Comparison of Mandibular Arch Expansion by the Schwartz Appliance Using Two Activation Protocols: A Preliminary Retrospective Clinical Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
- -
- Class 1 malocclusion
- -
- Mixed dentition
- -
- Moderate to severe crowding (−4 mm or more)
- -
- Age at the beginning of the treatment < 9 years
- -
- Exclusion criteria were:
- -
- Posterior cross-bite
- -
- Previous orthodontic treatment
- -
- Dental agenesis
- -
- Systemic syndromes
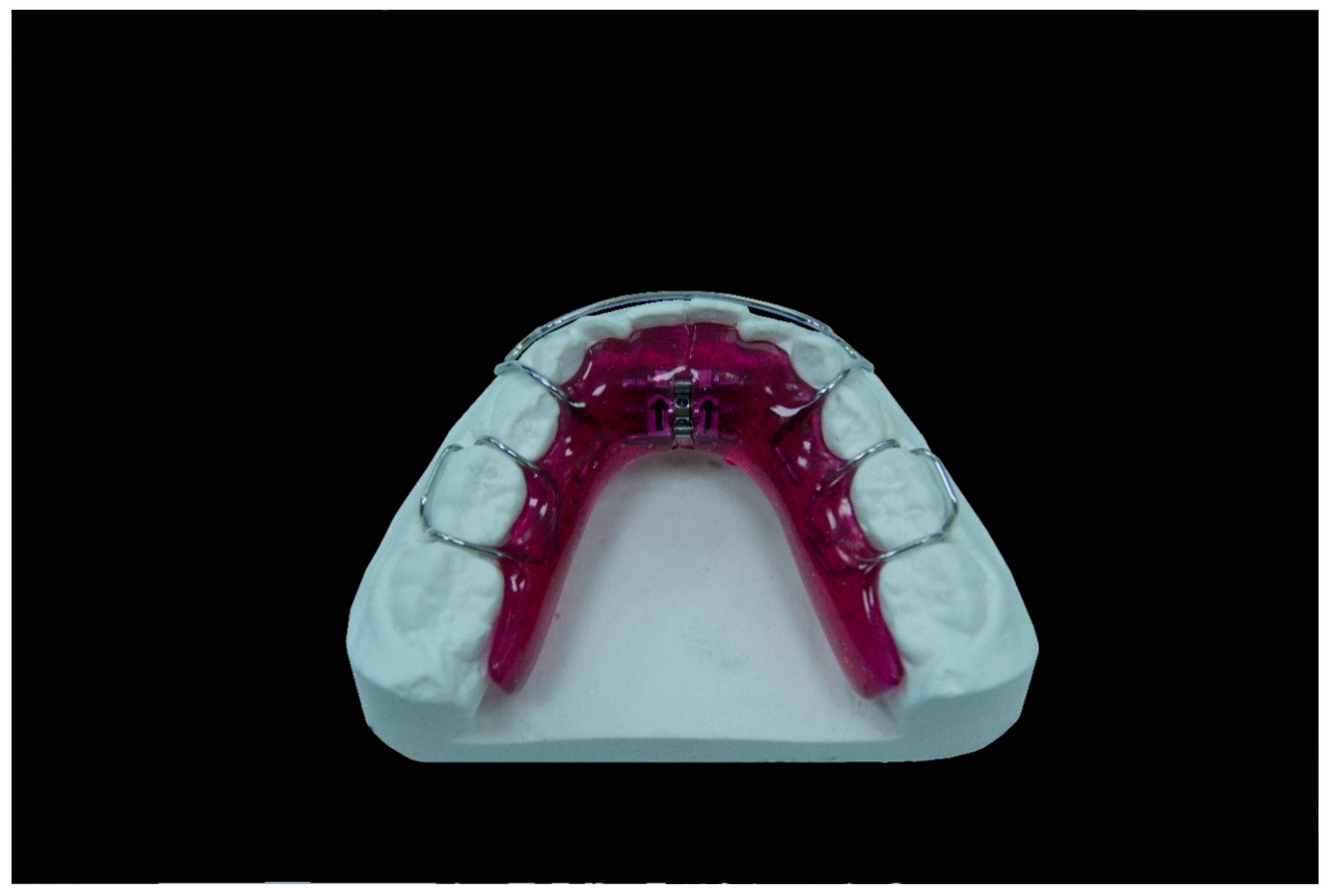
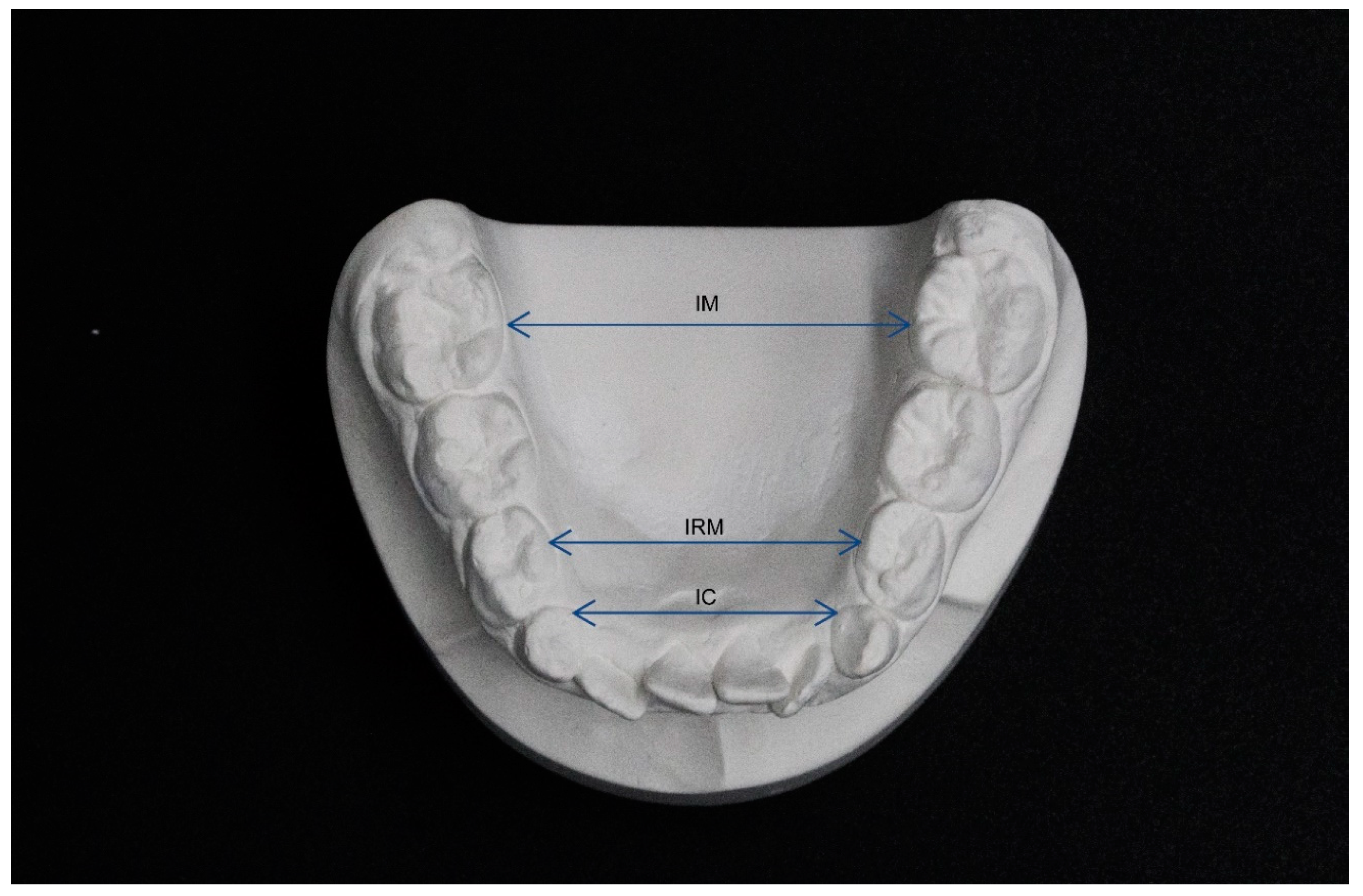
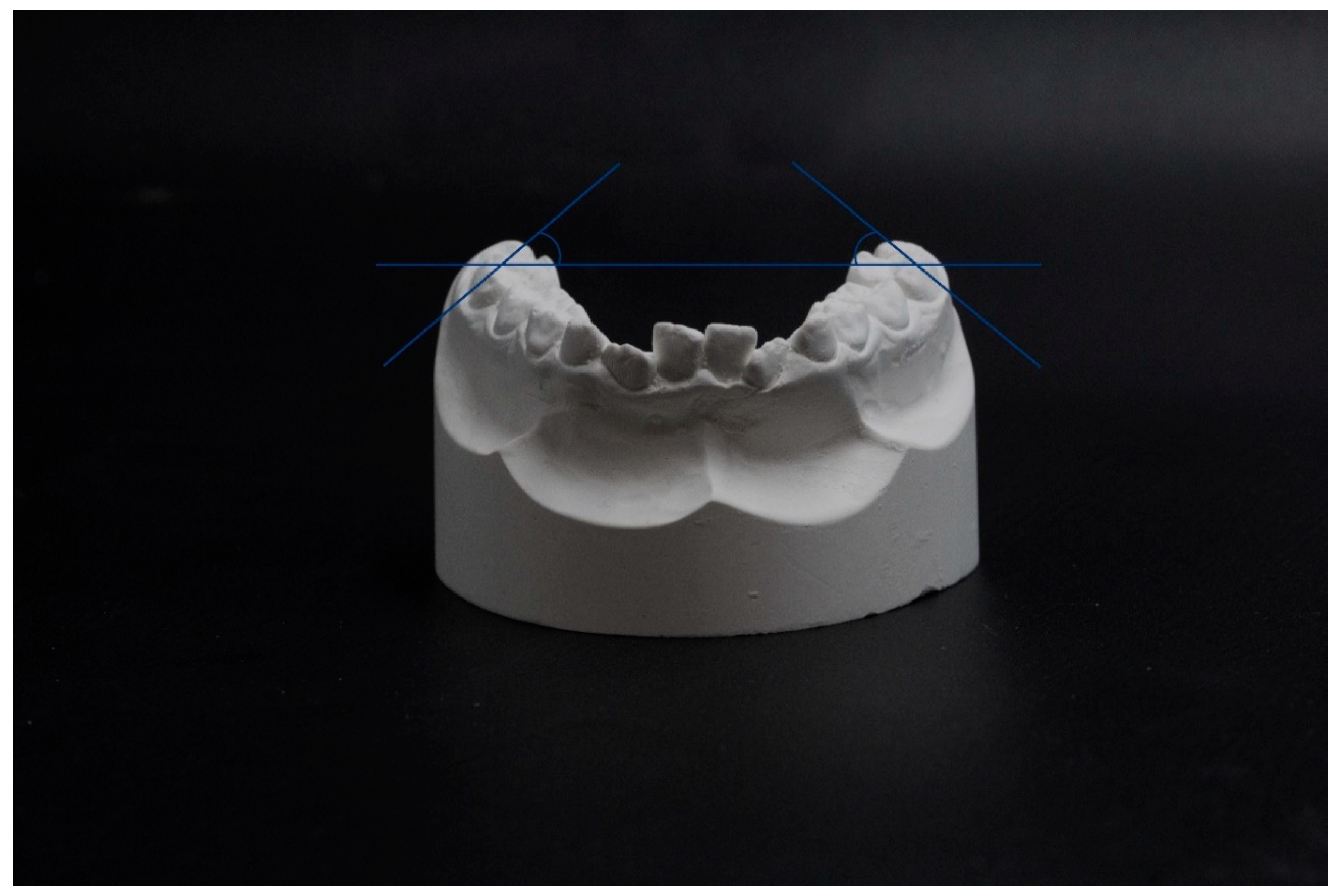
2.2. Measurements of Dental Cast
- -
- segment (a): from the mesial aspect of the right first permanent molar to the distal aspect of the right permanent or deciduous canine
- -
- segment (b): from the distal aspect of the right permanent or deciduous canine to the contact point between the permanent central incisors
- -
- segment (c): from the contact point between the permanent central incisors to the distal aspect of the left permanent or deciduous canine
- -
- segment (d): from the distal aspect of the left permanent or deciduous canine to the mesial aspect of the left first permanent molar.
2.3. Treatment Protocols
2.4. Statistical Methods
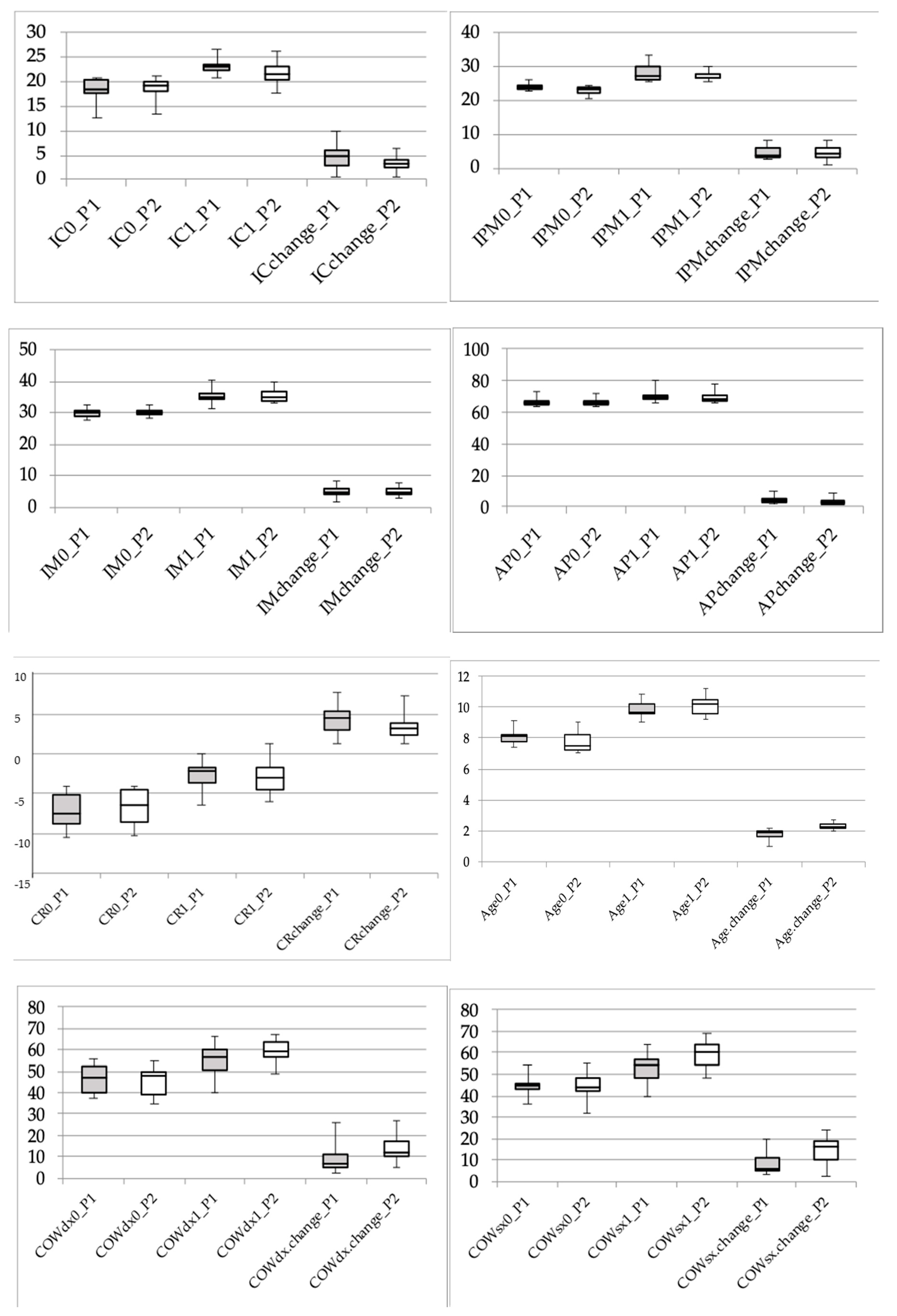
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Leighton, B.C. The early development of normal occlusion. Trans. Eur. Orthod. Soc. 1975, 7, 67–77. [Google Scholar]
- Brunelle, J.A.; Bhat, M.; Lipton, J.A. Prevalence and distribution of selected occlusal characteristcs in the US population, 1988–1991. J. Dent. Res. 1996, 75, 706–713. [Google Scholar] [CrossRef] [PubMed]
- Buschang, P.H. Class I malocclusion—The development and etiology of mandibular malaligments. Semin. Orthod. 2004, 20, 3–15. [Google Scholar] [CrossRef]
- Sillmann, J.H. Dimensional changes of the dental arches: Longitudinal study from birth to 25 years. Am. J. Orthod. 1964, 50, 824–842. [Google Scholar] [CrossRef]
- Mauad, B.A.; Silva, R.C.; Aragón, M.L.S.C.; Pontes, L.F.; Silva Júnior, N.G.; Normando, D. Changes in lower dental arch dimensions and tooth alignment in young adults without orthodontic treatment. Dent. Press J. Orthod. 2015, 20, 64–68. [Google Scholar] [CrossRef][Green Version]
- Von Cramon-Taubadel, N. Global human mandibular variation reflects differences in agricultural and hunter-gatherer subsistence strategies. Proc. Natl. Acad. Sci. USA 2011, 108, 19546–19551. [Google Scholar] [CrossRef]
- Thilander, B. Dentoalveolar development in subjects with normal occlusion. A longitudinal study between the ages of 5 and 31 years. Eur. J. Ortod. 2009, 31, 109–120. [Google Scholar] [CrossRef]
- Crossley, A.M.; Campbell, P.M.; Tadlock, L.P.; Schneiderman, E.; Buschang, P.H. Is there a relationsip between dental crowding and the size of the maxillary or mandibular apical base? Angle Orthod. 2020, 90, 216–223. [Google Scholar] [CrossRef]
- Zigante, M.; Pavlic, A.; VandevskaRadunovic, V.; Mathewson, A.; KotaracKnezevic, A.; Spalj, S. Changes of mandibular dental arch shape during adolescence and its influence on late mandibular incisor crowding. J. Comp. Hum. Biol. 2019, 70, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Giannelly, A. Treatment of crowding in the mixed dentition. Am. J. Orthod. Dentofac. Orthop. 2002, 121, 569–571. [Google Scholar] [CrossRef]
- Tai, K.; Hotokezaka, H.; Park, J.H.; Tai, H.; Miyajima, K.; Choi, M.; Kai, L.M.; Mishima, K. Preliminary cone-beam computed tomography study evaluating the dental and skeletal changes after treatment with a mandibular Schwartz appliance. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 262e.1–262e.11. [Google Scholar] [CrossRef]
- Tai, K.; Park, J.H.; Mishima, K.; Shin, J. 3-Dimensional cone-beam computed tomography analysis of transverse changes with Schwartz appliances on both jaws. Angle Orthod. 2011, 81, 670–677. [Google Scholar] [CrossRef] [PubMed]
- O’Grady, P.W.; McNamara, J.A., Jr.; Baccetti, T.; Franchi, L. A long-term evaluation of the mandibular Schwartz appliance and the acrylic splint expander in early mixed dentition patients. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 202–213. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.A., Jr. Maxillary transverse deficiency. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 567–570. [Google Scholar] [CrossRef]
- Bishara, S.E.; Staley, R.N. Maxillary expansion: Clinical implications. Am. J. Orthod. Dentofac. Orthop. 1987, 91, 3–14. [Google Scholar] [CrossRef]
- Raucci, G.; Pachêco-Pereira, C.; Elyasi, M.; d’Apuzzo, F.; Flores-Mir, C.; Perillo, L. Short- and long-term evaluation of mandibular dental arch dimensional changes in patients treated with lip bumper during mixed dentition followed by fixed appliances. Angle Orthod. 2016, 86, 753–760. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Wahlsten, D. Chapter 5—Sample size. In Mouse Behavioral Testing; Wahlsten, D., Ed.; Academic Press: London, UK, 2011. [Google Scholar]
- Reuscl, R.P.; Heuer, W.; Stiesch, M.; Wenzel, D.; Dittmer, M.P. Reliability and validity of measurements on digital study models and plaster models. Eur. J. Orthod. 2016, 38, 22–26. [Google Scholar] [CrossRef]
- Santoro, M.; Galkin, S.; Teredesai, M.; Nicolay, O.F.; Cangialosi, T.J. Comparison of measurements made on digital and plaster models. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 101–105. [Google Scholar] [CrossRef]
- Wendling, L.K.; McNamara, J.A., Jr.; Franchi, L.; Baccetti, T. A prospective study of the short term treatment effects of the acrylic-splint rapid maxillary expander combined with the lower Schwartz appliance. Angle Orthod. 2004, 75, 7–14. [Google Scholar]
- Walter, D.C. Changes in the form and dimentions of dental arches resulting from orthodontic treatment. Angle Orthod. 1953, 23, 3–18. [Google Scholar]
- Quinzi, V.; Rossi, O.; Paglia, L.; Marzo, G.; Caprioglio, A. Paediatric orthodontics part 2: Periodontal effects of maxillary expansion. Eur. J. Paediatr. Dent. 2019, 20, 164–166. [Google Scholar] [PubMed]
- Quinzi, V.; Scibetta, E.T.; Marchetti, E.; Mummolo, S.; Bruno Giannì, A.; Romano, M.; Beltramini, G.; Marzo, G. Analyze my face. J. Biol. Regul. Homeost. Agents 2018, 32, 149–158. [Google Scholar] [PubMed]
- Dinoi, M.T.; Marchetti, E.; Garagiola, U.; Caruso, S.; Mummolo, S.; Marzo, G. Orthodontic treatment of an unerupted mandibular canine tooth in a patient with mixed dentition: A case report. J. Med. Case Rep. 2016, 10, 1–4. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Santonocito, S.; Alibrandi, A.; Ferlito, S. Expression of salivary and serum malondialdehyde and lipid profile of patients with periodontitis and coronary heart disease. Int. J. Mol. Sci. 2019, 20, 6061. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Iorio-Siciliano, V.; Alibrandi, A.; Ramaglia, L.; Leonardi, R. Effectiveness of a nutraceutical agent in the non-surgical periodontal therapy: A randomized, controlled clinical trial. Clin. Oral Investig. 2020, 1007, 1–11. [Google Scholar] [CrossRef]
- Isola, G.; Alibrandi, A.; Currò, M.; Matarese, M.; Ricca, S.; Matarese, G.; Ientile, R.; Kocher, T. Evaluation of salivary and serum ADMA levels in patients with periodontal and cardiovascular disease as subclinical marker of cardiovascular risk. J. Periodontol. 2020, 1–9. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Alibrandi, A.; Indelicato, F.; Ferlito, S. Analysis of endothelin-1 concentrations in individuals with periodontitis. Sci. Rep. 2020, 10, 1652. [Google Scholar] [CrossRef]
- Isola, G.; Alibrandi, A.; Rapisarda, E.; Matarese, G.; Williams, R.C.; Leonardi, R. Association of Vitamin D in patients with periodontitis: A cross-sectional study. J. Periodontal Res. 2020, 1–11. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Ortensi, L.; Farronato, M.; Lucchese, A.; Lo Castro, E.; Isola, G. The step further smile virtual planning: Milled versus prototyped mock-ups for the evaluation of the designed smile characteristics. BMC Oral Health 2020, 20, 165. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Ronsivalle, V.; Grippaudo, C.; Lucchese, A.; Muraglie, S.; Lagravère, M.O.; Isola, G. One step before 3D printing-evaluation of imaging software accuracy for 3-dimensional analysis of the mandible: A comparative study using a surface-to-surface matching technique. Materials 2020, 13, 2798. [Google Scholar] [CrossRef] [PubMed]

| Protocol | 1 | Protocol | 2 | Effectsize | ANOVA’s p | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 95 | % | CI | 95 | % | CI | Prot | Sex | P*S | Time | P*T | S*T | P*S*T | |||||||||||
| Variable | n | Mean | ± | SD | Lower | ; | Upper | n | Mean | ± | SD | Lower | ; | Upper | Cohen’s d | ||||||||
| IC | 0.639 | 0.764 | 0.170 | < 0.001 | 0.139 | 0.047 | 0.524 | ||||||||||||||||
| T0 | 12 | 18.5 | ± | 2.3 | 17.1 | ; | 19.9 | 11 | 18.6 | ± | 2.1 | 17.2 | ; | 20.0 | 0.05 | - | |||||||
| T1 | 12 | 23.0 | ± | 1.4 | 22.1 | ; | 23.9 | 11 | 22.0 | ± | 2.4 | 20.3 | ; | 23.6 | 0.52 | s | |||||||
| change | 12 | 4.5 | ± | 2.4 | 3.0 | ; | 6.0 | 11 | 3.4 | ± | 1.8 | 2.2 | ; | 4.5 | 0.52 | s | |||||||
| IPM | 0.050 | 0.463 | 0.024 | < 0.001 | 0.699 | 0.856 | 0.301 | ||||||||||||||||
| T0 | 12 | 24.1 | ± | 1.1 | 23.4 | ; | 24.8 | 11 | 22.7 | ± | 1.3 | 21.9 | ; | 23.6 | 1.17 | ml | |||||||
| T1 | 12 | 28.5 | ± | 2.5 | 26.9 | ; | 30.1 | 11 | 27.4 | ± | 1.4 | 26.4 | ; | 28.3 | 0.54 | s | |||||||
| change | 12 | 4.4 | ± | 2.0 | 3.1 | ; | 5.7 | 11 | 4.6 | ± | 2.1 | 3.2 | ; | 6.0 | 0.10 | s | |||||||
| IM | 0.842 | 0.772 | 0.087 | < 0.001 | 0.861 | 0.930 | 0.192 | ||||||||||||||||
| T0 | 12 | 30.2 | ± | 1.4 | 29.3 | ; | 31.1 | 11 | 30.3 | ± | 1.3 | 29.5 | ; | 31.2 | 0.07 | - | |||||||
| T1 | 12 | 35.2 | ± | 2.2 | 33.8 | ; | 36.6 | 11 | 35.6 | ± | 2.2 | 34.1 | ; | 37.1 | 0.18 | s | |||||||
| change | 12 | 5.0 | ± | 1.8 | 3.9 | ; | 6.2 | 11 | 5.3 | ± | 1.6 | 4.2 | ; | 6.3 | 0.18 | s | |||||||
| Archperimeter | 0.879 | 0.745 | 0.537 | < 0.001 | 0.547 | 0.455 | 0.709 | ||||||||||||||||
| T0 | 12 | 66.2 | ± | 2.5 | 64.6 | ; | 67.7 | 11 | 66.2 | ± | 2.4 | 64.6 | ; | 67.9 | 0.00 | - | |||||||
| T1 | 12 | 70.2 | ± | 4.0 | 67.7 | ; | 72.8 | 11 | 69.5 | ± | 4.4 | 66.6 | ; | 72.5 | 0.17 | s | |||||||
| change | 12 | 4.1 | ± | 2.7 | 2.4 | ; | 5.7 | 11 | 3.3 | ± | 2.4 | 1.6 | ; | 4.9 | 0.31 | s | |||||||
| Crowding | 0.762 | 0.532 | 0.583 | < 0.001 | 0.493 | 0.229 | 0.197 | ||||||||||||||||
| T0 | 12 | −7.1 | ± | 2.3 | −8.5 | ; | −5.6 | 11 | −6.6 | ± | 2.3 | −8.1 | ; | −5.0 | 0.22 | s | |||||||
| T1 | 12 | −2.8 | ± | 1.9 | −4.0 | ; | −1.6 | 11 | −2.9 | ± | 2.3 | −4.5 | ; | −1.4 | 0.05 | - | |||||||
| change | 12 | 4.3 | ± | 2.0 | 3.0 | ; | 5.5 | 11 | 3.4 | ± | 1.7 | 2.3 | ; | 4.5 | 0.48 | s | |||||||
| COWR | 0.398 | 0.089 | 0.271 | < 0.001 | 0.107 | 0.562 | 0.608 | ||||||||||||||||
| T0 | 12 | 46.0 | ± | 6.9 | 41.6 | ; | 50.4 | 11 | 45.4 | ± | 7.0 | 40.7 | ; | 50.0 | 0.09 | - | |||||||
| T1 | 12 | 54.9 | ± | 8.2 | 49.7 | ; | 60.1 | 11 | 59.5 | ± | 5.4 | 55.9 | ; | 63.1 | 0.66 | sm | |||||||
| change | 12 | 8.9 | ± | 6.7 | 4.6 | ; | 13.2 | 11 | 14.1 | ± | 6.6 | 9.6 | ; | 18.5 | 0.78 | sm | |||||||
| COWL | 0.079 | 0.059 | 0.070 | < 0.001 | 0.024 | 0.775 | 0.514 | ||||||||||||||||
| T0 | 12 | 44.0 | ± | 4.7 | 41.0 | ; | 47.0 | 11 | 44.4 | ± | 6.8 | 39.8 | ; | 48.9 | 0.07 | - | |||||||
| T1 | 12 | 52.2 | ± | 7.0 | 47.7 | ; | 56.6 | 11 | 59.1 | ± | 6.8 | 54.5 | ; | 63.7 | 1.00 | m | |||||||
| change | 12 | 8.2 | ± | 4.9 | 5.0 | ; | 11.3 | 11 | 14.7 | ± | 6.8 | 10.2 | ; | 19.3 | 1.11 | ml | |||||||
| Age | < 0.001 | 0.291 | 0.378 | ||||||||||||||||||||
| T0 | 12 | 8.1 | ± | 0.5 | 7.8 | ; | 8.4 | 11 | 7.8 | ± | 0.7 | 7.3 | ; | 8.2 | 0.50 | s | |||||||
| T1 | 12 | 9.8 | ± | 0.5 | 9.5 | ; | 10.2 | 11 | 10.1 | ± | 0.6 | 9.7 | ; | 10.5 | 0.55 | s | |||||||
| change | 12 | 1.8 | ± | 0.4 | 1.5 | ; | 2.0 | 11 | 2.3 | ± | 0.2 | 2.2 | ; | 2.5 | 1.56 | l | |||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quinzi, V.; Mummolo, S.; Bertolazzi, F.; Campanella, V.; Marzo, G.; Marchetti, E. Comparison of Mandibular Arch Expansion by the Schwartz Appliance Using Two Activation Protocols: A Preliminary Retrospective Clinical Study. J. Funct. Morphol. Kinesiol. 2020, 5, 61. https://doi.org/10.3390/jfmk5030061
Quinzi V, Mummolo S, Bertolazzi F, Campanella V, Marzo G, Marchetti E. Comparison of Mandibular Arch Expansion by the Schwartz Appliance Using Two Activation Protocols: A Preliminary Retrospective Clinical Study. Journal of Functional Morphology and Kinesiology. 2020; 5(3):61. https://doi.org/10.3390/jfmk5030061
Chicago/Turabian StyleQuinzi, Vincenzo, Stefano Mummolo, Francesca Bertolazzi, Vincenzo Campanella, Giuseppe Marzo, and Enrico Marchetti. 2020. "Comparison of Mandibular Arch Expansion by the Schwartz Appliance Using Two Activation Protocols: A Preliminary Retrospective Clinical Study" Journal of Functional Morphology and Kinesiology 5, no. 3: 61. https://doi.org/10.3390/jfmk5030061
APA StyleQuinzi, V., Mummolo, S., Bertolazzi, F., Campanella, V., Marzo, G., & Marchetti, E. (2020). Comparison of Mandibular Arch Expansion by the Schwartz Appliance Using Two Activation Protocols: A Preliminary Retrospective Clinical Study. Journal of Functional Morphology and Kinesiology, 5(3), 61. https://doi.org/10.3390/jfmk5030061







