Abstract
In full-arch rehabilitation with implant-supported fixed prostheses, using monolithic zirconia seems to have several advantages regarding function and esthetics. However, the current scientific evidence is still limited. Thus, the aim of this investigation was to systematically review the literature on monolithic zirconia restorations for full-arch rehabilitation, particularly pursuing the survival rate and mechanical and biological complications. This study’s protocol was registered in PROSPERO (CRD42022301799). The primary literature search was performed in PubMed/MedLine and Web of Science, and a manual search was performed (checking cross-references). The focused question was, “In an adult population with one or both edentulous arches (P), the oral rehabilitation with implant-supported fixed-monolithic zirconia (full arch) (I), compared with oral rehabilitation using fixed-metal-ceramic prosthesis on implants (C), did show superior clinical results (O) in a minimum follow-up of 1 year (T)?” Inclusion and exclusion criteria were defined. Joana Briggs Institute tools were used to evaluate the quality of the studies. Meta-analysis was performed for the variable survival rate (%), applying the specific continuous moderator (follow-up). Data heterogeneity (I2) was assessed. From the initial search, 327 references were obtained. After eliminating duplicates and applying the inclusion/exclusion criteria by reading the titles, abstracts, and full text, seven articles were included. All included articles were observational longitudinal retrospective studies, with a number of prostheses between 7 and 2039. The mean age was 60 years, and the mean follow-up was 49.7 months. They had mandibular, maxillary, or bimaxillary rehabilitations, always with screw-retained retention, with an average survival rate of 97.23%. The number of implants ranged between four and eight. The quality of the articles was over 70%, and the heterogeneity was considered low (I2 = 28.64%). Within a mean follow-up of around four years, full-arch implant-supported monolithic zirconia rehabilitations had a high survival rate and minimal complications.
1. Introduction
Full-arch implant-supported fixed prostheses are one of the best treatment options for rehabilitating edentulous patients [1,2,3]. Full-arch rehabilitations differ in four parameters: retention mode (screw-retained or cemented), design (single piece or two pieces), prosthodontic material (acrylic/composite metal–resin, metal–ceramic, monolithic zirconia, or zirconia–ceramic), and material to mimic the gingiva (acrylic/composite resin, ceramic, or just gingival shade pigmentation) [2]. Combining a metal infrastructure with veneer ceramics is still considered the gold standard due to its cost, high modulus of elasticity, easy ceramic application and casting, and pleasing esthetic associated with a high success rate [4]. Over the years, the design of full-arch metal–ceramic prostheses has demonstrated success in rehabilitating completely edentulous patients [5]. Therefore, the proper selection of the prosthetic material is critical for the longevity of fixed dental prostheses (FDPs) supported by dental implants. The type of material used can affect how stress is distributed during the chewing cycle and ultimately determines the load-bearing capacity of the FDPs [6,7,8,9,10]. Zirconia has joined this field because of esthetic demands, combining esthetics with excellent mechanical properties [3].
Zirconium (Zr) is a metal with chemical and physical properties similar to titanium (Ti). Zirconium oxide (ZrO2) or zirconia has been used in Dentistry for over 15 years with many indications, focusing on replacing metal and improving esthetics [11]. Zirconia is a polymorphic material with three forms: monoclinic, tetragonal, and cubic [12,13]. It has optimal properties for medical-dental use [11,12,14]. Moreover, zirconia has an excellent survival rate, minimal technical complications, and good biocompatibility and esthetics [2,3,4]. On the other hand, zirconia has an opaque white color, which it has been suggested to stain to improve the esthetics of the structure. However, in recent years, more translucent zirconia has appeared [15].
Within this context, prosthetic restorations in monolithic zirconia retained by dental implants have shown a survival rate of 99.3% in 5 years, compared to metal–ceramics, which have a survival rate of 98.2 to 98.8% in 5 years [5,16,17]. Monolithic zirconia restorations appear to cause wear on the opposing dentition similar to metal–ceramics and seem to have a better fit than zirconia prostheses [18,19]. According to Sailer et al. [20], fixed zirconia and fixed metal–ceramic prostheses exhibited excellent 10-year survival rates, with no statistical differences and similar overall technical results. Therefore, metal–ceramic prosthetic rehabilitations had technical complications of 4.5% in 5 years and 14% in 10 years [21]. In contrast, clinical complications for zirconia were found in the prosthetic infrastructure, the fracture of the ceramics (chipping) (ranging from 15% to 54%) [11], and the fracture of the distal extension (cantilever) [22].
Monolithic zirconia prostheses are emerging as a promising option in the implant-based rehabilitation of edentulous patients, and their clinical performance is not fully documented. This systematic study aimed to analyze the current scientific evidence on fixed full-arch rehabilitation with monolithic zirconia verifying the survival rate and complications.
2. Materials and Methods
This systematic study followed the PRISMA guidelines to analyze the scientific evidence published on the topic under analysis. This investigation was registered in the PROSPERO (CRD42022301799) and followed the Participants, Intervention, Control, Outcomes, and Time (PICOT) protocol. The focused question was, “In an adult population with one or both edentulous arches (P), the oral rehabilitation with implant-supported fixed-monolithic zirconia (full arch) (I), compared with oral rehabilitation using fixed-metal-ceramic prosthesis on implants (C), did show superior clinical results (O) in a minimum follow-up of 1 year (T)?”
The PICOT research question was defined as follows: Population, adult patients with one or both edentulous arches; Intervention, creation of implant-supported complete fixed prostheses in monolithic zirconia; Comparison, implant-supported complete metal-ceramic fixed prostheses; Outcomes, mechanical and biological complications, and survival rates; Time, minimum follow-up of 1 year.
2.1. Source of Information and Research Strategy
The electronic search was performed in January 2022 in two databases: PubMed/MedLine and Web of Science. The MeSH terms and the terms in “natural language” associated with the PICOT parameters are described in Table 1. Furthermore, the search strategy for both databases, after selecting these terms, was defined (Table 1). A manual search was also carried out in the systematic reviews about this theme to find cross-references. Due to the specificity of the theme, it was decided not to use search filters.

Table 1.
MESH terms and search strategy.
2.2. Eligibility Criteria
The following inclusion/exclusion criteria were defined for selecting the articles. The inclusion criteria were (i) randomized clinical trials, (ii) longitudinal (prospective and retrospective) studies, (iii) adult patients, (iv) patients with one or both edentulous arches, (v) patients with implant-supported full-fixed prostheses made of monolithic zirconia without porcelain veneering or with coverage limited to the gingival region/non-functional area, (vi) patients with a minimum follow-up of 1 year, (vii) articles with information on survival/success rates and/or biological complications and/or mechanical complications. The exclusion criteria were (i) studies that enrolled patients ASA III or above, (ii) studies that involved patients with bruxism, (iii) in vitro or preclinical studies, (iv) review articles, (v) total implant-fixed prostheses supported in monolithic zirconia with porcelain veneering in the coronal region.
2.3. Screening and Data Extraction
Two independent reviewers (LV and AC) were responsible for the searches and screening of the articles. After eliminating duplicates, the articles passed through 3 stages: (i) reading of the title, (ii) reading of the abstract, and (iii) reading the full text. In disagreement, a third reviewer (LA) broke the tie. The analysis of agreement between reviewers was performed using the agreement of Cohen’s kappa coefficient. The same independent reviewers selected data from each included article and recorded them in an Excel® sheet (version 15.17, Microsoft, Redmond, Washington, DC, USA). Any potential disagreement and/or discrepancy was resolved by consensus and in the presence of a third reviewer (LA).
The following variables were defined in this investigation: author’s last name; year of publication; sample size (n); average age; follow-up period; number of dropouts; rehabilitation position (maxillary/mandibular); prosthetic framework material (trademark); type of retention; number of implants; types of complications; and success/survival rates.
2.4. Quality Assessment/Risk of Bias
The tool provided by the JBI organization (Joanna Briggs Institute, University of Adelaide, North Adelaide, Australia) was used to assess the quality of the included studies. The purpose of this tool is to evaluate the methodological quality of research and determine the extent to which the possibility of risk of bias has been addressed in its design, execution, and analysis. It includes 11 questions with the following responses: yes, no, undefined, and not applicable. A value below 50% indicates a low quality of the article; between 50 and 69% corresponds to an average quality, and ≥70% reflects a high quality [23].
2.5. Statistical Analysis
Meta-analysis was performed for the variable survival rate (%), applying as a specific continuous moderator to the follow-up of the patients. The heterogeneity of the data (I2) was evaluated. If between 0% and 40%, there was no heterogeneity. Between 40% and 60%, there was moderate heterogeneity. Between 60% and 80%, there was substantial heterogeneity. Between 80% and 100%, there was high heterogeneity. A funnel plot was drawn to verify heterogeneity and whether studies were within the confidence interval (95%) [24].
3. Results
Initially, a total of 327 articles were found. After removing duplicates and applying the eligibility criteria, seven articles were included in this study (Figure 1 and Table 2) (k = 0.908 for the title and abstract selection, and k = 1 for the full-text selection). All articles included were retrospective longitudinal observational studies. They had a minimum number of prostheses of 7 [25] to a maximum of 2039 [16]. The patients’ age average was 60 years. One article [26] referred only to mandibular prostheses, and five referred to [5,16,22,25,27] double-arch prostheses. All articles referred to prostheses with screw retention on a number of implants ranging from 4 to 8. The follow-up average was 49.7 months (4 years). Details of each study are in Table 3.
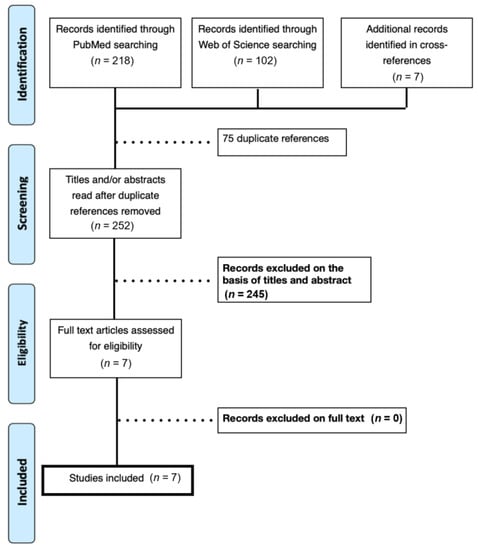
Figure 1.
PRISMA flowchart—screening and selection of articles.

Table 2.
Included articles.

Table 3.
Data extracted from the studies included.
The quality assessment showed (Table 4) that the articles included in this systematic review had values greater than 70%, considered high quality. The forest plot (Figure 2) and funnel plot (Figure 3) showed low heterogeneity among the studies. The largest variation in the confidence interval was observed in Bidra et al.’s study [16], which may be due to the number of prostheses initially evaluated. However, the heterogeneity found was I2 = 28.64%, which represented a low level of heterogeneity. The average survival rate in the studies was 97.23%.

Table 4.
JBI quality assessment.
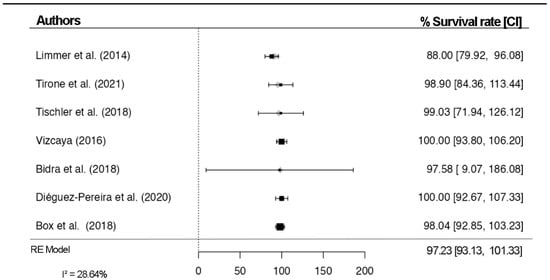
Figure 2.
Forest plot for survival rates (%) [11,14,16,22,25,26,27].
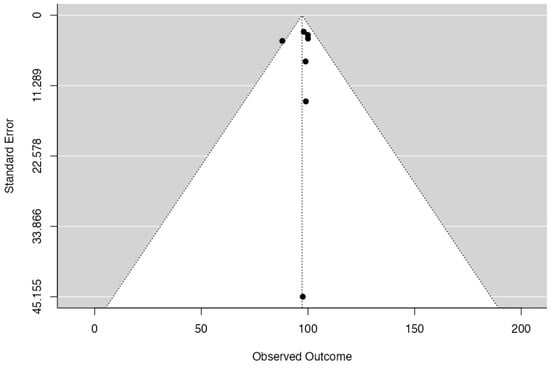
Figure 3.
Funnel plot for the studies included.
4. Discussion
The success of rehabilitation is defined by its function, good esthetics, stability, no infection presence, and patient satisfaction [28]. Zirconium oxide (ZrO2) has been used in Dentistry for over 15 years with many indications, focusing on replacing metal and improving esthetics [11], with an excellent survival rate, minimal technical complications, and good biocompatibility and esthetics [2,3,4]. It has optimal properties, such as superior tenacity, resistance to fatigue and bending, excellent wear properties, biocompatibility, osseointegration, and less bacterial colonization, which makes it a suitable biomaterial to be used as a dental implant [11,12,14]. It is most often stabilized by yttria (Y2O3), being called polycrystalline tetragonal zirconia (Y-TZP), which has a high stiffness (ranging from 5 to 10 MPa) and flexural strength (ranging from 900 to 1400 MPa) [11,13]. These physical properties are the highest available dental ceramics [11]. On the other hand, due to zirconia having an opaque white color, most dental zirconia systems suggest staining the structure to improve the esthetics of crowns with full anatomical contours. However, more translucent zirconia has appeared, improving the esthetics, but with a lower strength to fracture [15].
Its success directly depends on the survival of each associated element (implants and restorations). Then, the survival of prostheses is directly associated with their functional presence within the mouth [28]. Moreover, the survival rate can be divided into follow-up intervals, which can be considered short term (1 to 5 years) or long term (5 to 20 years) [29]. For the articles included in this review, the mean follow-up was 49.7 months (around 4 years), corresponding to a short-term follow-up. In addition, even though it was considered a short period, it reached a high survival rate (97.23%), which was compared to the survival of metal–ceramic fixed prostheses (98.2–98.8%), which are considered the gold standard [5,17]. The zirconia found in the various studies was mainly from Zirconzahn, and only one study used Amanngirrbach zirconia, but without specifying the product. Each brand has several zirconia versions with different physical and esthetic characteristics, from the most to the least resistant zirconia or multilayer zirconia. Each layer has differences in color and translucency, respectively, as well as resistance.
Rehabilitation can suffer several complications. The biological complication involves dental implants with inflammatory processes that can reach peri-implantitis, and, if not treated, may lead to implant loss and failure of the prosthesis. A typical biological complication in all included studies was implant loss. However, no inference can be made regarding the fact that the prostheses were made of monolithic zirconia. The implant loss in strategic areas can compromise the viability of the entire rehabilitation, implying the creation of a new one, but this does not mean that the monolithic zirconia has failed. The mechanical/structural complications associated with the prosthesis material’s integrity may range from simple chipping to catastrophic fracture of the rehabilitation [30,31,32].
According to Sailer [33], in an article carried out within the scope of the 3rd Consensus of the European Association of Osseointegration, screw-retained structures are recommended in extensive implant-supported reconstructions. All articles included in this systematic review used the screw-retained system. Therefore, some professionals do not consider cemented retention in extensive rehabilitation because of the irreversibility characteristic. Otherwise, it offers a better occlusal fit. The use of screw retention allows rapid reversibility in case of removal to control or solve complications. On the other hand, the screw channel compromises the stiffness of the material, leading to an increased fracture probability [34]. Cemented prostheses have some advantages compared to screw-retained implant prostheses when the issue of reversibility is not considered. These prostheses have a better passive fit and are easy to adjust in the presence of tensions, thus allowing better passivity [34,35]. In some cases, it is difficult to justify using screws to retain prostheses, except for limited abutment height where there is a diminished surface area for cementation, or in abutments with a subgingival margin where removal of abutments could be complicated when trying to check extravasated cementing material. The cemented system can facilitate the insertion of prostheses in areas with insufficient mouth opening [34,35].
4.1. Mechanical/Structural Complications
A common complication in all articles included was the loss of covering material in the screw access hole. This is a non-specific complication for zirconia restorations. It cannot be defined as a “compromising” complication because it did not alter the functional/esthetic quality or the mechanical characteristics of the zirconia, being easily repaired with the addition of new material.
Fracture of the prosthetic structure was found in two articles. In the study carried out by Tirone et al. [22], four fractures were found, which were classified into two types: one was (i) Type I, a fracture that occurred in the middle, not involving the two most posterior holes for accessing the screws, and three were (ii) Type II, with a fracture on the distal extension (cantilever). Limmer et al.’s [26] study reported a single fracture of the structure in a distal extension. These fractures are related to the length of the distal extension, which received excessive tension in the zirconia, causing consequent fracture [36]. According to Durkan’s study [31], a maximum of 9 mm of distal extension is recommended with 30° angled implants, reducing stresses on the bone and zirconia. In Limmer et al.’s article [26], the distal fracture extension was 17 mm, whereas, in Tirone et al. [22], the average length of the distal extensions fractured was 10.04 mm. Alshahrani et al. [32], in an in vitro study, demonstrated that the length of the distal extension and the occlusal-cervical size are important factors in determining the load values for fracture of these extensions [32].
Higher load values were required for the fracture (7672 N), even with distal extensions with a shorter length [32] and larger occlusal-cervical size (10 mm), while distal extensions with a greater length (17 mm) and smaller occlusal-cervical size [36] fractured once a load of 1543 N was reached [37]. Even though those load values are much higher than the “normal” masticatory loads found in the oral cavity, the normal average peaks at 762 N (in the male molar region, it has an average of 624 N with a peak of 847 N; in females, an average of 537 N with a peak of 613 N) and reaches 806 N in patients with bruxism [37,38,39]. Otherwise, the literature reported a value of mastication force ranging from 244 to 859 N [38], which is below the maximum flexural strength values of short posterior extensions with increased occlusal-cervical size.
Limmer et al. [26] also reported other structural complications (decementation of a pillar, fracture of two pillars, and loss of another pillar). Similar complications were reported in the article by Bidra et al. [16], with six decemented prostheses (titanium abutment) and three titanium abutment fractures. Factors that can cause decementation of the abutment are the zirconia surface’s bonding properties, inadequate cement space, insufficient light diffusion through the zirconia to polymerize dual cement, and lack of strength caused by the abutment design [40]. This last factor was analyzed in the study by Calderon et al. [41], where tapered titanium abutments showed a higher rate of debonding and micromovements than other titanium abutment designs.
Four of the seven articles reported prostheses in monolithic zirconia with pink veneering ceramics [11,16,22,27]. Only one study [27] reported an episode of chipping of the pink ceramic in the palatal zone of the maxillary prosthesis (unknown etiology). Caramês et al. [42] noted that chipping of the veneering ceramic is a frequent complication, which in some cases is not possible to resolve with simple polishing. The main cause of chippings is not clear, but there are three factors suggested: (i) binding interface; (ii) compatibility between the infrastructure material and the covering material; and (iii) resistance of the covering ceramic. Furthermore, the porcelain veneering technique potentially affects ceramic chipping due to its processing methods, which include repeated sintering [43].
Other types of complications were reported in two articles: chipping/fracture of teeth in the opposing arch [44] in six removable prostheses and another [45] greater wear between the arches. The wear of any material is related to the type of mechanical contact, surface roughness, microstructural characteristics, fracture resistance, occlusal load, and environment [46]. The hardness of the material has no significant correlation with wear on the teeth of the opposing arch [47].
4.2. Survival Rate
In Papaspyridakos et al.’s study [17], the complications of 55 full arches rehabilitated with implant-supported metal–ceramic prostheses were studied in an average follow-up time of 5 years. The prostheses exhibited a 98.2% survival rate, with only one failure after 5 years. Complications were divided into minor complications (ceramic wear in 20 prostheses, 84 chipping points in 29 prostheses, and 7 pillars lost in 4 prostheses). Regarding major complications, there were 26 fractures of the veneering ceramic in 9 prostheses, 1 fracture of the infrastructure, and 6 fractures of the screws in 2 prostheses. Gonzalez-Gonzalez et al. [5] reported a 98.8% survival of 80 prostheses in the 5-year follow-up, presenting the loss of the covering material for the screw access cavities, chipping of the covering ceramic, and loss of retaining screws as the main complications. Regarding fixed metal–acrylic prostheses, Barootchi et al. [48] referred to 43 prostheses with a success rate of 83% in 5 years, 67.6% in 8 years, and 51.7% in 10 years. The minor complication was the displacement or fracture of a tooth (94 times in 22 prostheses), and, as a major complication, the fracture of multiple teeth (40 times in 17 prostheses).
Approaching another type of material, two studies by Caramês et al. [2,49] addressed the rehabilitation of full arches in monolithic zirconia. In the first study, 177 fixed prostheses with all-ceramic veneer and ceramic veneer in non-functional areas were observed with a follow-up of 2 years. During the follow-up, two fractures were observed, one for each group, and a minor complication was chipping. The survival between groups was similar: 98.7% for full-arch ceramic-veneered zirconia and 99% for monolithic zirconia with porcelain veneering limited to buccal rehabilitations (non-functional areas). However, the latter only presented complications when the opposing arch was made of monolithic zirconia [2]. In the second study [49], the author mentioned 92 prostheses of which 50% did not have any complications, 28 (30.4%) reported small chipping easily resolved with polishing, 16 (17.4%) exhibited complications that required removal and repair in the laboratory and only 2 prostheses fractured and were remade. The final success rate was 83.4% after a 5-year follow-up, and the authors reported that prostheses without distal extension had an increased risk of major chipping.
4.3. Study Limitations
The main limitation of this investigation was centered on the reduced number of articles found for the theme proposed. Furthermore, another question raised was that several authors define monolithic zirconia with porcelain veneering limited to non-functional areas as monolithic zirconia. However, the word monolithic is defined by the glossary of prosthodontic terms [11] as an object with the same chemical and physical properties throughout its thickness. This is understood as just one material in a single block without any porcelain veneering, other than just the placement of a pigment or final glaze. Our study also included monolithic zirconia prostheses with a slight gingival area covered by a ceramic layer. The development of new studies on this topic must produce more scientific evidence with follow-ups greater than 5 years to permit the assessment of the survival rate and complications in the long term.
5. Conclusions
Within the limitations of this investigation, it was possible to conclude that implant-supported full-arch rehabilitations in monolithic zirconia demonstrated a high survival rate and a minimal level of complications in an average period of 4 years.
Author Contributions
Conceptualization, A.C. and L.M.V.; methodology, L.M.V., L.A., A.C.; software, L.M.V., L.A.; validation, L.M.V., L.A., P.F., F.A., G.V.O.F., A.C.; formal analysis, L.M.V., L.A., A.C.; investigation, L.M.V., L.A., J.C.H.F., P.F., F.A., W.T., G.V.O.F., A.C.; resources, P.F., F.A., G.V.O.F., A.C.; data curation, L.M.V., L.A., G.V.O.F., A.C.; writing—original draft preparation, J.C.H.F., P.F., F.A., W.T., G.V.O.F., A.C.; writing—review and editing, J.C.H.F., W.T., G.V.O.F., A.C.; visualization, P.F., F.A., G.V.O.F., A.C.; supervision, P.F., F.A., A.C.; project administration, A.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bidra, A.S.; Rungruanganunt, P.; Gauthier, M. Clinical outcomes of full arch fixed implant-supported zirconia prostheses: A systematic review. Eur. J. Oral. Implantol. 2017, 10 (Suppl. 1), 35–45. [Google Scholar] [PubMed]
- Carames, J.; Marques, D.; Malta Barbosa, J.; Moreira, A.; Crispim, P.; Chen, A. Full-arch implant-supported rehabilitations: A prospective study comparing porcelain-veneered zirconia frameworks to monolithic zirconia. Clin. Oral. Implant. Res. 2019, 30, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Barbin, T.; Silva, L.D.R.; Veloso, D.V.; Borges, G.A.; Presotto, A.G.C.; Barao, V.A.R.; Groppo, F.C.; Mesquita, M.F. Biomechanical behavior of CAD/CAM cobalt-chromium and zirconia full-arch fixed prostheses. J. Adv. Prosthodont. 2020, 12, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Dieguez-Pereira, M.; Chavarri-Prado, D.; Estrada-Martinez, A.; Perez-Pevida, E.; Brizuela-Velasco, A. Monolithic and Minimally Veneered Zirconia Complications as Implant-Supported Restorative Material: A Retrospective Clinical Study up to 5 Years. Biomed. Res. Int. 2020, 2020, 8821068. [Google Scholar] [CrossRef]
- Gonzalez-Gonzalez, I.; Dellanos-Lanchares, H.; Brizuela-Velasco, A.; Alvarez-Riesgo, J.-A.; Llorente-Pendas, S.; Herrero-Climent, M.; Alvarez-Arenal, A. Complications of Fixed Full-Arch Implant-Supported Metal-Ceramic Prostheses. Int. J. Environ. Res. Public Health 2020, 17, 4250. [Google Scholar] [CrossRef]
- Nazari, V.; Ghodsi, S.; Alikhasi, M.; Sahebi, M.; Shamshiri, A.R. Fracture Strength of Three-Unit Implant Supported Fixed Partial Dentures with Excessive Crown Height Fabricated from Different Materials. J. Dent. 2016, 13, 400–406. [Google Scholar]
- Cevik, P.; Schimmel, M.; Yilmaz, B. New generation CAD-CAM materials for implant-supported definitive frameworks fabricated by using subtractive technologies. Biomed. Res. Int. 2022, 2022, 3074182. [Google Scholar] [CrossRef]
- Alarcón-Sánchez, M.A.; Heboyan, A.; Fernandes, G.V.O.; Castro-Alarcón, N.; Romero-Castro, N.S. Potential Impact of Prosthetic Biomaterials on the Periodontium: A Comprehensive Review. Molecules 2023, 28, 1075. [Google Scholar] [CrossRef]
- Desai, S.R.; Koulgikar, K.D.; Alqhtani, N.R.; Alqahtani, A.R.; Alqahtani, A.S.; Alenazi, A.; Heboyan, A.; Fernandes, G.V.O.; Mustafa, M. Three-Dimensional FEA Analysis of the Stress Distribution on Titanium and Graphene Frameworks Supported by 3 or 6-Implant Models. Biomimetics 2023, 8, 15. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Scarano, A.; Cortellari, G.C.; Fernandes, G.V.O.; Mesquita, A.M.M.; Bianchini, M.A. Marginal Bone Level and Biomechanical Behavior of Titanium-Indexed Abutment Base of Conical Connection Used for Single Ceramic Crowns on Morse-Taper Implant: A Clinical Retrospective Study. J. Funct. Biomater. 2023, 14, 128. [Google Scholar] [CrossRef]
- Tischler, M.; Patch, C.; Bidra, A.S. Rehabilitation of edentulous jaws with zirconia complete-arch fixed implant-supported prostheses: An up to 4-year retrospective clinical study. J. Prosthet. Dent. 2018, 120, 204–209. [Google Scholar] [CrossRef]
- Ferro, K.J.; Morgano, S.M.; Driscoll, C.F.; Freilich, M.A.; Guckes, A.D.; Knoernschild, K.L.; McGarry, T.J. The Glossary of Prosthodontic Terms: Ninth Edition. J. Prosthet. Dent. 2017, 117, e1–e105. [Google Scholar]
- Apratim, A.; Eachempati, P.; Krishnappa Salian, K.K.; Singh, V.; Chhabra, S.; Shah, S. Zirconia in dental implantology: A review. J. Int. Soc. Prev. Community Dent. 2015, 5, 147–156. [Google Scholar] [CrossRef]
- Borges, H.; Correia, A.R.M.; Castilho, R.M.; Fernandes, G.V.O. Zirconia Implants and Marginal Bone Loss: A Systematic Review and Meta-Analysis of Clinical Studies. Int. J. Oral. Maxillofac. Implants. 2020, 35, 707–720. [Google Scholar] [CrossRef]
- Bona, A.D.; Pecho, O.E.; Alessandretti, R. Zirconia as a Dental Biomaterial. Materials 2015, 8, 4978–4991. [Google Scholar] [CrossRef]
- Bidra, A.S.; Tischler, M.; Patch, C. Survival of 2039 complete arch fixed implant-supported zirconia prostheses: A retrospective study. J. Prosthet. Dent. 2018, 119, 220–224. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Bordin, T.B.; Natto, Z.S.; El-Rafie, K.; Pagni, S.E.; Chochlidakis, K.; Ercoli, C.; Weber, H.-P. Complications and survival rates of 55 metal-ceramic implant-supported fixed complete-arch prostheses: A cohort study with mean 5- year follow-up. J. Prosthet. Dent. 2019, 122, 441–449. [Google Scholar] [CrossRef]
- Esquivel-Upshaw, J.; Kim, M.; Hsu, S.; Abdulhameed, N.; Jenkins, R.; Neal, D.; Ren, F.; Clark, A. Randomized clinical study of wear of enamel antagonists against polished monolithic zirconia crowns. J. Dent. 2018, 68, 19–27. [Google Scholar] [CrossRef]
- Stober, T.; Bermejo, J.L.; Rammelsberg, P.; Schmitter, M. Enamel wear caused by monolithic zirconia crowns after 6 months of clinical use. J. Oral. Rehabil. 2014, 41, 314–322. [Google Scholar] [CrossRef]
- Sailer, I.; Balmer, M.; Husler, J.; Hammerle, C.H.F.; Kanel, S.; Thoma, D.S. 10- year randomized trial (RCT) of zirconia-ceramic and metal-ceramic fixed dental prostheses. J. Dent. 2018, 76, 32–39. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Tan, K.; Lang, N.P.; Bragger, U.; Egger, M.; Zwahlen, M. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin. Oral. Implant. Res. 2004, 15, 625–642. [Google Scholar] [CrossRef]
- Tirone, F.; Salzano, S.; Rolando, E.; Pozzatti, L.; Rodi, D. Framework Fracture of Zirconia Supported Full Arch Implant Rehabilitation: A Retrospective Evaluation of Cantilever Length and Distal Cross-Sectional Connection Area in 140 Patients Over an Up-To-7 Year Follow-Up Period. J. Prosthodont. 2022, 31, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Franco, A.; Vidigal, M.T.C.; de Oliveira, M.N.; de Nascimento, C.T.; da Silva, R.F.; Paranhos, L.R. Evidence-based mapping of third molar techniques for age estimation applied to Brazilian adolescents—A systematic review. Res. Soc. Dev. 2020, 9, e9339109395. [Google Scholar] [CrossRef]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, 6th ed.; Cochrane: London, UK, 2019. [Google Scholar]
- Box, V.H.; Sukotjo, C.; Knoernschild, K.L.; Campbell, S.D.; Afshari, F.S. Patient-Reported and Clinical Outcomes of Implant-Supported Fixed Complete Dental Prostheses: A Comparison of Metal-Acrylic, Milled Zirconia, and Retrievable Crown Prostheses. J. Oral. Implantol. 2018, 44, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Limmer, B.; Sanders, A.E.; Reside, G.; Cooper, L.F. Complications and patient-centered outcomes with an implant-supported monolithic zirconia fixed dental prosthesis: 1 year results. J. Prosthodont. 2014, 23, 267–275. [Google Scholar] [CrossRef]
- Rojas Vizcaya, F. Retrospective 2- to 7-Year Follow-Up Study of 20 Double Full-Arch Implant-Supported Monolithic Zirconia Fixed Prostheses: Measurements and Recommendations for Optimal Design. J. Prosthodont. 2018, 27, 501–508. [Google Scholar] [CrossRef]
- Ferreira, P.W.; Nogueira, P.J.; Nobre, M.A.A.; Guedes, C.M.; Salvado, F. Impact of Mechanical Complications on Success of Dental Implant Treatments: A Case-Control Study. Eur. J. Dent. 2022, 16, 179–187. [Google Scholar] [CrossRef]
- Ettl, T.; Junold, N.; Zeman, F.; Hautmann, M.; Hahnel, S.; Kolbeck, C.; Müller, S.; Klingelhöffer, C.; Reichert, T.E.; Meier, J.K. Implant survival or implant success? Evaluation of implant-based prosthetic rehabilitation in head and neck cancer patients-a prospective observational study. Clin. Oral. Investig. 2020, 24, 3039–3047. [Google Scholar] [CrossRef]
- Chang, J.S.; Ji, W.; Choi, C.H.; Kim, S. Catastrophic failure of a monolithic zirconia prosthesis. J. Prosthet. Dent. 2015, 113, 86–90. [Google Scholar] [CrossRef]
- Durkan, R.; Oyar, P.; Deste, G. Effects of Cantilever Length and Implant Inclination on the Stress Distribution of Mandibular Prosthetic Restorations Constructed from Monolithic Zirconia Ceramic. Int. J. Oral. Maxillofac. Implant. 2020, 35, 121–129. [Google Scholar] [CrossRef]
- Alshahrani, F.A.; Yilmaz, B.; Seidt, J.D.; McGlumphy, E.A.; Brantley, W.A. A load-to-fracture and strain analysis of monolithic zirconia cantilevered frameworks. J. Prosthet. Dent. 2017, 118, 752–758. [Google Scholar] [CrossRef]
- Sailer, I.; Muhlemann, S.; Zwahlen, M.; Hammerle, C.H.; Schneider, D. Cemented and screw-retained implant reconstructions: A systematic review of the survival and complication rates. Clin. Oral. Implant. Res. 2012, 23 (Suppl. 6), 163–201. [Google Scholar] [CrossRef]
- Wright, S.P.; Hayden, J.; Lynd, J.A.; Walker-Finch, K.; Willett, J.; Ucer, C.; Speechley, S.D. Factors affecting the complexity of dental implant restoration—What is the current evidence and guidance? Br. Dent. J. 2016, 221, 615–622. [Google Scholar] [CrossRef]
- Gaddale, R.; Mishra, S.K.; Chowdhary, R. Complications of screw- and cement-retained implant-supported full-arch restorations: A systematic review and meta-analysis. Int. J. Oral. Implantol. 2020, 13, 11–40. [Google Scholar]
- Oda, Y.; Mori, G.; Sasaki, H.; Furuya, Y.; Ito, T.; Iijima, T.; Sekine, H.; Yajima, Y. Dimensional changes of buccal bone in the edentulous maxilla with telescopic-retained implant-supported fixed dental prostheses. J. Prosthet. Dent. 2021. [Google Scholar] [CrossRef]
- Waltimo, A.; Kononen, M. A novel bite force recorder and maximal isometric bite force values for healthy young adults. Scand J. Dent. Res. 1993, 101, 171–175. [Google Scholar] [CrossRef]
- Cosme, D.C.; Baldisserotto, S.M.; Andrade, C.S.; Shinkai, R.S. Bruxism and voluntary maximal bite force in young dentate adults. Int. J. Prosthodont. 2005, 18, 328–332. [Google Scholar]
- Umesh, S.; Padma, S.; Asokan, S.; Srinivas, T. Fiber Bragg Grating based bite force measurement. J. Biomech. 2016, 49, 2877–2881. [Google Scholar] [CrossRef]
- Gonzalez, J.; Triplett, R.G. Complications and Clinical Considerations of the Implant-Retained Zirconia Complete-Arch Prosthesis with Various Opposing Dentitions. Int. J. Oral. Maxillofac. Implant. 2017, 32, 864–869. [Google Scholar] [CrossRef]
- Calderon, U.; Hicklin, S.; Mojon, P.; Fehmer, V.; Nesic, D.; Mekki, M.; Sailer, I. Influence of the Titanium Base Abutment Design on Monolithic Zirconia Multiple-Unit Implant Fixed Dental Prostheses: A Laboratory Study. Int. J. Oral. Maxillofac. Implant. 2022, 37, 19–29. [Google Scholar] [CrossRef]
- Carames, J.; Tovar Suinaga, L.; Yu, Y.C.; Perez, A.; Kang, M. Clinical Advantages and Limitations of Monolithic Zirconia Restorations Full Arch Implant Supported Reconstruction: Case Series. Int. J. Dent. 2015, 2015, 392496. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Oh, S.H.; Kim, J.H.; Ju, S.W.; Seo, D.G.; Jun, S.H.; Ahn, J.S.; Ryu, J.J. Wear evaluation of the human enamel opposing different Y-TZP dental ceramics and other porcelains. J. Dent. 2012, 40, 979–988. [Google Scholar] [CrossRef] [PubMed]
- Rammelsberg, P.; Meyer, A.; Lorenzo-Bermejo, J.; Kappel, S.; Zenthofer, A. Long-term chipping and failure rates of implant-supported and combined tooth-implant-supported metal-ceramic and ceramic fixed dental prostheses: A cohort study. J. Prosthet. Dent. 2021, 126, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Schwindling, F.S.; Waldecker, M.; Rammelsberg, P.; Rues, S.; Bomicke, W. Tooth substance removal for ceramic single crown materials-an in vitro comparison. Clin. Oral. Investig. 2019, 23, 3359–3366. [Google Scholar] [CrossRef]
- Sripetchdanond, J.; Leevailoj, C. Wear of human enamel opposing monolithic zirconia, glass ceramic, and composite resin: An in vitro study. J. Prosthet. Dent. 2014, 112, 1141–1150. [Google Scholar] [CrossRef]
- Jung, Y.S.; Lee, J.W.; Choi, Y.J.; Ahn, J.S.; Shin, S.W.; Huh, J.B. A study on the in-vitro wear of the natural tooth structure by opposing zirconia or dental porcelain. J. Adv. Prosthodont. 2010, 2, 111–115. [Google Scholar] [CrossRef]
- Barootchi, S.; Askar, H.; Ravida, A.; Gargallo-Albiol, J.; Travan, S.; Wang, H.L. Long-term Clinical Outcomes and Cost-Effectiveness of Full-Arch Implant-Supported Zirconia-Based and Metal-Acrylic Fixed Dental Prostheses: A Retrospective Analysis. Int. J. Oral. Maxillofac. Implant. 2020, 35, 395–405. [Google Scholar] [CrossRef]
- Carames, J.M.M.; da Mata, A.D.S.P.; da Silva Marques, D.N.; de Oliveira Francisco, H.C. Ceramic-Veneered Zirconia Frameworks in Full-Arch Implant Rehabilitations: A 6-Month to 5-Year Retrospective Cohort Study. Int. J. Oral. Maxillofac. Implant. 2016, 31, 1407–1414. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).