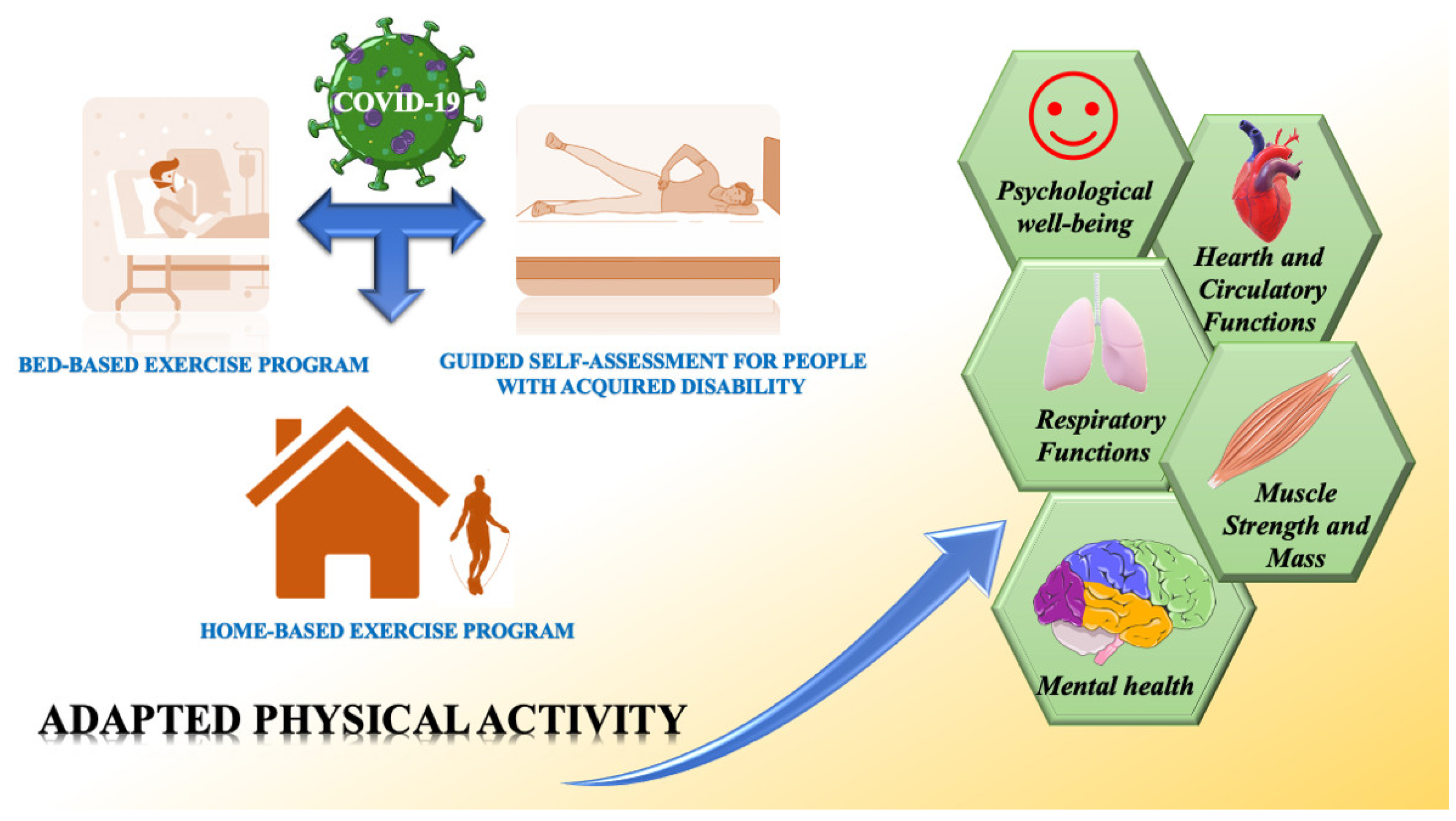
Adapted Physical Activity to Ensure the Physical and Psychological Well-Being of COVID-19 Patients
Abstract
1. Introduction
2. The Beneficial Effects of Physical Activity before COVID-19 Infection
3. Adapted Physical Activity Program during COVID-19 Infection
4. Adapted Physical Activity Program Post COVID-19 Infection
5. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Koh, D. COVID-19 lockdowns throughout the world. Occup. Med. 2020, 70, kqaa073. [Google Scholar] [CrossRef]
- Mishra, M.K. The World after COVID-19 and Its Impact on Global Economy. 2020. Available online: https://www.econstor.eu/handle/10419/215931 (accessed on 26 January 2021).
- Fernandes, N. Economic Effects of Coronavirus Outbreak (Covid-19) on the World Economy; SSRN: Rochester, NY, USA, 2020. [Google Scholar]
- Horton, R. Offline: COVID-19 is not a pandemic. Lancet 2020, 396, 874. [Google Scholar] [CrossRef]
- Bergamin, M.; Musumeci, G. The utility of Anti-Covid-19 desks in Italy, doubts and criticism. J. Funct. Morphol. Kinesiol. 2021, 6, 2. [Google Scholar] [CrossRef] [PubMed]
- Ravalli, S.; Musumeci, G. Coronavirus outbreak in Italy. Physiological benefits of home-based exercise during pandemic. J. Funct. Morphol. Kinesiol. 2020, 5, 31. [Google Scholar] [CrossRef] [PubMed]
- Giustino, V.; Parroco, A.M.; Gennaro, A.; Musumeci, G.; Palma, A.; Battaglia, G. Physical activity levels and related energy expenditure during covid-19 quarantine among the sicilian active population: A cross-sectional online survey study. Sustainability 2020, 12, 4356. [Google Scholar] [CrossRef]
- Paoli, A.; Musumeci, G. Elite athletes and covid-19 lockdown: Future health concerns for an entire sector. J. Funct. Morphol. Kinesiol. 2020, 5, 30. [Google Scholar] [CrossRef]
- Methnani, J.; Amor, D.; Yousfi, N.; Bouslama, A.; Omezzine, A.; Bouhlel, E. Sedentary behavior, exercise and COVID-19: Immune and metabolic implications in obesity and its comorbidities. J. Sports Med. Phys. Fit. 2020. [Google Scholar] [CrossRef]
- Narici, M.; De Vito, G.; Franchi, M.; Paoli, A.; Moro, T.; Marcolin, G.; Grassi, B.; Baldassarre, G.; Zuccarelli, L.; Biolo, G.; et al. Impact of sedentarism due to the COVID-19 home confinement on neuromuscular, cardiovascular and metabolic health: Physiological and pathophysiological implications and recommendations for physical and nutritional countermeasures. Eur. J. Sport Sci. 2020, 12, 1–22. [Google Scholar] [CrossRef]
- Castrogiovanni, P.; Di Rosa, M.; Ravalli, S.; Castorina, A.; Guglielmino, C.; Imbesi, R.; Vecchio, M.; Drago, F.; Szychlinska, M.A.; Musumeci, G. Moderate physical activity as a prevention method for knee osteoarthritis and the role of synoviocytes as biological key. Int. J. Mol. Sci. 2019, 20, 511. [Google Scholar] [CrossRef]
- Szychlinska, M.A.; Castrogiovanni, P.; Trovato, F.M.; Nsir, H.; Zarrouk, M.; Lo Furno, D.; Di Rosa, M.; Imbesi, R.; Musumeci, G. Physical activity and Mediterranean diet based on olive tree phenolic compounds from two different geographical areas have protective effects on early osteoarthritis, muscle atrophy and hepatic steatosis. Eur. J. Nutr. 2019, 58, 565–581. [Google Scholar] [CrossRef]
- Maugeri, G.; D’agata, V. Effects of physical activity in amyotrophic lateral sclerosis. J. Funct. Morphol. Kinesiol. 2020, 5, 29. [Google Scholar] [CrossRef] [PubMed]
- Van Praag, H.; Christie, B.R.; Sejnowski, T.J.; Gage, F.H. Running enhances neurogenesis, learning, and long-term potentiation in mice. Proc. Natl. Acad. Sci. USA 1999, 96, 13427–13431. [Google Scholar] [CrossRef] [PubMed]
- Van Minnen, A.; Hendriks, L.; Olff, M. When do trauma experts choose exposure therapy for PTSD patients? A controlled study of therapist and patient factors. Behav. Res. Ther. 2010, 48, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Cao, X. COVID-19: Immunopathology and its implications for therapy. Nat. Rev. Immunol. 2020, 20, 269–270. [Google Scholar] [CrossRef] [PubMed]
- Parsons, T.; Banks, S.; Bae, C.; Gelber, J.; Alahmadi, H.; Tichauer, M. COVID-19-associated acute disseminated encephalomyelitis (ADEM). J. Neurol. 2020, 267, 2799–2802. [Google Scholar] [CrossRef] [PubMed]
- Paterson, R.W.; Brown, R.L.; Benjamin, L.; Nortley, R.; Wiethoff, S.; Bharucha, T.; Jayaseelan, D.L.; Kumar, G.; Raftopoulos, R.E.; Zambreanu, L.; et al. The emerging spectrum of COVID-19 neurology: Clinical, radiological and laboratory findings. Brain 2020, 143, 3104–3120. [Google Scholar] [CrossRef]
- Padroni, M.; Mastrangelo, V.; Asioli, G.M.; Pavolucci, L.; Abu-Rumeileh, S.; Piscaglia, M.G.; Querzani, P.; Callegarini, C.; Foschi, M. Guillain-Barré syndrome following COVID-19: New infection, old complication? J. Neurol. 2020, 267, 1877–1879. [Google Scholar] [CrossRef]
- Wu, Y.; Xu, X.; Chen, Z.; Duan, J.; Hashimoto, K.; Yang, L.; Liu, C.; Yang, C. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav. Immun. 2020, 87, 18–22. [Google Scholar] [CrossRef]
- Di Rosa, M.; Castrogiovanni, P.; Musumeci, G. The synovium theory: Can exercise prevent knee osteoarthritis? the role of “mechanokines”, a possible biological key. J. Funct. Morphol. Kinesiol. 2019, 4, 11. [Google Scholar] [CrossRef]
- Nieman, D.C.; Wentz, L.M. The compelling link between physical activity and the body’s defense system. J. Sport Health Sci. 2019, 8, 201–217. [Google Scholar] [CrossRef]
- Liu, J.; Li, S.; Liu, J.; Liang, B.; Wang, X.; Wang, H.; Li, W.; Tong, Q.; Yi, J.; Zhao, L.; et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. EBioMedicine 2020, 55, 102763. [Google Scholar] [PubMed]
- Merad, M.; Martin, J.C. Pathological inflammation in patients with COVID-19: A key role for monocytes and macrophages. Nat. Rev. Immunol. 2020, 20, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Petersen, A.M.W.; Pedersen, B.K. The anti-inflammatory effect of exercise. J. Appl. Physiol. 2005, 98, 1154–1162. [Google Scholar] [CrossRef]
- Fernández-Lázaro, D.; González-Bernal, J.J.; Sánchez-Serrano, N.; Navascués, L.J.; Ascaso-Del-Río, A.; Mielgo-Ayuso, J. Physical Exercise as a Multimodal Tool for COVID-19: Could It Be Used as a Preventive Strategy? Int. J. Environ. Res. Public Health 2020, 17, 8496. [Google Scholar] [CrossRef]
- Scully, D.; Kremer, J.; Meade, M.M.; Graham, R.; Dudgeon, K. Physical exercise and psychological well-being: A critical review. Br. J. Sports Med. 1998, 32, 111–120. [Google Scholar] [CrossRef]
- Fox, K.R. The influence of physical activity on mental well-being. Publ. Health Nutr. 1999, 2, 411–418. [Google Scholar] [CrossRef]
- Crews, D.J.; Landers, D.M. A meta-analytic review of aerobic fitness and reactivity to psychosocial stressors. Med. Sci. Sports Exerc. 1987, 19 (Suppl. 5), S114–S120. [Google Scholar] [CrossRef]
- Bodnar, R.J.; Klein, G.E. Endogenous opiates and behavior: 2003. Peptides 2004, 25, 2205–2256. [Google Scholar] [CrossRef]
- Phillips, C. Brain-derived neurotrophic factor, depression, and physical activity: Making the neuroplastic connection. Neural. Plast. 2017, 7260130. [Google Scholar] [CrossRef]
- Lesser, I.A.; Nienhuis, C.P. The impact of COVID-19 on physical activity behavior and well-being of Canadians. Int. J. Environ. Res. Public Health 2020, 17, 3899. [Google Scholar] [CrossRef]
- Maugeri, G.; Castrogiovanni, P.; Battaglia, G.; Pippi, R.; D’Agata, V.; Palma, A.; Di Rosa, M.; Musumeci, G. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon 2020, 6, e04315. [Google Scholar] [CrossRef] [PubMed]
- Duncan, G.E.; Avery, A.R.; Seto, E.; Tsang, S. Perceived change in physical activity levels and mental health during COVID-19: Findings among adult twin pairs. PLoS ONE 2020, 15, e0237695. [Google Scholar] [CrossRef] [PubMed]
- Carriedo, A.; Cecchini, J.A.; Fernandez-Rio, J.; Méndez-Giménez, A. COVID-19, Psychological well-being and physical activity levels in older adults during the nationwide lockdown in spain. Am. J. Geriatr. Psychiatry 2020, 28, 1146–1155. [Google Scholar] [CrossRef] [PubMed]
- Brailovskaia, J.; Cosci, F.; Mansueto, G.; Miragall, M.; Herrero, R.; Baños, R.M.; Krasavtseva, Y.; Kochetkov, Y.; Margraf, J. The association between depression symptoms, psychological burden caused by Covid-19 and physical activity: An investigation in Germany, Italy, Russia, and Spain. Psychiatry Res. 2020, 295, 113596. [Google Scholar] [CrossRef]
- McCoy, J.G.; McKenna, J.T.; Connolly, N.P.; Poeta, D.L.; Ling, L.; McCarley, R.W.; Strecker, R.E. One week of exposure to intermittent hypoxia impairs attentional set-shifting in rats. Behav. Brain Res. 2010, 210, 123–126. [Google Scholar] [CrossRef][Green Version]
- Nunnari, G.; Sanfilippo, C.; Castrogiovanni, P.; Imbesi, R.; Volti, G.L.; Barbagallo, I.; Musumeci, G.; Di Rosa, M. Network perturbation analysis in human bronchial epithelial cells following SARS-CoV2 infection. Exp. Cell Res. 2020, 395, 112204. [Google Scholar] [CrossRef]
- Danese, A.; Moffitt, T.E.; Pariante, C.M.; Ambler, A.; Poulton, R.; Caspi, A. Elevated inflammation levels in depressed adults with a history of childhood maltreatment. Arch. Gen. Psychiatry 2008, 65, 409–415. [Google Scholar] [CrossRef]
- Vivar, C.; Potter, M.C.; van Praag, H. All about running: Synaptic plasticity, growth factors and adult hippocampal neurogenesis. Curr. Top Behav. Neurosci. 2013, 15, 189–210. [Google Scholar]
- Ryan, S.M.; Nolan, Y.M. Neuroinflammation negatively affects adult hippocampal neurogenesis and cognition: Can exercise compensate? Neurosci. Biobehav. Rev. 2016, 61, 121–131. [Google Scholar] [CrossRef]
- Song, H.; Peng, W.; Lee, K.M. Promoting exercise self-efficacy with an exergame. J. Health Commun. 2011, 16, 148–162. [Google Scholar] [CrossRef] [PubMed]
- Viana, R.B.; de Lira, C.A.B. Exergames as coping strategies for anxiety disorders during the COVID-19 quarantine period. Games Health 2020, 9, 3. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Szabo, A. Effects of yoga on stress among healthy adults: A systematic review. Altern. Ther. Health Med. 2020, 26, AT6214. [Google Scholar]
- Pellegrini, B.; Peyré-Tartaruga, L.; Zoppirolli, C.; Bortolan, L.; Bacchi, E.; Figard-Fabre, H.; Schena, F. Exploring muscle activation during nordic walking: A comparison between conventional and uphill walking. PLoS ONE 2015, 10, e0138906. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, G.; Carnazza, M.L.; Loreto, C.; Leonardi, R.; Loreto, C. β-Defensin-4 (HBD-4) is expressed in chondrocytes derived from normal and osteoarthritic cartilage encapsulated in PEGDA scaffold. Acta Histochem. 2012, 114, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Bieler, T.; Siersma, V.; Magnusson, S.P.; Kjaer, M.; Christensen, H.E.; Beyer, N. In hip osteoarthritis, Nordic Walking is superior to strength training and home-based exercise for improving function. Scand. J. Med. Sci. Sports 2017, 27, 873–886. [Google Scholar] [CrossRef] [PubMed]
- Lipowski, M.; Walczak-Kozłowska, T.; Lipowska, M.; Kortas, J.; Antosiewicz, J.; Falcioni, G.; Ziemann, E. Improvement of attention, executive functions, and processing speed in elderly women as a result of involvement in the nordic walking training program and vitamin d supplementation. Nutrients 2019, 11, 1311. [Google Scholar] [CrossRef]
- Park, S.D.; Yu, S.H. The effects of Nordic and general walking on depression disorder patients’ depression, sleep, and body composition. J. Phys. Ther. Sci. 2015, 27, 2481–2485. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maugeri, G.; Musumeci, G. Adapted Physical Activity to Ensure the Physical and Psychological Well-Being of COVID-19 Patients. J. Funct. Morphol. Kinesiol. 2021, 6, 13. https://doi.org/10.3390/jfmk6010013
Maugeri G, Musumeci G. Adapted Physical Activity to Ensure the Physical and Psychological Well-Being of COVID-19 Patients. Journal of Functional Morphology and Kinesiology. 2021; 6(1):13. https://doi.org/10.3390/jfmk6010013
Chicago/Turabian StyleMaugeri, Grazia, and Giuseppe Musumeci. 2021. "Adapted Physical Activity to Ensure the Physical and Psychological Well-Being of COVID-19 Patients" Journal of Functional Morphology and Kinesiology 6, no. 1: 13. https://doi.org/10.3390/jfmk6010013
APA StyleMaugeri, G., & Musumeci, G. (2021). Adapted Physical Activity to Ensure the Physical and Psychological Well-Being of COVID-19 Patients. Journal of Functional Morphology and Kinesiology, 6(1), 13. https://doi.org/10.3390/jfmk6010013





