Filling Gaps on Stability Data: Development, Validation and Application of a Multianalyte UHPLC-DAD Method to Determine the Stability of Commonly Administered Drugs in Different Carrier Solutions Used in Palliative Care
Abstract
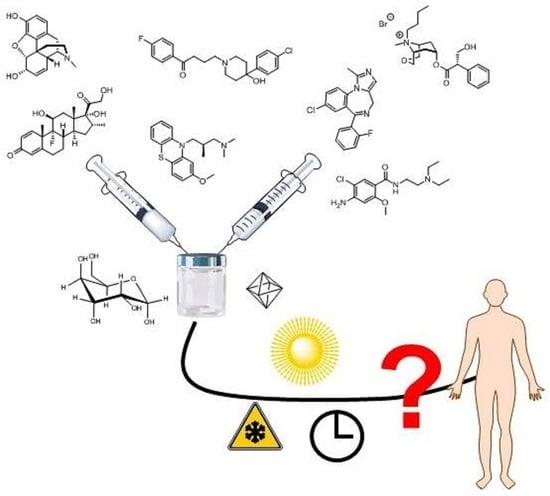
:1. Introduction
2. Materials and Methods
2.1. Method Development
2.2. Preparation of Calibration and Quality Control (QC) Samples
2.3. Preparation of Therapeutic Solutions
2.4. Sample Preparation
2.5. Method Validation
2.6. Data Analysis
3. Results
3.1. Method Developement
3.2. Application of the Method
3.2.1. Binary Mixtures
3.2.2. Ternary Mixture of Morphine—Midazolam—Scopolamine Butylbromide
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Guter, A. Standard zur subkutanen Applikation von Parenteralia in der Palliativmedizin. Krankenhauspharmazie 2011, 32, 484–489. [Google Scholar]
- Thomas, T.; Barclay, S. Continuous subcutaneous infusion in palliative care: A review of current practice. Int. J. Palliat. Nurs. 2015, 21, 62–64. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Mansfield, B.; Wilcox, M.H. Subcutaneous fluid administration—Better than the intravenous approach? J. Hosp. Infect. 1999, 41, 269–272. [Google Scholar] [CrossRef] [PubMed]
- Dickman, A.; Schneider, J. The Syringe Driver—Continuous Subcutaneous Infusions in Palliative Care, 4th ed.; Oxford University Press: Oxford, UK, 2016. [Google Scholar]
- Frühwald, T. Ist die subkutane Infusion eine praktische Alternative in der Geriatrie? J. Für Ernährungsmedizin 2001, 3, 16–18. [Google Scholar]
- Baker, J.; Dickman, A.; Mason, S.; Ellershaw, J. The current evidence base for the feasibility of 48-hour continuous subcutaneous infusions (CSCIs): A systematically-structured review. PLoS ONE 2018, 13, e0194236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bausewein, C.; Rémi, C. Besonderheiten der Pharmakotherapie in der Palliative Care, Bigorio. 2012. Available online: https://www.palliative.ch/fileadmin/user_upload/palliative/fachwelt/E_Standards/Besonderheiten_der_Pharmakotherapie_in_der_Palliative_Care.pdf (accessed on 5 August 2020).
- Masman, A.D.; van Dijk, M.; Tibboel, D.; Baar, F.P.; Mathot, R.A. Medication use during end-of-life care in a palliative care centre. Int. J. Clin. Pharm. 2015, 37, 767–775. [Google Scholar] [CrossRef] [Green Version]
- Sutherland, A.E.; Curtin, J.; Bradley, V.; Bush, O.; Presswood, M.; Hedges, V.; Naessens, K. Subcutaneous levetiracetam for the management of seizures at the end of life. BMJ Support Palliat Care 2018, 8, 129–135. [Google Scholar] [CrossRef]
- Dickman, A.; Bickerstaff, M.; Jackson, R.; Schneider, J.; Mason, S.; Ellershaw, J. Identification of drug combinations administered by continuous subcutaneous infusion that require analysis for compatibility and stability. BMC Palliat. Care 2017, 16, 22. [Google Scholar] [CrossRef] [Green Version]
- Aeberhard, C.; Steuer, C.; Saxer, C.; Huber, A.; Stanga, Z.; Muhlebach, S. Physicochemical stability and compatibility testing of levetiracetam in all-in-one parenteral nutrition admixtures in daily practice. Eur. J. Pharm. Sci. 2017, 96, 449–455. [Google Scholar] [CrossRef]
- Gomez, M.A.; Arenas, V.J.; Sanjuan, M.M.; Hernandez, M.J.; Almenar, C.B.; Torres, V.J. Stability studies of binary mixtures of haloperidol and/or midazolam with other drugs for parenteral administration. J. Palliat. Med. 2007, 10, 1306–1311. [Google Scholar] [CrossRef]
- IBM. IBM Micromedex (Trissel online); IBM: Armonk, NY, USA, 2018. [Google Scholar]
- Scholes, S.; William, L.; Halliwell, D.; Sherwen, P.; Whelan, T.; Clifton, C. Syringe Driver Drug Compatibilities—Guide to Palliative Care Practice. East. Metrop. Reg. Palliat. Care Consort. 2016. Available online: https://www.emrpcc.org.au/uploads/136/Syringe-Driver-Drug-Compatibilities-May-2016.pdf (accessed on 5 August 2020).
- Rossignol, E.; Sorrieul, J.; Beaussart, H.; Kieffer, H.; Folliard, C.; Dupoiron, D.; Devys, C. Validation Study of UPLC Method for Determination of Morphine, Ropivacaïne and Ziconotide in Combination for Intrathecal Analgesia. J. Anal. Bioanal. Tech. 2016, 7, 1000310. [Google Scholar]
- Destro, M.; Ottolini, L.; Vicentini, L.; Boschetti, S. Physical compatibility of binary and ternary mixtures of morphine and methadone with other drugs for parenteral administration in palliative care. Support Care Cancer 2012, 20, 2501–2509. [Google Scholar] [CrossRef] [PubMed]
- Negro, S.; Reyes, R.; Azuara, M.L.; Sanchez, Y.; Barcia, E. Morphine, haloperidol and hyoscine N-butyl bromide combined in s.c. infusion solutions: Compatibility and stability. Evaluation in terminal oncology patients. Int. J. Pharm. 2006, 307, 278–284. [Google Scholar] [CrossRef]
- Good, P.D.; Schneider, J.J.; Ravenscroft, P.J. The compatibility and stability of midazolam and dexamethasone in infusion solutions. J. Pain Symptom Manag. 2004, 27, 471–475. [Google Scholar] [CrossRef]
- Negro, S.; Azuara, M.L.; Sanchez, Y.; Reyes, R.; Barcia, E. Physical compatibility and in vivo evaluation of drug mixtures for subcutaneous infusion to cancer patients in palliative care. Support Care Cancer 2002, 10, 65–70. [Google Scholar] [CrossRef]
- Wong, H.A.; Law, S.; Walker, S.E.; Bowles, S.K. Concentration-Dependent Compatibility and Stability of Dexamethasone and Midazolam. Can. J. Hosp. Pharm. 2000, 53, 24–31. [Google Scholar]
- Barcia, E.; Reyes, R.; Azuara, M.L.; Sanchez, Y.; Negro, S. Stability and compatibility of binary mixtures of morphine hydrochloride with hyoscine-n-butyl bromide. Support Care Cancer 2005, 13, 239–245. [Google Scholar] [CrossRef]
- Al-Tannak, N.F.; Cable, C.G.; McArthur, D.A.; Watson, D.G. A stability indicating assay for a combination of morphine sulphate with levomepromazine hydrochloride used in palliative care. J. Clin. Pharm. Ther. 2012, 37, 71–73. [Google Scholar] [CrossRef]
- Schrijvers, D.; Tai-Apin, C.; De Smet, M.C.; Cornil, P.; Vermorken, J.B.; Bruyneel, P. Determination of compatibility and stability of drugs used in palliative care. J Clin Pharm Ther. 1998, 23, 311–314. [Google Scholar] [CrossRef]
- Peters, F.T.; Hartung, M.; Herbold, M.; Schmitt, G.; Daldrup, T.; Mußhoff, F. APPENDIX B Requirements for the validation of analytical methods. Toxichem. Krimtech. 2009, 76, 185–208. [Google Scholar]
- Oliva, A.; Monzon, C.; Santovena, A.; Farina, J.B.; Llabres, M. Development of an ultra high performance liquid chromatography method for determining triamcinolone acetonide in hydrogels using the design of experiments/design space strategy in combination with process capability index. J. Sep. Sci. 2016, 39, 2689–2701. [Google Scholar] [CrossRef] [PubMed]
- Leardi, R. Experimental design in chemistry: A tutorial. Anal. Chim. Acta. 2009, 652, 161–172. [Google Scholar] [CrossRef] [PubMed]
- Binz, T.M.; Braun, U.; Baumgartner, M.R.; Kraemer, T. Development of an LC-MS/MS method for the determination of endogenous cortisol in hair using (13)C3-labeled cortisol as surrogate analyte. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2016, 1033–1034, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Van de Merbel, N.C. Quantitative determination of endogenous compounds in biological samples using chromatographic techniques. Trac-Trend Anal. Chem. 2008, 27, 924–933. [Google Scholar] [CrossRef]
- Steuer, C.; Schuetz, P.; Bernasconi, L.; Huber, A.R. Quantification of Quaternary Ammonium Compounds Against Surrogate Matrix by HILIC-MS/MS. CHIMIA Int. J. Chem. 2017, 71, 601. [Google Scholar] [CrossRef] [Green Version]




| Range mg/mL | Cal. Model | QC High | QC Med | QC Low | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bias [%] | RSDR [%] | RSDT [%] | Bias [%] | RSDR [%] | RSDT [%] | Bias [%] | RSDR [%] | RSDT [%] | |||
| Dex | 0.04–0.41 | 1/x2 | −8.9 | 3.3 | 3.8 | −11.2 | 1.9 | 3.5 | −12.4 | 3.5 | 6.2 |
| Hal | 0.05–0.52 | 1/x2 | 0.7 | 3.0 | 3.0 | −1.4 | 1.4 | 3.0 | 5.5 | 3.9 | 4.8 |
| Lev | 0.32–3.24 | 1/x2 | −7.5 | 3.4 | 3.4 | −9.8 | 2.1 | 3.0 | −8.9 | 2.3 | 4.7 |
| Met | 0.33–3.30 | 1/x2 | −0.6 | 3.4 | 3.4 | −3.0 | 2.0 | 2.9 | −2.0 | 2.5 | 4.4 |
| Mid | 0.12–1.2 | 1/x2 | 2.2 | 3.2 | 3.1 | −0.6 | 1.8 | 3.1 | 0.4 | 2.6 | 4.5 |
| Mor | 0.52–5.18 | 1/x2 | −4.3 | 2.6 | 2.4 | 4.4 | 2.0 | 2.4 | −6.5 | 3.3 | 6.1 |
| Sco | 0.73–7.32 | 1/x2 | 5.1 | 3.1 | 3.5 | 3.3 | 2.1 | 3.3 | 1.4 | 2.8 | 5.0 |
| Met | Lev | Hal | Lev | Sco | Lev | Sco | Mor | Sco | Hal | ||||||||||||
| Time [h] | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | |
| 0.9% NaCl RT | 0 | 100.0 | 2.9 | 100.0 | 2.4 | 100.0 | 1.6 | 100.0 | 1.9 | 100.0 | 5.8 | 100.0 | 2.8 | 100.0 | 0.5 | 100.0 | 2.6 | 99.8 | 1.2 | 100.0 | 1.3 |
| 4 | 93.7 | 2.3 | 93.0 | 1.8 | 94.7 | 1.3 | 94.6 | 1.9 | 95.1 | 0.2 | 95.3 | 0.7 | 95.9 | 2.1 | 92.6 | 2.3 | 98.8 | 0.2 | 99.3 | 0.4 | |
| 8 | 95.7 | 1.1 | 94.9 | 0.9 | 93.9 | 1.4 | 94.4 | 0.9 | 92.8 | 0.2 | 92.6 | 0.2 | 96.0 | 3.2 | 92.2 | 3.1 | 96.8 | 4.6 | 96.5 | 3.1 | |
| 24 | 97.0 | 0.4 | 96.2 | 0.4 | 95.8 | 0.8 | 95.8 | 0.4 | 92.3 | 3.8 | 92.2 | 3.2 | 99.1 | 0.9 | 95.1 | 0.9 | 99.6 | 0.3 | 99.2 | 0.4 | |
| 48 | 97.1 | 0.5 | 95.1 | 0.3 | 95.0 | 0.8 | 94.7 | 0.9 | 97.3 | 3.5 | 97.4 | 1.3 | 99.4 | 0.1 | 94.1 | 0.3 | 100.0 | 0.1 | 98.8 | 0.6 | |
| Met | Lev | Hal | Lev | Sco | Lev | Sco | Mor | Sco | Hal | ||||||||||||
| Time [h] | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | |
| 0.9% NaCl 0 °C | 0 | 100.0 | 3.1 | 100.0 | 3.0 | 100.0 | 3.7 | 100.0 | 3.4 | 99.1 | 3.2 | 99.3 | 3.3 | 99.9 | 2.1 | 98.6 | 2.0 | 100.0 | 1.5 | 100.0 | 1.7 |
| 4 | 94.7 | 0.3 | 94.8 | 0.4 | 96.6 | 1.8 | 96.3 | 1.4 | 95.9 | 5.0 | 97.9 | 5.0 | 98.7 | 1.0 | 96.7 | 0.8 | 97.4 | 1.0 | 98.3 | 2.0 | |
| 8 | 95.2 | 1.0 | 94.5 | 1.2 | 97.7 | 1.3 | 97.6 | 0.8 | 100.0 | 0.9 | 100.0 | 0.8 | 97.7 | 0.4 | 96.0 | 0.6 | 99.0 | 0.8 | 100.0 | 1.3 | |
| 24 | 95.9 | 1.7 | 94.8 | 1.7 | 93.6 | 2.4 | 94.3 | 1.8 | 98.2 | 2.9 | 97.6 | 2.8 | 99.0 | 0.4 | 99.3 | 0.8 | 96.9 | 0.2 | 96.0 | 0.7 | |
| 48 | 95.2 | 0.6 | 95.0 | 0.7 | 91.0 | 5.1 | 91.9 | 5.2 | 96.6 | 2.2 | 96.2 | 2.0 | 100.0 | 0.3 | 100.0 | 0.5 | 99.6 | 2.0 | 98.6 | 2.3 | |
| Mid | Lev | Sco | Mid | Sco | Met | Sco | Mor | Sco | DexP | ||||||||||||
| Time [h] | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | |
| 5% Glucose RT | 0 | 100.0 | 2.2 | 100.0 | 2.4 | 100.0 | 1.4 | 100.0 | 1.1 | 100.0 | 2.8 | 99.5 | 3.2 | 100.0 | 0.3 | 100.0 | 0.3 | 100.0 | 1.6 | 100.0 | 2.7 |
| 4 | 95.5 | 0.3 | 95.9 | 0.1 | 97.7 | 0.2 | 97.6 | 0.3 | 98.6 | 0.9 | 98.8 | 0.6 | 96.7 | 0.2 | 96.1 | 0.4 | 99.5 | 0.2 | 97.4 | 0.4 | |
| 8 | 96.2 | 1.3 | 97.0 | 1.1 | 97.1 | 0.3 | 96.0 | 0.6 | 98.6 | 0.9 | 99.4 | 1.0 | 97.7 | 0.4 | 96.6 | 0.1 | 97.6 | 0.7 | 94.9 | 0.7 | |
| 24 | 95.6 | 0.0 | 96.1 | 0.1 | 98.4 | 0.4 | 97.7 | 0.3 | 99.7 | 0.7 | 100.0 | 0.2 | 98.5 | 0.2 | 97.4 | 0.3 | 96.6 | 0.9 | 94.4 | 0.9 | |
| 48 | 95.1 | 0.2 | 96.9 | 0.5 | 99.8 | 0.1 | 98.0 | 0.3 | 98.6 | 0.6 | 99.5 | 0.4 | 99.2 | 0.3 | 99.4 | 0.5 | 97.9 | 0.7 | 95.7 | 0.5 | |
| Mor | Mid | Sco | |||||
| Time [h] | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | |
| 0.9% NaCl RT | 0 | 100.0 | 0.7 | 100.0 | 0.7 | 100.0 | 0.5 |
| 4 | 96.7 | 0.1 | 98.7 | 0.4 | 97.6 | 0.4 | |
| 8 | 93.1 | 2.7 | 95.4 | 3.2 | 94.4 | 2.9 | |
| 24 | 94.3 | 3.9 | 96.7 | 3.9 | 95.7 | 3.9 | |
| 48 | 95.2 | 2.9 | 98.6 | 2.7 | 96.4 | 2.7 | |
| Mor | Mid | Sco | |||||
| Time [h] | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | |
| 0.9% NaCl 0 °C | 0 | 100.0 | 2.2 | 100.0 | 2.2 | 100.0 | 1.9 |
| 4 | 95.7 | 2.6 | 96.1 | 2.4 | 95.5 | 2.5 | |
| 8 | 98.0 | 1.2 | 98.2 | 1.0 | 98.0 | 1.1 | |
| 24 | 99.9 | 0.4 | 99.7 | 0.9 | 98.9 | 0.2 | |
| 48 | 96.6 | 4.4 | 97.0 | 4.4 | 96.6 | 4.0 | |
| Mor | Mid | Sco | |||||
| Time [h] | Mean [%] | SD | Mean [%] | SD | Mean [%] | SD | |
| 5% Glucose RT | 0 | 100.0 | 1.0 | 100.0 | 1.1 | 100.0 | 1.9 |
| 4 | 97.6 | 0.6 | 97.7 | 0.2 | 97.0 | 0.6 | |
| 8 | 98.0 | 0.4 | 98.1 | 0.3 | 97.9 | 0.8 | |
| 24 | 97.8 | 0.6 | 99.0 | 0.2 | 98.7 | 0.4 | |
| 48 | 98.3 | 0.8 | 99.2 | 0.4 | 98.1 | 0.4 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Steuer, C.; Müller, U.; Haller, F.; Wiedemeier, P. Filling Gaps on Stability Data: Development, Validation and Application of a Multianalyte UHPLC-DAD Method to Determine the Stability of Commonly Administered Drugs in Different Carrier Solutions Used in Palliative Care. Analytica 2020, 1, 33-43. https://doi.org/10.3390/analytica1010005
Steuer C, Müller U, Haller F, Wiedemeier P. Filling Gaps on Stability Data: Development, Validation and Application of a Multianalyte UHPLC-DAD Method to Determine the Stability of Commonly Administered Drugs in Different Carrier Solutions Used in Palliative Care. Analytica. 2020; 1(1):33-43. https://doi.org/10.3390/analytica1010005
Chicago/Turabian StyleSteuer, Christian, Ursina Müller, Fiona Haller, and Peter Wiedemeier. 2020. "Filling Gaps on Stability Data: Development, Validation and Application of a Multianalyte UHPLC-DAD Method to Determine the Stability of Commonly Administered Drugs in Different Carrier Solutions Used in Palliative Care" Analytica 1, no. 1: 33-43. https://doi.org/10.3390/analytica1010005
APA StyleSteuer, C., Müller, U., Haller, F., & Wiedemeier, P. (2020). Filling Gaps on Stability Data: Development, Validation and Application of a Multianalyte UHPLC-DAD Method to Determine the Stability of Commonly Administered Drugs in Different Carrier Solutions Used in Palliative Care. Analytica, 1(1), 33-43. https://doi.org/10.3390/analytica1010005