Current Updates in Bleomycin-Based Electrochemotherapy for Deep-Seated Soft-Tissue Tumors
Abstract
1. Introduction
2. Benefits of Electrochemotherapy
3. ECT for Deep-Seated Tumors
3.1. Previous Oncological Treatment
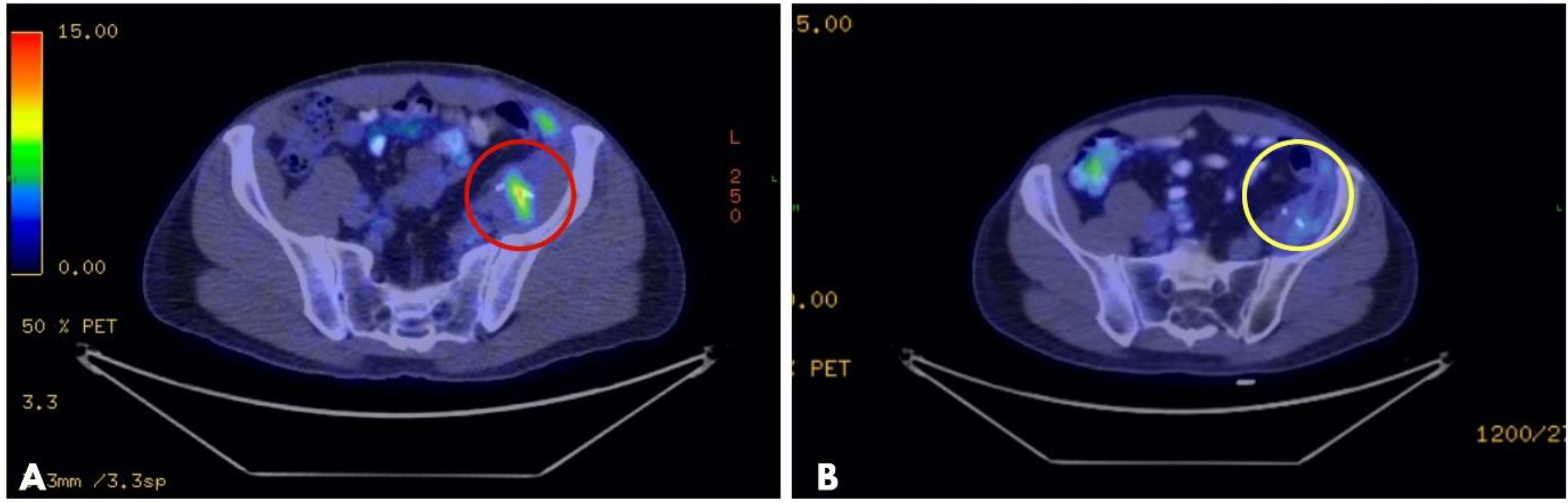
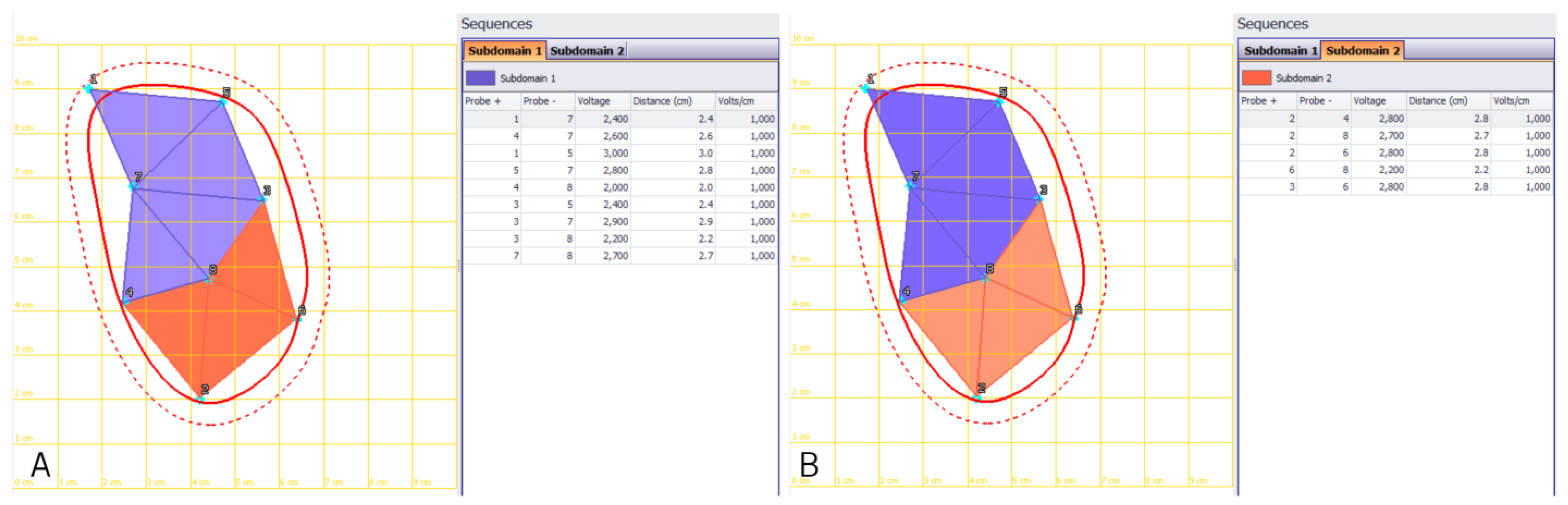
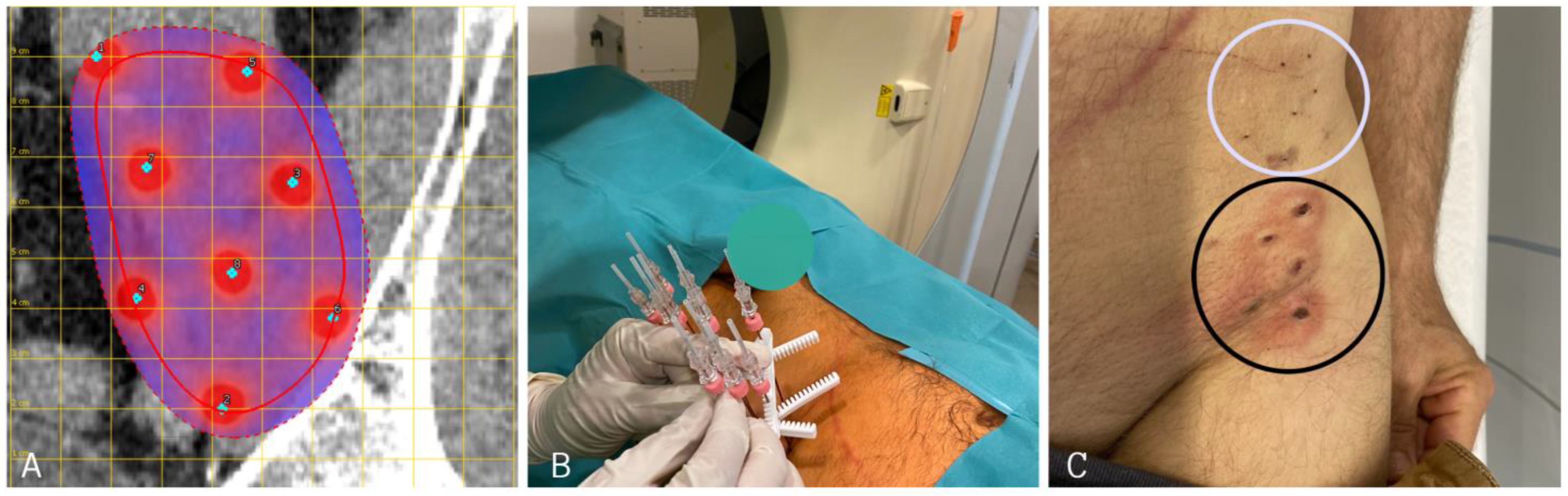
3.2. Electrode Placement Planning
3.3. Electrodes
3.4. Adverse Events
4. Summary and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
Abbreviations
References
- Ottlakan, A.; Lazar, G.; Hideghety, K.; Koszo, R.L.; Deak, B.; Nagy, A.; Besenyi, Z.; Bottyan, K.; Vass, G.Z.; Olah, J.; et al. Clinical considerations of bleomycin based electrochemotherapy with variable electrode geometry electrodes for inoperable, deep-seated soft tissue sarcomas. Bioelectrochemistry 2022, 148, 108220. [Google Scholar] [CrossRef]
- Mali, B.; Jarm, T.; Snoj, M.; Sersa, G.; Miklavcic, D. Antitumor effectiveness of electrochemotherapy: A systematic review and meta-analysis. Eur. J. Surg. Oncol. 2013, 39, 4–16. [Google Scholar] [CrossRef] [PubMed]
- Campana, L.G.; Edhemovic, I.; Soden, D.; Perrone, A.M.; Scarpa, M.; Campanacci, L.; Cemazar, M.; Valpione, S.; Miklavčič, D.; Mocellin, S.; et al. Electrochemotherapy-Emerging applications technical advances, new indications, combined approaches, and multi-institutional collaboration. Eur. J. Surg. Oncol. 2019, 45, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Probst, U.; Fuhrmann, I.; Beyer, L.; Wiggermann, P. Electrochemotherapy as a New Modality in Interventional Oncology: A Review. Technol. Cancer Res. Treat. 2018, 17, 1533033818785329. [Google Scholar] [CrossRef] [PubMed]
- Miraglia, E.; Curatolo, P.; Iacovino, C.; Careri, R.; Calvieri, S.; Giustini, S. Electrochemotherapy in Gorlin-Goltz syndrome. Ital. J. Dermatol. Venereol. 2021, 156 (Suppl. 1), 95–97. [Google Scholar] [CrossRef]
- Granata, V.; Fusco, R.; D’Alessio, V.; Simonetti, I.; Grassi, F.; Silvestro, L.; Palaia, R.; Belli, A.; Patrone, R.; Piccirillo, M.; et al. Percutanous Electrochemotherapy (ECT) in Primary and Secondary Liver Malignancies: A Systematic Review. Diagnostics 2023, 13, 209. [Google Scholar] [CrossRef]
- Spiliotis, A.E.; Holländer, S.; Rudzitis-Auth, J.; Wagenpfeil, G.; Eisele, R.; Nika, S.; Mallis Kyriakides, O.; Laschke, M.W.; Menger, M.D.; Glanemann, M.; et al. Evaluation of Electrochemotherapy with Bleomycin in the Treatment of Colorectal Hepatic Metastases in a Rat Model. Cancers 2023, 15, 1598. [Google Scholar] [CrossRef] [PubMed]
- Groselj, A.; Kos, B.; Cemazar, M.; Urbancic, J.; Kragelj, G.; Bosnjak, M.; Veberic, B.; Strojan, P.; Miklavcic, D.; Sersa, G. Coupling treatment planning with navigation system: A new technological approach in treatment of head and neck tumors by electrochemotherapy. Biomed. Eng. Online 2015, 14 (Suppl. 3), S2. [Google Scholar] [CrossRef]
- Fuhrmann, I.; Probst, U.; Wiggermann, P.; Beyer, L. Navigation Systems for Treatment Planning and Execution of Percutaneous Irreversible Electroporation. Technol. Cancer Res. Treat. 2018, 17, 1533033818791792. [Google Scholar] [CrossRef] [PubMed]
- Sersa, G.; Jarm, T.; Kotnik, T.; Coer, A.; Podkrajsek, M.; Sentjurc, M.; Miklavcic, D.; Kadivec, M.; Kranjc, S.; Secerov, A.; et al. Vascular disrupting action of electroporation and electrochemotherapy with bleomycin in murine sarcoma. Br. J. Cancer 2008, 98, 388–398. [Google Scholar] [CrossRef]
- Jarm, T.; Cemazar, M.; Miklavcic, D.; Sersa, G. Antivascular effects of electrochemotherapy: Implications in treatment of bleeding metastases. Expert Rev. Anticancer Ther. 2010, 10, 729–746. [Google Scholar] [CrossRef]
- Mole, R.H. Whole body irradiation; radiobiology or medicine? Br. J. Radiol. 1953, 26, 234–241. [Google Scholar] [CrossRef]
- Justesen, T.F.; Orhan, A.; Raskov, H.; Nolsoe, C.; Gögenur, I. Electroporation and Immunotherapy-Unleashing the Abscopal Effect. Cancers 2022, 14, 2876. [Google Scholar] [CrossRef]
- Djokic, M.; Dezman, R.; Cemazar, M.; Stabuc, M.; Petric, M.; Smid, L.M.; Jansa, R.; Plesnik, B.; Bosnjak, M.; Tratar, U.L.; et al. Percutaneous image guided electrochemotherapy of hepatocellular carcinoma: Technological advancement. Radiol. Oncol. 2020, 54, 347–352. [Google Scholar] [CrossRef]
- Gong, X.; Chen, Z.; Hu, J.J.; Liu, C. Advances of Electroporation-Related Therapies and the Synergy with Immunotherapy in Cancer Treatment. Vaccines 2022, 10, 1942. [Google Scholar] [CrossRef] [PubMed]
- Spallek, H.; Bischoff, P.; Zhou, W.; de Terlizzi, F.; Jakob, F.; Kovàcs, A. Percutaneous electrochemotherapy in primary and secondary liver malignancies-local tumor control and impact on overall survival. Radiol. Oncol. 2022, 56, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Zmuc, J.; Gasljevic, G.; Sersa, G.; Edhemovic, I.; Boc, N.; Seliskar, A.; Plavec, T.; Brloznik, M.; Milevoj, N.; Brecelj, E.; et al. Large Liver Blood Vessels and Bile Ducts Are Not Damaged by Electrochemotherapy with Bleomycin in Pigs. Sci. Rep. 2019, 9, 3649. [Google Scholar] [CrossRef] [PubMed]
- Kos, B.; Voigt, P.; Miklavcic, D.; Moche, M. Careful treatment planning enables safe ablation of liver tumors adjacent to major blood vessels by percutaneous irreversible electroporation (IRE). Radiol. Oncol. 2015, 49, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Izzo, F.; Granata, V.; Fusco, R.; D’Alessio, V.; Petrillo, A.; Lastoria, S.; Piccirillo, M.; Albino, V.; Belli, A.; Tafuto, S.; et al. Clinical Phase I/II Study: Local Disease Control and Survival in Locally Advanced Pancreatic Cancer Treated with Electrochemotherapy. J. Clin. Med. 2021, 10, 1305. [Google Scholar] [CrossRef]
- Djokic, M.; Cemazar, M.; Popovic, P.; Kos, B.; Dezman, R.; Bosnjak, M.; Zakelj, M.N.; Miklavcic, D.; Potrc, S.; Stabuc, B.; et al. Electrochemotherapy as treatment option for hepatocellular carcinoma, a prospective pilot study. Eur. J. Surg. Oncol. 2018, 44, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Bertino, G.; Groselj, A.; Campana, L.G.; Kunte, C.; Schepler, H.; Gehl, J.; Muir, T.; Clover, J.A.P.; Quaglino, P.; Kis, E.; et al. Electrochemotherapy for the treatment of cutaneous squamous cell carcinoma: The INSPECT experience (2008-2020). Front Oncol. 2022, 12, 951662. [Google Scholar] [CrossRef] [PubMed]
- Edhemovic, I.; Brecelj, E.; Gasljevic, G.; Marolt Music, M.; Gorjup, V.; Mali, B.; Jarm, T.; Kos, B.; Pavliha, D.; Grcar Kuzmanov, B.; et al. Intraoperative electrochemotherapy of colorectal liver metastases. J. Surg. Oncol. 2014, 110, 320–327. [Google Scholar] [CrossRef]
- Mir, L.M.; Glass, L.F.; Sersa, G.; Teissié, J.; Domenge, C.; Miklavcic, D.; Jaroszeski, M.J.; Orlowski, S.; Reintgen, D.S.; Rudolf, Z.; et al. Effective treatment of cutaneous and subcutaneous malignant tumours by electrochemotherapy. Br. J. Cancer 1998, 77, 2336–2342. [Google Scholar] [CrossRef] [PubMed]
- Mir, L.M.; Orlowski, S.; Belehradek Paoletti, C., Jr. Electrochemotherapy potentiation of antitumour effect of bleomycin by local electric pulses. Eur. J. Cancer 1991, 27, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Rudolf, Z.; Stabuc, B.; Cemazar, M.; Miklavcic, D.; Vodovnik, L.; Sersa, G. Electrochemotherapy with bleomycin. The first clinical experience in malignant melanoma patients. Radiol. Oncol. 1995, 29, 229–235. [Google Scholar]
- Orlowski, S.; Belehradek JJr Paoletti, C.; Mir, L.M. Transient electropermeabilization of cells in culture. Increase of the cytotoxicity of anticancer drugs. Biochem. Pharmacol. 1988, 37, 4727–4733. [Google Scholar] [CrossRef]
- Mir, L.M.; Gehl, J.; Sersa, G.; Collins, C.G.; Garbay, J.R.; Billard, V. Standard operating procedures of the electrochemotherapy: Instructions for the use of bleomycin or cisplatin administered either systemically or locally and electric pulses delivered by the Cliniporator (TM) by means of invasive or non-invasive electrodes. EJC Suppl. 2006, 4, 14–25. [Google Scholar] [CrossRef]
- Gehl, J.; Sersa, G.; Matthiessen, L.W.; Muir, T.; Soden, D.; Occhini, A.; Quaglino, P.; Curatolo, P.; Campana, L.G.; Kunte, C.; et al. Updated standard operating procedures for electrochemotherapy of cutaneous tumours and skin metastases. Acta Oncol. 2018, 57, 874–882. [Google Scholar] [CrossRef]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef]
- Matthiessen, L.W.; Keshtgar, M.; Curatolo, P.; Kunte, C.; Grischke, E.M.; Odili, J.; Muir, T.; Mowatt, D.; Clover, J.P.; Liew, S.H.; et al. Electrochemotherapy for Breast Cancer-Results From the INSPECT Database. Clin. Breast Cancer 2018, 18, e909–e917. [Google Scholar] [CrossRef]
- Clover, A.J.P.; de Terlizzi, F.; Bertino, G.; Curatolo, P.; Odili, J.; Campana, L.G.; Kunte, C.; Muir, T.; Brizio, M.; Sersa, G.; et al. Electrochemotherapy in the treatment of cutaneous malignancy: Outcomes and subgroup analysis from the cumulative results from the pan-European International Network for Sharing Practice in Electrochemotherapy database for 2482 lesions in 987 patients (2008–2019). Eur. J. Cancer 2020, 138, 30–40. [Google Scholar] [CrossRef]
- Perera-Bel, E.; Aycock, K.N.; Salameh, Z.S.; Gomez-Barea, M.; Davalos, R.V.; Ivorra, A.; Ballester, M.A.G. PIRET-A Platform for Treatment Planning in Electroporation-Based Therapies. IEEE Trans. Biomed. Eng. 2022, 1–9, Epub ahead of print. [Google Scholar] [CrossRef]
- Zupanic, A.; Kos, B.; Miklavcic, D. Treatment planning of electroporation-based medical interventions: Electrochemotherapy, gene electrotransfer and irreversible electroporation. Phys. Med. Biol. 2012, 57, 5425–5440. [Google Scholar] [CrossRef] [PubMed]
- Marčan, M.; Pavliha, D.; Kos, B.; Forjanič, T.; Miklavčič, D. Web-based tool for visualization of electric field distribution in deep-seated body structures and planning of electroporation-based treatments. Biomed. Eng. Online 2015, 14 (Suppl. 3), S4. [Google Scholar] [CrossRef] [PubMed]
- Marčan, M.; Kos, B.; Miklavčič, D. Effect of blood vessel segmentation on the outcome of electroporation-based treatments of liver tumors. PLoS ONE 2015, 10, e0125591. [Google Scholar] [CrossRef]
- Edhemovic, I.; Brecelj, E.; Cemazar, M.; Boc, N.; Trotovsek, B.; Djokic, M.; Dezman, R.; Ivanecz, A.; Potrc, S.; Bosnjak, M.; et al. Intraoperative electrochemotherapy of colorectal liver metastases: A prospective phase II study. Eur. J. Surg. Oncol. 2020, 46, 1628–1633. [Google Scholar] [CrossRef] [PubMed]
- Trotovsek, B.; Hadzialjevic, B.; Cemazar, M.; Sersa, G.; Djokic, M. Laparoscopic electrochemotherapy for the treatment of hepatocellular carcinoma: Technological advancement. Front. Oncol. 2022, 12, 996269. [Google Scholar] [CrossRef]
- Schipilliti, F.M.; Onorato, M.; Arrivi, G.; Panebianco, M.; Lerinò, D.; Milano, A.; Roberto, M.; Capalbo, C.; Mazzuca, F. Electrochemotherapy for solid tumors: Literature review and presentation of a novel endoscopic approach. Radiol. Oncol. 2022, 56, 285–291. [Google Scholar] [CrossRef]
- Mali, B.; Gorjup, V.; Edhemovic, I.; Brecelj, E.; Cemazar, M.; Sersa, G.; Strazisar, B.; Miklavcic, D.; Jarm, T. Electrochemotherapy of colorectal liver metastases-an observational study of its effects on the electrocardiogram. Biomed. Eng. Online 2015, 14 (Suppl. 3), S5. [Google Scholar] [CrossRef]
- Deodhar, A.; Dickfeld, T.; Single, G.W.; Hamilton, W.C., Jr.; Thornton, R.H.; Sofocleous, C.T.; Maybody, M.; Gónen, M.; Rubinsky, B.; Solomon, S.B. Irreversible electroporation near the heart: Ventricular arrhythmias can be prevented with ECG synchronization. AJR Am. J. Roentgenol. 2011, 196, W330–W335. [Google Scholar] [CrossRef]
- Djokic, M.; Cemazar, M.; Bosnjak, M.; Dezman, R.; Badovinac, D.; Miklavcic, D.; Kos, B.; Stabuc, M.; Stabuc, B.; Jansa, R.; et al. A Prospective Phase II Study Evaluating Intraoperative Electrochemotherapy of Hepatocellular Carcinoma. Cancers 2020, 12, 3778. [Google Scholar] [CrossRef] [PubMed]
- Ranieri, G.; Laface, C.; Fazio, V.; De Ceglia, D.; Macina, F.; Gisone, V.; Porcelli, M.; Vinciarelli, G.; Carella, C.; Molinari, P.; et al. Local treatment with deep percutaneous electrochemotherapy of different tumor lesions: Pain relief and objective response results from an observational study. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 7764–7775. [Google Scholar] [CrossRef] [PubMed]
- Simioni, A.; Valpione, S.; Granziera, E.; Rossi, C.R.; Cavallin, F.; Spina, R.; Sieni, E.; Aliberti, C.; Stramare, R.; Campana, L.G. Ablation of soft tissue tumours by long needle variable electrode-geometry electrochemotherapy: Final report from a single-arm, single-centre phase-2 study. Sci. Rep. 2020, 10, 2291. [Google Scholar] [CrossRef] [PubMed]
- Campanacci, L.; Bianchi, G.; Cevolani, L.; Errani, C.; Ciani, G.; Facchini, G.; Spinnato, P.; Tognù, A.; Massari, L.; Cornelis, F.H.; et al. Operating procedures for electrochemotherapy in bone metastases: Results from a multicenter prospective study on 102 patients. Eur. J. Surg. Oncol. 2021, 47, 2609–2617. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ottlakan, A.; Lazar, G.; Olah, J.; Nagy, A.; Vass, G.; Vas, M.; Pereira, R.; Kis, E. Current Updates in Bleomycin-Based Electrochemotherapy for Deep-Seated Soft-Tissue Tumors. Electrochem 2023, 4, 282-290. https://doi.org/10.3390/electrochem4020019
Ottlakan A, Lazar G, Olah J, Nagy A, Vass G, Vas M, Pereira R, Kis E. Current Updates in Bleomycin-Based Electrochemotherapy for Deep-Seated Soft-Tissue Tumors. Electrochem. 2023; 4(2):282-290. https://doi.org/10.3390/electrochem4020019
Chicago/Turabian StyleOttlakan, Aurel, Gyorgy Lazar, Judit Olah, Andras Nagy, Gabor Vass, Marton Vas, Raissa Pereira, and Erika Kis. 2023. "Current Updates in Bleomycin-Based Electrochemotherapy for Deep-Seated Soft-Tissue Tumors" Electrochem 4, no. 2: 282-290. https://doi.org/10.3390/electrochem4020019
APA StyleOttlakan, A., Lazar, G., Olah, J., Nagy, A., Vass, G., Vas, M., Pereira, R., & Kis, E. (2023). Current Updates in Bleomycin-Based Electrochemotherapy for Deep-Seated Soft-Tissue Tumors. Electrochem, 4(2), 282-290. https://doi.org/10.3390/electrochem4020019





