Abnormal Gait Pattern Examination Screening for Physical Activity Level after One Year in Patients with Knee Osteoarthritis
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Measurements and Methods
Abnormal Gait Pattern Examination
2.3. Statistical Analysis
Sample Size Estimates
3. Results
3.1. Subject Descriptive Statistics
3.2. Relationship of Physical Activity
3.3. Predictive Validity of Gait Pattern
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Item I: |
| Increase in foot progression angle in the early stance phase (frontal plane) |
| 0 = The toe in the early stance phase is in the propulsion direction (The physiological foot progression angle is approximately 5°). 1 = The toe in the early stance phase is placed slightly in the toe-out direction (reference value: 15°). 2 = The toe in the early stance phase is placed clearly in the toe-out direction (reference value 25°). |
| Item II: |
| Decrease in the foot contact angle in the early stance phase (sagittal plane) |
| 0 = The heel contact in the early stance phase is clear, and the ankle is in neutral ankle position to the floor. 1 = The heel contact in the early stance phase can be seen, but the ankle is in neutral ankle position to the floor. 2 = The contact to the floor in the early stance phase is a plantar contact. |
| Item III: |
| Decrease in ankle plantar flexion in the late stance phase (sagittal plane) |
| 0 = Ankle plantar flexion to the floor is clear in the late stance phase. 1 = In the late stance phase, the ankle is in neutral ankle position to the floor. 2 = The ankle plantar flexion angle to the floor is reduced and is in dorsiflexion. |
| Item IV: |
| Increase in knee adduction in the early stance phase (frontal plane) |
| 0 = No knee adduction is seen in the early stance phase. 1 = Knee adduction appears in the early stance phase. 2 = Contact occurs with the knee in adduction from the initial contact phase, after which the adduction angle increases. |
| Item V: |
| Decrease in knee extension in the mid-stance phase (sagittal plane) |
| 0 = Knee extension (0°) can be seen in the mid-stance phase. 1 = A decrease in knee extension (−5 to 15°) can be seen in the mid-stance phase. 2 = Knee flexion is seen from the initial contact stage, and there is no knee extension in the mid-stance phase (no angle change). |
| Item VI: |
| Decrease in knee flexion in the swing phase (sagittal plane) |
| 0 = Knee flexion (40 to 60°) can be seen in the mid-swing phase. 1 = Knee flexion in the mid-swing phase is decreased (<20–40°). 2 = Knee flexion in the mid-swing phase is considerably decreased (<20°). |
| Item VII: |
| Decrease in hip extension in the late stance phase (sagittal plane) |
| 0 = In the late stance phase (single limb support phase), the femur is found to be angled clearly posteriorly to the vertical line from the trunk to the floor (posterior angle of 10°–15°) (pay due care to the anteversion of the pelvis). 1 = In the late stance phase (single limb support phase), the angle of the femur oriented posteriorly to the vertical line from the trunk to the floor is decreased (0–5°). 2 = In the late stance phase (single limb support phase), the femur is oriented along the vertical line from the trunk to the floor or angled, anteriorly. |
References
- Dekker, J.; van Dijk, G.M.; Veenhof, C. Risk factors for functional decline in osteoarthritis of the hip or knee. Curr. Opin. Rheumatol. 2009, 21, 520–524. [Google Scholar] [CrossRef] [PubMed]
- Verlaan, L.; Bolink, S.A.; Van Laarhoven, S.N.; Lipperts, M.; Heyligers, I.C.; Grimm, B.; Senden, R. Accelerometer-based physical activity Monitoring in patients with knee osteoarthritis: Objective and ambulatory assessment of actual physical activity during daily life circumstances. Open Biomed Eng. J. 2015, 9, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Scott, D.; Blizzard, L.; Fell, J.; Jones, G. Prospective study of self—Reported pain, radiographic osteoarthritis, sarcopenia progression, and falls risk in community—Dwelling older adults. Arthritis Care Res. 2012, 64, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Dunlop, D.D.; Song, J.; Semanik, P.A.; Sharma, L.; Bathon, J.M.; Eaton, C.B.; Hochberg, M.C.; Jackson, R.D.; Kwoh, C.K.; Mysiw, W.J.; et al. Relation of physical activity time to incident disability in community dwelling adults with or at risk of knee arthritis: Prospective cohort study. BMJ 2014, 348, g2472. [Google Scholar] [CrossRef] [PubMed]
- Palmieri-Smith, R.M.; Thomas, A.C.; Karvonen-Gutierrez, C.; Sowers, M.F. Isometric quadriceps strength in women with mild, moderate, and severe knee osteoarthritis. Am. J. Phys. Med. Rehabil. 2010, 89, 541–548. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Functioning, Disability and Health (ICF). Available online: http://apps.who.int/iris/handle/10665/42407?search-result=true&query=ICF&scope=&rpp=10&sort_by=score&order=desc (accessed on 25 December 2022).
- Lo, G.H.; Harvey, W.F.; McAlindon, T.E. Associations of varus thrust and alignment with pain in knee osteoarthritis. Arthritis Rheum. 2012, 64, 2252–2259. [Google Scholar] [CrossRef] [PubMed]
- Mündermann, A.; Asay, J.L.; Mündermann, L.; Andriacchi, T.P. Implications of increased medio-lateral trunk sway for ambulatory mechanics. J. Biomech. 2008, 41, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.; Hurwitz, D.; Dunlop, D.; Song, J.; Cahue, S.; Hayes, K.; Sharma, L. The relationship between toe-out angle during gait and progression of medial tibiofemoral osteoarthritis. Ann. Rheum. Dis. 2007, 66, 1271–1275. [Google Scholar] [CrossRef] [PubMed]
- Mündermann, A.; Dyrby, C.O.; Andriacchi, T.P. Secondary gait changes in patients with medial compartment knee osteoarthritis: Increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005, 52, 2835–2844. [Google Scholar] [CrossRef] [PubMed]
- Iijima, H.; Fukutani, N.; Aoyama, T.; Fukumoto, T.; Uritani, D.; Kaneda, E.; Ota, K.; Kuroki, H.; Matsuda, S. Clinical phenotype classifications based on static varus alignment and varus thrust in Japanese patients with medial knee osteoarthritis. Arthritis Rheum. 2015, 67, 2354–2362. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.; Hayes, K.; Dunlop, D.; Hurwitz, D.; Song, J.; Cahue, S.; Genge, R.; Sharma, L. Thrust during ambulation and the progression of knee osteoarthritis. Arthritis Rheum. 2004, 50, 3897–3903. [Google Scholar] [CrossRef] [PubMed]
- Pisters, M.F.; Veenhof, C.; van Dijk, G.M.; Heymans, M.W.; Twisk, J.W.; Dekker, J. The course of limitations in activities over 5 years in patients with knee and hip osteoarthritis with moderate functional limitations: Risk factors for future functional decline. Osteoarthr. Cartil. 2012, 20, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Kato, S.; Shimogaki, H.; Onodera, A.; Ueda, H.; Oikawa, K.; Ikeda, K.; Kosaka, A.; Imai, Y.; Hasegawa, K. Development of the revised version of Hasegawa’s dementia scale (HDS-R). Jpn. J. Geriatr. Psychiatry 1991, 11, 1339–1347. [Google Scholar]
- Kohn, M.D.; Sassoon, A.A.; Fernando, N.D. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin. Orthop. Relat. Res. 2016, 474, 1886–1893. [Google Scholar] [CrossRef] [PubMed]
- Holla, J.F.; Steultjens, M.P.; Roorda, L.D.; Heymans, M.W.; Ten Wolde, S.; Dekker, J. Prognostic factors for the two-year course of activity limitations in early osteoarthritis of the hip and/or knee. Arthritis Care Res. 2010, 62, 1415–1425. [Google Scholar] [CrossRef] [PubMed]
- Yamashina, S.; Harada, K.; Ono, S.; Adachi, M.; Miyake, K.; Kawamura, K. Evaluation of observable items of gait abnormality in patients with knee osteoarthritis: Criterion-related validity using three-dimensional gait analysis and test-retest reliability. Jpn. J. Rehabil. Med. 2019, 56, 1032–1043. [Google Scholar] [CrossRef]
- Yamashina, S.; Harada, K.; Tamari, K.; Tanaka, R.; Yamada, E.; Moriyama, H.; Anan, M.; Kyogoku, M. Research for construction of gait abnormality evaluation based on observation in patients with knee osteoarthritis: Item characteristics, factor validity, concurrent validity and inter-rater reliability. Jpn. J. Phys. Ther. 2021, 55, 922–930. [Google Scholar]
- Lee, I.M.; Shiroma, E.J.; Kamada, M.; Bassett, D.R.; Matthews, C.E.; Buring, J.E. Association of step volume and intensity with all-cause mortality in older women. JAMA Int. Med. 2019, 179, 1105–1112. [Google Scholar] [CrossRef] [PubMed]
| Follow-Up Group n: 24 | Dropout Group n: 22 | p-Value | |
|---|---|---|---|
| Age, years | 76.33 (8.02) | 70.36 (6.19) | 0.01 |
| Sex | Men: 5, Women: 19 | Men: 5, Women: 17 | N/A |
| BMI | 23.42 (3.97) | 27.11 (5.51) | 0.012 |
| K-L severity | I: 10, II: 6, III: 3, IV: 5 | I: 4, II: 9, III: 6, IV: 3 | N/A |
| Knee flexion ROM, ° | 131.88 (12.23) | 132.73 (6.70) | 0.78 |
| Knee extension muscle strength, Nm/kg | 0.79 (0.39) | 0.78 (0.37) | 0.94 |
| Knee flexion muscle strength, Nm/kg | 0.43 (0.17) | 0.42 (0.23) | 0.92 |
| Abnormal gait pattern | 5.46 (3.16) | 4.27 (2.60) | 0.18 |
| Gait speed, m/s | 1.22 (0.36) | 1.24 (0.20) | 0.76 |
| Physical activity, steps/day | |||
| Baseline | 4803.50 (2785.80) | 3862.0 (1925.0) | 0.19 |
| After 1 year | 4363.21 (2779.80) | N/A |
| Physical Activity | F-Value | p-Value | |||
|---|---|---|---|---|---|
| Low Group n: 6 | Intermediate Group n: 7 | High Group n: 11 | |||
| Age, years | 84.83 (5.74) | 74.42 (7.81) | 72.91 (6.51) | 6.46 | 0.01 * † |
| Knee flexion ROM, ° | 128.33 (9.83) | 137.14 (8.09) | 130.45 (15.56) | 0.93 | 0.41 |
| Knee extension muscle strength, Nm/kg | 0.57 (0.16) | 0.84 (0.51) | 0.88 (0.39) | 1.35 | 0.28 |
| Knee flexion muscle strength, Nm/kg | 0.35 (0.18) | 0.40 (0.10) | 0.49 (0.19) | 1.58 | 0.23 |
| Abnormal gait pattern | 12.67 (1.28) | 9.00 (1.19) | 4.27 (0.95) | 14.62 | 0.00 † ‡ |
| Gait speed, m/s | 0.83 (0.17) | 1.17 (0.31) | 1.46 (0.28) | 10.92 | 0.001 † |
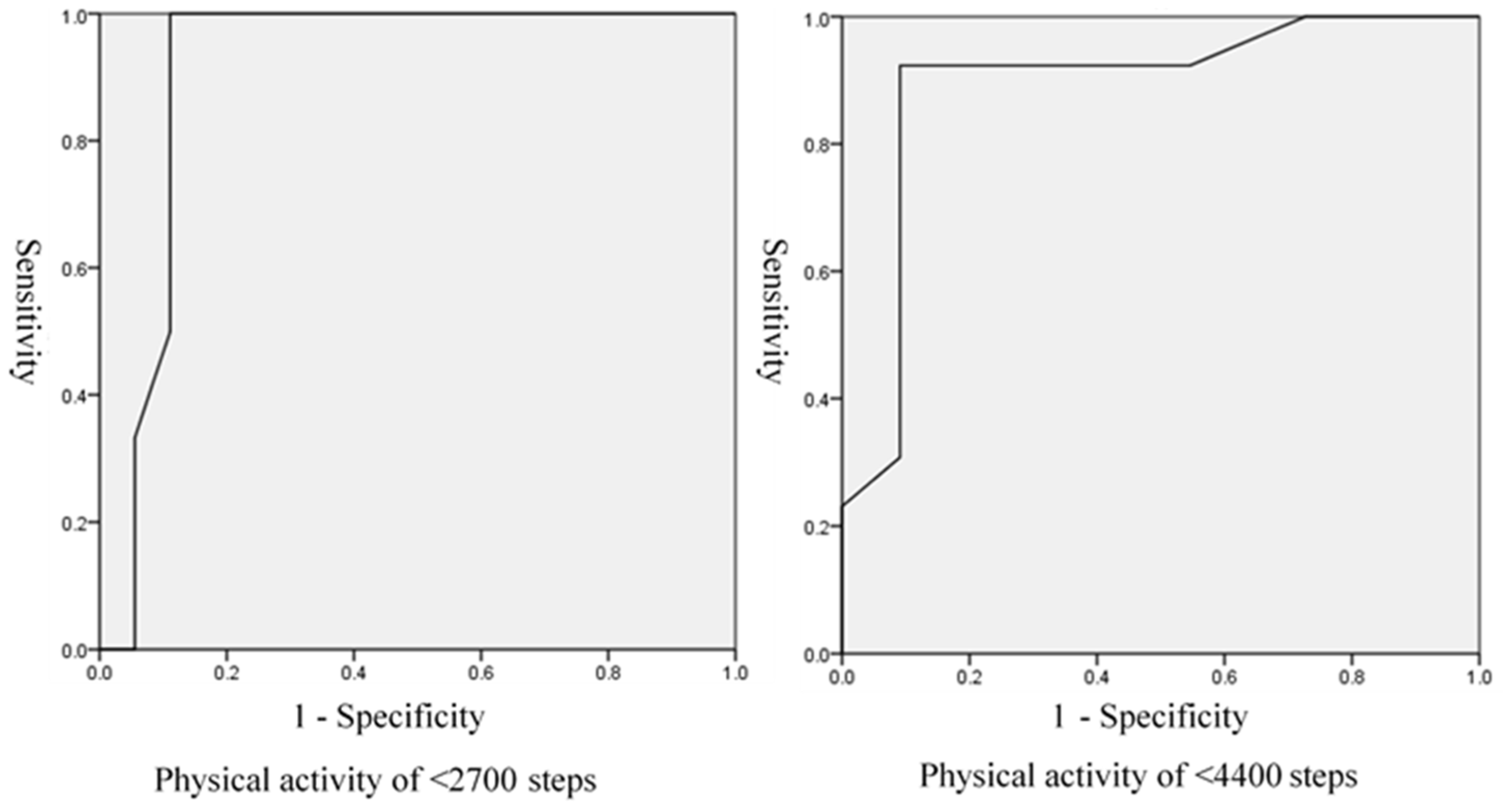
| AUC | Cut-Off Value | Sensitivity | Specificity | PLR | NLR | |
|---|---|---|---|---|---|---|
| <2700 steps | 0.91 | 8 | 1.00 | 0.89 | 9.09 | 0 |
| <4400 steps | 0.89 | 5 | 0.92 | 0.91 | 10.2 | 0.09 |
| Decrease in PA <2700 Steps | No Decrease in PA ≥2700 Steps | Decrease in PA <4400 Steps | No Decrease in PA ≥4400 Steps | |
|---|---|---|---|---|
| Test positive | 6 | 2 | 12 | 1 |
| Test negative | 0 | 16 | 1 | 10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamashina, S.; Harada, K.; Tanaka, R.; Inoue, Y. Abnormal Gait Pattern Examination Screening for Physical Activity Level after One Year in Patients with Knee Osteoarthritis. J. Funct. Morphol. Kinesiol. 2023, 8, 24. https://doi.org/10.3390/jfmk8010024
Yamashina S, Harada K, Tanaka R, Inoue Y. Abnormal Gait Pattern Examination Screening for Physical Activity Level after One Year in Patients with Knee Osteoarthritis. Journal of Functional Morphology and Kinesiology. 2023; 8(1):24. https://doi.org/10.3390/jfmk8010024
Chicago/Turabian StyleYamashina, Shunsuke, Kazuhiro Harada, Ryo Tanaka, and Yu Inoue. 2023. "Abnormal Gait Pattern Examination Screening for Physical Activity Level after One Year in Patients with Knee Osteoarthritis" Journal of Functional Morphology and Kinesiology 8, no. 1: 24. https://doi.org/10.3390/jfmk8010024
APA StyleYamashina, S., Harada, K., Tanaka, R., & Inoue, Y. (2023). Abnormal Gait Pattern Examination Screening for Physical Activity Level after One Year in Patients with Knee Osteoarthritis. Journal of Functional Morphology and Kinesiology, 8(1), 24. https://doi.org/10.3390/jfmk8010024






