1. Introduction
Removable partial dentures equipped with a metal framework, even today, remain one of the most widespread rehabilitations, especially in those conditions in which it is not possible to resort to fixed implant prostheses for clinical choice or economic reasons [
1,
2,
3]. This type of prosthesis is mechanically resistant, long-lasting, and capable of excellently restoring the masticatory function for years [
4,
5]. Unfortunately, sometimes, the patient who uses this type of prosthesis is forced to undergo tooth extractions due to untreatable periodontitis or caries. These clinical conditions mean that the clinician has to modify the prosthesis by adding the missing tooth or teeth or even building a new prosthesis due to the impossibility of obtaining a perfectly reusable and resistant prosthesis, especially due to the forces involved during chewing [
6,
7].
In most cases, prostheses, equipped with a metal framework, are modified by adding the missing teeth with the aid of the resin used alone, which is anchored to the residual metallic and resinous parts of the prosthesis; this type of modification of the prosthesis is often understood as temporary, while waiting for new prosthetic rehabilitation to occur within about six months [
8,
9,
10,
11,
12]. In some particular clinical conditions, this modification may not be very mechanically resistant to masticatory loads, and the clinician may have to hesitate in the detachment of the added part [
4,
13,
14,
15], with the total failure of the adopted repair procedure, forcing them to create a new cast piece of framework to be laser welded to the rest of the pre-existing structure, with the help of the laboratory dental technician [
16,
17]. In this way, by providing the added resin and tooth with a metal support, the structural modification certainly appears more robust and long-lasting.
The downside is represented by the very long waiting times, because it is necessary to first model the metal piece to be added in wax and then melt it in metal [
18]; alternatively, the new piece of structure to be added could be obtained via milling or laser melting [
19,
20,
21,
22]. The second step is represented by the laser welding of the new piece to the pre-existing framework, and finally the missing tooth or teeth are added using resin [
23]. Unfortunately, the whole procedure described here is often uneconomical and pushes the prosthetist to prefer the creation of a new prosthesis with rather high final costs for the patient.
This research has focused its attention on a new and experimental intermediate solution for the realization of modifications on partial dentures equipped with a metal framework, which require the joining of one or two contiguous teeth, through the use of preformed and pre-cast metal pins, and welding using the “cold welding method”.
The experimental procedure proposed in this research presents numerous advantages compared to traditional methods both from economic and temporal points of view, representing a rapid and at the same time effective solution for the patient.
This type of welding is performed using devices where the learning curve of the procedure that they are used in is quite short; moreover, the level of mechanical robustness of the welded joint is considerable and far superior to that required by the clinical application being tested. Furthermore, due to its particular characteristics, welding can be carried out without a risk of overheating the pre-existing structure of the prosthesis and without the appearance of burnished discolorations on the metal, which would have an unsightly effect on the final result. Lastly, these cold welding devices clearly have lower costs than the analogous laser welders normally used for similar purposes [
24].
This experimental protocol can be easily implemented with a substantial reduction in both the operating times and in the final cost for the patient who may not even be in the economic position to face the reconstruction of a new denture in the short term. This solution, tested by us, guarantees the functional predictability of the modifications made to the prostheses with an adequate social cost.
2. Materials and Methods
Sixty-eight patients with upper or lower partial removable prostheses equipped with a metal framework who lost one or two contiguous teeth, due to caries or periodontal disease, were selected.
The sample size was determined according to the chosen margin of error, which was equal to 10%, which was appropriate considering that this is a preliminary study which foresees further development in the future. The confidence level was 90% with a standard deviation of 50%.
In choosing the sample, the rules of RTC (randomized controlled trial) research were followed, which allowed us to better evaluate the efficacy of what was tested compared to traditional dental technology protocols.
We initially selected 223 patients who had suitable prostheses fabricated within four years of performing this study; a further selection criterion was adhered to by only including prostheses with similar metal frameworks in the search, to eliminate variables due to the shape of the supporting structure as much as possible. The final number of subjects treated was 68; they were divided into two groups and their assignment was random in order to increase the probability that other variables, not considered in the study design, were uniformly distributed.
Group 1: 32 prostheses were repaired with the addition of one or two contiguous teeth, using resin only (pink Sintodent Weltrade).
Group 2: 36 prostheses were repaired with the addition of one or two contiguous teeth through the use of resin reinforced with a preformed metal pin welded to the main structure using the cold welding technique (see
Table 1).
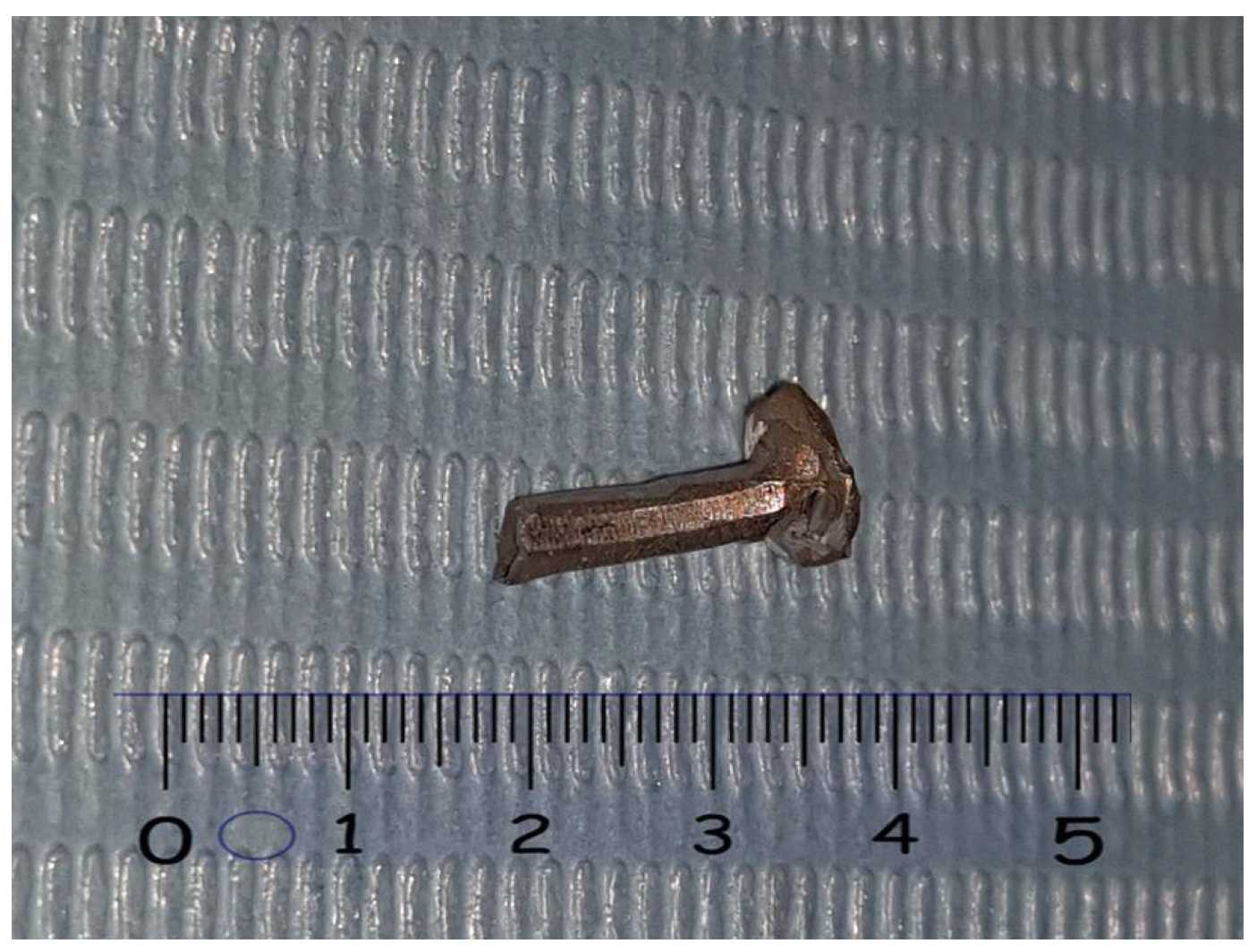
In this regard, several pins were previously made in wax and subsequently cast using a die-casting machine (Tecnogaz ASM 20); the cobalt–chromium–molybdenum alloy (Mesa Magnum H60, composition: Co 63%—Cr 29%—Mo 6.5%—C, Si, Fe, Mn 1.5%), with a cylindrical shape, variable length between 10 and 15 mm, diameter of 2 mm, and, at one end, a 4 mm diameter nail head, was designed to facilitate the welding procedures [
25,
26,
27] (
Figure 1).
All of the modifications on the prostheses were conducted three weeks after the dental extraction in order to allow the tissues to heal adequately. Patients were also invited to continue wearing the prostheses from the day following the dental extraction itself in order to avoid unwanted movement of the residual natural teeth present in the arch [
28].
At the time of making the modifications to the prostheses, an alginate impression of the opposing arch and occlusal wax were taken for all patients; for patients in group 1 (repairs performed with resin only), an alginate impression was taken of the position of the prosthesis under examination. For group 2 patients, in order to facilitate the insertion of the preformed metal pin, a 2 mm diameter hole was drilled on the pre-existing framework exactly at the point where teeth were to be added. At this point, an alginate position impression of the thus modified prosthesis was also taken for patients in group 2.
Plaster casting of the position impressions of all of the patients made it possible to obtain models containing the prostheses, making the foreseen modifications possible.
For all cases in group 1, we proceeded with the wax modeling of the piece to be added, with the creation of silicone masks and with the traditional modification of the prosthesis by anchoring the tooth or teeth added with the aid of pink resin only.
For the cases in group 2, before proceeding as described above, the preformed metal pin was inserted into the hole previously made and the two metal parts were joined by means of cold welding (Andeli TIG-250PL, Andeli Group Co., Ltd., Zhejiang, China) (
Figure 2) [
29].
The rest of the repair procedure was exactly the same as that carried out for the group 1 cases, with the substantial difference being that a metal framework (the pin) was incorporated in the added resin, which was integral to the main metal structure of the prosthesis (
Figure 3).
Cold welders are characterized by a tungsten electrode which, placed close to the structures to be welded (without physical contact), sets off an electric arc capable of melting metals in a small area; this makes it possible to reach the temperatures necessary for joining the metals via a limited area, avoiding the overheating of the entire metal piece [
30,
31]. This feature is essential in order to weld metal frameworks of prostheses where the prosthetic teeth are still mounted using pink resin. These resinous components do not tolerate high temperatures, which in this case remained limited to an area of a few millimeters.
More specifically, the setting of the cold welder used in the study allowed for single current pulses between 70 and 90 amperes protracted for milliseconds, with a direct current electrode negative polarity which allowed for the connection of the negative pole to the tungsten and the positive pole to the piece to be welded. This type of setting concentrates about two thirds of its welding heat on the framework and the remaining one third on the tungsten; a higher heat input to the weld results in deeper penetration.
Given the small size of the pin to be welded, the number of electric arcs required is limited to 4 or 5 and they can also be temporally distant from each other in order to further reduce the already low risk of overheating. This is possible because each single electric arc is effective in creating the necessary delta T in a single area and giving rise to the junction of the two metals without the need for preheating the piece or continuous welding. The entire welding process takes place in an argon-protected atmosphere which prevents any tendency for oxidation, which normally occurs following a rise in temperature at the junction point [
32]. In our study, the flow of protective gas was kept within a range between 4.5 and 5.5 L per minute so that the jet was totally invested in the whole area involved in the welding process and it was therefore continuously protected [
33].
In this regard, cold welders, as well as all TIG welders, among the possible adjustments, allow the argon gas outflow to be brought forward with respect to the striking of the electric arc (pre-flow time) so as to ensure that the inert atmosphere is well formed before the moment of welding; regarding the same principle, it can be set for how long the gas flow must continue for after the arc has finished (post-flow time), so that even when the welded pieces are being cooled, oxidation phenomena do not occur. In our study, the pre-flow and post-flow times were set at 2 s and 3 s, respectively.
A 1.6 mm diameter electrode of the WL20 BLUE type with 2% lanthanum (LaO2: 1.8–2.2%) was inserted in the welding machine handpiece which offers excellent ignition performance and durability, keeps the shape clean and the tip unaltered, and finally does not contain thorium and therefore is not harmful to health and the environment. For cold welding, it is also necessary to sharpen the tip of the tungsten electrode longitudinally, giving it the shape of a pointed cone. The sharp tip of the electrode provides a constant and concentrated arc in the workpiece. The sharpening angle and the length have an effect on the width of the arc and on the depth of penetration; in our study, the electrode was sharpened at 25°, creating a rather long and pointed terminal cone which, compared to a shorter and more squat one, ensures better arc penetration especially with low currents such as those used on prostheses.
All of the modified prostheses were delivered to the patients following a clinical check of the inter-arch relationships in order to exclude any pre-contact; a six-month follow-up was performed with bimonthly checks in order to verify the presence of any anomalies, such as cracks or detachments of the resin and/or the added teeth.
The obtained results were statistically processed in order to verify the hypothesis and ensure that the data corresponded to what was expected, i.e., that a dental procedure based on the use of preformed pins and welding via the cold welding technique is more resistant than a procedure performed solely with resin. The chi-square test was applied using JMP statistical software (version 2023, JMP Statistical Discovery LLC., Cary, NC, USA) by setting alpha = 0.1, which corresponded with an error percentage of 10%.
3. Results
Considering the 68 modifications made on as many prostheses, the results obtained were as follows:
The total incidence of failures seen via detachment and/or fracture of the parts added to the patients’ prostheses can be summarized into 14 cases, equal to 20.58%. Within this value, the difference between group 1 (13 failures) and group 2 (1 failure) is significant. In percentage terms, out of 32 group 1 prostheses, 40.62% were failures, and out of 36 group 2 prostheses, 2.77% were failures.
More specifically, within group 1, out of 20 prostheses where only one tooth was added, nine failures were recorded, equal to 45%; on the other hand, out of 12 prostheses, two contiguous teeth were added and four failures were recorded, equal to 33.33%. Out of 10 prostheses of the 32 modified with resin only, the opposing tooth was a natural tooth, and in these clinical conditions, there were eight detachments, equal to 80%. Out of 22 prostheses of the 32 modified with resin only, the antagonist tooth was a tooth forming part of a removable prosthesis, and in these clinical conditions, there were five detachments, equal to 27.77%.
Still in group 1, 14 prostheses out of 32 were related to the upper arch, and there were seven detachments, equal to 50%, while 18 prostheses were related to the upper arch and there were six detachments, equal to 33.33%.
Considering the total of 13 failures in group 1 (32 modified prostheses), the percentage ratio between the junction of a single tooth and the junction of two teeth was equal to 69.23% compared to 33.76%; the percentage ratio between clinical conditions in which the opposing tooth was a natural tooth and conditions in which it was part of a removable partial prosthesis was equal to 61.53% compared to 38.46%; and the percentage ratio between the detachments found in the upper prostheses compared to the lower ones was equal to 53.84% compared to 46.15%.
More specifically, within group 2, out of 24 prostheses whereby only one tooth was added, only one failure was recorded, equal to 4.16%; on the other hand, out of 12 prostheses, two teeth were added, and no failures were recorded (0%). Out of 12 prostheses of the 36 modified with the welded pin and with resin, the antagonist tooth was a natural tooth, and in these clinical conditions, only a detachment equal to 8.33% was highlighted. In 24 prostheses out of the 36 modified with the soldered pin plus resin, the opposing tooth was a tooth belonging to a removable prosthesis, and in these clinical conditions, no detachments were recorded (0%).
Still in group 2, 16 out of 36 prostheses were related to the upper arch, and only one detachment was noted, equal to 6.25%, while 20 prostheses were related to the upper arch and no failure was detected (0%).
Considering the only failure in group 2 (36 modified prostheses), the percentage ratio between the junction of a single tooth and the junction of two teeth is equal to 100% compared to 0%; the percentage ratio between clinical conditions in which the opposing tooth was a natural tooth and conditions in which it was part of a removable partial prosthesis was equal to 100% versus 0%; and the percentage ratio between the detachments found in the upper prostheses compared to the lower ones was equal to 100% compared to 0% (see
Table 1,
Table 2 and
Table 3).
4. Discussion
The modification of partial removable prostheses equipped with a metal framework, necessary to meet changing clinical conditions, has always represented a critical moment for both the patient and the prosthetist. The loss of teeth in wearers of these prostheses is a frequent event often resolved via the creation of new prostheses, which, based on a new clinical design, represent the most valid solution.
However, we must not forget that some patients choose this type of prosthesis for economic reasons, and having the same type of prosthesis implementation repeated several times in their life could represent a serious economical problem. Similarly, modifying the prosthesis through complex procedures such as the creation of new laser-welded castings could be uneconomical.
The innovative repair method investigated in this research was based on the use of pins, like the one visible in
Figure 1, pre-built in a dental laboratory, which can be joined via the cold welding method, as seen in
Figure 2, to the main metal structure of the prosthesis.
Furthermore, our study showed significantly better clinical results compared to the classic method of repair without pins, highlighting only one case of breakage in 6 months out of 36 modified planned follow-ups of the prostheses.
In any case, a single failure is not significant and is also limited to a small part of the resin used to block the added tooth. These modifications carried out in this way have shown structural robustness even at the level of the most risky conditions, which are those where the tooth or the antagonist teeth of the newly added ones are natural teeth; as evidence of this, the data relating to the failures of the group 1 prostheses show that in 80%, the opposing tooth was actually a natural tooth. In fact, in this case, the masticatory forces involved were really high and were concentrated on a restricted area of the modified prosthesis which, just at that point, could be structurally weaker.
It seems useful to note that in group 1 (use of resin only), adding two contiguous teeth allowed for repairs that were more resistant to masticatory loads than the addition of a single tooth; in fact, as many as 45% of the prostheses where only one tooth was added showed breakage under masticatory loads. On the other hand, only 33.33% of the prostheses where two contiguous teeth were added broke. These data were also confirmed by the percentage distribution within the 13 failures of group 1: 69.23% of the failures were noted in the case of the addition of a single tooth and 33.76% were noted in the case of the addition of two contiguous teeth. It is most likely that the presence of a larger edentulous space increases the possibility of connection between the newly added resin, to block the two dental elements, and the pre-existing resinous and metallic structures.
There was no statistically significant difference between the failures noted in the upper jaw compared to those in the lower jaw.
Ultimately, the conditions most at risk of failure are those in which only one tooth is added and the antagonist is a natural tooth. Precisely, in these clinical cases, the addition of a preformed post welded via the cold welding technique can make the difference, significantly increasing the predictability of the results without excessively increasing the final costs for the patient.
All of the results of the experimental research seemed to validate the effectiveness of the proposed method which, compared to the more usual and traditional odontotechnical procedures for modifying removable prostheses (based only on the use of pink resin), managed to give more predictable results.
Furthermore, the materials and equipment involved are low-cost compared to customized castings made for a single clinical case that are then laser welded.
Finally, the aesthetic result of the modified prosthesis was excellent, despite important changes having been made, such as those on the metal structure. An example of the aesthetics achieved is shown in
Figure 3.
5. Conclusions
This study has highlighted the possibility of modifying a suitable partial removable prosthesis equipped with a metal framework in a patient who has lost one or two contiguous teeth using a fairly simple technique which allows one to make, in a standardized way, structural modifications capable of withstanding masticatory loads without the risk of the newly added teeth coming off, as often happens when they are supported by resin alone. Clearly, if there are more than two dental elements to be added or the prosthesis shows age and incongruity with the patient’s clinical situation, the most suitable solution is to replace it with a new one.
In any case, rather than modifying pre-existing prostheses, it would be better to redo a new denture every time clinical changes occur in the patient’s mouth, such as the loss of one or more teeth. However, in everyday reality, we must not forget the need to find solutions for patients with limited financial resources that are both valid and affordable for them.