1. Introduction
TKR is a relatively frequent procedure that aims to regain function and eliminate discomfort in end-stage osteoarthritic patients. The 2023 Annual Report reported that primary knee arthroplasty procedures comprised 51.0% of all cases from the period 2012–2022. TKR had a mean age of 67.4 years, with surgeons performing a mean of 56 cases annually in 2022, compared to 35.5 cases in the previous year. Among all reported procedures, 58.5% of the patients were women, which represents a higher percentage of women having knee replacement surgery. Despite its great success rate, approximately.
20% of patients will go through recurrent pain and dissatisfaction with the outcome of the operation [
1]. Malalignment, instability, and implant wear are the principal concerns, frequently leading to complex and costly revision surgeries [
2].
As a component of the move to improve outcomes and extend knee implant life, researchers have designed smart knee implants that incorporate sensor technology to provide real-time feedback regarding implant performance, patient activity level, and joint stability. These advancements allow for intraoperative data-driven decision-making in surgery and long-term postoperative monitoring, ultimately reducing complications and enhancing patient recovery [
3,
4]. Besides this, the development of autonomous implants that can scavenge energy from triboelectric and piezoelectric fields has brought about enhanced efficiency and reliability in these smart systems [
5]. Engineering developments have enabled the integration of miniaturized sensors, wireless modules, and electronic circuits directly into the structure of knee implants. These features allow continuous tracking of joint loading, movement, and alignment. Such innovations improve surgical decision-making, help monitor recovery in real time, and contribute to reducing complications and implant failure.
As more older patients present worldwide and life expectancy rises, knee replacement demand continues to grow, necessitating longer implant survival and postoperative function. Sensor-augmented knee replacement has also been found to enhance joint balance, improve soft tissue management, and lower failure rates compared with traditional implants [
6]. Apart from improving surgical precision, these smart implants use artificial intelligence (AI) and Internet of Things (IoT) to enable remote monitoring of patients, early detection of complications, and personalized rehabilitation protocols [
6]. Despite these significant benefits, the wide-scale use of smart knee implants is hindered by high costs, regulatory barriers, and the need for extended clinical evidence. Continued research and technological development will be critical to surmounting these barriers and establishing smart knee implants as standard in orthopedic practice [
7]. Currently, there are no official statistics available that detail what portion of TKR in the United States involve smart implants. These sensor-enabled devices, while promising, still make up only a small and emerging segment of the TKR market. Uptake has primarily occurred in specialized orthopedic centers and among surgeons engaged in research or early clinical trials. The first smart knee implant, Zimmer Biomet’s Persona IQ (intelligent quotient), was introduced to the market following de novo authorization by the United States Food and Drug Administration (FDA) in August 2021 [
8]. Unlike other knee implants, which would generally fall under general Class II, Persona IQ was placed under a new Class II device type, of implants that track joint movement and other real-time parameters [
9]. This classification allows for special controls, reflective of the device’s new design and digital capabilities.
While early clinical observations have shown potential for improving patient outcomes such as earlier detection of complications or better soft tissue balancing, there is still a lack of large-scale post-market data. So far, the FDA’s public databases, such as MAUDE, offer limited entries specifically related to these smart systems, and peer-reviewed studies are mostly limited to early case reports and pilot studies. As the technology evolves and more cases are tracked, broader outcome data will likely become available to guide future adoption. This review provides a focused summary of recent developments and key challenges in smart knee implant technology, offering an interpretive perspective rather than following the structured methods of a meta-analysis or systematic review.
2. Methodology
This article is a narrative review that synthesizes recent developments in the design, clinical application, and biomechanical performance of smart knee implants. This approach involved gathering and examining information from a wide range of credible sources related to orthopedic implant technology. Special attention was given to studies discussing implant performance, integration of sensors, patient outcomes, and mechanical reliability. References were selected based on their relevance and utility in understanding how smart implants differ from conventional designs both in structure and function.
In addition to scholarly and clinical sources, several patents were also cited for better understanding of the present technological developments in the area. To investigate how safety, data protection, and device approval are managed for implant-based sensors, the study also investigated proper medical practices and regulatory bodies. This provided a good foundation on which to investigate current trends and follow future paths for the development of smart knee implants.
3. Difference Between Conventional and Smart Knee Implants
Traditional knee replacements are designed to approximate the motion and stability of a natural joint. Their designs will vary in whether to leave the cruciate ligaments intact, and typically consist of durable, human-compatible materials like titanium, cobalt–chrome alloys, and polyethylene. To better enhance their operation, engineers apply computer simulations of real forces mimicking walking and standing to see how stress is distributed by the joint. Additionally, beneficial methods, such as pressure-sensitive film, are applied to confirm the extent to which the implant is a perfect fit and functions properly. Although such implants are precision-made for both longevity and functionality, they cannot transmit or record information after they have been implanted [
10]. The implants are effective in restoring function without feedback in real time on joint motion, pressure distribution, or implant wear.
Smart knee implants, however, incorporate sensors, actuators, and wireless telemetry that enable continuous joint movement monitoring, joint alignment, and pressure distribution [
11]. Sensors allow rehabilitation optimization through monitoring of the patient’s healing and real-time feedback to the practitioner for improved post-surgery management [
12]. Traditional knee implants primarily tackle pain elimination and restoration of motion, but smart knee implants adjust dynamically to patient activity and motion and offer improved long-term function [
13].
Smart knee implants are advanced orthopedic prostheses with wireless connectivity, biomechanical sensing, and AI-based movement analysis [
14]. With the aid of real-time feedback, smart implants enable better mobility, more durable implants, and better long-term orthopedic function [
15]. With continued advances in medical technology, smart knee implants will enhance patients’ independence and quality of life, and establish a new standard of care for knee replacement surgery.
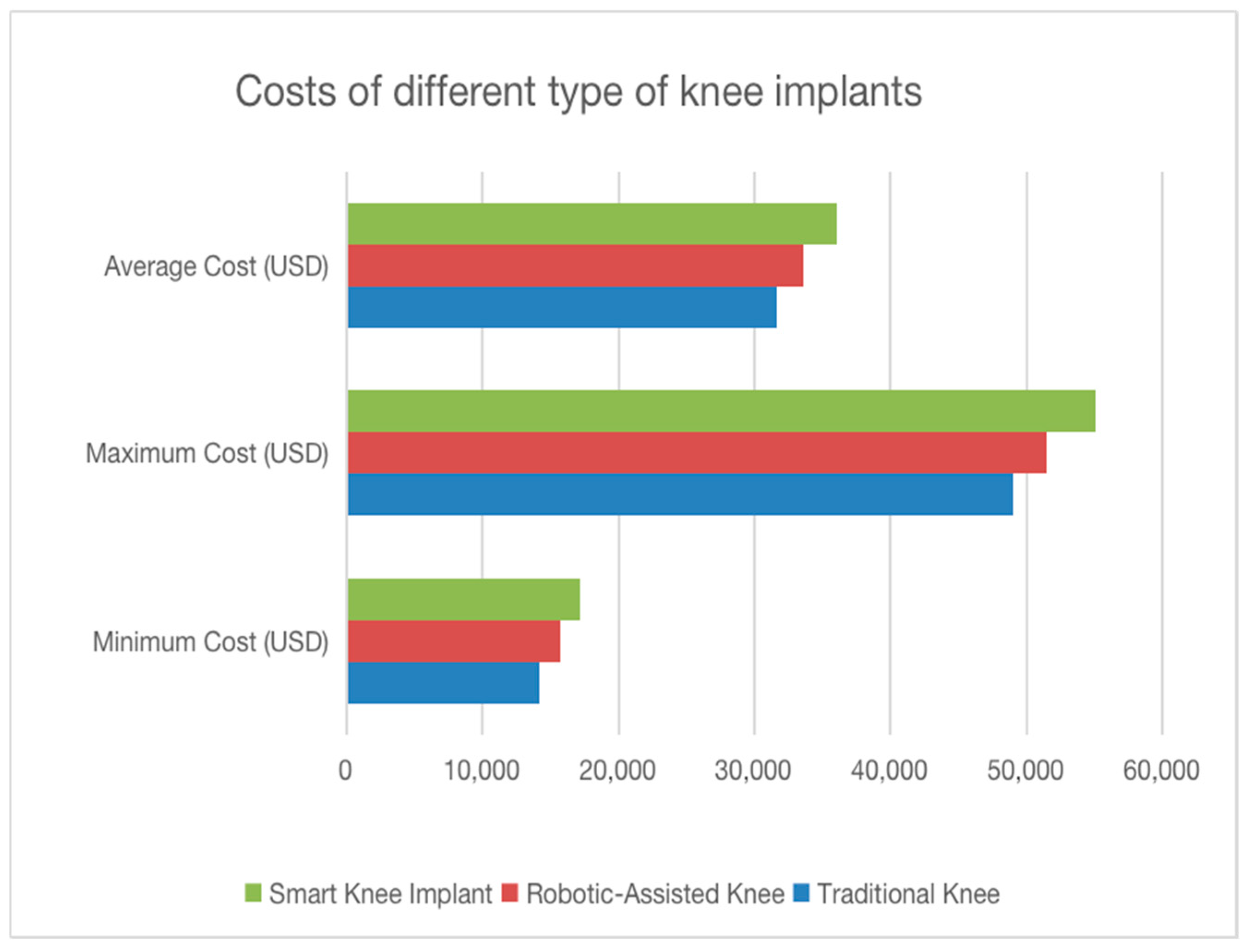
As shown in
Figure 1, traditional knee implants remain the most cost-effective option, with the lowest minimum, average, and maximum cost estimates [
10]. Robotic-assisted implants are more expensive due to the integration of robotic tools that enhance surgical accuracy and alignment [
11,
12]. Smart knee implants have the highest costs in all categories, largely because of the added components such as embedded sensors and wireless monitoring systems [
13,
14]. Despite the higher initial investment, these implants may reduce the need for future revisions and allow for improved post-operative care, which can support their long-term value [
15].
3.1. Drawbacks of Traditional Knee Implants
Orthopedic surgery of the knee joint is widely recognized in traditional approaches for joint replacement; however, there are some shortcomings which may adversely affect the results of a procedure. The main disadvantage of conventional joint replacement consists of no real-time feedback on joint movement or function post-surgery [
7]. These kinds of implants are designed to work in a set, mechanical way and cannot change depending on the activities performed, resulting in the discomfort for a patient while moving. With the passing of time, there may be complications associated with loosening of the implants, infections, or the wear of the material itself, thus demanding revisions [
13]. Some patients have continued to be in pain and cannot get out of bed comfortably, even after the procedure. This causes an alteration in their entire healing process and daily lives. Another complication of the method is the impossibility of making a customized implant, which means that most of them conform to standard designs that may not meet the biomechanical demands of all patients. In addition, limited longevity due to wear and tear over time may cause a need for further surgery [
16]. All these factors underpin the urgent need for better knee implant technology aimed at improved performance and patient satisfaction in the future.
3.2. Need for Smart Knee Implants
Smart knee implants have recently been designed to overcome the limitations of traditional knee replacements by embedding sensor technology and real-time monitoring, with great advantages. One important aspect is the continuous monitoring of joint function, in which sensors note joint angle, loading patterns, and movement for more precise evaluations and adjustments [
17]. The technology also allows for personalized rehabilitation regimens, allowing attending physicians to prescribe treatment according to real-time data to help optimize recovery and improve patient outcomes. Another important capability related to smart knee implants is adaptive support, meaning that the implant’s mechanical properties can be adapted based on the activity levels of the patient, resulting in improved stability and comfort [
18]. These implants also allow for patient engagement in their recovery as they can monitor and track their progress through electronic monitoring, which leads to better participation in their rehabilitation [
19]. Another major benefit is early identification of potential implant failures, misalignment, or excessive wear before they become severe, since continuous feedback could, for such situations, inform the clinicians regarding such medical failure, as perhaps an implant receiving excessively wear or misalignment before they become severe, thus bypassing the revisions or extra surgery [
20]. Although smart knee implants have been said to be more expensive at first, studies suggest that with worthwhile long-term cost benefits—reduced complications following surgeries and better overall implant performance—they should pay off. These improvements lead to the capability of better rehabilitation by improving mobility, leading to better general health as well as patient satisfaction, contributing to them resuming their routine lives with more confidence [
21].
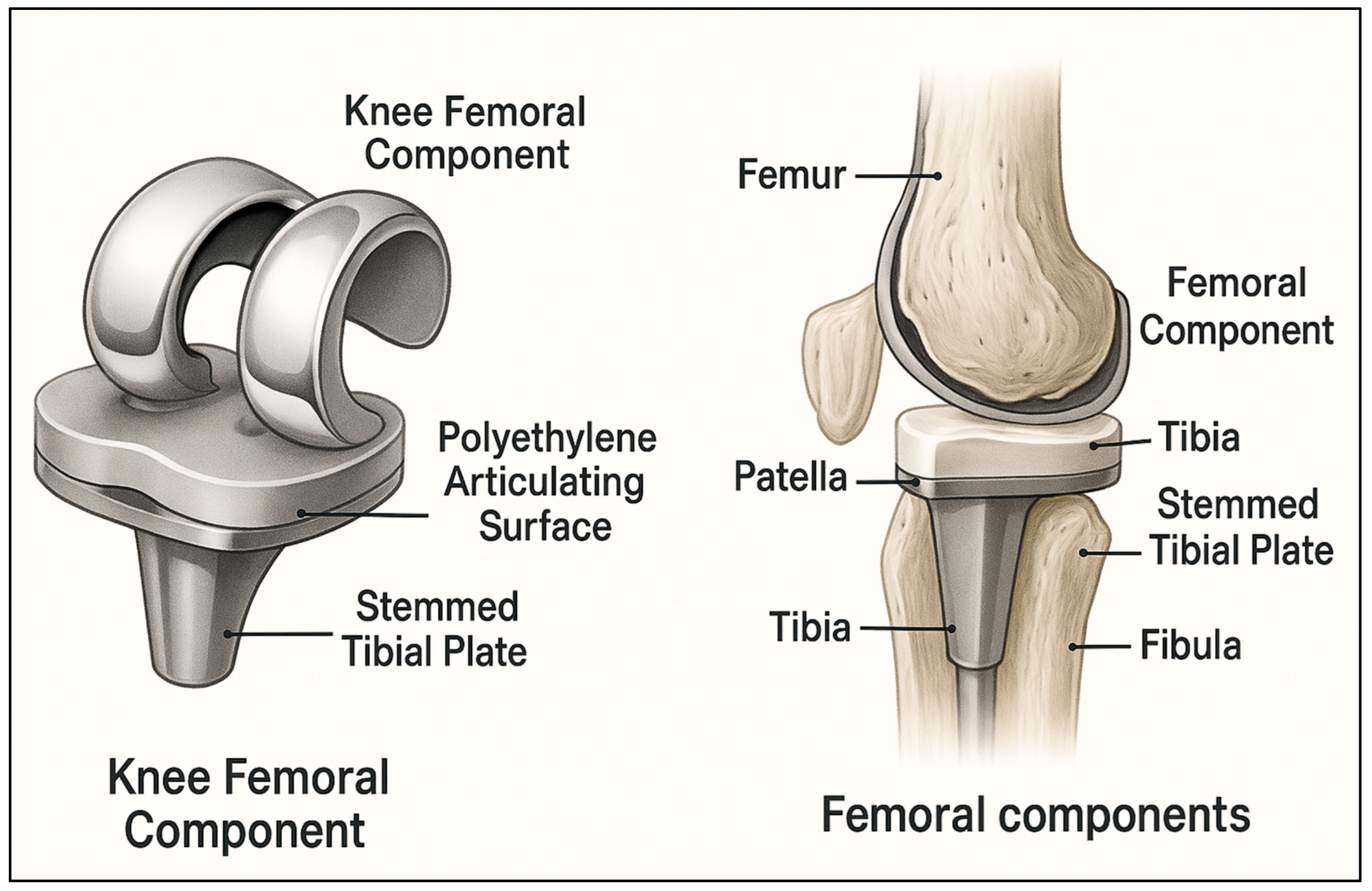
4. Understanding the Anatomy of Human Knee
The knee is among the most intricate joints in the human body, functioning to provide movement and stability. It is formed from three articulate bony components—the femur, tibia, and patella—constituting the basic platform geared toward motion and weight distribution [
22]. The patella protects the joint, while the lateral and medial femoral condyles rest on tibial plateaus, ensuring smooth motion and weight distribution. Each intercondylar crenation harbors the attachment point, where the cruciate ligaments for static support are attached during motion [
23].
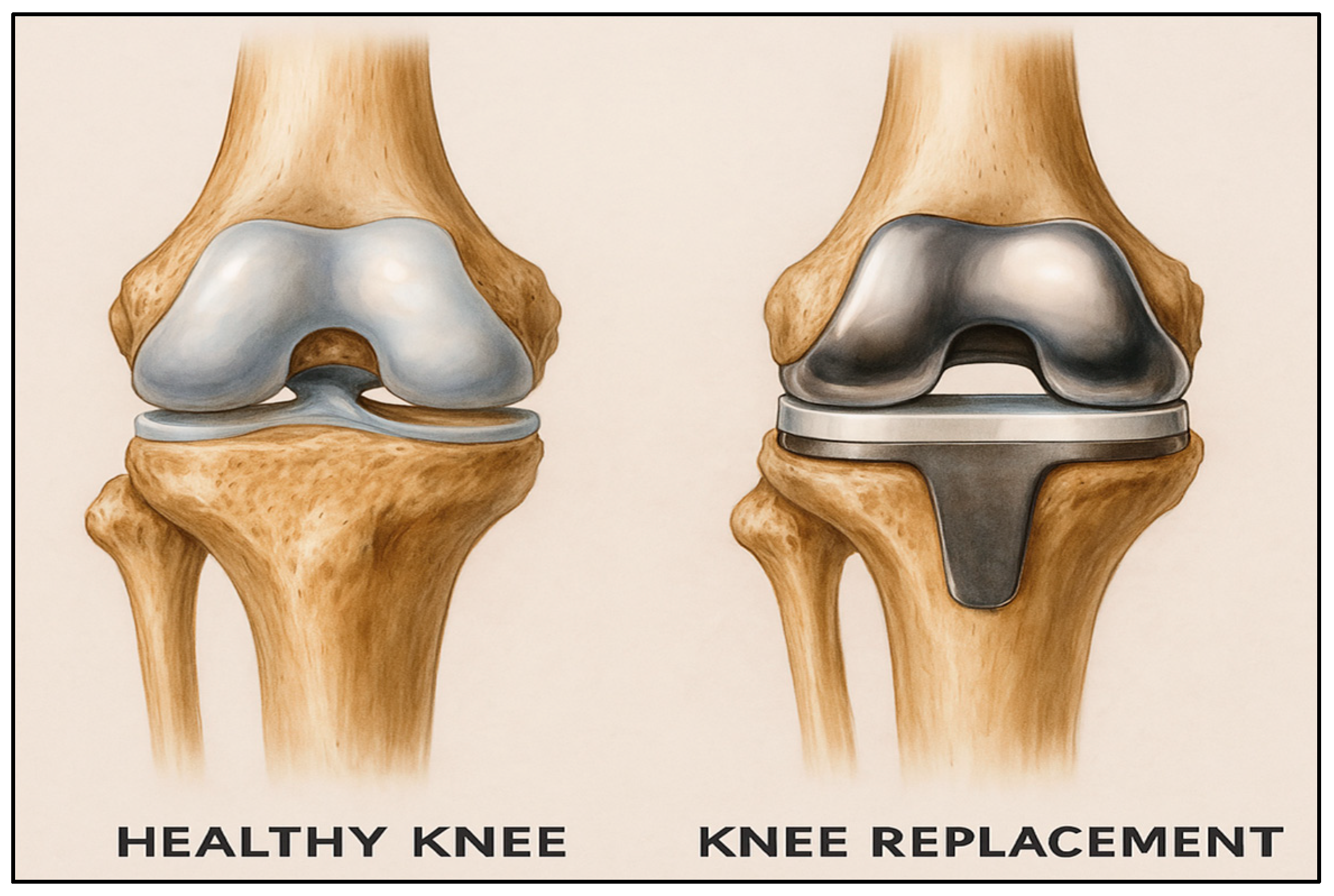
Figure 2 shows a side-by-side comparison of a natural, healthy knee joint and a knee after total replacement surgery. It clearly depicts how the damaged joint surfaces are replaced with metal and plastic components to restore movement and reduce pain.
The cartilage that surrounds the knee absorbs much of the shock force and reduces friction, thus facilitating smooth motions of bending and straightening. The medial and lateral menisci are C-shaped cartilage structures interposed between the femur and the tibia [
24]. They act as shock absorbers and distribute weight while preventing the joint from undergoing excessive stress [
25]. The connective exterior coverings that envelop the knee in joint integrity make up the joint capsule. Inside this capsule, synovial membrane provides a lubricant through joint fluid to prevent wear and promote painless movement. Many important ligaments improve stability for the knee joint. The medial collateral ligament (MCL) and lateral collateral ligament (LCL) prevent excessive lateral movement, while the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) limit excessive anterior and posterior displacement of the tibia [
26]. The quadriceps tendon is involved in the attachment of the patella to the quadriceps muscle. It is very important for knee function and stability. The quadriceps and hamstring are the main muscle groups that perform actions at the knee. The hamstrings at the rear of the thigh allow for knee flexion, while the quadriceps at the front of the thigh provide an extension effect at the knee. The muscles work combinedly toward joint stabilization, motion control, and supporting knee function [
27].
5. Types of Smart Sensors
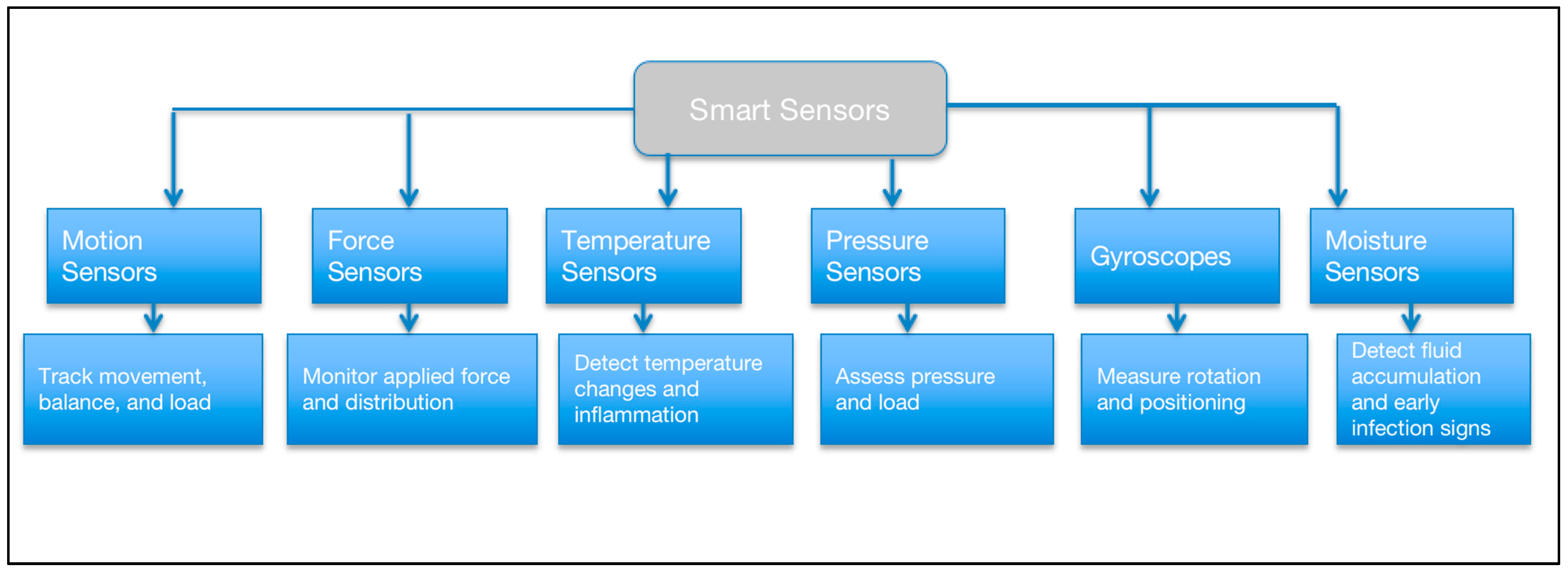
From the detection of infection-related complications to monitoring motion and load distribution, smart sensors used in knee implants perform various functions. The motion sensors incorporated in the implants can track the motion of the implant inside the body, providing doctors with insight on recovery and gait patterns of individuals [
28]. The force sensors make sure that an even load distribution is being applied to the implant for its long-term durability and stability. Temperature sensors allow for the detection of small temperature changes around the implant, which can help reveal the early signs of either infection or inflammation [
29]. Pressure sensors help to keep the joint from moving in a manner that would not be advantageous for the proper mechanics, stability, or mobility of the implant. Gyroscopes track rotation and help detect whether abnormal motion of the joint could affect proper implant positioning [
30]. Similar sensors measure fluid build-up to look for indications of inflammation or infection, and the monitoring of this opens possibilities for early intervention to prevent complications. Such sensors make use of wireless communication technologies, such as Bluetooth low energy (BLE) and radio frequency (RF), to permit real-time monitoring and feedback. The addition of smart technology into knee implants greatly improves the outcomes for patients and the effectiveness of intervention, while increasing the overall success of knee replacement surgeries [
31].
Figure 3 shows the categories of smart sensors used in knee implants and their individual functions. Motion and gyroscope sensors help track joint movement, balance, and orientation. Force and pressure sensors measure load distribution and stress on the implant. Temperature and moisture sensors assist in identifying signs of inflammation or infection, allowing for early clinical response.
5.1. Smart Sensor Workflow in Orthopedic Implants
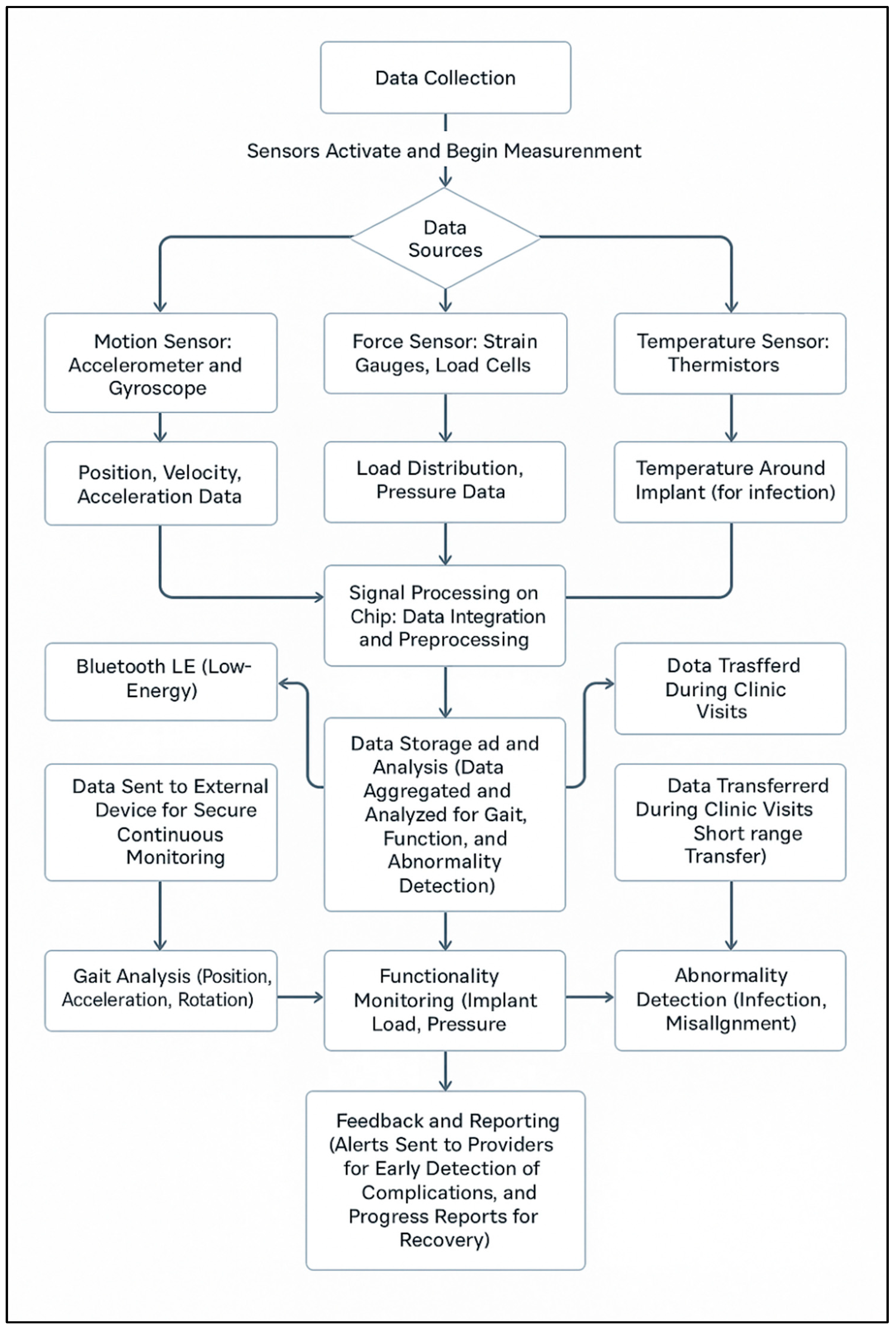
The flowchart as shown in
Figure 4 outlines the data acquisition and transmission process of intelligent knee implants involving the integration of different sensors to detect movement, force, pressure, and temperature in real time. The movement of joints, distribution of load, and stability are sensed by motion and force sensors, while the detection of infection or inflammation is possible with temperature and moisture sensors [
32]. The data is pre-processed on an embedded chip before being sent using Bluetooth low energy (BLE) for ongoing monitoring or near-field communication (NFC) for clinical measurement. After transmission, the data undergoes sophisticated analysis to identify conditions like gait abnormalities, malalignment, or implant failure. Healthcare professionals receive automatic notifications for timely intervention to minimize complications and enhance long-term patient outcomes [
33]. In addition, machine learning techniques and cloud-based analytics enhance predictive modeling, identifying subtle gait deviations and pressure distributions that may herald early implant wear or biomechanical stress. The data are made available in easy-to-read dashboards to allow clinicians to make sound decisions [
34]. Some self-regulating implants can be modified in stiffness or alignment with real-time sensor feedback, which maximizes support for different activities. Such technologies ensure increased mobility, reduced revision surgery, and individualized recovery protocols, yielding better patient comfort and long-term success of implants [
35].
5.2. Pre-Operative and Post-Operative Data Analysis for the Smart Implants
The evaluation of smart knee implants compares pre-op baseline data with post-op observation and assessment, giving information about the recovery of the patient and functionality of the implant. Range of motion (ROM) is one of the crucial parameters, wherein pre-op knee flexion is normally 90–100 degrees and there is a deficit of 10–15 degrees in extension due to stiffness [
36]. After surgery, flexion is 110–120 degrees and full extension is restored, and joint function and mobility are enhanced. The visual analog scale (VAS) and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) disability and pain scores also significantly improve. Pre-operatively, the patient experiences a high level of pain (VAS 7–9) and WOMAC scores between 70 and 80, but post-operatively, pain reduces (VAS 2–3), and WOMAC scores to 20–30, reflecting increased mobility and less pain [
37].
Pre-surgical load and force distribution becomes asymmetrical with degeneration of joints and results in uneven stresses in certain locations. Smart implants create even normal pressure distribution, such that there is equitable loading over the knee joint [
38]. Gait analysis also improves, whereby stride length is increased, knee flexion during walking is enhanced, and gait velocity improves from 0.8 to 1.0 m per second to 1.2–1.5 m per second after surgery [
39]. Muscle strength, particularly for quadriceps and hamstrings, gradually strengthens, with a contribution to joint function and stability. Radiographic proof provides implant position, where no loosening or displacement has been noted over time [
40]. Smart sensors also detect infection and inflammation markers, measuring temperature, swelling, and inflammatory markers for complications. Synovial fluid volumes are evaluated for deviation from normal and can indicate infection, and smart implant battery or power levels are watched to maintain continued function. Long-term wear and tear of the implant is also tracked over time, allowing early intervention in cases of degradation of the material, and enhancing long-term implant function and patient mobility.
6. Biomechanical and Clinical Parameters
6.1. Wear Behavior and Gait-Informed Design Considerations in Smart Knee Implants
Improving the function and durability of TKR requires a good understanding of how the implants function in practice. Investigations based on retrieved polyethylene liners have revealed a wide range of surface damage, and this suggests that knee joint loading and articulation are not consistent for all patients. Irregular patterns of wear such as this suggest that early failure can often be ascribed to issues with the motion distribution of forces. Computational models of such liners have also demonstrated that stress concentrations based on localization and altered load paths are of primary significance in wear development, particularly if the joint is out-of-balance during use [
41].
This challenge ties back directly to more general rules of implant design. A properly working knee substitute must take note of the path the loads follow throughout the joint via activities like walking or climbing stairs. Past work in the field of implant biomechanics emphasizes that proper alignment, materials, and surface geometry of the contact surfaces are all critical to controlling force transmission between components [
10]. But traditional designs prefer to make general assumptions regarding the way the knee works, assumptions which do not always reflect the whole complexity of human gait.
Real gait data provides important insight into this complexity. Research that captures how forces are distributed across the knee throughout the walking cycle reveals that loading patterns are static, but change in both timing and magnitude from one phase of gait to another. For example, compressive forces peak shortly after heel strike, then decrease as the body moves through the stance and swing phases. These patterns of force also differ between individuals. In one study, gait mechanical differences between genders were attributed to differences in step frequency and stride width, both of which influenced the forces experienced by the anterior cruciate ligament (ACL) [
42]. The medial compartment shows greater wear depth than the lateral compartment, which reflects the uneven loading characteristic of failing implants. During gait cycles, ACL forces are consistently higher in females than in males, particularly at mid-stance and toe-off, suggesting gender-specific load patterns that may affect implant longevity. Additionally, sensor measurements from smart implants also indicate that abnormal gait patterns generate higher joint loads than normal gait, suggesting the value of real-time monitoring for the earliest detection of harmful loading and potential implant failure.
A comparison study among trained dancers and non-dancers reported that the ones with specialized training showed also smoother and more controlled movement of the joints, with decreased acceleration around the joints during walking [
43]. These differences highlight that both muscle control and anatomy play roles in joint loading. The integration of wear analysis and gait profiling is particularly valuable in the application of smart implants. In contrast to traditional knee prostheses, smart systems incorporate internal sensors capable of measuring and reacting to joint forces in real time. In combination with data on wear behavior and patient-specific gait profiles, these types of technologies allow for an adaptive response to implant function. Smart implants would be able to identify abnormal loading at an early stage, adjust rehabilitation protocols based on real-time performance, and guide future design refinements. As sensor technology evolves, the incorporation of this kind of biomechanical data will play a key role in reducing revision rates and improving long-term function.
6.2. Positioning of Knee Implant Components
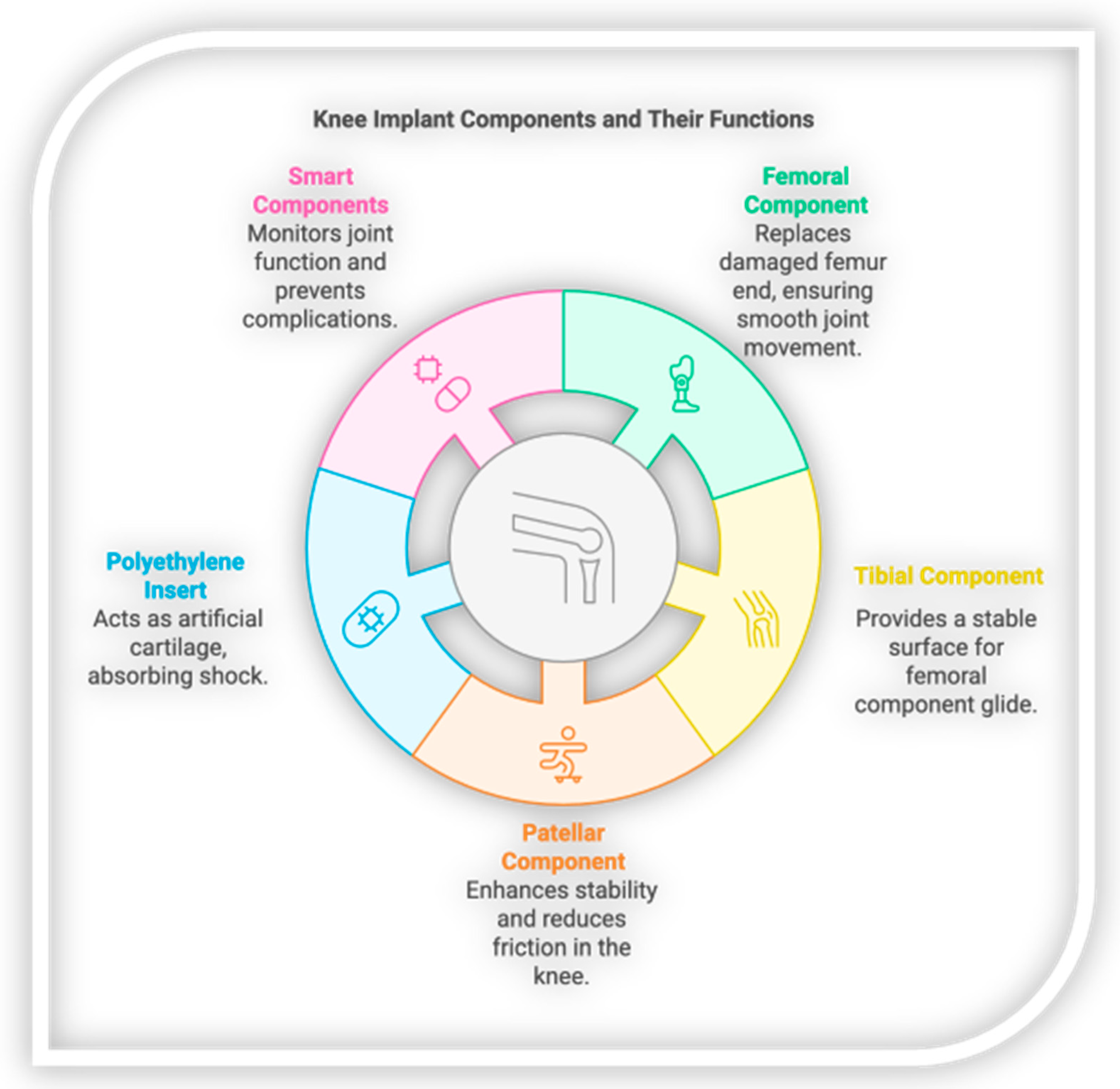
6.2.1. Femoral Component
Location: the femoral component replaces the damaged or worn-out end of the femur (thigh bone). It is contoured to match the normal convexity of the femoral condyles to provide silky smooth articulation with the tibial component [
44].
Reason for Replacement:
Cartilage loss: osteoarthritis (OA) can lead to cartilage loss on the femur to result in painful bone-on-bone contact.
Fracture or bone injury: trauma or degenerative disease may result in femoral surface injury or fractures, reducing the mobility and stability of joints.
Deformities: degenerative or congenital disorders leading to deformed or misaligned femoral condyles can be replaced to achieve normal joint function.
6.2.2. Tibial Component
Placement: the tibial component is placed on the surface of the top of the tibia, most often a metal tray with a spacer of polyethylene, to provide a smooth surface on which the femoral component will ride.
Reason for Replacement:
Severe arthritis: end-stage OA or rheumatoid arthritis (RA) leads to wear and tear of the cartilage on the tibial plateau, resulting in pain and stiffness in the joint, swelling, and limited mobility.
Bone destruction: trauma-induced secondary arthritis can leave the tibial surface in a distorted condition, and joint instability as well as further cartilage destruction may ensue.
Congenital/acquired deformities: bow leg or knock-knee malalignment causes asymmetrical stresses to the tibial surface, developing uneven wear and injury.
6.2.3. Patellar Component
Placement: the patellar component is placed at the posterior surface of the kneecap, such that it rides smoothly on the femoral component. In smart implants, this aspect can be equipped with sensors to verify patellar movement [
45].
Replacement for patellofemoral arthritis: wear of cartilage at the back surface of the patella causes friction and pain on movement.
Misalignment problems: failure to monitor the patella along the femoral groove leads to instability and uneven joint surface wear.
Patellar malformations or fractures: traumatic or congenital kneecap conditions may require a patellar component to stabilize the patellofemoral joint.
6.2.4. Polyethylene Insert
Insertion: this spacer, inserted between the tibial and femoral components, is an artificial cartilage layer that absorbs shock and facilitates smooth motion [
46].
Reason for Replacement:
Loss of cushioning: degeneration of the cartilage in the normal cartilage leads to pain and reduced cushioning, and needs a polyethylene insert to restore balance and even stress distribution on the knee joint.
Decreasing wear and friction: the insert decreases bone–metal contact to prevent excessive wear of the metal part and increase the survival time of the implant.
6.2.5. Smart Components Integration
Location: implants may incorporate sensors within metallic structures (tibial, femoral, sometimes patellar) or within the polyethylene structure. Triboelectric energy-harvesting may also be contained within tibial or femoral implants to facilitate motion-independent charging [
47].
Indications:
Prosthetic Sensors:
Real-time monitoring: real-time kinematic tracking in patients with joint instability, active individuals, or systemic illness is a benefit.
Complication prevention: data from intelligent elements helps to detect complications such as malalignment, overloading, and anomalous motion patterns, which can prevent revision procedures.
Wear reduction: clever implants will sense at an early-stage areas of stress or malalignment, reducing wear on implants and increasing implant survival.
Figure 5 shows the main parts of a knee implant and their roles. The femoral, tibial, patellar, and polyethylene components support movement, stability, and shock absorption, while smart components monitor joint function and detect complications.
Figure 6 shows the key parts of a knee replacement focusing on the femoral components. The image includes the knee femoral component, a polyethylene surface that allows smooth movement, and a stemmed tibial plate that helps secure the implant. It also shows how these parts fit with the bones of the leg including the femur, tibia, fibula, and patella to restore knee stability and function.
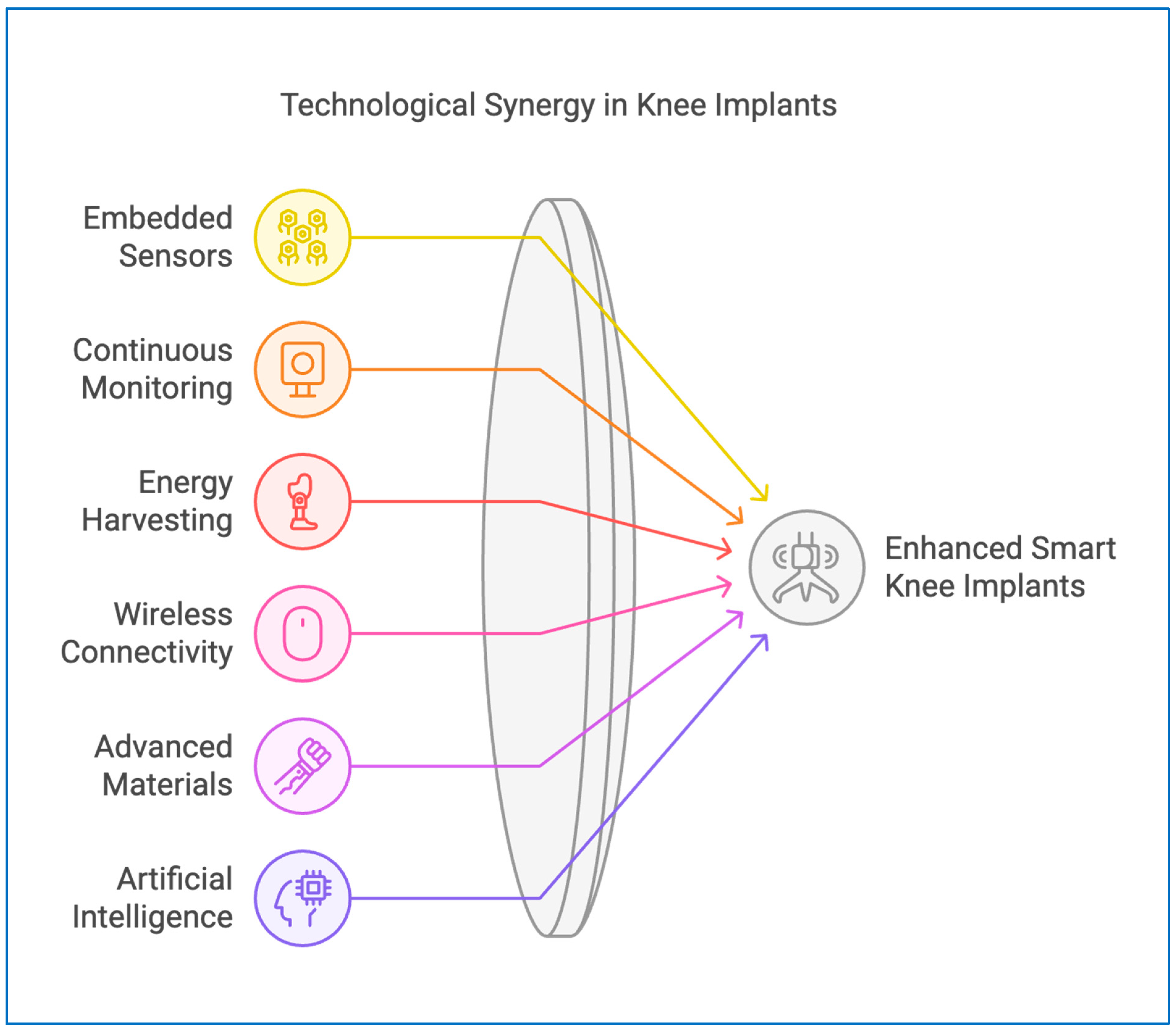
7. Evaluating Current Technologies of Smart Knee Implants
Analyzing the current smart knee implant technologies, there is an emphasis on the performance and efficiency of embedded sensors, energy harvesters, and wireless communication. The embedded elements of smart implants, such as embedded sensors, provide real-time information on joint movement, pressure distribution, alignment, and even temperature. The
Figure 7 shows the technological synergy in knee implants, illustrating how embedded sensors, continuous monitoring, energy harvesting, wireless connectivity, advanced materials, and artificial intelligence collectively contribute to enhanced smart knee implant functionality.
7.1. Embedded Sensors
Smart knee implants possess advanced sensors that capture current information regarding joint movement, pressure distribution, alignment, and temperature. Strain gauges track forces and pressure that facilitate evaluation of the ability of the implant to sustain daily stress, while accelerometers track patterns of movement, which detect gait abnormalities and instability, particularly in rehabilitation patients [
48].
7.2. Continuous Monitoring
Continued remote monitoring allows clinicians to track implant status and detect complications before they become serious. These sensors must be highly accurate and responsive to mechanical stress and wear in the knee joint [
49].
7.3. Energy-Harvesting Technologies
Energy supply to in-body embedded electronics throughout the lifetime of an implant is among the most significant challenges of smart knee implants. Energy-harvesting technology, such as piezoelectric systems and triboelectric nanogenerators (TENGs), has the potential to convert mechanical motion into electricity and reduce external battery reliance [
50].
7.4. Wireless Connectivity
Wireless communication is one of the features that set advanced smart knee prosthetics apart, enabling lossless data transfer to external systems, like smartphones, tablets, or healthcare systems. Bluetooth low energy (BLE) and near-field communication (NFC) are two of the technologies supporting power-efficient and secure data transmission [
51].
7.5. Advanced Materials
The incorporation of advanced technology materials has transformed smart knee implants with greater strength and personalization. Biocompatible 3D-printed materials and self-healing polymers allow for accurate anatomical customization, enhancing implant fit, function, and comfort [
52].
7.6. Artificial Intelligence Integration
Artificial intelligence (AI) is being increasingly incorporated into smart knee implants by processing large amounts of data from inbuilt sensors to provide predictive data on implant performance and patient-specific features [
53].
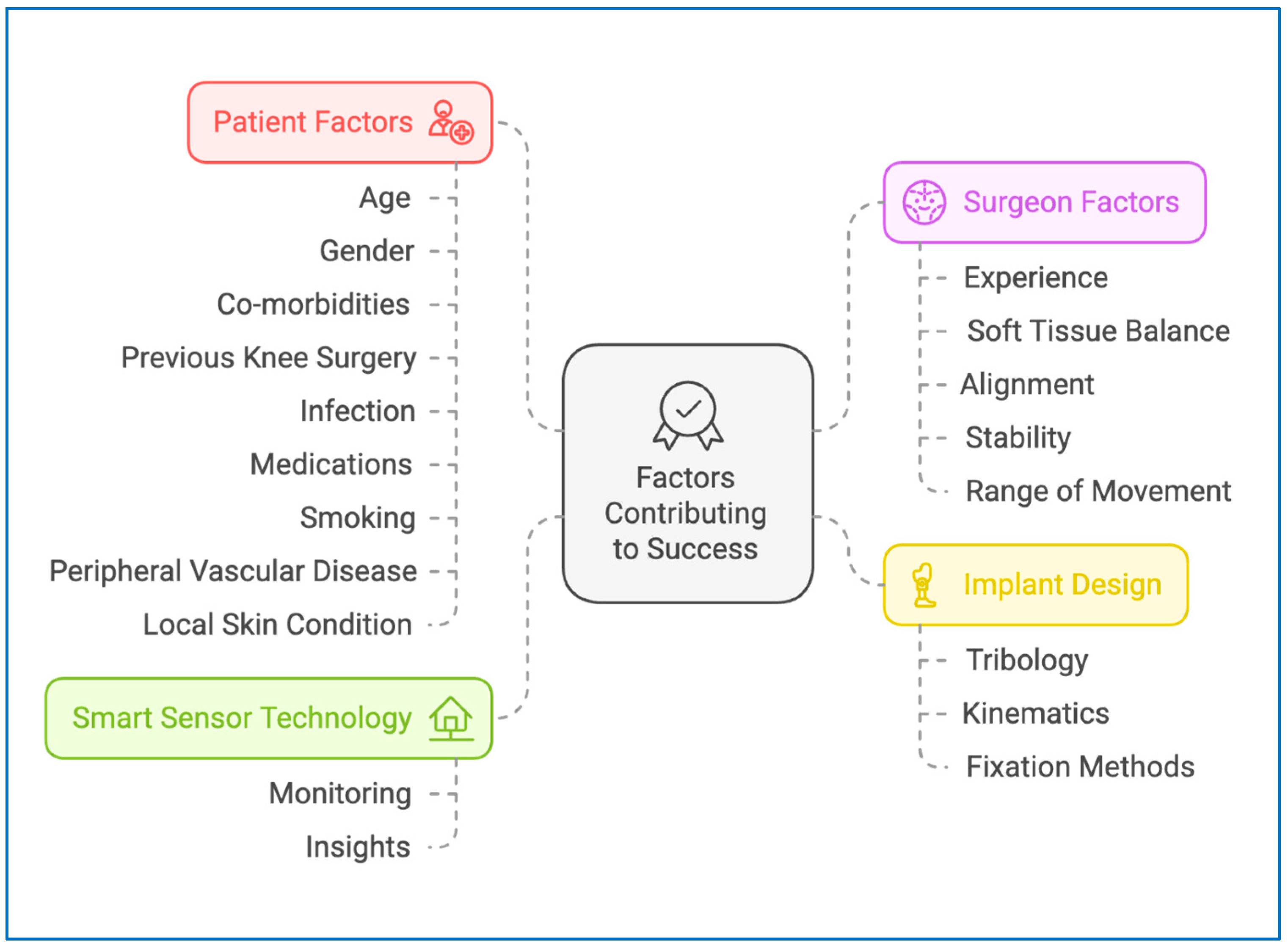
8. Physiological and Mechanical Analysis
The success of smart knee replacements depends on a synergy of patient-dependent characteristics, surgical expertise, smart sensor technology, and implant design. Patient-specific parameters such as age, sex, co-morbidities, history of previous knee surgery, medications, smoking, peripheral vascular disease, and local soft tissue status significantly impact implant integration, healing, and long-term functioning [
54]. Surgeon skill emerges as a concern along with soft tissue balance, accurate alignment, joint stability, and maximum range of motion, directly affecting the performance and longevity of the implant. Inadequate positioning or tensioning imbalance could lead to early wear of the implant, instability, or malalignment, with a likelihood to multiply complications. Real-time feedback with internal sensors allows clinicians to track joint motion, pressure distribution, and early wear, making it possible to detect problems before they reach a critical point [
19,
20]. Ongoing feedback loops built into the system ensure that the rehabilitation process is optimized for the individual’s needs, reducing the likelihood of implant failure while maximizing functional outcomes.
Further, beyond long-term survival and biomechanical success, the material and implant used are important. Tribology, implant surface wear, and friction technology are of greatest importance in reducing component wear and ensuring smoothness over time [
55]. Kinematics, or joint motion, determines how the implant simulates natural knee motion and enables more mobility and load transmission. Technological advancement in fixation methods involving biocompatible materials like ultra-high-molecular-weight polyethylene (UHMWPE) and titanium plating maximizes implant stability, wear, and bone structure integration [
56]. The utilization of artificial intelligence (AI) in sensor-integrated implants also supports predictive maintenance and performance tracking to enable adaptive adjustment towards premature failure and wear. With wireless communications linking implants to patient monitoring networks and clinical databases, real-time data maximizes rehabilitation programs by ensuring that the implant augments natural patterns of motion and long-term joint function [
57]. The
Figure 8 shows the key factors contributing to the success of knee implant outcomes, highlighting the roles of patient-specific conditions, surgeon expertise, implant design features, and smart sensor technology in achieving optimal performance and recovery.
9. Standards of Smart Sensor Network
Smart sensor networks comply with various industry standards for reliability, safety, accuracy, and quality. Common standards, such as ISO 13485 [
58] and ISO/IEC 17025 [
59], regulate the testing and quality management of industrial and medical devices for manufacturing and calibration homogeneity. Standards for measurement precision, such as ISO 5725 [
60] and ISO 81060-2 [
61], focus on precision and reliability in measurement data acquisition, particularly for industrial and health sensors. Standards such as IEEE 802.15.4 [
62], Bluetooth Low Energy (BLE), and NFC (ISO/IEC 18092) [
63] offer power-efficient, low-power data transmission and are essential in IoT and wearable health sensors, as they support data communication without excessive energy consumption. Testing and calibration processes, such as NIST calibration protocols [
64] and ISO/IEC 17025 [
59], ensure precise and continuous sensor function. IEC 60601-1 [
65] provides safety standards for medical electrical devices.
For medical applications, ISO 14971 [
66] and FDA 21 CFR Part 820 [
67] emphasize patient safety and risk management under stringent regulatory expectations. Adherence to these international standards enhances the reliability, safety, and interoperability of smart sensor networks across clinical and industrial applications.
10. Risk Assessment
10.1. Technological and Functional Risks
Smart knee implants have advanced components such as sensors, energy harvesters, and wireless systems, which carry specific risks. Sensors within the implants monitor critical parameters such as joint load, motion, and alignment. The sensors themselves can be deteriorated with time and present with inaccurate readings, which might mislead healthcare professionals and patients. Energy harvesters, in some cases based on triboelectric or piezoelectric effects, lose efficiency and limit continuous data gathering and wireless transmission; thus, they lose the advantages of real-time monitoring. Additionally, the polymers and metals used in these implants must be both biocompatible and long-lasting; however, the use of electronic components leads to augmented material degradation, which may result in implant failure and revision surgery [
50,
68].
10.2. Patient Safety Risks
The addition of electronic components to smart knee implants generates new safety concerns. While biocompatible materials for conventional implants are employed, the novel sensors, wires, and energy harvesters add novel materials to the immune system, increasing the likelihood of inflammatory or allergic reactions, which can result in implant removal. Electronic implants also possess a larger surface area, and therefore are more likely to be colonized by bacteria. This increased chance of infection can lead to severe complications, for which the implant must be completely removed as a cure. The technical sophistication of such implants also makes surgical malpractice more likely, like misalignment or destruction of the device during implantation, which can impair their long-term performance [
69].
10.3. Data Privacy and Security Risks
Since smart knee implants continuously collect and report health data, security and privacy are a primary concern. The appliances receive detailed information about joint health and patient activity, and therefore are susceptible to misuse if security measures are not taken. Cyberattacks can lead to data misuse, thus violating patient confidentiality and even safety. Ethical concerns are also raised for the ownership of information in that no single entity can decide whose end ownership is the accumulated information—the patient’s, the healthcare provider’s, or the manufacturer’s. Maintaining good policies on access to data and security is key to ensuring transparency and protecting patients’ rights [
70]. The integration of wireless communication and sensor data in smart knee implants introduces critical concerns regarding patient privacy, data security, and ownership. In clinical settings, patient health data is protected under established regulations. In the United States, the Health Insurance Portability and Accountability Act (HIPAA) outlines safeguards for how patient information is collected, stored, and shared. In Europe, General Data Protection Regulation (GDPR) provides a similar framework, emphasizing patient consent and data minimization. Additionally, the ISO/IEC 27001 [
71] standard offers guidance on maintaining secure information systems, including procedures for encryption, access control, and audit trails. Despite these protections, questions remain regarding who ultimately owns the data generated by the implant—the patient, the treating physician, or the device manufacturer. As smart implants become more common, it will be essential to develop clear policies for data access, long-term storage, and ethical use. Transparency with patients about how their data is used and ensuring informed consent at every stage will be key to maintaining trust in these technologies.
Figure 9 shows the key risks associated with smart knee implants, organized into five main categories. These include ethical and social risks involving patient accessibility and autonomy, technological risks related to sensor and energy harvester reliability, and patient safety risks such as allergic reactions or surgical complications. It also highlights data privacy risks from potential breaches of sensitive information, and concerns about long-term reliability and environmental interference.
10.4. Reliability and Longevity Risks
Success in the long term in the case of smart knee implants is dependent upon the mechanical reliability of the implant, along with the longevity of electronic components. While knee implants will last longer than ten years, smart implants are equipped with sensors and power supplies that will need replacement or servicing much earlier. Physical surroundings, such as strong heat or magnetic forces, might also disrupt the workings of the sensors and develop glitches compromising the patient’s safety, as well as device reliability. An overarching challenge continues to be to ensure the long-term stability of implants [
72].
10.5. Ethical and Social Risks
The smart knee implants are very expensive, making them out of reach for most patients, and possibly even sustaining health inequalities. Moreover, patients must be adequately informed about how their information is reaped and utilized by such implants so that they can make fully informed healthcare decisions. Patients may also become over-reliant on their implant data and lose some level of autonomy in managing their own health. For these problems to be solved, proper patient education and transparent policies for data management and implant functioning are essential [
73].
Mitigation Strategies
To reduce these risks, continuous advances in sensor technology and material science must be achieved to improve the lifespan of smart knee implants. Sensor reliability and performance of energy harvesters can be ensured through periodic testing and calibration. Strong encryption methods and secure storage policies must be implemented to safeguard patient data from unauthorized users. Clear ethical guidelines for ownership of data will improve patient trust and decision-making. Additionally, professional training for surgeons can decrease implantation complications, and educating patients about the benefits and potential risks of smart implants will improve informed decision-making and safe usage [
74].
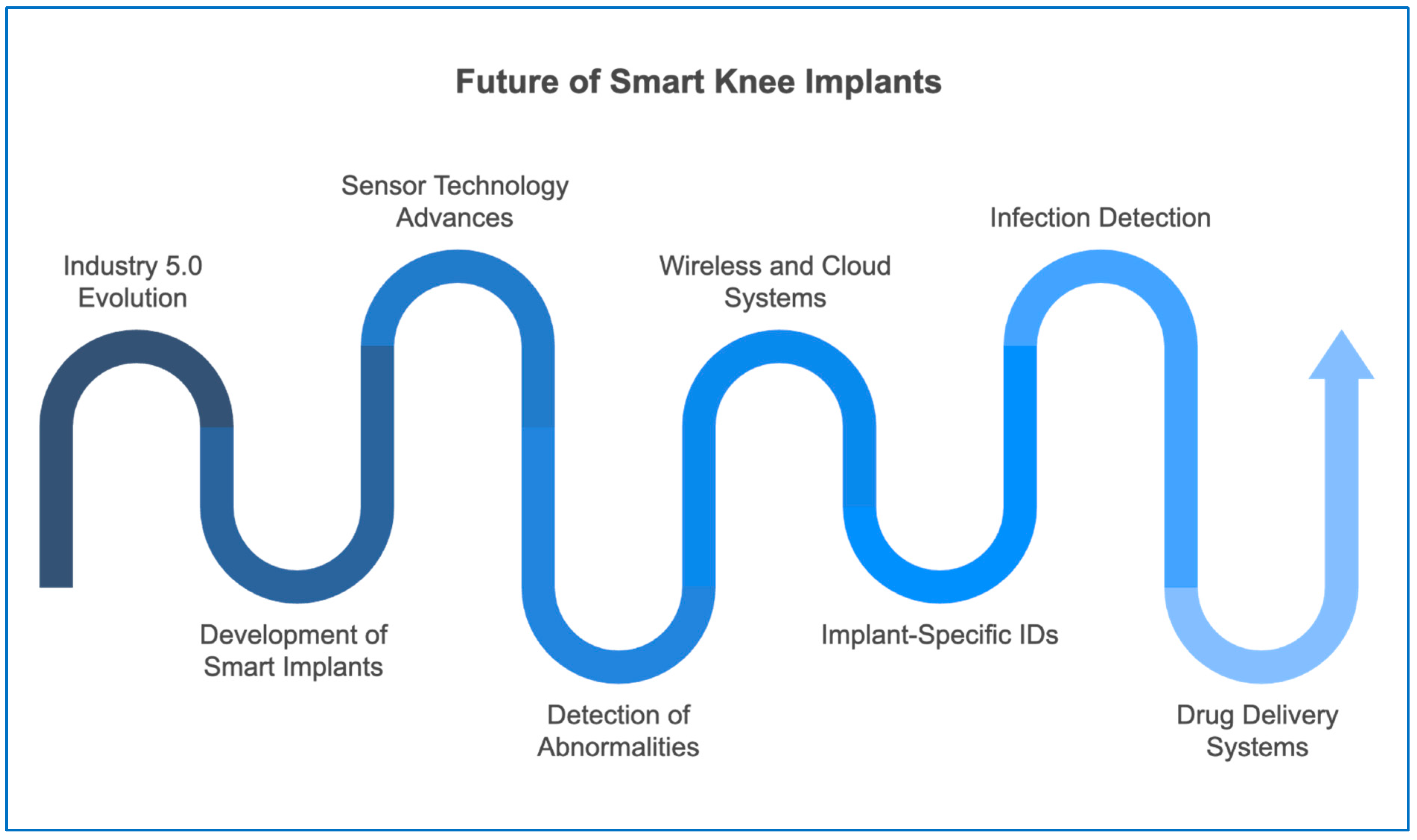
11. Future Perspectives on Smart Knee Implants
Industry 5.0 growth is founded on fusion and sustainability, with high-tech production integrated with nature-based and human-centered philosophies. In orthopedics, its emphasis is the creation of self-diagnosing and self-healing implants [
75]. Future knee implants will be produced using AI, IoT, and machine learning to increase real-time flexibility, implants with extended lifespan, and improved patient care. Such features will bridge the gap between technology and human needs, driving orthopedics toward personalized, streamlined, and smart healthcare solutions [
76].
Figure 10 shows the expected direction of smart knee implant technology. It begins with the impact of Industry 5.0 and the development of smart implants. As the timeline progresses, improvements in sensor technology, wireless and cloud systems, and implant-specific identification are shown. Later stages include the ability to detect abnormalities and infections, ending with the future goal of incorporating drug delivery systems into the implant. This figure outlines how smart implants are likely to evolve to support more personalized and responsive patient care.
Self-Diagnostics and Surveillance
Developments in sensor technology are enabling continuous real-time, intra-operative, and post-operative monitoring of orthopedic implants. Implantable sensors can be inert until abnormal pressure, strain, or biochemical alteration is detected. Wireless communication and cloud-based platforms enable early detection of complications, with response times for intervention and patient safety improved [
77]. In addition, implant-specific digital IDs enable the monitoring of implant function over time, enabling long-term monitoring, predictive analytics, and proactive treatment planning.
Self-Treatment of Orthopedic Infections
Future implants will also be able to incorporate smart sensors that detect pre-clinical infection and initiate localized drug release systems. Bioactive coatings and nanotechnology will enable implants to release antimicrobial agents locally at the site of infection to suppress bacterial colonization and biofilm growth. These preventive interventions will reduce revision surgery rates and healthcare costs, and enhance patient recovery [
78]. The integration of smart drug delivery and infection control systems into knee implants is an orthopedic treatment innovation that is transforming the treatment of post-surgical complications.
Figure 10 shows the expected direction of smart knee implant technology. It begins with the impact of Industry 5.0 and the development of smart implants. As the timeline progresses, improvements in sensor technology, wireless and cloud systems, and implant-specific identification are shown. Later stages include the ability to detect abnormalities and infections, ending with the future goal of incorporating drug delivery systems into the implant. This figure outlines how smart implants are likely to evolve to support more personalized and responsive patient care.
12. Discussion
Sensor technology integration in knee implants is a milestone achievement in joint arthroplasty. Compared to the older prostheses of mechanical matching and visual examination, intelligent knee replacements offer active data-based patient control [
10,
11]. The implants contain sensors to monitor parameters such as load distribution, joint angle, temperature, and pressure, and can identify early patterns of deviation that can predict implant malalignment or wear acceleration [
12,
13,
31]. Accordingly, intraoperative tuning and postoperative rehabilitation may be tailored more precisely to the individual patient [
20,
21]. Clinical experience has shown that sensor-augmented implant patients often exhibit more significant improvement in range of motion, reduced pain levels, and better gait function [
36,
37,
39]. The ability to relay data wirelessly to clinicians supports remote monitoring and more responsive rehabilitation plans, which can lead to a smoother and more personalized recovery process [
14,
19].
However, several concerns must be addressed before smart implants become a standard option. With electronics integrated into the joint, however, there are new problems, such as component fatigue, energy limitation, and potential interference by the implant’s biological environment [
59,
67]. As appealing as such movement or pressure energy-harvesting devices for extending the lifespan of a device are proving to be, their long-term stability is only now being researched [
5,
76]. In addition, regulating such advanced systems is complex, especially with regard to data protection and patient confidentiality. Ensuring compliance with medical device directives and data protection legislation is of the utmost importance [
60,
72]. Another major concern is cost; smart implants are currently more expensive than their traditional counterparts, which may limit access to them for a wide group of patients [
15,
23]. For these technologies to extend beyond niche applications, there must be a balance among innovation, safety, cost-effectiveness, and equity. Although recent studies highlight the promise of smart knee implants in enhancing intraoperative precision and postoperative monitoring, there are still inconsistencies in reported clinical outcomes. Some trials demonstrate improvements in early rehabilitation and complication detection, while others show minimal differences compared to conventional implants. These variations likely reflect differences in implant design, data transmission protocols, patient populations, and follow-up duration. Additionally, concerns around power limitations, sensor calibration, data security, and regulatory classification continue to limit broader adoption.
Table 1 provides a structured comparison to highlight these differences and outline the strengths and trade-offs between conventional and smart systems. Continued multidisciplinary research, with long-term clinical trials and clearer reimbursement models, is essential to validate their added value in routine practice.
13. Conclusions
Smart knee implants represent a meaningful advancement in the field of orthopedic surgery by introducing sensor-integrated systems into traditional joint replacement procedures. These devices are designed to monitor key biomechanical parameters such as joint loading, alignment, motion, and temperature in real time. This allows clinicians to gain deeper insight into implant performance both during and after surgery. With this information, healthcare providers can identify early signs of complications, personalize rehabilitation strategies, and make timely adjustments to improve recovery outcomes. Unlike conventional implants, smart systems support a more dynamic, responsive model of patient care. This evolution in implant design merges biomedical engineering with clinical care, enhancing not only the mechanical function of the joint, but also the quality of surgical feedback and postoperative management.
Ongoing developments in sensor technology, wireless communication, power efficiency, and data analytics continue to enhance the functionality and clinical relevance of smart implants. Improvements in sensor miniaturization, durability, and biocompatibility have made it possible to collect precise measurements without compromising implant integrity. The integration of mobile platforms and cloud-based dashboards has allowed clinicians and patients to further track recovery progress remotely. These advances not only optimize implant longevity and joint function, but also encourage greater patient participation in the rehabilitation process. These patient-centered technologies are also shaping new regulatory considerations, pushing toward outcome-based approval pathways.
Despite these promising features, several challenges must be addressed before smart implants can become a routine part of orthopedic practice. Long-term clinical evidence remains limited, and concerns persist around data privacy, signal stability, and regulatory classification. Questions related to cost, reimbursement models, and surgeon training also require attention. To fully realize the benefits of these technologies, collaboration between engineers, clinicians, regulators, and health systems is essential. With careful validation and responsible implementation, smart knee implants have the potential to redefine joint replacement by making it more personalized, preventative, and outcome-driven.
14. Patents
(15.1) US11478314B1—System and method for implanting smart implants using robotic telesurgery
Date of publication: 25 October 2022
The robotic telesurgery system links a remote doctor module to an operating room module through a cloud network. It employs a robotic arm to aid in the insertion of a smart implant. Prior to surgery, it conducts tests on the implant, compares real-time data with historical data, and verifies the proper functioning of the sensors. Communication with the smart implant is then transmitted to a user device for real-time monitoring of the implant’s performance and the patient’s condition [
79].
(15.2) US20230285167A1—Smart Implant Peripheral Services
Date of publication: 19 February 2015
The disclosed systems and methods involve creating a patient account on a monitoring platform to manage sensor data from an implant. It includes determining which sensor information to collect, the duration of data transfer, and analyzing this data through an external device. Corrective steps are then communicated back to the patient, or the implant based on the analysis [
80].
(15.3) US20180140251A9- Smart joint implant sensors
Date of publication: 14 September 2023
The prosthesis contains a sensor array with multiple sensors attached to it. Additionally, there is an electronics structure responsible for receiving signals from the sensor array and wirelessly transmitting corresponding signals to a remote receiver. These sensors can detect pressure applied to the prosthesis by another object in at least two axes that are generally perpendicular to each other [
81].
(15.4) AU2020287174A1—Intelligent joint prosthesis
Date of publication: 3 February 2022
Medical devices connected to a sensor, along with systems incorporating these devices, have the capability to produce data and conduct analysis using that data. This information can be utilized to detect and/or resolve issues related to the implanted medical device, such as incorrect positioning, unexpected deterioration, and unintended shifting of the device. Additionally, there are medical devices linked to a sensor, as well as devices and techniques for dealing with issues that have been identified with an implanted medical device [
82].
(15.5) IN202041034734—WEARABLE BIOFEEDBACK KNEE CARE SYSTEM
Date of publication: 18 February 2022
The invention presented here introduces a system for knee care that provides biofeedback and can be worn as a wearable device. The system includes a smart knee assembly with two band members and a smart sock assembly. The band member is designed to snugly cover the knee and surrounding areas of the leg. The smart sock assembly is meant to be worn on the user’s foot. A sensor assembly, comprising one or more sensors within the band member and smart sock assembly, is included [
83].