Continuous Glucose Monitoring (CGM) and Metabolic Control in a Cohort of Patients with Type 1 Diabetes and Coeliac Disease
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gale, E.A.M. Type 1 diabetes in the young: The harvest of sorrow goes on. Diabetologia 2005, 48, 1435–1438. [Google Scholar] [CrossRef]
- Paschou, S.A.; Papadopoulou-Marketou, N.; Chrousos, G.P.; Kanaka-Gantenbein, C. On type 1 diabetes mellitus pathogenesis. Endocr. Connect. 2018, 7, R38–R46. [Google Scholar] [CrossRef] [PubMed]
- Bauer, W.; Gyenesei, A.; Krętowski, A. The Multifactorial Progression from the Islet Autoimmunity to Type 1 Diabetes in Children. Int. J. Mol. Sci. 2021, 22, 7493. [Google Scholar] [CrossRef]
- McAllister, B.P.; Williams, E.; Clarke, K. A Comprehensive Review of Celiac Disease/Gluten-Sensitive Enteropathies. Clin. Rev. Allergy Immunol. 2018, 57, 226–243. [Google Scholar] [CrossRef] [PubMed]
- Walker-Smith, J.A.; Grigor, W. COELIAC DISEASE IN A DIABETIC CHILD. Lancet 1969, 293, 1021. [Google Scholar] [CrossRef]
- Horton, R.; Wilming, L.; Rand, V.; Lovering, R.C.; Bruford, E.A.; Khodiyar, V.K.; Lush, M.J.; Povey, S.; Talbot, C.C.; Wright, M.W.; et al. Gene map of the extended human MHC. Nat. Rev. Genet. 2004, 5, 889–899. [Google Scholar] [CrossRef] [PubMed]
- Liu, E.; Rewers, M.; Eisenbarth, G.S. Genetic testing: Who should do the testing and what is the role of genetic testing in the setting of celiac disease? Gastroenterology 2005, 128, S33–S37. [Google Scholar] [CrossRef]
- Barera, G.; Bonfanti, R.; Viscardi, M.; Bazzigaluppi, E.; Calori, G.; Meschi, F.; Bianchi, C.; Chiumello, G. Occurrence of Celiac Disease After Onset of Type 1 Diabetes: A 6-Year Prospective Longitudinal Study. Pediatrics 2002, 109, 833–838. [Google Scholar] [CrossRef]
- Cerutti, F.; Bruno, G.; Chiarelli, F.; Lorini, R.; Meschi, F.; Sacchetti, C.; The Diabetes Study Group of Italian Society of Pediatric Endocrinology and Diabetology. Younger Age at Onset and Sex Predict Celiac Disease in Children and Adolescents with Type 1 Diabetes: An Italian multicenter study. Diabetes Care 2004, 27, 1294–1298. [Google Scholar] [CrossRef]
- Sud, S.; Marcon, M.; Assor, E.; Palmert, M.R.; Daneman, D.; Mahmud, F.H. Celiac Disease and Pediatric Type 1 Diabetes: Diagnostic and Treatment Dilemmas. Int. J. Pediatr. Endocrinol. 2010, 2010, 161285. [Google Scholar] [CrossRef]
- Diabetes Control and Complications Trial Research Group; Nathan, D.M.; Genuth, S.; Lachin, J.; Cleary, P.; Crofford, O.; Davis, M.; Rand, L.; Siebert, C. The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus. N. Engl. J. Med. 1993, 329, 977–986. [Google Scholar] [CrossRef] [PubMed]
- The Writing Team for the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Effect of Intensive Therapy on the Microvascular Complications of Type 1 Diabetes Mellitus. JAMA J. Am. Med. Assoc. 2002, 287, 2563–2569. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, M.A.; Eisenbarth, G.S.; Michels, A.W. Type 1 diabetes. Lancet 2014, 383, 69–82. [Google Scholar] [CrossRef]
- Lane, J.E.; Shivers, J.P.; Zisser, H. Continuous glucose monitors: Current status and future developments. Curr. Opin. Endocrinol. Diabetes Obes. 2013, 20, 106–111. [Google Scholar] [CrossRef]
- Markowitz, J.T.; Garvey, K.C.; Laffel, L.M. Developmental Changes in the Roles of Patients and Families in Type 1 Diabetes Management. Curr. Diabetes Rev. 2015, 11, 231–238. [Google Scholar] [CrossRef]
- Dovc, K.; Battelino, T. Evolution of Diabetes Technology. Endocrinol. Metab. Clin. North Am. 2019, 49, 1–18. [Google Scholar] [CrossRef]
- Battelino, T.; Danne, T.; Bergenstal, R.M.; Amiel, S.A.; Beck, R.; Biester, T.; Bosi, E.; Buckingham, B.A.; Cefalu, W.T.; Close, K.L.; et al. Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations from the International Consensus on Time in Range. Diabetes Care 2019, 42, 1593–1603. [Google Scholar] [CrossRef]
- Al-Toma, A.; Volta, U.; Auricchio, R.; Castillejo, G.; Sanders, D.S.; Cellier, C.; Mulder, C.J.; Lundin, K.E.A. European Society for the Study of Coeliac Disease (ESsCD) guideline for coeliac disease and other gluten-related disorders. United Eur. Gastroenterol. J. 2019, 7, 583–613. [Google Scholar] [CrossRef]
- Lionetti, E.; Antonucci, N.; Marinelli, M.; Bartolomei, B.; Franceschini, E.; Gatti, S.; Catassi, G.N.; Verma, A.K.; Monachesi, C.; Catassi, C. Nutritional Status, Dietary Intake, and Adherence to the Mediterranean Diet of Children with Celiac Disease on a Gluten-Free Diet: A Case-Control Prospective Study. Nutrients 2020, 12, 143. [Google Scholar] [CrossRef] [PubMed]
- Marsh, K.; Barclay, A.; Colagiuri, S.; Brand-Miller, J. Glycemic Index and Glycemic Load of Carbohydrates in the Diabetes Diet. Curr. Diabetes Rep. 2011, 11, 120–127. [Google Scholar] [CrossRef]
- Pham-Short, A.; Donaghue, K.C.; Ambler, G.; Garnett, S.; Craig, M.E. Quality of Life in Type 1 Diabetes and Celiac Disease: Role of the Gluten-Free Diet. J. Pediatr. 2016, 179, 131–138.e1. [Google Scholar] [CrossRef]
- Cacciari, E.; Milani, S.; Balsamo, A.; Spada, E.; Bona, G.; Cavallo, L.; Cerutti, F.; Gargantini, L.; Greggio, N.; Tonini, G.; et al. Italian cross-sectional growth charts for height, weight and BMI (2 to 20 yr). J. Endocrinol. Investig. 2006, 29, 581–593. [Google Scholar] [CrossRef] [PubMed]
- Cacciari, E.; Milani, S.; Balsamo, A.; Dammacco, F.; De Luca, F.; Chiarelli, F.; Pasquino, A.; Tonini, G.; Vanelli, M. Italian cross-sectional growth charts for height, weight and BMI (6–20 y). Eur. J. Clin. Nutr. 2002, 56, 171–180. [Google Scholar] [CrossRef]
- Monnier, L.; Colette, C.; Wojtusciszyn, A.; Dejager, S.; Renard, E.; Molinari, N.; Owens, D.R. Toward Defining the Threshold Between Low and High Glucose Variability in Diabetes. Diabetes Care 2016, 40, 832–838. [Google Scholar] [CrossRef]
- Rewers, M.; Eisenbarth, G.S. Celiac disease in T1DM—The need to look long term. Nat. Rev. Endocrinol. 2012, 8, 7–8. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jabri, B.; Sollid, L.M. Tissue-mediated control of immunopathology in coeliac disease. Nat. Rev. Immunol. 2009, 9, 858–870. [Google Scholar] [CrossRef]
- Berry, S.; McMahon, N.; Henderson, J. Guidelines for diagnosing coeliac disease: European Society Paediatric Gastroenterology, Hepatology and Nutrition. Arch. Dis. Child.-Educ. Pr. Ed. 2021, 106, 362–366. [Google Scholar] [CrossRef] [PubMed]
- Cohn, A.; Sofia, A.M.; Kupfer, S.S. Type 1 Diabetes and Celiac Disease: Clinical Overlap and New Insights into Disease Pathogenesis. Curr. Diabetes Rep. 2014, 14, 517. [Google Scholar] [CrossRef] [PubMed]
- Marchese, A.; Lovati, E.; Biagi, F.; Corazza, G.R. Coeliac disease and type 1 diabetes mellitus: Epidemiology, clinical implications and effects of gluten-free diet. Endocrine 2012, 43, 1–2. [Google Scholar] [CrossRef]
- Bascuñán, K.A.; Vespa, M.C.; Araya, M. Celiac disease: Understanding the gluten-free diet. Eur. J. Nutr. 2017, 56, 449–459. [Google Scholar] [CrossRef]
- Laffel, L.M.; Kanapka, L.G.; Beck, R.W.; Bergamo, K.; Clements, M.A.; Criego, A.; DeSalvo, D.J.; Goland, R.; Hood, K.; Liljenquist, D.; et al. Effect of Continuous Glucose Monitoring on Glycemic Control in Adolescents and Young Adults with Type 1 Diabetes: A Randomized Clinical Trial. JAMA 2020, 323, 2388–2396. [Google Scholar] [CrossRef]
- Yoo, J.H.; Kim, J.H. Advances in Continuous Glucose Monitoring and Integrated Devices for Management of Diabetes with Insulin-Based Therapy: Improvement in Glycemic Control. Diabetes Metab. J. 2023, 47, 27–41. [Google Scholar] [CrossRef] [PubMed]
- Ajjan, R.A.; Cummings, M.H.; Jennings, P.; Leelarathna, L.; Rayman, G.; Wilmot, E.G. Optimising use of rate-of-change trend arrows for insulin dosing decisions using the FreeStyle Libre flash glucose monitoring system. Diabetes Vasc. Dis. Res. 2019, 16, 3–12. [Google Scholar] [CrossRef]
- Majithia, A.R.; Wiltschko, A.B.; Zheng, H.; Walford, G.A.; Nathan, D.M. Rate of Change of Premeal Glucose Measured by Continuous Glucose Monitoring Predicts Postmeal Glycemic Excursions in Patients with Type 1 Diabetes: Implications for Therapy. J. Diabetes Sci. Technol. 2018, 12, 76–82. [Google Scholar] [CrossRef]
- Mahmud, F.H.; Clarke, A.B.M.; Joachim, K.C.; Assor, E.; McDonald, C.; Saibil, F.; Lochnan, H.A.; Punthakee, Z.; Parikh, A.; Advani, A.; et al. Screening and Treatment Outcomes in Adults and Children with Type 1 Diabetes and Asymptomatic Celiac Disease: The CD-DIET Study. Diabetes Care 2020, 43, 1553–1556. [Google Scholar] [CrossRef] [PubMed]
- Kaur, P.; Agarwala, A.; Makharia, G.; Bhatnagar, S.; Tandon, N. Effect of Gluten-FREE Diet on Metabolic Control and Anthropometric Parameters in Type 1 Diabetes with Subclinical Celiac Disease: A Randomized Controlled Trial. Endocr. Pract. 2020, 26, 660–667. [Google Scholar] [CrossRef] [PubMed]

| Variables | T1D and CD Patients | Only T1D Patients | p Value |
|---|---|---|---|
| Age (years) | 13.44 ± 4.65 | 13.45 ± 4.66 | 0.61 |
| Weight (Kg) | 52.03 ± 19.71 | 51.88 ± 18.10 | 0.925 |
| SDS weight | 0.38 ± 1.14 | 0.40 ± 0.72 | 0.95 |
| Height (cm) | 151.15 ± 22.98 | 151.53 ± 22.04 | 0.788 |
| SDS height | −0.12 ± 1.11 | −0.08 ± 0.82 | 0.849 |
| SDS BMI | 0.51 ± 1 | 0.54 ± 0.71 | 0.855 |
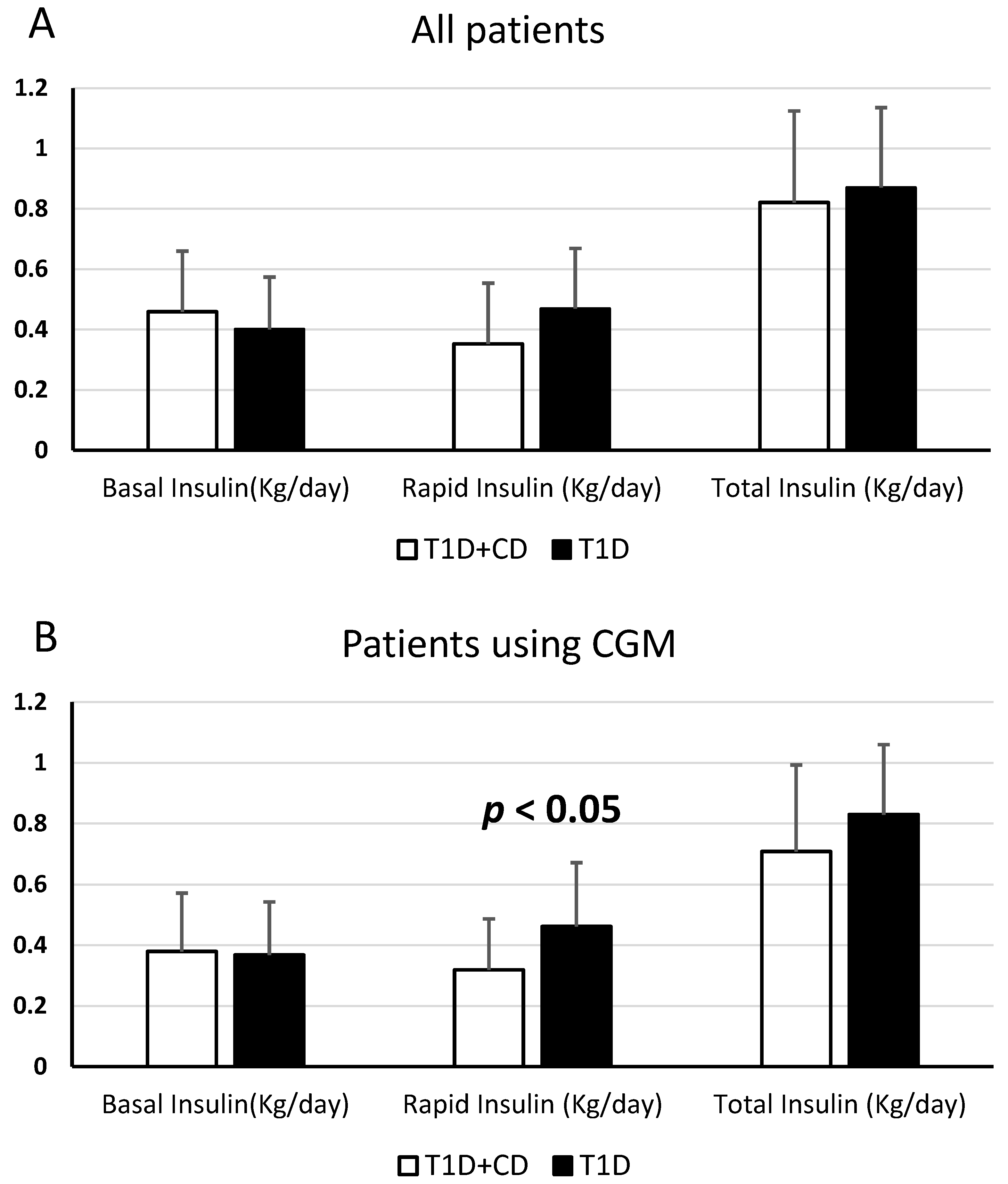
| Daily doses basal insulin (U/kg) | 0.46 ± 0.2 | 0.40 ± 0.17 | 0.083 |
| Daily doses rapid insulin (U/kg) | 0.35 ± 0.2 | 0.47 ± 0.2 | 0.014 (<0.05) |
| Daily total insulin (U/kg) | 0.82 ± 0.3 | 0.87 ± 0.26 | 0.394 |
| Insulin sensitivity factor | 89.29 ± 64.77 | 84.76 ± 87.34 | 0.831 |
| I:CHO ratio | 14.68 ± 11.23 | 12.21 ± 7.61 | 0.296 |
| Glucose levels mean (mg/dL) | 177.59 ± 46.83 | 164.81 ± 28.26 | 0.189 |
| SD (mg/dL) | 76.25 ± 29.83 | 66.62 ± 16.76 | 0.102 |
| CV (%) | 43.25 ± 9.22 | 40.76 ± 7.3 | 0.241 |
| HbA1c (%) | 7.44 ± 1.44 | 7.20 ± 1.12 | 0.443 |
| Variables | T1D and CD Patients | Only T1D Patients | p Value |
|---|---|---|---|
| Age (years) | 12.12 ± 5.64 | 12.12 ± 5.60 | 1 |
| Weight (Kg) | 45.77 ± 20.12 | 45.66 ± 19.42 | 0.96 |
| SDS weight | 0.4 ± 1.22 | 0.41 ± 0.79 | 0.99 |
| Height (cm | 144.44 ± 27.28 | 144.35 ± 25.95 | 0.97 |
| SDS height | 0.09 ± 1.29 | 0.07 ± 0.9 | 0.95 |
| SDS BMI | 0.49 ± 0.98 | 0.49 ± 0.73 | 0.98 |
| Daily doses basal insulin (U/Kg) | 0.38 ± 0.17 | 0.37 ± 0.17 | 0.76 |
| Daily doses rapid insulin (U/Kg) | 0.32 ± 0.20 | 0.46 ± 0.21 | 0.03 (<0.05) |
| Daily total insulin (U/Kg) | 0.71 ± 0.29 | 0.83 ± 0.23 | 0.14 |
| Insulin sensitivity factor | 89.12 ± 69.69 | 93.82 ± 94.66 | 0.86 |
| I:CHO ratio | 15 ± 11.78 | 12.41 ± 7.99 | 0.33 |
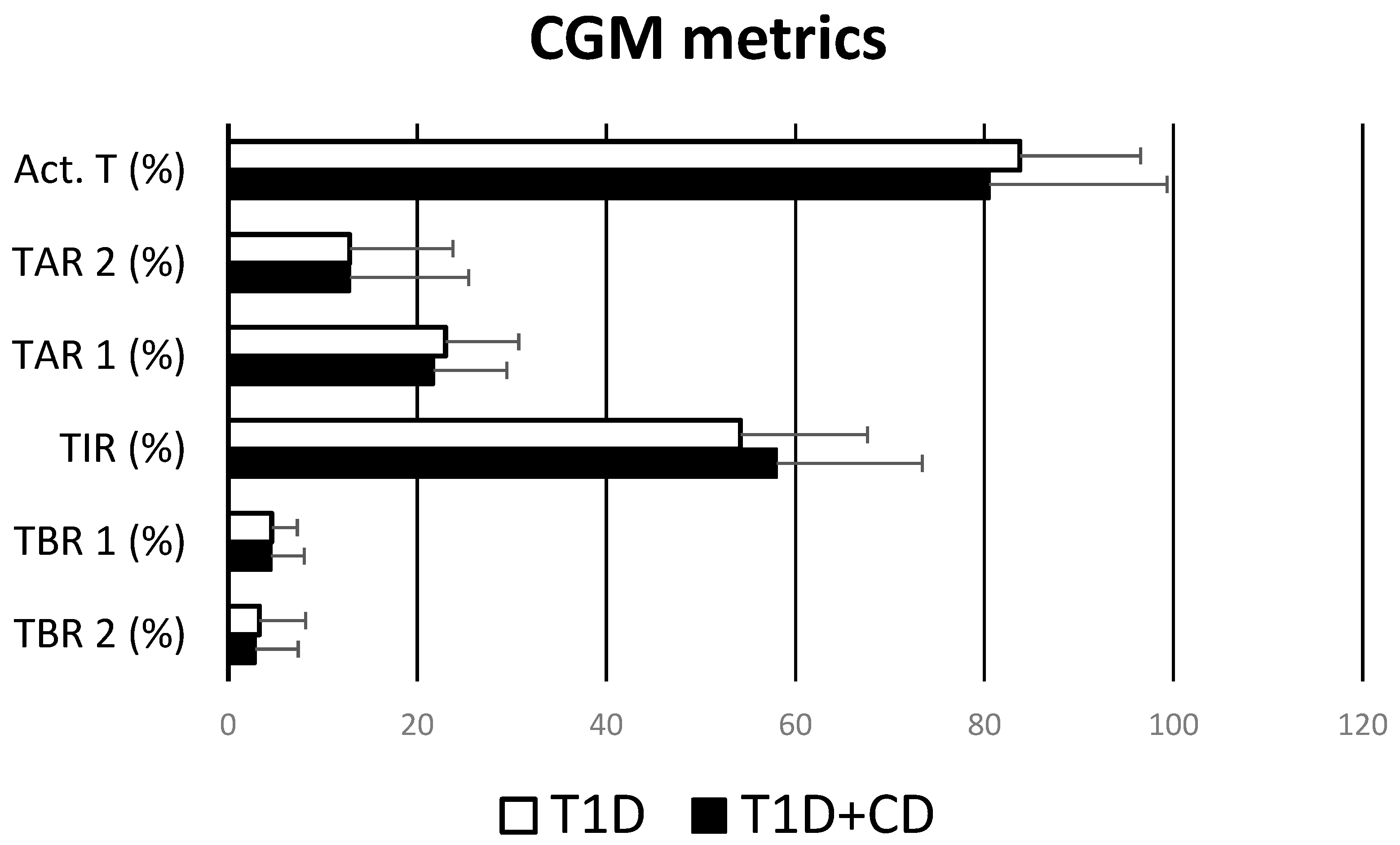
| %TBR2 | 2.85 ± 4.55 | 3.30 ± 4.88 | 0.77 |
| %TBR1 | 4.5 ± 3.53 | 4.6 ± 2.7 | 0.93 |
| %TIR | 58 ± 15.41 | 54.2 ± 13.42 | 0.39 |
| %TAR1 | 21.7 ± 7.77 | 23 ± 7.74 | 0.61 |
| %TAR2 | 12.85 ± 12.58 | 14.95 ± 10.91 | 0.61 |
| % Activity time | 80.5 ± 18.82 | 83.75 ± 12.75 | 0.53 |
| Glucose levels mean (mg/dL) | 164.3 ± 33.05 | 167.4 ± 29.45 | 0.78 |
| SD (mg/dL) | 68.01 ± 22.09 | 70.7 ± 16.2 | 0.69 |
| CV (%) | 41.34 ± 8.59 | 42.55 ± 6.83 | 0.66 |
| HbA1c (%) | 6.92 ± 1.24 | 7.45 ± 1.27 | 0.18 |
| Variables | T1D and CD Patients | Only T1D Patients | p Value |
|---|---|---|---|
| Daily doses basal insulin (U/Kg) | 0.55 ± 0.17 | 0.44 ± 0.17 | 0.05 |
| Daily doses rapid insulin (U/Kg) | 0.39 ± 0.23 | 0.48 ± 0.19 | 0.23 |
| Daily doses total insulin (U/Kg) | 0.95 ± 0.27 | 0.92 ± 0.3 | 0.66 |
| I:CHO ratio | 12 ± 5.66 | 10.5 ± 3.54 | 0.5 |
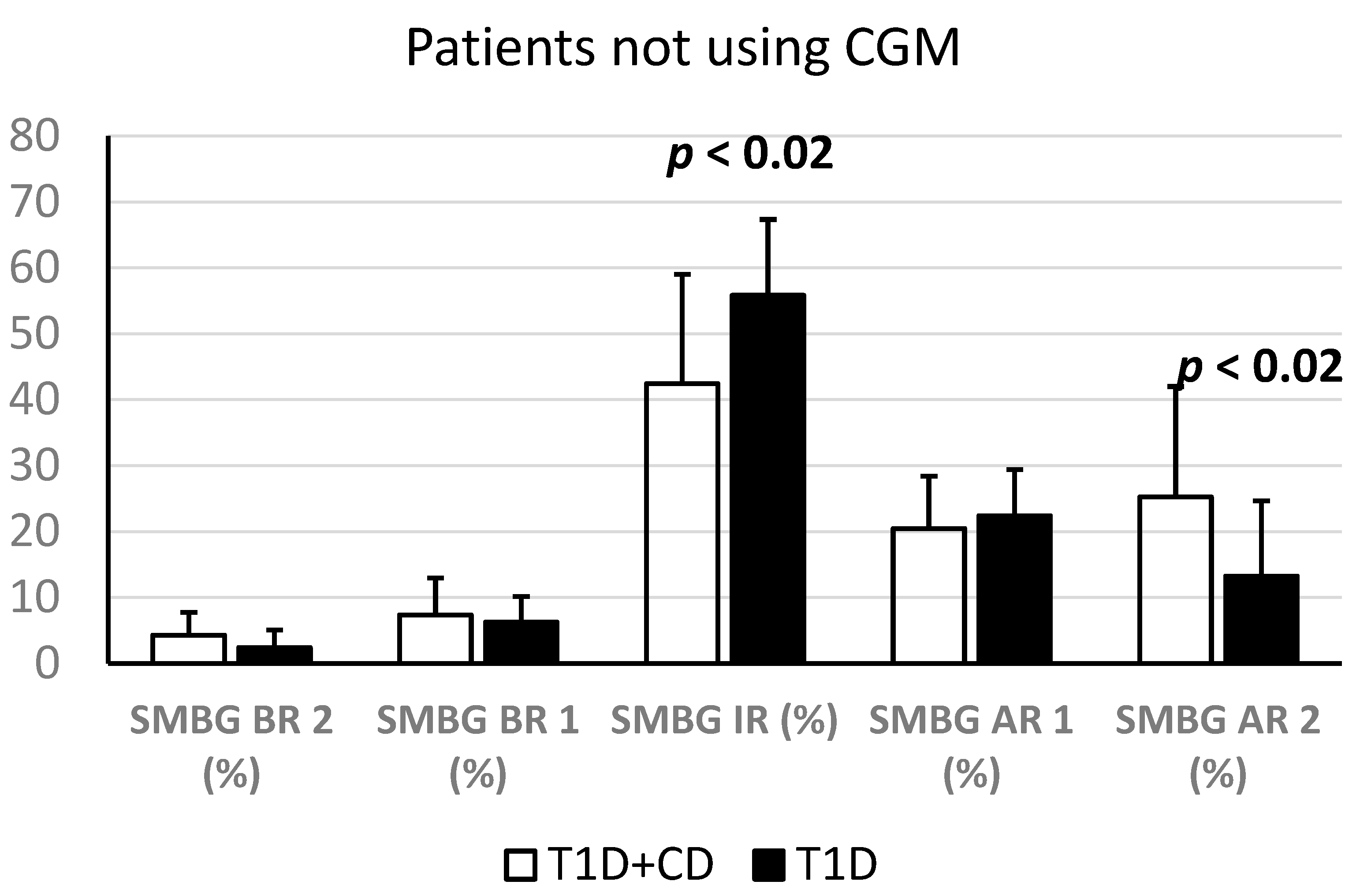
| % SMBG Below Range 2 | 4.29 ± 3.48 | 2.41 ± 2.67 | 0.13 |
| % SMBG Below Range 1 | 7.35 ± 5.61 | 6.24 ± 3.95 | 0.56 |
| % SMBG In Range | 42.41 ± 16.59 | 55.82 ± 11.5 | 0.02 (<0.05) |
| % SMBG Above Range1 | 20.47 ± 7.95 | 22.41 ± 7.01 | 0.53 |
| % SMBG Above Range 2 | 25.24 ± 16.78 | 13.24 ± 11.44 | 0.02 (<0.05) |
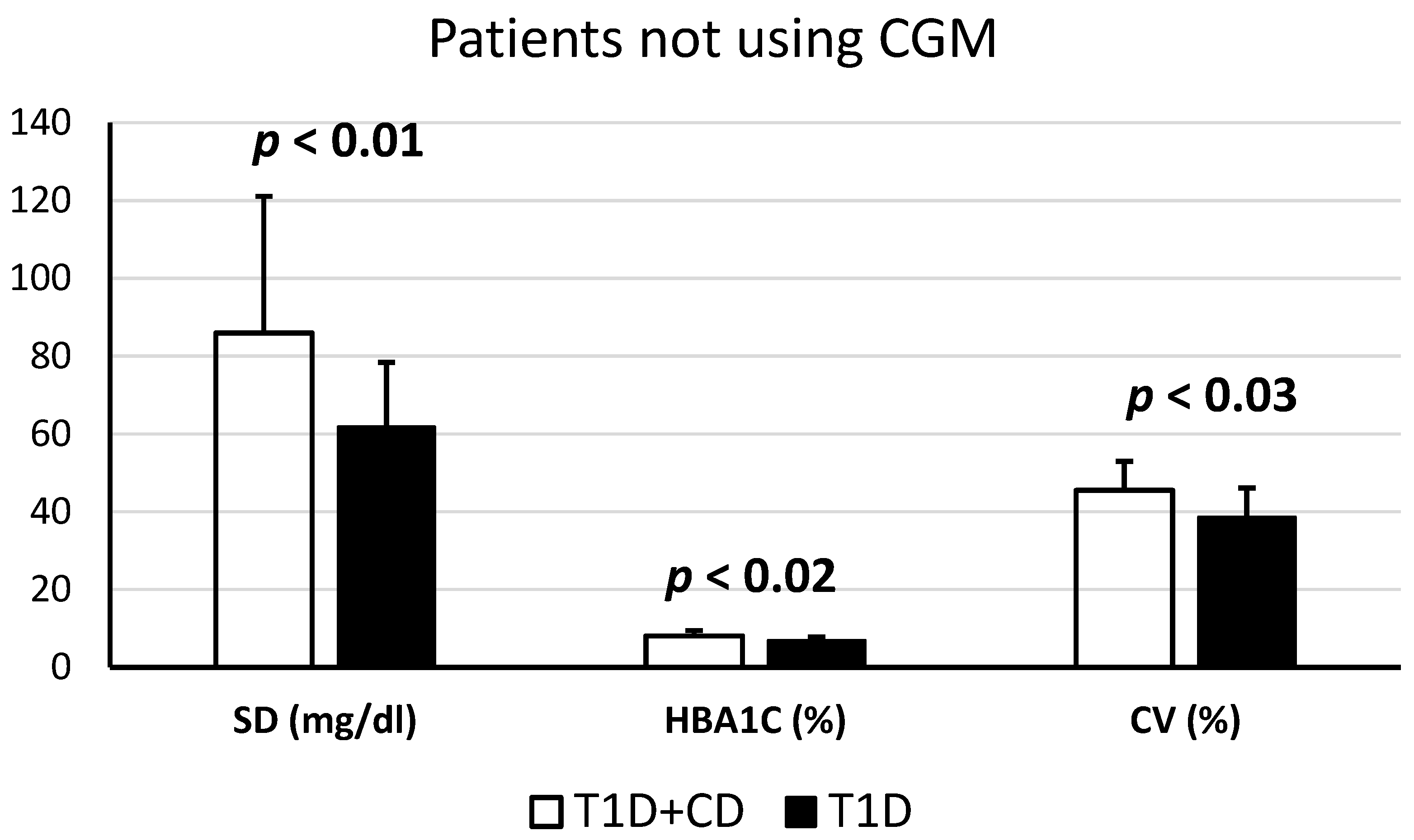
| Glucose levels mean (mg/dL) | 193.22 ± 56.19 | 161.76 ± 27.36 | 0.06 |
| SD (mg/dL) | 85.95 ± 35.18 | 61.82 ± 16.59 | 0.01 (<0.05) |
| CV (%) | 45.5 ± 9.67 | 38.65 ± 7.47 | 0.03 (<0.05) |
| HbA1c (%) | 8.05 ± 1.46 | 6.91 ± 0.86 | 0.02 (<0.05) |
| Age (years) | 14.98 ± 2.49 | 15.02 ± 2.61 | 0.58 |
| Weight (Kg) | 59.39 ± 16.93 | 59.21 ± 13.55 | 0.94 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amaro, F.; Saltarelli, M.A.; Primavera, M.; Cerruto, M.; Tumini, S. Continuous Glucose Monitoring (CGM) and Metabolic Control in a Cohort of Patients with Type 1 Diabetes and Coeliac Disease. Endocrines 2023, 4, 595-606. https://doi.org/10.3390/endocrines4030042
Amaro F, Saltarelli MA, Primavera M, Cerruto M, Tumini S. Continuous Glucose Monitoring (CGM) and Metabolic Control in a Cohort of Patients with Type 1 Diabetes and Coeliac Disease. Endocrines. 2023; 4(3):595-606. https://doi.org/10.3390/endocrines4030042
Chicago/Turabian StyleAmaro, Flavia, Maria Alessandra Saltarelli, Marina Primavera, Marina Cerruto, and Stefano Tumini. 2023. "Continuous Glucose Monitoring (CGM) and Metabolic Control in a Cohort of Patients with Type 1 Diabetes and Coeliac Disease" Endocrines 4, no. 3: 595-606. https://doi.org/10.3390/endocrines4030042
APA StyleAmaro, F., Saltarelli, M. A., Primavera, M., Cerruto, M., & Tumini, S. (2023). Continuous Glucose Monitoring (CGM) and Metabolic Control in a Cohort of Patients with Type 1 Diabetes and Coeliac Disease. Endocrines, 4(3), 595-606. https://doi.org/10.3390/endocrines4030042








