1. Introduction
Radiation has been employed for many good reasons in numerous sectors, including diagnostic and therapeutic medicine [
1]. The second largest exposure to radiation for human beings comes from medical radiation, following environmental or background radiation. Studies have shown that radiation-induced cancer directly rises with the absorbed dose of radiation [
2]. Ionising radiation, a key tool in medical imaging, presents inherent risks to patients and healthcare professionals. Exposure to ionising radiation can damage living tissue and increase the risk of cancer development. Recognising that long-term exposure or inadequate protection can lead to adverse health effects is crucial. In healthcare settings, awareness of these risks is paramount to implementing rigorous safety measures and ensuring that radiography professionals are adequately trained to minimise exposure and safeguard their and their patients’ well-being [
3]. The field of radiography demands a high level of expertise to ensure accurate diagnostic imaging and patient safety. Skilled radiography professionals possess the knowledge and proficiency necessary to operate radiation-emitting equipment safely, interpret complex images, and collaborate effectively with healthcare teams. Their competence is vital in delivering precise diagnoses and treatments, underscoring their critical role in modern healthcare [
4,
5,
6].
Safety measures in radiography practice are paramount to mitigate the potential risks associated with ionising radiation. These measures encompass stringent protocols for equipment operation, shielding, and radiation monitoring. Emphasising the importance of adhering to these safety practices ensures the well-being of patients, radiography professionals, and the broader healthcare community. By prioritising safety, healthcare institutions can maintain the highest standards of care while minimising the health hazards associated with radiation exposure, reinforcing the commitment to patient and staff safety in radiology departments.
The term “occupational exposure” describes radiation exposure that a worker receives due to the nature of their work [
7,
8]. Monitoring occupational radiation dose is motivated by a profound commitment to safeguarding radiography students, professionals, and patients’ health and well-being. Ionising radiation exposure at work can occur in various settings, including healthcare facilities and academic and research organisations. Further, ionising radiation, while essential in medical imaging, poses inherent risks [
9]. By systematically tracking and assessing the radiation exposure experienced by radiography students during their training, we aim to identify potential health hazards, ensure compliance with safety guidelines, and continuously improve the training protocols. This proactive approach protects individuals and contributes to the long-term sustainability and excellence of the radiography profession, fostering trust in healthcare delivery. Employees exposed to medical radiation sources are advised to adhere to and implement all radiation safety protocols for radiation protection [
7,
10]. The ALARA concept (as low as reasonably achievable) must be observed, and lower exposure levels must be used [
7] by all healthcare professionals in radiology, complying with both international and national requirements, to lower the risk of occupationally exposed workers, regardless of individual and collective dosage levels [
7,
8]. A radiation worker who practices ionising radiation always wears one or more dosimeters, particularly TLDs, which have been authorised by the International Atomic Energy Agency (IAEA) to estimate personal doses. The radiation workers’ exposed area, which typically includes the neck, torso, or waist, is where the TLD badge is meant to be worn. TLDs should be employed in occupational radiation exposure to assess and ensure that the received doses fall below the permitted ranges following national and international radiation protection laws.
Radiography and medical imaging students are required to complete clinical training at a licensed medical facility under the guidance of a certified teacher or preceptor [
11]. The minimal prerequisite information necessary for students before practising ionising radiation is covered in radiation protection and radiobiology courses; nevertheless, there is a learning curve in understanding and implementing radiation protection and safety principles in an actual clinical setting, during which students are exposed to ionising radiation [
12]. Therefore, radiation dose monitoring is necessary during clinical training to give radiography students a sense of safety that they will carry throughout their careers.
Annual exposure limits are provided for workers and students in millisieverts (mSv), and administrative actions are taken when medical radiation exceeds the defined dose limits by comparing the recorded effective dose equivalent to these limits. Trainees’ occupational exposure to radiation and the annual dose limits established by the IAEA [
13], the International Commission on Radiological Protection (ICRP) [
14], and the Federal Nuclear Regulatory Authority of the United Arab Emirates (UAE) [
15] are shown in
Table 1. This study presents a change in the effective radiation dose of students during clinical training since 2015. It compares it with results from previous years and similar studies in other countries. This paves the way for initiating steps to reduce exposure doses to values as low as possible for students and interns.
2. Materials and Methods
This study collected and analysed data on occupational radiation doses through a meticulous and systematic approach. To gather this crucial information, we employed several key methodologies:
- (1)
Dosimetry Devices: Radiography students were equipped with dosimetry devices (TLDs) worn during their training sessions. These dosimeters recorded real-time radiation exposure levels, capturing dose rates and cumulative exposure data.
- (2)
Record-Keeping: Comprehensive records of the radiography training sessions, including imaging modalities, patient types, and procedural details, were meticulously maintained. This information served as valuable contextual data for the dose measurements.
- (3)
Data Compilation: Data from the dosimetry devices and training records were compiled and organised into a database, ensuring data integrity and accessibility for analysis.
- (4)
Statistical Analysis: Various statistical methods, such as descriptive statistics, regression analysis, and comparative studies, were employed to analyse the collected data. These analyses allowed us to identify trends, correlations, and potential areas of concern related to occupational doses.
- (5)
Interpretation: The results of our analysis were interpreted in the context of radiation safety guidelines and industry standards, helping us conclude the implications for safety and training in radiography. By utilising these comprehensive data collection and analysis methods, we gained valuable insights into the occupational radiation dose experienced by radiography students. This information forms the basis of our study’s findings and recommendations to enhance safety protocols and optimise radiography education.
2.1. Sample Background
The Department of Radiation Protection, Ministry of Health, UAE, granted TLDs to undergraduate radiography students from the Department of Diagnostic Medical Imaging at the University of Sharjah between 2015 and 2022 to track their radiation exposure during clinical placement. TLD readings were conducted every 15 weeks of the clinical placement, during which the students spent 384 clinical placement working hours. The students’ ages in this study ranged from 18 to 25 years.
The clinical placement during the study period included general radiography, special fluoroscopy procedures, operation theatre, mammography, dental mobile radiography, computed tomography, interventional radiology, and nuclear medicine. During the placement, a student should finish a minimum number of patient cases: 750 cases of general radiography, 150 of fluoroscopy, 50 of interventional radiology, 150 CT scans, 50 cases in the operation theatre, and 50 cases of nuclear medicine.
2.2. Description of TLDs
TLD cards manufactured by Harshaw™ (Rotunda Scientific Technologies LLC, Stow, OH, USA) contain specially doped lithium fluoride (Li: Mg, Cu, P). The element is covered in the front and back with a thin PTFE (Teflon)-retaining layer, which protects it from contamination. The TLD element is placed in a holder consisting of polypropylene housing with a thick PTFE and a polypropylene filter for the proper placement and accurate measurement of the HP (10). The holder has a circular window covered with PTFE and a thin sleeve placed over a thin TLD window [
16,
17,
18].
The Thermo Scientific model 6600 TLD reader (Waltham, MA, USA) and automated readers are used for whole-body, extremity, neutron, and environmental monitoring. This reader uses nitrogen gas or dry air to control overheating and has a linearity of less than 5%, between 10 μGy and 1 Gy. The system employs LiF material, which provides a high sensitivity and a long monitoring period. In addition, its effective atomic number is nearly comparable to tissue and, thus, exhibits an excellent energy response [
19].
Employing TLDs during occupational exposure is essential to ascertain whether the dosage received is below the permitted limits established by national and international radiological protection regulations. When a crystal is heated in a detector, a TLD monitors the amount of visible light that the heated crystal emits when exposed to ionising radiation. This characteristic is known as thermoluminescence. Radiation exposure affects the light’s intensity when it is released. A curve illustrates this light transmission, which is proportional to the dose applied to the detector.
2.3. Dose Evaluation Procedure
TLD dose measurements are reported every 15 weeks and include HP (0.07) and HP (10), where HP (0.07) measures shallow doses (doses on the skin’s surface) and HP (10) measures deep doses. HP (10) and HP (0.07) are individual measurement reciprocals representing the likelihood of stochastic well-being impacts from radiation; HP (10) is a profound dosage equivalent [
20,
21]. The measurement is the same at 10 mm below the body’s specified location. HP (0.07) refers to surface measurements equivalent and comparable or proportionate to a shallow dosage. The measurement is the same at a depth of 0.07 mm below the body’s surface. One centimetre beneath the skin, the total body dose is measured, and the skin’s surface is marked to measure it. When determining the monitored yearly effective dosage, HP (10) is considered.
2.4. Data Analysis
TLDs from clinical training students who consented to participate in this research each year were obtained for this study. All TLD readings were entered into Excel (Office16, Microsoft, Redmond, WA, USA) and analysed. The mean and standard deviation (SD) were calculated for the annual doses of HP (10) and HP (0.07), and bar graphs and box–whisker plots were created.
3. Results
A data analysis was performed on TLD data gathered from 599 dosimeters belonging to 233 students, with 384 working hours for each reading.
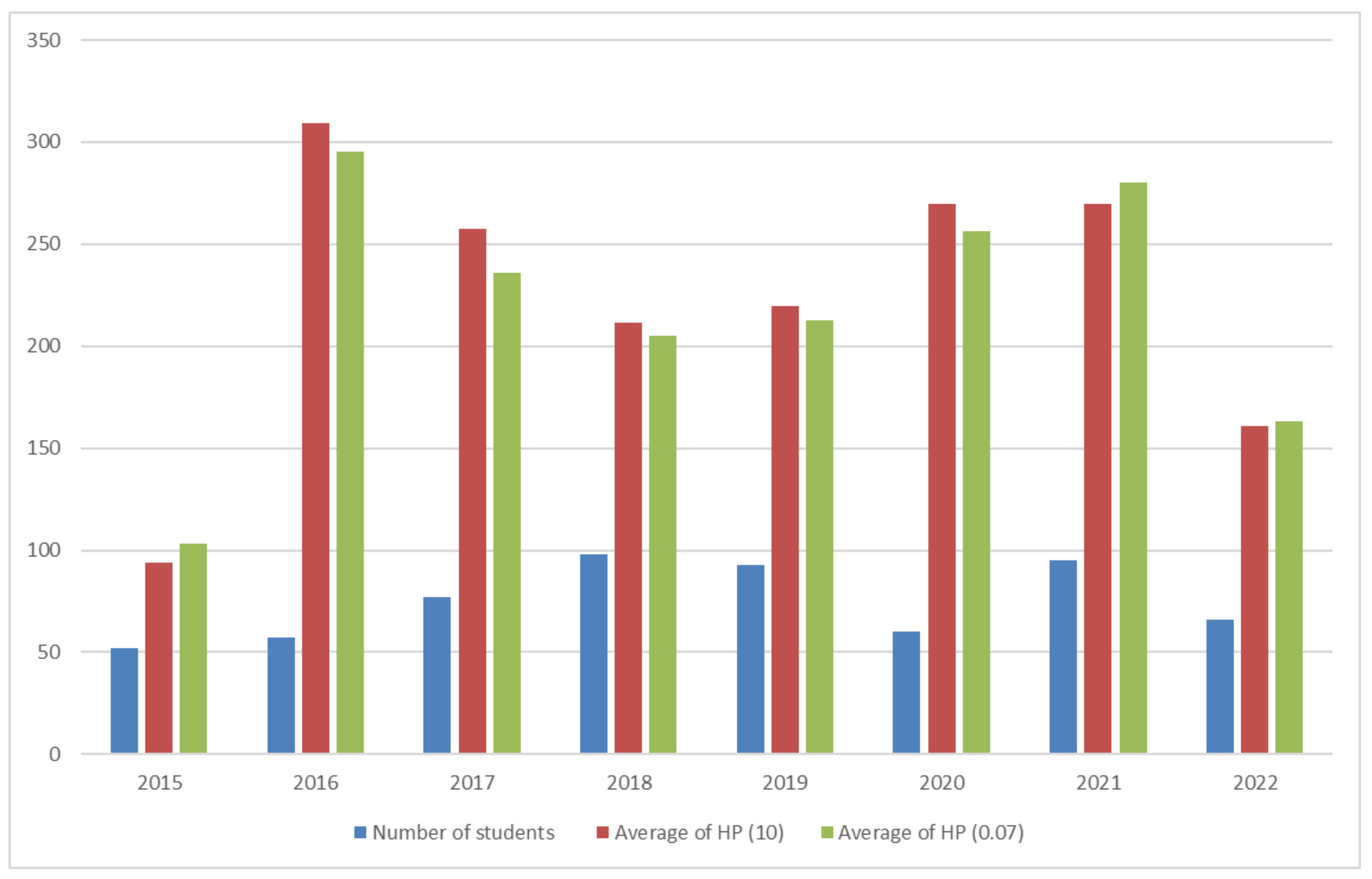
Figure 1 shows the number of students between 2015 and 2022, ranging from 52 to 98, with an average of 74 students per year. The HP (10) and HP (0.07) averages for all the dosimeter readings were 0.227 and 0.222 mSv, respectively. The readings were obtained from students across four courses. Course 1 included readings during a single academic year, while courses 2 and 3 encompassed readings from two and three consecutive academic years. The clinical practice courses comprised readings spanning five consecutive academic semesters during the study program.
Table 2 shows the student distribution and average HP (10) and HP (0.07) readings across the four courses. There was a steady increase in the averages from courses 1 to 4, where the maximum readings obtained in course 4 were 0.266 mSv in HP (10) and 0.256 mSv in HP (0.07).
An ANOVA analysis was conducted to analyse the difference in the doses (HP (10) and HP (0.07)) across the different courses. This analysis concluded that there was no statistically significant difference across the different courses in the HP (10) (p = 2.645) and HP (0.07) (p = 2.645).
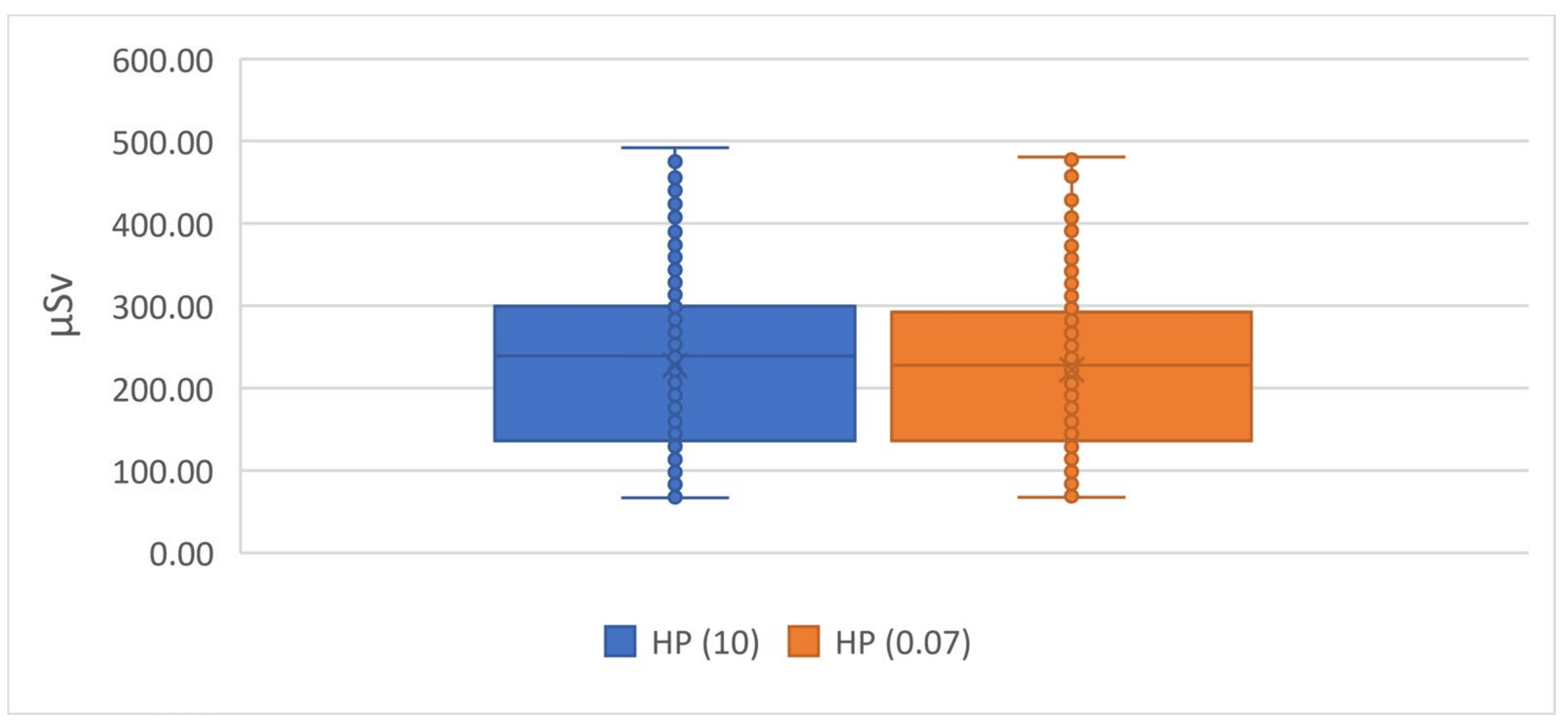
The overall HP (10) results ranged between 66.9 and 492.1 μSv, with a mean and SD of 227.2 ± 100.6, while the overall HP (0.07) ranged between 67.6 and 480.9 μSv, with a mean and SD of 222.4 ± 96. In
Figure 2, the box–whisker plot shows the mean HP (10) and HP (0.07). The box indicates the values from the first to the third quartiles, the line indicates the median quartile, and the whiskers indicate the minimum and maximum values.
The personal dose equivalent, HP (10), recorded and presented as an effective dose, is the operational dose quantity used to determine doses from external radiation. The students whose active dose was below 0.05 mSv, the minimum dose limit (MDL), were deemed non-exposed and recorded as zero. The readings from these students were not included in this study. The distribution of the dosimeter measurements for whole-body doses is shown in
Figure 1 and
Figure 2. Even though the number of students varied, the results between 2015 and 2022 revealed a nearly identical distribution.
4. Discussion
Owing to the lack of studies quantifying the effective radiation exposure dose of students during clinical placements, our study addressed this gap by comparing the results with studies based on radiation workers from other countries. The yearly workload of the students during the clinical training placement was similar to that of the radiographers. Furthermore, the results of our study are comparable with those of other trained personnel in diagnostic radiology, as shown in
Table 3. The effective dose of the students in our study was 0.23 mSv, which was only higher than the annual average effective dose of the radiography students in Slovenia (0.13 mSv). Compared against data which were received before the year 2000, our results were slightly higher than those measured in Slovenia (0.13 mSv) but considerably lower than those in Lithuania (1.51 mSv), India (1.34 mSv), and Australia (0.35 mSv). Notably, the average effective dose in Slovenia (0.13 mSv) during 1993–1994 was 43.5% lower than that recorded in our study’s data between 2015 and 2022. The results of this current study are also lower than the annual average effective dose between the years 2001 and 2015.
Amidst the COVID-19 lockdowns, the clinical modalities for students were rescheduled to the subsequent semester within the same academic year, thereby maintaining consistency in their clinical hours. In response to substantial modifications in the operation of multiple screening centres and dedicated COVID hospitals, the university in our study implemented special rotation schedules for its students. These schedules were designed to ensure the coverage of the originally intended modalities while affording students the opportunity to engage in a diverse array of examinations. This proactive initiative by the university may have played a role in mitigating the significant decline in the annual average radiation exposure dose observed in 2019 in comparison to both the preceding and subsequent years.
While the initial effective doses recorded among the students enrolled in course 1 stood at a comparatively lower level of 0.13 mSv, our findings revealed a consistent upward trend in the effective doses throughout the four courses. This observed pattern is a noteworthy indicator of students’ escalating workload as they advance into the upper years of their academic curriculum, including extensive clinical training programs (10). A Korean-based [
22] study conducted a comparative analysis to assess the radiation doses between individuals in radiation-related occupational roles and clinical practice students in the same area. The study concluded statistically significant differences in the radiation dose levels between these two groups, where the surface dose received by the students was substantially (0.151 ± 0.139 mSv) less than that of the workers (0.744 ± 1.676 mSv). This finding is notably distinct from our study, where the average effective dose was comparable to the occupational dose of healthcare workers in radiation-exposed professions. Another study conducted in Incheon, Korea [
23], recorded that the average surface dose received by students over one year, from January 2021, was 0.98 ± 0.14mSv. This is the most recent study quantifying students’ radiation exposure during a clinical placement, although it is limited by a short duration of 1 year.
Our study recorded a 75.79% reduction in the effective radiation exposure dose compared to a similar study conducted between 2009 and 2015 among students in clinical practice in the UAE, where the average effective dose for students was 0.95 mSv. Although this figure is higher than the results obtained in the current study, it is important to note that it still falls within the recommended radiation exposure limits.
Although the effective dose in our study was almost equal to that of workers in the radiation field, the maximum effective dose recorded was 0.49 mSv, which is significantly less than the average annual dose limit of 20 mSv recommended by national organisations such as the Federal Authority of Nuclear Regulation (FANAR) and the International Commission on Radiological Protection (ICRP).
The radiation safety protocols [
24,
25] within hospital settings are primarily designed to address and provide directives concerning the safety of medical staff and patients. Notably, students’ clinical rotations in hospital settings undergo periodic changes, typically on a semester basis. Consequently, these established protocols generally lack explicit guidelines tailored specifically to accommodate students; instead, students are generally encompassed within the broader category of hospital staff. Including students within the overarching staff category puts them in the blind spot of radiation safety management. Given the inherent differences in students’ roles, responsibilities, and activities compared to full-time hospital staff, continuous monitoring and quantifying the effective radiation dose that students receive are necessary for a nuanced and evidence-based approach to radiation safety management within educational and healthcare contexts.
5. Conclusions
Clinical placement is integral to radiography programs during which students are exposed to occupational radiation hazards. The curriculum and training guidelines prepare students for safe practice and protecting patients, the public, and themselves during radiation exposure. The results showed that the occupational radiation exposure dose for undergraduate students was below the limits allowed. Students should have the knowledge and skills necessary to use radiation protection equipment and monitoring devices during practice. Educational institutions should monitor and follow up on these dose measurements and ensure their students’ safety.
The reduction in the annual average effective radiation exposure dose in this study compared to the results from 2009 to 2015 shows the impact of monitoring doses, following up with students, and iterating the safety protocols to students throughout their practice, which can all effectively contribute to minimising the radiation exposure dose for students, staff, and the patients involved. Failure in monitoring the above could overlook situations or practices where there is an increase in the annual radiation exposure doses among students, which not only violates radiation protection regulations but also engenders ionising radiation risks among said students. In such a scenario, practices that lead to increased exposure would be left uncurbed and could continue throughout the students’ careers.
6. Study Limitations
This study only used TLDs to monitor radiation exposure and did not explore other monitoring methods. Furthermore, this study did not provide information on the long-term effects of radiation exposure on the students or the patients involved. Future studies should investigate the impact of safety protocols and training on reducing radiation exposure.
7. Practical Implications
The practical implications of this paper are that educational institutions should continue to monitor and follow up on radiation exposure dose measurements to ensure the safety of their students. This study showed that the occupational radiation dose for the undergraduate students observed was below the limits allowed, indicating that the curriculum and training guidelines had prepared them for safe practice and protecting patients, the public, and themselves during exposure. Vigilance in radiation dose monitoring and continuous student follow up while educating them on safety protocols during clinical practice has successfully reduced the annual effective dose in our current study. This paper highlights the importance of radiation protection education and training for radiography students and the need for educational institutions to prioritise the safety of their students and patients [
26].
8. Recommendations
Revelations from current and past studies based in the UAE could be utilised for time-series forecasting to study trends in radiation exposure doses among students through the years, allowing us to understand the reasons behind these variations and initiate safety protocols.
Author Contributions
Conceptualisation, M.A. and W.E.; methodology, M.A. and Z.N.; validation, M.A. and W.E.; formal analysis, Z.N. and M.I.; investigation, Z.N. and M.I.; resources, M.A. and W.E.; data curation, M.A. and W.E.; writing—original draft preparation, M.A. and W.E.; writing—review and editing, M.A. and W.E.; visualisation, W.E. and Z.N.; supervision, M.A.; project administration, M.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the University of Sharjah Ethics Committee (REC-17-02-02-03).
Informed Consent Statement
Not applicable.
Data Availability Statement
Data will be available upon request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Abuzaid, M.M.; Elshami, W.; Tekin, H.O. Infection control and radiation safety practices in the radiology department during the COVID-19 outbreak. PLoS ONE 2022, 17, e0279607. [Google Scholar] [CrossRef] [PubMed]
- Zangeneh, M.; Deevband, M.R.; Mohsenzadeh, B. Lifetime attributable risk of cancer incidence and mortality in routine digital radiology procedures. Clin. Imaging 2020, 67, 226–236. [Google Scholar] [CrossRef] [PubMed]
- Donya, M.; Radford, M.; ElGuindy, A.; Firmin, D.; Yacoub, M.H. Radiation in medicine: Origins, risks and aspirations. Glob. Cardiol. Sci. Pract. 2015, 2014, 57. [Google Scholar] [CrossRef] [PubMed]
- Cowling, C. A global overview of the changing roles of radiographers. Radiography 2008, 14, e28–e32. [Google Scholar] [CrossRef]
- Dowd, S.B. The radiographer’s role: Part scientist, part humanist. Radiol. Technol. 1992, 63, 240–243. [Google Scholar] [PubMed]
- DeMaio, D.N.; Herrmann, T.; Noble, L.B.; Orth, D.; Peterson, P.; Young, J.; Odle, T.G. Best practices in digital radiography. Radiol. Technol. 2019, 91, 198–201. [Google Scholar] [PubMed]
- ICRP. International Commission on Radiological Protection 2009 Annual Report; SAGE Publications Ltd.: London, UK, 2009. [Google Scholar]
- Directorate-General for Energy and Transport, European Commission; Ambrosi, P.; Bartlett, D.; Garcia-Alves, J. Technical Recommendations for Monitoring Individuals Occupationally Exposed to External Radiation; EU Publications Office: Brussels, Belgium, 2009; Available online: https://data.europa.eu/doi/10.2768/19817 (accessed on 4 April 2023).
- Lubis, L.E.; Aida, N.; Pratiwi, N.G.; Pawiro, S.A.; Wigati, K.T.; Soejoko, D.S. Occupational Dose Measurement in an Interventional Radiology Facility in Jakarta. In World Congress on Medical Physics and Biomedical Engineering, 7–12 June 2015, Toronto, Canada; Springer International Publishing: Berlin/Heidelberg, Germany, 2015. [Google Scholar] [CrossRef]
- Martin, C.J. Personal dosimetry for interventional operators: When and how should monitoring be done? Br. J. Radiol. 2011, 84, 639–648. [Google Scholar] [CrossRef] [PubMed]
- Medical Diagnostic Imaging Department, University of Sharjah. Bachelor of Science in Medical Diagnostic Imaging. Available online: https://www.sharjah.ac.ae/en/academics/Colleges/healthsciences/dept/mdi/Pages/Bachelor-of-Science-in-Medical-Diagnostic-Imaging.aspx (accessed on 4 April 2023).
- Morrison, G.; John, S.D.; Goske, M.J.; Charkot, E.; Herrmann, T.; Smith, S.N.; Culbertson, J.; Carbonneau, K. Pediatric digital radiography education for radiologic technologists: Current state. Pediatr. Radiol. 2011, 41, 602–610. [Google Scholar] [CrossRef] [PubMed]
- Rehani, M.M.; Berris, T. International Atomic Energy Agency study with referring physicians on patient radiation exposure and its tracking: A prospective survey using a web-based questionnaire. BMJ Open 2012, 2, e001425. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Monty, W.C. ICRP Publication 103: Recommendations of the ICRP; IRRP: Ottawa, ON, Canada, 2008; pp. 500–508. [Google Scholar]
- Abuzaid, M.M.; Elshami, W.; Steelman, C. Measurements of Radiation Exposure of Radiography Students During Their Clinical Training Using Thermoluminescent Dosimetry. Radiat. Prot. Dosim. 2018, 179, 244–247. [Google Scholar] [CrossRef] [PubMed]
- Foti, C.; Padovani, R.; Trianni, A.; Bokou, C.; Christofides, S.; Corbett, R.H.; Kepler, K.; Koreňová, Z.; Kosunen, A.; Malone, J.; et al. Staff dosimetry in interventional cardiology: Survey on methods and level of exposure. Radiat. Prot. Dosim. 2008, 129, 100–103. [Google Scholar] [CrossRef] [PubMed]
- Sina, S.; Zeinali, B.; Karimipoorfard, M.; Lotfalizadeh, F.; Sadeghi, M.; Zamani, E.; Faghihi, R. Investigation of the entrance surface dose and dose to different organs in lumbar spine imaging. J. Biomed. Phys. Eng. 2014, 4, 119–126. [Google Scholar]
- Elshami, W.; Abuzaid, M.; Rajab, O.; Almajed, N.; Alnuwaiser, O.; Alghareeb, A.; Alhomoud, B. A snapshot of occupational radiation dose in veterinary radiology. Radiat. Phys. Chem. 2020, 168, 108581. [Google Scholar] [CrossRef]
- Tamam, N.; Almuqrin, A.H.; Mansour, S.; Elnour, A.; Musa, M.; Omer, H.; Sulieman, A.; Bradley, D.A. Occupational and patient effective radiation doses in dental imaging. Appl. Radiat. Isot. 2021, 177, 109899. [Google Scholar] [CrossRef]
- Chiriotti, S.; Ginjaume, M.; Vano, E.; Sanchez, R.; Fernandez, J.M.; Duch, M.A.; Sempau, J. Performance of several active personal dosemeters in interventional radiology and cardiology. Radiat. Meas. 2011, 46, 1266–1270. [Google Scholar] [CrossRef]
- Stranden, E.; Widmark, A.; Sekse, T. Assessing doses to interventional radiologists using a personal dosimeter worn over a protective apron. Acta Radiol. 2008, 49, 415–418. [Google Scholar] [CrossRef]
- Lee, J.A. Analysis of individual exposure dose of workers and clinical practice students in radiation management area. J. Korea Contents Assoc. 2017, 17, 383–388. [Google Scholar] [CrossRef]
- Lee, J.A. A review of the radiation exposure dose to regular visitors of radiology (radiology) clinical trainees. J. Korean Soc. Radiol. 2023, 17, 249–255. [Google Scholar]
- Walker, D.; Voutchkov, M.; McKenzie, C.; Barned, H. Radiation Safety Standards for X-ray Facilities: Protocol for Plain Radiography. West Indian Med. J. 2016. [Google Scholar] [CrossRef][Green Version]
- Bell, L.A. Promoting Radiation Safety Protocols in Computed Tomography. Radiol. Technol. 2016, 87, 344–348. [Google Scholar]
- Abuzaid, M.M.; Elshami, W.; Abdelrazig, A.; McFadden, S. Direct digital radiography: Exploring applications, misuse, and training needs in medical imaging. Health Technol. 2023, 13, 1025–1032. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).