Blood Lead Levels and Subsequence Risk of Malaria in the African Population: A Systematic Review and Meta-Analysis
Abstract
:1. Background
2. Methods
2.1. Protocol and Search Strategy
2.2. Eligibility Criteria
2.3. Study Selection and Data Extraction
2.4. Quality of the Included Studies
2.5. Data Syntheses
3. Results
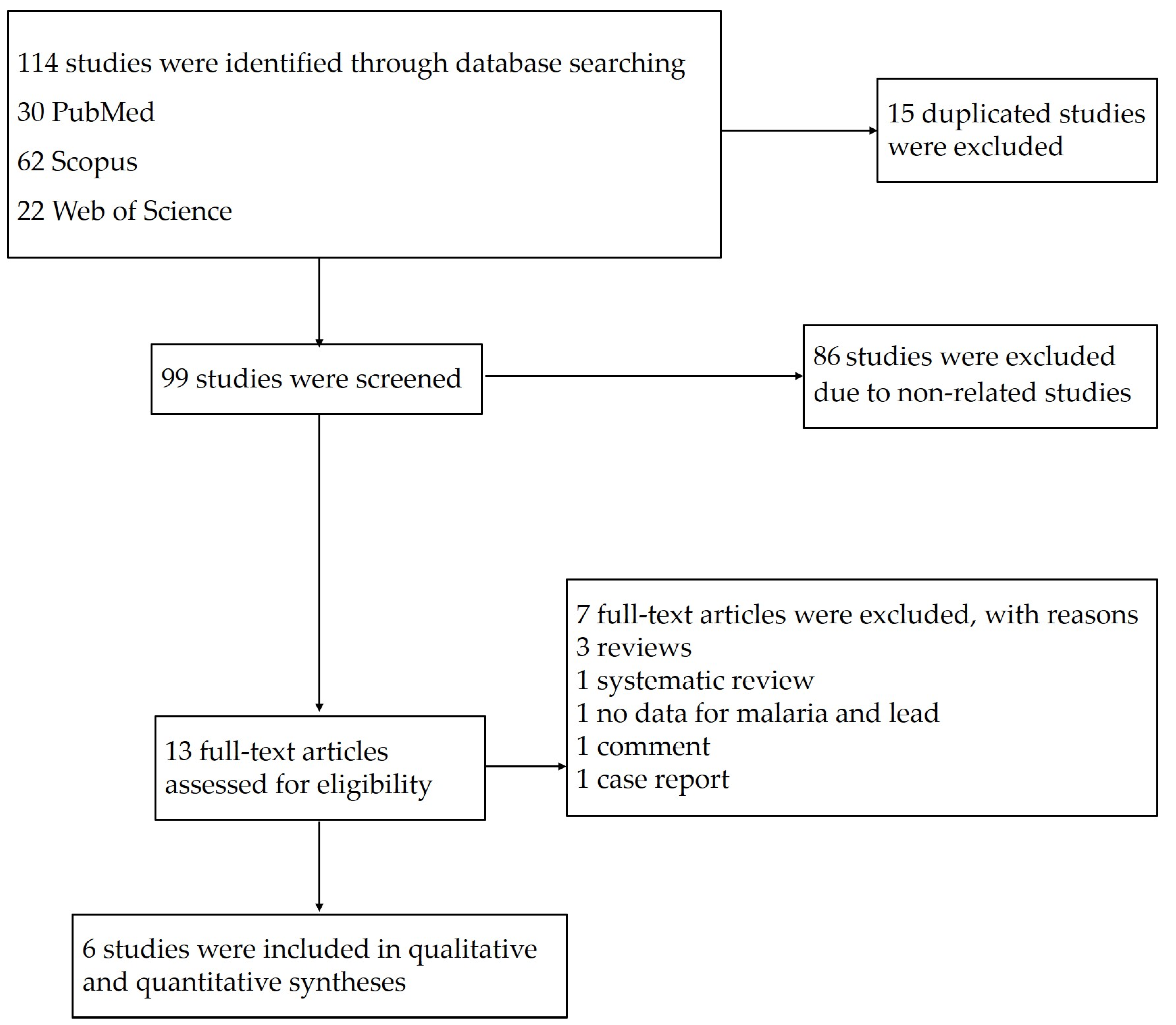
3.1. Search Results
3.2. Characteristics of the Included Studies
3.3. Mean BLL of Participants Enrolled in the Included Studies
3.4. Prevalence of Malaria among Participants
3.5. BLL and Risk of Malaria Infection
3.6. BLL and Risk of Severe Malaria
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Obeng-Gyasi, E. Sources of lead exposure in various countries. Rev. Environ. Health 2019, 34, 25–34. [Google Scholar] [CrossRef]
- Prathumratana, L.; Kim, R.; Kim, K.W. Lead contamination of the mining and smelting district in Mitrovica, Kosovo. Environ. Geochem. Health 2020, 42, 1033–1044. [Google Scholar] [CrossRef] [PubMed]
- Hore, P.; Alex-Oni, K.; Sedlar, S.; Nagin, D. A spoonful of lead: A 10-year look at spices as a potential source of lead exposure. J. Publ. Health Manag. Pract. 2019, 25, S63–S70. [Google Scholar] [CrossRef]
- Vlasak, T.; Jordakieva, G.; Gnambs, T.; Augner, C.; Crevenna, R.; Winker, R.; Barth, A. Blood lead levels and cognitive functioning: A meta-analysis. Sci. Total Environ. 2019, 668, 678–684. [Google Scholar] [CrossRef] [PubMed]
- Hertz-Picciotto, I.; Croft, J. Review of the relation between blood lead and blood pressure. Epidemiol. Rev. 1993, 15, 352–373. [Google Scholar] [CrossRef]
- Nowack, R.; Wiecek, A.; Ritz, E. Lead and hypertension. Contrib. Nephrol. 1992, 100, 25–34. [Google Scholar]
- Kuraeiad, S.; Kotepui, M. Blood lead level and renal impairment among adults: A meta-analysis. Int. J. Environ. Res. Publ. Health 2021, 18, 4147. [Google Scholar] [CrossRef]
- Landrigan, P.J.; Boffetta, P.; Apostoli, P. The reproductive toxicity and carcinogenicity of lead: A critical review. Am. J. Ind. Med. 2000, 38, 231–243. [Google Scholar] [CrossRef]
- Rahman, A.; Rao, M.S.; Khan, K.M. Intraventricular infusion of quinolinic acid impairs spatial learning and memory in young rats: A novel mechanism of lead-induced neurotoxicity. J. Neuroinflamm. 2018, 15, 263. [Google Scholar] [CrossRef] [PubMed]
- Silbergeld, E.K.; Waalkes, M.; Rice, J.M. Lead as a carcinogen: Experimental evidence and mechanisms of action. Am. J. Ind. Med. 2000, 38, 316–323. [Google Scholar] [CrossRef]
- Ugwuja, E.I.; Ejikeme, B.; Obuna, J.A. Impacts of elevated prenatal blood lead on trace element status and pregnancy outcomes in occupationally non-exposed women. Int. J. Occup. Med. Environ. Health 2011, 2, 143–156. [Google Scholar]
- Mahittikorn, A.; Masangkay, F.R.; Kotepui, K.U.; Milanez, G.J.; Kotepui, M. Comparison of Plasmodium ovale curtisi and Plasmodium ovale wallikeri infections by a meta-analysis approach. Sci. Rep. 2021, 11, 6409. [Google Scholar] [CrossRef] [PubMed]
- Lalremruata, A.; Magris, M.; Vivas-Martinez, S.; Koehler, M.; Esen, M.; Kempaiah, P.; Metzger, W.G. Natural infection of Plasmodium brasilianum in humans: Man and monkey share quartan malaria parasites in the Venezuelan Amazon. EBioMed. 2015, 2, 1186–1192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kotepui, M.; Masangkay, F.R.; Kotepui, K.U.; Milanez, G.J. Preliminary review on the prevalence, proportion, geographical distribution, and characteristics of naturally acquired Plasmodium cynomolgi infection in mosquitoes, macaques, and humans: A systematic review and meta-analysis. BMC Infect. Dis. 2021, 21, 259. [Google Scholar] [CrossRef]
- Kotepui, M.; Kotepui, K.U.; Milanez, G.J.; Masangkay, F.R. Prevalence and risk factors related to poor outcome of patients with severe Plasmodium vivax infection: A systematic review, meta-analysis, and analysis of case reports. BBMC Infect. Dis. 2020, 20, 363. [Google Scholar] [CrossRef]
- Kotepui, M.; Kotepui, K.U.; Milanez, G.D.; Masangkay, F.R. Prevalence of severe Plasmodium knowlesi infection and risk factors related to severe complications compared with non-severe P. knowlesi and severe P. falciparum malaria: A systematic review and meta-analysis. Infect. Dis. Poverty 2020, 9, 106. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Malaria Report 2020. Available online: https://www.who.int/publications/i/item/9789240015791 (accessed on 30 May 2021).
- Moya-Alvarez, V.; Mireku, M.O.; Ayotte, P.; Cot, M.; Bodeau-Livinec, F. Elevated blood lead levels are associated with reduced risk of malaria in Beninese infants. PLoS ONE 2016, 11, e0149049. [Google Scholar] [CrossRef] [Green Version]
- Nriagu, J.; Afeiche, M.; Linder, A.; Arowolo, T.; Ana, G.; Sridhar, M.K.; Adesina, A. Lead poisoning associated with malaria in children of urban areas of Nigeria. Int. J. Hyg. Environ. Health 2008, 211, 591–605. [Google Scholar] [CrossRef]
- Greig, J.; Thurtle, N.; Cooney, L.; Ariti, C.; Ahmed, A.O.; Ashagre, T.; Dargan, P.I. Association of blood lead level with neurological features in 972 children affected by an acute severe lead poisoning outbreak in Zamfara State, northern Nigeria. PLoS ONE 2014, 9, e93716. [Google Scholar] [CrossRef] [PubMed]
- Mukisa, A.; Kasozi, D.; Aguttu, C.; Vuzi, P.C.; Kyambadde, J. Relationship between blood Lead status and anemia in Ugandan children with malaria infection. BMC Pediatr. 2020, 20, 521. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moola, S.M.Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Qureshi, R.; Mattis, P.; Lisy, K.; Mu, P.-F. Chapter 7: Systematic Reviews of Etiology and Risk JBI; 2020. Available online: https://synthesismanual.jbi.global (accessed on 30 May 2021).
- Garrison, A.; Khoshnood, B.; Courtin, D.; Milet, J.; Garcia, A.; Massougbodji, A.; Bodeau-Livinec, F. Blood lead level in infants and subsequent risk of malaria: A prospective cohort study in Benin, Sub-Saharan Africa. PLoS ONE 2019, 14, e0220023. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Varshavsky, J.; Smith, A.; Wang, A.; Hom, E.; Izano, M.; Huang, H.; Woodruff, T.J. Heightened susceptibility: A review of how pregnancy and chemical exposures influence maternal health. Reprod. Toxicol. 2020, 92, 14–56. [Google Scholar] [CrossRef] [PubMed]
- Heo, Y.; Parsons, P.J.; Lawrence, D.A. Lead differentially modifies cytokine production in vitro and in vivo. Toxicol. Appl. Pharmacol. 1996, 138, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Lynes, M.A.; Fontenot, A.P.; Lawrence, D.A.; Rosenspire, A.J.; Pollard, K.M. Gene expression influences on metal immunomodulation. Toxicol. Appl. Pharmacol. 2006, 210, 9–16. [Google Scholar] [CrossRef]
- Kwong, W.T.; Friello, P.; Semba, R.D. Interactions between iron deficiency and lead poisoning: Epidemiology and pathogenesis. Sci. Total Environ. 2004, 330, 21–37. [Google Scholar] [CrossRef] [PubMed]
- Bayoumi, R.A. Does the mechanism of protection from falciparum malaria by red cell genetic disorders involve a switch to a balanced TH1/TH2 cytokine production mode? Med. Hypotheses 1997, 48, 11–17. [Google Scholar] [CrossRef]
- Maizels, R.M.; Balic, A.; Gomez-Escobar, N.; Nair, M.; Taylor, M.D.; Allen, J.E. Helminth parasites-masters of regulation. Immunol Rev. 2004, 201, 89–116. [Google Scholar] [CrossRef] [PubMed]
- Graziano, J.H.; Slavkovic, V.; Factor-Litvak, P.; Popovac, D.; Ahmedi, X.; Mehmeti, A. Depressed serum erythropoietin in pregnant women with elevated blood lead. Archives of environmental health. 1991, 46, 347–350. [Google Scholar] [CrossRef] [PubMed]
- Bouharoun-Tayoun, H.; Druilhe, P. Plasmodium falciparum malaria: Evidence for an isotype imbalance which may be responsible for delayed acquisition of protective immunity. Infect. Immun. 1992, 60, 1473–1481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
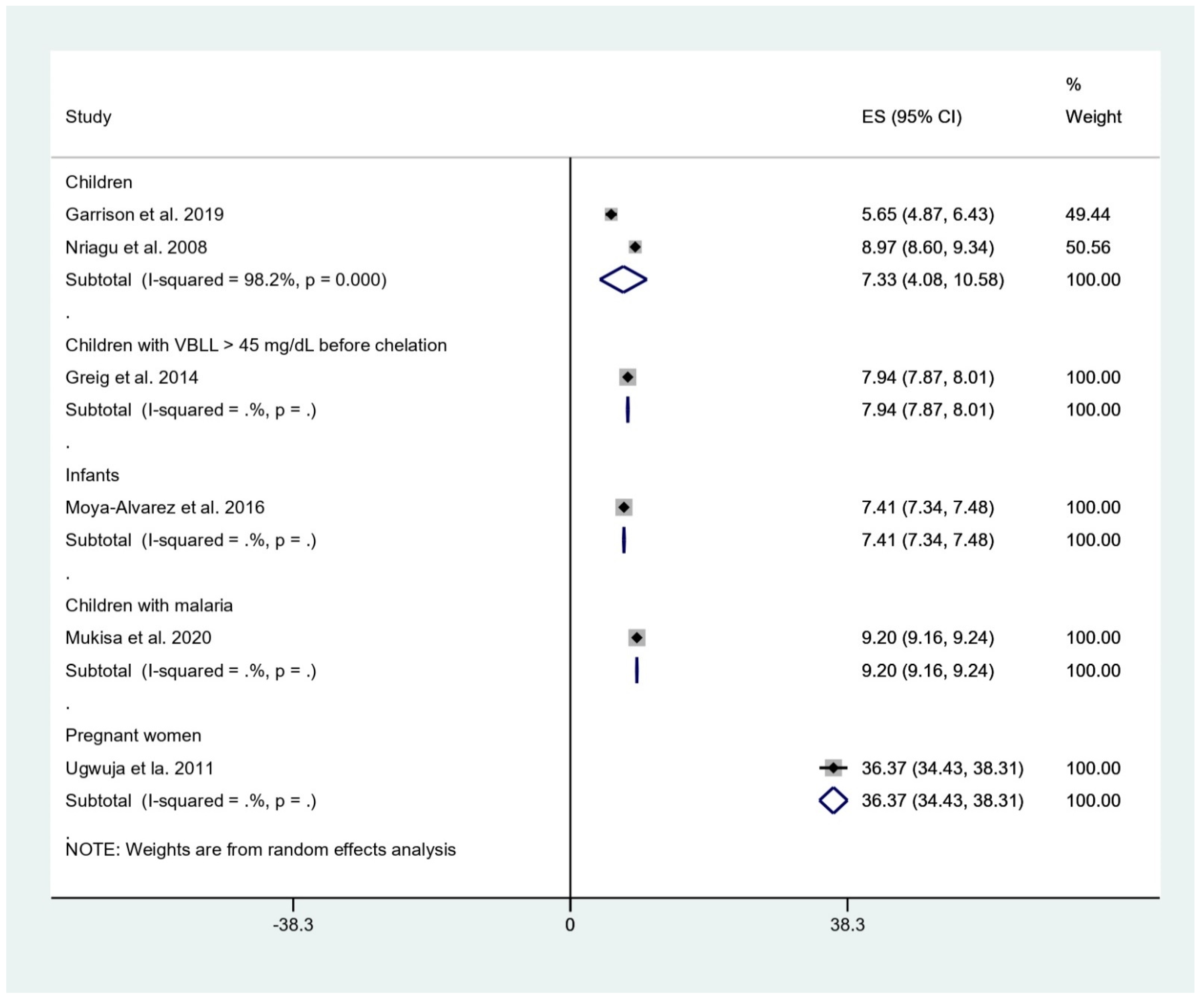
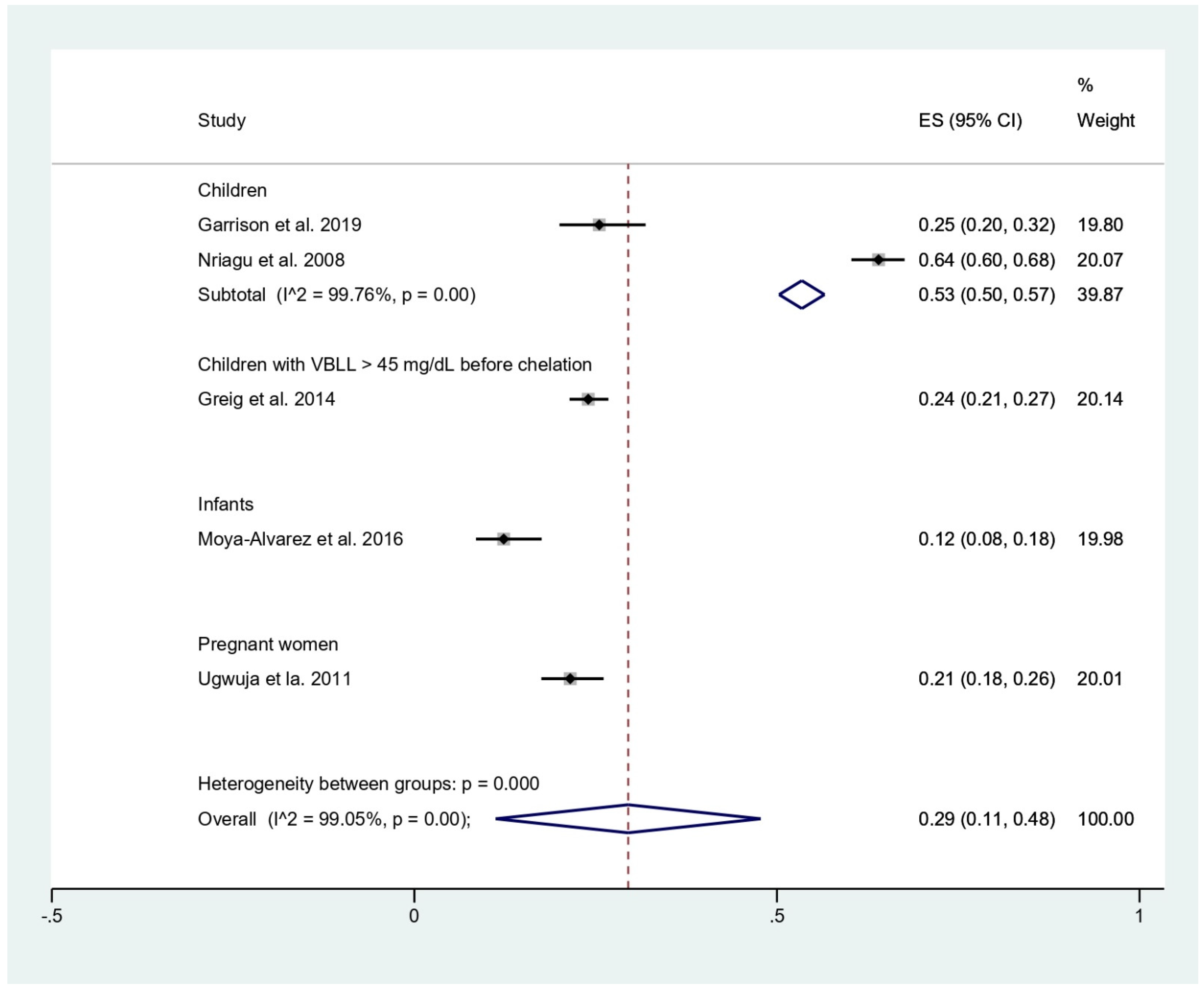
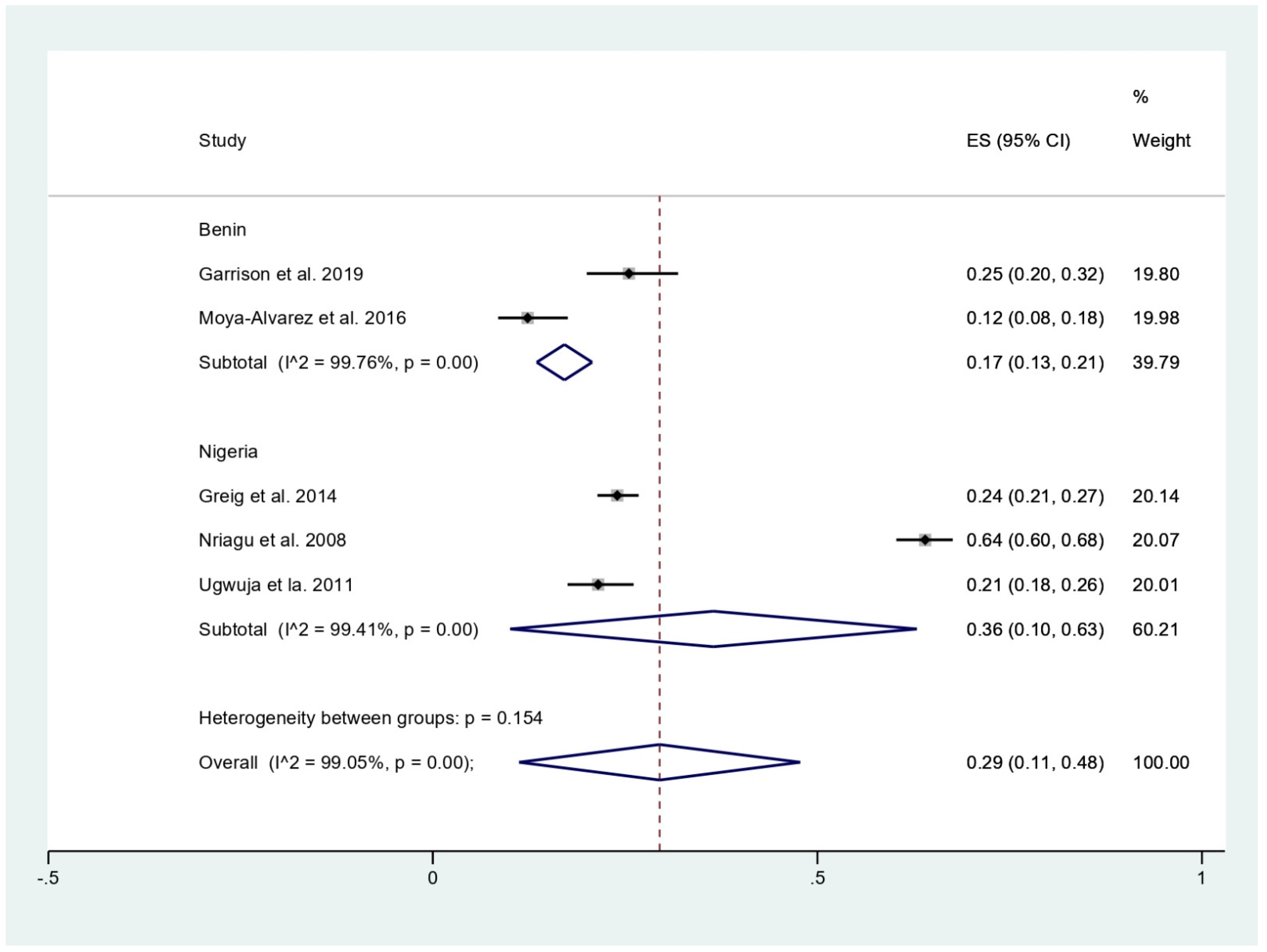
| Author | Study Site | Year of Conduction | Study Design | Number of Participants | Participants | Age Range (Years) | Male % | Research Questions | Mean ± SD BLL (μg/dL) | Number of Malaria | Outcomes | Outcome Parameters | Test for Malaria | Test for BLL |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Garrison et al., 2019 | Benin | 2008–2013 | Cohort study | 204 | Children | 1–2 | 51 | BLL and malaria | 5.65 ± 5.683 | 52 | No association between BLL and malaria | IRR of BLL in 4th quartile and malaria, 0.94 (95%CI, 0.68, 1.30, p = 0.7) | Microscopy, RDT | Mass spectrometry |
| Greig et al., 2014 | Nigeria | 2010–2011 | Prospective observational study | 972 | Children with VBLL > 45 mg/dL before chelation | <5 | 49.02 | Effect of BLL on neurological features in malaria and non-malaria | 7.94 ± 1.115 | 233 | Malaria associated with BLL < 80 mg/dL and any neurological features | OR of malaria and neurological features (p = 0.016) | RDT | Mass spectrometry |
| Moya-Alvarez et al., 2016 | Benin | 2010–2012 | Cross-sectional study | 203 | Infants | 1 | 48.48 | BLL and malaria | 7.41 ± 0.514 | 25 | BLL associated with decreased risk of malaria | AOR of BLL in 4th quartile and malaria, 0.19 (95%CI, 0.04–0.95, p = 0.04) | Microscopy | Mass spectrometry |
| Mukisa et al., 2020 | Uganda | NS | Cross-sectional study | 198 | Children with malaria positive | NS | NS | BLL and anemia among malaria | 9.2 ± 0.3 | 198 | No association between BLL and malaria parasite density | Correlation coefficient of BLL and parasite density, 0.124 (p = 0.082) | Microscopy | Mass spectrometry |
| Nriagu et al., 2008 | Nigeria | 2005–2006 | Cross-sectional study | 653 | Children | 2–9 | 56.5 | BLL and malaria | 8.97 ± 4.8 | 418 | BLL associated with decreased risk of malaria | Correlation coefficient of BLL and malaria, −0.149 (p < 0.0001) | NS | Inductively coupled plasma/mass spectrometer (ICP–MS) |
| Ugwuja et al., 2011 | Nigeria | 2007–2008 | Prospective observational study | 349 | Pregnant women | 15–40 | 0 | BLL and pregnancy outcomes | 36.37 ± 18.45 | 75 | BLL associated with increased risk of malaria | OR of BLL and malaria, (p < 0.05) | Microscopy | Atomic absorption spectrophotometer |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuraeiad, S.; Kotepui, M. Blood Lead Levels and Subsequence Risk of Malaria in the African Population: A Systematic Review and Meta-Analysis. Trop. Med. Infect. Dis. 2021, 6, 149. https://doi.org/10.3390/tropicalmed6030149
Kuraeiad S, Kotepui M. Blood Lead Levels and Subsequence Risk of Malaria in the African Population: A Systematic Review and Meta-Analysis. Tropical Medicine and Infectious Disease. 2021; 6(3):149. https://doi.org/10.3390/tropicalmed6030149
Chicago/Turabian StyleKuraeiad, Saruda, and Manas Kotepui. 2021. "Blood Lead Levels and Subsequence Risk of Malaria in the African Population: A Systematic Review and Meta-Analysis" Tropical Medicine and Infectious Disease 6, no. 3: 149. https://doi.org/10.3390/tropicalmed6030149
APA StyleKuraeiad, S., & Kotepui, M. (2021). Blood Lead Levels and Subsequence Risk of Malaria in the African Population: A Systematic Review and Meta-Analysis. Tropical Medicine and Infectious Disease, 6(3), 149. https://doi.org/10.3390/tropicalmed6030149







