Occupational COVID-19 Prevention among Congolese Healthcare Workers: Knowledge, Practices, PPE Compliance, and Safety Imperatives
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Sites, and Participants
2.2. Survey Questionnaire and Data Collection
2.3. Ethical Approval
2.4. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics of the Participants
3.2. Knowledge of Congolese Health Care Workers about COVID-19
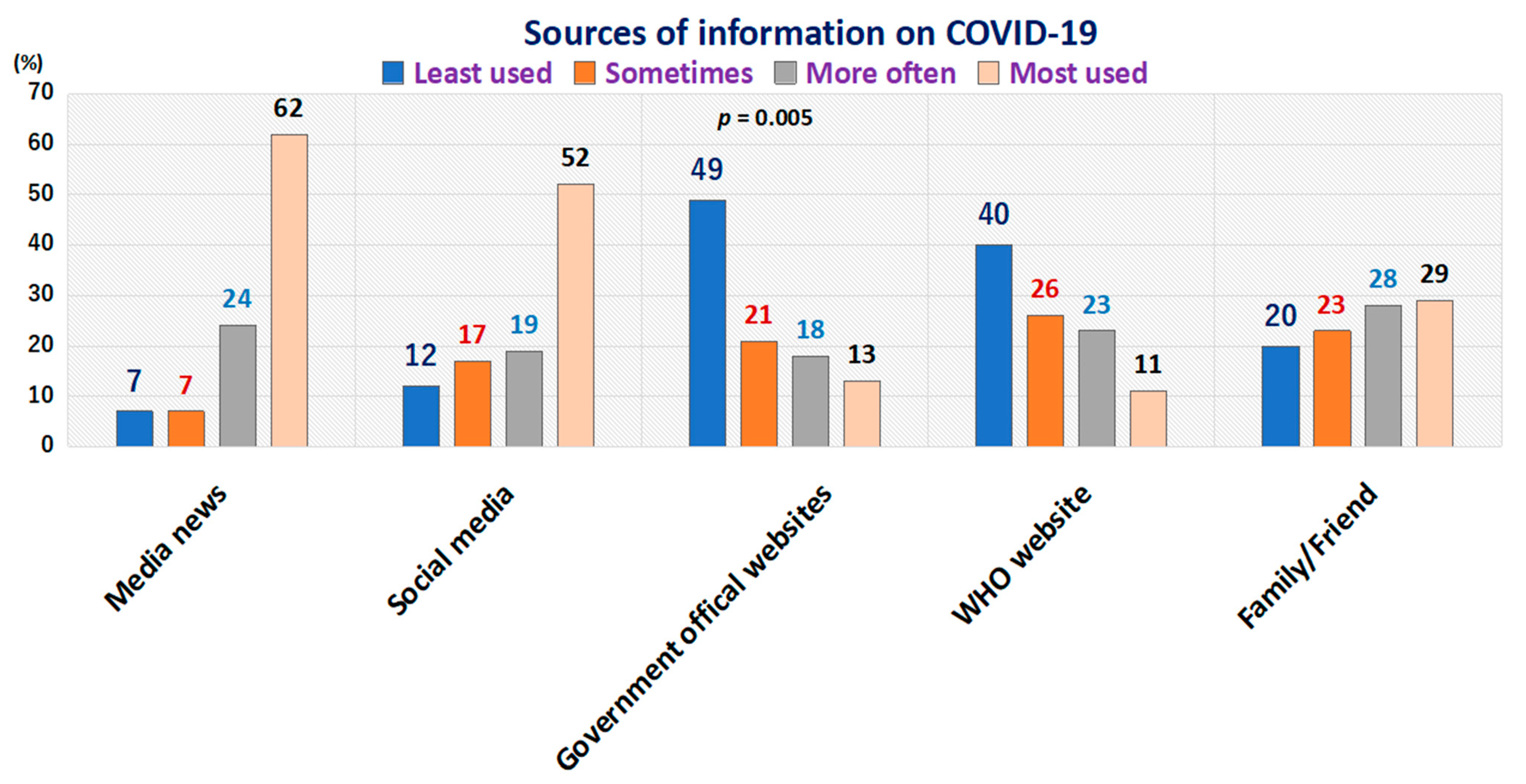
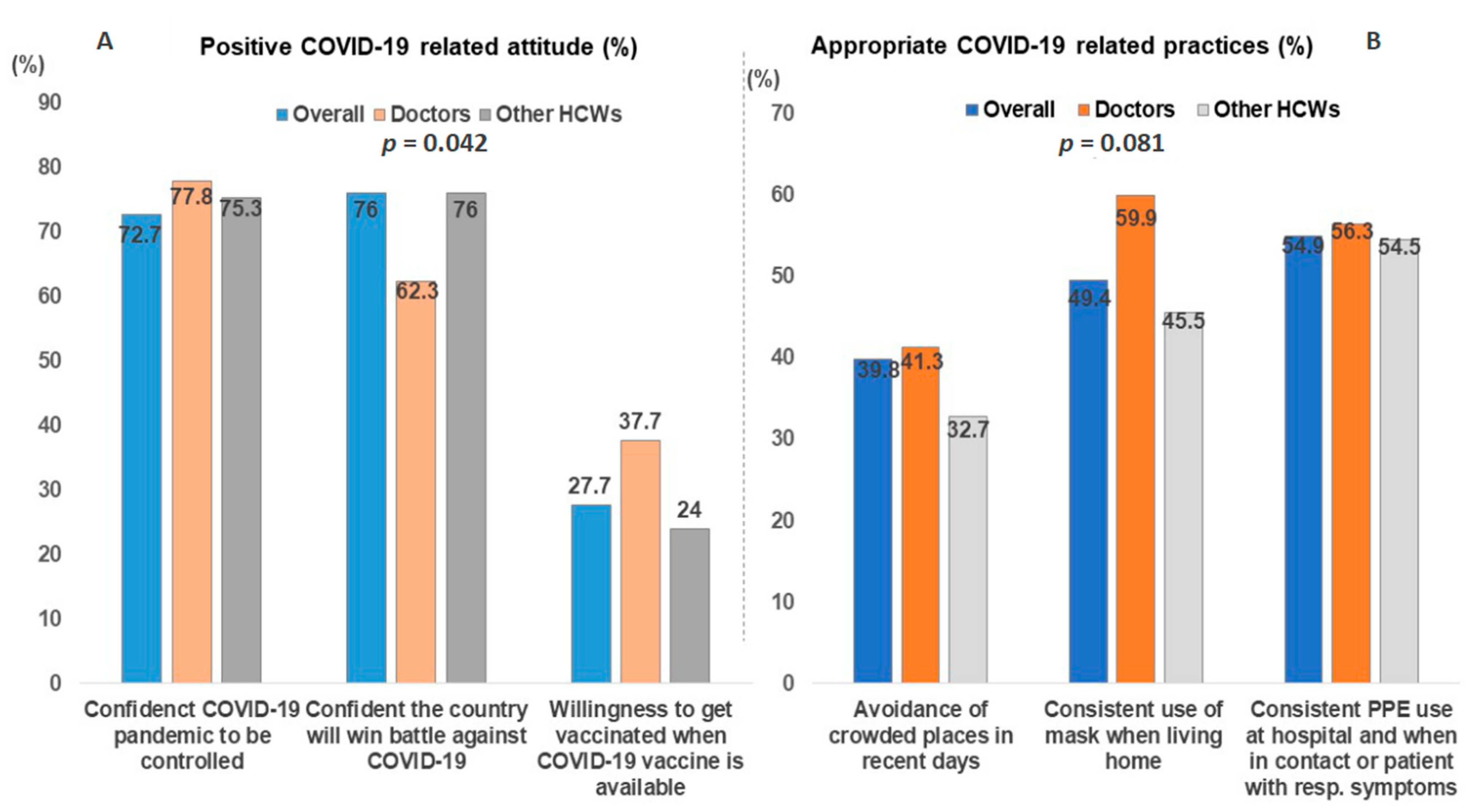
3.3. Attitudes and Practices of Health Care Workers towards COVID-19
3.4. KAPs’ Determinants among Congolese Healthcare Workers
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stübinger, J.; Schneider, L. Epidemiology of coronavirus COVID-19: Forecasting the future incidence in different countries. Healthcare 2020, 8, 99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shigemura, J.; Ursano, R.J.; Morganstein, J.C.; Kurosawa, M.; Benedek, D.M. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin. Neurosci. 2020, 74, 281–282. [Google Scholar] [CrossRef] [PubMed]
- Ranney, M.L.; Griffeth, V.; Jha, A.K. Critical supply shortages-The need for ventilators and personal protective equipment during the Covid-19 pandemic. N. Engl. J. Med. 2020, 382, e41. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. 2020. Available online: https://covid19.who.int/ (accessed on 29 September 2020).
- DRC Ministry of Health. COVID-19 Epidemiological Status in Democratic Republic of Congo. Available online: https://www.stopcoronavirusrdc.info/ (accessed on 12 August 2020).
- Nunez-Delgado, A. What we know about the SARS-CoVi2 coronavirus in the environment? Sci. Total. Environ. 2020, 727, 138647. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Han, X.; Jiang, N.; Cao, Y.; Alwalid, O.; Gu, J.; Fan, Y.; Zheng, C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: A descriptive study. Lancet Infect. Dis. 2020, 20, 425–434. [Google Scholar] [CrossRef]
- Tian, S.; Hu, N.; Lou, J.; Chen, K.; Xiang, Z. Characteristics of COVID-19 infection in Beijing. J. Infect. 2020, 80, 401–406. [Google Scholar] [CrossRef] [Green Version]
- International Council of Nurses. High Proportion of Healthcare Workers with COVID-19 in Italy Is a Stark Warning to the World: Protecting Nurses and Their Colleagues Must Be the Number One Priority. Available online: www.icn.ch/news/highproportion-healthcare-workers-covid-19-italy-stark-warning-world-protecting-nursesand (accessed on 19 August 2020).
- Afrikarabia. Democratic of Congo Divided into 26 Provinces. Available online: http://afrikarabia.com/wordpress/rdc-vers-le-grand-redecoupage/ (accessed on 19 August 2020). (In French).
- World Health Organization (WHO). Risk Assessment and Management of Exposure of Healthcare Workers in the Context of COVID-19. Available online: https://apps.who.int/iris/handle/10665/331496 (accessed on 18 August 2020).
- Ehrlich, H.; McKenney, M.; Elkbuli, A. Protecting our healthcare workers during the COVID-19 pandemic. Am. J. Emerg. Med. 2020, 38, 1527–1528. [Google Scholar] [CrossRef]
- Pittet, D.; Allegranzi, B.; Sax, H.; Bertinato, L.; Concia, E.; Cookson, B.; Fabry, J.; Richet, H.; Philip, P.; Spencer, R.C.; et al. Considerations for a WHO European strategy on health-care-associated infection, surveillance, and control. Lancet Infect. Dis. 2005, 5, 242–250. [Google Scholar] [CrossRef]
- Hopmans, T.E.M.; Blok, H.E.M.; Troelstra, A.; Bonten, M.J.M. Prevalence of hospital-acquired infections during successive surveillance surveys conducted at a University Hospital in The Netherlands. Infect. Control Hosp. Epidemiol. 2007, 28, 459–465. [Google Scholar] [CrossRef]
- Sridhar, M.R.; Boopathi, S.; Lodha, R.; Kabra, S.K. Standard precautions and post-exposure prophylaxis for prevention of infection. Indian J. Paediatr. 2004, 71, 617–625. [Google Scholar] [CrossRef]
- Olum, R.; Chekwech, G.; Wekha, G.; Nassozi, D.R.; Bongomin, F. Coronavirus disease-2019: Knowledge, attitude, and practices of health care workers at Makerere University Teaching Hospitals, Uganda. Front. Public Health 2020, 8, 181. [Google Scholar] [CrossRef] [PubMed]
- Kaliyaperumal, K. Guideline for conducting a knowledge, attitude and practice (KAP) study. AECS Illum. 2004, 4, 7–9. [Google Scholar]
- Engelbrecht, M.; Rau, A.; Kigozi, G.; Van Rensburg, A.J.; Wouters, E.; Sommerland, N.; Masquillier, C.; Uebel, K. Waiting to inhale: Factors associated with healthcare workers’ fears of occupationally-acquired tuberculosis (TB). BMC Infect. Dis. 2019, 19, 475. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Zhou, M.; Tang, F.; Wang, Y.; Nie, H.; Zhang, L.; You, G. Knowledge, attitude, and practice regarding COVID-19 among healthcare workers in Henan, China. J. Hosp. Infect. 2020, 105, 183–187. [Google Scholar] [CrossRef]
- Zhou, W.K.; Wang, A.L.; Xia, F.; Xiao, Y.; Tang, S. Effects of media reporting on mitigating spread of COVID-19 in the early phase of the outbreak. Math. Biosci. Eng. 2020, 17, 2693–2707. [Google Scholar] [CrossRef]
- Mputu, P.; Mupepe, D.; Kayembe, J.M. Occupational risk of exposure to blood in healthcare workers at Biamba Marie Mutombo hospital. Ann. Afr. Med. 2011, 4, 12. [Google Scholar]
- Ngatu, R.N.; Phillips, E.K.; Wembonyama, O.S.; Yoshikawa, T.; Jagger, J.; Suganuma, N. Practice of universal precautions and risk of occupational blood-borne viral infection among Congolese healthcare workers. Am. J. Infect. Control 2012, 40, 68–70. [Google Scholar] [CrossRef]
- Ngatu, R.N.; Kayembe, N.J.M.; Phillips, E.K.; Okech-Ojony, J.; Patou-Musumari, M.; Gaspard-Kibukusa, M.; Madone-Mandina, N.; Godefroid-Mayala, M.; Mutaawe, L.; Manzengo, C. Epidemiology of ebolavirus disease (EVD) and occupational EVD in healthcare workers in sub-Saharan Africa: Necessity for strengthened public health preparedness. J. Epidemiol. 2017, 27, 455–461. [Google Scholar] [CrossRef]
- Aruna, A.; Mbala, P.; Minikulu, L.; Mukadi, D.; Bulemfu, D.; Edidi, F.; Bulabula, J.; Tshapenda, G.; Nsio, J.; Kitenge, R.; et al. Ebola virus disease outbreak—Democratic Republic of the Congo, August 2018–November 2019. Morb. Mortal Wkly. Rep. 2019, 68, 1162–1165. [Google Scholar] [CrossRef] [Green Version]
- Chughtai, A.A.; Khan, W. Use of personal protective equipment to protect against respiratory infections in Pakistan: A systematic review. J. Infect. Public Health 2020, 13, 385–390. [Google Scholar] [CrossRef]
- Gondi, S.; Beckman, A.L.; Deveau, N.; Raja, A.S.; Ranney, M.L.; Popkin, R.; He, S. Personal protective equipment needs in the USA during the COVID-19 pandemic. Lancet 2020, 395, e90–e91. [Google Scholar] [CrossRef]
- Livingston, E.H.; Desai, A.; Berkwits, M. Sourcing personal protective equipment during the COVID-19 pandemic. JAMA 2020, 323, 1912–1914. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adams, J.G.; Walls, R.M. Supporting the healthcare workforce during the COVID19 global epidemic. JAMA 2020, 323, 1439–1440. [Google Scholar] [CrossRef] [Green Version]
- Sabillo, K. The Department of Health (DOH): Over 3000 Doctors, Nurses Directly Affected by COVID-19. Available online: https://news.abs-cbn.com/news/04/28/20/doh-over-3000-doctors-nurses-directly-affected-by-covid-19 (accessed on 20 August 2020).
- Goussanou, W. COVID-19 Trials at Risk after Africa ‘Racism’ Backlash. Available online: https://www.scidev.net/global/health/news/covid-19-trials-at-risk-after-africa-racism-backlash.html (accessed on 20 August 2020).
- Muzembo, B.A.; Ntontolo, N.P.; Ngatu, N.R.; Khatiwada, J.; Ngombe, K.L.; Numbi, O.L.; Nzaji, K.M.; Maotela, K.J.; Ngoyi, M.J.; Suzuki, T.; et al. Local perspectives on Ebola during its tenth outbreak in DR Congo: A nationwide qualitative study. PLoS ONE 2020, 15, e0241120. [Google Scholar] [CrossRef] [PubMed]
- African Union. Africa CDC Condemns Vaccine Trial Proposal on Continent. Available online: https://www.aa.com.tr/en/africa/africa-cdc-condemns-vaccine-trial-proposal-on-continent/1799512 (accessed on 20 August 2020).
- Abdelhafiz, A.S.; Mohammed, Z.; Ibrahim, M.E.; Ziady, H.H.; Alorabi, M.; Ayyad, M.; Sultan, E.A. Knowledge, perceptions, and attitude of Egyptians towards the novel coronavirus disease (COVID-19). J. Community Health 2020, 45, 881–890. [Google Scholar] [CrossRef] [PubMed]

| Variable | Participants (%) |
|---|---|
| Gender | |
| Male | 312 (50.9) |
| Female | 301 (49.1) |
| Age, mean ± SD | 40.31 ± 11.67 |
| <25 years | 29 (4.7) |
| 25–40 years | 386 (63.0) |
| ˃40 years | 198 (32.3) |
| Marital status | |
| Married | 408 (66.6) |
| Unmarried and widowed | 205 (33.4) |
| Occupation | |
| Doctor | 167 (27.2) |
| Nurses | 332 (54.2) |
| Laboratory technician and medical biologist | 58 (9.5) |
| Pharmacist | 23 (3.8) |
| Administrator–manager | 21 (3.4) |
| Dentist | 8 (1.3) |
| Midwife | 4 (0.7) |
| Years of working experience | |
| ≤10 | 328 (53.5) |
| ˃10 | 285 (46.5) |
| Town of residence | |
| Lubumbashi (Haut-Katanga province) | 334 (54.5) |
| Kamina (Haut-Lomami province) | 102 (16.6) |
| Mbuji-Mayi (Kasai-oriental province) | 177 (28.9) |
| Heard about novel coronavirus (SARS-CoV2) | |
| Yes | 609 (99.3) |
| No | 4 (0.7) |
| Attended lecture/discussion on Covid-19 | |
| Yes | 257 (41.9) |
| No | 356 (58.1) |
| Items | All HCWs | Doctors | Other HCWs | p |
|---|---|---|---|---|
| 1. Common symptoms associated with COVID-19 infection | 509 (83.0) | 149 (89.2) | 360 (80.7) | 0.013 |
| 2. Clinical difference between COVID-19 and other lung disease symptoms | 286 (46.7) | 69 (41.3) | 217 (48.7) | 0.105 |
| 3. Currently, in absence of effective cure, symptomatic and supportive treatments help most patients to recover | 521(85.0) | 150 (89.8) | 371 (83.8) | 0.041 |
| 4. Not all infected persons develop severe disease; elderly and people with chronic conditions are likely to develop severe disease | 448 (73.1) | 120 (71.9) | 328 (73.5) | 0.675 |
| 5. Eating or getting in contact with wild animals as one risk factor for COVID-19 infection | 277 (45.2) | 91 (54.5) | 186 (41.7) | 0.005 |
| 6. In absence of fever, a person with COVID-19 may not transmit the virus to others | 403 (65.7) | 140 (83.8) | 263 (59.0) | 0.000 |
| 7. COVID-19 spreading via respiratory droplets of infected individuals | 567 (92.5) | 160 (95.8) | 407 (91.3) | 0.057 |
| 8. For ordinary residents, wearing general medical masks can prevent COVID-19 infection | 481(78.5) | 126 (75.4) | 355 (79.6) | 0.266 |
| 9. Strict adherence to COVID-19 prevention guidelines may not totally be applicable to children and young adults | 180 (29.4) | 40 (24.0) | 140 (31.4) | 0.072 |
| 10. Avoiding crowded places and public transportation as a way to prevent COVID-19 infection | 566 (92.3) | 155 (92.8) | 411 (92.2) | 0.784 |
| 11. Isolation and treatment of COVID-19-infected persons are effective ways to reduce the spread of the virus | 590 (96.2) | 164 (98.2) | 426 (95.5) | 0.119 |
| 12. People having contact with COVID-19 patient are to be isolated for at least 14 days. | 573 (93.5) | 159 (95.2) | 414 (92.8) | 0.287 |
| Variables | Knowledge | Attitudes | Practices | |||
|---|---|---|---|---|---|---|
| aOR (SE) | 95%CI | aOR (SE) | 95%CI | aOR (SE) | 95%CI | |
| Gender (F vs. M) | 0.45 (1.62) | 0.22–0.91 | 0.65 (0.12) | 0.46-0.93 | 1.03 (0.17) | 0.74–1.44 |
| Age (>40 y vs. 40 y or older) | 1.08 (0.31) | 1.01–1.14 | 1.02 (0.16) | 0.99-1.06 | 1.01 (0.01) | 0.99–1.03 |
| Occupation (doctor vs. others) | 0.97 (0.12) | 0.76–1.24 | 0.82 (0.59) | 0.72-0.94 | 0.85 (0.58) | 0.74–0.97 |
| Working experience | 0.96 (0.31) | 0.91–1.03 | 0.97 (0.16) | 0.93–1.04 | 1.02 (0.15) | 0.98–1.03 |
| Category of residence (town without/with COVID-19 cases) | 0.46 (0.93) | 0.31–0.69 | 1.64 (0.18) # | 1.32–2.05 | 2.79 (0.28) # | 1.93–4.06 |
| Information: social media | 1.69 (0.56) * | 1.87–3.25 | 1.15 (0.43) | 0.86–2.63 | 1.43 (0.24) * | 1.02–2.17 |
| Information: family or friend | 1.93 (0.74) # | 2.90–4.11 | 0.89 (0.19) | 0.58–1.36 | 1.71 (0.29) # | 1.22–2.38 |
| Information: official sites | 2.17 (0.99) | 0.88–5.34 | 0.81 (0.17) | 0.54–1.21 | 1.31 (0.52) | 0.59–2.86 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michel-Kabamba, N.; Ngatu, N.R.; Leon-Kabamba, N.; Katumbo-Mukemo, A.; Mukuku, O.; Ngoyi-Mukonkole, J.; Ngoie-Mwamba, G.; Kilolo-Ngoie, E.; Bwana-Kangulu, I.; Kafusthi-Mukemo, D.; et al. Occupational COVID-19 Prevention among Congolese Healthcare Workers: Knowledge, Practices, PPE Compliance, and Safety Imperatives. Trop. Med. Infect. Dis. 2021, 6, 6. https://doi.org/10.3390/tropicalmed6010006
Michel-Kabamba N, Ngatu NR, Leon-Kabamba N, Katumbo-Mukemo A, Mukuku O, Ngoyi-Mukonkole J, Ngoie-Mwamba G, Kilolo-Ngoie E, Bwana-Kangulu I, Kafusthi-Mukemo D, et al. Occupational COVID-19 Prevention among Congolese Healthcare Workers: Knowledge, Practices, PPE Compliance, and Safety Imperatives. Tropical Medicine and Infectious Disease. 2021; 6(1):6. https://doi.org/10.3390/tropicalmed6010006
Chicago/Turabian StyleMichel-Kabamba, Nzaji, Nlandu Roger Ngatu, Ngombe Leon-Kabamba, Astrid Katumbo-Mukemo, Olivier Mukuku, Jean Ngoyi-Mukonkole, Guillaume Ngoie-Mwamba, Elie Kilolo-Ngoie, Ignace Bwana-Kangulu, Dora Kafusthi-Mukemo, and et al. 2021. "Occupational COVID-19 Prevention among Congolese Healthcare Workers: Knowledge, Practices, PPE Compliance, and Safety Imperatives" Tropical Medicine and Infectious Disease 6, no. 1: 6. https://doi.org/10.3390/tropicalmed6010006
APA StyleMichel-Kabamba, N., Ngatu, N. R., Leon-Kabamba, N., Katumbo-Mukemo, A., Mukuku, O., Ngoyi-Mukonkole, J., Ngoie-Mwamba, G., Kilolo-Ngoie, E., Bwana-Kangulu, I., Kafusthi-Mukemo, D., Banza-Ndala, D. B., Kabila-Mutombo, D., Balela-Kabasu, M.-C., Kanyiki-Katala, M., Syed-Mahfuz, A. H., Murakami, A., Kanda, K., Mashima, Y., Oscar-Luboya, N., & Hirao, T. (2021). Occupational COVID-19 Prevention among Congolese Healthcare Workers: Knowledge, Practices, PPE Compliance, and Safety Imperatives. Tropical Medicine and Infectious Disease, 6(1), 6. https://doi.org/10.3390/tropicalmed6010006








