Survival of Single Immediate Implants and Reasons for Loss: A Systematic Review
Abstract
1. Summary Box
- What is known:
- What this study adds:
2. Introduction
3. Materials and Methods
3.1. Search Strategy
- Randomised controlled trial;
- Study included a minimum of six human subjects or more, including split mouth studies;
- Used single-unit immediate implants;
- Minimum follow-up time of one year;
- Full-text study published in English
3.2. Study Selection
3.3. Data Extraction
3.4. Risk of Bias Assessment
| Study | Group | Settings | Follow-Up Time (Months) | Imp Survival % (IPL) | Imp Survival % (IPR) | Imp Survival % (IPDL) | Imp Survival % (DP) | Reason for Implant Failure | Antibiotics | Bone Grafting | Implant System/ Platform/ Geometry | Location in Jaw: No. of Imps |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Canullo et al., 2009/2017 [21,22] | IPR | Mc (2 PP) | 25, 120 | N/A | 100 | N/A | N/A | N/A | Augmentin: 1 h pre-op and 6 days post-op | Bovine bone matrix (Bio-Oss Collagen, Geistlich-Pharma, Wolhusen, Switzerland) | Global imp, 5.5 mm, 13 mm | Mx: 19 |
| Tallarico et al., 2016/2017 [23,24] | IPDL vs. DP | PP | 12 (6 months post loading) | N/A | N/A | 100 | 100 | N/A | Amoxicillin/Clindamycin: 1 h pre-op | Corticocancellous heterologous bone (OsteoBiol Gen-Os; Tecnoss srl, Giaveno, Italy) | Osstem TSIII Ultra-Wide 7 mm-diameter. 8.5 mm long (n = 4), 10 mm long (n = 18), and 11.5 mm long (n = 2) | Mx: 12 Md: 12 |
| Cannizzaro et al., 2010 [25] | IPL, IPR vs. DP | Mc (4 PP) | 36 | 40 | 80 | N/A | 97 | 1 IPL imp failed as bruxism habit was only diagnosed after failure; 4 imps failed to osseointegrate | Amoxicillin/Clindamycin: pre-op and 6 days post-op if graft was performed | Autogenous bone or bone substitutes | Z-Look3 zirconia implants, 3.25–6 mm, 10–15.5 mm | Mx: 29 Md: 11 |
| Shibly et al., 2012 [26] | IPL vs. IPDL | U | 3, 6, 12 | 96.6 | N/A | 93.3 | N/A | 1 imp failed due to mobility; 1 imp failed from acute infection 3 months after placement; 1 imp failed with no reason for implant failure given | Amoxicillin: 2 days pre-op and 10 days post-op | Sterile demineralized freeze-dried bone (DFDBA)—OraGRAFT, LifeNet Health, Virginia Beach, VA, USA. | NobelReplace™ Straight Groovy, with TiUnite® surface, Nobel Biocare | Mx: 36 Md: 19 |
| Block et al., 2009 [27] | IPR vs. IPDL | Not specified | 1, 2, 3, 4, 10, 16, 22 28 | N/A | 84.6 | 96.6 | N/A | 5 implants failed with no reason given | Cephalosporin: 7 days post-op | Human mineralized bone allograft | 3i, 11.5–13 mm | Mx: 55 |
| Canullo et al., 2010 [28] | IPR | Mc (3 PP) | 36 | N/A | 100 | N/A | N/A | N/A | Augmentin: 1 h pre-op | Nano-structured hydroxyapatite (Sintlife, Faenza, Italy) | Global Implant, 5.5 mm, 13 mm | Mx: 32 |
| De Rouck et al., 2009 [29] | IPR vs. IPDL | U | 12 | N/A | 96 | 92 | N/A | 1 imp failed due to mobility at 1 month; 2 imps failed due to mobility and pain at 3 months | Amoxicillin: 1 h pre-op and 5 days post-op | Bio-Oss®, (Geistlich Biomaterials, Mediplus, Rixensart, Belgium) | NobelReplace Tapered TiUnite, mostly diameter 4.3 mm, 16 mm | Mx: 30 |
| Degidi et al., 2014 [30] | IPR | PP | 24 | N/A | 100 | N/A | N/A | N/A | Amoxicillin: 1 h pre-op and 5 days post-op | Not specified | Square-threaded, grit-blasted, and acid-etched implant with a tapered connection (ANKYLOS®, DENTSPLY) | Mx: 53 |
| Esposito et al., 2015 [31] | IPR/IPDL vs. DP | Mc (3 PP) | 12 | N/A | 96.3 Study did not give separate results for IPR and IPDL imp | 100 | 1 imp failed due to mobility and pain at 1 month; 1 imp failed due to mobility at 4 months and imp crown was loose 20 days earlier | Amoxicillin/Clindamycin: 1 h pre-op and 6 days post-op if grafting was performed | Bio-Oss (Geistlich Pharma AG, Wolhusen, Switzerland) | Tapered titanium EZ Plus dental implants (MegaGen Implant, Gyeongbuk, Republic of Korea) with an internal connection, and RBM-treated surfaces, already provided with their definitive straight abutments | Mx: 106 | |
| Felice et al., 2015 [32] | IPR/IPDL vs. DP | Mc (4 PP) | 4, 12 | N/A | 92 Study did not give separate results for IPR and IPDL imp | 100 | 2 imps failed with unpleasant sensation/pain and mobility after 2 months after loading | Amoxicillin/Clindamycin: 1 h pre-op and 6 days post-op if grafting was performed | Frios Algipore (Dentsply, Friadent) | XiVE S plus (Dentsply Friadent, Mannheim, Germany) titanium, self-tapping, conical implants with an internal hexagon.Length choices: 8.0, 9.5, 11.0, 13.0, or 15.0 mm and diameters choices: 3.8, 4.5, or 5.5 mm | Mx: 48 | |
| Grandi et al., 2014 [33] | IPR | Mc | 12 | N/A | 100 | N/A | N/A | N/A | Augmentin/Clarithromycin: pre-op and 6/7 days post-op | Bio-Oss (Geistlich Bio-Oss, Geistlich Pharma, Wolhusen, Switzerland) | Tapered implants with internal connection and double acid-etched surface | Mx: 36 |
| Migliorati et al., 2015 [34] | IPR | Not specified | 0, 0.5, 12, 24 | N/A | 100 | N/A | N/A | N/A | Amoxicillin/Clindamycin: 1 h pre-op | Bio-Oss (Geistlich Pharma North America, Inc., Princeton, NJ, USA) | Tapered Effect or Bone Level SLActive, Straumann Co., Basel, Switzerland | Mx: 48 |
| Palatella et al., 2008 [35] | IPR vs. DP | U | 24 | N/A | 100 | N/A | 100 | N/A | Augmentin: 5 days post-op | - | Tapered effect (Institut Straumann AG, Waldenburg, Switzerland | Mx: 18 |
| Pieri et al., 2011 [36] | IPR | U | 12 | N/A | 97.4 | N/A | N/A | 1 imp failed with an abscess associated with a fistula | Augmentin: pre-op and 1 week post-op | Mixture of autogenous bone and Bio-Oss | Samo Smiler, root-shaped, microthreads in coronal portion, microporous and nanoroughened calcium and phosphorus-enriched titanium oxide surface. Platform switched when using Morse taper abutment | Mx: 38 |
| Slagter et al., 2015 [37] | IPR vs. IPDL | U | 12 | N/A | 100 | 100 | N/A | N/A | Amoxicillin: 7 days pre-op | Mixture of autogenous bone and Bio-Oss | NobelActive, Nobel BIocare AB | Mx: 40 |
| Yoshino et al., 2014 [38] | IPR | U | 12 | N/A | 100 | N/A | N/A | N/A | Did not specify antibiotic regime | BioOss, Osteohealth | Bone Level, Straumann USA. Dimensions: 3.3 mm, 14 mm (n = 5), 4.1 mm, 14 mm (n = 14), and 4.8 mm, 14 mm (n = 1) | Mx: 20 |
| Zuiderveld et al., 2018 [39] | IPR | U | 12 | N/A | 96.7 | N/A | N/A | 2 imps failed to osseointegrate | Amoxicillin/Clindamycin: 1 day pre-op and 7 days post-op | Bio-Oss and autogenous bone | Not specified | Mx: 60 |
| Cecchinato et al., 2015 [40] | IPDL | Mc | 36 | N/A | N/A | 98.9 | N/A | 1 imp was mobile at 16 weeks | No antibiotics used | Not specified | Either a cylindrical, 3.5 mm or 4.0 mm implant or a conical/cylindrical 4.5 or 5.0 mm implant (Osseospeed, DENTSPLY Implants) | Mx: 92 |
| Cordaro et al., 2009 [41] | IPDL | PP | 0, 1.5, 3, 6, 12, 18 | N/A | N/A | 96.6 | N/A | 1 imp failed due to prosthetic overload from under-trimming the removable prosthesis | No antibiotics used | Not specified | Tapered TE implants (Straumann) | Not specified (n = 30) |
| Cucchi et al., 2017 [42] | IPDL vs. DP | Mc | 12, 36 | N/A | N/A | 95.5 | 100 | 2 imps failed to osseointegrate | Amoxicillin: 1 h pre-op and 6 h post-op | Resorbable B-tricalcium phosphate (Oxofix, Biotec BTK, Dueville, Vicenza, Italy, BTK Italy) | BT SAFE Bone Level—double lead threads with a hexagonal conical connection and integrated platform shifting | Mx: 25 Md: 24 |
| De Angelis et al., 2011 [43] | IPDL | Mc (4 PP) | 12 | N/A | N/A | 91.3 | N/A | 6 imps were mobile at abutment connection at 3–4 months; 1 imp failed after 3-month loading at 6–7 months after placement | Amoxicillin/clindamycin: 1 h pre-op and 6 days post-op | Endobon® (Biomet 3i), a bovine-derived, deproteinised, osteoconductive hydroxyapatite ceramic | NanoTite™ Tapered Certain® Prevail® titanium alloy (Ti6Al4V) implants (Biomet 3i, Palm Beach, FL, USA) with internal connection. Dual acid etched and then partially covered with nanoscale calcium phosphate crystals. Biomet 3i platform-switched abutments | Mx: 50 Md: 30 |
| Koh et al., 2011 [44] | IPDL | U | 12 | N/A | N/A | 95.5 | N/A | 1 imp failed with no reason given | Amoxicillin/Azithromycin: pre-op and 7/3 days post-op | Mixture of cortical and cancellous particulates allograft (MinerOss) | Tapered internal implant, BioHorizon, Birmingham, AL | Mx: 21 |
| Prosper et al., 2003 [45] | IPDL | U | 3, 6, 9, 12, 24, 36, 48 | N/A | N/A | 100 | N/A | N/A | Augmentin: 6 days post-op | Synthetic hydroxyapatite (Biosite; Vebas, Milan, Italy) | Sandblasted, titanium (Bioactive Covering, Winsix, London, United Kingdom), self-threading cylindric screw, 5.9, 11, or 13 mm | Mx: 75 Md: 36 |
| Urban et al., 2011 [46] | IPDL | Not specified | 0.25, 12 | N/A | N/A | 83.7 | N/A | 15 imps failed to osseointegrate | Phenoxymethylpenicillin: 5 days pre-op | Autologous bone | Brånemark System, Mk III Groovy, Wide Platform implant (NobelBiocare, Göteborg, Sweden) with an external hex connection, 5.0 mm and a thread spacing of 0.8 mm | Mx: 45 Md: 47 |
| Crespi et al., 2008 [47] | IPL vs. IPDL | U | 24 | 100 | N/A | 100 | N/A | N/A | Amoxicillin: 1 h pre-op and 1 week post-op | Not specified | 40 outlink, Sweden & Marina, Pafova implants. 30 implants: 5 mm, 10 implants: 3.75 mm, 13 mm | Mx: 40 |
| Van Nimwegen et al., 2018 [48] | IPR | U | 12 | N/A | 96.7 | N/A | N/A | 2 imps failed to osseointegrate | Amoxicillin: pre-op and 7 days post-op | Mixture of autogenous bone and Bio-Oss | NobelActive (Nobel Biocare) | Mx: 60 |
4. Results
4.1. Survival Rates
4.2. Reasons Given for Implant Failure
4.3. Patient Selection Criteria
4.4. Loading Protocol
4.5. Antibiotic Therapy
4.6. Setting
4.7. Grafting Materials
4.8. Implants System/Geometry
4.9. Location of the Implant
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bhola, M.; Neely, A.L.; Kolhatkar, S. Immediate Implant Placement: Clinical Decisions, Advantages, and Disadvantages. J. Prosthodont. 2008, 17, 576–581. [Google Scholar] [CrossRef]
- Hebel, K.; Gajjar, R.; Hofstede, T. Single-tooth replacement: Bridge vs. implant-supported restoration. J. (Can. Dent. Assoc.) 2000, 66, 435. [Google Scholar]
- Wilson, T.G., Jr.; Schenk, R.; Buser, D.; Cochran, D. Implants Placed in Immediate Extraction Sites: A Report of Histologic and Histometric Analyses of Human Biopsies. Int. J. Oral Maxillofac. Implant. 1998, 13, 333–341. [Google Scholar]
- Solderer, A.; Al-Jazrawi, A.; Sahrmann, P.; Jung, R.; Attin, T.; Schmidlin, P.R. Removal of failed dental implants revisited: Questions and answers. Clin. Exp. Dent. Res. 2019, 5, 712–724. [Google Scholar] [CrossRef] [PubMed]
- Chee, W.; Jivraj, S. Failures in implant dentistry. Br. Dent. J. 2007, 202, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Heimisdottir, K. Dental implants—Are they better than natural teeth? Eur. J. Oral Sci. 2018, 126, 81–87. [Google Scholar] [CrossRef]
- International Team for Implantology. Implant Survival and Complications. In Proceedings of the Third ITI Consensus Conference, Gstaad, Switzerland, August 2003; pp. 7–154. [Google Scholar]
- Esposito, M.; Hirsch, J.-M.; Lekholm, U.; Thomsen, P. Biological factors contributing to failures of osseointegrated oral implants, (II). Etiopathogenesis. Eur. J. Oral Sci. 1998, 106, 721–764. [Google Scholar] [CrossRef] [PubMed]
- Atieh, M.A.; Payne, A.G.T.; Duncan, W.J.; de Silva, R.K.; Cullinan, M.P. Immediate Placement or Immediate Restoration/Loading of Single Implants for Molar Tooth Replacement: A Systematic Review and Meta-analysis. Int. J. Oral Maxillofac. Implant. 2010, 25, 401–415. [Google Scholar]
- Chen, S.T.; Buser, D. Esthetic outcomes following immediate and early implant placement in the anterior maxilla—A systematic review. Int. J. Oral Maxillofac. Implant. 2014, 29, 186–215. [Google Scholar] [CrossRef]
- Cosyn, J.; De Lat, L.; Seyssens, L.; Doornewaard, R.; Deschepper, E.; Vervaeke, S. The effectiveness of immediate implant placement for single tooth replacement compared to delayed implant placement: A systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46, 224–241. [Google Scholar] [CrossRef]
- Lang, N.P.; Pun, L.; Lau, K.Y.; Li, K.Y.; Wong, M.C. A systematic review on survival and success rates of implants placed immediately into fresh extraction sockets after at least 1 year. Clin. Oral Implant. Res. 2012, 23, 39–66. [Google Scholar] [CrossRef] [PubMed]
- Mello, C.C.; Lemos, C.A.A.; Verri, F.R.; dos Santos, D.M.; Goiato, M.C.; Pellizzer, E.P. Immediate implant placement into fresh extraction sockets versus delayed implants into healed sockets: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2017, 46, 1162–1177. [Google Scholar] [CrossRef]
- Pigozzo, M.N.; Rebelo da Costa, T.; Sesma, N.; Laganá, D.C. Immediate versus early loading of single dental implants: A systematic review and meta-analysis. J. Prosthet. Dent. 2018, 120, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Brägger, U.; Lang, N.P.; Zwahlen, M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin. Oral Implant. Res. 2007, 18, 97–113. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Needleman, I.G. A guide to systematic reviews. J. Clin. Periodontol. 2002, 29, 6–9. [Google Scholar] [CrossRef]
- Hämmerle, C.H.; Chen, S.T.; Wilson, T.G., Jr. Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets. Int. J. Oral Maxillofac. Implant. 2004, 19, 26–28. [Google Scholar]
- Cochran, D.L.; Morton, D.; Weber, H.P. Consensus statements and recommended clinical procedures regarding loading protocols for endosseous dental implants. Int. J. Oral Maxillofac. Implant. 2004, 19, 109–113. [Google Scholar]
- Higgins, J.P.T.; Altman, D.G.; Sterne, J.A.C. (Eds.) Chapter 8: Assessing Risk of Bias in Included Studies. In Cochrane Handbook for Systematic Reviews of Interventions Version 510 (Updated March 2011); The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- Canullo, L.; Caneva, M.; Tallarico, M. Ten-year hard and soft tissue results of a pilot double-blinded randomized controlled trial on immediately loaded post-extractive implants using platform-switching concept. Clin. Oral Implant. Res. 2017, 28, 1195–1203. [Google Scholar] [CrossRef]
- Canullo, L.; Goglia, G.; Iurlaro, G.; Iannello, G. Short-term bone level observations associated with platform switching in immediately placed and restored single maxillary implants: A preliminary report. Int. J. Prosthodont. 2009, 22, 277. [Google Scholar]
- Tallarico, M.; Xhanari, E.; Pisano, M.; De Riu, G.; Tullio, A.; Meloni, S.M. Single post-extractive ultra-wide 7 mm-diameter implants versus implants placed in molar healed sites after socket preservation for molar replacement: 6-month post-loading results from a randomised controlled trial. Eur. J. Oral Implantol. 2016, 9, 263. [Google Scholar] [PubMed]
- Tallarico, M.; Xhanari, E.; Pisano, M.; Gatti, F.; Meloni, S.M. Molar replacement with 7 mm-wide diameter implants: To place the implant immediately or to wait 4 months after socket preservation? 1 year after loading results from a randomised controlled trial. Eur. J. Oral Implantol. 2017, 10, 169. [Google Scholar] [PubMed]
- Cannizzaro, G.; Torchio, C.; Felice, P.; Leone, M.; Esposito, M. Immediate occlusal versus non-occlusal loading of single zirconia implants. A multicentre pragmatic randomised clinical trial. Eur. J. Oral. Implantol. 2010, 3, 111–120. [Google Scholar]
- Shibly, O.; Kutkut, A.; Patel, N.; Albandar, J.M. Immediate implants with immediate loading vs. conventional loading: 1-year randomized clinical trial. Clin. Implant. Dent. Relat. Res. 2012, 14, 663–671. [Google Scholar] [CrossRef] [PubMed]
- Block, M.S.; Mercante, D.E.; Lirette, D.; Mohamed, W.; Ryser, M.; Castellon, P. Prospective evaluation of immediate and delayed provisional single tooth restorations. J. Oral Maxillofac. Surg. 2009, 67, 89–107. [Google Scholar] [CrossRef] [PubMed]
- Canullo, L.; Bignozzi, I.; Cocchetto, R.; Cristalli, M.P.; Iannello, G. Immediate positioning of a definitive abutment versus repeated abutment replacements in post-extractive implants: 3-year follow-up of a randomised multicentre clinical trial. Eur. J. Oral Implantol. 2010, 3, 285. [Google Scholar] [PubMed]
- De Rouck, T.; Collys, K.; Wyn, I.; Cosyn, J. Instant provisionalization of immediate single-tooth implants is essential to optimize esthetic treatment outcome. Clin. Oral Implant. Res. 2009, 20, 566–570. [Google Scholar] [CrossRef]
- Degidi, M.; Nardi, D.; Daprile, G.; Piattelli, A. Nonremoval of Immediate Abutments in Cases Involving Subcrestally Placed Postextractive Tapered Single Implants: A Randomized Controlled Clinical Study. Clin. Implant. Dent. Relat. Res. 2014, 16, 794–805. [Google Scholar] [CrossRef]
- Esposito, M.; Barausse, C.; Pistilli, R.; Jacotti, M.; Grandi, G.; Tuco, L.; Felice, P. Immediate loading of post-extractive versus delayed placed single implants in the anterior maxilla: Outcome of a pragmatic multicenter randomised controlled trial 1-year after loading. Eur. J. Oral Implantol. 2015, 8, 347. [Google Scholar]
- Felice, P.; Pistilli, R.; Barausse, C.; Trullenque-Eriksson, A.; Esposito, M. Immediate non-occlusal loading of immediate post-extractive versus delayed placement of single implants in preserved sockets of the anterior maxilla: 1-year post-loading outcome of a randomised controlled trial. Eur. J. Oral Implantol. 2015, 8, 361. [Google Scholar]
- Grandi, T.; Guazzi, P.; Samarani, R.; Maghaireh, H.; Grandi, G. One abutment-one time versus a provisional abutment in immediately loaded post-extractive single implants: A 1-year follow-up of a multicentre randomised controlled trial. Eur. J. Oral Implantol. 2014, 7, 141. [Google Scholar] [PubMed]
- Migliorati, M.; Amorfini, L.; Signori, A.; Biavati, A.S.; Benedicenti, S. Clinical and Aesthetic Outcome with Post-Extractive Implants with or without Soft Tissue Augmentation: A 2-Year Randomized Clinical Trial. Clin. Implant. Dent. Relat. Res. 2015, 17, 983–995. [Google Scholar] [CrossRef] [PubMed]
- Palattella, P.; Torsello, F.; Cordaro, L. Two-year prospective clinical comparison of immediate replacement vs. immediate restoration of single tooth in the esthetic zone. Clin. Oral Implant. Res. 2008, 19, 1148–1153. [Google Scholar] [CrossRef]
- Pieri, F.; Aldini, N.N.; Marchetti, C.; Corinaldesi, G. Influence of implant-abutment interface design on bone and soft tissue levels around immediately placed and restored single-tooth implants: A randomized controlled clinical trial. Int. J. Oral Maxillofac. Implant. 2011, 26, 169. [Google Scholar]
- Slagter, K.W.; Meijer, H.J.A.; Bakker, N.A.; Vissink, A.; Raghoebar, G.M. Feasibility of immediate placement of single-tooth implants in the aesthetic zone: A 1-year randomized controlled trial. J. Clin. Periodontol. 2015, 42, 773–782. [Google Scholar] [CrossRef]
- Yoshino, S.; Kan, J.Y.K.; Rungcharassaeng, K.; Roe, P.; Lozada, J.L. Effects of connective tissue grafting on the facial gingival level following single immediate implant placement and provisionalization in the esthetic zone: A 1-year randomized controlled prospective study. Int. J. Oral Maxillofac. Implant. 2014, 29, 432–440. [Google Scholar] [CrossRef]
- Zuiderveld, E.G.; Meijer, H.J.A.; den Hartog, L.; Vissink, A.; Raghoebar, G.M. Effect of connective tissue grafting on peri-implant tissue in single immediate implant sites: A RCT. J. Clin. Periodontol. 2018, 45, 253–264. [Google Scholar] [CrossRef] [PubMed]
- Cecchinato, D.; Lops, D.; Salvi, G.E.; Sanz, M. A prospective, randomized, controlled study using OsseoSpeed™ implants placed in maxillary fresh extraction socket: Soft tissues response. Clin. Oral Implant. Res. 2015, 26, 20–27. [Google Scholar] [CrossRef]
- Cordaro, L.; Torsello, F.; Roccuzzo, M. Clinical outcome of submerged vs. non-submerged implants placed in fresh extraction sockets. Clin. Oral Implant. Res. 2009, 20, 1307–1313. [Google Scholar] [CrossRef]
- Cucchi, A.; Vignudelli, E.; Franco, S.; Levrini, L.; Castellani, D.; Pagliani, L.; Rea, M.; Modena, C.; Sandri, G.; Longhi, C. Tapered, double-lead threads single implants placed in fresh extraction sockets and healed sites of the posterior jaws: A multicenter randomized controlled trial with 1 to 3 years of follow-up. BioMed Res. Int. 2017, 2017, 8017116–8017175. [Google Scholar] [CrossRef]
- De Angelis, N.; Felice, P.; Pellegrino, G.; Camurati, A.; Gambino, P.; Esposito, M. Guided bone regeneration with and without a bone substitute at single post-extractive implants: 1-year post-loading results from a pragmatic multicentre randomised controlled trial. Eur. J. Oral Implantol. 2011, 4, 313. [Google Scholar]
- Koh, R.U.; Oh, T.J.; Rudek, I.; Neiva, G.F.; Misch, C.E.; Rothman, E.D.; Wang, H.L. Hard and soft tissue changes after crestal and subcrestal immediate implant placement. J. Periodontol. 2011, 82, 1112–1120. [Google Scholar] [CrossRef] [PubMed]
- Prosper, L.; Gherlone, E.F.; Redaelli, S.; Quaranta, M. Four-year follow-up of larger-diameter implants placed in fresh extraction sockets using a resorbable membrane or a resorbable alloplastic material. Int. J. Oral Maxillofac. Implant. 2003, 18, 856. [Google Scholar]
- Urban, T.; Kostopoulos, L.; Wenzel, A. Immediate implant placement in molar regions: A 12-month prospective, randomized follow-up study. Clin. Oral Implant. Res. 2012, 23, 1389–1397. [Google Scholar] [CrossRef] [PubMed]
- Crespi, R.; Capparé, P.; Gherlone, E.; Romanos, G.E. Immediate versus delayed loading of dental implants placed in fresh extraction sockets in the maxillary esthetic zone: A clinical comparative study. Int. J. Oral Maxillofac. Implant. 2008, 23, 753–758. [Google Scholar]
- van Nimwegen, W.G.; Raghoebar, G.M.; Zuiderveld, E.G.; Jung, R.E.; Meijer, H.J.A.; Muehlemann, S. Immediate placement and provisionalization of implants in the aesthetic zone with or without a connective tissue graft: A 1-year randomized controlled trial and volumetric study. Clin. Oral Implant. Res. 2018, 29, 671–678. [Google Scholar] [CrossRef]
- Amato, F.; Polara, G.; Spedicato, G.A. Tissue Dimensional Changes in Single-Tooth Immediate Extraction Implant Placement in the Esthetic Zone: A Retrospective Clinical Study. Int. J. Oral Maxillofac. Implant. 2018, 33, 439–447. [Google Scholar] [CrossRef]
- Al Nashar, A.; Yakoob, H. Evaluation of the use of plasma rich in growth factors with immediate implant placement in periodontally compromised extraction sites: A controlled prospective study. Int. J. Oral Maxillofac. Surg. 2015, 44, 507–512. [Google Scholar] [CrossRef]
- Chu, S.; Salama, M.; Salama, H.; Garber, D.; Saito, H.; Sarnachiaro, G.; Tarnow, D. The dual-zone therapeutic concept of managing immediate implant placement and provisional restoration in anterior extraction sockets. Compend. Contin. Educ. Dent. 2012, 33, 524–532, 534. [Google Scholar]
- Becker, B.E.; Becker, W.; Ricci, A.; Geurs, N. A Prospective Clinical Trial of Endosseous Screw-Shaped Implants Placed at the Time of Tooth Extraction without Augmentation. J. Periodontol. 1998, 69, 920–926. [Google Scholar] [CrossRef]
- Aires, I.; Berger, J. Immediate Placement in Extraction Sites Followed by Immediate Loading: A Pilot Study and Case Presentation. Implant. Dent. 2002, 11, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Boardman, N.; Darby, I.; Chen, S. A retrospective evaluation of aesthetic outcomes for single-tooth implants in the anterior maxilla. Clin. Oral Implant. Res. 2016, 27, 443–451. [Google Scholar] [CrossRef]
- Kohal, R.; Klaus, G.; Strub, J. Clinical investigation of a new dental immediate implant system. The reimplant-system. Dtsch. Zahnarztl. Z. 2001, 57, 495–497. [Google Scholar]
- De Sanctis, M.; Vignoletti, F.; Discepoli, N.; Zucchelli, G.; Sanz, M. Immediate implants at fresh extraction sockets: Bone healing in four different implant systems. J. Clin. Periodontol. 2009, 36, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Assaf, J.H.; Assaf, D.d.C.; Antoniazzi, R.P.; Osório, L.B.; França, F.M.G. Correction of Buccal Dehiscence during Immediate Implant Placement Using the Flapless Technique: A Tomographic Evaluation. J. Periodontol. 2017, 88, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Alves, C.C.; Correia, A.R.; Neves, M. Immediate implants and immediate loading in periodontally compromised patients-a 3-year prospective clinical study. Int. J. Periodontics Restor. Dent. 2010, 30, 447–455. [Google Scholar]
- Cornelini, R.; Scarano, A.; Covani, U.; Petrone, G.; Piattelli, A. Immediate one-stage postextraction implant: A human clinical and histologic case report. Int. J. Oral Maxillofac. Implant. 2000, 15, 432–437. [Google Scholar]
- Becker, W.; Lynch, S.E.; Lekholm, U.; Becker, B.E.; Caffesse, R.; Donath, K.; Sanchez, R. A Comparison of ePTFE Membranes Alone or in Combination with Platelet-Derived Growth Factors and Insulin-Like Growth Factor-I or Demineralized Freeze-Dried Bone in Promoting Bone Formation around Immediate Extraction Socket Implants. J. Periodontol. 1992, 63, 929–940. [Google Scholar] [CrossRef]
- Becker, W. Immediate implant placement: Treatment planning and surgical steps for successful outcomes. Br. Dent. J. 2006, 201, 199–205. [Google Scholar] [CrossRef]
- Buser, D.; Chappuis, V.; Kuchler, U.; Bornstein, M.M.; Wittneben, J.G.; Buser, R.; Cavusoglu, Y.; Belser, U.C. Long-term Stability of Early Implant Placement with Contour Augmentation. J. Dent. Res. 2013, 92, 176S–182S. [Google Scholar] [CrossRef]
- Basa, S.; Varol, A.; Turker, N. Alternative Bone Expansion Technique for Immediate Placement of Implants in the Edentulous Posterior Mandibular Ridge: A Clinical Report. Int. J. Oral Maxillofac. Implant. 2004, 19, 554–558. [Google Scholar]
- Anitua, E.; Piñas, L.; Alkhraisat, M.H. Long-Term Outcomes of Immediate Implant Placement into Infected Sockets in Association with Immediate Loading: A Retrospective Cohort Study. J. Periodontol. 2016, 87, 1135–1140. [Google Scholar] [CrossRef]
- de Molon, R.S.; de Avila, E.D.; de Barros-Filho, L.A.B.; Ricci, W.A.; Tetradis, S.; Cirelli, J.A.; Borelli de Barros, L.A. Reconstruction of the Alveolar Buccal Bone Plate in Compromised Fresh Socket after Immediate Implant Placement Followed by Immediate Provisionalization. J. Esthet. Restor. Dent. 2015, 27, 122–135. [Google Scholar] [CrossRef] [PubMed]
- Garber, D.A. The esthetic dental implant: Letting restoration be the guide. J. Am. Dent. Assoc. 1995, 126, 319–325. [Google Scholar] [CrossRef]
- Becker, C.M.; Wilson Jr, T.G.; Jensen, O.T. Minimum criteria for immediate provisionalization of single-tooth dental implants in extraction sites: A 1-year retrospective study of 100 consecutive cases. J. Oral Maxillofac. Surg. 2011, 69, 491–497. [Google Scholar] [CrossRef]
- Casap, N.; Zeltser, C.; Wexler, A.; Tarazi, E.; Zeltser, R. Immediate Placement of Dental Implants Into Debrided Infected Dentoalveolar Sockets. J. Oral Maxillofac. Surg. 2007, 65, 384–392. [Google Scholar] [CrossRef]
- Bell, C.; Bell, R.E. Immediate Restoration of NobelActive Implants Placed into Fresh Extraction Sites in the Anterior Maxilla. J. Oral Implantol. 2014, 40, 455–458. [Google Scholar] [CrossRef] [PubMed]
- Blus, C.; Szmukler-Moncler, S. Split-crest and immediate implant placement with ultra-sonic bone surgery: A 3-year life-table analysis with 230 treated sites. Clin. Oral Implant. Res. 2006, 17, 700–707. [Google Scholar] [CrossRef]
- Harvey, B.V. Optimizing the esthetic potential of implant restorations through the use of immediate implants with immediate provisionals. J. Periodontol. 2007, 78, 770–776. [Google Scholar] [CrossRef]
- Gelb, D.A. Immediate implant surgery: Three-year retrospective evaluation of 50 consecutive cases. Int. J. Oral Maxillofac. Implant. 1993, 8, 388–399. [Google Scholar]
- Bruno, V.; Badino, M.; Sacco, R.; Catapano, S. The use of a prosthetic template to maintain the papilla in the esthetic zone for immediate implant placement by means of a radiographic procedure. J. Prosthet. Dent. 2012, 108, 394–397. [Google Scholar] [CrossRef] [PubMed]
- Eghbali, A.; De Bruyn, H.; De Rouck, T.; Cleymaet, R.; Wyn, I.; Cosyn, J. Single Implant Treatment in Healing versus Healed Sites of the Anterior Maxilla: A Clinical and Radiographic Evaluation. Clin. Implant. Dent. Relat. Res. 2012, 14, 336–346. [Google Scholar] [CrossRef] [PubMed]
- Botticelli, D.; Berglundh, T.; Lindhe, J. Hard-tissue alterations following immediate implant placement in extraction sites. J. Clin. Periodontol. 2004, 31, 820–828. [Google Scholar] [CrossRef]
- Bogaerde, L.V.; Pedretti, G.; Sennerby, L.; Meredith, N. Immediate/Early Function of Neoss Implants Placed in Maxillas and Posterior Mandibles: An 18-Month Prospective Case Series Study. Clin. Implant. Dent. Relat. Res. 2010, 12, e83–e94. [Google Scholar] [CrossRef]
- Park, J.-B. Immediate Placement of Dental Implants into Fresh Extraction Socket in the Maxillary Anterior Region: A Case Report. J. Oral Implantol. 2010, 36, 153–157. [Google Scholar] [CrossRef]
- Gomez-Roman, G.; Schulte, W.; d’Hoedt, B.; Axman-Krcmar, D. The Frialit-2 implant system: Five-year clinical experience in single-tooth and immediately postextraction applications. Int. J. Oral Maxillofac. Implant. 1997, 12, 299–309. [Google Scholar]
- Le, B.; Borzabadi-Farahani, A.; Pluemsakunthai, W. Is buccolingual angulation of maxillary anterior implants associated with the crestal labial soft tissue thickness? Int. J. Oral Maxillofac. Surg. 2014, 43, 874–878. [Google Scholar] [CrossRef]
- Caiazzo, A.; Brugnami, F.; Mehra, P. Buccal plate preservation with immediate post-extraction implant placement and provisionalization: Preliminary results of a new technique. Int. J. Oral Maxillofac. Surg. 2013, 42, 666–670. [Google Scholar] [CrossRef] [PubMed]
- Cosyn, J.; De Bruyn, H.; Cleymaet, R. Soft tissue preservation and pink aesthetics around single immediate implant restorations: A 1-year prospective study. Clin. Implant. Dent. Relat. Res. 2013, 15, 847–857. [Google Scholar] [CrossRef]
- Paul, S. Risk versus gain in the flapless immediate approach for anterior implant esthetics: Case reports. Eur. J. Esthet. Dent. 2007, 2, 14–27. [Google Scholar]
- Hämmerle, C.H.; Brägger, U.; Schmid, B.; Lang, N.P. Successful bone formation at immediate transmucosal implants: A clinical report. Int. J. Oral Maxillofac. Implant. 1998, 13, 522–530. [Google Scholar]
- Chang, S.-W.; Shin, S.-Y.; Hong, J.-R.; Yang, S.-M.; Yoo, H.-M.; Park, D.-S.; Oh, T.-S.; Kye, S.-B. Immediate implant placement into infected and noninfected extraction sockets: A pilot study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Proussaefs, P.; Kan, J.; Lozada, J.; Kleinman, A.; Farnos, A. Effects of immediate loading with threaded hydroxyapatite-coated root-form implants on single premolar replacements: A preliminary report. Int. J. Oral Maxillofac. Implant. 2002, 17, 567–572. [Google Scholar]
- Calvo Guirado, J.L.; Saez Yuguero, M.R.; Pardo Zamora, G.; Muñoz Barrio, E. Immediate provisionalization on a new implant design for esthetic restoration and preserving crestal bone. Implant. Dent. 2007, 16, 155–164. [Google Scholar] [CrossRef]
- Covani, U.; Cornelini, R.; Barone, A. Bucco-Lingual Bone Remodeling around Implants Placed into Immediate Extraction Sockets: A Case Series. J. Periodontol. 2003, 74, 268–273. [Google Scholar] [CrossRef]
- Penarrocha, M.; Lamas, J.; Penarrocha, M.; Garcia, B. Immediate maxillary lateral incisor implants with nonocclusal loading provisional crowns. J. Prosthodont. 2008, 17, 55–59. [Google Scholar] [CrossRef]
- Lang, N.P.; Brägger, U.; Hämmerle, C.H.; Sutter, F. Immediate transmucosal implants using the principle of guided tissue regeneration. I. Rationale, clinical procedures and 30-month results. Clin. Oral Implant. Res. 1994, 5, 154–163. [Google Scholar] [CrossRef]
- Chen, S.T.; Buser, D. Clinical and Esthetic Outcomes of Implants Placed in Postextraction Sites. Int. J. Oral Maxillofac. Implant. 2009, 24, 186–217. [Google Scholar]
- Ryser, M.R.; Block, M.S.; Mercante, D.E. Correlation of papilla to crestal bone levels around single tooth implants in immediate or delayed crown protocols. J. Oral. Maxillofac. Surg. 2005, 63, 1184–1195. [Google Scholar] [CrossRef]
- Chen, S.T.; Darby, I.B.; Reynolds, E.C.; Clement, J.G. Immediate Implant Placement Postextraction without Flap Elevation. J. Periodontol. 2009, 80, 163–172. [Google Scholar] [CrossRef]
- Covani, U.; Bortolaia, C.; Barone, A.; Sbordone, L. Bucco-Lingual Crestal Bone Changes after Immediate and Delayed Implant Placement. J. Periodontol. 2004, 75, 1605–1612. [Google Scholar] [CrossRef] [PubMed]
- Rebele, S.F.; Zuhr, O.; Hurzeler, M.B. Pre-extractive interradicular implant bed preparation: Case presentations of a novel approach to immediate implant placement at multirooted molar sites. Int. J. Periodontics Restor. Dent. 2013, 33, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Rosenquist, B.; Grenthe, B. Immediate placement of implants into extraction sockets: Implant survival. Int. J. Oral Maxillofac. Implant. 1996, 11, 205–209. [Google Scholar] [CrossRef]
- Daif, E.T.P. Effect of a Multiporous Beta-Tricalicum Phosphate on Bone Density around Dental Implants Inserted into Fresh Extraction Sockets. J. Oral Implantol. 2013, 39, 339–344. [Google Scholar] [CrossRef]
- Sarnowski, A.A.; Paul, B.F. A retrospective analysis of 12 immediate-implant restorations in the maxillary premolar region. Compend. Contin. Educ. Dent. 2012, 33, e83–e87. [Google Scholar]
- Chu, S.J.; Salama, M.A.; Garber, D.A.; Salama, H.; Sarnachiaro, G.O.; Sarnachiaro, E.; Gotta, S.L.; Reynolds, M.A.; Saito, H.; Tarnow, D.P. Flapless postextraction socket implant placement, Part 2: The effects of bone grafting and provisional restoration on peri-implant soft tissue height and thickness—A retrospective study. Int. J. Periodontics Restor. Dent. 2015, 35, 803–809. [Google Scholar] [CrossRef]
- Crespi, R.; Capparè, P.; Gherlone, E.; Romanos, G.E. Immediate occlusal loading of implants placed in fresh sockets after tooth extraction. Int. J. Oral Maxillofac. Implant. 2007, 22, 955–962. [Google Scholar]
- Ross, S.B.; Pette, G.A. Immediate implant placement and provisionalization using a customized anatomic temporary abutment (CATA) to achieve gingival margin stability. Compend. Contin. Educ. Dent. 2013, 34, 344–350. [Google Scholar]
- Schwartz-Arad, D.; Chaushu, G. The ways and wherefores of immediate placement of implants into fresh extraction sites: A literature review. J. Periodontol. 1997, 68, 915–923. [Google Scholar] [CrossRef]
- Enríquez-Sacristán, C.; Barona-Dorado, C.; Calvo-Guirado, J.L.; Leco-Berrocal, I.; Martínez-González, J.M. Immediate post-extraction implants subject to immediate loading: A meta-analytic study. Med. Oral Patol. Oral Y Cirugía Bucal 2011, 16, e919–e924. [Google Scholar] [CrossRef]
- Schropp, L.; Kostopoulos, L.; Wenzel, A. Bone healing following immediate versus delayed placement of titanium implants into extraction sockets: A prospective clinical study. Int. J. Oral Maxillofac. Implant. 2003, 18, 189–199. [Google Scholar]
- Chu, S.J.; Saito, H.; Salama, M.A.; Garber, D.A.; Salama, H.; Sarnachiaro, G.O.; Reynolds, M.A.; Tarnow, D.P. Flapless Postextraction Socket Implant Placement, Part 3: The Effects of Bone Grafting and Provisional Restoration on Soft Tissue Color Change—A Retrospective Pilot Study. Int. J. Periodontics Restor. Dent. 2018, 38, 509–516. [Google Scholar] [CrossRef] [PubMed]
- Crespi, R.; Capparè, P.; Gherlone, E. Radiographic evaluation of marginal bone levels around platform-switched and non-platform-switched implants used in an immediate loading protocol. Int. J. Oral Maxillofac. Implant. 2009, 24, 920–926. [Google Scholar]
- Schiroli, G. Immediate tooth extraction, placement of a Tapered Screw-Vent implant, and provisionalization in the esthetic zone: A case report. Implant. Dent. 2003, 12, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Schwartz-Arad, D.; Chaushu, G. Immediate Implant Placement: A Procedure without Incisions. J. Periodontol. 1998, 69, 743–750. [Google Scholar] [CrossRef]
- Froum, S.J.; Cho, S.-C.; Francisco, H.; Park, Y.-S.; Elian, N.; Tarnow, D.P. Immediate implant placement and provisionalization--two case reports. Pract. Proced. Aesthetic Dent. PPAD 2007, 19, 621–628. [Google Scholar]
- Schropp, L.; Kostopoulos, L.; Wenzel, A.; Isidor, F. Clinical and radiographic performance of delayed-immediate single-tooth implant placement associated with peri-implant bone defects. A 2-year prospective, controlled, randomized follow-up report. J. Clin. Periodontol. 2005, 32, 480–487. [Google Scholar] [CrossRef]
- Covani, U.; Crespi, R.; Cornelini, R.; Barone, A. Immediate implants supporting single crown restoration: A 4-year prospective study. J. Periodontol. 2004, 75, 982–988. [Google Scholar] [CrossRef]
- Crespi, R.; Capparè, P.; Gherlone, E. A 4-Year Evaluation of the Peri-Implant Parameters of Immediately Loaded Implants Placed in Fresh Extraction Sockets. J. Periodontol. 2010, 81, 1629–1634. [Google Scholar] [CrossRef]
- Trimpou, G.; Weigl, P.; Krebs, M.; Parvini, P.; Nentwig, G.H. Rationale for esthetic tissue preservation of a fresh extraction socket by an implant treatment concept simulating a tooth replantation. Dent. Traumatol. 2010, 26, 105–111. [Google Scholar] [CrossRef]
- Simion, M.; Baldoni, M.; Zaffe, D. Jawbone enlargement using immediate implant placement associated with a split-crest technique and guided tissue regeneration. Int. J. Periodontics Restor. Dent. 1992, 12, 462–473. [Google Scholar]
- Fugazzotto, P.A.; Hains, F.O. Immediate implant placement in posterior areas, Part 2: The maxillary arch. Compend. Contin. Educ. Dent. 2013, 34, 518–528. [Google Scholar]
- Covani, U.; Cornelini, R.; Barone, A. Buccal Bone Augmentation around Immediate Implants with and without Flap Elevation: A Modified Approach. Int. J. Oral Maxillofac. Implant. 2008, 23, 841–846. [Google Scholar]
- Capelli, M.; Esposito, M.; Zuffetti, F.; Galli, F.; Del Fabbro, M.; Testori, T. A 5-year report from a multicentre randomised clinical trial: Immediate non-occlusal versus early loading of dental implants in partially edentulous patients. Eur. J. Oral Implantol. 2010, 3, 209–219. [Google Scholar]
- Turkyilmaz, I.; Suarez, J.C.; Company, A.M. Immediate implant placement and provisional crown fabrication after a minimally invasive extraction of a peg-shaped maxillary lateral incisor: A clinical report. J. Contemp. Dent. Pract. 2009, 10, E073–E080. [Google Scholar]
- Tritten, C.B.; Bragger, U.; Fourmousis, I.; Lang, N.P. Guided bone regeneration around an immediate transmucosal implant for single tooth replacement: A case report. Pract. Periodontics Aesthet Dent. 1995, 7, 29–38. [Google Scholar] [PubMed]
- Fugazzotto, P.A.; Hains, F.O. Immediate implant placement in posterior areas: The mandibular arch. Compend. Contin. Educ. Dent. 2012, 33, 494–496. [Google Scholar]
- Di Girolamo, M.; Arullani, C.; Calcaterra, R.; Manzi, J.; Arcuri, C.; Baggi, L. Preservation of extraction socket in immediate implant placement: A clinical study. Oral Implantol. 2016, 9, 222. [Google Scholar]
- Crespi, R.; Capparè, P.; Gherlone, E. Electrical mallet provides essential advantages in split-crest and immediate implant placement. Oral Maxillofac. Surg. 2014, 18, 59–64. [Google Scholar] [CrossRef]
- Werbitt, M.J.; Goldberg, P.V. The immediate implant: Bone preservation and bone regeneration. Int. J. Periodontics Restor. Dent. 1992, 12, 206–217. [Google Scholar]
- Gluckman, H.; Pontes, C.C.; Du Toit, J. Radial plane tooth position and bone wall dimensions in the anterior maxilla: A CBCT classification for immediate implant placement. J. Prosthet. Dent. 2018, 120, 50–56. [Google Scholar] [CrossRef] [PubMed]
- El-Chaar, E.S. Immediate Placement and Provisionalization of Implant-Supported, Single-Tooth Restorations: A Retrospective Study. Int. J. Periodontics Restor. Dent. 2011, 31, 408–419. [Google Scholar] [CrossRef] [PubMed]
- Crespi, R.; Capparè, P.; Gastaldi, G.; Gherlone, E.F. Buccal-Lingual Bone Remodeling in Immediately Loaded Fresh Socket Implants: A Cone Beam Computed Tomography Study. Int. J. Periodontics Restor. Dent. 2018, 38, 43–49. [Google Scholar] [CrossRef]
- Wilson, T.G., Jr. Guided tissue regeneration around dental implants in immediate and recent extraction sites: Initial observations. Int. J. Periodontics Restor. Dent. 1992, 12, 185–193. [Google Scholar]
- Greenstein, G.; Cavallaro, J. Immediate dental implant placement: Technique, part I. Dent Today 2014, 33, 98, 100–104. [Google Scholar] [PubMed]
- Evian, C.I.; Emling, R.; Rosenberg, E.S.; Waasdorp, J.A.; Halpern, W.; Shah, S.; Garcia, M. Retrospective analysis of implant survival and the influence of periodontal disease and immediate placement on long-term results. Int. J. Oral Maxillofac. Implant. 2004, 19, 393–398. [Google Scholar]
- Danza, M.; Guidi, R.; Carinci, F. Spiral Family Implants Inserted in Postextraction Bone Sites. Implant. Dent. 2009, 18, 270–278. [Google Scholar] [CrossRef]
- Wohrle, P.S. Single-tooth replacement in the aesthetic zone with immediate provisionalization: Fourteen consecutive case reports. Pract. Periodontics Aesthet. Dent. 1998, 10, 1107–1114. [Google Scholar]
- Holst, S.; Hegenbarth, E.A.; Schlegel, K.A.; Holst, A.I. Restoration of a nonrestorable central incisor using forced orthodontic eruption, immediate implant placement, and an all-ceramic restoration: A clinical report. J. Prosthet. Dent. 2007, 98, 251–255. [Google Scholar] [CrossRef]
- Felice, P.; Soardi, E.; Piattelli, M.; Pistilli, R.; Jacotti, M.; Esposito, M. Immediate non-occlusal loading of immediate post-extractive versus delayed placement of single implants in preserved sockets of the anterior maxilla: 4-month post-loading results from a pragmatic multicentre randomised controlled trial. Eur. J. Oral Implantol. 2011, 4, 329–344. [Google Scholar]
- Davarpanah, M.; Caraman, M.; Szmukler-Moncler, S.; Jakubowicz-Kohen, B.; Alcolforado, G. Preliminary Data of a Prospective Clinical Study on the Osseotite NT Implant: 18-month Follow-up. Int. J. Oral Maxillofac. Implant. 2005, 20, 448–454. [Google Scholar]
- Kan, J.Y.; Rungcharassaeng, K. Immediate placement and provisionalization of maxillary anterior single implants: A surgical and prosthodontic rationale. Pract. Periodontics Aesthet. Dent. 2000, 12, 817–824. [Google Scholar] [PubMed]
- Felice, P.; Zucchelli, G.; Cannizzaro, G.; Barausse, C.; Diazzi, M.; Trullenque-Eriksson, A.; Esposito, M. Immediate, immediate-delayed (6 weeks) and delayed (4 months) post-extractive single implants: 4-month post-loading data from a randomised controlled trial. Eur. J. Oral Implantol. 2016, 9, 233–247. [Google Scholar]
- Degidi, M.; Piattelli, A.; Carinci, F. Immediate Loaded Dental Implants: Comparison between Fixtures Inserted in Postextractive and Healed Bone Sites. J. Craniofacial Surg. 2007, 18, 965–971. [Google Scholar] [CrossRef] [PubMed]
- Kan, J.Y.; Rungcharassaeng, K.; Kois, J.C. Removable ovate pontic for peri-implant architecture preservation during immediate implant placement. Pract. Proced. Aesthet Dent. 2001, 13, 711–715. [Google Scholar] [PubMed]
- Fernandez Diaz, J.O.; Naval Gias, L. Rehabilitation of edentulous posterior atrophic mandible: Inferior alveolar nerve lateralization by piezotome and immediate implant placement. Int. J. Oral Maxillofac. Surg. 2013, 42, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Piattelli, A. Comparative Analysis Study of 702 Dental Implants Subjected to Immediate Functional Loading and Immediate Nonfunctional Loading to Traditional Healing Periods with a Follow-up of up to 24 Months. Int. J. Oral Maxillofac. Implant. 2005, 20, 99–107. [Google Scholar] [CrossRef]
- Kan, J.Y.; Rungcharassaeng, K.; Lozada, J.L. Bilaminar subepithelial connective tissue grafts for immediate implant placement and provisionalization in the esthetic zone. J. Calif. Dent. Assoc. 2005, 33, 865–871. [Google Scholar]
- Ferrus, J.; Cecchinato, D.; Pjetursson, E.B.; Lang, N.P.; Sanz, M.; Lindhe, J. Factors influencing ridge alterations following immediate implant placement into extraction sockets. Clin. Oral Implant. Res. 2010, 21, 22–29. [Google Scholar] [CrossRef]
- Del Fabbro, M.B.P.; Boggian, C.D.D.S.; Taschieri, S.M.D.D.D.S. Immediate Implant Placement into Fresh Extraction Sites with Chronic Periapical Pathologic Features Combined with Plasma Rich in Growth Factors: Preliminary Results of Single-Cohort Study. J. Oral Maxillofac. Surg. 2009, 67, 2476–2484. [Google Scholar] [CrossRef]
- Kan, J.Y.K.; Rungcharassaeng, K.; Deflorian, M.; Weinstein, T.; Wang, H.L.; Testori, T. Immediate implant placement and provisionalization of maxillary anterior single implants. Periodontol 2000 2018, 77, 197–212. [Google Scholar] [CrossRef]
- Granić, M.; Katanec, D.; Vučićević Boras, V.; Sušić, M.; Jurič, I.B.; Gabrić, D. Implant stability comparison of immediate and delayed maxillary implant placement by use of resonance frequency analysis—A clinical study. Acta Clin. Croat. 2015, 54, 3–8. [Google Scholar] [PubMed]
- Deng, F.; Zhang, H.; Zhang, H.; Shao, H.; He, Q.; Zhang, P. A comparison of clinical outcomes for implants placed in fresh extraction sockets versus healed sites in periodontally compromised patients: A 1-year follow-up report. Int. J. Oral Maxillofac. Implant. 2010, 25, 1036–1040. [Google Scholar]
- Kher, U.; Tunkiwala, A.; Umrigar, Z. Management of Fenestration Defects During Flapless Immediate Implant Placement in the Esthetic Zone. Int. J. Periodontics. Restor. Dent. 2015, 35, e90–e96. [Google Scholar] [CrossRef] [PubMed]
- Groenendijk, E.; Staas, T.A.; Graauwmans, F.E.J.; Bronkhorst, E.; Verhamme, L.; Maal, T.; Meijer, G.J. Immediate implant placement: The fate of the buccal crest. A retrospective cone beam computed tomography study. Int. J. Oral Maxillofac. Surg. 2017, 46, 1600–1606. [Google Scholar] [CrossRef] [PubMed]
- Koh, R.U.; Rudek, I.; Wang, H.L. Immediate implant placement: Positives and negatives. Implant. Dent. 2010, 19, 98–108. [Google Scholar] [CrossRef]
- Grunder, U. Crestal ridge width changes when placing implants at the time of tooth extraction with and without soft tissue augmentation after a healing period of 6 months: Report of 24 consecutive cases. Int. J. Periodontics Restor. Dent. 2011, 31, 9–17. [Google Scholar]
- Erakat, M.S.; Chuang, S.-K.; Yoo, R.H.; Weed, M.; Dodson, T.B. Immediate loading of splinted locking-taper implants: 1-year survival estimates and risk factors for failure. Int. J. Oral Maxillofac. Implant. 2008, 23, 105–110. [Google Scholar]
- Hossain, M.A.; Uddoula, M.S.; Mahmuduzzaman, M.; Rahman, M.A. Clinical Evaluation of Bucco-lingual Crestal Bone Remodeling in Mandibular Posterior Implants placed immediately and Delayed into Extraction Sites. Mymensingh Med. J. 2017, 26, 87–91. [Google Scholar]
- Finne, K.; Rompen, E.; Toljanic, J. Prospective multicenter study of marginal bone level and soft tissue health of a one-piece implant after two years. J Prosthet Dent 2007, 97 (Suppl. S6), S79–S85. [Google Scholar] [CrossRef]
- Lemongello, G.J. Customized provisional abutment and provisional restoration for an immediately-placed implant. Pract. Proced. Aesthet. Dent. 2007, 19, 419–424. [Google Scholar] [PubMed]
- Huynh-Ba, G.; Pjetursson, B.E.; Sanz, M.; Cecchinato, D.; Ferrus, J.; Lindhe, J.; Lang, N.P. Analysis of the socket bone wall dimensions in the upper maxilla in relation to immediate implant placement. Clin. Oral Implant. Res. 2010, 21, 37–42. [Google Scholar] [CrossRef]
- Fugazzotto, P.A. Implant placement in maxillary first premolar fresh extraction sockets: Description of technique and report of preliminary results. J. Periodontol. 2002, 73, 669–674. [Google Scholar] [CrossRef]
- Levine, R.A.; Ganeles, J.; Kan, J.; Fava, P.L. 10 Keys for Successful Esthetic-Zone Single Implants: Importance of Biotype Conversion for Lasting Success. Compend. Contin. Educ. Dent. 2018, 39, 522–529. [Google Scholar]
- Jofre, J.; Valenzuela, D.; Quintana, P.; Asenjo-Lobos, C. Protocol for immediate implant replacement of infected teeth. Implant. Dent. 2012, 21, 287–294. [Google Scholar] [CrossRef]
- Fugazzotto, P.A. Implant placement at the time of maxillary molar extraction: Treatment protocols and report of results. J. Periodontol. 2008, 79, 216–223. [Google Scholar] [CrossRef]
- Meltzer, A.M. Primary stability and initial bone-to-implant contact: The effects on immediate placement and restoration of dental implants. J. Implant. Reconstr. Dent. 2009, 1, 35–41. [Google Scholar]
- Kamperos, G.; Zambara, I.; Petsinis, V.; Zambaras, D. The Impact of Buccal Bone Defects and Immediate Placement on the Esthetic Outcome of Maxillary Anterior Single-Tooth Implants. J. Oral. Implantol. 2016, 42, 337–341. [Google Scholar] [CrossRef]
- Gokcen-Rohlig, B.; Meric, U.; Keskin, H. Clinical and radiographic outcomes of implants immediately placed in fresh extraction sockets. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, e1–e7. [Google Scholar] [CrossRef]
- Palti, A. Immediate placement and loading of implants in extraction sites: Procedures in the aesthetic zone. Dent. Implantol. Update 2004, 15, 41–47. [Google Scholar] [PubMed]
- Kolinski, M.L.; Cherry, J.E.; McAllister, B.S.; Parrish, K.D.; Pumphrey, D.W.; Schroering, R.L. Evaluation of a variable-thread tapered implant in extraction sites with immediate temporization: A 3-year multicenter clinical study. J. Periodontol. 2014, 85, 386–394. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Roman, G.; Kruppenbacher, M.; Weber, H.; Schulte, W. Immediate postextraction implant placement with root-analog stepped implants: Surgical procedure and statistical outcome after 6 years. Int. J. Oral Maxillofac. Implant. 2001, 16, 503–513. [Google Scholar]
- Ramsey, C.D. Single-tooth replacement of a maxillary central incisor via immediate implant placement. Pract. Proced. Aesthet. Dent. 2007, 19, 355–357. [Google Scholar] [PubMed]
- Lang, N.P.; Tonetti, M.S.; Suvan, J.E.; Pierre Bernard, J.; Botticelli, D.; Fourmousis, I.; Hallund, M.; Jung, R.; Laurell, L.; Salvi, G.E.; et al. Immediate implant placement with transmucosal healing in areas of aesthetic priority. A multicentre randomized-controlled clinical trial I. Surgical outcomes. Clin. Oral Implant. Res. 2007, 18, 188–196. [Google Scholar] [CrossRef]
- Grunder, U.; Polizzi, G.; Goene, R.; Hatano, N.; Henry, P.; Jackson, W.J.; Kawamura, K.; Kohler, S.; Renouard, F.; Rosenberg, R.; et al. A 3-year prospective multicenter follow-up report on the immediate and delayed-immediate placement of implants. Int. J. Oral Maxillofac. Implant. 1999, 14, 210–216. [Google Scholar]
- Saadoun, A.P. Immediate implant placement and temporization in extraction and healing sites. Compend. Contin. Educ. Dent. 2002, 23, 309–312, 314. [Google Scholar]
- Lee, E.A.; Gonzalez-Martin, O.; Fiorellini, J. Lingualized flapless implant placement into fresh extraction sockets preserves buccal alveolar bone: A cone beam computed tomography study. Int. J. Periodontics Restor. Dent. 2014, 34, 61–68. [Google Scholar] [CrossRef]
- Han, C.H.; Mangano, F.; Mortellaro, C.; Park, K.B. Immediate Loading of Tapered Implants Placed in Postextraction Sockets and Healed Sites. J. Craniofac. Surg. 2016, 27, 1220–1227. [Google Scholar] [CrossRef]
- Waki, T.; Kan, J.Y. Immediate placement and provisionalization of maxillary anterior single implant with guided bone regeneration, connective tissue graft, and coronally positioned flap procedures. Int. J. Esthet. Dent. 2016, 11, 174–185. [Google Scholar]
- Levin, B.P.; Chu, S.J. Changes in Peri-implant Soft Tissue Thickness with Bone Grafting and Dermis Allograft: A Case Series of 15 Consecutive Patients. Int. J. Periodontics Restor. Dent. 2018, 38, 719–727. [Google Scholar] [CrossRef]
- Hayacibara, R.M.; Gonçalves, C.S.; Garcez-Filho, J.; Magro-Filho, O.; Esper, H.; Hayacibara, M.F. The success rate of immediate implant placement of mandibular molars: A clinical and radiographic retrospective evaluation between 2 and 8 years. Clin. Oral Implant. Res. 2013, 24, 806–811. [Google Scholar] [CrossRef] [PubMed]
- Weigl, P.; Strangio, A. The impact of immediately placed and restored single-tooth implants on hard and soft tissues in the anterior maxilla. Eur. J. Oral. Implantol. 2016, 9 (Suppl. S1), S89–S106. [Google Scholar]
- Lops, D.; Chiapasco, M.; Rossi, A.; Bressan, E.; Romeo, E. Incidence of inter-proximal papilla between a tooth and an adjacent immediate implant placed into a fresh extraction socket: 1-year prospective study. Clin. Oral Implant. Res. 2008, 19, 1135–1140. [Google Scholar] [CrossRef] [PubMed]
- Heinemann, F.; Biffar, R.; Schwahn, C.; Mundt, T. Bone level changes in dental implants with platform-switched design after immediate and delayed placement in the maxilla. Int. J. Periodontics Restor. Dent. 2013, 33, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Yan, Q.; Xiao, L.Q.; Su, M.Y.; Mei, Y.; Shi, B. Soft and Hard Tissue Changes Following Immediate Placement or Immediate Restoration of Single-Tooth Implants in the Esthetic Zone: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Implant. 2016, 31, 1327–1340. [Google Scholar] [CrossRef]
- Malo, P.; Rangert, B.; Dvarsater, L. Immediate function of Branemark implants in the esthetic zone: A retrospective clinical study with 6 months to 4 years of follow-up. Clin. Implant. Dent. Relat. Res. 2000, 2, 138–146. [Google Scholar] [CrossRef]
- Heinemann, F.; Bourauel, C.; Hasan, I.; Gedrange, T. Influence of the implant cervical topography on the crestal bone resorption and immediate implant survival. J. Physiol. Pharmacol. 2009, 60 (Suppl. S8), 99–105. [Google Scholar]
- Matarasso, S.; Salvi, G.E.; Iorio Siciliano, V.; Cafiero, C.; Blasi, A.; Lang, N.P. Dimensional ridge alterations following immediate implant placement in molar extraction sites: A six-month prospective cohort study with surgical re-entry. Clin. Oral Implant. Res. 2009, 20, 1092–1098. [Google Scholar] [CrossRef]
- Horwitz, J.; Zuabi, O.; Peled, M.; Machtei, E.E. Immediate and delayed restoration of dental implants in periodontally susceptible patients: 1-year results. Int. J. Oral Maxillofac. Implant. 2007, 22, 423–429. [Google Scholar]
- Miyamoto, Y.; Obama, T. Dental cone beam computed tomography analyses of postoperative labial bone thickness in maxillary anterior implants: Comparing immediate and delayed implant placement. Int. J. Periodontics Restor. Dent. 2011, 31, 215–225. [Google Scholar]
- Jo, H.Y.; Hobo, P.K.; Hobo, S. Freestanding and multiunit immediate loading of the expandable implant: An up-to-40-month prospective survival study. J. Prosthet. Dent. 2001, 85, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Nemcovsky, C.E.; Artzi, Z.; Moses, O. Rotated split palatal flap for soft tissue primary coverage over extraction sites with immediate implant placement. Description of the surgical procedure and clinical results. J. Periodontol. 1999, 70, 926–934. [Google Scholar] [CrossRef]
- Khorsand, A.; Rasouli-Ghahroudi, A.A.; Naddafpour, N.; Shayesteh, Y.S.; Khojasteh, A. Effect of Microthread Design on Marginal Bone Level around Dental Implants Placed in Fresh Extraction Sockets. Implant. Dent. 2016, 25, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Nemcovsky, C.E.; Moses, O.; Artzi, Z.; Gelernter, I. Clinical coverage of dehiscence defects in immediate implant procedures: Three surgical modalities to achieve primary soft tissue closure. Int. J. Oral Maxillofac. Implant. 2000, 15, 843–852. [Google Scholar]
- Laviv, A.; Levin, L.; Usiel, Y.; Schwartz-Arad, D. Survival of immediately provisionalized dental implants: A case-control study with up to 5 years follow-up. Clin. Implant. Dent. Relat. Res. 2010, 12, e23–e27. [Google Scholar] [CrossRef]
- Nemcovsky, C.E.; Artzi, Z. Comparative study of buccal dehiscence defects in immediate, delayed, and late maxillary implant placement with collagen membranes: Clinical healing between placement and second-stage surgery. J. Periodontol. 2002, 73, 754–761. [Google Scholar] [CrossRef]
- Malchiodi, L.; Corrocher, G.; Cucchi, A.; Ghensi, P.; Bissolotti, G.; Nocini, P.F. Long-term results of immediately loaded fast bone regeneration-coated implants placed in fresh extraction sites in the upper jaw. J. Oral Implantol. 2010, 36, 251–261. [Google Scholar] [CrossRef]
- Parel, S.M.; Schow, S.R. Early clinical experience with a new one-piece implant system in single tooth sites. J. Oral Maxillofac. Surg. 2005, 63, 2–10. [Google Scholar] [CrossRef]
- Malchiodi, L.; Ghensi, P.; Cucchi, A.; Corrocher, G. A comparative retrospective study of immediately loaded implants in postextraction sites versus healed sites: Results after 6 to 7 years in the maxilla. Int. J. Oral Maxillofac. Implant. 2011, 26, 373–384. [Google Scholar]
- Peron, C.; Romanos, G. Immediate Placement and Occlusal Loading of Single-Tooth Restorations on Partially Threaded, Titanium-Tantalum Combined Dental Implants: 1-Year Results. Int. J. Periodontics Restor. Dent. 2016, 36, 393–399. [Google Scholar] [CrossRef]
- Malo, P.; Friberg, B.; Polizzi, G.; Gualini, F.; Vighagen, T.; Rangert, B. Immediate and early function of Branemark System implants placed in the esthetic zone: A 1-year prospective clinical multicenter study. Clin Implant. Dent. Relat Res 2003, 5 (Suppl. S1), 37–46. [Google Scholar] [CrossRef]
- Pirker, W.; Kocher, A. Immediate, non-submerged, root-analogue zirconia implants placed into single-rooted extraction sockets: 2-year follow-up of a clinical study. Int. J. Oral Maxillofac. Surg. 2009, 38, 1127–1132. [Google Scholar] [CrossRef]
- Mankoo, T. Maintenance of interdental papillae in the esthetic zone using multiple immediate adjacent implants to restore failing teeth--a report of ten cases at 2 to 7 years follow-up. Eur. J. Esthet. Dent. 2008, 3, 304–322. [Google Scholar]
- Redemagni, M.; Cremonesi, S.; Garlini, G.; Maiorana, C. Soft tissue stability with immediate implants and concave abutments. Eur. J. Esthet. Dent. 2009, 4, 328–337. [Google Scholar] [PubMed]
- McAllister, B.S.; Cherry, J.E.; Kolinski, M.L.; Parrish, K.D.; Pumphrey, D.W.; Schroering, R.L. Two-year evaluation of a variable-thread tapered implant in extraction sites with immediate temporization: A multicenter clinical trial. Int. J. Oral Maxillofac. Implant. 2012, 27, 611–618. [Google Scholar]
- Rieder, D.; Eggert, J.; Krafft, T.; Weber, H.P.; Wichmann, M.G.; Heckmann, S.M. Impact of placement and restoration timing on single-implant esthetic outcome—A randomized clinical trial. Clin. Oral Implant. Res. 2016, 27, e80–e86. [Google Scholar] [CrossRef]
- Meltzer, A.M. Immediate implant placement and restoration in infected sites. Int. J. Periodontics Restor. Dent. 2012, 32, e169–e173. [Google Scholar]
- Rungcharassaeng, K.; Kan, J.Y.; Yoshino, S.; Morimoto, T.; Zimmerman, G. Immediate implant placement and provisionalization with and without a connective tissue graft: An analysis of facial gingival tissue thickness. Int. J. Periodontics Restor. Dent. 2012, 32, 657–663. [Google Scholar]
- Mura, P. Immediate loading of tapered implants placed in postextraction sockets: Retrospective analysis of the 5-year clinical outcome. Clin. Implant. Dent. Relat. Res. 2012, 14, 565–574. [Google Scholar] [CrossRef]
- Noelken, R.; Neffe, B.A.; Kunkel, M.; Wagner, W. Maintenance of marginal bone support and soft tissue esthetics at immediately provisionalized OsseoSpeed implants placed into extraction sites: 2-year results. Clin. Oral Implant. Res. 2014, 25, 214–220. [Google Scholar] [CrossRef]
- Saito, H.; Chu, S.J.; Reynolds, M.A.; Tarnow, D.P. Provisional Restorations Used in Immediate Implant Placement Provide a Platform to Promote Peri-implant Soft Tissue Healing: A Pilot Study. Int. J. Periodontics Restor. Dent. 2016, 36, 47–52. [Google Scholar] [CrossRef]
- Noelken, R.; Kunkel, M.; Jung, B.A.; Wagner, W. Immediate nonfunctional loading of NobelPerfect implants in the anterior dental arch in private practice--5-year data. Clin. Implant. Dent. Relat. Res. 2014, 16, 21–31. [Google Scholar] [CrossRef]
- Sanz, M.; Cecchinato, D.; Ferrus, J.; Pjetursson, E.B.; Lang, N.P.; Lindhe, J. A prospective, randomized-controlled clinical trial to evaluate bone preservation using implants with different geometry placed into extraction sockets in the maxilla. Clin. Oral Implant. Res. 2010, 21, 13–21. [Google Scholar] [CrossRef]
- Noelken, R.; Oberhansl, F.; Kunkel, M.; Wagner, W. Immediately provisionalized OsseoSpeed(™) Profile implants inserted into extraction sockets: 3-year results. Clin. Oral Implant. Res. 2016, 27, 744–749. [Google Scholar] [CrossRef] [PubMed]
- Sarnachiaro, G.O.; Chu, S.J.; Sarnachiaro, E.; Gotta, S.L.; Tarnow, D.P. Immediate Implant Placement into Extraction Sockets with Labial Plate Dehiscence Defects: A Clinical Case Series. Clin. Implant. Dent. Relat. Res. 2016, 18, 821–829. [Google Scholar] [CrossRef] [PubMed]
- Noelken, R.; Moergel, M.; Kunkel, M.; Wagner, W. Immediate and flapless implant insertion and provisionalization using autogenous bone grafts in the esthetic zone: 5-year results. Clin. Oral Implant. Res. 2018, 29, 320–327. [Google Scholar] [CrossRef]
- Scarano, A. Traditional Postextractive Implant Site Preparation Compared with Pre-extractive Interradicular Implant Bed Preparation in the Mandibular Molar Region, Using an Ultrasonic Device: A Randomized Pilot Study. Int. J. Oral Maxillofac. Implant. 2017, 32, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Ormianer, Z.; Palti, A. Retrospective clinical evaluation of tapered screw-vent implants: Results after up to eight years of clinical function. J. Oral Implantol. 2008, 34, 150–160. [Google Scholar] [CrossRef] [PubMed]
- Somanathan, R.V.; Simůnek, A.; Bukac, J.; Brázda, T.; Kopecká, D. Soft tissue esthetics in Implant. Dent.istry. Acta Med. (Hradec Kral.) 2007, 50, 183–186. [Google Scholar] [CrossRef]
- Ormianer, Z.; Piek, D.; Livne, S.; Lavi, D.; Zafrir, G.; Palti, A.; Harel, N. Retrospective clinical evaluation of tapered implants: 10-year follow-up of delayed and immediate placement of maxillary implants. Implant. Dent. 2012, 21, 350–356. [Google Scholar] [CrossRef]
- Tomasi, C.; Sanz, M.; Cecchinato, D.; Pjetursson, B.; Ferrus, J.; Lang, N.P.; Lindhe, J. Bone dimensional variations at implants placed in fresh extraction sockets: A multilevel multivariate analysis. Clin. Oral Implant. Res. 2010, 21, 30–36. [Google Scholar] [CrossRef]
- Paolantonio, M.; Dolci, M.; Scarano, A.; d’Archivio, D.; di Placido, G.; Tumini, V.; Piattelli, A. Immediate implantation in fresh extraction sockets. A controlled clinical and histological study in man. J. Periodontol. 2001, 72, 1560–1571. [Google Scholar] [CrossRef] [PubMed]
- van Kesteren, C.J.; Schoolfield, J.; West, J.; Oates, T. A prospective randomized clinical study of changes in soft tissue position following immediate and delayed implant placement. Int. J. Oral Maxillofac. Implant. 2010, 25, 562–570. [Google Scholar]
- Penarrocha-Diago, M.; Demarchi, C.L.; Maestre-Ferrin, L.; Carrillo, C.; Penarrocha-Oltra, D.; Penarrocha-Diago, M.A. A retrospective comparison of 1,022 implants: Immediate versus nonimmediate. Int. J. Oral Maxillofac. Implant. 2012, 27, 421–427. [Google Scholar]
- Vandeweghe, S.; Nicolopoulos, C.; Thevissen, E.; Jimbo, R.; Wennerberg, A.; De Bruyn, H. Immediate loading of screw-retained all-ceramic crowns in immediate versus delayed single implant placement. Int. J. Prosthodont. 2013, 26, 458–464. [Google Scholar] [CrossRef]
- Penarrocha-Oltra, D.; Demarchi, C.L.; Maestre-Ferrin, L.; Penarrocha-Diago, M.; Penarrocha-Diago, M. Comparison of immediate and delayed implants in the maxillary molar region: A retrospective study of 123 implants. Int. J. Oral Maxillofac. Implant. 2012, 27, 604–610. [Google Scholar]
- Vidigal, G.M., Jr.; Groisman, M.; Clavijo, V.G.; Barros Paulinelli Santos, I.G.; Fischer, R.G. Evaluation of Pink and White Esthetic Scores for Immediately Placed and Provisionally Restored Implants in the Anterior Maxilla. Int. J. Oral Maxillofac. Implant. 2017, 32, 625–632. [Google Scholar] [CrossRef]
- Perry, J.; Lenchewski, E. Clinical performance and 5-year retrospective evaluation of Frialit-2 implants. Int. J. Oral Maxillofac. Implant. 2004, 19, 887–891. [Google Scholar]
- West, J.D.; Oates, T.W. Identification of stability changes for immediately placed dental implants. Int. J. Oral Maxillofac. Implant. 2007, 22, 623–630. [Google Scholar]
- Polizzi, G.; Grunder, U.; Goené, R.; Hatano, N.; Henry, P.; Jackson, W.J.; Kawamura, K.; Renouard, F.; Rosenberg, R.; Triplett, G.; et al. Immediate and delayed implant placement into extraction sockets: A 5-year report. Clin. Implant. Dent. Relat. Res. 2000, 2, 93–99. [Google Scholar] [CrossRef]
- Younis, L.; Taher, A.; Abu-Hassan, M.I.; Tin, O. Evaluation of bone healing following immediate and delayed dental implant placement. J. Contemp. Dent. Pract. 2009, 10, 35–42. [Google Scholar] [CrossRef]
- Siebers, D.; Gehrke, P.; Schliephake, H. Delayed function of dental implants: A 1- to 7-year follow-up study of 222 implants. Int. J. Oral Maxillofac. Implant. 2010, 25, 1195–1202. [Google Scholar]
- Siebert, T.; Jurkovic, R.; Statelova, D.; Strecha, J. Immediate Implant Placement in a Patient with Osteoporosis Undergoing Bisphosphonate Therapy: 1-Year Preliminary Prospective Study. J. Oral Implantol. 2015, 41, 360–365. [Google Scholar] [CrossRef]
- Simsek, B.; Simsek, S. Evaluation of success rates of immediate and delayed implants after tooth extraction. Chin. Med. J. 2003, 116, 1216–1219. [Google Scholar] [PubMed]
- Stefanski, S.; Svensson, B.; Thor, A. Implant survival following sinus membrane elevation without grafting and immediate implant installation with a one-stage technique: An up-to-40-month evaluation. Clin. Oral Implant. Res. 2017, 28, 1354–1359. [Google Scholar] [CrossRef] [PubMed]
- Tsai, E.S.; Crohin, C.C.; Weber, H.P. A five-year evaluation of implants placed in extraction sockets. J. West. Soc. Periodontol. Abstr. 2000, 48, 37–47. [Google Scholar]
- van Steenberghe, D.; Callens, A.; Geers, L.; Jacobs, R. The clinical use of deproteinized bovine bone mineral on bone regeneration in conjunction with immediate implant installation. Clin. Oral Implant. Res. 2000, 11, 210–216. [Google Scholar] [CrossRef]
- Vanden Bogaerde, L.; Rangert, B.; Wendelhag, I. Immediate/early function of Branemark System TiUnite implants in fresh extraction sockets in maxillae and posterior mandibles: An 18-month prospective clinical study. Clin Implant. Dent. Relat Res 2005, 7 (Suppl. S1), S121–S130. [Google Scholar] [CrossRef]
- Vidal, R.; Greenwell, H.; Hill, M.; Papageorgakopoulos, G.; Scheetz, J.P. Success rate of immediate implants placed and restored by novice operators. Implant. Dent. 2010, 19, 81–90. [Google Scholar] [CrossRef]
- Villa, R.; Rangert, B. Immediate and early function of implants placed in extraction sockets of maxillary infected teeth: A pilot study. J. Prosthet. Dent. 2007, 97 (Suppl. S6), S96–S108. [Google Scholar] [CrossRef]
- Wagenberg, B.; Froum, S.J. A retrospective study of 1925 consecutively placed immediate implants from 1988 to 2004. Int. J. Oral Maxillofac. Implant. 2006, 21, 71–80. [Google Scholar]
- Wagenberg, B.D.; Froum, S.J.; Eckert, S.E. Long-term bone stability assessment around 1,187 immediately placed implants with 1- to 22-year follow-up. Int. J. Oral Maxillofac. Implant. 2013, 28, 605–612. [Google Scholar] [CrossRef] [PubMed]
- Wagenberg, B.; Froum, S.J. Long-Term Bone Stability around 312 Rough-Surfaced Immediately Placed Implants with 2-12-Year Follow-Up. Clin. Implant. Dent. Relat. Res. 2015, 17, 658–666. [Google Scholar] [CrossRef]
- Wilson, T.G., Jr.; Carnio, J.; Schenk, R.; Cochran, D. Immediate implants covered with connective tissue membranes: Human biopsies. J. Periodontol. 2003, 74, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Wychowanski, P.; Wolinski, J.; Kacprzak, M.; Tomkiewicz, W.; Bartlomiej, I.; Szubinska-Lelonkiewicz, D.; Wojtowicz, A.; Nevins, M. Immediate Palatal Molar Implants: A Simple, Safe, Minimally Invasive Technique. Int. J. Periodontics Restor. Dent. 2017, 37, e297–e301. [Google Scholar] [CrossRef]
- Aguilar-Salvatierra, A.; Calvo-Guirado, J.L.; González-Jaranay, M.; Moreu, G.; Delgado-Ruiz, R.A.; Gómez-Moreno, G. Peri-implant evaluation of immediately loaded implants placed in esthetic zone in patients with diabetes mellitus type 2: A two-year study. Clin. Oral Implant. Res. 2016, 27, 156–161. [Google Scholar] [CrossRef]
- Amato, F.; Polara, G. Immediate Implant Placement in Single-Tooth Molar Extraction Sockets: A 1-to 6-Year Retrospective Clinical Study. Int. J. Periodontics Restor. Dent. 2018, 38, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Arora, H.; Ivanovski, S. Correlation between pre-operative buccal bone thickness and soft tissue changes around immediately placed and restored implants in the maxillary anterior region: A 2-year prospective study. Clin. Oral Implant. Res. 2017, 28, 1188–1194. [Google Scholar] [CrossRef]
- Arora, H.; Ivanovski, S. Clinical and aesthetic outcomes of immediately placed single-tooth implants with immediate vs. delayed restoration in the anterior maxilla: A retrospective cohort study. Clin. Oral Implant. Res. 2018, 29, 346–352. [Google Scholar] [CrossRef]
- Arora, H.; Ivanovski, S. Evaluation of the influence of implant placement timing on the esthetic outcomes of single tooth implant treatment in the anterior maxilla: A retrospective study. J. Esthet. Restor. Dent. 2018, 30, 338–345. [Google Scholar] [CrossRef]
- Arora, H.; Ivanovski, S. Immediate and early implant placement in single-tooth gaps in the anterior maxilla: A prospective study on ridge dimensional, clinical, and aesthetic changes. Clin. Oral Implant. Res. 2018, 29, 1143–1154. [Google Scholar] [CrossRef] [PubMed]
- Arora, H.; Khzam, N.; Roberts, D.; Bruce, W.L.; Ivanovski, S. Immediate implant placement and restoration in the anterior maxilla: Tissue dimensional changes after 2–5 year follow up. Clin. Implant. Dent. Istry Relat. Res. 2017, 19, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Atalay, B.; Öncü, B.; Emes, Y.; Bultan, Ö.; Aybar, B.; Yalçin, S. Immediate implant placement without bone grafting: A retrospective study of 110 cases with 5 years of follow-up. Implant. Dent. 2013, 22, 360–365. [Google Scholar] [CrossRef] [PubMed]
- Atieh, M.A.; Alsabeeha, N.H.; Duncan, W.J.; de Silva, R.K.; Cullinan, M.P.; Schwass, D.; Payne, A.G. Immediate single implant restorations in mandibular molar extraction sockets: A controlled clinical trial. Clin. Oral Implant. Res. 2013, 24, 484–496. [Google Scholar] [CrossRef]
- Avvanzo, P.; Ciavarella, D.; Avvanzo, A.; Giannone, N.; Carella, M.; Lo Muzio, L. Immediate placement and temporization of implants: Three-to five-year retrospective results. J. Oral Implantol. 2009, 35, 136–142. [Google Scholar] [CrossRef]
- Balaji, P.; Balaji, S.; Ugandhar, P. Immediate implant in single rooted teeth-Study on primary stability and bone formation. Indian J. Dent. Res. 2015, 26, 421. [Google Scholar] [CrossRef]
- Barone, A.; Rispoli, L.; Vozza, I.; Quaranta, A.; Covani, U. Immediate restoration of single implants placed immediately after tooth extraction. J. Periodontol. 2006, 77, 1914–1920. [Google Scholar] [CrossRef] [PubMed]
- Barone, A.; Toti, P.; Quaranta, A.; Derchi, G.; Covani, U. The clinical outcomes of immediate versus delayed restoration procedures on immediate implants: A comparative cohort study for single-tooth replacement. Clin. Implant. Dent. Relat. Res. 2015, 17, 1114–1126. [Google Scholar] [CrossRef]
- Becker, W.; Dahlin, C.; Lekholm, U.; Bergstrom, C.; van Steenberghe, D.; Higuchi, K.; Becker, B.E. Five-year evaluation of implants placed at extraction and with dehiscences and fenestration defects augmented with ePTFE membranes: Results from a prospective multicenter study. Clin. Implant. Dent. Relat. Res. 1999, 1, 27–32. [Google Scholar] [CrossRef]
- Becker, W.; Sennerby, L.; Bedrossian, E.; Becker, B.E.; Lucchini, J.P. Implant stability measurements for implants placed at the time of extraction: A cohort, prospective clinical trial. J. Periodontol. 2005, 76, 391–397. [Google Scholar] [CrossRef]
- Benic, G.I.; Mokti, M.; Chen, C.J.; Weber, H.P.; Hämmerle, C.H.; Gallucci, G.O. Dimensions of buccal bone and mucosa at immediately placed implants after 7 years: A clinical and cone beam computed tomography study. Clin. Oral Implant. Res. 2012, 23, 560–566. [Google Scholar] [CrossRef]
- Berberi, A.N.; Noujeim, Z.N.; Kanj, W.H.; Mearawi, R.J.; Salameh, Z.A. Immediate placement and loading of maxillary single-tooth implants: A 3-year prospective study of marginal bone level. J. Contemp. Dent. Pract. 2014, 15, 202. [Google Scholar] [CrossRef]
- Bianchi, A.E.; Sanfilippo, F. Single-tooth replacement by immediate implant and connective tissue graft: A 1–9-year clinical evaluation. Clin. Oral Implant. Res. 2004, 15, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Blus, C.; Szmukler-Moncler, S. Atraumatic tooth extraction and immediate implant placement with Piezosurgery: Evaluation of 40 sites after at least 1 year of loading. Int. J. Periodontics Restor. Dent. 2010, 30, 355. [Google Scholar]
- Bonnet, F.; Karouni, M.; Antoun, H. Esthetic evaluation of periimplant soft tissue of immediate single-implant placement and provisionalization in the anterior maxilla. Int. J. Esthet. Dent. 2018, 13, 378–392. [Google Scholar]
- Botticelli, D.; Renzi, A.; Lindhe, J.; Berglundh, T. Implants in fresh extraction sockets: A prospective 5-year follow-up clinical study. Clin. Oral Implant. Res. 2008, 19, 1226–1232. [Google Scholar] [CrossRef]
- Brignardello-Petersen, R. Immediately placed and restored single-tooth implants in the anterior maxilla shown to have good esthetic outcomes 1 year after treatment. J. Am. Dent. Assoc. 2017, 148, e103. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.D.; Payne, A.G. Immediately restored single implants in the aesthetic zone of the maxilla using a novel design: 1-year report. Clin. Oral Implant. Res. 2011, 22, 445–454. [Google Scholar] [CrossRef]
- Bruno, V.; O’Sullivan, D.; Badino, M.; Catapano, S. Preserving soft tissue after placing implants in fresh extraction sockets in the maxillary esthetic zone and a prosthetic template for interim crown fabrication: A prospective study. J. Prosthet. Dent. 2014, 111, 195–202. [Google Scholar] [CrossRef]
- Cabello, G.; Rioboo, M.; Fábrega, J.G. Immediate placement and restoration of implants in the aesthetic zone with a trimodal approach: Soft tissue alterations and its relation to gingival biotype. Clin. Oral Implant. Res. 2013, 24, 1094–1100. [Google Scholar] [CrossRef]
- Cafiero, C.; Annibali, S.; Gherlone, E.; Grassi, F.; Gualini, F.; Magliano, A.; Romeo, E.; Tonelli, P.; Lang, N.P.; Salvi, G. Immediate transmucosal implant placement in molar extraction sites: A 12-month prospective multicenter cohort study. Clin. Oral Implant. Res. 2008, 19, 476–482. [Google Scholar] [CrossRef]
- Calvo Guirado, J.L.; Sáez Yuguero, R.; Ferrer Pérez, V.; Moreno Pelluz, A. Immediate anterior implant placement and early loading by provisional acrylic crowns: A prospective study after a one-year follow-up Period. J. Ir. Dent. Assoc. 2002, 48, 43–49. [Google Scholar] [PubMed]
- Calvo-Guirado, J.L.; Gómez-Moreno, G.; Aguilar-Salvatierra, A.; Guardia, J.; Delgado-Ruiz, R.A.; Romanos, G.E. Marginal bone loss evaluation around immediate non-occlusal microthreaded implants placed in fresh extraction sockets in the maxilla: A 3-year study. Clin. Oral Implant. Res. 2015, 26, 761–767. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Guirado, J.L.; Ortiz-Ruiz, A.J.; López-Marí, L.; Delgado-Ruiz, R.; Maté-Sánchez, J.; Bravo Gonzalez, L.A. Immediate maxillary restoration of single-tooth implants using platform switching for crestal bone preservation: A 12-month study. Int. J. Oral Maxillofac. Implant. 2009, 24, 275–281. [Google Scholar]
- Canullo, L.; Rasperini, G. Preservation of peri-implant soft and hard tissues using platform switching of implants placed in immediate extraction sockets: A proof-of-concept study with 12-to 36-month follow-up. Int. J. Oral Maxillofac. Implant. 2007, 22, 995–1000. [Google Scholar]
- Cardaropoli, D.; Tamagnone, L.; Roffredo, A.; Gaveglio, L. Soft tissue contour changes at immediate postextraction single-tooth implants with immediate restoration: A 12-month prospective cohort study. Int. J. Periodontics Restor. Dent. 2015, 35, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Carlino, P.; Pepe, V.; Pollice, G.; Grassi, F. Immediate transmucosal implant placement in fresh maxillary and mandibular molar extraction sockets: Description of technique and preliminary results. Minerva Stomatol. 2008, 57, 471. [Google Scholar] [PubMed]
- Chaushu, G.; Chaushu, S.; Tzohar, A.; Dayan, D. Immediate loading of single-tooth implants: Immediate versus non-immediate implantation. A clinical report. Int. J. Oral Maxillofac. Implant. 2001, 16, 267–272. [Google Scholar]
- Chen, S.T.; Darby, I.B.; Adams, G.G.; Reynolds, E.C. A prospective clinical study of bone augmentation techniques at immediate implants. Clin. Oral Implant. Res. 2005, 16, 176–184. [Google Scholar] [CrossRef]
- Chen, S.T.; Darby, I.B.; Reynolds, E.C. A prospective clinical study of non-submerged immediate implants: Clinical outcomes and esthetic results. Clin. Oral Implant. Res. 2007, 18, 552–562. [Google Scholar] [CrossRef]
- Chen, Y.; Yuan, S.; Zhou, N.; Man, Y. Transcrestal sinus floor augmentation with immediate implant placement applied in three types of fresh extraction sockets: A clinical prospective study with 1-year follow-up. Clin. Implant. Dent. Relat. Res. 2017, 19, 1034–1043. [Google Scholar] [CrossRef]
- Chung, S.; Rungcharassaeng, K.; Kan, J.Y.K.; Roe, P.; Lozada, J.L. Immediate Single Tooth Replacement with Subepithelial Connective Tissue Graft Using Platform Switching Implants: A Case Series. J. Oral Implantol. 2011, 37, 559–569. [Google Scholar] [CrossRef]
- Cooper, L.F.; Raes, F.; Reside, G.J.; Garriga, J.S.; Tarrida, L.G.; Wiltfang, J.; Kern, M.; de Bruyn, H. Comparison of radiographic and clinical outcomes following immediate provisionalization of single-tooth dental implants placed in healed alveolar ridges and extraction sockets. Int. J. Oral Maxillofac. Implant. 2010, 25, 1222–1232. [Google Scholar]
- Cooper, L.F.; Reside, G.J.; Raes, F.; Garriga, J.S.; Tarrida, L.G.; Wiltfang, J.; Kern, M.; De Bruyn, H. Immediate provisionalization of dental implants placed in healed alveolar ridges and extraction sockets: A 5-year prospective evaluation. Int. J. Oral Maxillofac. Implant. 2014, 29, 709–717. [Google Scholar] [CrossRef] [PubMed]
- Cornelini, R.; Barone, A.; Covani, U. Connective tissue grafts in postextraction implants with immediate restoration: A prospective controlled clinical study. Pract. Proced. Aesthetic Dent. PPAD 2008, 20, 337–343. [Google Scholar] [PubMed]
- Cornelini, R.; Cangini, F.; Covani, U.; Wilson Jr, T.G. Immediate restoration of implants placed into fresh extraction sockets for single-tooth replacement: A prospective clinical study. Int. J. Periodontics Restor. Dent. 2005, 25, 439–447. [Google Scholar] [CrossRef]
- Cosyn, J.; Eghbali, A.; De Bruyn, H.; Collys, K.; Cleymaet, R.; De Rouck, T. Immediate single-tooth implants in the anterior maxilla: 3-year results of a case series on hard and soft tissue response and aesthetics. J. Clin. Periodontol. 2011, 38, 746–753. [Google Scholar] [CrossRef]
- Cosyn, J.; Eghbali, A.; Hanselaer, L.; De Rouck, T.; Wyn, I.; Sabzevar, M.M.; Cleymaet, R.; De Bruyn, H. Four modalities of single implant treatment in the anterior maxilla: A clinical, radiographic, and aesthetic evaluation. Clin. Implant. Dent. Relat. Res. 2013, 15, 517–530. [Google Scholar] [CrossRef]
- Cosyn, J.; Eghbali, A.; Hermans, A.; Vervaeke, S.; De Bruyn, H.; Cleymaet, R. A 5-year prospective study on single immediate implants in the aesthetic zone. J. Clin. Periodontol. 2016, 43, 702–709. [Google Scholar] [CrossRef]
- Covani, U.; Canullo, L.; Toti, P.; Alfonsi, F.; Barone, A. Tissue stability of implants placed in fresh extraction sockets: A 5-year prospective single-cohort study. J. Periodontol. 2014, 85, e323–e332. [Google Scholar] [CrossRef]
- Covani, U.; Chiappe, G.; Bosco, M.; Orlando, B.; Quaranta, A.; Barone, A. A 10-year evaluation of implants placed in fresh extraction sockets: A prospective cohort study. J. Periodontol. 2012, 83, 1226–1234. [Google Scholar] [CrossRef] [PubMed]
- Covani, U.; Marconcini, S.; Galassini, G.; Cornelini, R.; Santini, S.; Barone, A. Connective tissue graft used as a biologic barrier to cover an immediate implant. J. Periodontol. 2007, 78, 1644–1649. [Google Scholar] [CrossRef] [PubMed]
- Crespi, R.; Capparé, P.; Crespi, G.; Lo Giudice, G.; Gastaldi, G.; Gherlone, E. Immediate implant placement in sockets with asymptomatic apical periodontitis. Clin. Implant. Dent. Relat. Res. 2017, 19, 20–27. [Google Scholar] [CrossRef]
- Crespi, R.; Capparè, P.; Polizzi, E.; Gherlone, E. Fresh-Socket Implants of Different Collar Length: Clinical Evaluation in the Aesthetic Zone. Clin. Implant. Dent. Relat. Res. 2015, 17, 871–878. [Google Scholar] [CrossRef] [PubMed]
- Cristalli, M.P.; Marini, R.; La Monaca, G.; Sepe, C.; Tonoli, F.; Annibali, S. Immediate loading of post-extractive single-tooth implants: A 1-year prospective study. Clin. Oral Implant. Res. 2015, 26, 1070–1079. [Google Scholar] [CrossRef]
- De Bruyn, H.; Raes, F.; Cooper, L.F.; Reside, G.; Garriga, J.S.; Tarrida, L.G.; Wiltfang, J.; Kern, M. Three-years clinical outcome of immediate provisionalization of single Osseospeed™ implants in extraction sockets and healed ridges. Clin. Oral Implant. Res. 2013, 24, 217–223. [Google Scholar] [CrossRef]
- de Carvalho, B.C.F.; de Carvalho, E.M.O.F.; Xediek Consani, R.L. Flapless single-tooth immediate implant placement. Int. J. Oral Maxillofac. Implant. 2013, 2, 783–789. [Google Scholar] [CrossRef] [PubMed]
- De Kok, I.J.; Chang, S.S.; Moriarty, J.D.; Cooper, L.F. A retrospective analysis of peri-implant tissue responses at immediate load/provisionalized microthreaded implants. Int. J. Oral Maxillofac. Implant. 2006, 21, 405–412. [Google Scholar]
- De Rouck, T.; Collys, K.; Cosyn, J. Immediate single-tooth implants in the anterior maxilla: A 1-year case cohort study on hard and soft tissue response. J. Clin. Periodontol. 2008, 35, 649–657. [Google Scholar] [CrossRef]
- Degidi, M.; Daprile, G.; Nardi, D.; Piattelli, A. Buccal bone plate in immediately placed and restored implant with Bio-Oss® collagen graft: A 1-year follow-up study. Clin. Oral Implant. Res. 2013, 24, 1201–1205. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Daprile, G.; Nardi, D.; Piattelli, A. Immediate Provisionalization of Implants Placed in Fresh Extraction Sockets Using a Definitive Abutment: The Chamber Concept. Int. J. Periodontics Restor. Dent. 2013, 33, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Nardi, D.; Daprile, G.; Piattelli, A. Buccal bone plate in the immediately placed and restored maxillary single implant: A 7-year retrospective study using computed tomography. Implant. Dent. 2012, 21, 62–66. [Google Scholar] [CrossRef]
- Degidi, M.; Nardi, D.; Piattelli, A. Peri-implant tissue and radiographic bone levels in the immediately restored single-tooth implant: A retrospective analysis. J. Periodontol. 2008, 79, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Di Alberti, L.; Donnini, F.; Di Alberti, C.; Camerino, M.; Sgaramella, N.; Lo Muzio, L. Clinical and radiologic evaluation of 70 immediately loaded single implants in the maxillary esthetic zone: Preliminary results after 1 year of functional loading. Int. J. Oral Maxillofac. Implant. 2012, 27, 181–186. [Google Scholar]
- Evans, C.D.; Chen, S.T. Esthetic outcomes of immediate implant placements. Clin. Oral Implant. Res. 2008, 19, 73–80. [Google Scholar] [CrossRef]
- Fagan, M.C.; Owens, H.; Smaha, J.; Kao, R.T. Simultaneous hard and soft tissue augmentation for implants in the esthetic zone: Report of 37 consecutive cases. J. Periodontol. 2008, 79, 1782–1788. [Google Scholar] [CrossRef]
- Ferrara, A.; Galli, C.; Mauro, G.; Macaluso, G.M. Immediate provisional restoration of postextraction implants for maxillary single-tooth replacement. Int. J. Periodontics Restor. Dent. 2006, 26, 371–377. [Google Scholar]
- Fugazzotto, P. A retrospective analysis of immediately placed implants in 418 sites exhibiting periapical pathology: Results and clinical considerations. Int. J. Oral Maxillofac. Implant. 2012, 27, 194–202. [Google Scholar]
- Fugazzotto, P.A. A retrospective analysis of implants immediately placed in sites with and without periapical pathology in sixty-four patients. J. Periodontol. 2012, 83, 182–186. [Google Scholar] [CrossRef]
- Fürhauser, R.; Mailath-Pokorny, G.; Haas, R.; Busenlechner, D.; Watzek, G.; Pommer, B. Immediate Restoration of Immediate Implants in the Esthetic Zone of the Maxilla Via the Copy-Abutment Technique: 5-Year Follow-Up of Pink Esthetic Scores. Clin. Implant. Dent. Relat. Res. 2017, 19, 28–37. [Google Scholar] [CrossRef]
- Ganeles, J.; Norkin, F.J.; Zfaz, S. Single-Tooth Implant Restorations in Fresh Extraction Sockets of the Maxillary Esthetic Zone: Two-Year Results of a Prospective Cohort Study. Int. J. Periodontics Restor. Dent. 2017, 37, e154–e162. [Google Scholar] [CrossRef] [PubMed]
- Garber, D.A.; Salama, M.; Salama, H. Immediate total tooth replacement. Compend. Contin. Educ. Dent. 2001, 22, 210–216. [Google Scholar] [PubMed]
- Goldstein, M.; Boyan, B.D.; Schwartz, Z. The palatal advanced flap: A pedicle flap for primary coverage of immediately placed implants. Clin. Oral Implant. Res. 2002, 13, 644–650. [Google Scholar] [CrossRef] [PubMed]
- Grandi, T.; Garuti, G.; Samarani, R.; Guazzi, P.; Forabosco, A. Immediate loading of single post-extractive implants in the anterior maxilla: 12-month results from a multicenter clinical study. J. Oral Implantol. 2012, 38, 477–484. [Google Scholar] [CrossRef]
- Grandi, T.; Guazzi, P.; Samarani, R.; Grandi, G. Immediate provisionalisation of single post-extractive implants versus implants placed in healed sites in the anterior maxilla: 1-year results from a multicentre controlled cohort study. Eur. J. Oral Implantol. 2013, 6, 285–295. [Google Scholar]
- Guarnieri, R.; Belleggia, F.; Grande, M. Immediate versus delayed treatment in the anterior maxilla using single implants with a laser-microtextured collar: 3-year results of a case series on hard-and soft-tissue response and esthetics. J. Prosthodont. 2016, 25, 135–145. [Google Scholar] [CrossRef]
- Guarnieri, R.; Ceccherini, A.; Grande, M. Single-tooth replacement in the anterior maxilla by means of immediate implantation and early loading: Clinical and aesthetic results at 5 years. Clin. Implant. Dent. Relat. Res. 2015, 17, 314–326. [Google Scholar] [CrossRef]
- Guarnieri, R.; Placella, R.; Testarelli, L.; Iorio-Siciliano, V.; Grande, M. Clinical, radiographic, and esthetic evaluation of immediately loaded laser microtextured implants placed into fresh extraction sockets in the anterior maxilla: A 2-year retrospective multicentric study. Implant. Dent. 2014, 23, 144. [Google Scholar] [CrossRef]
- Hartlev, J.; Kohberg, P.; Ahlmann, S.; Andersen, N.T.; Schou, S.; Isidor, F. Patient satisfaction and esthetic outcome after immediate placement and provisionalization of single-tooth implants involving a definitive individual abutment. Clin. Oral Implant. Res. 2014, 25, 1245–1250. [Google Scholar] [CrossRef]
- Hartlev, J.; Kohberg, P.; Ahlmann, S.; Gotfredsen, E.; Andersen, N.T.; Isidor, F.; Schou, S. Immediate placement and provisionalization of single-tooth implants involving a definitive individual abutment: A clinical and radiographic retrospective study. Clin. Oral Implant. Res. 2013, 24, 652–658. [Google Scholar] [CrossRef]
- Hassan, K.S.; Kassim, A.; Al Ogaly, A.-U.R. A comparative evaluation of immediate dental implant with autogenous versus synthetic guided bone regeneration. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2008, 106, e8–e15. [Google Scholar] [CrossRef]
- Hattingh, A.; Hommez, G.; De Bruyn, H.; Huyghe, M.; Vandeweghe, S. A prospective study on ultra-wide diameter dental implants for immediate molar replacement. Clin. Implant. Dent. Relat. Res. 2018, 20, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Hof, M.; Pommer, B.; Ambros, H.; Jesch, P.; Vogl, S.; Zechner, W. Does timing of implant placement affect implant therapy outcome in the aesthetic zone? A clinical, radiological, aesthetic, and patient-based evaluation. Clin. Implant. Dent. Relat. Res. 2015, 17, 1188–1199. [Google Scholar] [CrossRef] [PubMed]
- Hu, C.; Gong, T.; Lin, W.; Yuan, Q.; Man, Y. Immediate implant placement into posterior sockets with or without buccal bone dehiscence defects: A retrospective cohort study. J. Dent. 2017, 65, 95–100. [Google Scholar] [CrossRef]
- Hui, E.; Chow, J.; Li, D.; Liu, J.; Wat, P.; Law, H. Immediate provisional for single-tooth implant replacement with Brånemark system: Preliminary report. Clin. Implant. Dent. Relat. Res. 2001, 3, 79–86. [Google Scholar] [CrossRef]
- Jiansheng, H.; Dongying, X.; Xianfeng, W.; Baoyi, X.; Qiong, L.; Jincai, Z. Clinical evaluation of short and wide-diameter implants immediately placed into extraction sockets of posterior areas: A 2-year retrospective study. J. Oral Implantol. 2012, 38, 729–737. [Google Scholar] [CrossRef] [PubMed]
- Juodzbalys, G.; Wang, H.-L. Socket Morphology--Based Treatment for Implant Esthetics: A Pilot Study. Int. J. Oral Maxillofac. Implant. 2010, 25, 970–978. [Google Scholar]
- Juodzbalys, G.; Wang, H.L. Soft and hard tissue assessment of immediate implant placement: A case series. Clin. Oral Implant. Res. 2007, 18, 237–243. [Google Scholar] [CrossRef]
- Kahnberg, K.-E. Immediate implant placement in fresh extraction sockets: A clinical report. Int. J. Oral Maxillofac. Implant. 2009, 24, 282–288. [Google Scholar]
- Kan, J.Y.; Rungcharassaeng, K.; Liddelow, G.; Henry, P.; Goodacre, C.J. Periimplant tissue response following immediate provisional restoration of scalloped implants in the esthetic zone: A one-year pilot prospective multicenter study. J. Prosthet. Dent. 2007, 97, S109–S118. [Google Scholar] [CrossRef]
- Kan, J.Y.; Rungcharassaeng, K.; Lozada, J.L.; Zimmerman, G. Facial gingival tissue stability following immediate placement and provisionalization of maxillary anterior single implants: A 2-to 8-year follow-up. Int. J. Oral Maxillofac. Implant. 2011, 26, 179–187. [Google Scholar]
- Kan, J.Y.; Rungcharassaeng, K.; Morimoto, T.; Lozada, J. Facial gingival tissue stability after connective tissue graft with single immediate tooth replacement in the esthetic zone: Consecutive case report. J. Oral Maxillofac. Surg. 2009, 67, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Kan, J.Y.; Rungcharassaeng, K.; Sclar, A.; Lozada, J.L. Effects of the facial osseous defect morphology on gingival dynamics after immediate tooth replacement and guided bone regeneration: 1-year results. J. Oral Maxillofac. Surg. 2007, 65, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Kan, J.Y.; Rungcharassaeng, K.; Umezu, K.; Kois, J.C. Dimensions of peri-implant mucosa: An evaluation of maxillary anterior single implants in humans. J. Periodontol. 2003, 74, 557–562. [Google Scholar] [CrossRef]
- Khzam, N.; Mattheos, N.; Roberts, D.; Bruce, W.L.; Ivanovski, S. Immediate placement and restoration of dental implants in the esthetic region: Clinical case series. J. Esthet. Restor. Dent. 2014, 26, 332–344. [Google Scholar] [CrossRef]
- Koirala, D.P.; Singh, S.V.; Chand, P.; Siddharth, R.; Jurel, S.K.; Aggarwal, H.; Tripathi, S.; Ranabhatt, R.; Mehrotra, D. Early loading of delayed versus immediately placed implants in the anterior mandible: A pilot comparative clinical study. J. Prosthet. Dent. 2016, 116, 340–345. [Google Scholar] [CrossRef]
- Kolerman, R.; Mijiritsky, E.; Barnea, E.; Dabaja, A.; Nissan, J.; Tal, H. Esthetic Assessment of Implants Placed into Fresh Extraction Sockets for Single-Tooth Replacements Using a Flapless Approach. Clin. Implant. Dent. Relat. Res. 2017, 19, 351–364. [Google Scholar] [CrossRef]
- Kolerman, R.; Nissan, J.; Mijiritsky, E.; Hamoudi, N.; Mangano, C.; Tal, H. Esthetic assessment of immediately restored implants combined with GBR and free connective tissue graft. Clin. Oral Implant. Res. 2016, 27, 1414–1422. [Google Scholar] [CrossRef]
- Kolerman, R.; Nissan, J.; Rahmanov, A.; Zenziper, E.; Slutzkey, S.; Tal, H. Radiological and biological assessment of immediately restored anterior maxillary implants combined with GBR and free connective tissue graft. Clin. Implant. Dent. Relat. Res. 2016, 18, 1142–1152. [Google Scholar] [CrossRef]
- Kuchler, U.; Chappuis, V.; Gruber, R.; Lang, N.P.; Salvi, G.E. Immediate implant placement with simultaneous guided bone regeneration in the esthetic zone: 10-year clinical and radiographic outcomes. Clin. Oral Implant. Res. 2016, 27, 253–257. [Google Scholar] [CrossRef]
- Lee, Y.-M.; Kim, D.-Y.; Kim, J.Y.; Kim, S.-H.; Koo, K.-T.; Kim, T.-I.; Seol, Y.-J. Peri-implant soft tissue level secondary to a connective tissue graft in conjunction with immediate implant placement: A 2-year follow-up report of 11 consecutive cases. Int. J. Periodontics Restor. Dent. 2012, 32, 213–222. [Google Scholar]
- Li, P.; Zhu, H.; Huang, D. Autogenous DDM versus Bio-Oss granules in GBR for immediate implantation in periodontal postextraction sites: A prospective clinical study. Clin. Implant. Dent. Relat. Res. 2018, 20, 923–928. [Google Scholar] [CrossRef] [PubMed]
- Lindeboom, J.A.; Tjiook, Y.; Kroon, F.H. Immediate placement of implants in periapical infected sites: A prospective randomized study in 50 patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2006, 101, 705–710. [Google Scholar] [CrossRef]
- Locante, W.M. Single-tooth replacements in the esthetic zone with an immediate function implant: A preliminary report. J. Oral Implantol. 2004, 30, 369–375. [Google Scholar] [CrossRef]
- Lops, D.; Romeo, E.; Chiapasco, M.; Procopio, R.M.; Oteri, G. Behaviour of soft tissues healing around single bone-level-implants placed immediately after tooth extraction A 1 year prospective cohort study. Clin. Oral Implant. Res. 2013, 24, 1206–1213. [Google Scholar] [CrossRef] [PubMed]
- Lorenzoni, M.; Pertl, C.; Zhang, K.; Wimmer, G.; Wegscheider, W.A. Immediate loading of single-tooth implants in the anterior maxilla. Preliminary results after one year. Clin. Oral Implant. Res. 2003, 14, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud Aly, T.; Mohamed Arafat, S. Immediate loading of implants placed into fresh extraction sockets with periapical lesions without augmentation. Smile Dent. J. 2008, 3, 6–22. [Google Scholar]
- Malchiodi, L.; Cucchi, A.; Ghensi, P.; Nocini, P.F. Evaluation of the esthetic results of 64 nonfunctional immediately loaded postextraction implants in the maxilla: Correlation between interproximal alveolar crest and soft tissues at 3 years of follow-up. Clin. Implant. Dent. Relat. Res. 2013, 15, 130–142. [Google Scholar] [CrossRef] [PubMed]
- Malchiodi, L.; Scarano, A.; Corrocher, G.; Trevisiol, L.; Quaranta, A.; Gerosa, R. Experimental study of a new surgical technique for anatomic remodeling of atrophic socket in maxillary postextraction single implant. Minerva Stomatol. 2008, 57, 519–528. [Google Scholar]
- Mangano, F.; Mangano, C.; Ricci, M.; Sammons, R.L.; Shibli, J.A.; Piattelli, A. Single-tooth Morse taper connection implants placed in fresh extraction sockets of the anterior maxilla: An aesthetic evaluation. Clin. Oral Implant. Res. 2012, 23, 1302–1307. [Google Scholar] [CrossRef]
- Mangano, F.G.; De Franco, M.; Caprioglio, A.; Macchi, A.; Piattelli, A.; Mangano, C. Immediate, non-submerged, root-analogue direct laser metal sintering (DLMS) implants: A 1-year prospective study on 15 patients. Lasers Med. Sci. 2014, 29, 1321–1328. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.G.; Mangano, C.; Ricci, M.; Sammons, R.L.; Shibli, J.A.; Piattelli, A. Esthetic evaluation of single-tooth Morse taper connection implants placed in fresh extraction sockets or healed sites. J. Oral Implantol. 2013, 39, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.G.; Mastrangelo, P.; Luongo, F.; Blay, A.; Tunchel, S.; Mangano, C. Aesthetic outcome of immediately restored single implants placed in extraction sockets and healed sites of the anterior maxilla: A retrospective study on 103 patients with 3 years of follow-up. Clin. Oral Implant. Res. 2017, 28, 272–282. [Google Scholar] [CrossRef] [PubMed]
- Mijiritsky, E.; Mardinger, O.; Mazor, Z.; Chaushu, G. Immediate provisionalization of single-tooth implants in fresh-extraction sites at the maxillary esthetic zone: Up to 6 years of follow-up. Implant. Dent. 2009, 18, 326–333. [Google Scholar] [CrossRef]
- Montoya-Salazar, V.; Castillo-Oyagüe, R.; Torres-Sánchez, C.; Lynch, C.D.; Gutiérrez-Pérez, J.-L.; Torres-Lagares, D. Outcome of single immediate implants placed in post-extraction infected and non-infected sites, restored with cemented crowns: A 3-year prospective study. J. Dent. 2014, 42, 645–652. [Google Scholar] [CrossRef]
- Morimoto, T.; Tsukiyama, Y.; Morimoto, K.; Koyano, K. Facial bone alterations on maxillary anterior single implants for immediate placement and provisionalization following tooth extraction: A superimposed cone beam computed tomography study. Clin. Oral Implant. Res. 2015, 26, 1383–1389. [Google Scholar] [CrossRef]
- Noelken, R.; Kunkel, M.; Wagner, W. Immediate implant placement and provisionalization after long-axis root fracture and complete loss of the facial bony lamella. Int. J. Periodontics Restor. Dent. 2011, 31, 175. [Google Scholar]
- Noelken, R.; Moergel, M.; Pausch, T.; Kunkel, M.; Wagner, W. Clinical and esthetic outcome with immediate insertion and provisionalization with or without connective tissue grafting in presence of mucogingival recessions: A retrospective analysis with follow-up between 1 and 8 years. Clin. Implant. Dent. Relat. Res. 2018, 20, 285–293. [Google Scholar] [CrossRef]
- Norton, M.R. A short-term clinical evaluation of immediately restored maxillary TiOblast single-tooth implants. Int. J. Oral Maxillofac. Implant. 2004, 19, 1333–1343. [Google Scholar]
- Norton, M.R. The influence of insertion torque on the survival of immediately placed and restored single-tooth implants. Int. J. Oral Maxillofac. Implant. 2011, 26, 1333–1343. [Google Scholar]
- Ormianer, Z.; Schiroli, G. Maxillary single-tooth replacement utilizing a novel ceramic restorative system: Results to 30 months. J. Oral Implantol. 2006, 32, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Paul, S.; Held, U. Immediate supracrestal implant placement with immediate temporization in the anterior dentition: A retrospective study of 31 implants in 26 patients with up to 5.5-years follow-up. Clin. Oral Implant. Res. 2013, 24, 710–717. [Google Scholar] [CrossRef] [PubMed]
- Peñarrocha-Diago, M.; Carrillo-Garcîa, C.; Boronat-Lopez, A.; García-Mira, B. Comparative study of wide-diameter implants placed after dental extraction and implants positioned in mature bone for molar replacement. Int. J. Oral Maxillofac. Implant. 2008, 23, 497–501. [Google Scholar]
- Perrotti, V.; Vozza, I.; Tumedei, M.; Pompa, G.; Iaculli, F.; Quaranta, A. Rehabilitation of Postextractive Socket in the Premaxilla: A 12-Year Study on 27 Titanium Plasma Spray Resorbable Calcium Phosphate Coated Single Implants. Implant. Dent.istry 2018, 27, 452–460. [Google Scholar] [CrossRef] [PubMed]
- Prosper, L.; Crespi, R.; Valenti, E.; Capparé, P.; Gherlone, E. Five-year follow-up of wide-diameter implants placed in fresh molar extraction sockets in the mandible: Immediate versus delayed loading. Int. J. Oral Maxillofac. Implant. 2010, 25, 607–612. [Google Scholar]
- Quaranta, A.; Perrotti, V.; Putignano, A.; Malchiodi, L.; Vozza, I.; Guirado, J.L.C. Anatomical remodeling of buccal bone plate in 35 premaxillary post-extraction immediately restored single TPS implants: 10-year radiographic investigation. Implant. Dent. 2016, 25, 186–192. [Google Scholar] [CrossRef]
- Raes, F.; Cooper, L.F.; Tarrida, L.G.; Vandromme, H.; De Bruyn, H. A case-control study assessing oral-health-related quality of life after immediately loaded single implants in healed alveolar ridges or extraction sockets. Clin. Oral Implant. Res. 2012, 23, 602–608. [Google Scholar] [CrossRef]
- Raes, F.; Cosyn, J.; Crommelinck, E.; Coessens, P.; De Bruyn, H. Immediate and conventional single implant treatment in the anterior maxilla: 1-year results of a case series on hard and soft tissue response and aesthetics. J. Clin. Periodontol. 2011, 38, 385–394. [Google Scholar] [CrossRef]
- Raes, F.; Cosyn, J.; De Bruyn, H. Clinical, aesthetic, and patient-related outcome of immediately loaded single implants in the anterior maxilla: A prospective study in extraction sockets, healed ridges, and grafted sites. Clin. Implant. Dent. Istry Relat. Res. 2013, 15, 819–835. [Google Scholar] [CrossRef]
- Raes, S.; Cosyn, J.; Noyelle, A.; Raes, F.; De Bruyn, H. Clinical Outcome After 8 to 10 Years of Immediately Restored Single Implants Placed in Extraction Sockets and Healed Ridges. Int. J. Periodontics Restor. Dent. 2018, 38, 337–345. [Google Scholar] [CrossRef]
- Ribeiro, F.S.; Pontes, A.E.F.; Marcantonio, E.; Piattelli, A.; Neto, R.J.B.; Marcantonio Jr, E. Success rate of immediate nonfunctional loaded single-tooth implants: Immediate versus delayed implantation. Implant. Dent. 2008, 17, 109–117. [Google Scholar] [CrossRef]
- Rodrigo, D.; Martin, C.; Sanz, M. Biological complications and peri-implant clinical and radiographic changes at immediately placed dental implants. A prospective 5-year cohort study. Clin. Oral Implant. Res. 2012, 23, 1224–1231. [Google Scholar] [CrossRef] [PubMed]
- Roe, P.; Kan, J.Y.; Rungcharassaeng, K.; Caruso, J.M.; Zimmerman, G.; Mesquida, J. Horizontal and vertical dimensional changes of peri-implant facial bone following immediate placement and provisionalization of maxillary anterior single implants: A 1-year cone beam computed tomography study. Int. J. Oral Maxillofac. Implant. 2012, 27, 393–400. [Google Scholar]
- Romeo, E.; Lops, D.; Rossi, A.; Storelli, S.; Rozza, R.; Chiapasco, M. Surgical and prosthetic management of interproximal region with single-implant restorations: 1-year prospective study. J. Periodontol. 2008, 79, 1048–1055. [Google Scholar] [CrossRef]
- Carlos Martins da Rosa, J.; Cristina Pértile de Oliveira Rosa, A.; Eduardo Francischone, C.; Salles Sotto-Maior, B. Esthetic outcomes and tissue stability of implant placement in compromised sockets following immediate dentoalveolar restoration: Results of a prospective case series at 58 months follow-up. Int. J. Periodontics Restor. Dent. 2014, 34, 198–208. [Google Scholar] [CrossRef]
- Ross, S.B.; Pette, G.A.; Parker, W.B.; Hardigan, P. Gingival margin changes in maxillary anterior sites after single immediate implant placement and provisionalization: A 5-year retrospective study of 47 patients. Int. J. Oral Maxillofac. Implant. 2014, 29, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Saito, H.; Chu, S.J.; Zamzok, J.; Brown, M.; Smith, R.; Sarnachiaro, G.; Hochman, M.; Fletcher, P.; Reynolds, M.A.; Tarnow, D.P. Flapless Postextraction Socket Implant Placement: The Effects of a Platform Switch-Designed Implant on Peri-implant Soft Tissue Thickness—A Prospective Study. Int. J. Periodontics Restor. Dent. 2018, 38, s9–s15. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.; Cecchinato, D.; Ferrus, J.; Salvi, G.E.; Ramseier, C.; Lang, N.P.; Lindhe, J. Implants placed in fresh extraction sockets in the maxilla: Clinical and radiographic outcomes from a 3-year follow-up examination. Clin. Oral Implant. Res. 2014, 25, 321–327. [Google Scholar] [CrossRef]
- Sato, R.K.; Thomé, G.; Fontão, F.N.G.; de Melo Filho, A.; Melo, A.C.M. Morse Taper Implants Immediately Loaded in Fresh Extraction Sockets: A Prospective Cohort Study. Implant. Dent. 2017, 26, 345–350. [Google Scholar] [CrossRef]
- Schwartz-Arad, D.; Grossman, Y.; Chaushu, G. The clinical effectiveness of implants placed immediately into fresh extraction sites of molar teeth. J. Periodontol. 2000, 71, 839–844. [Google Scholar] [CrossRef]
- Shibly, O.; Kutkut, A.; Albandar, J.M. One-year re-entry results of guided bone regeneration around immediately placed implants with immediate or conventional loading: A case series. J. Int. Acad. Periodontol. 2012, 14, 62–68. [Google Scholar]
- Siciliano, V.I.; Salvi, G.E.; Matarasso, S.; Cafiero, C.; Blasi, A.; Lang, N.P. Soft tissues healing at immediate transmucosal implants placed into molar extraction sites with buccal self-contained dehiscences. A 12-month controlled clinical trial. Clin. Oral Implant. Res. 2009, 20, 482–488. [Google Scholar] [CrossRef]
- Siegenthaler, D.W.; Jung, R.E.; Holderegger, C.; Roos, M.; Hämmerle, C.H. Replacement of teeth exhibiting periapical pathology by immediate implants. A prospective, controlled clinical trial. Clin. Oral Implant. Res. 2007, 18, 727–737. [Google Scholar] [CrossRef] [PubMed]
- Soardi, C.M.; Bianchi, A.E.; Zandanel, E.; Spinato, S. Clinical and radiographic evaluation of immediately loaded one-piece implants placed into fresh extraction sockets. Quintessence Int. 2012, 43, 449–456. [Google Scholar] [PubMed]
- Spinato, S.; Agnini, A.; Chiesi, M.; Agnini, A.M.; Wang, H.L. Comparison between graft and no-graft in an immediate placed and immediate nonfunctional loaded implant. Implant. Dent. 2012, 21, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Steigmann, M.; Wang, H.L. Esthetic buccal flap for correction of buccal fenestration defects during flapless immediate implant surgery. J. Periodontol. 2006, 77, 517–522. [Google Scholar] [CrossRef] [PubMed]
- Takeshita, K.; Vandeweghe, S.; Vervack, V.; Sumi, T.; Bruyn, H.D.; Jimbo, R. Immediate Implant Placement and Loading of Single Implants in the Esthetic Zone: Clinical Outcome and Esthetic Evaluation in a Japanese Population. Int. J. Periodontics Restor. Dent. 2015, 35, 715–723. [Google Scholar] [CrossRef]
- Tarnow, D.P.; Chu, S.J.; Salama, M.A.; Stappert, C.F.; Salama, H.; Garber, D.A.; Sarnachiaro, G.O.; Sarnachiaro, E.; Luis Gotta, S.; Saito, H. Flapless postextraction socket implant placement in the esthetic zone: Part 1. The effect of bone grafting and/or provisional restoration on facial-palatal ridge dimensional change-a retrospective cohort study. Int. J. Periodontics Restor. Dent. 2014, 34, 322–331. [Google Scholar] [CrossRef]
- Tortamano, P.; Otávio Alves Camargo, L.; Stella Bello-Silva, M.; Hirokuni Kanashiro, L. Immediate implant placement and restoration in the esthetic zone: A prospective study with 18 months of follow-up. Int. J. Oral Maxillofac. Implant. 2010, 25, 345–350. [Google Scholar]
- Truninger, T.C.; Philipp, A.O.; Siegenthaler, D.W.; Roos, M.; Hämmerle, C.H.; Jung, R.E. A prospective, controlled clinical trial evaluating the clinical and radiological outcome after 3 years of immediately placed implants in sockets exhibiting periapical pathology. Clin. Oral Implant. Res. 2011, 22, 20–27. [Google Scholar] [CrossRef]
- Tsirlis, A.T. Clinical evaluation of immediate loaded upper anterior single implants. Implant. Dent. 2005, 14, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Tsuda, H.; Rungcharassaeng, K.; Kan, J.Y.; Roe, P.; Lozada, J.L.; Zimmerman, G. Peri-implant tissue response following connective tissue and bone grafting in conjunction with immediate single-tooth replacement in the esthetic zone: A case series. Int. J. Oral Maxillofac. Implant. 2011, 26, 427. [Google Scholar]
- Valentini, P.; Abensur, D.; Albertini, J.F.; Rocchesani, M. Immediate Provisionalization of Single Extraction-Site Implants in the Esthetic Zone: A Clinical Evaluation. Int. J. Periodontics Restor. Dent. 2010, 30, 41. [Google Scholar]
- Velasco-Ortega, E.; Wojtovicz, E.; España-Lopez, A.; Jimenez-Guerra, A.; Monsalve-Guil, L.; Ortiz-Garcia, I.; Serrera-Figallo, M.-A. Survival rates and bone loss after immediate loading of implants in fresh extraction sockets (single gaps). A clinical prospective study with 4 year follow-up. Med. Oral Patol. Oral Y Cir. Bucal 2018, 23, e230. [Google Scholar] [CrossRef]
- Parithimarkalaignan, S.; Padmanabhan, T.V. Osseointegration: An update. J. Indian Prosthodont. Soc. 2013, 13, 2–6. [Google Scholar] [CrossRef]
- Levin, L. Dealing with dental implant failures. J. Appl. Oral Sci. 2008, 16, 171–175. [Google Scholar] [CrossRef]
- Waasdorp, J.A.; Evian, C.I.; Mandracchia, M. Immediate Placement of Implants Into Infected Sites: A Systematic Review of the Literature. J. Periodontol. 2010, 81, 801–808. [Google Scholar] [CrossRef] [PubMed]
- Levin, L.; Schwartz-Arad, D. The effect of cigarette smoking on dental implants and related surgery. Implant. Dent. 2006, 14, 357–361. [Google Scholar] [CrossRef] [PubMed]
- Alsaadi, G.; Quirynen, M.; Komárek, A.; van Steenberghe, D. Impact of local and systemic factors on the incidence of late oral implant loss. Clin. Oral Implant. Res. 2008, 19, 670–676. [Google Scholar] [CrossRef]
- Zhu, Y.; Zheng, X.; Zeng, G.; Xu, Y.; Qu, X.; Zhu, M.; Lu, E. Clinical efficacy of early loading versus conventional loading of dental implants. Sci. Rep. 2015, 5, 15995. [Google Scholar] [CrossRef]
- Testori, T.; Zuffetti, F.; Capelli, M.; Galli, F.; Weinstein, R.L.; Del Fabbro, M. Immediate versus conventional loading of post-extraction implants in the edentulous jaws. Clin. Implant. Dent. Relat. Res. 2014, 16, 926–935. [Google Scholar] [CrossRef] [PubMed]
- Del Fabbro, M.; Ceresoli, V.; Taschieri, S.; Ceci, C.; Testori, T. Immediate loading of postextraction implants in the esthetic area: Systematic review of the literature. Clin. Implant. Dent. Relat. Res. 2015, 17, 52–70. [Google Scholar] [CrossRef] [PubMed]
- Villa, R.; Rangert, B. Early Loading of Interforaminal Implants Immediately Installed after Extraction of Teeth Presenting Endodontic and Periodontal Lesions. Clin. Implant. Dent. Relat. Res. 2005, 7, s28–s35. [Google Scholar] [CrossRef] [PubMed]
- Lata, J.; Parmar, M. Placement of single tooth implant in healed socket with immediate temporization: Clinical study. Contemp. Clin. Dent. 2012, 3, 412–415. [Google Scholar] [CrossRef] [PubMed]
- Tolstunov, L. Implant Zones of the Jaws: Implant Location and Related Success Rate. J. Oral Implantol. 2007, 33, 211–220. [Google Scholar] [CrossRef]
- Ata-Ali, J.; Ata-Ali, F. Do antibiotics decrease implant failure and postoperative infections? A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2013, 43, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Kashani, H.; Hilon, J.; Rasoul, M.H.; Friberg, B. Influence of a single preoperative dose of antibiotics on the early implant failure rate. A randomized clinical trial. Clin. Implant. Dent. Relat. Res. 2019, 21, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, N.; Saad, N. Effects of antibiotics on dental implants: A review. J. Clin. Med. Res. 2012, 4, 1–6. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Prophylactic antibiotic regimen and dental implant failure: A meta-analysis. J. Oral Rehabil. 2014, 41, 941–956. [Google Scholar] [CrossRef]
- Givens, E., Jr.; Bencharit, S.; Byrd, W.C.; Phillips, C.; Hosseini, B.; Tyndall, D. Immediate placement and provisionalization of implants into sites with periradicular infection with and without antibiotics: An exploratory study. J. Oral Implantol. 2015, 41, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Sharaf, B.; Jandali-Rifai, M.; Susarla, S.M.; Dodson, T.B. Do Perioperative Antibiotics Decrease Implant Failure? J. Oral Maxillofac. Surg. 2011, 69, 2345–2350. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Grusovin, M.G.; Worthington, H.V. Interventions for replacing missing teeth: Antibiotics at dental implant placement to prevent complications. Cochrane Database Syst. Rev. 2013, 2013, CD004152. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez Sánchez, F.; Rodríguez Andrés, C.; Arteagoitia, I. Which antibiotic regimen prevents implant failure or infection after dental implant surgery? A systematic review and meta-analysis. J. Cranio-Maxillo-Facial Surg. 2018, 46, 722–736. [Google Scholar] [CrossRef] [PubMed]
- Romandini, M.; De Tullio, I.; Congedi, F.; Kalemaj, Z.; D‘Ambrosio, M.; Laforí, A.; Quaranta, C.; Buti, J.; Perfetti, G. Antibiotic prophylaxis at dental implant placement: Which is the best protocol? A systematic review and network meta-analysis. J. Clin. Periodontol. 2019, 46, 382–395. [Google Scholar] [CrossRef]
- Kim, A.; Abdelhay, N.; Levin, L.; Walters, J.D.; Gibson, M.P. Antibiotic prophylaxis for implant placement: A systematic review of effects on reduction of implant failure. Br. Dent. J. 2020, 228, 943–951. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Tennant, M.; Walsh, L.J.; Kruger, E. Is there a consensus on antibiotic usage for dental implant placement in healthy patients? Aust. Dent. J. 2018, 63, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Gregoire, C. How are odontogenic infections best managed? J. Can. Dent. Assoc. 2010, 76, a37. [Google Scholar]
- Jun, S.H.; Park, C.-J.; Hwang, S.-H.; Lee, Y.K.; Zhou, C.; Jang, H.-S.; Ryu, J.-J. The influence of bone graft procedures on primary stability and bone change of implants placed in fresh extraction sockets. Maxillofac. Plast. Reconstr. Surg. 2018, 40, 8. [Google Scholar] [CrossRef] [PubMed]
- Willenbacher, M.; Al-Nawas, B.; Berres, M.; Kämmerer, P.W.; Schiegnitz, E. The Effects of Alveolar Ridge Preservation: A Meta-Analysis. Clin. Implant. Dent. Relat. Res. 2016, 18, 1248–1268. [Google Scholar] [CrossRef]
- Sbordone, L.; Levin, L.; Guidetti, F.; Sbordone, C.; Glikman, A.; Schwartz-Arad, D. Apical and marginal bone alterations around implants in maxillary sinus augmentation grafted with autogenous bone or bovine bone material and simultaneous or delayed dental implant positioning. Clin. Oral Implant. Res. 2011, 22, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Cionca, N.; Hashim, D.; Mombelli, A. Zirconia dental implants: Where are we now, and where are we heading? Periodontol. 2000 2017, 73, 241–258. [Google Scholar] [CrossRef] [PubMed]
- Hashim, D.; Cionca, N.; Courvoisier, D.; Mombelli, A. A systematic review of the clinical survival of zirconia implants. Clin. Oral Investig. 2016, 20, 1403–1417. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, D.; Sennerby, L.; Meredith, N. Measurements Comparing the Initial Stability of Five Designs of Dental Implants: A Human Cadaver Study. Clin. Implant. Dent. Relat. Res. 2000, 2, 85–92. [Google Scholar] [CrossRef]
- Strietzel, F.P.; Neumann, K.; Hertel, M. Impact of platform switching on marginal peri-implant bone-level changes. A systematic review and meta-analysis. Clin. Oral Implant. Res. 2015, 26, 342–358. [Google Scholar] [CrossRef]
- Rocha, S.; Wagner, W.; Wiltfang, J.; Nicolau, P.; Moergel, M.; Messias, A.; Behrens, E.; Guerra, F. Effect of platform switching on crestal bone levels around implants in the posterior mandible: 3 years results from a multicentre randomized clinical trial. J. Clin. Periodontol. 2016, 43, 374–382. [Google Scholar] [CrossRef]
- Renouard, F.; Nisand, D. Impact of implant length and diameter on survival rates. Clin. Oral Implant. Res. 2006, 17, 35–51. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-T.; Chen, Y.-W.; Starr, J.R.; Chuang, S.-K. Survival analysis of wide dental implant: Systematic review and meta-analysis. Clin. Oral Implant. Res. 2016, 27, 1251–1264. [Google Scholar] [CrossRef]
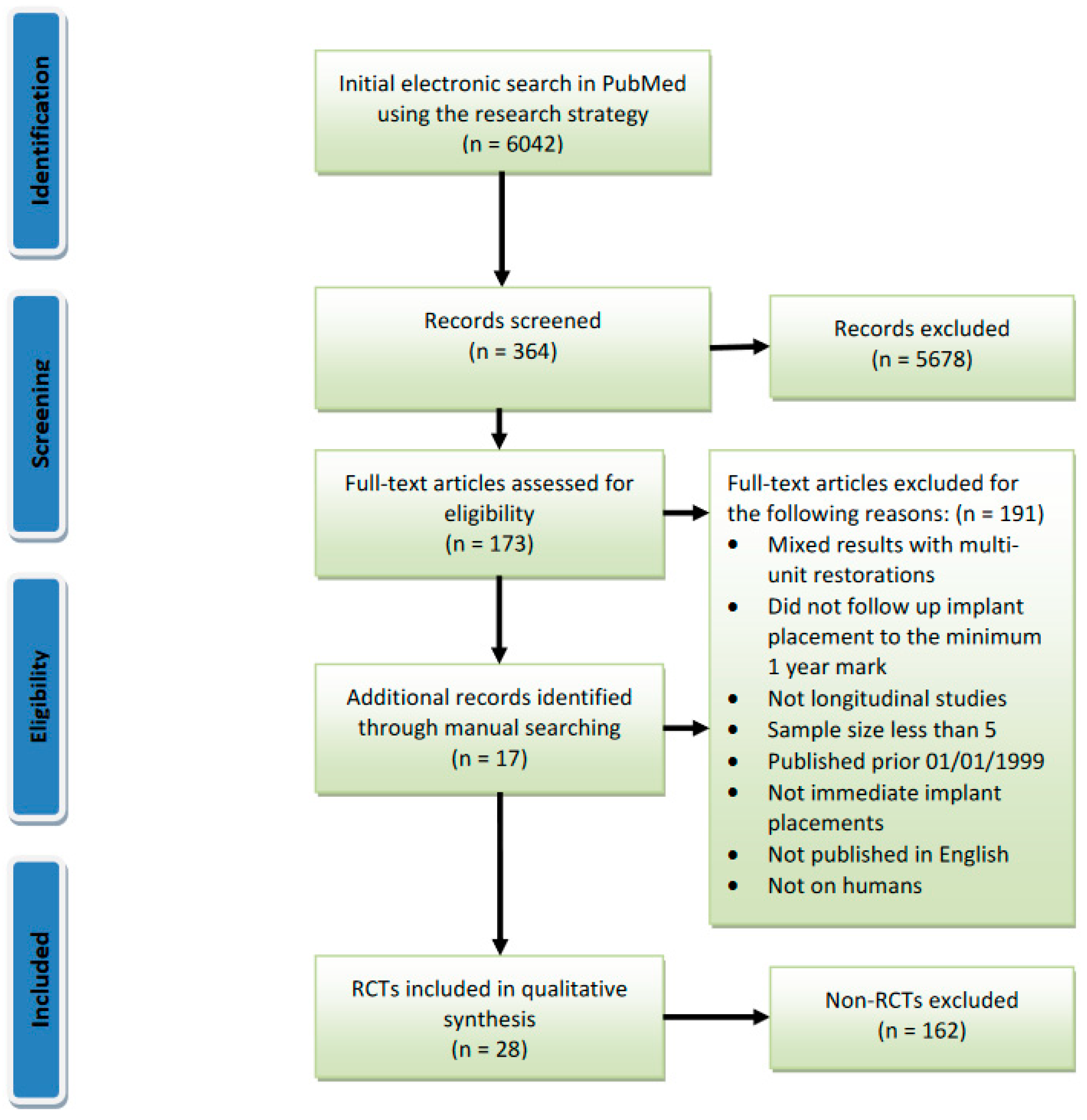
| Study | Survival Rate (Follow-Up Period) | Limitations |
|---|---|---|
| Atieh et al., 2010 [9] | 94–100% (6–36 months) | Included studies with follow-up of less than 1 year Published 10 years ago Included non-randomised control trials Did not assess for bias risk for the RCTs included Inclusion criteria for follow up was only 6 months |
| Chen et al., 2014 [10] | N/A (1–3 years) | Did not investigate and define survival, success, and failure Included non-randomised controlled trials |
| Cosyn et al., 2019 [11] | 94.9% (12–96 months) | Included non-randomised controlled studies Small number of studies included (n = 8) 7 out of 8 studies had high risk of bias Did not investigate the implant loading protocol |
| Lang et al., 2012 [12] | 98.4% (2 years) 97.5% (4 years) | Included multiple-unit IIP Included non-randomised controlled trials Published 8 years ago |
| Mello et al., 2017 [13] | 95.2% (6 months) | Did not define survival Included studies with follow-up of less than 12 months Included multiple-unit implants Included non-randomised controlled studies Did not define survival |
| Pigozzo et al., 2018 [14] | 95% (1–5 years) | Small sample size (n = 5) Did not define survival |
| Pjetturson et al., 2007 [15] | 92–99% (3 years) | Included multiple-unit Implants Did not mention whether the implants were immediate or delayed placements Did not define survival Included non-randomised controlled trials Did not investigate loading protocols Did not assess bias risk |
| Study | Random Sequence Generation | Allocation Concealment | Blinding of Participant & Personnel | Blinding of Outcome Data | Incomplete Outcome Data | Selective Reporting | Other Bias | Overall Quality |
|---|---|---|---|---|---|---|---|---|
| Canullo et al., 2009/2017 [21,22] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear risk | Unclear risk |
| Tallarico et al., 2016/2017 [23,24] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Cannizzaro et al., 2010 [25] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear risk | Unclear risk |
| Shibly et al., 2012 [27] | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Blocker et al., 2009 [28] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Canullo et al., 2010 [29] | Low risk | High risk | Unclear risk | Low risk | High risk | Low risk | Low risk | High risk |
| De Rouck et al., 2009 [30] | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear risk |
| Degidi et al., 2014 [31] | Low risk | Unclear risk | Low risk | Low risk | High risk | Low risk | Low risk | High risk |
| Esposito et al., 2015 [32] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear risk | Unclear risk |
| Felice et al., 2015 [33] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear risk | Unclear risk |
| Grandi et al., 2014 [34] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Migliorati et al., 2015 [35] | Low risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Unclear risk |
| Palatella et al., 2008 [37] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Unclear risk | Unclear risk |
| Pieri et al., 2011 [38] | Low risk | Low risk | Low risk | Unclear risk | Low risk | Low risk | Unclear risk | Unclear risk |
| Slagter et al., 2015 [39] | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Yoshino et al., 2014 [40] | Low risk | Unclear risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Unclear risk |
| Zuiderveld et al., 2018 [41] | Low risk | Low risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Unclear risk |
| Cecchinato et al., 2015 [42] | High risk | Unclear risk | Unclear risk | High risk | High risk | Low risk | Low risk | High risk |
| Cordaro et al., 2009 [43] | Low risk | Unclear risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | High risk |
| Cucchi et al., 2017 [44] | Low risk | High risk | High risk | Unclear risk | Low risk | Low risk | Low risk | Unclear risk |
| De Angelis et al., 2011 [45] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Koh et al., 2011 [46] | Low risk | Unclear risk | Unclear risk | Low risk | High risk | Low risk | Low risk | High risk |
| Prosper et al., 2003 [47] | Unclear risk | Unclear risk | Low risk | Unclear risk | Low risk | Low risk | Unclear risk | Unclear risk |
| Crespi et al., 2008 [49] | Unclear risk | Unclear risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Unclear risk |
| Urban et al., 2011 [48] | Low risk | Unclear risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Unclear risk |
| Van Nim-wegen et al., 2018 [50] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Follow-Up | Multiple-Units | Sample Size | Year of Publication | Not a Clinical Study | Non-Immediate Implants | Not in English | Animal Study |
|---|---|---|---|---|---|---|---|
| Amato et al., 2018 [51] | Al Nashar and Yakoob 2015 [52] | Chu et al., 2012 [53] | Becker et al., 1998 [54] | Lang et al., 2012 [10] | Boardman et al., 2016 [56] | Kohal et al., 2002 [57] | De Sanctis et al., 2009 [58] |
| Assaf et al., 2017 [59] | Alves et al., 2010 [60] | Cornelini et al., 2000, [61] | Becker et al., 1992 [62] | Chen et al., 2014 [12] | Buser et al., 2013 [64] | ||
| Basa et al., 2004 [65] | Anitua et al., 2016 [66] | De Molon et al., 2015 [67] | Garber et al., 1995 [68] | Aires and Berger 2002 [55] | Casap et al., 2007 [70] | ||
| Bell et al., 2014 [71] | Blus et al., 2006 [72] | Harvey 2007 [73] | Gelb 1993 [74] | Becker 2006 [63] | Eghbali et al., 2012 [76] | ||
| Botticelli et al., 2004 [77] | Eghbali et al., 2012 [76] | Park et al., 2010 [79] | Gomez-Roman et al. 1997, [80] | Becker et al., 2011 [69] | Le et al., 2014 [81] | ||
| Caiazzo et al., 2013 [82] | Bogaerde et al., 2010 [78] | Paul 2007 [84] | Hammerle et al., 1998 [85] | Bruno et al., 2012 [75] | Proussaefs et al., 2002 [87] | ||
| Calvo Guirado et al., 2007 [88] | Cosyn et al., 2013 [83] | Peñarrocha et al., 2006 [90] | Lang et al., 1994 [91] | Chang et al., 2009 [86] | Ryser et al., 2005 [93] | ||
| Chen et al. 2009, [94] | Covani et al., 2003 [89] | Rebele 2013 [96] | Rosenquist and Grenthe 1996 [97] | Chen et al., 2009 [92] | Sarnowski et al., 2012 [99] | ||
| Chu et al., 2015 [100] | Covani et al., 2004 [95] | Ross et al., 2013 [102] | Schwartz-Arad 1997 [103] | Daif et al., 2013 [98] | Schropp et al., 2003 [105] | ||
| Chu et al., 2018 [106] | Crespi et al., 2007 [101] | Schiroli 2003 [108] | Schwartz-Arad 1998 [109] | Enrique-Sacristan et al., 2011 [104] | Schropp et al., 2005 [111] | ||
| Covani et al., 2004 [112] | Crespi et al., 2009 [107] | Trimpou et al., 2010 [114] | Simion et al., 1992 [115] | Froum et al., 2007 [110] | |||
| Covani et al., 2008 [117] | Crespi et al., 2010 [113] | Turkyilmaz et al., 2009 [119] | Tritten et al., 1995 [120] | Fugazzotto and Hains 2013 [116] | |||
| Di Girolamo et al., 2016 [122] | Capelli et al., 2010 [118] | Werbitt and Goldberg 1992 [124] | Fugazzotto et al., 2012 [121] | ||||
| El Chaar et al., 2011 [126] | Crespi et al., 2014 [123] | Wilson 1992 [128] | Gluckman et al., 2018 [125] | ||||
| Evian et al., 2004 [130] | Crespi et al., 2018 [127] | Wöhrle 1998 [132] | Greenstein and Cavallaro 2014 [129] | ||||
| Felice et al., 2011 [134] | Danza et al., 2009 [131] | Holst et al., 2007 [133] | |||||
| Felice et al., 2016 [137] | Davarpanah et al., 2005 [135] | Kan et al., 2000 [136] | |||||
| Fernandes Diaz et al., 2012 [140] | Degidi et al., 2007 [138] | Kan et al., 2001 [139] | |||||
| Ferrus et al., 2010 [143] | Degidi et al., 2005 [141] | Kan et al., 2005 [142] | |||||
| Granić et al., 2015 [146] | Del Fabbro et al., 2009 [144] | Kan et al., 2018 [145] | |||||
| Groenendij et al., 2017 [149] | Deng et al., 2010 [147] | Kher et al., 2015 [148] | |||||
| Grunder 2011 [151] | Erakat et al., 2008 [152] | Koh et al., 2010 [150] | |||||
| Hossain et al., 2017 [153] | Finne et al., 2007 [154] | Lemongello 2007 [155] | |||||
| Huynh-Ba et al., 2019 [156] | Fugazzotto 2002 [157] | Levine et al., 2018 [158] | |||||
| Jofre et al., 2012 [159] | Fugazzotto 2008 [160] | Meltzer 2009 [161] | |||||
| Kamperos et al., 2016 [162] | Gokcen-Rohlig et al., 2010 [163] | Palti 2004 [164] | |||||
| Kolinski et al., 2014 [165] | Gomez-Roman et al., 2001 [166] | Ramsey 2007 [167] | |||||
| Lang et al., 2007 [168] | Grunder et al., 1999 [169] | Saadoun 2002 [170] | |||||
| Lee et al., 2014 [171] | Han et al., 2016 [172] | Waki 2016 [173] | |||||
| Levin and Chu 2018 [174] | Hayacibara et al., 2013 [175] | Weigl et al., 2016 [176] | |||||
| Lops et al., 2008 [177] | Heineman et al., 2013 [178] | Yan et al., 2016 [179] | |||||
| Malo et al., 2000 [180] | Herinemann et al., 2009 [181] | ||||||
| Matarasso et al., 2009 [182] | Horwitz et al., 2007 [183] | ||||||
| Miyamoto 2011 [184] | Jo et al., 2001 [185] | ||||||
| Nemcovsky et al., 1999 [186] | Khorsand et al., 2016 [187] | ||||||
| Nemcovsky et al., 2000 [188] | Laviv et al., 2010 [189] | ||||||
| Nemcovsky et al., 2002 [190] | Malchiodi et al., 2010 [191] | ||||||
| Parel and Schow 2005 [192] | Malchiodi et al., 2011 [193] | ||||||
| Peron et al., 2016 [194] | Malo et al., 2003 [195] | ||||||
| Pirker and Kocher 2009 [196] | Mankoo 2008 [197] | ||||||
| Redemagni et al., 2009 [198] | McAllister et al., 2012 [199] | ||||||
| Rieder et al., 2016 [200] | Meltzer 2012 [201] | ||||||
| Runcharassaeng et al., 2012 [202] | Mura 2012 [203] | ||||||
| Rungcharassaeng et al., 2012 [202] | Noelken et al., 2014 [204] | ||||||
| Saito et al., 2016 [205] | Noelken et al., 2014 [206] | ||||||
| Sanz et al., 2010 [207] | Noelken et al., 2016 [208] | ||||||
| Sarnachiaro et al., 2016 [209] | Noelken et al., 2018 [210] | ||||||
| Scarano 2017 [211] | Ormanier and Palti 2008 [212] | ||||||
| Somanthan et al., 2007 [213] | Ormanier et al., 2012 [214] | ||||||
| Tomasi et al., 2010 [215] | Paolantonio et al., 2001 [216] | ||||||
| Van Kesteren et al., 2010 [217] | Peñarrocha-Diago et al., 2012 [218] | ||||||
| Vanderweghe et al., 2013 [219] | Peñarrocha-Oltra et al., 2012 [220] | ||||||
| Vidigal et al., 2017 [221] | Perry and Lenchewski 2004 [222] | ||||||
| West and Oates 2007 [223] | Polizzi et al., 2000 [224] | ||||||
| Younis et al., 2009 [225] | Siebers et al., 2010 [226] | ||||||
| Siebert et al., 2015 [227] | |||||||
| Simsek and Simsek 2003 [228] | |||||||
| Stefanski et al., 2017 [229] | |||||||
| Tsai et al., 2000 [230] | |||||||
| Van Steenberghe et al., 2000 [231] | |||||||
| Vanden Bogaerde et al., 2005 [232] | |||||||
| Vidal et al., 2010 [233] | |||||||
| Villa and Rangert 2007 [234] | |||||||
| Wagenberg and Froum 2006 [235] | |||||||
| Wagenberg et al., 2013 [236] | |||||||
| Wagenberg et al., 2015 [237] | |||||||
| Wilson et al., 2003, [238] | |||||||
| Wychowanski et al., 2017 [239] |
| Study | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Block et al., 2009, [28] | Present for recalls and maintenance cleaning. Single rooted maxillary central or lateral incisor, canine, or premolar, with no signs of acute infection (purulent exudate, erythema, pain, and swelling). Intact first molar occlusion to control occlusal forces on the implant restoration. Intact bony socket within 3 mm of the gingival margin of the planned restoration. Adequate space for satisfactory restoration. No active periodontal disease or exhibited controllable periodontal disease such that their teeth were clinically nonmobile and had probing depths less than 3 mm. Crown–root ratio of at least 1:2. 2 mm of attached or keratinized gingiva. Crestal bone sufficient for 4 mm diameter implant for the central incisor, canine, and premolar sites, or a 3.25 mm diameter implant. | ASA III or IV. Postmenopausal women with known osteoporosis. Alcohol abuse was excluded. No uncontrolled diabetes (any type), existing malignancy, and were not receiving any therapy that suppresses their immune system. |
| Cannizzaro et al., 2010, [25] | Requires one single implant. Residual bone height of at least 10 mm and a thickness of at least 5 mm. Informed consent. | General contraindications to implant surgery. No opposite occluding dentition in the area. Acute infection. Immunosuppression or immunodepression. Active periodontitis. Poor OH. Irradiation in the head or neck area. Bruxism. Treatment or past treatment with intra-venous amino bisphosphonates. Uncontrolled diabetes. Pregnant or lactating. Substance abuse. Psychiatric disorders or unrealistic expectations. Participation in other clinical trials. Unable to be followed for at least 1 year. Requiring the use of a membrane at implant placement. Subjectively evaluated sites as soft bone quality. Implants placed with an insertion torque < 35 Ncm. |
| Canullo et al., 2009/2017, [21,22] | Single tooth scheduled for extraction. Maxillary tooth from right second bicuspid to left one. Well-preserved alveolar ridge after extraction. General good health. | Acute infection. FMPS and a FMBS > 25%. Interproximal space narrower than 9 mm or with interproximal and buccal bone defects. Smoking >10 cigarettes per day. Uncontrolled diabetes (glycaemic level > 110 mg/L and HbA1c > 6%). Pregnant or lactating. |
| Canullo et al., 2010, [29] | ≥18 years. Requires a single implant in premolar areas of the maxilla. FMPS and FMBS < 25%. Opposing natural teeth. Adjacent teeth. Intact alveolar bone walls. At least 4 mm of bone beyond the root apex. | Chronic systemic diseases. Smoking >10 cigarettes per day. Pregnant or lactating females. Acute infection at the sites. Interproximal space narrower than 9 mm. Interproximal or buccal bone defects. |
| Cecchinato et al., 2015, [42] | ≥18 years of age subjects in need of one or more implants replacing teeth to be removed from 15 to 25. Presence of at least 20 teeth with expected functional occlusion. Intact extraction socket suitable for both cylindrical and conical/cylindrical implants. A marginal border of the facial bone crest that deviated 2 mm from normal location. Potential facial fenestration at least 3 mm apical of the marginal bone crest. | Untreated rampant caries and uncontrolled periodontal disease. Absence of adjacent (mesial and/or distal) natural tooth root. Uncontrolled diabetes or any other systemic or local disease. Systemic corticosteroids. Unable to return for follow-up. Unlikely to be able to comply. Bone alterations after immediate implant installation. Cigarette consumption in excess of 10 cigarettes or equivalent/day. |
| Cordaro et al., 2009, [43] | Type 1 procedure to replace maxillary incisors, canines and premolars or mandibular canines or premolars. 18–70 years old. | Systemic diseases. Uncontrolled periodontitis. Inadequate oral hygiene. Heavy smoking (4–10 cigarettes/day). Adjacent implants. If, at the moment of placement, the horizontal distance between the implant and the bony walls of the socket was 42 mm the patient should not be evaluated for the study purposes. |
| Crespi et al., 2008, [49] | 4 bony walls of the alveolus. At least 4 mm of bone beyond the root apex. Adjacent teeth. Good health. No chronic systemic disease. Informed consent. Immediate loading of the implants was performed with an implant stability quotient > 60 and implant insertion torque > 25 Ncm. | Dehiscence or fenestration of the residual bony walls. Uncontrolled diabetes. Coagulation disorders. Acute infection around the alveolar bone at the surgical site. Heavy smoking (more than 10 cigarettes per day). Alcohol or drug abuse. Bruxism. |
| Cucchi et al., 2017, [44] | One single immediate post-extractive implant in the posterior maxilla and mandible (only premolar and molar regions). Adequate bone volume to place an implant at least 3.7 mm in diameter and 10 mm in length, without bone augmentation procedures. Natural occluding dentition. Comprehension, acceptance, and full compliance for the treatment and follow-up. | Available bone length < 10 mm and bone width < 4.5 mm. Untreated and/or active periodontitis. FMPI > 20%; FMBI > 20%. Heavy smoking habit (>20 cigarettes/day). General contraindication to implant surgery. Uncontrolled systemic diseases. Immunosuppression. HIV/HCV/HBV infection. Chemotherapy and/or irradiation in the head and neck area. Treatment with amino bisphosphonates. Pregnancy or nursing. Inability to complete follow up. |
| De Angelis et al., 2011, [45] | ≥18 years. Single-tooth replacement in upper arch from premolar to central incisor. Good oral hygiene. Tooth to be replaced should have been in place at the time of study enrolment. Alveolar bone walls intact. Adjacent teeth in place. | General contraindications to implant surgery. Immunosuppressed or immunocompromised patients. Irradiation in the head or neck area. Uncontrolled diabetes. Pregnant or lactating. Untreated periodontitis. Poor oral hygiene. Substance abuse. Psychiatric disorders or unrealistic expectations. Acute infection (abscess) in the site intended for imp placement. Necessity to lift the maxillary sinus epithelium. Unable to follow-up post loading. IV amino bisphosphonates. Participation in other clinical trials interfering with the present protocol. Missing buccal bone sufficient to compromise the aesthetic outcome. |
| De Rouck et al., 2009, [30] | Good OH. Gingival harmony. Normal to thick biotype. Apical bone ≥ 5 mm | Systemic disease. Smoking ≥ 10 cigarettes/day. Bruxism. Lack of posterior support. Active periodontitis. Loss of labial bone. |
| Degidi et al., 2014, [31] | ≥18 years of age. Single compromised tooth in canine to canine maxillary anterior sector. | Active infection. Systemic disease that could compromise osseointegration. Radiation therapy in the craniofacial region within the previous 12 months. Smoking > 10 cigarettes per day. Pregnancy or lactation. Bruxism. Unsuitable quantity of bone in the surgery site or need of bone augmentation procedures prior to implant placement. Implant insertion torque < 25 Ncm. ISQ < 60. Dehiscence, fenestration, or fracture. |
| Esposito et al., 2015, [32] | One single immediate post-extractive implant in the maxilla from second to second premolar. Adjacent teeth. ≥18 years old. Signed an informed consent form. Sufficient bone to allow the placement of a single implant at least 7 mm long with a 4 mm diameter. | General contraindications to implant surgery. Immunosuppressed or immunocompromised. Irradiation in the head or neck area. Uncontrolled diabetes. Pregnant or lactating. Untreated periodontitis. Poor oral hygiene. Substance abuse. Psychiatric disorders. Acute infection. Necessity to lift the maxillary sinus epithelium. Unable to attend recalls. Intravenous amino bisphosphonates. Participation in other clinical trials interfering with present protocol. More than 4 mm in height of the buccal wall was missing after tooth extraction. |
| Felice et al., 2015, [33] | One single immediate post-extractive implant in the maxilla from second to second premolar. Adjacent teeth. ≥18 years old. Signed an informed consent form. Sufficient bone to allow the placement of a single implant at least 8 mm long with a minimal diameter of 3.8 mm. For patients who required multiple edentulous areas to be restored, the operator was free to select one implant site to be included in the trial at the screening visit. | General contraindications to implant surgery. Immunosuppressed or immunocompromised. Irradiation in the head or neck area. Uncontrolled diabetes. Pregnancy or lactation. Untreated periodontitis. Poor oral hygiene and motivation. Addiction to alcohol or drugs. Psychiatric disorders. Unrealistic expectations. Acute infection (abscess). Necessity to lift the maxillary sinus epithelium. Unable to commit to follow-up. IV amino bisphosphonates. Lack of one or both adjacent natural teeth. >4 mm of buccal wall missing (in terms of height), assessed using the highest peak of the palatal wall as a reference point. Participation in other studies which interfere with present protocol. |
| Grandi et al., 2014, [34] | ≥18 years of age. Single immediate post-extractive implant from 15 to 25 with adjacent teeth. Sufficient bone to allow the placement of an implant at least 11.5 mm long with a 3.7 mm diameter. Maximum plaque index score of 13 less than or equal to 2. | Dehiscence or lack of buccal bone plate after tooth extraction. General contraindications to implant surgery. Irradiation in the head and neck area. Immunosuppressed or immunocompromised patientsTreated or under treatment with IV bisphosphonates. Uncontrolled diabetes. Substance abuse. Heavy smoking (20 cigarettes daily). Lack of opposing occluding dentition. |
| Koh et al., 2011, [46] | >18 years of age. Systemically healthy. Tooth in the maxillary premolar or anterior region requiring extraction. Stable occlusion, adjacent and opposing teeth. Healthy periodontium. | Unstable systemic disease precluding surgical procedures. Compromised healing conditions. Bone disorders. Pregnant. Alcoholism or recreational drug abuse. Smoking > 10 cigarettes per day, long term (>2 weeks). Anti-inflammatories. Steroids. Bisphosphonates in the past 3 months. O’Leary plaque score > 20%. Parafunctional habits. Active dental disease. Anatomic limitations. |
| Migliorati et al., 2013, [35] | >21 years. Absence of periodontal disease. Adequate bone to achieve implant primary stability. KM width of at least 2 mm. Soft tissue level on the same level to the contralateral tooth. Single-tooth replacement in the anterior maxilla (from first bicuspid to first bicuspid). | Systemic diseases that could alter the tissue integration of dental implants. Pregnancy. Smoking > 10 cigarettes per day. |
| Palatella et al., 2008, [37] | ≥18 years. Single-tooth replacement in maxillary arch from premolar to central incisor. Good oral hygiene. Tooth to be replaced present at the time of enrolment, Alveolar bone walls intact after the extraction. Adjacent teeth were in place. | Uncontrolled diabetes. Coagulation impairments. Acute infections and/or suppuration at the surgical site. Bruxers. |
| Pieri et al., 2011, [38] | FMPS and FMBS < 25%. Four intact bony walls. ≥4 mm bone beyond apex. ≥3 mm KM. Presence of adjacent/opposing teeth. | Tobacco use (>20 cigarettes/day). History of radiotherapy in the head and neck region. Severe bleeding disorder. Diabetes mellitus. Pregnancy or lactation. Alcohol or drug abuse. Psychiatric problems. Bruxism or clenching. Untreated periodontitis. Acute infection and/or suppuration. |
| Prosper et al., 2003, [47] | 21–75 years. Compliance with home oral hygiene. Extraction because of caries, dental fracture, periodontitis, or endodontic treatment failure. Sufficiently wide, fresh extraction socket such that after 5.9 mm-diameter implant there would still be a residual bone defect. Good occlusion. | Criterion for exclusion was the presence of any dysmetabolic, chronic, and/or infectious disease. |
| Shibly et al., 2012, [27] | Maintenance periodontal recall after receiving active periodontal treatment because of a past history of periodontal disease. Single implant to replace a “hopeless” tooth. ESOP were included in this surgical protocol. GBR procedures were indicated to treat all ESOP defects. | Compromised general health conditions. Chemotherapy for the treatment of cancer. Antimetabolic therapy (e.g., methotrexate) for the treatment of arthritis. Uncontrolled diabetes. Severely impaired cardiovascular function. Immunodeficiency. Kidney or liver disease. Bruxism. |
| Slagter et al., 2015, [39] | ≥18 years old. Failing single tooth in maxillary aesthetic zone (up to first premolar) Adequate OH | Buccal socket wall with bony defect ≥5 mm in a vertical direction. |
| Tallarico et al., 2016/2017, [23,24] | One implant-supported single restoration to replace a failed tooth in the molar region of both jaws. Less than 5 mm between the root apex and the inferior alveolar nerve or maxillary sinus. ≥18 years old. Signed informed consent form. Fresh extraction sockets had to have intact buccal walls after extraction. | General contraindications to oral surgery (such as stroke, recent cardiac infarction, severe bleeding disorder, uncontrolled diabetes or cancer). Heavy smokers (≥11 cigarettes/day). Addiction to alcohol or drugs. Acute and chronic infections in the site intended for implant placement. Full mouth bleeding and full mouth plaque index higher than 25%. Pregnancy or nursing. Psychiatric therapy. Intravenous amino bisphosphonates. Radiotherapy of the oral and maxillofacial region within the last 5 years. Absence of opposing teeth. Severe clenching or bruxism. Unable to commit to the scheduled follow-up. |
| Urban et al., 2011, [48] | >18 years of age. Classified as ASA class 1—a normal healthy patient, and class 2—a patient with mild systemic disease (e.g., mild hypertension). Molar tooth. Adequate bone for placing at least a 10 mm long implant. | Systemic diseases affecting bone turnover and pregnant or lactating women. |
| Van Nimwegen et al., 2018, [50] | ≥18 years of age. Incisor, canine, or first bicuspid in the maxilla. Adjacent and opposing natural teeth. Adequate oral hygiene. Absence of active and uncontrolled periodontal disease. Sufficient mesial–distal and interocclusal space for placement of the implant and definitive restoration. Sufficient interocclusal space to design a non-occluding provisional restoration. An intact facial bone wall is present on the preoperative CBCT. | ASA score ≥ III. Periodontal disease. Smoking. Radiotherapy to the head and neck region. Pregnancy. Post-extraction bony defect and a distance that exceeded 5 mm. |
| Yoshino et al., 2014, [40] | ≥18 years or older. Good OH. Single failing maxillary tooth in the aesthetic zone (between and including the first premolars). Adjacent and opposing natural dentition. No active infection. Sufficient bone volume to accommodate placement of a single implant with minimum dimensions of 3.3 × 12.0 mm. | A history of smoking or head and neck radiation treatment. Bruxism and/or parafunction. Lack of stable posterior occlusion. In whom primary implant stability could not be achieved |
| Zuiderveld et al., 2018, [41] | ≥18 years of age. Modified plaque and sulcus bleeding index ≤1. Diastema width of ≥6 mm and sufficient inter-occlusal space for a non-occluding provisional restoration. No medical and general contraindications for the surgical procedure. No active and uncontrolled periodontal disease. Buccal socket wall had a bony defect of <5 mm in a vertical direction. | Smokers. Received head neck radiation. Pregnant |
| Systemically Healthy | No Acute Periodontal/Peri-Apical Infection in Area | Intact Tooth Socket or Sufficient Buccal Bone |
|---|---|---|
| Block et al., 2009, [28] | Block et al., 2009, [28] | Block et al., 2009, [28] |
| Cannizzarro et al., 2010, [25] | Cannizzarro et al., 2010, [25] | Cannizzarro et al., 2010, [25] |
| Canullo et al., 2009/2017, [21,22] | Canullo et al., 2009/2017, [21,22] | Canullo et al., 2009/2017, [21,22] |
| Canullo et al., 2010, [29] | Canullo et al., 2010, [29] | Canullo et al., 2010, [29] |
| Cecchinato et al., 2015, [42] | Cecchinato et al., 2015, [42] | Cordaro et al., 2009, [43] |
| Cordaro et al., 2009, [43] | Cordaro et al., 2009, [43] | Crespi et al., 2008, [49] |
| Crespi et al., 2008, [49] | Crespi et al., 2008, [49] | Cucchi et al., 2017, [44] |
| Cucchi et al., 2017, [44] | Cucchi et al., 2017, [44] | De Angelis et al., 2011, [45] |
| De Angelis et al., 2011, [45] | De Angelis et al., 2011, [45] | De Rouck et al., 2009, [30] |
| De Rouck et al., 2009, [30] | De Rouck et al., 2009, [30] | Degidi et al., 2014, [31] |
| Degidi et al., 2014, [31] | Degidi et al., 2014, [31] | Esposito et al., 2015, [32] |
| Esposito et al., 2015, [32] | Esposito et al., 2015, [32] | Felice et al., 2015, [33] |
| Felice et al., 2015, [33] | Felice et al., 2015, [33] | Grandi et al., 2014, [34] |
| Grandi et al., 2014, [34] | Koh et al., 2011, [46] | Migliorati et al., 2015, [35] |
| Koh et al., 2011, [46] | Migliorati et al., 2015, [35] | Pallatella et al., 2008, [37] |
| Migliorati et al., 2015, [35] | Pallatella et al., 2008, [37] | Pieri et al., 2011, [38] |
| Pallatella et al., 2008, [37] | Pieri et al., 2011, [38] | Slagter et al., 2015, [39] |
| Pieri et al., 2011, [38] | Shibly et al., 2012, [27] | Tallarico et al., 2016/2017, [23,24] |
| Prosper et al., 2003, [47] | Tallarico et al., 2016/2017, [23,24] | Urban et al., 2012, [48] |
| Shibly et al., 2012, [27] | Van Nimwegen et al., 2018, [50] | Van Nimwegen et al., 2018, [50] |
| Tallarico et al., 2016/2017, [23,24] | Yoshino et al., 2014, [40] | Yoshino et al., 2014, [40] |
| Urban et al., 2012, [48] | Zuiderveld et al., 2018, [41] | Zuiderveld et al., 2018, [41] |
| Van Nimwegen et al., 2018, [50] | ||
| Zuiderveld et al., 2018, [41] |
| Excluded Smokers | Included Smokers of ≤10 Cigarettes/Day | Included Smokers of >20 Cigarettes a Day | Did Not Exclude or Include Smokers | |
|---|---|---|---|---|
| Van Nimwegen et al., 2018, [50] | Canullo et al., 2009/2017, [21,22] * | Cucchi et al., 2017, [44] | Block et al., 2009, [28] # | |
| Yoshino et al., 2014, [40] * | Canullo et al., 2010, [29] * | Grandi et al., 2014, [34] * | Cannizzaro et al., 2010, [25] # | |
| Zuiderveld et al., 2018, [41] | Cecchinato et al., 2015, [42] | Pieri et al., 2011, [38] | Cordaro et al., 2009, [43] | |
| Crespi et al., 2008, [49] * | De Angelis et al., 2011, [45] | |||
| De Rouck et al., 2009, [30] | Esposito et al., 2015, [32] | |||
| Degidi et al., 2014, [31] * | Felice et al., 2015, [33] | |||
| Koh et al., 2011, [46] | Palattella et al., 2008, [37] * | |||
| Migliorati et al., 2015, [35] * | Prosper et al., 2003, [47] * | |||
| Tallarico et al., 2016/2017, [23,24] * | Shibly et al., 2012, [27] | |||
| Urban et al., 2012, [48] # | Slagter et al., 2015, [39] * | |||
| Survival rate ranges | 96.7–100% | 83.7–100% | 95.5–100% | 40–100% |
| IPL Implants | IPR Implants | IPDL Implants | |
|---|---|---|---|
| Cannizzaro et al., 2010, [25] # | Block et al., 2009, [28] # | Block et al., 2009, [28] #,† | |
| Crespi et al., 2008, [49] * | Cannizzaro et al., 2010, [25] # | Cecchinato et al., 2015, [42] † | |
| Shibly et al., 2012, [27] † | Canullo et al., 2009/2017, [21,22] * | Cordaro et al., 2009, [43] † | |
| Canullo et al., 2010, [29] * | Crespi et al., 2008, [49] * | ||
| De Rouck et al., 2009, [30] † | Cucchi et al., 2017, [44] † | ||
| Degidi et al., 2014, [31] * | De Angelis et al., 2011, [45] † | ||
| Grandi et al., 2014, [34] * | De Rouck et al., 2009, [30] | ||
| Migliorati et al., 2013, [35] * | Koh et al., 2011, [46] † | ||
| Van Nimwegen et al., 2018, [50] † | Prosper et al., 2003, [47] * | ||
| Palatella et al., 2008, [37] * | Shibly et al., 2012, [27] † | ||
| Pieri et al., 2011, [38] † | Slagter et al., 2015, [39] * | ||
| Slagter et al., 2015, [39] * | Tallarico et al., 2016/2017, [23,24] * | ||
| Yoshino et al., 2014, [40] * | Urban et al., 2011, [48] # | ||
| Zuiderveld et al., 2018, [41] † | |||
| Survival rate ranges | 40–100% | 80–100% | |
| Amoxicillin | Amoxicillin with Clavulanic Acid | Antibiotics Used Not Specified | Other Antibiotics Used | Did Not Use Antibiotics |
|---|---|---|---|---|
| Cannizzaro et al., 2010, [25] #,‡ | Canullo et al., 2010, [29] * | Yoshino et al., 2014, [40] * | Block et al., 2009, [28] #,Δ | Cecchinato et al., 2015, [42] † |
| Crespi et al., 2008, [49] * | Canullo et al., 2009/2017, [21,22] * | Urban et al., 2012, [48] #,¶ | Cordaro et al., 2009, [43] † | |
| Cucchi et al., 2017, [44] | Grandi et al., 2014, [34] *,‖ | |||
| De Angelis et al., 2011, [45] ‡ | Palattella et al., 2008, [37] * | |||
| De Rouck et al., 2009, [30] | Pieri et al., 2011, [38] | |||
| Degidi et al., 2014, [31] * | Prosper et al., 2003, [47] * | |||
| Esposito et al., 2015, [32] ‡ | ||||
| Felice et al., 2015, [33] ‡ | ||||
| Koh et al., 2011, [46] § | ||||
| Migliorati et al., 2013, [35] *,‡ | ||||
| Shibly et al., 2012, [27] | ||||
| Slagter et al., 2015, [39] * | ||||
| Tallarico et al., 2016/2017, [23,24] * | ||||
| Van Nimwegen et al., 2018, [50] | ||||
| Zuiderveld et al., 2018, [41] ‡ |
| Used Pre-Operative Antibiotics Only | Used Post-Operative Antibiotics Only | Used Both Pre- and Post-Operative Antibiotics | Only Used Post-Operative Antibiotics When Graft Was Used | |
|---|---|---|---|---|
| Canullo et al., 2010, [29] * | Block et al., 2009, [28] # | Canullo et al., 2009/2017, [21,22] * | Cannizarro et al., 2010, [25] # | |
| Migliorati et al., 2015, [35] * | Palattella et al., 2009, [37] * | Crespi et al., 2008, [49] * | Esposito et al., 2015, [32] | |
| Slagter et al., 2015, [39] * | Prosper et al., 2003, [47] * | Cucchi et al., 2017, [44] | Felice et al., 2015, [33] | |
| Tallarico et al., 2016/2017, [23,24] * | Yoshino et al., 2014, [40] * | De Angelis et al., 2011, [45] | ||
| Urban et al., 2012, [48] # | De Rouck et al., 2008, [30] | |||
| Degidi et al., 2014, [31] * | ||||
| Grandi et al., 2014, [34] * | ||||
| Koh et al., 2011, [46] | ||||
| Pieri et al., 2011, [38] | ||||
| Shibly et al., 2012, [27] | ||||
| Van Nimwegen et al., 2018, [50] | ||||
| Zuiderveld et al., 2018, [41] | ||||
| Survival rate ranges | 87.3–100% | 84.6–100% | 91.3–100% | 40–95.9% |
| Private Practice | University | Non-Specified | |
|---|---|---|---|
| Cannizarro et al., 2010, [25] # | Crespi et al., 2008, [49] * | Block et al., 2009, [28] # | |
| Canullo et al., 2010, [29] *,^ | De Rouck et al., 2008, [30] | Migliorati et al., 2015, [35] * | |
| Canullo et al., 2009/2017, [21,22] *,^ | Koh et al., 2011, [46] | Urban et al., 2012, [48] # | |
| Cecchinato et al., 2015, [42] ^ | Palattella et al., 2008, [37] * | ||
| Cordaro et al., 2009, [43] | Pieri et al., 2011, [38] | ||
| Cucchi et al., 2017, [44] ^ | Prosper et al., 2003, [47] * | ||
| De Angelis et al., 2011, [45] ^ | Shibly et al., 2012, [27] | ||
| Degidi et al., 2014, [31] * | Slagter et al., 2015, [39] * | ||
| Esposito et al., 2015, [32] | Van Nimwegen et al., 2018, [50] | ||
| Felice et al., 2015, [33] | Yoshino et al., 2014, [40] * | ||
| Grandi et al., 2014, [34] *,^ | Zuiderveld et al., 2018, [41] | ||
| Tallarico et al., 2016/2017, [23,24] * | |||
| Survival rate ranges | 40–100% | 92–100% | 84.6–100% |
| No Bone Graft | Xenografts | Mixture of Autograft and Xenograft | Autografts | Allografts | Alloplasts | |
|---|---|---|---|---|---|---|
| Cecchinato et al., 2015, [42] | Canullo et al., 2009/2017, [21,22] | Pieri et al., 2011, [38] | Cannizzaro et al., 2010, [25] | Block et al., 2009, [28] | Canullo et al., 2010, [29] | |
| Cordaro et al., 2009, [43] | De Angelis et al., 2011, [45] | Slagter et al., 2015, [39] | Urban et al., 2012, [48] | Koh et al., 2011, [46] | Cucchi et al., 2017, [44] | |
| Crespi et al., 2008, [49] | De Rouck et al., 2009, [30] | Van Nimwegen et al., 2018, [50] | Zuiderveld et al., 2018, [41] | Shibly et al., 2012, [27] | Prosper et al., 2003, [47] | |
| Degidi et al., 2014, [31] | Esposito et al., 2015, [32] | |||||
| Palattella et al., 2008, [37] | Felice et al., 2015, [33] | |||||
| Grandi et al., 2014, [34] | ||||||
| Migliorati et al., 2015, [35] | ||||||
| Tallarico et al., 2016/2017, [23,24] | ||||||
| Yoshino et al., 2014, [40] | ||||||
| Survival rates | 95–100% | 91.3–100% | 96.7–100% | 40–96.7% | 84.6–96.6% | 95.5–100% |
| Zirconia Implants | Titanium Implants | |||
|---|---|---|---|---|
| Standard Implant | Tapered Implants | Platform-Switching Implants | Wide/Ultra-Wide Diameter Implants | |
| Cannizzaro et al., 2010, [25] # | Cordaro et al., 2009, [43] | Canullo et al., 2009/2017, [21,22] * | Canullo et al., 2009/2017, [21,22] * | |
| De Angelis et al., 2011, [45] | Canullo et al., 2010, [29] * | Canullo et al., 2010, [29] * | ||
| Degidi et al., 2014, [31] * | Cucchi et al., 2017, [44] | Cecchinato et al., 2015, [42] | ||
| De Rouck et al., 2009, [30] | De Angelis et al., 2011, [45] | Felice et al., 2015, [33] | ||
| Esposito et al., 2015, [32] | Grandi et al., 2014, [34] * | Prosper et al., 2003, [47] * | ||
| Grandi et al., 2014, [34] * | Pieri et al., 2011, [38] | Tallarico et al., 2016/2017, [23,24] * | ||
| Koh et al., 2011, [46] | Tallarico et al., 2016/2017, [23,24] * | Urban et al., 2012, [48] # | ||
| Migliorati et al., 2015, [35] * | Yoshino et al., 2014, [40] * | |||
| Palattella et al., 2008, [37] * | ||||
| Survival rate ranges | 40–80% | 91.3–100% | 91.3–100% | 83.7–100% |
| Maxillary Aesthetic Zone (14–24) | Premaxilla (15–25) | Maxillary Anterior (13–23) | Maxillary Posterior | Both Maxilla and Mandible | |
|---|---|---|---|---|---|
| Migliorati et al., 2013, [35] * | Block et al., 2009, [28] †,# | Degidi et al., 2014, [31] * | Pieri et al., 2011, [38] † | Cucchi et al., 2017, [44] *,† | |
| Slagter et al., 2015, [39] * | Canullo et al., 2009/2017, [21,22] * | Palatella et al., 2008, [37] * | Prosper et al., 2003, [47] * | ||
| Van Nimwegen et al., 2018, [50] † | Canullo et al., 2010, [29] * | Tallarico et al., 2016/2017, [23,24] * | |||
| Yoshino et al., 2014, [40] * | Cecchinato et al., 2015, [42] † | Urban et al., 2011, [48] # | |||
| Zuiderveld et al., 2018, [41] † | Crespi et al., 2008, [49] * | Cannizzaro et al., 2010, [25] # | |||
| De Rouck et al., 2009, [30] † | Cordaro et al., 2009, [43] † | ||||
| Esposito et al., 2015, [32] | De Angelis et al., 2011, [45] † | ||||
| Felice et al., 2015, [33] | Shibly et al., 2012, [27] † | ||||
| Grandi et al., 2014, [34] * | |||||
| Koh et al., 2014, [46] † | |||||
| Survival Rate Ranges | 96.7–100% | 84.62–100% | 100% | 97.40% | 40–100% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soegiantho, P.; Suryawinata, P.G.; Tran, W.; Kujan, O.; Koyi, B.; Khzam, N.; Algarves Miranda, L. Survival of Single Immediate Implants and Reasons for Loss: A Systematic Review. Prosthesis 2023, 5, 378-424. https://doi.org/10.3390/prosthesis5020028
Soegiantho P, Suryawinata PG, Tran W, Kujan O, Koyi B, Khzam N, Algarves Miranda L. Survival of Single Immediate Implants and Reasons for Loss: A Systematic Review. Prosthesis. 2023; 5(2):378-424. https://doi.org/10.3390/prosthesis5020028
Chicago/Turabian StyleSoegiantho, Patricia, Patricia Gillian Suryawinata, Wendy Tran, Omar Kujan, Bryar Koyi, Nabil Khzam, and Leticia Algarves Miranda. 2023. "Survival of Single Immediate Implants and Reasons for Loss: A Systematic Review" Prosthesis 5, no. 2: 378-424. https://doi.org/10.3390/prosthesis5020028
APA StyleSoegiantho, P., Suryawinata, P. G., Tran, W., Kujan, O., Koyi, B., Khzam, N., & Algarves Miranda, L. (2023). Survival of Single Immediate Implants and Reasons for Loss: A Systematic Review. Prosthesis, 5(2), 378-424. https://doi.org/10.3390/prosthesis5020028







