Abstract
This study evaluated the effectiveness of strategies used to recruit and retain overweight, inactive adults with intermediate hyperglycaemia (IHG) to a novel walking programme. Participant compliance to the nine-month randomised controlled trial (RCT) is also presented. Inactive overweight (BMI ≥ 25 kg/m2) adults (N = 42; n = 19 male, n = 23 female) aged between 18–65 years, with IHG were identified via three recruitment strategies (NHS database reviews, diabetic clinics, and a University population). Participants were randomly assigned to either Intervention Group (IG n = 22; n = 11 male, n = 11 female) or Usual Care (UC n = 20; n = 8 male, n = 12 female). IG followed a nine-month novel behaviour change intervention where they walked in accordance with physical activity guidelines using the beat of music to maintain appropriate cadence. UC received standard physical activity advice. Recruitment, retention, and intervention compliance were calculated using descriptive statistics (means or frequencies). Recruiting from a University population was the most successful strategy (64.2% response rate) followed by NHS database reviews (35.8%) and then diabetic clinics (0%). Study retention was ≥80% in both groups throughout the RCT. Intervention compliance was highest from baseline to four months (70.1 ± 39.2%) and decreased as the study progressed (43.4 ± 56.1% at four to six months and 37.5 ± 43.5% at follow-up). In total, 71.4% of IG walking completed throughout the study was at least moderate intensity. A novel walking intervention incorporating the use of music along with behaviour change techniques appears to positively influence the recruitment, retention, and walking compliance of this population.
1. Introduction
IHG is a hyperglycaemic state which is sufficient to cause glucometabolic dysfunction in target tissues, however due to its asymptomatic nature, hyperglycaemia often remains clinically undiagnosed before type 2 diabetes is identified [1]. As individuals with IHG are often unaware they have the pre-disease condition, identification and recruitment of this population is difficult. Furthermore, as IHG is usually asymptomatic and is considered an intermediate state rather than a disease [1,2], once diagnosed the severity and risks associated with the condition are often overlooked or generally underestimated by sufferers. IHG is not only associated with impaired glycaemic function but is also associated with other comorbidities and risks. A constant state of hyperglycaemia can cause glucometabolic dysfunction leading to damaged organs associated with cardiovascular disease including the heart and its blood vessels [3,4]. In overweight populations during the intermediate state, adaptations in response to chronic exposure to excess adipose tissue may cause impaired glucometabolic responses, increased oxidative stress, increased inflammation, endothelium dysfunction as well as impaired behavioural and psychological effects [4,5,6,7,8,9]. It is therefore salient that IHG sufferers are identified to reduce the risk of type 2 diabetes and developing associated comorbidities.
Quantifying the extent of this problem remains difficult. Most recent figures estimate that approximately 88 million US adults, more than one in three, meet the diagnostic criteria for IHG [10]. Prevalence within the Irish adult population is estimated at 18.7% [11]. The Diabetes Mellitus and Vascular health initiative (DMVhi) screened 29,144 adults aged 45–75 years in the Republic of Ireland results identified undetected abnormal glucose in at least 11.8% of Irish adults aged 45–75 years [12]. In the UK, around seven million people are projected to have IHG [2,13] and it is now estimated that in England one in every three people have IHG [2,14]. Overweight and obesity increase the risk of developing type 2 diabetes by 80–85% [15]. Six in ten Irish Adults are overweight or obese (37% overweight and a further 23% obese) and in the UK 66.6% of men and 57.2% of women were reported as overweight or obese in 2014 [16,17,18]. It is well established that increasing physical activity behaviour within overweight adults with IHG is one method to reduce the risk of developing glucometabolic and cardiovascular disease complications [2,4,19]. However, difficulties regarding the identification and recruitment of this significant population must be explored.
Once individuals become aware of their IHG condition and are recruited onto physical activity interventions, further challenges include retention, maintenance, and compliance. A recent systematic review and meta-analysis highlighted when assessing physical activity intervention feasibility, group differences in outcomes should be supported by reporting adoption, maintenance, adherence (compliance), and retention rates [20]. Therefore, intervention effectiveness should consider both the changes in outcome measures in addition to the implementation of physical activity interventions within the real world [20]. Reporting of additional study effectiveness rates along with changes in outcome measures would enable researchers to fully understand the real-world effectiveness of physical activity interventions. This study aims to report the strategies used to recruit overweight inactive adults with IHG to a free-living walking intervention with behaviour change support. This work also presents study retention and compliance to the novel free-living walking to music programme.
2. Materials and Methods
2.1. Participants
Inactive overweight (BMI ≥ 25 kg/m2) adults aged between 18–65 years, with IHG were recruited via one of the recruitment processes outlined below. The study was conducted in accordance with the Declaration of Helsinki, and ethical approval was received from the Ulster University Research Ethics Filter Committee and the Office for Research Ethics Committees in Northern Ireland (Approval number: 12/NI/0063, 21 June 2012).
2.2. Study Phase One: Recruitment Strategies
I. NHS Database Reviews: A review of previous oral glucose tolerance tests (OGTTs) completed within the South Eastern Health and Social Care Trust (SEHSCT) and the Western Health and Social Care Trust (WHSCT) in the previous three years (21 June 2010 and 20 May 2013) was performed. Following review, individuals who met the diagnostic criteria (fasting glucose 5.6–6.9 mmol/L−1 and/or two-hour glucose 7.8–11.0 mmol/L−1) were invited to take part by postal correspondence.
II. Diabetic Clinics: Recruitment from diabetic clinics based at the Ulster Hospital and Altnagelvin Area Hospital was conducted by the relevant consultant or designated nurse. The relevant health professional made initial contact with potential participants who were referred to the clinics due to their risk of developing type 2 diabetes because of being overweight, obese or with a family history of type 2 diabetes. Individuals were verbally advised about the study and offered a participant information sheet with the researchers contact details if they wished to receive further information.
III. University Population: Overweight University staff and student volunteers (BMI ≥ 25 kg/m2; across all Ulster University campuses) were recruited via email, poster, and word-of-mouth. Following an initial consultation interested individuals were invited to take part in Study Phase Two. If participants met the diagnostic criteria (fasting glucose 5.6–6.9 mmol/L−1 and/or two-hour glucose 7.8–11.0 mmol/L−1) a final screening letter aligned with study inclusion and exclusion criteria was sent to their G.P. to confirm suitability to participate in the research.
Following recruitment (by all 3 methods) interested individuals received a participant information sheet. Participants were required to provide informed consent and complete screening documents including a health history questionnaire before being invited to take part in the second phase of the study (glucometabolic and anthropometric measures). At this point participants completed a preferred choice of communication form to indicate their preferred time and mode of communication (telephone call, mobile phone call, SMS message, letter via post or email) throughout the study. Individuals were excluded if they had progressed to type 2 diabetes, returned to normoglycaemia or were aged ≤18 years of age or ≥65 years of age at inception of the study. Individuals with a history of cardiovascular disease events or an illness which would contraindicate participation in the intervention were not permitted to take part in the study. Finally, smokers or individuals prescribed medication which may interfere with blood biochemistry were excluded.
2.3. Study Phase Two: Glucometabolic and Anthropometric Status
Following expression of interest and providing informed consent, participants were invited to attend a screening to ensure their blood glucose response met the diagnostic criteria for the study (fasting glucose 5.6–6.9 mmol/L−1 and/or two-hour glucose 7.8–11.0 mmol/L−1; see Glucometabolic Status below). Individual height (cm), body mass (kg) and BMI (kg/m2) were also assessed to ensure participants had a BMI ≥ 25 (see Anthropometric Measurements below). Study Phase two took place either at their local hospital or at the Ulster University Human Performance Laboratory.
2.3.1. Glucometabolic Status
Fasted venous blood samples were collected following an overnight fast (at least eight hours) and 24 h rest from vigorous physical activity. Blood samples were collected via venepuncture method in a 2 mL sodium fluoride K3EDTA blood tube to inhibit glycolysis. Fasting plasma glucose (mmol/L−1) samples were analysed using the UV test principle. Participants with fasting plasma glucose 5.6–6.9 mmol/L−1 (110–125 mg/dL) underwent an OGTT to determine glucose tolerance status using standard methods [21,22].
2.3.2. Anthropometric Measurements
Height (cm) and body mass (kg) were recorded using a freestanding stadiometer (Holtain Ltd, Crymych, UK) and scales, respectively (Seca delta, Hamburg, Germany). Measurements were completed wearing light clothing, without footwear and in a fasted state. Height (cm) and body mass (kg) were recorded to the nearest 0.1 cm and 0.1 kg, respectively. BMI (kg/m2) was calculated for all participants at each assessment time point using the following equation [23]. BMI (kg/m2) = Body mass (kg)/Height (m2).
2.4. Study Phase Three: Physical Activity
To ensure participants were inactive, all individuals wore an Actigraph GT3X accelerometer (Actilife, Pensacola, FL, USA) for all waking hours on seven consecutive days to assess physical activity behaviour. This study employed the Freedson et al. activity cut-points for adults [24]. Devices were initialised with a start and end time of one week or seven days in duration. Non-wear periods were defined as 60 min or more of consecutive zeros. Similar to previous research sleep periods were ignored and considered non-wear time [25] ≥10 h of wear time was considered a valid day. The minimum number of valid days required was three days [26]. Time in sedentary behaviour was defined as 0–99 activity counts per minute (cpm). Time in light intensity was defined as 100–1951 activity cpm. A total of 1952–5724 activity cpm was considered moderate intensity activity and 5725–9498 activity cpm was considered vigorous intensity activity. ≥9499 activity cpm was considered very vigorous intensity activity.
2.5. Study Phase Four: Participant Randomisation and Experimental Design
When participants satisfied Study Phase Two and Three criteria a blinded third-party researcher randomly assigned participants (Figure 1) to either IG or UC. To reduce the risk of researcher bias, the name of the designated group was placed in a sealed opaque envelope which the participant then chose at random. IG participants received an individualised progressive weekly walking programme designed to increase moderate intensity walking to 30 min per day based on current physical activity guidelines for health [27]. IG participants used an MP3 music player (iPod touch 4, Apple Inc., Cupertino, CA, USA) with individually selected music set to a predetermined beat to regulate walking cadence [5]. Music tempo was individually established in accordance with previous height-related stride rate recommendations determined by Rowe and colleagues [28] to elicit moderate intensity exercise for each individual (50–70% maximum heart rate: 90–113 steps/min−1). The MP3 device was held in a case attached to a waistband. IG participants were instructed on how to use and store the data and MP3 device throughout the study. Cadence (steps/min−1) was recorded and saved through the use of the inbuilt accelerometer and app and later analysed via a Matlab application (MATLAB, The MathWorks Inc., Natick, MA, USA, 2014). UC received the standard or ‘usual care’ they would receive from their local health professional. This consisted of a standard physical activity information sheet only [27]. The intervention was completed over a 19-month period. The first participant was randomised onto the study in August 2012, with the final participant completing the nine-month intervention in March 2014.
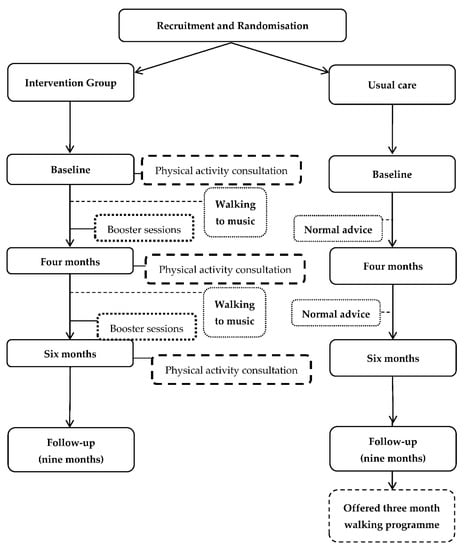
Figure 1.
Outline of the RCT delivery and assessment time points at baseline, four, six and nine (follow-up) months.
Assessment of RCT outcome measures included a range of clinical, physiological and behaviour change parameters at baseline, four, six and nine (follow-up) months as outlined in Figure 1 (full details of outcome measures are available in a previous publication [5]). At baseline, four- and six-month assessments, the IG participants received physical activity consultations. Between assessment points IG participants received booster sessions via their preferred mode of contact identified during Study Phase Two (Figure 1) [5] and were asked to complete their walking programme to music (an overview of behaviour change techniques and strategies used was previously published [5]). UC participants received no contact between assessments. At the end of the programme the UC participants were offered a three-month walking programme.
2.6. Sample Size and Statistical Analysis
In order to detect a difference of 1.0 mmol/L−1 in two-hour glucose levels between the IG and UC group at nine months, this study aimed to recruit 31 people per group. This calculation was based on a statistical power of 80%, a significance of 0.05, and a SD of 1.0 mmol/L−1. This power calculation also allowed for 50% dropout rate (non-completers and participants who develop type 2 diabetes) [29]. Therefore, to achieve statistical power at least 16 participants per group were required to complete the six-month intervention.
Participant recruitment and retention rates were calculated using descriptive statistics (means or frequencies). IG % walk compliance (volume and duration) was assessed by comparing the app recorded walks to walking prescribed in each programme. Walking intensity compliance was assessed by calculating the percentage of walks that, on average, were completed at or above the predetermined target cadence. An Independent Samples t-test was used to examine differences between groups at baseline (p < 0.05). All data were presented as mean value ± standard deviation or percentages. All statistical analysis was carried out using Microsoft Excel and SPSS version 22.0 for Windows (SPSS, Chicago, IL, USA).
3. Results
3.1. Recruitment and Randomisation
Following patient database searches n = 305 invitation letters (n = 256 SEHSCT, n = 49 WHSCT) were posted to suitable individuals who met the diagnostic criteria (fasting glucose 5.6–6.9 mmol/L−1 and/or two-hour glucose 7.8–11.0 mmol/L−1). Recruitment strategy one (NHS database reviews) resulted in n = 49 (n = 43 SEHSCT, n = 6 WHSCT) individuals expressing interest in taking part in the study. These individuals were invited to take part in Study Phase Two to ensure they met the study inclusion criteria. Overall response rate for recruitment strategy one was 16.1% (16.8% SEHSCT, 12.2% WHSCT). No participants (n = 0; 0%) were recruited from recruitment strategy two (Clinician led diabetic clinics). Recruitment strategy three (University population) generated n = 88 interested responses. Following an initial consultation these individuals (n = 88) were invited to take part in Study Phase Two. Overall, 137 responses were received from recruitment strategy one (n = 49), two (n = 0) and three (n = 88). Recruitment strategy three achieved the greatest response rate (64.2%). Recruitment strategy one accounted for 35.8% of overall responses (31.4% SEHSCT; 4.4% WHSCT) and recruitment strategy two resulted in no responses (0%). Figure 2 provides an overview of the recruitment strategies and randomisation procedures.
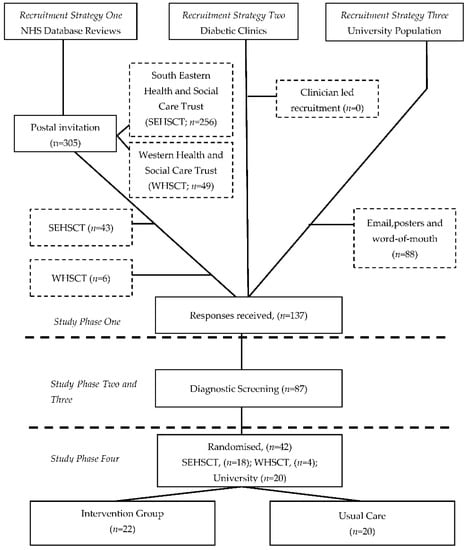
Figure 2.
Overview of Study Phase One, Two, Three and Four.
63.5% (n = 87) of respondents to Study Phase One (n = 137) accepted the invitation to complete Study Phase Two and Three to ensure they met the study inclusion criteria (Figure 2). Study Phase Three found approximately 65% of participants’ typical days (10 h) were spent in sedentary activity (≤100 cpm), 33% spent in light intensity activity (100–1951 cpm), 3% was spent in moderate intensity activity (1952–5724 cpm) and only 0.12% and 0.01% spent in vigorous intensity (5725–9498 cpm) and very vigorous intensity activity (≥9499 cpm), respectively.
48.3% (N = 42; IG n = 22, 50% (n = 11) male, 50% (n = 11) female; UC n = 20, 36.4% (n = 8) male, 54.6% (n = 12) female) of participants invited to complete Study Phase Two and Three met the inclusion criteria and were randomised onto the study (Study Phase Four). Ethnicity ranged within groups (IG 95% Caucasian and 5% Asian; UC participants 95% Caucasians and 5% Asian). No significant differences were observed between groups at baseline (p > 0.05; see Table 1 for participants’ baseline characteristics).

Table 1.
Overall and group baseline descriptives following randomisation. M = mean, SD = standard deviation, Min = minimum range, Max = maximum range, FPG = fasting plasma glucose, 2 h Gluc = two-hour glucose concentration. Independent Samples t-test found no statistically significant differences between groups at baseline (p > 0.05).
3.2. Study Retention
Participants were randomly assigned to an IG (n = 22) or UC group (n = 20) as part of the nine-month walking intervention (Figure 3). Five participants (n = 5; IG n = 5) who completed initial screening assessments only, i.e., OGTT (mmol/L−1), height (cm), body mass (kg) and BMI (kg/m2) were excluded from other baseline measurements due to an undisclosed cardiac event (n = 1), returning to normal glucose control (n = 1) and progressing to type 2 diabetes (n = 3). Therefore, a total of 37 participants (n = 37) progressed through the intervention (Figure 3). IG participants (n = 17) walked to self-selected music with a predetermined tempo based upon Rowe et al. [28] height related stride rate guidelines and received behavioural change support [5]. UC participants (n = 20) received a standard PA information sheet only. Study retention rates are provided in Table 2. Details of participant retention including exclusions and drop-outs are detailed in Figure 3.
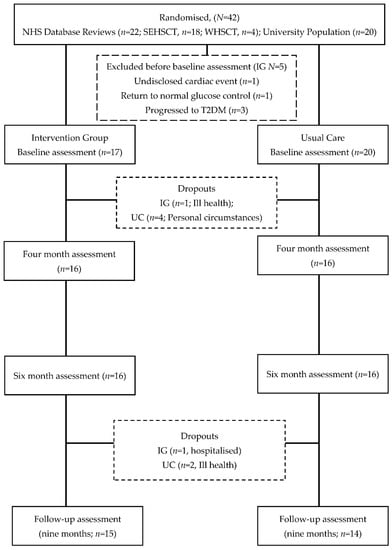
Figure 3.
Flowchart of participant retention from baseline to follow-up (nine months).

Table 2.
Outline of participant retention rates throughout the study.
3.3. Walking Programme Compliance
Walking volume and duration compliance among IG participants from baseline to four months was 70.1 ± 39.2% (range 9.0% to 158.4%). Walking compliance (volume and duration) decreased to 43.4 ± 56.1% (range 0% to 225%) from four to six months. Walking compliance (volume and duration) at follow-up was recorded as 37.5 ± 43.5% (range 0% to 125.3%). In total, 71.4%, 79.5% and 73.3% of walking completed was at least moderate intensity (predetermined target cadence) between baseline to four months, four to six months and six to nine months, respectively.
4. Discussion
This study describes the effectiveness of the strategies used to recruit overweight, inactive adults with IHG to a nine-month free-living walking and behaviour change RCT. Participant retention and intervention compliance were also examined. This study found that recruiting from a University population achieved the highest response rate accounting for 64.2% of responses received. Overall study retention rates were ≥80% in both groups throughout the RCT. Intervention compliance (volume and duration) was highest from baseline to four months (70.1 ± 39.2%) and decreased as the study progressed (43.4 ± 56.1% four to six months and 37.5 ± 43.5% six months to follow-up). Interestingly, ≥71.4% of walking completed was at least moderate intensity (predetermined target cadence) throughout the nine-month study. These latter results suggest walking to music with a predetermined individualised tempo may provide a novel method that enables this population to achieve moderate intensity activity in a free-living environment.
Several key issues exist when planning trials involving IHG participants. Identification of this asymptomatic population is the initial challenge faced by researchers and clinicians. Furthermore, as IHG is largely asymptomatic and is considered an intermediate state rather than a disease [1], once diagnosed, the severity and risks associated with the condition are often overlooked or generally underestimated by those affected. Thus, recruiting such ‘unaware’ high risk participants proves problematic. This study used three recruitment strategies in an effort to achieve a sufficient sample size. Recruiting through email and poster advertisements within the University setting (recruitment strategy three) was the most productive approach achieving almost two thirds of study responses (64.2%). NHS databases were reviewed (recruitment strategy one), and once suitable individuals were identified based on their fasting plasma glucose and/or OGTT records, invitation letters (n = 305) were posted. Following this lengthy process, a response rate of 16.1% (n = 49) was achieved. This contributed to approximately one third (35.8%) of the overall study response rate. No participants (n = 0, 0%) were recruited from recruitment strategy two (Clinician led recruitment via diabetic clinics). A recent review found overall recruitment rates of minority populations (South Asian) in behavioural interventions to improve type 2 diabetes outcomes were low [30]. Twelve studies had a mean recruitment rate of 44% among those screened, and nine studies with complete information on eligibility had a mean recruitment rate of 65.8% among those eligible [30]. Horowitz and colleagues [31] used community-based participatory research to compare the effectiveness of different strategies in recruiting and enrolling adults with prediabetes into a peer-led diabetes prevention intervention. Similar to the current study that used a campus-based researcher to recruit from the University population, the partner-led approach in which community partners developed and managed the recruitment efforts at their sites was most successful, recruiting 68% of people enrolled [31]. This was also the most efficient strategy with 34% of those approached through partners ultimately enrolled, versus 0–17% through the other four strategies (recruiting through clinicians, at large public events, organising special local recruitment events and recruiting at local organisations) [31]. These researchers highlighted the value of a partner-led recruitment to identify, reach out and motivate a vulnerable population into research, using techniques that may be unfamiliar to researchers, but are nevertheless rigorous and effective [31].
Once this at-risk population have been identified the challenge of ensuring participants are retained continue. Additionally, maintaining long term physical activity change in a free-living environment proves problematic. Study retention rates were ≥80% in both groups throughout this RCT. Dissatisfaction following the randomisation process often attributes to large drop-out rates of control group participants in trials [32]; however, in the current study UC retention rates were 80% throughout the nine-months. Not unusually study retention rates were higher for IG participants compared to UC participants at each assessment point (94.1% vs. 80% four months, 94.1% vs. 80% six months, and 88.3% vs. 80% nine months, respectively; Table 2). This may be attributed to the behavioural change support and novel techniques (walking to music via use of an app) used to facilitate IG participants to achieve and maintain the walking programme. Another potential contributing factor to the higher IG retention rates may be the opportunity presented to the researcher to build rapport during the physical activity consultation process. The importance of building rapport with eligible individuals can often be underestimated, however, gaining trust and showing empathy particularly towards at risk populations may contribute positively to recruitment and retention rates. The use of motivational interviewing, a participant centred behaviour change technique, with at-risk populations is one approach that has received much attention in recent years [33,34,35] and was applied within this RCT. A recent review [30] reported the mean retention rate of a South Asian ethnic minority population to behavioural interventions aimed at reducing type 2 diabetes was 79.4% across all 14 studies examined. However, these researchers highlighted that unstandardised and inconsistent reporting limited their ability to draw any conclusions regarding the best strategies to maximise recruitment and retention [30] reinforcing the need for researchers to sufficiently report recruitment strategies and retention methods and rates.
It is evident that individuals at risk of developing type 2 diabetes do not engage in adequate physical activity [6] and a minority of this population (<55%) have reported completing current physical activity guidelines for health [36]. Once participants have been recruited and randomised into a physical activity RCT, ensuring this typically inactive population achieve and maintain the prescribed activity is another challenge facing researchers and clinicians. Willenger and colleagues [20] concluded that adoption (an individual’s uptake of physical activity at recommended levels) and maintenance (long-term behaviour change) rates were rarely reported within physical activity interventions. In the current study IG walking compliance (volume and duration) was highest in the first four months of the study (70.1 ± 39.2%) after which a decrease was observed at each assessment point. One suggestion may be that as behavioural change support techniques were tapered as the study progressed, particularly after four months, this may have had a direct impact on IG walking compliance. Current physical activity guidelines recommend that physical activity should be at least moderate intensity to elicit health benefits [27]. A common issue facing researchers seeking to promote physical activity guidelines for health is ensuring that participants can self-regulate physical activity intensity in free-living environments. Interestingly, ≥71.4% of walking completed was at least moderate intensity (predetermined target cadence) throughout this nine-month study. These latter results suggest walking to music with a predetermined individualised tempo may provide a novel method that enables this population to achieve at least moderate intensity activity in a free-living environment.
Limitations
This study has a number of limitations. Although this study met its target sample size, it included a relatively small number of overall participants (N = 42). Therefore, generalisability of its results to larger populations should be cautioned. This research should be replicated in larger scale studies which include greater sample sizes. This study recruited participants from within Northern Ireland, replication of this intervention within other countries and including a broader range of demographics, e.g., ethnicity and socioeconomic characteristics, should be considered by future research. The compliance of these populations to the walking intervention and the effects on health outcomes within larger sample sizes also merits further study. As discussed previously the value of an on-campus or on-site researcher led recruitment appears to be the most productive recruitment strategy. Likely in part due to the opportunity presented to firstly identify and then build rapport and motivate potential participants. The current study had one researcher on-campus performing this role. While it is appreciated that resources are often a limiting factor, if a team of researchers were available to complete this role in future studies, perhaps the pool of potential participants targeted and identified would be larger resulting in a greater sample size.
5. Conclusions
This work explores the effectiveness of various recruitment strategies, study retention rates and walking compliance within the nine-month free-living RCT. This research highlights the issues surrounding identification of undiagnosed adults at risk of developing type 2 diabetes. Study retention rates were explored, and results suggest that the use of novel techniques, i.e., music and technology coupled with behaviour change techniques and skills such as purposefully gaining trust and displaying empathy, may positively affect the retention of intervention and control group participants. As recruitment and retention of this overweight IHG population remains a global challenge future studies should aim to replicate the use of this novel intervention, using individualised music and behaviour change support, to examine its effects on larger sample sizes with varying demographics, e.g., ethnicity and socioeconomic status. Compliance of these populations to the novel walking intervention and its resultant effects on health outcomes also merit further study.
In conclusion, there is a need for participant recruitment strategies, study retention and intervention compliance rates to be reliably reported by researchers to encourage successful delivery of physical activity interventions aimed at managing IHG and reducing the incidence of type 2 diabetes. It is generally accepted that populations at risk of developing type 2 diabetes, i.e., overweight inactive adults with IHG, are a cohort that are initially quite difficult to identify and then challenging to recruit, engage and retain in research. Consistent reporting and publication of this information will ensure research is guided and underpinned by the most efficient strategies.
Author Contributions
The following individual contributions were made: Conceptualization, M.M., D.R., A.H. and M.F.; methodology, M.F., M.M., G.D., D.R., A.H., E.D. and T.T.; software, M.F. and A.H.; validation, M.F. and A.H.; formal analysis, M.F. and A.N.; investigation, M.F.; resources, M.M., A.H., E.D. and T.T.; data curation, M.F.; writing—original draft preparation, M.F.; writing—review and editing, M.F., M.M., A.M. and G.D.; supervision, M.M., A.M. and G.D.; project administration, M.F. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by a Department of Education (Northern Ireland) grant as part of the PhD project of Maria Faulkner.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ulster University Research Ethics Committee and the Office for Research Ethics Northern Ireland (Approval number: 12/NI/0063).
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data Availability Statement
Data may be made available upon request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tuomilehto, J. Definitions of intermediate hyperglycaemia and progression to type 2 diabetes. Lancet Diabetes Endocrinol. 2019, 7, 243–245. [Google Scholar] [CrossRef]
- Diabetes.co.uk. Prediabetes (Borderline Diabetes). Available online: https://www.diabetes.co.uk/pre-diabetes.html (accessed on 20 April 2021).
- Hardman, A.E.; Stensel, D.J. Physical Activity and Health: The Evidence Explained; Routledge: London, UK, 2009. [Google Scholar]
- American Diabetes Association Standards of medical care in diabetes–2014. Diabetes Care 2014, 37 (Suppl. S1), S14–S80. [CrossRef] [PubMed] [Green Version]
- Faulkner, M.; Murphy, M.; Davison, G.; Rowe, D.; Hewitt, A.; Nevill, A.; Duly, E.; Trinick, T.; McNeilly, A.M. The physiological effects of a walking to music intervention in adults with intermediate hyperglycemia. Open J. Endocr. Metab. Dis. 2021, 11, 43–51. [Google Scholar] [CrossRef]
- Shah, A.D.; Vittinghoff, E.; Kandula, N.R.; Srivastava, S.; Kanaya, A.M. Correlates of prediabetes and type II diabetes in US South Asians: Findings from the mediators of atherosclerosis in South Asians living in America (MASALA) study. Ann. Epidemiol. 2015, 25, 77–83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diabetes.co.uk. Diabetes and Obesity. Available online: https://www.diabetes.co.uk/diabetes-and-obesity.html (accessed on 20 April 2021).
- Taylor, L.M.; Spence, J.C.; Raine, K.; Plotnikoff, R.C.; Vallance, J.K.; Sharma, A.M. Physical activity and health-related quality of life in individuals with prediabetes. Diabetes Res. Clin. Pract. 2010, 90, 15–21. [Google Scholar] [CrossRef]
- McNeilly, A.M.; Davison, G.W.; Murphy, M.H.; Nadeem, N.; Trinick, T.; Duly, E.; Novials, A.; McEneny, J. Effect of α-lipoic acid and exercise training on cardiovascular disease risk in obesity with impaired glucose tolerance. Lipids Health Dis. 2011, 10, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention National Diabetes Statistics Report. 2020. Available online: https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf (accessed on 20 April 2020).
- Buckley, C.; Kearney, P.; McHugh, S.; Harrington, J.; Bradley, C.; Perry, I. PS12 Diabetes and pre-diabetes prevalence rates in the survey of lifestyles, attitude and nutrition (Slan) in the republic of Ireland. J. Epidemiol. Community Health 2012, 66, A43. [Google Scholar] [CrossRef] [Green Version]
- Sinnott, M.; Kinsley, B.T.; Jackson, A.D.; Walsh, C.; O’Grady, T.; Nolan, J.J.; Gaffney, P.; Boran, G.; Kelleher, C.; Carr, B. Fasting plasma glucose as initial screening for diabetes and prediabetes in Irish adults: The diabetes mellitus and vascular health initiative (DMVhi). PLoS ONE 2015, 10, e0122704. [Google Scholar] [CrossRef]
- Diabetes UK Seven Million in UK Have ‘Prediabetes’. Available online: https://www.diabetes.org.uk/about_us/news_landing_page/7m-in-uk-have-prediabetes (accessed on 20 April 2021).
- Mainous, A.G.; Tanner, R.J.; Baker, R.; Zayas, C.E.; Harle, C.A. Prevalence of prediabetes in England from 2003 to 2011: Population-based, cross-sectional study. BMJ Open 2014, 4, e005002-2014. [Google Scholar] [CrossRef] [Green Version]
- Whicher, C.; O’Neill, S.; Holt, R.G. Diabetes in the UK: 2019. Diabet. Med. 2020, 37, 242–247. [Google Scholar] [CrossRef]
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the global burden of disease study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef] [Green Version]
- Department of Health/Ipsos MRBI Healthy Ireland Survey 2015 Summary of Findings. Available online: https://www.gov.ie/en/publication/fedbc9-healthy-ireland-survey-2015-summary-of-findings/?referrer=http://www.health.gov.ie/wp-content/uploads/2015/10/Healthy-Ireland-Survey-2015-Summary-of-Findings.pdf (accessed on 1 May 2020).
- HSE Healthy Eating and Active Living Programme: Key Facts. Available online: https://www.hse.ie/eng/about/who/healthwellbeing/our-priority-programmes/heal/key-facts/ (accessed on 2 July 2021).
- World Health Organisation Physical Activity. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 21 April 2021).
- Willinger, N.; Steele, J.; Atkinson, L.; Liguori, G.; Jimenez, A.; Mann, S.; Horton, E. Effectiveness of structured physical activity interventions through the evaluation of physical activity levels, adoption, retention, maintenance, and adherence rates: A systematic review and meta-analysis. J. Phys. Act. Health 2021, 18, 116–129. [Google Scholar] [CrossRef] [PubMed]
- Genuth, S.; Alberti, K.; Bennett, P.; Buse, J.; Defronzo, R.; Kahn, R.; Kitzmiller, J.; Knowler, W.; Lebovitz, H.; Lernmark, A. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 2003, 26, 3160. [Google Scholar] [PubMed] [Green Version]
- World Health Organization. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia: Report of a WHO/IDF Consultation; WHO Press: Geneva, Switzerland, 2006. [Google Scholar]
- Keys, A.; Fidanza, F.; Karvonen, M.J.; Kimura, N.; Taylor, H.L. Indices of relative weight and obesity. J. Chronic Dis. 1972, 25, 329–343. [Google Scholar] [CrossRef]
- Freedson, P.S.; Melanson, E.; Sirard, J. Calibration of the computer science and applications, inc. accelerometer. Med. Sci. Sports Exerc. 1998, 30, 777–781. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Locke, C.; Brashear, M.M.; Johnson, W.D.; Katzmarzyk, P.T. Accelerometer profiles of physical activity and inactivity in normal weight, overweight, and obese US men and women. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trost, S.G.; McIver, K.L.; Pate, R.R. Conducting accelerometer-based activity assessments in field-based research. Med. Sci. Sports Exerc. 2005, 37, S531. [Google Scholar] [CrossRef]
- Department of Health and Social Care UK Chief Medical Officers’ Physical Activity Guidelines. 2019. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/832868/uk-chief-medical-officers-physical-activity-guidelines.pdf (accessed on 21 April 2021).
- Rowe, D.A.; Welk, G.J.; Heil, D.P.; Mahar, M.T.; Kemble, C.D.; Calabró, M.A.; Camenisch, K. Stride rate recommendations for moderate-intensity walking. Med. Sci. Sports Exerc. 2011, 43, 312. [Google Scholar] [CrossRef]
- Yates, T.; Davies, M.; Gorely, T.; Bull, F.; Khunti, K. Effectiveness of a pragmatic education program designed to promote walking activity in individuals with impaired glucose tolerance: A randomized controlled trial. Diabetes Care 2009, 32, 1404–1410. [Google Scholar] [CrossRef] [Green Version]
- Mahmood, B.; Afshar, R.; Tang, T.S. Recruitment and retention of South Asian ethnic minority populations in behavioral interventions to improve type 2 diabetes outcomes. Curr. Diab. Rep. 2017, 17, 25. [Google Scholar] [CrossRef] [PubMed]
- Horowitz, C.R.; Brenner, B.L.; Lachapelle, S.; Amara, D.A.; Arniella, G. Effective recruitment of minority populations through community-led strategies. Am. J. Prev. Med. 2009, 37, S195–S200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vincent, D.; McEwen, M.M.; Hepworth, J.T.; Stump, C.S. Challenges and success of recruiting and retention for a culturally tailored diabetes prevention program for adults of Mexican descent. Diabetes Educ. 2013, 39, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Soderlund, P.D. Effectiveness of motivational interviewing for improving physical activity self-management for adults with type 2 diabetes: A review. Chronic Illn. 2018, 14, 54–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ekong, G.; Kavookjian, J. Motivational interviewing and outcomes in adults with type 2 diabetes: A systematic review. Patient Educ. Couns. 2016, 99, 944–952. [Google Scholar] [CrossRef]
- Samdal, G.B.; Eide, G.E.; Barth, T.; Williams, G.; Meland, E. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gopalan, A.; Lorincz, I.S.; Wirtalla, C.; Marcus, S.C.; Long, J.A. Awareness of prediabetes and engagement in diabetes risk-reducing behaviors. Am. J. Prev. Med. 2015, 49, 512–519. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).