Abstract
Individuals with lower-limb amputations may have a significant strength deficit. This deficit may be related to the stump length and can lead to changes in gait, reduced energy efficiency, walking resistance, altered joint load, and increased risk of osteoarthritis and chronic low back pain. This systematic review used the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA) guidelines to examine the effects of resistance training in lower limb amputees. Interventions with resistance training and other training methods were sufficient to achieve muscle strength gain in muscles of the lower limbs, improved balance, and improvements in gait pattern and speed when walking. However, it was impossible to determine from the results whether resistance training was mainly responsible for these benefits or even whether the positive effects presented would be observed with only this training method. When combined with other exercises, interventions with resistance training made possible gains for this population. Accordingly, it is noteworthy that the main finding of this systematic review is that the effects may be different according to the level of amputation, with mainly transtibial and transfemoral amputations studied.
1. Introduction
The number of people with disabilities is increasing. For instance, the WHO reported that 10% of the world’s population had some type of disability in 1970, whereas approximately one billion people currently live with some type of disability, or approximately 15% of the world’s population (considering the 2010 estimate) [1]. In the United States of America, 1.6 million people were living with the loss of a limb in 2005, which could reach 3.6 million people by 2050 [2]. People with lower-limb amputations may have a significant strength deficit. This deficit may be related to the stump length and can lead to changes in gait, reduced energy efficiency, walking resistance, altered joint load, and increased risk of osteoarthritis and chronic low back pain [3].
Strength imbalances caused by amputation can be relieved through several training programs that help to mitigate the complications caused by amputation in these individuals [3,4]. Resistance training is an exercise mode in which the body’s muscles move against an opposing force. This opposite force can be achieved using equipment, such as weights, elastic bands, machines, or even with the body’s own mass [5]. It is known that people with disabilities suffer from inaccessibility in their daily tasks. One aim of exercise is to facilitate the practitioner’s daily living activities. Physical exercise can be beneficial for people with disabilities, and lack of exercise and disuse of the prosthesis are considered reasons for the strength deficit in amputees [3]. There are several benefits of resistance training for lower limb amputees, such as improved walking, combatting muscle atrophy, bilateral strength deficit reduction, increased strength for stabilization, improved gait, and improved hip strength [4].
In addition to being a public health concern, amputations can generate significant discomfort in the lives of affected individuals. Investigating whether resistance training can help improve the living conditions of these individuals is essential. Furthermore, it is observed that there is a lack of systematic reviews and practical recommendations that contribute to a better understanding of this topic. This review aimed to examine the effects of resistance training in lower limb amputees in order to present practical guidance based on evidence of resistance training protocols in this population.
2. Materials and Methods
This systematic review used the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA) guidelines [6]. Articles published until March 2022 were analyzed. The search and selection of articles took place in two stages, from August to October 2021 and from February to March 2022.
2.1. Search Procedures and Study Selection
For the searching and selection of articles, the following databases were used: PubMed/Medline, Scopus, Web of Science, VHL, Cochrane, and Embase. The PICO strategy was used, defining the population as lower limb amputees; the intervention as resistance training; the comparison did not apply; and the outcome was any variable related to physical, motor, or physiological capacity on resistance training intervention as a primary or secondary outcome. This strategy defined descriptors in English and was selected from the MeSH vocabulary query. The descriptors “strength training”, “exercise program”, “strengthening program”, “resistance training”, “exercise prescription”, “amputee”, “amputation”, “lower limb”, and “lower extremity” were selected and combined with Booleans, as shown in Table 1.

Table 1.
Used descriptors.
2.2. Eligibility Criteria
The eligibility criteria were defined according to the previously mentioned PICO strategy. Studies were included that (I) were in Portuguese, English, or Spanish, and (II) had the descriptors listed above and titles that made clear the relationship with the theme of resistance training in lower limb amputees. In case there were doubts about the relevance of the article with the theme of the review, the abstract was read, and if the relevance was still in question, the entire article was read to corroborate the decision to include or exclude the study.
Articles were excluded that (I) referred only to upper limb amputations; (II) were literature reviews; (III) were related to resistance training but amputees were not included in their sample; (IV) were related to amputees but not related to resistance training. Several study designs were considered, as the intention was to examine as many studies as possible. The search did not contain a minimum date limit and studies published until March 2022 were considered.
2.3. Data Collection Process
A total of 156 articles were found. Table 2 shows the relationship between the articles found and the databases.

Table 2.
Found articles.
After reading the titles, 83 articles were excluded because they did not fit the scope of the research and 36 articles were excluded because they were duplicates. Thirty-eight articles were selected for reading of the abstract. After reading the abstract, 22 were excluded. From the remainder, 16 articles were selected for a full reading. Of the 16 articles, one was excluded due to language criteria, one was a literature review, one did not have resistance training as an intervention, and three did not fit the proposed theme. Therefore, 10 studies were selected for this systematic review. Data from the articles were extracted into an electronic card file. For a complete visualization of the data, the PRISMA flowchart adapted for the context of this work is available below in Figure 1.
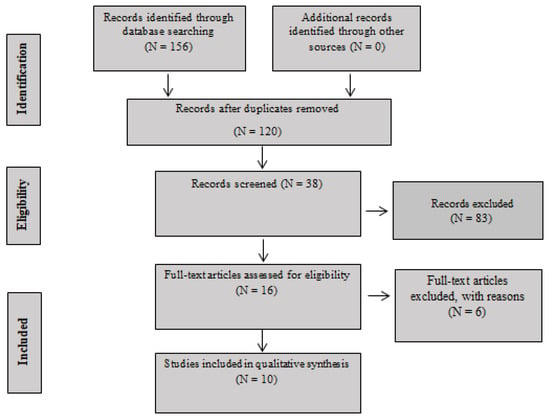
Figure 1.
PRISMA Flow Diagram.
2.4. Risk of Bias in Individual Studies
The quality of the selected studies was analyzed using the Tool for the assEssment of Study qualiTy and reporting in EXercise (TESTEX) scale [7].
3. Results
Through a structured methodology, the search resulted in 10 studies eligible for this systematic review. Table 3 contains the risk of bias within the studies and Table 4 and Table 5 contain theoretical and descriptive data on the articles.

Table 3.
TESTEX scale for analyzing the quality of studies.

Table 4.
Study characteristics.

Table 5.
Intervention characteristics and results.
3.1. Risk of Bias within Studies
The quality of the studies was analyzed using the TESTEX scale [7]. Table 3 displays the scores of the articles.
3.2. Study Characteristics
Table 4 highlights the heterogeneity of these findings. The studies were carried out in several countries, published between 2004 and 2021, and most were published in the last five years [8,9,10,11,12,13]. Among them, 90% of the studies presented amputees of both sexes. The age of the participants varied from childhood to old age. There were different levels of amputation among the participants. However, transtibial and transfemoral amputees were prevalent in the studies. Regarding the methodology, the studies showed plurality but only three (3) studies were randomized clinical trials [11,14,15].
3.3. Exercise Approaches and Studies Results
The exercise protocols are described in Table 5. It is noteworthy that this systematic review of the literature considered analyzing resistance training as an intervention; however, 70% of the studies used other techniques in addition to resistance training [8,9,10,11,14,15,16]. The duration of the exercise protocols ranged from 3 to 20 weeks, with the most significant number (30%) of studies lasting 8 weeks [12,14,17]. Weekly exercise frequency ranged from 1 to 3 times a week, with most (50%) studies exercising twice a week [9,12,13,15,17]. One study did not report the weekly exercise frequency [14] and two other studies varied the weekly exercise frequency according to their criteria [11,16]. Studies also reported sessions ranging from 30 min to 2 h for each training session.
4. Discussion
This systematic review aimed to examine the effects of resistance training in lower limb amputees. Such studies used various analysis techniques, training protocols, and resistance training as an intervention. It is believed that this systematic review is the first to analyze and compare the effects of resistance training in lower limb amputees.
4.1. Studies Qualities
The poor methodological quality of the majority of the studies presented in this review was notorious. However, it is worth noting that only three studies were randomized clinical trials [11,14,15], which can justify the low quality. In addition, one of the randomized clinical trials had reasonably lower quality than the other two [14]. Interestingly, although it was not a randomized clinical trial, one study [17] obtained the highest score in the TESTEX scale.
The failure to present the load used in the exercise protocols, the duration of the sessions, and the conclusion of the intervention, in addition to whether there was any withdrawal or signaling whether or not there were adverse effects may perhaps be the main reasons for the low quality of the studies found, which impacted the quality of this review. Despite the poor methodological quality, the importance of these studies must be considered since this is a topic of interest. Furthermore, the possible difficulty in carrying out more structured studies with this population should be considered, given the context of inaccessibility for people with disabilities and the particularities of each amputation.
4.2. Session Duration, Weekly Frequency, and Total Weeks (Months)
The exercise protocols ranged from 3 to 20 weeks, with 8-week interventions being the most common [12,14,17]. Four studies lasted less than eight weeks [9,10,13,14], while six studies lasted more than eight weeks [8,11,12,15,16,17], of which only one lasted longer than 12 weeks, lasting a total of 20 weeks [8]. Some authors consider studies of 8 to 12 weeks to be short, which may not contribute to long-term interventions [4]. It is noteworthy that three of the four studies lasting less than eight weeks did not obtain significant results in at least one outcome measure [10,13,14]. In addition, some studies of more than eight weeks in duration presented in this review also showed little or no significant change in any outcome measure [8,15,17], which may justify the need for new long-term investigations.
Regarding weekly exercise frequency, the importance of 2 to 3 times a week for each muscle group in resistance exercises is observed in the American College of Sports Medicine (ACSM) guidelines [18]. Seven studies included this recommendation [9,11,12,13,15,16,17]. However, one study did not report the weekly exercise frequency of the intervention [14].
Regarding the duration of the sessions, some studies did not describe the length of the sessions. Of those that presented this information, the sessions lasted between 30 min and 2 h. The lack of such information raises doubts about the volume of the exercise and compromises possible replicability.
4.3. Participants
The heterogeneity of the study participants can be considered a positive aspect, since it allows a better interpretation of different contexts. However, this can also lead to possible errors when the results are not specified for each type of lower limb amputation or even for each sex and age. Another point to note is the small number of participants in each study. Only one study contained more than fifty participants [14]. Considering studies may present different levels of amputation, sex, and age, as well as a low number of participants, it is important to pay attention to potentially inaccurate results.
4.4. Exercise Protocols
The exercise protocols were varied and determined by the specific objective of the investigated studies. Unfortunately, many studies did not present fundamental details regarding the exercise protocols. It should be noted that the ACSM guidelines does not present guidelines for amputees, which may have resulted in a lack of standardized guidelines in the studies.
4.4.1. Exercise Intensity
To calculate the intensity of a physical exercise, it is recommended to use the percentage calculation of 1RM, or another RM load, such as 10RM [5]. One study used the pre-test 10RM to define the 1RM load used in their intervention and then 50% of 1RM was used for the weightlifting circuit exercises [16]. According to the ACSM, exercises between 40–50% of 1RM can be beneficial for elderly and sedentary individuals [18].
In the case study [16], the individual was a 40-year-old man who was hypertensive, a smoker, and a bi-amputee. Due to the limitations above, exercises of 40–50% of 1RM may have been ideal in this case. Nevertheless, the exercise program contained closed chain exercises in addition to the weightlifting circuit, which were performed in three sets of ten repetitions with 50%, 75%, and 100% of 10RM.
In another study [17], the intensity of 10RM was established, as they considered it safe for patients with lower limb amputations.
Some studies did not report RM data but presented the load (kg) used in each exercise [10,15]. Furthermore, it should be noted that only these studies discussed exercise intensity with RM. This makes interpretation of the data difficult and also affects the study’s replicability.
4.4.2. Number of Sets, Repetitions, and Rest Interval Length
Due to differences between the exercise protocols, the sets and repetitions were consequently different. There was also a lack of information about the sets and repetitions used in the studies. Rest interval lengths of two to three minutes between sets are recommended by the ACSM [18]. Few studies indicated the rest intervals used in the protocols, but they ranged from one to two minutes when provided [8,10].
4.4.3. Type of Exercises
According to the ACSM [18], several models of resistance training and equipment can be used This review showed that different exercise models were used with a variety of equipment. Given the particularity of lower limb amputation, it may be necessary for exercises to be adapted so that they can be performed properly by an amputee [19,20]. Only a few studies [9,11] made clear that the researchers adapted the exercises for the participants. It is noteworthy that in addition to resistance training, the exercise protocols of some studies included other training modes, such as aerobic, flexibility, and balance exercises [9,10,11,14,15,16]. In addition, exercises for upper limbs were also used in some studies [16]. Furthermore, some investigations compared other exercise techniques with resistance training [11,14,15,17]. It is important to emphasize that using other exercise modes in the protocols can raise doubts about the effectiveness of resistance training in the interventions, making it impossible to affirm whether resistance training was the only type of activity that caused the outcomes reported in those investigations.
4.5. Resistance Training Effects
Strength deficit [3], balance-related adversities [21,22,23], changes in gait [3,24,25,26,27], and low back chronic pain [15,28] are some of the many problems that can accompany amputation. On this topic, the effects of resistance training on strength deficit, changes in gait, chronic low back pain, and adversities related to balance are reported below.
4.5.1. Strength Gains
The strength deficit may be associated with lack of exercise and disuse of the prosthesis [3]. A study with amputee individuals demonstrated resistance training can reduce the strength deficit in this population [28], which is in line with some of the findings in this review [12,13,15,16,17]. Various exercise protocols using resistance training as the primary intervention led to strength gains in amputees [12,13,15,16,17].
In a bilateral amputee, there was a more significant strength gain in the hip of the transtibial limb compared to the transfemoral limb stem [15]. This outcome [3] corroborated the findings of another study reporting that transfemoral amputees have a more significant deficit in their hip muscles than transtibial amputees.
4.5.2. Fall Risk and Balance Analyses
The increased risk of falling is related to a lack of balance [22,23]. As a result, the amputee becomes afraid of falling [21], increasing their distrust in their ability to balance. One study [9] demonstrated an improvement in dynamic balance during walking and an increase in balance confidence after an exercise protocol with resistance training and balance exercises. Likewise, another study used only resistance training as an intervention and reported improved balance confidence and attenuation of fear of falling [17].
In a resistance training intervention accompanied by dynamic balance exercises, there was an increase in balance in only one foot on an unstable surface, even without visual input and with imprecise somatosensory feedback [11]. However, unlike previous studies, no significant changes were seen in the activity-specific balance confidence test (ABC test) used to examine confidence in balance. There was also no relationship between postural control and confidence in balance.
4.5.3. Gait and Muscle Changes
When comparing the effects of resistance training with proprioceptive neuromuscular facilitation technique, a significant difference in gait patterns was reported in amputees, such as in stride length and cadence [14]. In contrast, another study [8] found no significant changes in walking speed and ability in two children. These results may have been because of the low number of participants, and according to the authors, a possible underestimation of exercise and training frequency. However, there is no way to confirm this outcome since the study [8] lacked fundamental information about the exercise protocol. Finally, some investigations [10,17] demonstrated improvements in gait after training sessions. In addition, transtibial amputees had more considerable improvements than transfemoral amputees in relation to the gait pattern [9].
One study reported an increase in body weight in the non-amputated limb among amputees in the control group who maintained their normal activities [11], which can lead to postural asymmetries that can influence gait and cause low back pain and osteoarthritis [24]. This finding indicated that individuals who kept their normal activities maintained or worsened their gait pattern, unlike those who engaged in resistance training, demonstrating that resistance training may be essential to attenuate changes in walking in this population.
Amputee individuals consume more energy when walking than non-amputees [26]. However, after an exercise protocol in one study [15], there was a reduction in the oxygen consumption of individuals in the intervention group. This also occurred in a case study preparing an amputee for a bicycle race [15]. Nevertheless, it should be noted that in this latter investigation, the participant also exercised on a stationary bicycle in addition to resistance training. Regarding the ability of amputees to run, one study [15] found most transtibial and transfemoral amputees were able to run, but the bilateral amputee did not want to attempt running in this study.
4.5.4. Chronic Low Back Pain
Many amputees suffer from low back pain [24], with one study reporting 46% of participants had chronic low back pain and 58% of these participants were not affected by this problem prior to amputation [29]. Only one investigation sought to identify the effects of resistance training in lower limb amputees with chronic low back pain [12]. Their findings demonstrated resistance training can contribute to strengthening essential muscles in the lumbar region. However, it should be noted that studies that attempted to understand changes in gait, attenuation of the strength deficit, and strengthening of the lumbar musculature after intervention with resistance training may contribute to the understanding of the topic of chronic low back pain, since changes in gait and strength deficit are factors associated with chronic low back pain [3,24,29].
4.6. Locomotion and Accessibility
It is known that people with disabilities suffer from a lack of accessibility. Some authors [30] reported one of the main difficulties in their research was the lack of accessible transportation for participants to travel to the intervention site. In line with this, one study [17] suggested that they could not obtain the results of their research if assistance for the transportation of participants was unavailable. In addition, another investigation [31] also presented transport as a barrier to the practice of resistance training by people with disabilities. They also mentioned that adaptations were necessary for the training space, equipment, and exercises. As this can be a determining factor for an intervention, it is essential to consider accessibility and transport issues.
One of the goals of resistance training is to facilitate the practitioner’s daily tasks [18]. In several studies presented in this review with walking and balance as an outcome measure, an improvement in these measures was reported after a resistance training protocol [9,10,15,17], including visual and somatosensory limitations [11]. In addition, another aspect to be highlighted is the study by Nolan [15] in which amputees could run after a training protocol.
4.7. Other Results
One study demonstrated cardiovascular improvement; however, resistance training was not the only exercise used in this study [16]. Changes in muscle tone occurred in another investigation [8].
Quality of life may be reduced after the amputation process [32,33]. Low back pain is one of the causes that affect the quality of life of amputees [3,34]. The findings of other studies [12] can contribute to the discussion of this problem, in addition to other investigations that can indirectly alleviate chronic low back pain. One study pointed to an improvement in the quality of life of people with disabilities; however, this study was not specifically conducted with amputees [30]. However, in contrast with this study [30], another study reported it was not possible to identify improvements in the amputee’s quality of life [10].
5. Review Limitations
The present work had some limitations. The varied study designs and other exercise methods, such as aerobic exercise, in addition to resistance training during the interventions should be highlighted. The short duration of the studies and lack of presented information regarding the number of sessions and their duration in some studies were also limiting factors. The low methodological quality of the studies should also be highlighted, including the lack of fundamental methodological details for future replicability of the studies. Another point that should be emphasized is the small sample size combined with the heterogeneity of the participants, making more solid analyses difficult.
6. Conclusions
This systematic review aimed to analyze the effects of resistance training in individuals with lower limb amputation by investigating whether resistance training for this population can provide benefits or has contraindications, as well as identify the main resistance training strategies for this population. Interventions with resistance training and other training methods were sufficient to achieve strength gains in muscles of the lower limbs, hips, core, and lumbar region. In addition, improved postural stability resulted in increased confidence in balance, improved gait pattern and speed when walking, as well as gaining the ability to run.
In light of the results reported in this review, it is worthwhile to note that resistance training combined with other exercises appears to be beneficial for this population, attenuating the strength deficit, risk of falling, changes in gait, and chronic low back pain. However, it is impossible to identify resistance training as the main factor responsible for these benefits from the findings in the investigations, nor even to indicate that the positive effects presented would be observed with this training method in isolation.
The benefits of resistance training in amputees, as well as in non-amputees, seem to outweigh the risks. Although unusual hazards were not found in this review, it is known that any training method can pose risks to healthy and unhealthy practitioners. It should be noted that it may be necessary to adapt resistance exercises to the condition of the lower limb amputee. Facilitating access to training can also assist in developing an effective exercise program.
Another point to consider is the need to develop new investigations, especially studies with higher methodological quality such as randomized clinical trials, preferably using only resistance training as an intervention to better understand the effects of the isolated intervention. As expected, interventions with resistance training made possible gains for this population. Given this, it is noteworthy that the main finding of this review is that the observed effects may differ according to the level of amputation, with mainly transtibial and transfemoral amputations analyzed.
7. Resistance Training Practical Recommendations for Amputees
Lower limb amputees can follow different exercise models, such as those using free weights, circuits, weight machines, and using their own body mass. However, closed chain exercises on weight machines should be prioritized. Other training modes, such as balance and aerobic exercises, should ideally be used to support resistance training. It should be noted that it is recommended that exercises be adapted to the practitioner if necessary. Training should be performed 2 to 3 times a week per muscle group, with sets varying between 1 and 3 for strength gains, with 10 to 12 or 15 repetitions, prioritizing the principle of progressivity. It was not possible to define an ideal rest period. Regarding the rest interval, we suggest following the ACMS recommendations (2014) of two to three minutes of rest.
It is recommended to use the 10RM test to define 1RM and the RM percentage should be defined based on the exercise program’s objectives. Thus, it is suggested to follow the ACSM’s recommendations (2014); however, one should consider starting an exercise program for this population with 40–50% of 1RM. Regarding the training objectives, strengthening the lumbar region, hips, and lower limbs is recommended to reduce the strength deficit. To alleviate chronic low back pain, strengthening the lumbar region is recommended. Finally, to improve balance and gait pattern, strengthening the muscles of the hips and lower limbs is recommended. Table 6 contain a Resistance training practical recommendations for amputees.

Table 6.
Resistance training practical recommendations for amputees.
Author Contributions
Conceptualization, M.L.V.V.R.; methodology, M.L.V.V.R., K.R.C.F. and C.M.B.; writing—original draft preparation, M.L.V.V.R. and C.M.B.; writing—review and editing, P.B.C., C.M.B.; G.C.-L., R.A.P., I.D. and A.L.B.d.S.; supervision, C.M.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. World Report on Disability 2011. 2011. Available online: https://apps.who.int/iris/rest/bitstreams/53067/retrieve (accessed on 22 July 2022).
- Ziegler-Graham, K.; MacKenzie, E.J.; Ephraim, P.L.; Travison, T.G.; Brookmeyer, R. Estimating the prevalence of limb loss in the united states: 2005 to 2050. Arch. Phys. Med. Rehabil. 2008, 89, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Hewson, A.; Dent, S.; Sawers, A. Strength deficits in lower limb prosthesis users: A scoping review. Prosthet. Orthot. Int. 2020, 44, 323–340. [Google Scholar] [CrossRef] [PubMed]
- Wilhoite, S.; Williams, S.; Cook, J.; Ryan, G. Rehabilitation, guidelines, and exercise prescription for lower limb amputees. Strength Cond. J. 2020, 42, 95–102. [Google Scholar] [CrossRef]
- Fleck, S.J.; Kraemer, W.J. Fundamentos do Treinamento de Força Muscular, 4th ed.; Artmed Editora: Porto Alegre, Brasil, 2017. [Google Scholar]
- Galvão, T.F.; de Souza Andrade Pansani, T.; Harrad, D. Principais itens para relatar Revisões sistemáticas e Meta-análises: A recomendação PRISMA. Epidemiol. Serv. Saúde 2015, 24, 335–342. [Google Scholar] [CrossRef]
- Smart, N.A.; Waldron, M.; Ismail, H.; Giallauria, F.; Vigorito, C.; Cornelissen, V.; Dieberg, G. Validation of a new tool for the assessment of study quality and reporting in exercise training studies: TESTEX. Int. J. Evid. Based Healthc. 2015, 13, 9–18. [Google Scholar] [CrossRef]
- García-García, Ó.; Mosteiro, S.; Suárez-Iglesias, D.; Ayán, C. Exercise training program in children with lower-limb amputation. Rev. Assoc. Med. Bras. 2021, 67, 277–281. [Google Scholar] [CrossRef]
- Miller, C.A.; Williams, J.E.; Durham, K.L.; Hom, S.C.; Smith, J.L. The effect of a supervised community–based exercise program on balance, balance confidence, and gait in individuals with lower limb amputation. Prosthet. Orthot. Int. 2017, 41, 446–454. [Google Scholar] [CrossRef]
- Mosteiro-Losada, S.; Varela, S.; García-García, O.; Martínez-Lemos, I.; Ayán, C. Effects of including core strengthening exercise as part of a comprehensive rehabilitation programmes on people with lower-limb amputation: A pilot study. Int. J. Ther. Rehabil. 2021, 28, 1–10. [Google Scholar] [CrossRef]
- Schafer, Z.A.; Vanicek, N. A block randomised controlled trial investigating changes in postural control following a personalised 12-week exercise programme for individuals with lower limb amputation. Gait Posture 2021, 84, 198–204. [Google Scholar] [CrossRef]
- Shin, M.K.; Yang, H.S.; Yang, H.E.; Kim, D.H.; Ahn, B.R.; Kwon, H.; Lee, J.H.; Jung, S.; Choi, H.C.; Yun, S.K.; et al. Effects of lumbar strengthening exercise in lower-limb amputees with chronic low back pain. Ann. Rehabil. Med. 2018, 42, 59. [Google Scholar] [CrossRef]
- Tipchatyotin, S.; Choochuay, S.; Kaewwongkot, C.; Wongphaet, P. The effects of isokinetic hip muscles training on gait performance in above-knee amputees: A quasi-experimental study. J. Med. Assoc. Thail. 2020, 103, 128–133. Available online: http://www.jmatonline.com/index.php/jmat/article/view/10624 (accessed on 7 July 2022).
- Anjum, H.; Amjad, I.; Malik, A.N. Effectiveness of proprioceptive neuromuscular facilitation techniques as compared to traditional strength training in gait training among transtibial amputees. J. Coll. Physicians Surg. Pak. 2016, 26, 503–506. [Google Scholar]
- Nolan, L. A training programme to improve hip strength in persons with lower limb amputation. J. Rehabil. Med. 2012, 44, 241–248. [Google Scholar] [CrossRef]
- Donachy, J.; Brannon, K.; Hughes, L.; Seahorn, J.; Crutcher, T.; Christian, E. Strength and endurance training of an individual with left upper and lower limb amputations. Disabil. Rehabil. 2004, 26, 495–499. [Google Scholar] [CrossRef]
- Pauley, T.; Devlin, M.; Madan-Sharma, P. A single-blind, cross-over trial of hip abductor strength training to improve Timed Up & Go performance in patients with unilateral, transfemoral amputation. J. Rehabil. Med. 2014, 46, 264–270. [Google Scholar] [CrossRef]
- Campos, D.B.P. Diretrizes do ACSM para os Testes de Esforço e sua Prescrição, 9th ed.; Editora Guanabara: Rio de Janeiro, Brasil, 2014. [Google Scholar]
- Ferreira, E.G.; De Souza, W.J.; Da Silva, C.A.P.; Novikoff, C.; Rosário, V.H.R.D.; De Oliveira, P.S.P.; Triani, F.D.S. O acesso para cadeirantes em academias de ginástica: Um estudo realizado na Zona Oeste do Rio de Janeiro. Rev. Assoc. Bras. Ativ. Mot. Adapt. 2018, 19, 39–48. [Google Scholar] [CrossRef]
- Medola, F.O.; Macedo, D.L.; Carreri, D.S.S.; Marques, E.F.A.; Kikuchi, L.T.; Costa, N.L.; Busto, R.M. Acessibilidade de um centro de treinamento esportivo para usuários de cadeira de rodas. Rev. Neurociências 2011, 19, 244–249. [Google Scholar] [CrossRef]
- Miller, W.C.; Speechley, M.; Deathe, B. The prevalence and risk factors of falling and fear of falling among lower extremity amputees. Arch. Phys. Med. Rehabil. 2001, 82, 1031–1037. [Google Scholar] [CrossRef]
- Baraúna, M.; Duarte, F.; Sanchez, H.; Canto, R.; Malusa, S.; Campelo-Silva, C.; Ventura-Silva, R. Avaliação do equilíbrio estático em indivíduos amputados de membros inferiores através da biofotogrametria computadorizada. Rev. Bras. Fisioter. 2006, 10, 83–90. [Google Scholar] [CrossRef]
- Wong, C.; Chihuri, S.; Li, G. Risk of fall-related injury in people with lower limb amputations: A prospective cohort study. J. Rehabil. Med. 2016, 48, 80–85. [Google Scholar] [CrossRef]
- Nolan, L.; Wit, A.; Dudziñski, K.; Lees, A.; Lake, M.; Wychowañski, M. Adjustments in gait symmetry with walking speed in trans-femoral and trans-tibial amputees. Gait Posture 2003, 17, 142–151. [Google Scholar] [CrossRef] [PubMed]
- Lamoth, C.J.C.; Ainsworth, E.; Polomski, W.; Houdijk, H. Variability and stability analysis of walking of transfemoral amputees. Med. Eng. Phys. 2010, 32, 1009–1014. [Google Scholar] [CrossRef] [PubMed]
- Bona, R.L.; Peyré-Tartaruga, L.A. Mecânica e Energética da Locomoção de Amputados: Uma Revisão. Pensar Prática 2011, 14, 1–14. [Google Scholar] [CrossRef]
- Kaufman, K.R.; Frittoli, S.; Frigo, C.A. Gait asymmetry of transfemoral amputees using mechanical and microprocessor-controlled prosthetic knees. Clin. Biomech. 2012, 27, 460–465. [Google Scholar] [CrossRef] [PubMed]
- Wasser, J.G.; Vincent, K.R.; Herman, D.C.; Vincent, H.K. Potential lower extremity amputation-induced mechanisms of chronic low back pain: Role for focused resistance exercise. Disabil. Rehabil. 2020, 42, 3713–3721. [Google Scholar] [CrossRef]
- Schinaider, A.P.S.; Garcez, A.; Sant’Anna, P.C.F. Prevalência de dor lombar em pacientes com amputação de membro inferior atendidos em um centro de reabilitação da região metropolitana de Porto Alegre/RS (Br). RSD 2020, 9, e866998004. [Google Scholar] [CrossRef]
- Sanchez, G.C.; Alves, M.H.; Arroyo, C.T.; de Olveira, E.L. Treinamento resistido para pessoas com deficiência física: Qualidade de vida, autonomia e independência. Rev. Assoc. Bras. Ativ. Mot. Adapt. 2021, 22, 15–26. [Google Scholar] [CrossRef]
- Monteiro, J.A.; Silva, M.S. A importância da atividade física para os deficientes físicos. Lect. Educ. Física Deportes 2010, 148. Available online: https://efdeportes.com/efd148/atividade-fisica-para-os-deficientes-fisicos.htm (accessed on 7 July 2022).
- Pastre, C.M.; Salioni, J.F.; Oliveira, B.A.F.; Micheletto, M.; Netto Júnior, J. Fisioterapia e amputação transtibial. Arq. Ciênc. Saúde 2005, 120–124. Available online: http://repositorio-racs.famerp.br/racs_ol/Vol-12-2/11.pdf (accessed on 7 July 2022).
- Sinha, R.; van den Heuvel, W.J.; Arokiasamy, P. Factors affecting quality of life in lower limb amputees. Prosthet. Orthot. Int. 2011, 35, 90–96. [Google Scholar] [CrossRef]
- Christensen, J.; Ipsen, T.; Doherty, P.; Langberg, H. Physical and social factors determining quality of life for veterans with lower-limb amputation(S): A systematic review. Disabil. Rehabil. 2016, 38, 2345–2353. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).