Associations among Alcohol Drinking, Smoking, and Nonrestorative Sleep: A Population-Based Study in Japan
Abstract
1. Introduction
2. Results
2.1. Participant Characteristics
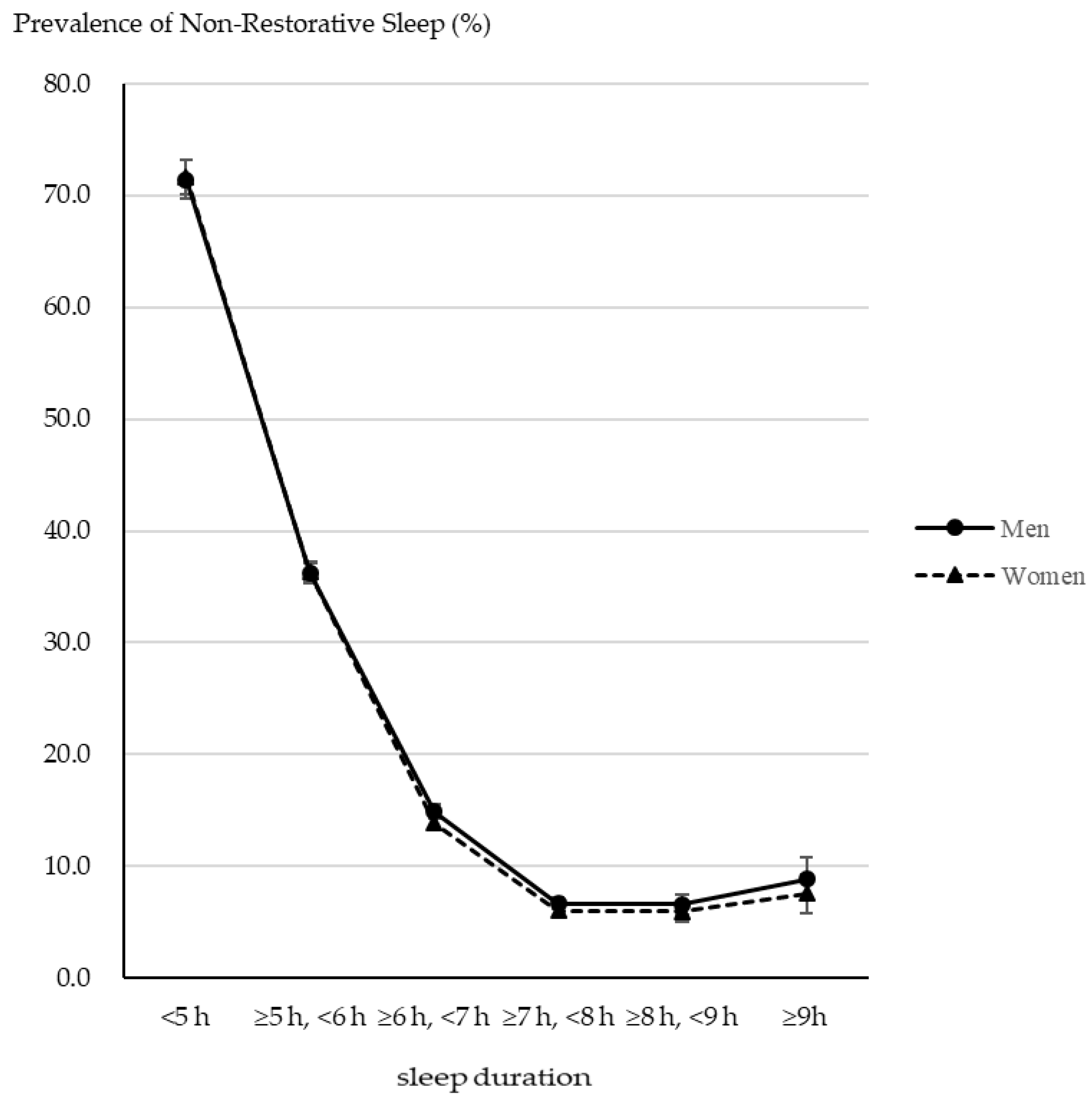
2.2. The Prevalence of NRS
2.3. Associations among Drinking Alcohol, Smoking, and NRS
3. Discussion
4. Material and Methods
4.1. Participants
4.2. Measures
4.2.1. Nonrestorative Sleep
4.2.2. Alcohol Drinking
4.2.3. Smoking
4.3. Covariates
4.4. Statistical Analyses
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wilkinson, K.; Shapiro, C. Nonrestorative sleep: Symptom or unique diagnostic entity? Sleep Med. 2012, 13, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Stone, K.C.; Taylor, D.J.; McCrae, C.S.; Kalsekar, A.; Lichstein, K.L. Nonrestorative sleep. Sleep Med. Rev. 2008, 12, 275–288. [Google Scholar] [CrossRef] [PubMed]
- Ohayon, M.M. Prevalence and correlates of nonrestorative sleep complaints. Arch. Intern. Med. 2005, 165, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Sarsour, K.; Van Brunt, D.L.; Johnston, J.A.; Foley, K.A.; Morin, C.M.; Walsh, J.K. Associations of nonrestorative sleep with insomnia, depression, and daytime function. Sleep Med. 2010, 11, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Wakasugi, M.; Kazama, J.J.; Narita, I.; Iseki, K.; Moriyama, T.; Yamagata, K.; Fujimoto, S.; Tsuruya, K.; Asahi, K.; Konta, T.; et al. Association between Combined Lifestyle Factors and Non-Restorative Sleep in Japan: A Cross-Sectional Study Based on a Japanese Health Database. PLoS ONE 2014, 9, e108718. [Google Scholar]
- Matsumoto, T.; Chin, K. Prevalence of sleep disturbances: Sleep disordered breathing, short sleep duration, and non-restorative sleep. Respir. Investig. 2019, 57, 227–237. [Google Scholar] [CrossRef]
- Vernon, M.K.; Dugar, A.; Revicki, D.; Treglia, M.; Buysse, D. Measurement of non-restorative sleep in insomnia: A review of the literature. Sleep Med. Rev. 2010, 14, 205–212. [Google Scholar] [CrossRef]
- Roth, T.; Zammit, G.; Lankford, A.; Mayleben, D.; Stern, T.; Pitman, V.; Clark, D.; Werth, J.L. Nonrestorative sleep as a distinct component of insomnia. Sleep 2010, 33, 449–458. [Google Scholar] [CrossRef]
- Tinajero, R.; Williams, P.G.; Cribbet, M.R.; Rau, H.K.; Bride, D.L.; Suchy, Y. Nonrestorative sleep in healthy, young adults without insomnia: Associations with executive functioning, fatigue, and pre-sleep arousal. Sleep Health 2018, 4, 284–291. [Google Scholar] [CrossRef]
- Okamoto, M.; Kobayashi, Y.; Nakamura, F.; Musha, T. Association between nonrestorative sleep and risk of diabetes: A cross-sectional study. Behav. Sleep Med. 2017, 15, 483–490. [Google Scholar] [CrossRef]
- Saitoh, K.; Yoshiike, T.; Kaneko, Y.; Utsumi, T.; Matsui, K.; Nagao, K.; Otsuki, R.; Aritake-Okada, S.; Kadotani, H.; Kuriyama, K.; et al. Associations of nonrestorative sleep and insomnia symptoms with incident depressive symptoms over 1–2 years: Longitudinal results from the Hispanic Community Health Study/Study of Latinos and Sueño Ancillary Study. Depress. Anxiety 2022, 39, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Yoshiike, T.; Utsumi, T.; Matsui, K.; Nagao, K.; Saitoh, K.; Otsuki, R.; Aritake-Okada, S.; Suzuki, M.; Kuriyama, K. Mortality associated with nonrestorative short sleep or nonrestorative long time-in-bed in middle-aged and older adults. Sci. Rep. 2022, 12, 189. [Google Scholar] [CrossRef] [PubMed]
- Hu, N.; Ma, Y.; He, J.; Zhu, L.; Cao, S. Alcohol consumption and incidence of sleep disorder: A systematic review and meta-analysis of cohort studies. Drug Alcohol Depend. 2020, 217, 108259. [Google Scholar] [CrossRef]
- Ohayon, M.M.; Bader, G. Prevalence and correlates of insomnia in the Swedish population aged 19–75 years. Sleep Med. 2010, 11, 980–986. [Google Scholar] [CrossRef] [PubMed]
- Phillips, B.; Mannino, D. Correlates of sleep complaints in adults: The ARIC Study. J. Clin. Sleep Med. 2005, 1, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Amiri, S.; Behnezhad, S. Smoking and risk of sleep-related issues: A systematic review and meta-analysis of prospective studies. Can. J. Public Health 2020, 111, 775–786. [Google Scholar] [CrossRef] [PubMed]
- Wetter, D.; Young, T. The Relation Between Cigarette Smoking and Sleep Disturbance. Prev. Med. 1994, 23, 328–334. [Google Scholar] [CrossRef]
- Matsumoto, T.; Tabara, Y.; Murase, K.; Takahashi, Y.; Setoh, K.; Kawaguchi, T.; Muro, S.; Kadotani, H.; Kosugi, S.; Sekine, A.; et al. Combined association of clinical and lifestyle factors with non-restorative sleep: The Nagahama Study. PLoS ONE 2017, 12, e0171849. [Google Scholar] [CrossRef]
- Tomioka, K.; Kurumatani, N.; Saeki, K. The association between education and smoking prevalence, independent of occupation: A nationally representative survey in Japan. J. Epidemiol. 2020, 30, 136–142. [Google Scholar] [CrossRef]
- Kinjo, A.; Purevdorj, B.; Okada, T.; Kuwabara, Y.; Fujii, M.; Higuchi, S.; Osaki, Y. Trends and differences in alcohol-related mortality rates by gender and by prefectures in Japan between 1995 and 2016. Drug Alcohol Depend. 2021, 221, 108586. [Google Scholar] [CrossRef]
- Kim, B.S.; Jeon, H.J.; Hong, J.P.; Bae, J.N.; Lee, J.Y.; Chang, S.M.; Lee, Y.M.; Son, J.; Cho, M.J. DSM-IV psychiatric comorbidity according to symptoms of insomnia: A nationwide sample of Korean adults. Soc. Psychiatry Psychiatr. Epidemiol. 2012, 47, 2019–2033. [Google Scholar] [CrossRef] [PubMed]
- Ohayon, M.M.; Hong, S.C. Prevalence of insomnia and associated factors in South Korea. J. Psychosom. Res. 2002, 53, 593–600. [Google Scholar] [CrossRef]
- Arnedt, J.T.; Rohsenow, D.J.; Almeida, A.B.; Hunt, S.K.; Gokhale, M.; Gottlieb, D.J.; Howland, J. Sleep following alcohol intoxication in healthy, young adults: Effects of sex and family history of alcoholism. Alcohol. Clin. Exp. Res. 2011, 35, 870–878. [Google Scholar] [CrossRef]
- Roehrs, T.; Roth, T. Sleep, sleepiness, sleep disorders and alcohol use and abuse. Sleep Med. Rev. 2001, 5, 287–297. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumi, W.; Miyazaki, S.; Itasaka, Y.; Togawa, K. Influence of alcohol on respiratory disturbance during sleep. Psychiatry Clin. Neurosci. 2000, 54, 332–333. [Google Scholar] [CrossRef] [PubMed]
- Jaehne, A.; Unbehaun, T.; Feige, B.; Lutz, U.C.; Batra, A.; Riemann, D. How smoking affects sleep: A polysomnographical analysis. Sleep Med. 2012, 13, 1286–1292. [Google Scholar] [CrossRef]
- Nakata, A.; Takahashi, M.; Haratani, T.; Ikeda, T.; Hojou, M.; Fujioka, Y.; Araki, S. Association of active and passive smoking with sleep disturbances and short sleep duration among Japanese working population. Int. J. Behav. Med. 2008, 15, 81. [Google Scholar] [CrossRef]
- Franklin, K.A.; Holmgren, P.A.; Jonsson, F.; Poromaa, N.; Stenlund, H.; Svanborg, E. Snoring, pregnancy-induced hypertension, and growth retardation of the fetus. Chest 2000, 117, 137–141. [Google Scholar] [CrossRef]
- Franklin, K.A.; Gislason, T.; Omenaas, E.; Jõgi, R.; Jensen, E.J.; Lindberg, E.; Gunnbjörnsdóttir, M.; Nyström, L.; Laerum, B.N.; Björnsson, E. The influence of active and passive smoking on habitual snoring. Am. J. Respir. Crit. Care Med. 2004, 170, 799–803. [Google Scholar] [CrossRef]
- Zhang, L.; Samet, J.; Caffo, B.; Punjabi, N.M. Cigarette smoking and nocturnal sleep architecture. Am. J. Epidemiol. 2006, 164, 529–537. [Google Scholar] [CrossRef]
- Wilkinson, K.; Shapiro, C. Development and validation of the Nonrestorative Sleep Scale (NRSS). J. Clin. Sleep Med. 2013, 9, 929–937. [Google Scholar] [CrossRef]
- Drake, C.L.; Hays, R.D.; Morlock, R.; Wang, F.; Shikiar, R.; Frank, L.; Downey, R.; Roth, T. Development and evaluation of a measure to assess restorative sleep. J. Clin. Sleep Med. 2014, 10, 733–741. [Google Scholar] [CrossRef]
- Hasan, A.; Uzma, N.; Swamy, T.L.; Shoba, A.; Kumar, B.S. Correlation of clinical profiles with obstructive sleep apnea and metabolic syndrome. Sleep Breath 2012, 16, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare. The Comprehensive Survey of Living Conditions. Available online: https://www.mhlw.go.jp/toukei/list/20-21kekka.html (accessed on 25 May 2022).
- Pierce, J.P.; Messer, K.; White, M.M.; Cowling, D.W.; Thomas, D.P. Prevalence of heavy smoking in California and the United States, 1965–2007. JAMA 2011, 305, 1106–1112. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.-L.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef] [PubMed]
- Sakurai, K.; Nishi, A.; Kondo, K.; Yanagida, K.; Kawakami, N. Screening performance of K6/K10 and other screening instruments for mood and anxiety disorders in Japan. Psychiatry Clin. Neurosci. 2011, 65, 434–441. [Google Scholar] [CrossRef]
- Kessler, R.C.; Barker, P.R.; Colpe, L.J.; Epstein, J.F.; Gfroerer, J.C.; Hiripi, E.; Howes, M.J.; Normand, S.L.; Manderscheid, R.W.; Walters, E.E.; et al. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry 2003, 60, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, T.A.; Kawakami, N.; Saitoh, M.; Ono, Y.; Nakane, Y.; Nakamura, Y.; Tachimori, H.; Iwata, N.; Uda, H.; Nakane, H.; et al. The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int. J. Methods Psychiatr. Res. 2008, 17, 152–158. [Google Scholar] [CrossRef]
- Vgontzas, A.N.; Liao, D.; Pejovic, S.; Calhoun, S.; Karataraki, M.; Basta, M.; Fernandez-Mendoza, J.; Bixler, E.O. Insomnia with short sleep duration and mortality: The Penn State cohort. Sleep 2010, 33, 1159–1164. [Google Scholar] [CrossRef]
- Cappuccio, F.P.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Sleep duration and all-cause mortality: A systematic review and meta-analysis of prospective studies. Sleep 2010, 33, 585–592. [Google Scholar] [CrossRef]
- United Nations Educational, Scientific and Cultural Organization (UNESCO). International Standard Classification of Education ISCED 2011; UNESCO Institute for Statistic: Montreal, QC, Canada, 2012. [Google Scholar]
- Verplaetse, T.L.; McKee, S.A. An overview of alcohol and tobacco/nicotine interactions in the human laboratory. Am. J. Drug Alcohol Abus. 2017, 43, 186–196. [Google Scholar] [CrossRef] [PubMed]
| Men (N = 35,717) | Women (N = 39,911) | ||||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Age class | |||||
| 20–29 | 4013 | 11.2 | 4122 | 10.3 | |
| 30–39 | 5729 | 16.0 | 6005 | 15.1 | |
| 40–49 | 6362 | 17.8 | 6703 | 16.8 | |
| 50–59 | 5787 | 16.2 | 6140 | 15.4 | |
| 60–69 | 6971 | 19.5 | 7565 | 19.0 | |
| 70–79 | 4880 | 13.7 | 5901 | 14.8 | |
| 80+ | 1975 | 5.5 | 3475 | 8.7 | |
| Alcohol | |||||
| None | 14,157 | 39.6 | 28,191 | 70.6 | |
| ≥0, <23 g | 10,507 | 29.4 | 8539 | 21.4 | |
| ≥23, <46 g | 6379 | 17.9 | 1875 | 4.7 | |
| ≥46, <69 g (men) ≥46 g (women) | 2713 | 7.6 | 915 | 2.3 | |
| ≥69 g (men) | 1591 | 4.5 | - | - | |
| Missing | 370 | 1.0 | 391 | 1.0 | |
| Smoking | |||||
| Non-smoker | 23,368 | 65.4 | 35,386 | 84.1 | |
| Light smoker | 9546 | 26.7 | 3771 | 9.0 | |
| Heavy smoker | 2460 | 6.9 | 405 | 1.0 | |
| Missing | 343 | 1.0 | 349 | 0.8 | |
| Mental distress | |||||
| Light | 25,097 | 70.3 | 26,058 | 65.3 | |
| Moderate | 8027 | 22.5 | 10,262 | 25.7 | |
| Serious | 1281 | 3.6 | 1788 | 4.5 | |
| Missing | 1312 | 3.7 | 1803 | 4.5 | |
| Health behavior | |||||
| Eating regular meals | 17,996 | 50.4 | 23,345 | 58.5 | |
| Moderately exercising | 13,527 | 37.9 | 13,492 | 33.8 | |
| Marital status | |||||
| Unmarried | 10,898 | 30.5 | 15,085 | 37.8 | |
| Married | 24,819 | 69.5 | 24,826 | 62.2 | |
| Education class | |||||
| Low | 4613 | 12.9 | 5994 | 15.0 | |
| Middle | 15,810 | 44.3 | 19,403 | 48.6 | |
| High | 11,263 | 31.5 | 9902 | 24.8 | |
| Missing | 4031 | 11.3 | 4612 | 11.6 | |
| Men (N = 35,717) | Women (N = 39,911) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | 95%CI | p-Value | % | 95%CI | p-Value | |||||
| Total | 22.2 | 21.8 | - | 22.7 | 23.4 | 23.0 | - | 23.8 | ||
| Age class | ||||||||||
| 20–29 | 24.1 | 22.8 | - | 25.4 | <0.001 | 23.7 | 22.4 | - | 25.1 | <0.001 |
| 30–39 | 29.3 | 28.2 | - | 30.5 | 27.9 | 26.8 | - | 29.1 | ||
| 40–49 | 31.2 | 30.0 | - | 32.3 | 33.5 | 32.3 | - | 34.6 | ||
| 50–59 | 25.6 | 24.5 | - | 26.8 | 29.8 | 28.7 | - | 31.0 | ||
| 60–69 | 14.7 | 13.9 | - | 15.6 | 17.3 | 16.5 | - | 18.2 | ||
| 70–79 | 11.8 | 11.0 | - | 12.8 | 14.3 | 13.4 | - | 15.2 | ||
| 80+ | 11.0 | 9.7 | - | 12.5 | 13.3 | 12.2 | - | 14.5 | ||
| Alcohol/day | ||||||||||
| None | 22.5 | 21.8 | - | 23.2 | <0.001 | 22.6 | 22.1 | - | 23.1 | <0.001 |
| ≥0, <23 g | 22.5 | 21.7 | - | 23.3 | 24.6 | 23.7 | - | 25.5 | ||
| ≥23, <46 g | 19.9 | 19.0 | - | 20.9 | 26.3 | 24.4 | - | 28.4 | ||
| ≥46, <69 g (men) ≥ 46 g (women) | 22.0 | 20.5 | - | 23.7 | 32.8 | 29.8 | - | 35.9 | ||
| ≥69 g (men) | 28.6 | 26.4 | - | 30.9 | ||||||
| Smoking | ||||||||||
| Non-smoker | 21.1 | 20.5 | - | 21.6 | <0.001 | 22.5 | 22.1 | - | 23.0 | <0.001 |
| Light smoker | 23.7 | 22.8 | - | 24.6 | 31.0 | 29.5 | - | 32.5 | ||
| Heavy smoker | 27.9 | 26.2 | - | 29.7 | 35.8 | 31.1 | - | 40.7 | ||
| Mental distress | ||||||||||
| Light | 15.5 | 15.1 | - | 16.0 | <0.001 | 15.8 | 15.4 | - | 16.3 | <0.001 |
| Moderate | 36.6 | 35.6 | - | 37.7 | 36.9 | 35.9 | - | 37.8 | ||
| Serious | 61.6 | 58.9 | - | 64.3 | 58.4 | 56.1 | - | 60.7 | ||
| Model 1 (N = 35,129) | Model 2 (N = 33,903) | Model 3 (N = 30,424) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | ||||||||
| Alcohol/day (ref non-alcohol drink) | ||||||||||||||||
| ≥0, <23 g | 1.02 | 0.95 | - | 1.10 | 0.565 | 1.08 | 0.99 | - | 1.17 | 0.104 | 1.02 | 0.93 | - | 1.12 | 0.735 | |
| ≥23, <46 g | 0.91 | 0.83 | - | 1.00 | 0.055 | 1.04 | 0.93 | - | 1.16 | 0.505 | 0.96 | 0.86 | - | 1.08 | 0.525 | |
| ≥46, <69 g | 1.12 | 0.98 | - | 1.29 | 0.097 | 1.21 | 1.03 | - | 1.42 | 0.019 | 1.08 | 0.91 | - | 1.28 | 0.384 | |
| ≥69 g | 1.43 | 1.20 | - | 1.69 | <0.001 | 1.38 | 1.12 | - | 1.70 | 0.002 | 1.31 | 1.05 | - | 1.63 | 0.015 | |
| Smoking (ref non-smoker) | ||||||||||||||||
| Light smoker | 1.05 | 0.95 | - | 1.15 | 0.350 | 0.96 | 0.86 | - | 1.08 | 0.500 | 0.97 | 0.87 | - | 1.10 | 0.668 | |
| Heavy smoker | 1.59 | 1.36 | - | 1.87 | <0.001 | 1.13 | 0.94 | - | 1.37 | 0.199 | 1.14 | 0.94 | - | 1.40 | 0.191 | |
| Model 1 (N = 39,333) | Model 2 (N = 37,652) | Model 3 (N = 33,695) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | ||||||||
| Alcohol/day (ref non-alcohol drink) | ||||||||||||||||
| ≥0, <23 g | 1.01 | 0.95 | - | 1.07 | 0.814 | 0.96 | 0.89 | - | 1.03 | 0.238 | 0.95 | 0.88 | - | 1.02 | 0.170 | |
| ≥23, <46 g | 1.12 | 0.98 | - | 1.26 | 0.088 | 1.11 | 0.96 | - | 1.29 | 0.152 | 1.11 | 0.95 | - | 1.29 | 0.201 | |
| ≥46 g | 1.47 | 1.22 | - | 1.78 | <0.001 | 1.44 | 1.14 | - | 1.82 | 0.002 | 1.36 | 1.06 | - | 1.73 | 0.014 | |
| Smoking (ref non-smoker) | ||||||||||||||||
| Light smoker | 1.41 | 1.28 | - | 1.56 | <0.001 | 1.02 | 0.90 | - | 1.15 | 0.741 | 1.04 | 0.91 | - | 1.18 | 0.587 | |
| Heavy smoker | 2.14 | 1.61 | - | 2.84 | <0.001 | 0.95 | 0.66 | - | 1.37 | 0.782 | 1.08 | 0.72 | - | 1.60 | 0.720 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Otsuka, Y.; Takeshima, O.; Itani, O.; Matsumoto, Y.; Kaneita, Y. Associations among Alcohol Drinking, Smoking, and Nonrestorative Sleep: A Population-Based Study in Japan. Clocks & Sleep 2022, 4, 595-606. https://doi.org/10.3390/clockssleep4040046
Otsuka Y, Takeshima O, Itani O, Matsumoto Y, Kaneita Y. Associations among Alcohol Drinking, Smoking, and Nonrestorative Sleep: A Population-Based Study in Japan. Clocks & Sleep. 2022; 4(4):595-606. https://doi.org/10.3390/clockssleep4040046
Chicago/Turabian StyleOtsuka, Yuichiro, Ohki Takeshima, Osamu Itani, Yuuki Matsumoto, and Yoshitaka Kaneita. 2022. "Associations among Alcohol Drinking, Smoking, and Nonrestorative Sleep: A Population-Based Study in Japan" Clocks & Sleep 4, no. 4: 595-606. https://doi.org/10.3390/clockssleep4040046
APA StyleOtsuka, Y., Takeshima, O., Itani, O., Matsumoto, Y., & Kaneita, Y. (2022). Associations among Alcohol Drinking, Smoking, and Nonrestorative Sleep: A Population-Based Study in Japan. Clocks & Sleep, 4(4), 595-606. https://doi.org/10.3390/clockssleep4040046





