The Relationship of Internalized Weight Bias to Weight Change in Treatment-Seeking Adults with Overweight
Abstract
1. Introduction
2. Materials and Methods
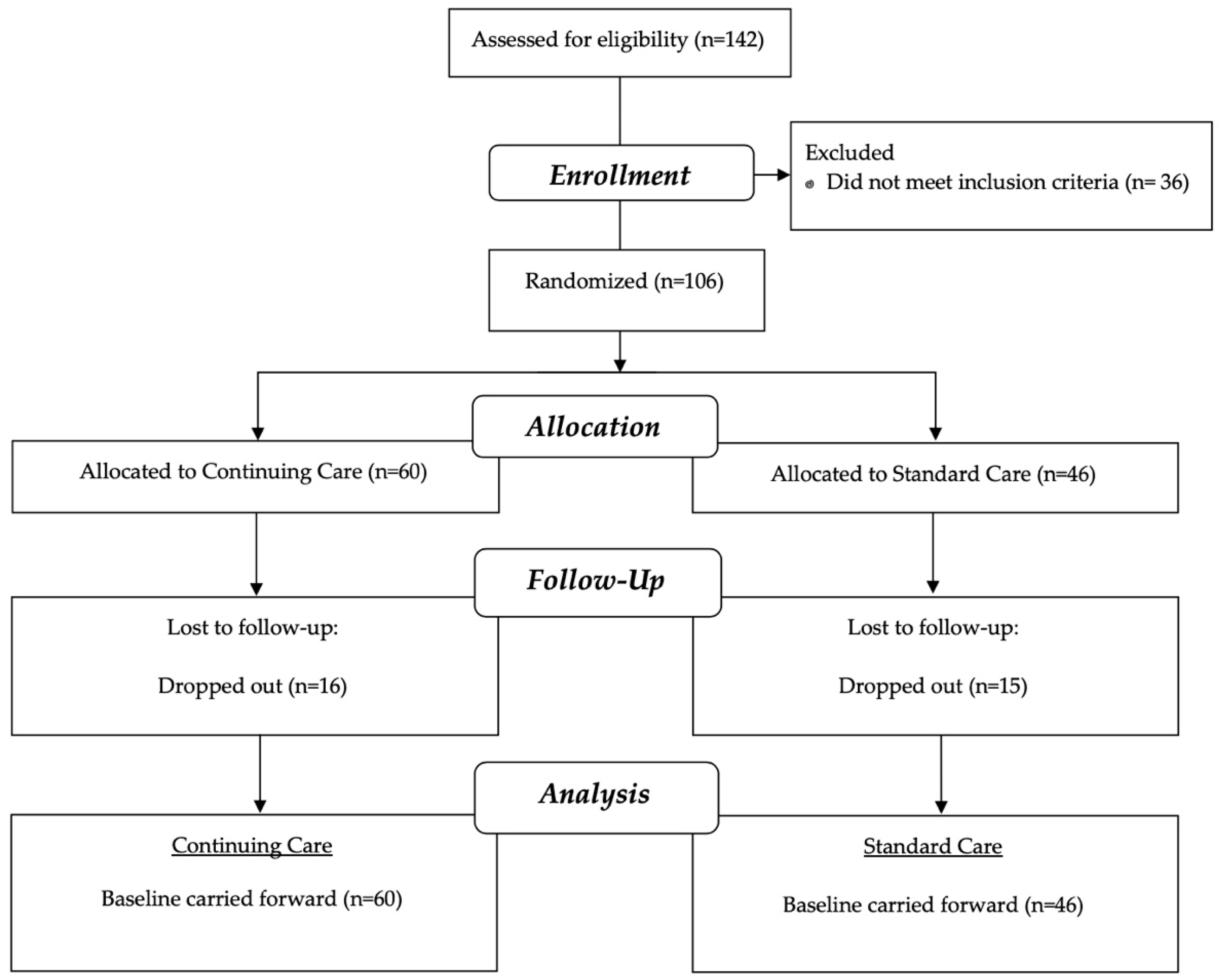
2.1. Study Participants
2.2. Randomization
2.3. Study Procedures
2.4. Measures
2.4.1. Weight Bias Internalization Scale (WBIS)
2.4.2. Anti-Fat Attitudes Questionnaire (AAQ)
2.4.3. Rosenberg Self-Esteem Scale (RSE)
2.4.4. Depression Anxiety Stress Scales (DASS)
2.4.5. Body Shape Questionnaire (BSQ)
2.5. Statistical Analyses
2.5.1. Weight Change at Post-Treatment and Follow-Up
2.5.2. Central Hypothesis: Change in Internalized Weight Bias over Time
2.5.3. RQ1: Relationship of Internalized Weight Bias to Weight Change
2.5.4. RQ2: Relationship of Internalized Weight Bias to Psychological Functioning
3. Results
3.1. Weight Change at Post-Treatment and Follow-Up
3.2. Change in Internalized Weight Bias over Time
3.3. RQ1: How Is Internalized Weight Bias Related to Weight Change?
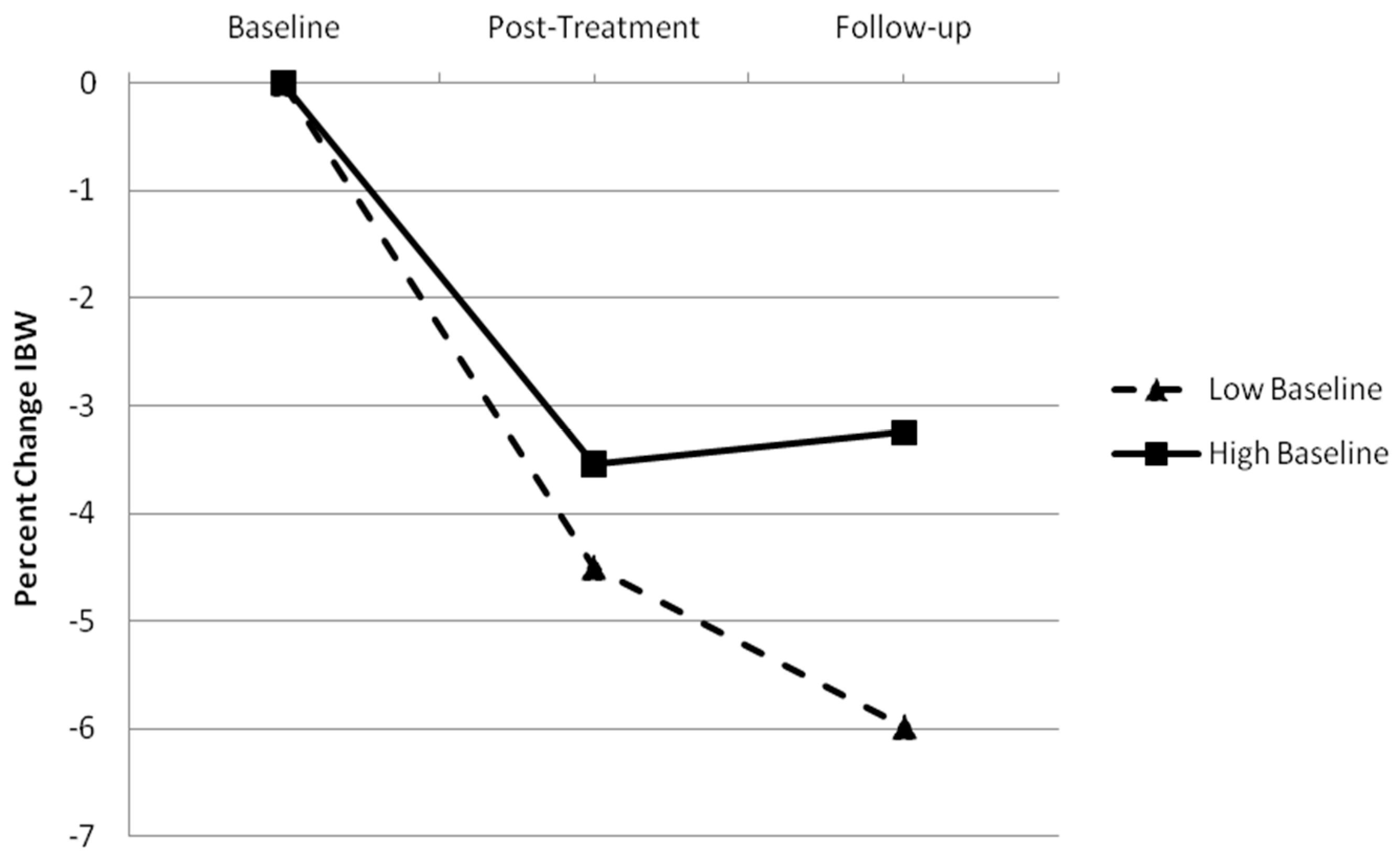
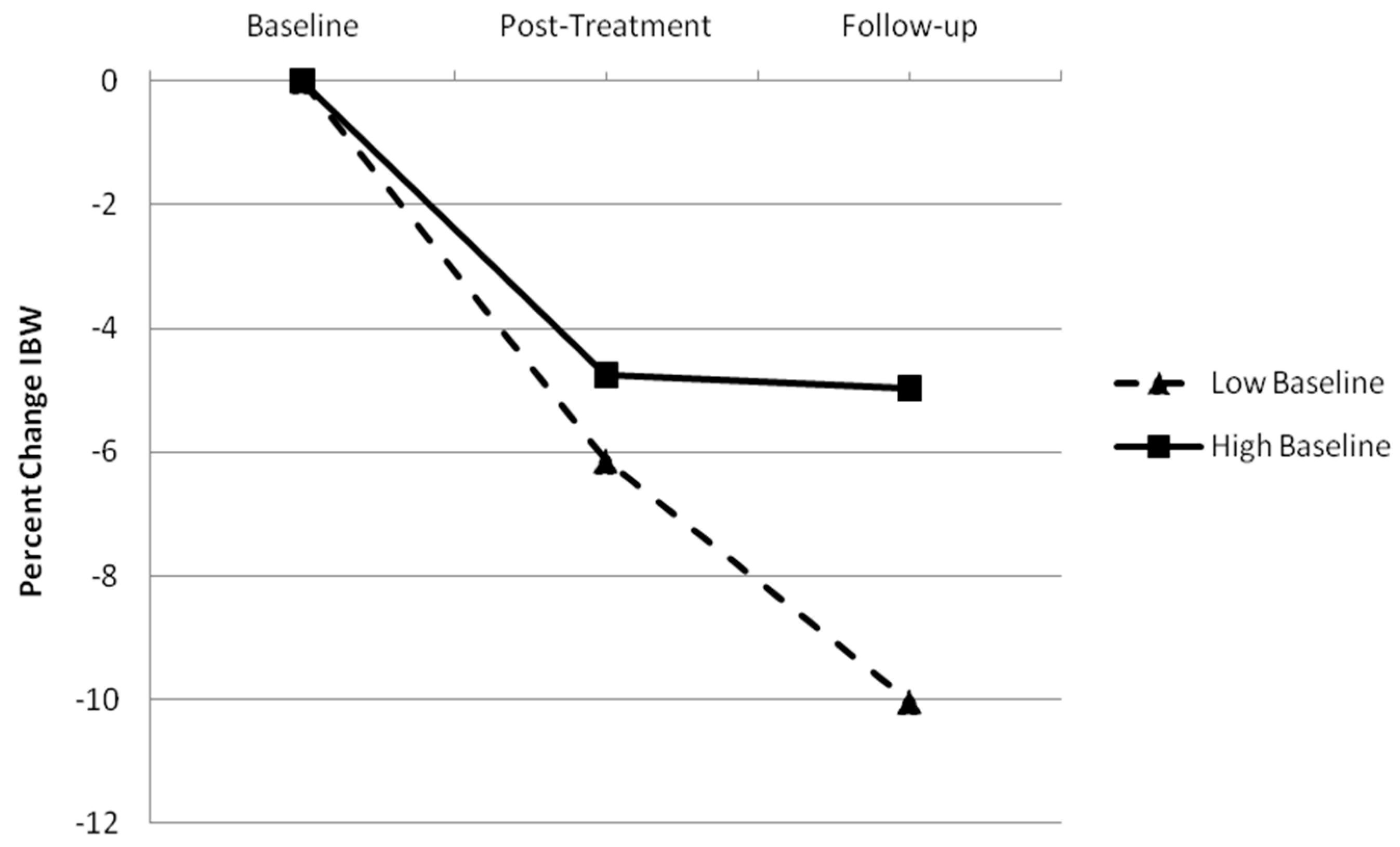
3.3.1. Relationship of Baseline WBIS Score to Weight Change
3.3.2. Correlation between Change in IBW and Internalized Weight Bias and Psychological Functioning
3.4. RQ2: Do Levels of Internalized Weight Bias Predict Psychological Functioning?
Correlation between Internalized Weight Bias and Psychological Functioning
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
Appendix A
| Baseline WBIS | Post-Treatment WBIS | Follow-Up WBIS | |
|---|---|---|---|
| Post-Treatment Scores | |||
| BMI | 0.07 | 0.15 | 0.06 |
| BSQ | 0.53 ** | 0.60 ** | 0.72 ** |
| RSE | −0.41 ** | −0.67 ** | −0.65 ** |
| AAQ Dislike | −0.07 | 0.37 * | a. |
| AAQ Fear of Fat | 0.37 * | 0.66 ** | a. |
| AAQ Willpower | 0.11 | 0.21 | 0.11 |
| DASS Total | 0.19 | 0.30 * | 0.25 |
| DASS Depression | 0.23 | 0.43 ** | 0.37 * |
| DASS Anxiety | 0.25 | 0.21 | 0.2 |
| DASS Stress | 0.06 | 0.15 | 0.11 |
| Follow-Up Scores | |||
| BMI | 0.12 | 0.18 | 0.15 |
| BSQ | 0.28 | 0.15 | a. |
| RSE | −0.47 ** | −0.35 * | a. |
| AAQ Dislike | a. | a. | a. |
| AAQ Fear of Fat | a. | a. | a. |
| AAQ Willpower | a. | a. | a. |
| DASS Total | 0.03 | 0.11 | a. |
| DASS Depression | 0.13 | 0.25 | a. |
| DASS Anxiety | −0.06 | −0.08 | a. |
| DASS Stress | 0.02 | 0.1 | a. |
References
- Fryar, C.D.; Carroll, M.; Afful, J. Prevalence of Overweight, Obesity, and Severe Obesity among Adults Aged 20 and Over: United States, 1960–1962 through 2017–2018. Available online: https://www.cdc.gov/nchs/data/hestat/obesity-adult-17-18/obesity-adult.htm (accessed on 5 December 2021).
- Varkevisser, R.D.M.; van Stralen, M.M.; Kroeze, W.; Ket, J.C.F.; Steenhuis, I.H.M. Determinants of weight loss maintenance: A systematic review. Obes. Rev. 2019, 20, 171–211. [Google Scholar] [CrossRef]
- Christian, J.G.; Tsai, A.G.; Bessesen, D.H. Interpreting weight losses from lifestyle modification trials: Using categorical data. Int. J. Obes. 2010, 34, 207–209. [Google Scholar] [CrossRef] [PubMed]
- Wadden, T.A.; Butryn, M.L.; Byrne, K.J. Efficacy of Lifestyle Modification for Long-Term Weight Control. Obes. Res. 2004, 12, 151S–162S. [Google Scholar] [CrossRef]
- Sarwer, D.B.; von Sydow Green, A.; Vetter, M.L.; Wadden, T.A. Behavior therapy for obesity: Where are we now? Curr. Opin. Endocrinol. Diabetes Obes. 2009, 16, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Lasikiewicz, N.; Myrissa, K.; Hoyland, A.; Lawton, C.L. Psychological benefits of weight loss following behavioural and/or dietary weight loss interventions. A systematic research review. Appetite 2014, 72, 123–137. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, E.M.; Rosen, J.C. A comparison of weight control and weight control plus body image therapy for obese men and women. J. Consult. Clin. Psychol. 2001, 69, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Halyburton, A.K.; Brinkworth, G.D.; Wilson, C.J.; Noakes, M.; Buckley, J.D.; Keogh, J.B.; Clifton, P.M. Low- and high- carbohydrate weight-loss diets have similar effects on mood but not cognitive performance. Am. J. Clin. Nutr. 2007, 86, 580–587. [Google Scholar] [CrossRef] [PubMed]
- Foster, G.D.; Wadden, T.A.; Kendall, P.C.; Stunkard, A.J.; Vogt, R.A. Psychological effects of weight loss and regain: A prospective evaluation. J. Consult. Clin. Psychol. 1996, 64, 752–757. [Google Scholar] [CrossRef] [PubMed]
- Fabricatore, A.N.; Wadden, T.A.; Higginbotham, A.J.; Faulconbridge, L.F.; Nguyen, A.M.; Heymsfield, S.B.; Faith, M.S. Intentional weight loss and changes in symptoms of depression: A systematic review and meta-analysis. Int. J. Obes. 2011, 35, 1363–1376. [Google Scholar] [CrossRef] [PubMed]
- Blaine, B.E.; Rodman, J.; Newman, J.M. Weight loss treatment and psychological well-being: A review and meta-analysis. J. Health Psychol. 2007, 12, 66–82. [Google Scholar] [CrossRef] [PubMed]
- Grilo, C.M.; Masheb, R.M. A randomized controlled comparison of guided self-help cognitive behavioral therapy and behavioral weight loss for binge eating disorder. Behav. Res. Ther. 2005, 43, 1509–1525. [Google Scholar] [CrossRef] [PubMed]
- Wadden, T.A.; Foster, G.D.; Sarwer, D.B.; Anderson, D.A.; Gladis, M.; Sanderson, R.S.; Letchak, R.V.; Berkowitz, R.I.; Phelan, S. Dieting and the development of eating disorders in obese women: Results of a randomized controlled trial. Am. J. Clin. Nutr. 2004, 80, 560–568. [Google Scholar] [CrossRef] [PubMed]
- Palmeira, A.L.; Branco, T.L.; Martins, S.C.; Minderico, C.S.; Silva, M.N.; Vieira, P.N.; Barata, J.T.; Serpa, S.O.; Sardinha, L.B.; Teixeira, P.J. Change in body image and psychological well-being during behavioral obesity treatment: Associations with weight loss and maintenance. Body Image 2010, 7, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Palmeira, A.L.; Markland, D.A.; Silva, M.N.; Branco, T.L.; Martins, S.C.; Minderico, C.S.; Vieira, P.N.; Barata, J.T.; Serpa, S.O.; Sardinha, L.B.; et al. Reciprocal effects among changes in weight, body image, and other psychological factors during behavioral obesity treatment: A mediation analysis. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 9. [Google Scholar] [CrossRef] [PubMed]
- Durso, L.E.; Latner, J.D. Understanding self-directed stigma: Development of the weight bias internalization scale. Obesity 2008, 16 (Suppl. 2), S80–S86. [Google Scholar] [CrossRef]
- Carels, R.A.; Wott, C.B.; Young, K.M.; Gumble, A.; Koball, A.; Oehlhof, M.W. Implicit, explicit, and internalized weight bias and psychosocial maladjustment among treatment-seeking adults. Eat. Behav. 2010, 11, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Durso, L.E.; Latner, J.D.; Ciao, A.C. Weight bias internalization in treatment-seeking overweight adults: Psychometric validation and associations with self-esteem, body image, and mood symptoms. Eat. Behav. 2016, 21, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Pearl, R.L.; White, M.A.; Grilo, C.M. Weight bias internalization, depression, and self-reported health among overweight binge eating disorder patients. Obesity 2014, 22, E142–E148. [Google Scholar] [CrossRef]
- Pearl, R.L.; Puhl, R.M. Weight bias internalization and health: A systematic review. Obes. Rev. 2018, 19, 1141–1163. [Google Scholar] [CrossRef]
- Lillis, J.; Thomas, J.G.; Levin, M.E.; Wing, R.R. Self-stigma and weight loss: The impact of fear of being stigmatized. J. Health Psychol. 2020, 25, 922–930. [Google Scholar] [CrossRef]
- Mensinger, J.L.; Calogero, R.M.; Tylka, T.L. Internalized weight stigma moderates eating behavior outcomes in women with high BMI participating in a healthy living program. Appetite 2016, 102, 32–43. [Google Scholar] [CrossRef] [PubMed]
- Mensinger, J.L.; Meadows, A. Internalized weight stigma mediates and moderates physical activity outcomes during a healthy living program for women with high body mass index. Psychol. Sport Exerc. 2017, 30, 64–72. [Google Scholar] [CrossRef]
- Carels, R.A.; Selensky, J.C.; Rossi, J.; Solar, C.; Hlavka, R. A novel stepped-care approach to weight loss: The role of self-monitoring and health literacy in treatment outcomes. Eat. Behav. 2017, 26, 76–82. [Google Scholar] [CrossRef]
- Olson, K.L.; Lillis, J.; Graham Thomas, J.; Wing, R.R. Prospective evaluation of internalized weight bias and weight change among successful weight-loss maintainers. Obesity 2018, 26, 1888–1892. [Google Scholar] [CrossRef] [PubMed]
- Pearl, R.L.; Puhl, R.M.; Lessard, L.M.; Himmelstein, M.S.; Foster, G.D. Prevalence and correlates of weight bias internalization in weight management: A multinational study. SSM Popul. Health 2021, 13, 100755. [Google Scholar] [CrossRef] [PubMed]
- Lent, M.R.; Napolitano, M.A.; Wood, G.C.; Argyropoulos, G.; Gerhard, G.S.; Hayes, S.; Foster, G.D.; Collins, C.A.; Still, C.D. Internalized weight bias in weight-loss surgery patients: Psychosocial correlates and weight loss outcomes. Obes. Surg. 2014, 24, 2195–2199. [Google Scholar] [CrossRef]
- Raves, D.M.; Brewis, A.; Trainer, S.; Han, S.-Y.; Wutich, A. Bariatric surgery patients’ perceptions of weight-related stigma in healthcare settings impair post-surgery dietary adherence. Front. Psychol. 2016, 7, 1497. [Google Scholar] [CrossRef] [PubMed]
- Latner, J.D.; Ciao, A.C.; Wendicke, A.U.; Murakami, J.M.; Durso, L.E. Community-based behavioral weight-loss treatment: Long-term maintenance of weight loss, physiological, and psychological outcomes. Behav. Res. Ther. 2013, 51, 451–459. [Google Scholar] [CrossRef]
- Group, D.P.P.R. The Diabetes Prevention Program (DPP): Description of lifestyle intervention. Diabetes Care 2002, 25, 2165–2171. [Google Scholar] [CrossRef]
- Crandall, C.S. Prejudice against fat people: Ideology and self-interest. J. Pers. Soc. Psychol. 1994, 66, 882–894. [Google Scholar] [CrossRef]
- Elison, Z.M.; Çiftçi, A. Digesting antifat attitudes: Locus of control and social dominance orientation. Transl. Issues Psychol. Sci. 2015, 1, 262–270. [Google Scholar] [CrossRef]
- Rosenberg, M. Society and the Adolescent Self-Image; Princeton University Press: Princeton, NJ, USA, 1965; pp. 16–38. [Google Scholar]
- Lucas, R.E.; Diener, E.; Suh, E. Discriminant validity of well-being measures. J. Pers. Soc. Psychol. 1996, 71, 616–628. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.; Grilo, C.M.; Masheb, R.M.; White, M.A. Psychological and behavioral correlates of excess weight: Misperception of obese status among persons with class II obesity. Int. J. Eat. Disord. 2010, 43, 628–632. [Google Scholar] [CrossRef] [PubMed]
- Herbozo, S.; Schaefer, L.M.; Thompson, J.K. A comparison of eating disorder psychopathology, appearance satisfaction, and self-esteem in overweight and obese women with and without binge eating. Eat. Behav. 2015, 17, 86–89. [Google Scholar] [CrossRef] [PubMed]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Antony, M.M.; Bieling, P.J.; Cox, B.J.; Enns, M.W.; Swinson, R.P. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol. Assess. 1998, 10, 176–181. [Google Scholar] [CrossRef]
- Setayesh, L.; Ebrahimi, R.; Pooyan, S.; Yarizadeh, H.; Rashidbeygi, E.; Badrooj, N.; Imani, H.; Mirzaei, K. The possible mediatory role of adipokines in the association between low carbohydrate diet and depressive symptoms among overweight and obese women. PLoS ONE 2021, 16, e0257275. [Google Scholar] [CrossRef]
- Coffino, J.A.; Spoor, S.P.; Drach, R.D.; Hormes, J.M. Food insecurity among graduate students: Prevalence and association with depression, anxiety and stress. Public Health Nutr. 2021, 24, 1889–1894. [Google Scholar] [CrossRef]
- Dowson, J.; Henderson, L. The validity of a short version of the body shape questionnaire. Psychiatry Res. 2001, 102, 263–271. [Google Scholar] [CrossRef]
- Cooper, P.J.; Taylor, M.J.; Cooper, Z.; Fairburn, C.G. The development and validation of the body shape questionnaire. Int. J. Eat. Disord. 1987, 6, 485–494. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988; pp. 20–27. [Google Scholar]
- Marshall, R.D.; Latner, J.D.; Masuda, A. Internalized weight bias and disordered eating: The mediating role of body image avoidance and drive for thinness. Front. Psychol. 2020, 10, 2999. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, P.J.; Going, S.B.; Sardinha, L.B.; Lohman, T.G. A review of psychosocial pre-treatment predictors of weight control. Obes. Rev. 2005, 6, 43–65. [Google Scholar] [CrossRef] [PubMed]
- Katzer, L.; Bradshaw, A.J.; Horwath, C.C.; Gray, A.R.; O’Brien, S.; Joyce, J. Evaluation of a “nondieting” stress reduction program for overweight women: A randomized trial. Am. J. Health Promot. 2008, 22, 264–274. [Google Scholar] [CrossRef] [PubMed]
- Robinson, B.E.; Bacon, J.G. The “If only I were thin…” treatment program: Decreasing the stigmatizing effects of fatness. Prof. Psychol. Res. Pract. 1996, 27, 175–183. [Google Scholar] [CrossRef]
- Bacon, L.; Keim, N.L.; Van Loan, M.D.; Derricote, M.; Gale, B.; Kazaks, A.; Stern, J.S. Evaluating a ‘non-diet’ wellness intervention for improvement of metabolic fitness, psychological well-being and eating and activity behaviors. Int. J. Obes. Relat. Metab. Disord. 2002, 26, 854–865. [Google Scholar] [CrossRef]
- Podsakoff, P.M.; MacKenzie, S.B.; Lee, J.Y.; Podsakoff, N.P. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J. Appl. Psychol. 2003, 88, 879–903. [Google Scholar] [CrossRef] [PubMed]
- Dansinger, M.L.; Tatsioni, A.; Wong, J.B.; Chung, M.; Balk, E.M. Meta-analysis: The effect of dietary counseling for weight loss. Ann. Intern. Med. 2007, 147, 41–50. [Google Scholar] [CrossRef]
- Pearl, R.L.; Wadden, T.A.; Bach, C.; Gruber, K.; Leonard, S.; Walsh, O.A.; Tronieri, J.S.; Berkowitz, R.I. Effects of a cognitive-behavioral intervention targeting weight stigma: A randomized controlled trial. J. Consult. Clin. Psychol. 2020, 88, 470–480. [Google Scholar] [CrossRef] [PubMed]
- Pearl, R.L.; Hopkins, C.; Berkowitz, R.; Wadden, T. Group cognitive-behavioral treatment for internalized weight stigma: A pilot study. Eat. Weight Disord. 2018, 23, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Levin, M.E.; Potts, S.; Haeger, J.; Lillis, J. Delivering acceptance and commitment therapy for weight self-stigma through guided self-help: Results from an open pilot trial. Cogn. Behav. Pract. 2018, 25, 87–104. [Google Scholar] [CrossRef]
- Palmeira, L.; Pinto-Gouveia, J.; Cunha, M. Exploring the efficacy of an acceptance, mindfulness & compassionate-based group intervention for women struggling with their weight (Kg-Free): A randomized controlled trial. Appetite 2017, 112, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Berman, M.I.; Morton, S.N.; Hegel, M.T. Uncontrolled pilot study of an acceptance and commitment therapy and health at every size intervention for obese, depressed women: Accept yourself! Psychotherapy 2016, 53, 462–467. [Google Scholar] [CrossRef] [PubMed]
- Lillis, J.; Hayes, S.C.; Bunting, K.; Masuda, A. Teaching acceptance and mindfulness to improve the lives of the obese: A preliminary test of a theoretical model. Ann. Behav. Med. 2009, 37, 58–69. [Google Scholar] [CrossRef] [PubMed]
| Measure | Baseline | Post-Treatment | Six-Month Follow-Up | Univariate F (df1, df2) |
|---|---|---|---|---|
| BMI (Completers) | 35.66 (7.67) a | 32.43 (6.67) b | 31.92 (6.13) b | 22.83 (2, 60) * |
| BMI (ITT) | 35.66 (7.67) a | 34.73 (7.91) b | 34.21 (7.99) c | 30.27 (1.72, 169.74) *,† |
| WBIS | 3.83 (1.05) a | 3.55 (0.72) b | 3.40 (1.30) c | 12.05 (1.79, 185.89) *,† |
| BSQ | 3.61 (1.11) a | 2.86 (1.14) a | 2.95 (1.18) a | 0.26 (1.88, 184.12) † |
| RSE | 3.12 (0.51) a | 3.31 (0.51) b | 3.23 (0.54) b | 10.07 (1.81, 187.68) *,† |
| AAQ Dislike | 1.46 (1.19) a | 1.23 (1.45) b | 0.48 (0.57) c | 60.13 (2, 208) * |
| AAQ Fear of Fat | 4.93 (2.18) a | 4.74 (2.33) a | 3.81 (3.04) b | 21.37 (1.79, 186.63) *,† |
| AAQ Willpower | 4.68 (1.77) a | 4.66 (1.88) a | 3.69 (2.02) b | 32.58 (1.70, 176.34) *,† |
| DASS Total | 0.57 (0.44) a | 0.49 (0.44) a | 1.02 (0.62) b | 66.69 (2, 208) * |
| DASS Depression | 0.64 (0.51) a | 0.46 (0.50) b | 0.98 (0.67) c | 51.95 (2, 208) * |
| DASS Anxiety | 0.53 (0.43) a | 0.35 (0.40) b | 0.84 (0.61) c | 51.14 (2, 208) * |
| DASS Stress | 0.83 (0.51) a | 0.67 (0.60) b | 1.25 (0.72) c | 49.13 (2, 208) * |
| % Change in Body Weight at Post-Treatment | % Change in Body Weight at Follow-Up | |
|---|---|---|
| Baseline Body Mass Index | 0.13 | 0.10 |
| Baseline Weight Bias Internalization Scale | 0.14 | 0.26 ** |
| Baseline Body Shape Questionnaire | 0.16 | 0.22 * |
| Baseline Rosenberg Self-Esteem Scale | −0.21 * | −0.28 ** |
| Baseline Anti-Fat Attitudes Scale Total Score | 0.02 | −0.02 |
| Baseline Anti-Fat Attitudes Scale Dislike subscale | −0.03 | −0.03 |
| Baseline Anti-Fat Attitudes Scale Fear of Fat subscale | 0.01 | 0.13 |
| Baseline Anti-Fat Attitudes Scale Willpower subscale | 0.03 | −0.15 |
| Baseline Depression Anxiety Stress Scale Total Score | 0.15 | 0.20 |
| Baseline Depression Anxiety Stress Scale Depression subscale | 0.05 | 0.11 |
| Baseline Depression Anxiety Stress Scale Anxiety subscale | 0.00 | 0.07 |
| Baseline Depression Anxiety Stress Scale Stress subscale | 0.22 | 0.22 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marshall, R.D.; O’Brien, K.S.; Latner, J.D. The Relationship of Internalized Weight Bias to Weight Change in Treatment-Seeking Adults with Overweight. Obesities 2022, 2, 21-34. https://doi.org/10.3390/obesities2010003
Marshall RD, O’Brien KS, Latner JD. The Relationship of Internalized Weight Bias to Weight Change in Treatment-Seeking Adults with Overweight. Obesities. 2022; 2(1):21-34. https://doi.org/10.3390/obesities2010003
Chicago/Turabian StyleMarshall, Rachel D., Kerry S. O’Brien, and Janet D. Latner. 2022. "The Relationship of Internalized Weight Bias to Weight Change in Treatment-Seeking Adults with Overweight" Obesities 2, no. 1: 21-34. https://doi.org/10.3390/obesities2010003
APA StyleMarshall, R. D., O’Brien, K. S., & Latner, J. D. (2022). The Relationship of Internalized Weight Bias to Weight Change in Treatment-Seeking Adults with Overweight. Obesities, 2(1), 21-34. https://doi.org/10.3390/obesities2010003







