.; Artiles, A.M.; Mohanta, A.; Daneman, A.; Daneman, D. Dermatological complications of continuous subcutaneous insulin infusion in children and adolescents. J. Pediatr. 2008, 152, 622–628. [Google Scholar] [CrossRef]
- Pickup, J.C.; Yemane, N.; Brackenridge, A.; Pender, S. Nonmetabolic complications of continuous subcutaneous insulin infusion: A patient survey. Diabetes Technol. Ther. 2014, 16, 145–149. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Age-Adjusted Percentage of Adults with Diabetes Using Diabetes Medication, by Type of Medication, United States, 1997–2011. Available online: https://www.cdc.gov/diabetes/php/data-research/index.html (accessed on 21 July 2025).
- Garg, S.K.; Rewers, A.H.; Akturk, H.K. Ever-increasing insulin-requiring patients globally. Diabetes Technol. Ther. 2018, 20 (Suppl. S2), S21–S24. [Google Scholar] [CrossRef]
| The Patient | The Diabetes Team | The Pharmacist |
|---|---|---|
| Does not remove the inner pen needle cover | Does not know enough about injection techniques | Gives the patient inadequate needles that are too long |
| Does not press and keep down the pen piston at the end of the injection | Does not know enough about lipohypertrophy | Provides the patient with pen-incompatible threading |
| Does not press down enough on the pen piston due to hand problems | Has knowledge of lipohypertrophy but not its mechanisms | Gives the patient lancets non-compatible with the lancing device |
| Holds the pen incorrectly, so that the hand weakens and the injection is incomplete | Does not know how to manage lipodystrophies | Tells the patient to keep the drug in the refrigerator without saying that the daily pen has to be kept at room temperature |
| Injects into the nodules | Has poor communication skills | Offers little or no collaboration in therapeutic education |
| Does not rotate the injection sites | Is not aware of all possible errors made by patients during injection | Provides information different from or even contradictory to that coming from colleagues |
| Tends to reuse needles | Does not check injection sites systematically | Provides poor counseling on hypoglycemia prevention and care |
| Does not remove the needle from the pen after the injection | Does not monitor patients while injecting insulin | Provides poor counseling on hyperglycemia prevention and care |
| Uses long needles without inching the skin (pens or syringes) | Dose not check the pen used by the patient | Provides poor nutritional counseling |
| Injects ice-cold insulin | Does not teach patients how to manage hyperglycemia | |
| Makes mistakes when selecting the dose on the pen | Does not teach patients how to manage hypoglycemia | |
| Dose not dispose of the needles after use | Does not teach patients how to dispose of needles after use | |
| Exchanges pens in promiscuous environments | ||
| Do not have enough time for therapeutic education | ||
| Provides information different from or even contradictory to that coming from colleagues |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strollo, F.; Guarino, G.; Gentile, S. Unexpected Hyperglycemia? Check the Pen and Needle! An Opportunity to Prevent Injection Technique Errors and Find Causes and Possible Solutions. Diabetology 2025, 6, 89. https://doi.org/10.3390/diabetology6090089
Strollo F, Guarino G, Gentile S. Unexpected Hyperglycemia? Check the Pen and Needle! An Opportunity to Prevent Injection Technique Errors and Find Causes and Possible Solutions. Diabetology. 2025; 6(9):89. https://doi.org/10.3390/diabetology6090089
Chicago/Turabian StyleStrollo, Felice, Giuseppina Guarino, and Sandro Gentile. 2025. "Unexpected Hyperglycemia? Check the Pen and Needle! An Opportunity to Prevent Injection Technique Errors and Find Causes and Possible Solutions" Diabetology 6, no. 9: 89. https://doi.org/10.3390/diabetology6090089
APA StyleStrollo, F., Guarino, G., & Gentile, S. (2025). Unexpected Hyperglycemia? Check the Pen and Needle! An Opportunity to Prevent Injection Technique Errors and Find Causes and Possible Solutions. Diabetology, 6(9), 89. https://doi.org/10.3390/diabetology6090089








