Craniomandibular Disorders in Pregnant Women: An Epidemiological Survey
Abstract
1. Introduction
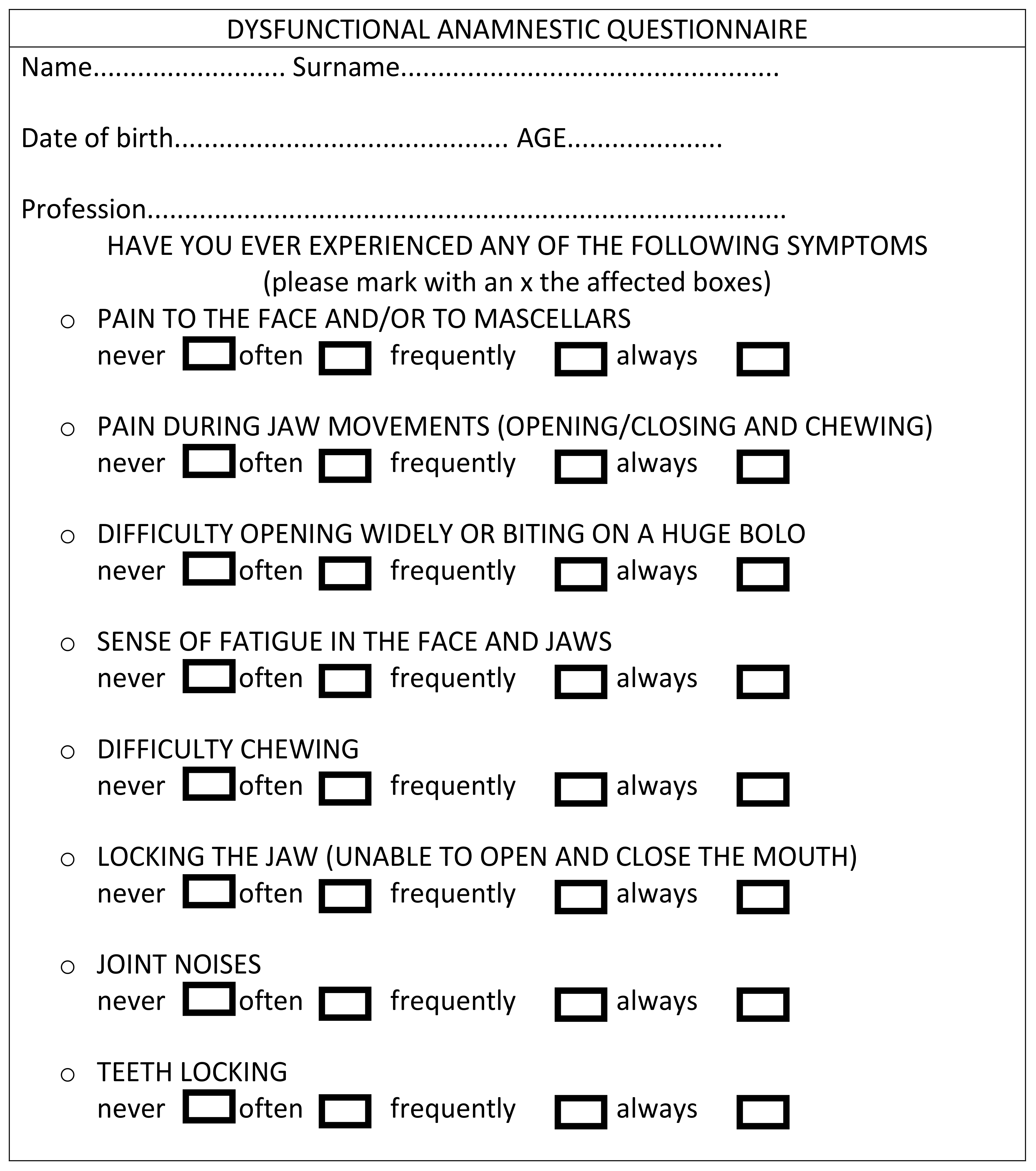
2. Materials and Methods
2.1. Study Design
2.2. Power Sample Analysis
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Furquim, B.D.; Flamengui, L.M.; Conti, P.C. TMD and chronic pain: A current view. Dent. Press J. Orthod. 2015, 20, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Castelo, P.M.; Gaviao, M.B.; Pereira, L.J.; Bonjardim, L.R. Relationship between oral parafunctional/nutritive sucking habits and temporomandibular joint dysfunction in primary dentition. Int. J. Paediatr. Dent. 2005, 15, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Mackie, A.; Lyons, K. The role of occlusion in temporomandibular disorders--a review of the literature. N. Z. Dent. J. 2008, 104, 54–59. [Google Scholar] [PubMed]
- Okeson, J.P. Management of Temporomandibular Disorder and Occlusion -E -Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2008; pp. 1–333. [Google Scholar] [CrossRef]
- Chisnoiu, A.M.; Chisnoiu, R.; Moldovan, M.; Lascu, L.M.; Picos, A.M. Etiological factors associated with temporomandibular joint disorder - Study on animal model. Rom. J. Morphol. Embryol. 2016, 57, 185–189. [Google Scholar] [PubMed]
- Mortazavi, S.H.; Motamedi, M.H.; Navi, F.; Pourshahab, M.; Bayanzadeh, S.M.; Hajmiragha, H.; Isapour, M. Outcomes of management of early temporomandibular joint disorders: How effective is nonsurgical therapy in the long-term? Natl. J. Maxillofac. Surg. 2010, 1, 108–111. [Google Scholar]
- Lo Giudice, A.; Rustico, L.; Caprioglio, A.; Migliorati, M.; Nucera, R. Evaluation of condylar cortical bone thickness in patient groups with different vertical facial dimensions using cone-beam computed tomography. Odontology 2020. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Brewer, I.; Leonardi, R.; Roberts, N.; Bagnato, G. Pain threshold and temporomandibular function in systemic sclerosis: Comparison with psoriatic arthritis. Clin. Rheumatol. 2018, 37, 1861–1867. [Google Scholar] [CrossRef]
- Ferendiuk, E.; Zajdel, K.; Pihut, M. Incidence of otolaryngological symptoms in patients with temporomandibular joint dysfunctions. Biomed Res. Int. 2014, 2014, 824684. [Google Scholar] [CrossRef][Green Version]
- Velly, A.M.; Schiffman, E.L.; Rindal, D.B.; Cunha-Cruz, J.; Gilbert, G.H.; Lehmann, M.; Horowitz, A.; Fricton, J. The feasibility of a clinical trial of pain related to temporomandibular muscle and joint disorders: The results of a survey from the Collaboration on Networked Dental and Oral Research dental practice-based research networks. J. Am. Dent. Assoc. 2013, 144, e1–e10. [Google Scholar] [CrossRef]
- Leonardi, R.; Loreto, C.; Talic, N.; Caltabiano, R.; Musumeci, G. Immunolocalization of lubricin in the rat periodontal ligament during experimental tooth movement. Acta Histochem. 2012, 114, 700–704. [Google Scholar] [CrossRef]
- Loreto, C.; Leonardi, R.; Musumeci, G.; Pannone, G.; Castorina, S. An ex vivo study on immunohistochemical localization of MMP-7 and MMP-9 in temporomandibular joint discs with internal derangement. Eur. J. Histochem. 2013, 57, e12. [Google Scholar] [CrossRef]
- Musumeci, G.; Castrogiovanni, P.; Leonardi, R.; Trovato, F.M.; Szychlinska, A.; Di Giunta, A.; Loreto, C.; Castorina, S. New perspectives for articular cartilage repair treatment through tissue engineering: A contemporary review. World J. Orthop. 2014, 18, 80–88. [Google Scholar] [CrossRef]
- Musumeci, G.; Trovato, F.M.; Loreto, C.; Leonardi, R.; Szychlinska, M.A.; Castorina, S.; Mobasheri, A. Lubricin expression in human osteoarthritic knee meniscus and synovial fluid: A morphological, immunohistochemical and biochemical study. Acta Histochem. 2014, 116, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Cavuoti, S.; Matarese, G.; Isola, G.; Abdolreza, J.; Femiano, F.; Perillo, L. Combined orthodontic-surgical management of a transmigrated mandibular canine. Angle Orthod. 2016, 86, 681–691. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, R.; Perrotta, R.E.; Almeida, L.E.; Loreto, C.; Musumeci, G. Lubricin in synovial fluid of mild and severe temporomandibular joint internal derangements. Med. Oral Patol. Oral Cir. Bucal. 2016, 21, e793–e799. [Google Scholar] [CrossRef] [PubMed]
- Szychlinska, M.A.; Trovato, F.M.; Di Rosa, M.; Malaguarnera, L.; Puzzo, L.; Leonardi, R.; Castrogiovanni, P.; Musumeci, G. Co-Expression and Co-Localization of Cartilage Glycoproteins CHI3L1 and Lubricin in Osteoarthritic Cartilage: Morphological, Immunohistochemical and Gene Expression Profiles. Int. J. Mol. Sci. 2016, 17, 359. [Google Scholar] [CrossRef]
- Loreto, C.; Chiarenza, G.P.; Musumeci, G.; Castrogiovanni, P.; Imbesi, R.; Ruggeri, A.; Almeida, L.E.; Leonardi, R.; Leonardi, R. ADAM10 localization in temporomandibular joint disk with internal derangement: An ex vivo immunohistochemical study. Acta Histochem. 2016, 118, 293–298. [Google Scholar] [CrossRef][Green Version]
- Leonardi, R.; Perrotta, R.E.; Loreto, C.; Musumeci, G.; Crimi, S.; Dos Santos, J.N.; Rusu, M.C.; Bufo, P.; Barbato, E.; Pannone, G. Toll-like Receptor 4 Expression in the Epithelium of Inflammatory Periapical Lesions. An Immunohistochemical Study. Eur. J. Histochem. 2015, 59, 2547. [Google Scholar] [CrossRef]
- Leonardi, R.; Lo Giudice, A.; Rugeri, M.; Muraglie, S.; Cordasco, G.; Barbato, E. Three-dimensional evaluation on digital casts of maxillary palatal size and morphology in patients with functional posterior crossbite. Eur. J. Orthod. 2018, 40, 556–562. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Fastuca, R.; Portelli, M.; Militi, A.; Bellocchio, M.; Spinuzza, P.; Briguglio, F.; Caprioglio, A.; Nucera, R. Effects of rapid vs slow maxillary expansion on nasal cavity dimensions in growing subjects: A methodological and reproducibility study. Eur. J. Paediatr. Dent. 2017, 18, 299–304. [Google Scholar] [CrossRef]
- Koidis, P.T.; Zarifi, A.; Grigoriadou, E.; Garefis, P. Effect of age and sex on craniomandibular disorders. J. Prosthet. Dent. 1993, 69, 93–101. [Google Scholar] [CrossRef]
- Leonardi, R.; Loreto, C.; Barbato, E.; Polimeni, A.; Caltabiano, R.; Lo Muzio, L. A histochemical survey of the human temporomandibular joint disc of patients with internal derangement without reduction. J. Craniofac. Surg. 2007, 18, 1429–1433. [Google Scholar] [CrossRef] [PubMed]
- Cutroneo, G.; Piancino, M.G.; Ramieri, G.; Bracco, P.; Vita, G.; Isola, G.; Vermiglio, G.; Favaloro, A.; Anastasi, G.P.; Trimarchi, F. Expression of muscle-specific integrins in masseter muscle fibers during malocclusion disease. Int. J. Mol. Med. 2012, 30, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Almeida, L.E.; Pierce, S.; Zacharias, J.; Cullinan, W.; Noronha, L.; Olandoski, M.; Tramontina, V.; Loreto, C.; Leonardi, R. Immunohistochemical analysis of IL-1 beta in the discs of patients with temporomandibular joint dysfunction. Cranio 2017, 35, 233–237. [Google Scholar] [CrossRef]
- Leonardi, R.; Muraglie, S.; Crimi, S.; Pirroni, M.; Musumeci, G.; Perrotta, R. Morphology of palatally displaced canines and adjacent teeth, a 3-D evaluation from cone-beam computed tomographic images. BMC Oral Health 2018, 18, 156. [Google Scholar] [CrossRef]
- Almeida, L.E.; Hresko, K.; Sorenson, A.; Butcher, S.; Tayebi, L.; Leonardi, R.; Loreto, C.; Bosio, J.; Camejo, F.; Doetzer, A. Immunohistochemical expression of TLR-4 in temporomandibular joint dysfunction. Cranio 2019, 37, 323–328. [Google Scholar] [CrossRef]
- Di Rosa, M.; Szychlinska, M.A.; Tibullo, D.; Malaguarnera, L.; Musumeci, G. Expression of CHI3L1 and CHIT1 in osteoarthritic rat cartilage model. A morphological study. Eur. J. Histochem. 2014, 58, 2423. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Santonocito, S.; Alibrandi, A.; Ferlito, S. Expression of salivary and serum malondialdehyde and lipid profile of patients with periodontitis and coronary heart disease. Int. J. Mol. Sci. 2019, 20, 6061. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Ortensi, L.; Farronato, M.; Lucchese, A.; Lo Castro, A.; Isola, G. The step further smile virtual planning: Milled versus prototyped mock-ups for the evaluation of the designed smile characteristics. A comparative study in the aesthetic area using surface-to-surface matching technique. BMC Oral Health 2020, 20, 166. [Google Scholar]
- Isola, G.; Alibrandi, A.; Pedulla, E.; Grassia, V.; Ferlito, S.; Perillo, L.; Rapisarda, E. Analysis of the effectiveness of lornoxicam and flurbiprofen on management of pain and sequelae following third molar surgery: A randomized, controlled, clinical trial. J. Clin. Med. 2019, 8, 325. [Google Scholar] [CrossRef]
- Isola, G.; Matarese, G.; Alibrandi, A.; Dalessandri, D.; Migliorati, M.; Pedulla, E.; Rapisarda, E. Comparison of effectiveness of etoricoxib and diclofenac on pain and perioperative sequelae after surgical avulsion of mandibular third molars: A randomized, controlled, clinical trial. Clin. J. Pain 2019, 35, 908–915. [Google Scholar] [CrossRef] [PubMed]
- Isola, G.; Perillo, L.; Migliorati, M.; Matarese, M.; Dalessandri, D.; Grassia, V.; Alibrandi, A.; Matarese, G. The impact of temporomandibular joint arthritis on functional disability and global health in patients with juvenile idiopathic arthritis. Eur. J. Orthod. 2019, 41, 117–124. [Google Scholar] [CrossRef]
- Loreto, C.; Filetti, V.; Almeida, L.E.; La Rosa, G.R.M.; Leonardi, R.; Grippaudo, C.; Lo Giudice, A. MMP-7 and MMP-9 are overexpressed in the synovial tissue from severe temporomandibular joint dysfunction. Eur. J. Histochem. 2020, 64. [Google Scholar] [CrossRef] [PubMed]
- Ferlazzo, N.; Curro, M.; Zinellu, A.; Caccamo, D.; Isola, G.; Ventura, V.; Carru, C.; Matarese, G.; Ientile, R. Influence of MTHFR genetic background on p16 and MGMT methylation in oral squamous cell cancer. Int. J. Mol. Sci. 2017, 18, 724. [Google Scholar] [CrossRef] [PubMed]
- Puri, J.; Hutchins, B.; Bellinger, L.L.; Kramer, P.R. Estrogen and inflammation modulate estrogen receptor alpha expression in specific tissues of the temporomandibular joint. Reprod. Biol. Endocrinol. 2009, 7, 155. [Google Scholar] [CrossRef] [PubMed]
- Papka, R.E.; Srinivasan, B.; Miller, K.E.; Hayashi, S. Localization of estrogen receptor protein and estrogen receptor messenger RNA in peripheral autonomic and sensory neurons. Neuroscience 1997, 79, 1153–1163. [Google Scholar] [CrossRef]
- Wang, J.; Chao, Y.; Wan, Q.; Zhu, Z. The possible role of estrogen in the incidence of temporomandibular disorders. Med. Hypotheses 2008, 71, 564–567. [Google Scholar] [CrossRef]
- Bettini, E.; Pollio, G.; Santagati, S.; Maggi, A. Estrogen receptor in rat brain: Presence in the hippocampal formation. Neuroendocrinology 1992, 56, 502–508. [Google Scholar] [CrossRef]
- Castrogiovanni, P.; Trovato, F.M.; Szychlinska, M.A.; Nsir, H.; Imbesi, R.; Musumeci, G. The importance of physical activity in osteoporosis. From the molecular pathways to the clinical evidence. Histol. Histopathol. 2016, 31, 1183–1194. [Google Scholar] [CrossRef]
- Helkimo, M. Studies on function and dysfunction of the masticatory system. 3. Analyses of anamnestic and clinical recordings of dysfunction with the aid of indices. Swed. Dent. J. 1974, 67, 165–181. [Google Scholar]
- Lo Giudice, A.; Nucera, R.; Leonardi, R.; Paiusco, A.; Baldoni, M.; Caccianiga, G. A comparative assessment of the efficiency of orthodontic treatment with and without photobiomodulation during mandibular decrowding in young subjects: A single-center, single-blind randomized controlled trial. Photobiomodul. Photomed. Laser Surg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, A.; Nucera, R.; Perillo, L.; Paiusco, A.; Caccianiga, G. Is Low-level laser therapy an effective method to alleviate pain induced by active orthodontic alignment archwire? A Randomized clinical trial. J. Evid. Based Dent. Pract. 2019, 19, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Mayoral, V.A.; Espinosa, I.A.; Montiel, A.J. Association between signs and symptoms of temporomandibular disorders and pregnancy (case control study). Acta Odontol. Latinoam. 2013, 26, 3–7. [Google Scholar] [PubMed]
- Woodrow, K.M.; Friedman, G.D.; Siegelaub, A.B.; Collen, M.F. Pain tolerance: Differences according to age, sex and race. Psychosom. Med. 1972, 34, 548–556. [Google Scholar] [CrossRef] [PubMed]
- Procacci, P.; Zoppi, M.; Maresca, M.; Romano, S. Studies on the pain threshold in man. Adv. Neurol. 1974, 4, 107–113. [Google Scholar]
- Perillo, L.; Isola, G.; Esercizio, D.; Iovane, M.; Triolo, G.; Matarese, G. Differences in craniofacial characteristics in Southern Italian children from Naples: A retrospective study by cephalometric analysis. Eur. J. Paediatr. Dent. 2013, 14, 195–198. [Google Scholar]
- Isola, G.; Alibrandi, A.; Rapisarda, E.; Matarese, G.; Williams, R.C.; Leonardi, R. Association of vitamin D in patients with periodontitis: A cross-sectional study. J. Periodontal Res. 2020. [Google Scholar] [CrossRef]
- Isola, G.; Giudice, A.L.; Polizzi, A.; Alibrandi, A.; Patini, R.; Ferlito, S. Periodontitis and tooth loss have negative systemic impact on circulating progenitor cell levels: A Clinical study. Genes 2019, 10, 1022. [Google Scholar] [CrossRef]
- Isola, G.; Matarese, G.; Ramaglia, L.; Pedulla, E.; Rapisarda, E.; Iorio-Siciliano, V. Association between periodontitis and glycosylated haemoglobin before diabetes onset: A cross-sectional study. Clin. Oral Investig. 2019. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Alibrandi, A.; Indelicato, F.; Ferlito, S. Analysis of Endothelin-1 Concentrations in individuals with periodontitis. Sci. Rep. 2020, 10, 1652. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Muraglie, S.; Leonardi, R.; Lo Giudice, A. Assessment of Vitamin C and Antioxidant profiles in saliva and serum in patients with periodontitis and ischemic heart disease. Nutrients 2019, 11, 2956. [Google Scholar] [CrossRef] [PubMed]
- Curro, M.; Matarese, G.; Isola, G.; Caccamo, D.; Ventura, V.P.; Cornelius, C.; Lentini, M.; Cordasco, G.; Ientile, R. Differential expression of transglutaminase genes in patients with chronic periodontitis. Oral Dis. 2014, 20, 616–623. [Google Scholar] [CrossRef] [PubMed]
- Briguglio, F.; Briguglio, E.; Briguglio, R.; Cafiero, C.; Isola, G. Treatment of infrabony periodontal defects using a resorbable biopolymer of hyaluronic acid: A randomized clinical trial. Quintessence Int. 2013, 44, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Lupton, D.E. Psychological aspects of temporomandibular joint dysfunction. J. Am. Dent. Assoc. 1969, 79, 131–136. [Google Scholar] [CrossRef]
- Molin, C.; Schalling, D.; Edman, G. Psychological studies of patients with mandibular pain dysfunction syndrome. 1. Personality traits in patients and controls. Sven. Tandlak. Tidskr. 1973, 66, 1–13. [Google Scholar]
- Matarese, G.; Curro, M.; Isola, G.; Caccamo, D.; Vecchio, M.; Giunta, M.L.; Ramaglia, L.; Cordasco, G.; Williams, R.C.; Ientile, R. Transglutaminase 2 up-regulation is associated with RANKL/OPG pathway in cultured HPDL cells and THP-1-differentiated macrophages. Amino Acids 2015, 47, 2447–2455. [Google Scholar] [CrossRef]
- Reiter, S.; Eli, I.; Mahameed, M.; Emodi-Perlman, A.; Friedman-Rubin, P.; Reiter, M.A.; Winocur, E. Pain catastrophizing and pain persistence in temporomandibular disorder patients. J. Oral Facial Pain Headache 2018, 32, 309–320. [Google Scholar] [CrossRef]
- Musumeci, G.; Magro, G.; Cardile, V.; Coco, M.; Marzagalli, R.; Castrogiovanni, P.; Imbesi, R.; Graziano, A.C.; Barone, F.; Di Rosa, M.; et al. Characterization of matrix metalloproteinase-2 and -9, ADAM-10 and N-cadherin expression in human glioblastoma multiforme. Cell Tissue Res. 2015, 362, 45–60. [Google Scholar] [CrossRef]
- Piancino, M.G.; Isola, G.; Cannavale, R.; Cutroneo, G.; Vermiglio, G.; Bracco, P.; Anastasi, G.P. From periodontal mechanoreceptors to chewing motor control: A systematic review. Arch. Oral Biol. 2017, 78, 109–121. [Google Scholar] [CrossRef]
- Matarese, G.; Isola, G.; Anastasi, G.P.; Favaloro, A.; Milardi, D.; Vermiglio, G.; Vita, G.; Cordasco, G.; Cutroneo, G. Immunohistochemical analysis of TGF-beta1 and VEGF in gingival and periodontal tissues: A role of these biomarkers in the pathogenesis of scleroderma and periodontal disease. Int. J. Mol. Med. 2012, 30, 502–508. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Caccianiga, G.; Crimi, S.; Cavallini, C.; Leonardi, R. Frequency and type of ponticulus posticus in a longitudinal sample of nonorthodontically treated patients: Relationship with gender, age, skeletal maturity, and skeletal malocclusion. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 126, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Sassarini, D.J. Depression in midlife women. Maturitas 2016, 94, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, L.R.; Gonzalez, Y.M.; Liu, Y.; Liu, H.; Markova, M.; Gallo, L.M.; Nickel, J.C. TMJ energy densities in healthy men and women. Osteoarthr. Cartil. 2017, 25, 846–849. [Google Scholar] [CrossRef] [PubMed]
- Huhtela, O.S.; Näpänkangas, R.; Joensuu, T.; Raustia, A.; Kunttu, K.; Sipilä, K. Self-Reported Bruxism and symptoms of temporomandibular disorders in Finnish University students. J. Oral Facial Pain Headache 2016, 30, 311–317. [Google Scholar] [CrossRef]
- Isola, G.; Matarese, M.; Briguglio, F.; Grassia, V.; Picciolo, G.; Fiorillo, L.; Matarese, G. Eectiveness of Low-Level Laser Therapy during Tooth Movement: A Randomized Clinical Trial. Materials 2019, 12, 2187. [Google Scholar] [CrossRef]
- Vannuccini, S.; Bocchi, C.; Severi, F.M.; Challis, J.R.; Petraglia, F. Endocrinology of human parturition. Ann. D’endocrinologie 2016, 77, 105–113. [Google Scholar] [CrossRef]
- Isola, G.; Matarese, M.; Ramaglia, L.; Cicciu, M.; Matarese, G. Evaluation of the efficacy of celecoxib and ibuprofen on postoperative pain, swelling, and mouth opening after surgical removal of impacted third molars: A randomized, controlled clinical trial. Int. J. Oral Maxillofac. Surg. 2019, 48, 1348–1354. [Google Scholar] [CrossRef]
- Goh, W.A.; Zalud, I. Placenta accreta: Diagnosis, management and the molecular biology of the morbidly adherent placenta. J. Matern. Fetal Neonatal Med. 2016, 29, 1795–1800. [Google Scholar] [CrossRef]
- Matarese, G.; Isola, G.; Ramaglia, L.; Dalessandri, D.; Lucchese, A.; Alibrandi, A.; Fabiano, F.; Cordasco, G. Periodontal biotype: Characteristic, prevalence and dimensions related to dental malocclusion. Minerva Stomatol. 2016, 65, 231–238. [Google Scholar]
- Cannavale, R.; Matarese, G.; Isola, G.; Grassia, V.; Perillo, L. Early treatment of an ectopic premolar to prevent molar-premolar transposition. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 559–569. [Google Scholar] [CrossRef]
- Isola, G.; Matarese, M.; Ramaglia, L.; Iorio-Siciliano, V.; Cordasco, G.; Matarese, G. Efficacy of a drug composed of herbal extracts on postoperative discomfort after surgical removal of impacted mandibular third molar: A randomized, triple-blind, controlled clinical trial. Clin. Oral Investig. 2019, 23, 2443–2453. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, R.; Almeida, L.E.; Trevilatto, P.C.; Loreto, C. Occurrence and regional distribution of TRAIL and DR5 on temporomandibular joint discs: Comparison of disc derangement with and without reduction. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, 244–251. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Matarese, G.; Isola, G.; Anastasi, G.P.; Cutroneo, G.; Favaloro, A.; Vita, G.; Cordasco, G.; Milardi, D.; Zizzari, V.L.; Tetè, S.; et al. Transforming Growth Factor Beta 1 and Vascular Endothelial Growth Factor levels in the pathogenesis of periodontal disease. Eur. J. Inflamm. 2013, 11, 479–488. [Google Scholar] [CrossRef]
- Trenti, A.; Tedesco, S.; Boscaro, C.; Trevisi, L.; Bolego, C.; Cignarella, A. Estrogen, Angiogenesis, immunity and cell metabolism: Solving the puzzle. Int. J. Mol. Sci. 2018, 19, 859. [Google Scholar] [CrossRef]
- Isola, G.; Anastasi, G.P.; Matarese, G.; Williams, R.C.; Cutroneo, G.; Bracco, P.; Piancino, M.G. Functional and molecular outcomes of the human masticatory muscles. Oral Dis. 2018, 24, 1428–1441. [Google Scholar] [CrossRef] [PubMed]
- Lo Muzio, L.; Campisi, G.; Farina, A.; Rubini, C.; Pastore, L.; Giannone, N.; Colella, G.; Leonardi, R.; Carinci, F. Effect of p63 expression on survival in oral squamous cell carcinoma. Cancer Investig. 2007, 25, 464–469. [Google Scholar] [CrossRef]
- Isola, G.; Alibrandi, A.; Curro, M.; Matarese, M.; Ricca, S.; Matarese, G.; Ientile, R.; Kocher, T. Evaluation of salivary and serum ADMA levels in patients with periodontal and cardiovascular disease as subclinical marker of cardiovascular risk. J. Periodontol. 2020. [Google Scholar] [CrossRef]
- Aufdemorte, T.B.; Van Sickels, J.E.; Dolwick, M.F.; Sheridan, P.J.; Holt, G.R.; Aragon, S.B.; Gates, G.A. Estrogen receptors in the temporomandibular joint of the baboon (Papio cynocephalus): An autoradiographic study. Oral Surg. Oral Med. Oral Pathol. 1986, 61, 307–314. [Google Scholar] [CrossRef]
- Perillo, L.; Padricelli, G.; Isola, G.; Femiano, F.; Chiodini, P.; Matarese, G. Class II malocclusion division 1: A new classification method by cephalometric analysis. Eur. J. Paediatr. Dent. 2012, 13, 192–196. [Google Scholar]
- Sorenson, A.; Hresko, K.; Butcher, S.; Pierce, S.; Tramontina, V.; Leonardi, R.; Loreto, C.; Bosio, J.; Almeida, L.E. Expression of Interleukin-1 and temporomandibular disorder: Contemporary review of the literature. Cranio 2018, 36, 268–272. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Iorio-Siciliano, V.; Alibrandi, A.; Ramaglia, L.; Leonardi, R. Effectiveness of a nutraceutical agent in the non-surgical periodontal therapy: A randomized, controlled clinical trial. Clin. Oral Investig. 2020, in press 7 June. [Google Scholar]
- Nucera, R.; Militi, A.; Lo Giudice, A.; Longo, V.; Fastuca, R.; Caprioglio, A.; Cordasco, G.; Papadopoulos, M.A. Skeletal and Dental Effectiveness of Treatment of Class II Malocclusion With Headgear: A Systematic Review and Meta-analysis. J Evid. Based. Dent. Pract. 2018, 18, 41–58. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, L. Spine and TMJ: A Pathophysiology report. J. Funct. Morphol. Kinesiol. 2020, 5, 24. [Google Scholar] [CrossRef]
- Fiorillo, L.; Musumeci, G. TMJ Dysfunction and Systemic Correlation. J. Funct. Morphol. Kinesiol. 2020, 5, 20. [Google Scholar] [CrossRef]

| TMJ Disfunction | |||||
|---|---|---|---|---|---|
| Positive | Negative | Total | |||
| Study Group | Observed | 87 | 21 | 108 | p < 0.05 |
| Percentage (%) | 81 | 19 | 100 | ||
| Study Group | Observed | 47 | 43 | 90 | |
| Percentage (%) | 52 | 48 | 100 | ||
| Articular Signs | Muscular Pain | Total | |||
|---|---|---|---|---|---|
| Study Group | Observed | 87 | 0 | 87 | p < 0.05 |
| Percentage (%) | 100 | 0 | 100 | ||
| Study Group | Observed | 37 | 10 | 47 | |
| Percentage (%) | 79 | 21 | 100 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fichera, G.; Polizzi, A.; Scapellato, S.; Palazzo, G.; Indelicato, F. Craniomandibular Disorders in Pregnant Women: An Epidemiological Survey. J. Funct. Morphol. Kinesiol. 2020, 5, 36. https://doi.org/10.3390/jfmk5020036
Fichera G, Polizzi A, Scapellato S, Palazzo G, Indelicato F. Craniomandibular Disorders in Pregnant Women: An Epidemiological Survey. Journal of Functional Morphology and Kinesiology. 2020; 5(2):36. https://doi.org/10.3390/jfmk5020036
Chicago/Turabian StyleFichera, Grazia, Alessandro Polizzi, Simone Scapellato, Giuseppe Palazzo, and Francesco Indelicato. 2020. "Craniomandibular Disorders in Pregnant Women: An Epidemiological Survey" Journal of Functional Morphology and Kinesiology 5, no. 2: 36. https://doi.org/10.3390/jfmk5020036
APA StyleFichera, G., Polizzi, A., Scapellato, S., Palazzo, G., & Indelicato, F. (2020). Craniomandibular Disorders in Pregnant Women: An Epidemiological Survey. Journal of Functional Morphology and Kinesiology, 5(2), 36. https://doi.org/10.3390/jfmk5020036






