Invasive Candidiasis in Contexts of Armed Conflict, High Violence, and Forced Displacement in Latin America and the Caribbean (2005–2025)
Abstract
1. Introduction
2. Historical Context of Armed Conflict and High Levels of Violence in Latin America and the Caribbean (LA&C) (Last 25 Years)
2.1. Conflicts in North America and the Caribbean
2.1.1. Conflicts in Central America
2.1.2. Conflicts in South America
3. Epidemiology and Burden of IC Disease in LA&C
- Delay in diagnosis: the speed with which candidemia is detected varies depending on the fungal species. While C. albicans can be detected in an average of 35 h, N. glabratus requires up to 80 h, which significantly delays the start of effective antifungal treatment [74].
- Age and clinical status at admission: a high APACHE II score and a diagnosis of septic shock are negative prognostic factors. On average, patients who die from candidemia are around 60 years old [79].
Epidemiology, Disease Burden in the Context of Armed Conflict and High Violence
4. Risk Factors for IC in the General Population and in Contexts of Forced Displacement in LA&C
4.1. Health Conditions and Risk of Fungal Infection in Migrant and Displaced Populations
4.1.1. Socio-Environmental Conditions and Social Determinants
- Overcrowding and informal settlements: in contexts such as Venezuelan refugee camps in Colombia and Haitian migrant settlements in the Dominican Republic, it is common for families to live in extremely small spaces (less than 5 m2 per person). These overcrowded conditions not only make privacy and hygiene difficult but also increase body moisture and skin maceration, promoting the development of fungal infections. In a recent survey, 28% of adult women in these environments reported intertriginous or vulvovaginal candidiasis [156]. An institutional report (2019–2020) on Mexico’s southern border with Guatemala revealed that Central American migrants housed in shelters without adequate ventilation showed a high prevalence of skin infections. Microbiological field studies found that 33% of cases with interdigital rashes tested positive for Candida, mainly C. parapsilosis, highlighting how the tropical climate, combined with poor hygiene, increases susceptibility to these infections [157].
- Limited access to drinking water and sanitation: in the Northern Triangle of Central America (Honduras, El Salvador, and Guatemala), recent studies have shown that more than 40% of informal settlements do not have a continuous supply of chlorinated water. This limitation prevents adequate hand and surface hygiene, creating conditions conducive to the proliferation of yeasts in the environment. Such microenvironments become potential reservoirs for infections such as cutaneous and vulvovaginal candidiasis [158]. In Bolivia, data collected between 2018 and 2019 in rural areas inhabited by returning migrants showed that only 35% of homes had adequate latrines. This deficiency in basic sanitation increases the environmental microbial load and favors fungal colonization of the skin and moist areas of the body, especially in crowded conditions and hot climates [159].
- Malnutrition and immune deficiency: an internal epidemiological surveillance report conducted between 2018 and 2019 among the displaced population in the department of Arauca, Colombia, revealed that 42% of children and 28% of pregnant women suffered from acute or chronic malnutrition. In this context, 30% of children with oral candidiasis showed signs of malnutrition, and within this group, 18% developed candidemia within less than ten days [160,161]. The lack of essential micronutrients—such as vitamins A and D and zinc—impairs both cellular and humoral immunity, promoting the transition of Candida from superficial colonization to systemic infection. This risk is exacerbated in displaced adults with irregular access to basic nutritional supplements [160].
4.1.2. Prevalent Comorbidities in Migrants and Displaced Persons
- HIV/AIDS: according to an institutional report for the period 2018–2019, the prevalence of HIV among Venezuelan migrants settled in Colombia was 3.2%, of whom 45% were not receiving antiretroviral treatment and had CD4 counts below 200 cells/µL. In this cohort, 38% developed oral candidiasis, and 12% developed esophageal candidiasis during the first year of follow-up [162]. A retrospective analysis conducted after the 2010 earthquake in Haitian displacement camps revealed that many people were living with HIV patients in advanced stages of the disease and without access to antiretroviral therapy. In this group, 55% were diagnosed with recurrent mucocutaneous candidiasis, and 12% had candidemia, which was associated with a 65% mortality rate due to the lack of timely diagnosis and effective antifungal drugs [163].
- Type 2 diabetes mellitus: in agricultural export plantations in Central America, studies conducted among migrant workers showed a prevalence of undiagnosed diabetes of 16%. Of this group, 30% had candidal vulvovaginitis and 8% developed complicated forms of cutaneous candidiasis, including infected ulcers [119,120]. Similarly, an internal epidemiological surveillance report on displaced indigenous communities in Peru documented that 14% of older adults had uncontrolled diabetes (fasting glucose greater than 126 mg/dL). In these patients, interdigital candidiasis occurred in 27% of cases, and an RR of 2.8 (95% CI: 1.6–4.9) was estimated for the development of disseminated candidiasis after hospitalization [164].
- Tuberculosis and co-infections: in camps for displaced persons located in the border areas between Venezuela and Colombia, a prevalence of tuberculosis (TB) of 350 cases per 100,000 inhabitants has been documented, with a high frequency of HIV/TB co-infection. This combination increases the risk of IC. A retrospective study conducted in Bogotá revealed that 22% of patients with TB/HIV coinfection developed candidemia, with an associated mortality rate of 58% [165]. On the other hand, a descriptive study in Guatemala observed that, in co-infected individuals, the presence of extrapulmonary TB—particularly in its peritoneal or gastrointestinal forms—caused damage to the digestive mucosa, facilitating the translocation of Candida spp. into the body. As a result, 14% of these patients developed intra-abdominal candidiasis [166].
4.1.3. Exposure to Iatrogenic Factors
- Use of antibiotics in mobile clinics and shelters: between 2019 and 2020, in mobile clinics providing medical care to Nicaraguan migrants in Mexican territory, it was observed that 78% of patients with fever were treated with broad-spectrum antibiotics, such as ceftriaxone or carbapenems, without prior blood cultures. This practice was associated with the onset of mucocutaneous candidiasis in 26% of cases and candidemia in approximately 5%, although significant underreporting is presumed due to the lack of diagnostic laboratories in these settings [167]. The widespread empirical use of antibiotics without proper assessment of the risk of fungal infection has contributed to the disruption of normal microbiota, facilitating the overgrowth of Candida spp.
- Use of invasive devices in border hospitals: an internal surveillance report from 2020, based on data from migrant reception units in Tapachula (Mexico–Guatemala region), found that 42% of patients hospitalized for sepsis required CVC insertion. Among these patients, 12% developed candidemia, which corresponds to a significantly elevated risk (OR 3.5; 95% CI: 2.0–6.1). Furthermore, due to a lack of specialized personnel, protocols for early catheter removal are not properly implemented, prolonging exposure to fungal biofilm and increasing the likelihood of invasive infections [168].
4.1.4. Demographic and Vulnerability Factors
- Age and gender: an epidemiological surveillance study in Colombia (2018–2019), focusing on displaced children, revealed that 18% of newborns from temporary shelters developed oral candidiasis in their first week of life. This finding was related to low birth weight (less than 2500 g) and maternal malnutrition, conditions that are common in contexts of forced displacement [160]. On the other hand, a study on reproductive health in migrant women (2019) found that 34% of women living in border settlements experienced episodes of vulvovaginal candidiasis in the last year, mainly linked to malnutrition, pregnancy, and limited access to adequate gynecological services [169].
- Ethnicity and inequalities: in displaced Guaraní indigenous communities in Paraguay, the rate of cutaneous candidiasis was almost three times higher than that observed in nearby urban populations. This difference has been attributed to difficulties in accessing adequate health services and language barriers that limit timely care [170]. Similarly, an internal report on Haitian migrants in the Dominican Republic reported that 46% of adults with HIV developed oral candidiasis, compared to 28% of the non-migrant population. Language barriers and experiences of discrimination contribute significantly to delays in diagnosis and treatment [171].
4.1.5. Environmental and Occupational Conditions
- Agricultural work and environmental exposure: among Central American migrants employed on sugar cane plantations in Guatemala, a 15% prevalence of skin colonization by C. parapsilosis has been identified, which is associated with repeated contact with humid environments and contaminated surfaces, such as wet soil and stagnant water [172]. On the other hand, an epidemiological surveillance report conducted in fruit-growing areas in Peru found that 22% of migrant workers of Peruvian and Bolivian origin developed interdigital candidiasis. This condition could be related to repeated exposure to insecticides, which alter the normal microbial flora of the skin [173].
- Climate and microenvironments: according to an epidemiological surveillance report, climatic conditions in coastal areas of Central America—characterized by humidity levels above 80% and constant temperatures around 28 °C—are favorable for the growth of yeast on the skin and mucous membranes. In Honduras, migrants traveling along routes near the coast were found to have intertriginous candidiasis in 31% of cases, a figure considerably higher than the 12% reported among those traveling along mountainous routes [174].
5. Diagnosis of IC in LA&C: Barriers and Diagnostic Methods in Resource-Limited Settings
5.1. Barriers and Limitations in the Diagnosis of Candidiasis
5.1.1. Infrastructure and Logistics
- Lack of local laboratories: mobile health centers and small shelters are not equipped with adequate biosafety facilities or protocols for mushroom cultivation. As a result, samples must be sent to reference laboratories, which are often located far away. This involves transportation without a cold chain, which increases the risk of contamination or decreases the viability of the fungi, reducing crop yields to less than 50% [9,12].
5.1.2. Human Resources and Training
- High turnover of volunteer staff: in NGOs operating in camps, constant staff turnover prevents continuity in the use of protocols and hinders the transfer of specialized knowledge. Although there are no exact figures, this recurring problem has been documented in border environments [111,190,191,192].
5.1.3. Costs and Availability of Reagents
- Scarce and expensive basic reagents: in many countries in the Andean region and the Caribbean, essential reagents such as KOH 10% solutions and Gram stains must be imported, which increases the cost of each test by approximately USD 5–10. This is a difficult expense for mobile clinics with limited resources to bear [111,176,180,189,193].
- Limited access to state-of-the-art testing: serological tests such as BDG or molecular methods such as qPCR are not covered by public health systems and are only offered in reference laboratories, usually located in capital cities. This situation forces patients to travel long distances to access these diagnostics [9,117,176,194].
5.1.4. Social and Cultural Limitations
- Distrust of the healthcare system: many displaced persons have been victims of violence or discrimination, which generates mistrust of medical services and reduces their willingness to participate in procedures such as blood tests. Although there are no specific data on candidiasis, reproductive health studies show that more than 40% of displaced populations avoid going to official centers for this reason [12,41,125,142,192].
- Language and communication barriers: in Haitian refugee shelters in the Dominican Republic and also in Venezuelan indigenous communities, a lack of fluency in Spanish hinders communication with healthcare personnel. Qualitative studies indicate that up to 30% of consultations are postponed or interrupted due to language problems or a lack of interpreters [11,131,192,195,196].
5.2. Recommendations for Strengthening Diagnosis in Areas of Forced Displacement
5.2.1. Optimization of Low-Cost Methods
- Technical training in KOH: it is recommended to train local staff through weekly workshops focused on the processing and interpretation of exudates using 10% potassium hydroxide (KOH 10%). The implementation of this strategy in areas with limited resources has been shown to improve diagnostic accuracy [106,180,189,195,197].
- Rotary direct microscopy with calcofluor: several studies have shown that calcofluor is consistently more sensitive than KOH and sometimes comparable to more sophisticated diagnostic methods. Its usefulness as a rapid diagnostic technique makes it especially valuable in resource-limited environments. In this context, the possibility of sharing UV equipment between nearby camps is suggested to facilitate the assessment of mucocutaneous lesions. This strategy could be applied in countries such as Haiti to reduce the false negative rate [180,189,198,199].
5.2.2. Implementation of Simplified Algorithms
- Adapted use of the “modified Candida Score” in primary care: in community settings where state-of-the-art testing is not available, a simplified version of the “Candida Score” is proposed for initiating empirical treatment. In patients with fever without apparent source and at least three of the following criteria—recent antibiotic use, presence of CVC, and malnutrition—it is recommended to initiate FCZ if the KOH test is positive. If BDG is available, consider echinocandins when this marker is positive. Studies in ICUs in Latin America show that a score equal to or greater than 3 predicts candidemia with a sensitivity of 70% [117,188].
- Creation of multilingual visual guides: designing and distributing illustrative materials on clinical signs of candidiasis, translated into Spanish, Haitian Creole, and indigenous languages, can be key to improving recognition of the infection. Experiences in community health programs have shown that incorporating these guides improves early detection by 18% [7,12,189,200].
5.2.3. Surveillance and Reference Networks
- Development of collaborative networks for sample processing: it is proposed to implement a referral system between camps and laboratories located in nearby urban areas, ensuring the transport of samples under appropriate cold chain conditions. This measure, accompanied by regular exchanges of volunteer microbiologists, has proven effective: in Latin America, agreements between mobile units and universities reduced the analysis time for mycological samples from seven to three days [6,12,111,175,176,187].
- Strengthening tele-mycology networks: the use of technology to share diagnostic images (cultures, smears, lesions) in real-time via mobile networks or satellite connections can significantly improve diagnostic accuracy. Creating virtual links with regional mycology experts would enable constant supervision and technical support, with at least one specialist recommended for every 5000 displaced persons [178,197,201,202,203].
5.2.4. Funding and Strategic Alliances
- Ensure donations of basic supplies: we propose coordinating with organizations such as GAFFI and PAHO to deliver essential supplies (KOH, dyes, culture media) to mobile clinics in border areas and hard-to-reach camps. Since 2019, these initiatives have made it possible to supply resources to more than 20 mobile units in Colombia and Peru, strengthening their diagnostic capacity [6,7,106,176,189,200,204].
- Formalize agreements with regional universities: emphasis is placed on the need to integrate essential diagnostics and strengthen national and hospital diagnostic networks. It is also proposed to establish biannual agreements with local universities for the provision of diagnostic supplies to reduce and lower transportation expenses and expand diagnostic coverage in remote areas [7,12,106,175,176,187,200].
6. Antifungal Treatment of IC in LA&C: Availability of Antifungals and Antifungal Resistance
- Restricted availability of essential antifungals: in most LA&C countries, access to antifungals is limited mainly to generic FCZ, due to its low cost and early inclusion in national essential medicines lists [10,193,206]. Although this drug is available, it is not the ideal option for candidemia in critically ill patients, as up to 50% of non-albicans isolates—such as N. glabratus, P. kudriavzevii, and C. auris—have reduced sensitivity or intrinsic resistance to FCZ.
- Suboptimal administration of D-AmB: in the absence of echinocandins, D-AmB is frequently used as an alternative. However, to ensure its safe use, constant monitoring of renal function and electrolyte balance is required, as well as continuous administration of intravenous fluids and potassium salts [207]. In hospitals with limited resources, such conditions are often inadequate. This has led many professionals to reduce doses as a precaution, especially when there is no access to ICUs or adequate laboratories. Additionally, D-AmB depends on a cold chain, which is challenging in hot environments with unstable power supplies.
- Increase in antifungal-resistant strains: during the C. auris outbreak in Venezuela, all isolates showed resistance to FCZ and VCZ, and 50% had high minimum inhibitory concentrations (MIC) against AmB [208]. Although echinocandins are considered the almost exclusive therapeutic resource in these cases, strains with reduced sensitivity to these drugs are beginning to be detected [65,216]. At the same time, N. glabratus shows increased resistance to azoles, and C. parapsilosis shows mutations associated with prolonged treatment with echinocandins [214,219,220,221]. In Brazil, clusters of FCZ-resistant C. parapsilosis have been documented [8,220,221,222], and in areas of armed conflict, the absence of surveillance and infection control facilitates their unnoticed spread.
- Incomplete treatments: the minimum duration of treatment for candidemia should be 14 days from the last negative blood culture, extending in the presence of metastatic foci [112,117,185]. In displacement settings, it is common for patients to discontinue treatment after one week due to continuous displacement or depletion of medications in centers, which increases the risk of relapse and promotes the development of resistance.
- Inequality in costs and access: while FCZ is relatively affordable, echinocandins and L-AmB are too expensive for most centers and are only available in private clinics. In countries such as Haiti and Venezuela, public systems lack these drugs, and NGOs rarely include them in their emergency supplies due to budget constraints [121,193,194,206]. This means that, in many refugee camps, optimal treatment for candidemia remains inaccessible.
- Lack of complementary critical support: effective management of IC goes beyond the provision of antifungal agents. It requires intensive care, surgical interventions to control foci (such as valve replacement in endocarditis or abscess drainage), as well as life support—dialysis in cases of renal failure or MV [106,176,185]. In conflict-affected areas, these resources are often lacking [194], meaning that even with adequate antifungal treatment, the outcome can be fatal due to the lack of comprehensive clinical support or access to interventions that remove the source of infection.
7. Access to Health Services and Antifungal Treatment in Areas of Conflict and High Violence in LA&C
- Forced internal migration and informal settlements: internally displaced persons and refugees living in temporary camps often have limited or no access to adequate healthcare services. In these contexts, cases of candidemia are rarely diagnosed or treated with antifungal medication, and deaths are often not officially reported [38,142,228].
- Risks for patients and healthcare personnel: in areas of active violence, transfer to a medical center can pose a life-threatening risk (bombing, snipers, checkpoints). In conflicts such as the one in Syria, attacks on hospitals and healthcare personnel have been documented, interrupting essential treatments for severe mycoses [229].
8. Regional Perspective
8.1. Mexico
8.2. Haiti
8.3. North Triangle (El Salvador, Guatemala, Honduras)
8.4. Colombia
8.5. Venezuela
8.6. Brazil
8.7. Peru
9. Recommendations for Future Research
- Quantify the prevalence of candidiasis (mucocutaneous and invasive) and its distribution by species, including resistance profiles.
- Identify specific risk factors of displacement, such as hygiene conditions, sanitary access barriers, and psychological stress.
- Evaluate interventions such as improved sanitation, educational programs, and the use of broad-spectrum antifungals in vulnerable populations [125].
- Multicenter prevalence studies
- Conduct cross-sectional studies in camps and shelters to quantify the prevalence of oral and vulvovaginal candidiasis, itemized by sociodemographic factors, nutritional status, and HIV co-infection [227].
- Species identification and antifungal profile
- Establish mobile laboratory units or partner with regional diagnostic centers (e.g., hospitals in host cities) to accurately identify Candida species and perform MIC determinations using broth microdilution [255].
- Establish a regional registry of isolates from migrants and displaced persons in LA&C, including genetic typing using MLST (multilocus sequence typing) [256].
- Study of risk factors associated with displacement
- Design clinical trials to evaluate preventive and therapeutic interventions
- Conduct a randomized study in patients with recurrent vulvovaginal candidiasis to compare short treatment regimens with FCZ versus topical therapy with azoles (miconazole), evaluating adherence and tolerance [259].
- Systematic monitoring in camp healthcare centers
- Integration of a One Health approach
- Establish partnerships with veterinarians and local bioresource centers to identify environmental reservoirs of Candida in temporary settlement sites [106].
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nucci, M.; Queiroz-Telles, F.; Alvarado-Matute, T.; Tiraboschi, I.N.; Cortes, J.; Zurita, J.; Guzman-Blanco, M.; Santolaya, M.E.; Thompson, L.; Sifuentes-Osornio, J.; et al. Epidemiology of Candidemia in Latin America: A laboratory-based survey. PLoS ONE 2021, 16, e0247357. [Google Scholar] [CrossRef]
- Yapar, N. Epidemiology and risk factors for invasive candidiasis. Ther. Clin. Risk Manag. 2014, 10, 95–105. [Google Scholar] [CrossRef]
- Falci, D.R.; Pasqualotto, A.C. Clinical mycology in Latin America and the Caribbean: A snapshot of diagnostic and therapeutic capabilities. Mycoses 2019, 62, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.N.; Ramatowski, J.W.; Marano, N.; Madoff, L.C.; Lassmann, B. Infectious disease outbreaks among forcibly displaced persons: An analysis of ProMED reports 1996–2016. Confl. Health 2020, 14, 32. [Google Scholar] [CrossRef] [PubMed]
- Denning, D.W. Global incidence and mortality of severe fungal disease. Lancet Infect. Dis. 2024, 24, e428–e438. [Google Scholar] [CrossRef] [PubMed]
- Global Action Fund for Fungal Infections (GAFFI). The Burden of Serious Fungal Infections in Latin America [Internet]. 2021. Available online: https://life-slides-and-videos.s3.eu-west-2.amazonaws.com/LIFE+articles/Burden+of+serious+fungal+infections+in+Latin+America.pdf (accessed on 13 June 2025).
- Global Action Fund for Fungal Infections (GAFFI). Report on Activities for 2015 [Internet]. 2016. Available online: http://www.life-slides-and-videos.s3.eu-west-2.amazonaws.com/LIFE+articles/Burden+of+serious+fungal+infections+in+Latin+America.pdf (accessed on 14 June 2025).
- Bays, D.J.; Jenkins, E.N.; Lyman, M.; Chiller, T.; Strong, N.; Ostrosky-Zeichner, L.; Hoenigl, M.; Pappas, P.G.; Thompson, G. Epidemiology of invasive candidiasis. Clin. Epidemiol. 2024, 16, 549–566. [Google Scholar] [CrossRef]
- Cortés, J.A.; Ruiz, J.F.; Melgarejo-Moreno, L.N.; Lemos, E.V. Candidemia en Colombia. Biomédica 2020, 40, 195–207. [Google Scholar] [CrossRef]
- Jenks, J.D.; Prattes, J.; Wurster, S.; Sprute, R.; Seidel, D.; Oliverio, M.; Egger, M.; Del Rio, C.; Sati, H.; Cornely, O.A.; et al. Social determinants of health as drivers of fungal disease. EClinicalMedicine 2023, 66, 101–109. [Google Scholar] [CrossRef]
- Plataforma, R.4.V. Refugiados y Migrantes de Venezuela [Internet]. 2024. Available online: https://www.r4v.info/es/refugiadosymigrantes (accessed on 13 June 2025).
- Tudela, J.L.R.; Cole, D.C.; Ravasi, G.; Bruisma, N.; Chiller, T.C.; Ford, N.; Denning, D.W. Integration of fungal diseases into health systems in Latin America. Lancet Infect. Dis. 2020, 20, 890–892. [Google Scholar] [CrossRef]
- Internal Displacement Monitoring Centre (IDMC). GRID 2022: Global Report on Internal Displacement [Internet]. 2022. Available online: https://www.internal-displacement.org/global-report/grid2022/ (accessed on 13 June 2025).
- International Committee of the Red Cross (ICRC). Latin America: Armed Violence, Conflict, Internal Displacement, Migration and Disappearances Were Main Humanitarian Challenges in 2021 [Internet]. 2021. Available online: https://www.icrc.org/en/document/latin-america-armed-violence-conflict-internal-displacement-migration-disappearances (accessed on 13 June 2025).
- Internal Displacement Monitoring Centre (IDMC). GRID 2024: Global Report on Internal Displacement [Internet]. 2024. Available online: https://www.internal-displacement.org/global-report/grid2024/ (accessed on 13 June 2025).
- UNICEF. Number of Unaccompanied and Separated Children Migrating in Latin America and the Caribbean Hits Record High [Internet]. 2024. Available online: https://www.unicef.org/lac/en/press-releases/number-unaccompanied-children-migrating-latin-america-caribbean-hits-record-high (accessed on 13 June 2025).
- Caparini, M.D. The Americas—Key general developments in the region. In SIPRI Yearbook 2022: Arm Conflict and Conflict Management 2021; Stockholm International Peace Research Institute: Stockholm, Sweden, 2022; pp. 77–81. [Google Scholar]
- Gousy, N.; Sateesh, B.A.; Denning, D.W.; Latchman, K.; Mansoor, E.; Joseph, J.; Honnavar, P. Fungal infections in the Caribbean: A review of the literature to date. J. Fungi 2023, 9, 1177. [Google Scholar] [CrossRef]
- Bernal, O.; Garcia-Betancourt, T.; León-Giraldo, S.; Rodríguez, L.M.; González-Uribe, C. Impact of the armed conflict in Colombia: Consequences in the health system, response and challenges. Confl. Health 2024, 18, 4. [Google Scholar] [CrossRef] [PubMed]
- Izcara-Palacios, S.P. Violencia contra inmigrantes en Tamaulipas. Eur. Rev. Lat. Am. Caribb. Stud. 2012, 93, 3–24. [Google Scholar] [CrossRef]
- UNHCR Dataviz Platform—Haiti: A Multi-Dimensional Crisis Leading to Continued Displacement [Internet]. 2024. Available online: https://dataviz.unhcr.org/product-gallery/2024/10/haiti-a-multi-dimensional-crisis-leading-to-continued-displacement/ (accessed on 13 June 2025).
- Restrepo-Betancur, L.F. Migración en Sudamérica en los últimos treinta años. El Ágora USB 2021, 21, 61–74. [Google Scholar] [CrossRef]
- UNHCR. EEl Salvador, Guatemala and Honduras Situation; United Nations High Commissioner for Refugees: Geneva, Switzerland, 2022; Available online: https://www.unhcr.org/sites/default/files/2023-07/2305336E_UNHCR-AR-2022_web_V3.pdf (accessed on 13 June 2025).
- UNHCR. Situación en Colombia [Internet]. 2024. Available online: https://reporting.unhcr.org/operational/situations/colombia-situation (accessed on 13 June 2025).
- Inter-American Development Bank. Migración Interna en Venezuela: En Busca de Oportunidades Antes y Durante la Crisis [Internet]. 2024. Available online: https://publications.iadb.org/es/migracion-interna-en-venezuela-en-busca-de-oportunidades-antes-y-durante-la-crisis (accessed on 13 June 2025).
- International Committee of the Red Cross (ICRC). Armed Violence in Mexico and Central America Continues to Cause Large-scale Suffering [Internet]. 2021. Available online: https://www.icrc.org/en/document/armed-violence-mexico-and-central-america-continues-cause-large-scale-suffering (accessed on 13 June 2025).
- The Guardian. More than 500 Mexicans Flee to Guatemala to Escape Cartel Violence in Chiapas [Internet]. 2024. Available online: https://www.theguardian.com/world/article/2024/jul/30/mexico-chiapas-flee-to-guatemala (accessed on 13 June 2025).
- The Times. The Pilgrimage Town That Went to War When the Drug Cartels Arrived [Internet]. 2025. Available online: https://www.thetimes.com/world/latin-america/article/a-town-that-went-to-war-local-feud-fuels-mexican-cartels-fight-for-control-fzqjmq302 (accessed on 13 June 2025).
- Wall Street Journal (WSJ). Haiti’s Beleaguered Government Launches Drones Against Gangs [Internet]. 2025. Available online: https://www.wsj.com/world/americas/haiti-drones-gangs-fight-27e8341f (accessed on 13 June 2025).
- International Committee of the Red Cross (ICRC). Haiti: Renewed Clashes Fuel Humanitarian Crisis [Internet]. 2025. Available online: https://www.icrc.org/en/article/haiti-renewed-clashes-fuel-humanitarian-crisis-has-no-end-sight (accessed on 13 June 2025).
- Pan American Health Organization (PAHO). Caring for the Displaced in Haiti: Overcoming Health Challenges Amid Escalating Armed Violence; Pan American Health Organization: Washington, DC, USA, 2024; Available online: https://www.paho.org/en/stories/caring-displaced-haiti-overcoming-health-challenges-amid-escalating-armed-violence (accessed on 13 June 2025).
- United Nations Office for the Coordination of Humanitarian Affairs (UN OCHA). Six Things to Know About the Humanitarian Crisis in Haiti [Internet]. 2024. Available online: https://www.unocha.org/news/six-things-know-about-humanitarian-crisis-haiti (accessed on 13 June 2025).
- Internal Displacement Monitoring Centre (IDMC). Crime and Displacement in Central America [Internet]. 2024. Available online: https://www.internal-displacement.org/research-areas/crime-and-displacement-in-central-america/ (accessed on 13 June 2025).
- Franco, S.; Suárez, C.M.; Naranjo, C.B.; Báez, L.C.; Rozo, P. The effects of the armed conflict on life and health in Colombia. Cien Saude Colet. 2006, 11, 349–361. [Google Scholar] [CrossRef]
- Internal Displacement Monitoring Centre (IDMC). The Last Refuge: Urban Displacement in Colombia [Internet]. 2020. Available online: https://story.internal-displacement.org/colombia-urban/index.html (accessed on 13 June 2025).
- Shultz, J.M.; Garfin, D.R.; Espinel, Z.; Araya, R.; Oquendo, M.A.; Wainberg, M.L.; Chaskel, R.; Gaviria, S.L.; Ordóñez, A.E.; Espinola, M.; et al. Internally displaced “victims of armed conflict” in Colombia: The trajectory and trauma signature of forced migration. Curr. Psychiatry Rep. 2014, 16, 460. [Google Scholar] [CrossRef]
- El País. Los 40 000 Desplazados del Catatumbo Marcan un Quiebre en la Larga Historia del Desplazamiento Forzado en Colombia [Internet]. 2025. Available online: https://elpais.com/america-colombia/2025-01-26/el-catatumbo-marca-un-record-en-la-larga-historia-del-desplazamiento-forzado-en-colombia.html (accessed on 13 June 2025).
- Human Rights Watch (HRW). World Report 2021: Venezuela [Internet]. 2021. Available online: https://www.hrw.org/world-report/2021/country-chapters/venezuela (accessed on 13 June 2025).
- Human Rights Watch (HRW). Venezuela: Security Force Abuses at Colombia Border [Internet]. 2021. Available online: https://www.hrw.org/news/2021/04/26/venezuela-security-force-abuses-colombia-border (accessed on 13 June 2025).
- Internal Displacement Monitoring Centre (IDMC). The Impact of COVID-19 on the Venezuelan Displacement Crisis [Internet]. 2020. Available online: https://www.internal-displacement.org/expert-analysis/the-impact-of-covid-19-on-the-venezuelan-displacement-crisis/ (accessed on 13 June 2025).
- Salas-Wright, C.P.; Pérez-Gómez, A.; Maldonado-Molina, M.M.; Mejia-Trujillo, J.; García, M.F.; Bates, M.M.; Vaughn, M.G.; Calderón, I.; Santos, V.G.D.L.; Brown, E.C.; et al. Cultural stress and mental health among Venezuelan migrants: Cross-national evidence from 2017 to 2024. Soc. Psychiatry Psychiatr. Epidemiol. 2024, 59, 831–842. [Google Scholar] [CrossRef]
- Cruz, M.S.; Silva, E.S.; Jakaite, Z.; Krenzinger, M.; Valiati, L.; Gonçalves, D.; Ribeiro, E.; Heritage, P.; Priebe, S. Experience of neighbourhood violence and mental distress in Brazilian favelas: A cross-sectional household survey. Lancet Reg. Health Am. 2021, 4, 100067. [Google Scholar] [CrossRef]
- Furumo, P.R.; Yu, J.; Hogan, J.A.; de Carvalho, L.T.M.; Brito, B.; Lambin, E.F. Land conflicts from overlapping claims in Brazil’s rural environmental registry. Proc. Natl. Acad. Sci. USA 2024, 121, e2407357121. [Google Scholar] [CrossRef]
- da Luz Scherf, E.; Viana da Silva, M.V. Brazil’s Yanomami health disaster: Addressing the public health emergency requires advancing criminal accountability. Front. Public Health 2023, 11, 1166167. [Google Scholar] [CrossRef]
- Internal Displacement Monitoring Centre (IDMC). Brazil—Internal Displacements Updates (IDU) [Internet]. 2024. Available online: https://data.humdata.org/dataset/idmc-event-data-for-bra (accessed on 13 June 2025).
- Randell, H. Forced migration and changing livelihoods in the Brazilian Amazon. Rural Sociol. 2017, 82, 548–573. [Google Scholar] [CrossRef]
- Chavez, L.J.E.; Lamy, Z.C.; Veloso, L.d.C.; da Silva, L.F.N.; Goulart, A.M.R.; Cintra, N.; Neal, S.; Riggirozzi, P. Barriers and facilitators for the sexual and reproductive health and rights of displaced Venezuelan adolescent girls in Brazil. J. Migr. Health 2024, 10, 100237. [Google Scholar] [CrossRef] [PubMed]
- Center for Latin American & Caribbean Studies. Peru: The Shining Path and the Emergence of the Human Rights Community in Peru [Internet]. 2021. Available online: https://clacs.berkeley.edu/peru-shining-path-and-emergence-human-rights-community-peru (accessed on 13 June 2025).
- Suarez, E.B. The association between post-traumatic stress-related symptoms, resilience, current stress and past exposure to violence: A cross-sectional study of the survival of Quechua women in the aftermath of the Peruvian armed conflict. Confl. Health 2013, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Internal Displacement Monitoring Centre (IDMC). Peru [Internet]. 2025. Available online: https://www.internal-displacement.org/countries/peru/ (accessed on 13 June 2025).
- Colombo, A.L.; Guimarães, T.; Silva, L.R.B.F.; Monfardini, L.P.A.; Cunha, A.K.B.; Rady, P.; Alves, T.; Rosas, R.C. Prospective observational study of candidemia in São Paulo, Brazil: Incidence rate, epidemiology, and predictors of mortality. Infect. Control Hosp. Epidemiol. 2007, 28, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Data and Statistics on Candidemia; CDC: Atlanta, GA, USA, 2024. Available online: https://www.cdc.gov/candidiasis/data-research/facts-stats/index.html (accessed on 13 June 2025).
- Bonaldo, G.; Jewtuchowicz, V.M. Candidiasis Invasiva en Pacientes con COVID-19 [Internet]. 2022. Available online: https://repositorio.uai.edu.ar/handle/123456789/400 (accessed on 13 June 2025).
- Villanueva-Lozano, H.; Treviño-Rangel, R.d.J.; González, G.M.; Ramírez-Elizondo, M.T.; Lara-Medrano, R.; Aleman-Bocanegra, M.C.; Guajardo-Lara, C.E.; Gaona-Chávez, N.; Castilleja-Leal, F.; Torre-Amione, G.; et al. Outbreak of Candida auris infection in a COVID-19 hospital in Mexico. Clin. Microbiol. Infect. 2021, 27, 813. [Google Scholar] [CrossRef]
- Alvarez-Moreno, C.A.; Cortés, J.A.; Denning, D.W. Burden of fungal infections in Colombia. J. Fungi 2018, 4, 41. [Google Scholar] [CrossRef]
- Ministério da Saúde. Comissão Nacional de Incorporação de Tecnologias no Sistema Único de Saúde—CONITEC. Análise de Custo-Efetividade e Impacto Orçamentário do Uso de Anidulafungina Como Tratamento de Primeira Linha Para Candidíase Invasiva No Brasil; Ministério da Saúde: Brasília, Brazil, 2020; pp. 12–15. Available online: https://www.gov.br/conitec/pt-br (accessed on 13 June 2025).
- de Mello Vianna, C.M.; Mosegui, G.B.G.; da Silva Rodrigues, M.P. Cost-effectiveness analysis and budgetary impact of anidulafungin treatment for patients with candidemia and other forms of invasive candidiasis in Brazil. Rev. Inst. Med. Trop. Sao Paulo 2023, 65, e9. [Google Scholar]
- Wan Ismail, W.N.A.; Jasmi, N.; Khan, T.M.; Hong, Y.H.; Neoh, C.F. The economic burden of candidemia and invasive candidiasis: A systematic review. Value Health Reg. Issues 2020, 21, 53–58. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Diekema, D.J. Epidemiology of invasive candidiasis: A persistent public health problem. Clin. Microbiol. Rev. 2007, 20, 133–163. [Google Scholar] [CrossRef]
- Sifuentes-Osornio, J.; Corzo-León, D.E.; Ponce-De-León, L.A. Epidemiology of invasive fungal infections in Latin America. Curr. Fungal Infect. Rep. 2012, 6, 23. [Google Scholar] [CrossRef]
- Márquez, F.; Iturrieta, I.; Calvo, M.; Urrutia, M.; Godoy-Martínez, P. Epidemiología y susceptibilidad antifúngica de especies causantes de candidemia en la ciudad de Valdivia, Chile. Rev. Chil. Infectol. 2017, 34, 441–446. [Google Scholar] [CrossRef]
- Groisman Sieben, R.; Paternina-de la Ossa, R.; Waack, A.; Casale Aragon, D.; Bellissimo-Rodrigues, F.; Israel do Prado, S.; Cervi, M.C. Risk factors and mortality of candidemia in a children’s public hospital in São Paulo, Brazil. Rev. Argent. Microbiol. 2024, 56, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Bhargava, A.; Klamer, K.; Sharma, M.; Ortiz, D.; Saravolatz, L. Candida auris: A continuing threat. Microorganisms 2025, 13, 402. [Google Scholar] [CrossRef] [PubMed]
- Chowdhary, A.; Sharma, C.; Meis, J.F. Candida auris: A rapidly emerging cause of hospital-acquired multidrug-resistant fungal infections globally. PLoS Pathog. 2017, 13, e1006290. [Google Scholar] [CrossRef] [PubMed]
- Lanna, M.; Lovatto, J.; de Almeida, J.N.; Medeiros, E.A.; Colombo, A.L.; García-Effron, G. Epidemiological and microbiological aspects of Candida auris in Latin America: A literature review. J. Med. Mycol. 2025, 35, 115–125. [Google Scholar] [CrossRef]
- Ortiz-Roa, C.; Valderrama-Rios, M.C.; Sierra-Umaña, S.F.; Rodríguez, J.Y.; Muñetón-López, G.A.; Solórzano-Ramos, C.A.; Escandón, P.; Alvarez-Moreno, C.A.; Cortés, J.A. Mortality caused by Candida auris bloodstream infections in comparison with other Candida species: A multicentre retrospective cohort. J. Fungi 2023, 9, 456. [Google Scholar] [CrossRef]
- Toda, M.; Williams, S.R.; Berkow, E.L.; Farley, M.M.; Harrison, L.H.; Bonner, L.; Marceaux, K.M.; Hollick, R.; Zhang, A.Y.; Schaffner, W. Population-based active surveillance for culture-confirmed candidemia—Four sites, United States, 2012–2016. MMWR Surveill. Summ. 2020, 68, 1–15. [Google Scholar] [CrossRef]
- Koehler, P.; Stecher, M.; Cornely, O.; Koehler, D.; Vehreschild, M.; Bohlius, J.; Wisplinghoff, H.; Vehreschild, J. Morbidity and mortality of candidemia in Europe: An epidemiologic meta-analysis. Clin. Microbiol. Infect. 2019, 25, 1200–1212. [Google Scholar] [CrossRef]
- Doi, A.M.; Pignatari, A.C.C.; Edmond, M.B.; Marra, A.R.; Camargo, L.F.A.; Siqueira, R.A.; da Mota, V.P.; Colombo, A.L. Epidemiology and microbiologic characterization of nosocomial candidemia from a Brazilian national surveillance program. PLoS ONE 2016, 11, e0146460. [Google Scholar] [CrossRef]
- Barahona Correra, J.E.; Calvo Valderrama, M.G.; Romero Alvernia, D.M.; Angulo Mora, J.; Alarcón Figueroa, L.F.; Rodríguez-Malagón, M.N.; Garzón, J.R. Epidemiology of candidemia at a university hospital in Colombia, 2008–2014. Univ. Med. 2019, 60, 305–315. [Google Scholar] [CrossRef]
- Santolaya, M.E.; Alvarado, T.; Queiroz-Telles, F.; Colombo, A.L.; Zurita, J.; Tiraboschi, I.N.; Cortes, J.A.; Thompson, L.; Guzman, M.; Sifuentes, J.; et al. Erratum: Active surveillance of candidemia in children from Latin America: A key requirement for improving disease outcome. Pediatr. Infect. Dis. J. 2014, 33, 333. [Google Scholar] [CrossRef]
- da Silva, C.M.; de Carvalho, A.M.R.; Macêdo, D.P.C.; Jucá, M.B.; Amorim Rde, J.M.; Neves, R.P. Candidemia in Brazilian neonatal intensive care units: Risk factors, epidemiology, and antifungal resistance. Braz. J. Microbiol. 2023, 54, 817–825. [Google Scholar] [CrossRef]
- de Medeiros, M.A.P.; de Melo, A.P.V.; de Oliveira Bento, A.; de Souza, L.B.F.C.; de Assis Bezerra Neto, F.; Garcia, J.B.L.; Zuza-Alves, D.L.; Francisco, E.C.; de Azevedo Melo, A.S.; Chaves, G.M. Epidemiology and prognostic factors of nosocomial candidemia in Northeast Brazil: A six-year retrospective study. PLoS ONE 2019, 14, e0221033. [Google Scholar] [CrossRef]
- Fernandez, J.; Erstad, B.L.; Petty, W.; Nix, D.E. Time to positive culture and identification for Candida bloodstream infections. Diagn. Microbiol. Infect. Dis. 2009, 64, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, B.; Varela, D.; Fontecha, G.; Torres, K.; Cornely, O.A.; Salmanton-García, J. Strengthening fungal infection diagnosis and treatment: An in-depth analysis of capabilities in Honduras. Open Forum Infect. Dis. 2024, 11, ofae578. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Zou, Y.; Dai, Y.; Lu, H.; Zhang, W.; Chang, W.; Wang, Y.; Nie, Z.; Wang, Y.; Jiang, X. Adaptive morphological changes link to poor clinical outcomes by conferring echinocandin tolerance in Candida tropicalis. PLoS Pathog. 2025, 21, e1013220. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Cai, L.; Bilal, H.; Khan, M.N.; Fang, W.; Zhang, D.; Yao, F.; Wang, X.; Wang, Q.; Hou, B.; et al. An 11-year retrospective analysis of candidiasis epidemiology, risk factors, and antifungal susceptibility in a tertiary care hospital in China. Sci. Rep. 2025, 15, 7240. [Google Scholar] [CrossRef]
- Govender, N.P.; Todd, J.; Nel, J.; Mer, M.; Karstaedt, A.; Cohen, C. HIV infection as risk factor for death among hospitalized persons with candidemia, South Africa, 2012–2017. Emerg. Infect. Dis. 2021, 27, 1607–1615. [Google Scholar] [CrossRef]
- González de Molina, F.J.; León, C.; Ruiz-Santana, S.; Saavedra, P. Assessment of candidemia-attributable mortality in critically ill patients using propensity score matching analysis. Crit. Care 2012, 16, R84. [Google Scholar] [CrossRef]
- World Health Organization, Pan American Health Organization. Health of Refugees and Migrants: Regional Situation; Pan American Health Organization: Washington, DC, USA, 2018; Available online: https://cdn.who.int/media/docs/default-source/documents/publications/health-of-refugees-migrants-paho-20181c89615b-3e93-4b59-9d25-2979e6b0cbcb.pdf?sfvrsn=2ca33a0b_1 (accessed on 13 June 2025).
- Ellis, D.; Marriott, D.; Hajjeh, R.A.; Warnock, D.; Meyer, W.; Barton, R. Epidemiology: Surveillance of fungal infections. Med. Mycol. 2000, 38, 173–182. [Google Scholar] [CrossRef]
- Ruiz, G.O.; Osorio, J.; Valderrama, S.; Álvarez, D.; Díaz, R.E.; Calderón, J.; Ballesteros, D.; Franco, A. Factores de riesgo asociados a candidemia en pacientes críticos no neutropénicos en Colombia. Med. Intensiva 2016, 40, 139–144. [Google Scholar] [CrossRef]
- Ministerio de Salud de Colombia. Incidencia de Candidemia en Migrantes Desplazados en Regiones Fronterizas (2008–2010); Informe interno; Ministerio de Salud de Colombia: Bogotá, Colombia, 2011; Plan de Respuesta. Available online: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/COM/plan-respuesta-salud-migrantes.pdf (accessed on 13 June 2025).
- Ministério da Saúde de Brasil. Incidencia de Candidemia en Pacientes Desplazados en Zonas Rurales Afectadas Por Violencia De Pandillas (2012–2015); [informe interno] No publicado; Ministério da Saúde de Brasil: Brasília, Brazil, 2016.
- Secretaría de Salud (México). Incidencia de Candidemia en Migrantes en Tránsito en Estado Fronterizo (2015–2018); [Informe interno] No publicado; Secretaría de Salud (México): Ciudad de México, Mexico, 2019.
- Ministerio de Salud (Haití). Brotes de Candidemia en Refugiados Internos en Puerto Príncipe (2020–2023); [Informe interno] No publicado; Ministerio de Salud (Haití): Puerto Príncipe, Haiti, 2024.
- Ministério da Saúde de Brasil. Costos Hospitalarios de Candidemia en Migrantes en Hospitales Públicos (2012–2015); [Informe interno] No publicado; Ministério da Saúde de Brasil: Brasília, Brazil, 2016.
- Ministerio de Salud (Colombia). Costos de Tratamientos Antifúngicos en Candidemia de Migrantes (2008–2010); [Informe interno] No publicado; Ministerio de Salud (Colombia): Bogotá, Colombia, 2011.
- International Organization for Migration (OIM). Secuelas de Candidemia en Población Desplazada: Impacto en Productividad (2016–2020); [Informe técnico]; OIM: Ginebra, Switzerland, 2021. [Google Scholar]
- UNHCR. Carga Económica Familiar de Enfermedades Fúngicas en Refugiados de Centroamérica (2018–2019); [Informe interno]; ACNUR: Ginebra, Switzerland, 2020. [Google Scholar]
- Médecins Sans Frontières (MSF). Asignación de Recursos Para Fungemias en Clínicas Móviles en Contextos de Conflicto (2018–2022); Informe interno; MSF: París, France, 2022. [Google Scholar]
- Ministério da Saúde de Brasil. Perfil de Especies de Candida en Pacientes Desplazados Atendidos en Campañas Móviles (2012–2015); [Informe interno] No publicado; Ministério da Saúde de Brasil: Brasília, Brazil, 2016.
- Ministerio de Salud (Colombia). Aislamientos de C. parapsilosis en Clínicas Móviles Para Migrantes (2008–2010); [Informe Interno] No publicado; Ministerio de Salud (Colombia): Bogotá, Colombia, 2011.
- Instituto de Salud de Venezuela. Resistencia a fluconazol en C. tropicalis en Campamentos de Desplazados (2017–2021); [Informe interno] No publicado; Instituto de Salud de Venezuela: Caracas, Venezuela, 2022.
- Secretaría de Salud de México. Resistencia a fluconazol en C. glabrata en Migrantes VIH Positivos y Diabéticos Sin Control (2015–2018); [Informe interno] No publicado; Secretaría de Salud de México: Ciudad de México, Mexico, 2019.
- Instituto Nacional de Salud (INAS) (Colombia), Ministerio de Salud (Venezuela). Brotes de Candida Auris en Campamentos de Desplazados (2017–2023); [Informe interno] No publicado; Instituto Nacional de Salud (INAS) (Colombia): Bogotá/Caracas, Colombia, 2024.
- Ministerio de Salud (Colombia). Mortalidad a 30 días de Candidemia en Pacientes Desplazados en Regiones Fronterizas (2008–2010); [Informe interno] No publicado; Ministerio de Salud (Colombia): Bogotá, Colombia, 2011.
- Cortés, J.A.; Montañez, A.M.; Carreño-Gutiérrez, A.M.; Reyes, P.; Gómez, C.H.; Pescador, A.; Ariza, B.; Rosso, F. Risk factors for mortality in Colombian patients with candidemia. J. Fungi 2021, 7, 460. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Salud (Colombia). Informe Interno Sobre Candidemia en Poblaciones Desplazadas; [Informe interno], Datos no publicados; Ministerio de Salud (Colombia): Bogotá, Colombia, 2022.
- Ministério da Saúde de Brasil. Mortalidad en Migrantes con Candidemia Atendidos en Unidad de Cuidados Intensivos Móvil en Zonas Rurales Afectadas por Violencia de Pandillas (2012–2015); [Informe interno] No publicado; Ministério da Saúde de Brasil: Brasília, Brazil, 2016.
- Secretaría de Salud de Honduras en Representación de la Red de Salud de Centroamérica. Mortalidad de Candidemia en Migrantes Atendidos en Clínicas Móviles a Lo Largo de Rutas Migratorias (2016–2019); [Informe interno] No publicado; Secretaría de Salud de Honduras en Representación de la Red de Salud de Centroamérica: Tegucigalpa, Honduras, 2020.
- Ministerio de Salud Pública (El Salvador). Guía de Manejo de Infecciones Fúngicas en Pacientes con VIH y Diabetes; [Informe interno] No publicado; Ministerio de Salud Pública (El Salvador): San Salvador, El Salvador, 2021.
- OPS/OMS Informe Epidemiológico de Infecciones Oportunistas en Honduras. Tegucigalpa: Organización Panamericana de la Salud. 2022. Available online: https://www.paho.org/es/honduras (accessed on 13 June 2025).
- Ministerio de Salud Pública y Población de Haití. Mortalidad por Candidemia en Refugiados Internos en Hospitales de Campaña tras Crisis Humanitaria (2020–2023); [Informe interno] No publicado; Ministerio de Salud Pública y Población de Haití: Puerto Príncipe, Haiti, 2024.
- Nucci, M.; Queiroz-Telles, F.; Tobón, A.M.; Restrepo, A.; Colombo, A.L. Epidemiology of opportunistic fungal infections in Latin America. Clin. Infect. Dis. 2010, 51, 561–570. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, M.L.; Nosanchuk, J.D. Fungal diseases as neglected pathogens: A wake-up call to public health officials. PLoS Negl. Trop. Dis. 2020, 14, e0007964. [Google Scholar] [CrossRef] [PubMed]
- Lage, A.L.; Guimarães, T.; Richtmann, R.; Queiroz-Telles, F.; Costa Salles, M.J.; Colombo, A.L. The north and south of candidemia: Issues for Latin America. Mycopathologia 2008, 165, 115–122. [Google Scholar]
- Eggimann, P.; Garbino, J.; Pittet, D. Epidemiology of Candida species infections in critically ill non-immunosuppressed patients. Lancet Infect. Dis. 2003, 3, 685–702. [Google Scholar] [CrossRef]
- Panel on Opportunistic Infections in Adults Adolescents with HIV. Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV: Candidiasis (Mucocutaneous); Department of Health and Human Services: Washington, DC, USA, 2025.
- Sobel, J.D. Recurrent vulvovaginal candidiasis. Am. J. Obstet. Gynecol. 2016, 214, 15–21. [Google Scholar] [CrossRef]
- Global Action Fund for Fungal Infections (GAFFI). Country Fungal Disease Burdens [Internet]. Geneva: GAFFI. 2023. Available online: https://gaffi.org/media/country-fungal-disease-burdens/ (accessed on 14 June 2025).
- Colombo, A.L.; Guimarães, T.; Camargo, L.F.R.; Richtmann, R.; Queiroz-Telles, F.; Costa Salles, M.J.; da Cunha, C.A.; Yasuda, M.A.S.; Moretti, M.L.; Nucci, M. Brazilian guidelines for the management of candidiasis: Joint report of three medical societies. Braz. J. Infect. Dis. 2012, 16 (Suppl. 1), S1–S34. [Google Scholar] [CrossRef]
- Castro, L.Á.; Álvarez, M.I.; Martínez, E. Pseudomembranous candidiasis in HIV/AIDS patients in Cali, Colombia. Mycopathologia 2013, 175, 91–98. [Google Scholar] [CrossRef]
- Ministerio de Salud (Perú). Análisis de Situación de Salud—Perú; Informe Técnico; MINSA: Lima, Peru, 2021.
- Flondor, A.E.; Sufaru, I.G.; Martu, I.; Burlea, S.L.; Flondor, C.; Toma, V. Nutritional deficiencies and oral candidiasis in children from northeastern Romania: A cross-sectional biochemical assessment. Nutrients 2025, 17, 1815. [Google Scholar] [CrossRef]
- Wirtz, A.L.; Guillén, J.R.; Stevenson, M.; Ortiz, J.; Talero, M.Á.B.; Page, K.R.; López, J.J.; Porras, D.M.; Correa, J.F.R.; Núñez, R.L.; et al. HIV infection and engagement in the care continuum among migrants and refugees from Venezuela in Colombia: A cross-sectional, biobehavioural survey. Lancet HIV 2023, 10, e461–e471. [Google Scholar] [CrossRef]
- Oñate, J.M.; Rivas, P.; Pallares, C.; Saavedra, C.H.; Martínez, E.; Coronell, W.; López, E.; Berrio, I.; Álvarez-Moreno, C.A.; Roncancio, G.E.; et al. Consenso colombiano para el diagnóstico, tratamiento y prevención de la enfermedad por Candida spp. en niños y adultos. Infectio 2019, 23, 271–304. [Google Scholar] [CrossRef]
- UNAIDS. Informe Regional 2022: VIH/SIDA; UNAIDS: Ginebra, Switzerland, 2022. [Google Scholar]
- Organización Panamericana de la Salud (OPS). Panorama de la Diabetes en la Región de las Américas; OPS: Washington, DC, USA, 2023. [Google Scholar]
- Organización Panamericana de la Salud. Diabetes; Pan American Health Organization: Washington, DC, USA, 2023; Available online: https://www.paho.org/es/temas/diabetes (accessed on 14 June 2025).
- Organización Panamericana de la Salud. La OPS y GARDP colaborarán para hacer frente a la resistencia a los antibióticos en América Latina y el Caribe; Pan American Health Organization: Washington, DC, USA, 2024; Available online: https://www.paho.org/es/noticias/26-9-2024-ops-gardp-colaboraran-para-hacer-frente-resistencia-antibioticos-america-latina (accessed on 14 June 2025).
- World Health Organization (WHO). Social Determinants of Health in Countries in Conflict; WHO: Geneva, Switzerland, 2008. [Google Scholar]
- Nucci, M.; Engelhardt, M.; Hamed, K. Mucormycosis in South. America: A review of 143 reported cases. Mycoses 2019, 62, 730–738. [Google Scholar] [CrossRef]
- Organización Mundial de la Salud (OMS). Hacinamiento en Los Hogares. NCBI Bookshelf [Internet]. 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK583397/ (accessed on 14 June 2025).
- World Health Organization (WHO). Health of Refugees and Migrants. [Internet]. 2025. Available online: https://www.who.int/es/health-topics/refugee-and-migrant-health#tab=tab_1 (accessed on 14 June 2025).
- Gómez-Vasco, J.D.; Candelo, C.; Victoria, S.; Luna, L.; Pacheco, R.; Ferro, B.E. Vulnerabilidad social, un blanco fatal de la coinfección tuberculosis-VIH en Cali. Infectio 2021, 25, 207–211. [Google Scholar] [CrossRef]
- Pan American Health Organization (PAHO). Tuberculosis in the Americas: Regional Report 2021; PAHO: Washington, DC, USA, 2021. [Google Scholar]
- Hassoun, N.; Kassem, I.I.; Hamze, M.; El Tom, J.; Papon, N.; Osman, M. Antifungal use and resistance in a lower–middle-income country: The case of Lebanon. Antibiotics 2023, 12, 1413. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Global Antimicrobial Resistance Surveillance System Early Implementation Protocol for Inclusion of Candida spp.; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Bezares Cóbar, P. Sistematización del Modelo de Vigilancia y Atención a la Salud del Trabajador Agrícola Migrante y su Familia en Guatemala; PAHO/WHO: Washington, DC, USA, 2021. [Google Scholar]
- United Nations Children’s Fund (UNICEF). Children on the Move: Refugees and Migrants; UNICEF: New York, NY, USA, 2023. [Google Scholar]
- Thomas-Rüddel, D.O.; Schlattmann, P.; Pletz, M.; Kurzai, O.; Bloos, F. Risk factors for invasive Candida infection in critically ill patients: A systematic review and meta-analysis. Chest 2022, 161, 345–355. [Google Scholar] [CrossRef] [PubMed]
- Instituto Colombiano de Bienestar Familiar (ICBF). Encuesta Nacional de Situación Nutricional 2015; ICBF: Bogotá, Colombia, 2015. [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. Colombia HIV Epidemiological Update 2023; UNAIDS: Geneva, Switzerland, 2023. [Google Scholar]
- Pan American Health Organization (PAHO). Tuberculosis Surveillance 2023; PAHO: Washington, DC, USA, 2023. [Google Scholar]
- Unidad para las Victimas de Colombia. Boletín Desplazamiento Interno 2022; UV: Bogotá, Colombia, 2022. [Google Scholar]
- Instituto Nacional de Salud (Colombia). Pro_Tuberculosis 2022: Lineamientos Para Manejo de la, TB; INS: Bogotá, Colombia, 2022.
- Pan American Health Organization. Latin America and Caribbean Regional Overview of Food Security and Nutrition 2022; PAHO: Washington, DC, USA, 2022. [Google Scholar]
- Ministerio de Desarrollo e Inclusión Social (Perú). Evaluación de Seguridad Alimentaria Ante Emergencias (ESAE) 2021; MIDIS: Lima, Peru, 2021.
- Pan American Health Organization (PAHO). Profiles of Diabetes Burden 2023; PAHO: Washington, DC, USA, 2023. [Google Scholar]
- Food and Agriculture Organization of the United Nations (FAO). Food Security and Nutrition in the World: Repurposing Food and Agricultural Policies to Make Healthy Diets More Affordable; FAO: Rome, Italy, 2022. [Google Scholar]
- World Health Organization (WHO). World Report on the Health of Refugees and Migrants 2022; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde Nutricional 2019; IBGE: Rio de Janeiro, Brazil, 2019. [Google Scholar]
- Ministry of Health Brazil. Epidemiological Bulletin HIV/AIDS 2020; MS: Brasília, Brazil, 2020.
- Médecins Sans Frontières (MSF). Protection Brief BRAZIL: Labour Market Inclusion of Haitian Refugees; MSF: Paris, France, 2024. [Google Scholar]
- Pan American Health Organization (PAHO). Burden of Kidney Diseases; PAHO: Washington, DC, USA, 2019. [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. Peru: HIV Epidemiological Update 2022; UNAIDS: Geneva, Switzerland, 2022. [Google Scholar]
- Rodriguez, L.; Bustamante, B.; Huaroto, L.; Agurto, C.; Illescas, R.; Ramirez, R.; Diaz, A.; Hidalgo, J. A multicentric study of Candida bloodstream infection in Lima-Callao, Peru: Species distribution, antifungal resistance and clinical outcomes. PLoS ONE 2017, 12, e0175172. [Google Scholar] [CrossRef] [PubMed]
- National Council for the Evaluation of Social Development Policy (Mexico). Informe Pobreza Alimentaria 2022; CONEVAL: Mexico City, Mexico, 2022. [Google Scholar]
- Cortés Cáceres, F.A.; Escobar Latapí, A.; Nahmad Sittón, S.; Andretta, J.S.; Teruel Belismelis, G.; Hernández Licona, G. Diagnóstico Sobre Alimentación y Nutrición: Report of Academic Investigators; CONEVAL: Mexico City, Mexico, 2025. [Google Scholar]
- Secretaría de Salud (México). EPOC en Población Rural 2019; Secretaría de Salud: Ciudad de México, Mexico, 2019.
- UNICEF. Update on the Context and Situation of Children—Haiti 2023 COAR; UNICEF: New York, NY, USA, 2023. [Google Scholar]
- Vega Ocasio, D.; Juin, S.; Berendes, D.; Heitzinger, K.; Prentice-Mott, G.; Desormeaux, A.M.; Charles, P.D.J.; Rigodon, J.; Pelletier, V.; Louis, R.J.; et al. Cholera outbreak—Haiti, September 2022–January 2023. MMWR Morb. Mortal. Wkly. Rep. 2024, 72, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Food and Agriculture Organization of the United Nations (FAO). Regional Overview of Food Security and Nutrition 2021; FAO: Rome, Italy, 2021. [Google Scholar]
- Food and Agriculture Organization of the United Nations (FAO). Latin America and the Caribbean Regional Overview of Food Security and Nutrition 2024; FAO: Rome, Italy, 2025. [Google Scholar]
- Ministerio de Salud (Colombia). Situación de Candidiasis en Campamentos de Refugiados Venezolanos (2018–2019); [Informe interno] No publicado; Ministerio de Salud (Colombia): Bogotá, Colombia, 2020.
- Secretaría de Salud (México). Estudio de Erupciones Interdigitales en Migrantes Centroamericanos en Tránsito (2019–2020); [Informe interno] No publicado; Secretaría de Salud (México): Tuxtla Gutiérrez, Mexico, 2021.
- UNICEF. Niñez en Movimiento: Revisión de Evidencia. UNICEF: New York, NY, USA; Available online: https://www.unicef.org/lac/media/40946/file/Ninez-en-movimiento-en-ALC.pdf (accessed on 13 June 2025).
- Ministerio de Salud (Bolivia). Condiciones Sanitarias y Candidiasis en Comunidades Rurales de Retornados (2018–2019); [Informe interno] No publicado; Ministerio de Salud (Bolivia): La Paz, Bolivia, 2020.
- Ministerio de Salud (Colombia). Malnutrición y Candidiasis en Desplazados de Arauca (2018–2019); [Informe interno] No publicado; Ministerio de Salud (Colombia): Bogotá, Colombia, 2020.
- Defensoría del Pueblo. Reporte desnutrición en niños y niñas menores de 5 años de edad en Colombia; Defensoría del Pueblo: Bogotá, Colombia, 2023. Available online: https://www.defensoria.gov.co/documents/20123/1657207/REPORTE%2BDESNUTRICI%C3%93N%2BEN%2BNI%C3%91OS%2BY%2BNI%C3%91AS%2BMENORES%2BDE%2B5%2BA%C3%91OS%2BDE%2BEDAD%2BEN%2BCOLOMBIA.pdf (accessed on 13 June 2025).
- Ministerio de Salud (Colombia). Prevalencia de VIH y Candidiasis en Migrantes Venezolanos (2018–2019); [Informe interno] No publicado; Ministerio de Salud (Colombia): Bogotá, Colombia, 2020.
- Ministerio de Salud Pública y Población (Haití). Informe Sobre Salud en Campamentos Pos-Terremoto (2010–2011); [Informe interno] No publicado; Ministerio de Salud Pública y Población (Haití): Puerto Príncipe, Haiti, 2012.
- Ministerio de Salud (Perú). Diabetes y Candidiasis en Comunidades Indígenas Desplazadas (2018); [Informe interno] No publicado; Ministerio de Salud (Perú): Lima, Peru, 2019.
- Instituto Nacional de Salud (Colombia). Coinfección TB/VIH y Candidemia en Desplazados Fronterizos (2017–2018); Informe interno; INS: Bogotá, Colombia, 2019.
- Ministerio de Salud (Guatemala). TB Extrapulmonar y Candidiasis Intraabdominal en Desplazados (2018); [Informe interno] No publicado; Ministerio de Salud (Guatemala): Ciudad de Guatemala, Guatemala, 2019.
- Secretaría de Salud (México). Uso de Antibióticos y Candidiasis en Migrantes Nicaragüenses (2019–2020); [Informe interno] No publicado; Secretaría de Salud (México): Ciudad de México, Mexico, 2021.
- Instituto Nacional de Salud Pública (México). Candidemia Asociada a Catéteres en Migrantes en Tapachula (2020); [Informe interno] No publicado; Instituto Nacional de Salud Pública (México): Cuernavaca, Mexico, 2021.
- Ministerio de Salud (Nicaragua). Salud Reproductiva y Candidiasis en Mujeres Migrantes (2019); [Informe interno] No publicado; Ministerio de Salud (Nicaragua): Managua, Nicaragua, 2020.
- Ministerio de Salud (Paraguay). Candidiasis Cutánea en Comunidades Indígenas Guaraní Desplazadas (2018); [Informe interno] No publicado; Ministerio de Salud (Paraguay): Asunción, Paraguay, 2019.
- Ministerio de Salud (República Dominicana). Candidiasis Oral en Migrantes Haitianos con VIH (2019–2020); [Informe interno] No publicado; Ministerio de Salud (República Dominicana): Santo Domingo, República Dominicana, 2021.
- Ministerio de Salud (Guatemala). Exposición a Candida Parapsilosis en Migrantes Agrícolas de Guatemala (2019); [Informe interno] No publicado; Ministerio de Salud (Guatemala): Washington, DC, USA, 2019. [Google Scholar]
- Ministerio de Salud (Perú). Candidiasis Interdigital en Trabajadores Agrícolas Expuestos a Plaguicidas (2019); [Informe interno] No publicado; Ministerio de Salud (Perú): Lima, Perú, 2020. [Google Scholar]
- Secretaría de Salud (Honduras). Impacto del Clima en Candidiasis de Migrantes en Rutas Costeras (2019); [Informe interno] No publicado; Secretaría de Salud (Honduras): Tegucigalpa, Honduras, 2020. [Google Scholar]
- Global Action Fund for Fungal Infections (GAFFI). Global Fungal Infection Forum 4 in Lima; GAFFI: Geneva, Switzerland, 2019. [Google Scholar]
- Global Action Fund for Fungal Infections (GAFFI). GAFFI’s Annual Report Outlines Its New Strategy—Access to Diagnostics and Antifungals, the Centerpiece of Its Efforts; GAFFI: Geneva, Switzerland, 2025. [Google Scholar]
- Koc, Ö.; Kessler, H.H.; Hoenigl, M.; Wagener, J.; Suerbaum, S.; Schubert, S.; Dichtl, K. Performance of multiplex PCR and β-1,3-D-glucan testing for the diagnosis of candidemia. J. Fungi 2022, 8, 614. [Google Scholar] [CrossRef]
- Pan American Health Organization (PAHO). Marco de Implementación de un Servicio de Telemedicina; PAHO: Washington, DC, USA, 2016. [Google Scholar]
- Donato, L.; González, T.; Canales, M.; Legarraga, P.; García, P.; Rabagliati, R. Evaluación del rendimiento de 1,3-β-D-glucano como apoyo diagnóstico de infecciones invasoras por Candida spp. en pacientes críticos adultos. Rev. Chil. Infectol. 2017, 34, 340–346. [Google Scholar] [CrossRef]
- Pemán, J.; Ruiz-Gaitán, A. Diagnosing invasive fungal infections in the laboratory today: It’s all good news? Rev. Iberoam. Micol. 2025, 42, 80–87. [Google Scholar] [CrossRef]
- Cornely, O.A.; Sprute, R.; Grothe, J.H.; Koehler, P.; Meis, J.F.; Reinhold, I.; Lass-Flörl, C.; Ostrosky-Zeichner, L.; Rautemaa-Richardson, R.; Revathi, G.; et al. Global guideline for the diagnosis and management of candidiasis: An initiative of the ECMM in cooperation with ISHAM and ASM. Lancet Infect. Dis. 2025, 25, e280–e293. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Pabón, J.C.; Tabares, B.; Gil, Ó.; Lugo-Sánchez, C.; Santana, A.; Barón, A.; Firacative, C. Candida non-albicans and non-auris causing invasive candidiasis in a fourth-level hospital in Colombia: Epidemiology, antifungal susceptibility, and genetic diversity. J. Fungi 2024, 10, 326. [Google Scholar] [CrossRef]
- Akpan, A.; Morgan, R. Oral candidiasis. Postgrad. Med. J. 2002, 78, 455–459. [Google Scholar] [CrossRef] [PubMed]
- Belmokhtar, Z.; Djaroud, S.; Matmour, D.; Merad, Y. Atypical and unpredictable superficial mycosis presentations: A narrative review. J. Fungi 2024, 10, 241. [Google Scholar] [CrossRef] [PubMed]
- Pappas, P.G.; Kauffman, C.A.; Andes, D.R.; Clancy, C.J.; Marr, K.A.; Ostrosky-Zeichner, L.; Reboli, A.C.; Schuster, M.G.; Vazquez, J.A.; Walsh, T.J.; et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 62, e1–e50. [Google Scholar] [CrossRef]
- Kullberg, B.J.; Arendrup, M.C. Invasive candidiasis. N. Engl. J. Med. 2015, 373, 1445–1456. [Google Scholar] [CrossRef]
- Pan American Health Organization (PAHO). GAFFI and PAHO Join Forces to Combat Fungal Disease in LATIN AMERICA and the Caribbean; PAHO: Washington, DC, USA, 2024. [Google Scholar]
- Tobar, A.; Silva, O.F.; Olivares, C.R.; Gaete, G.P.; Luppi, N.M.C. Candidiasis invasoras en el paciente crítico adulto. Rev. Chil. Infectol. 2011, 28, 41–49. [Google Scholar] [CrossRef]
- World Health Organization (WHO). WHO Issues Its First-Ever Reports on Tests and Treatments for Fungal Infections; WHO: Geneva, Switzerland, 2025. [Google Scholar]
- Pan American Health Organization (PAHO). La OPS Responde a la Crisis Humanitaria Grado 3 de Haití; PAHO: Washington, DC, USA, 2025. [Google Scholar]
- Pan American Health Organization (PAHO). El Libro Rojo: Documento de Orientación Para los Equipos Médicos que Responden a Emergencias de Salud en Conflictos Armados y Otros Entornos Inseguros; PAHO: Washington, DC, USA, 2025. [Google Scholar]
- Pan American Health Organization (PAHO). Salud y Migración en la Región de las AMÉRICAS al 31 de Marzo de 2024; PAHO: Washington, DC, USA, 2024. [Google Scholar]
- Global Action Fund for Fungal Infections (GAFFI). Antifungal Drug Maps; GAFFI: Geneva, Switzerland, 2025. [Google Scholar]
- Riera, F.; Luna, J.C.; Rabagliatti, R.; Scapellato, P.; Caeiro, J.P.; Magri, M.M.C.; Sotomayor, C.E.; Falci, D.R. Antifungal stewardship: The Latin American experience. Antimicrob. Steward. Health Care Epidemiol. 2023, 3, e78. [Google Scholar] [CrossRef]
- Pan American Health Organization (PAHO). Migración y Salud en las Américas; PAHO: Washington, DC, USA, 2023. [Google Scholar]
- USAID/International Organization for Migration. Sistematización de Buenas Prácticas y Lecciones Aprendidas en la Gestión de Centros de Recepción de Personas Migrantes Retornadas; IOM/USAID: Washington, DC, USA, 2024. [Google Scholar]
- Pan American Health Organization (PAHO). Ministerio de Salud Pública con Apoyo de OPS/OMS Lanza las Primeras Redes de Telemedicina en Tiempo Real de GUATEMALA; PAHO: Washington, DC, USA, 2020. [Google Scholar]
- Duque-Restrepo, C.M.; Muñoz-Monsalve, L.V.; Guerra-Bustamante, D.; Cardona-Maya, W.D.; Gómez-Velásquez, J.C. Blanco de calcoflúor: En búsqueda de un mejor diagnóstico. Rev. Med. Risaralda. 2023, 29, 39–48. [Google Scholar] [CrossRef]
- Gupta, M.; Chandra, A.; Prakash, P.; Banerjee, T.; Maurya, O.P.S.; Tilak, R. Fungal keratitis in north India: Spectrum and diagnosis by Calcofluor white stain. Indian. J. Med. Microbiol. 2015, 33, 462–463. [Google Scholar] [CrossRef]
- Global Action Fund for Fungal Infections (GAFFI). Report on Activities for 2020; GAFFI: Geneva, Switzerland, 2021. [Google Scholar]
- Brecha Cero. Haití Desarrolla Plataforma de Telemedicina [Internet]. 2020. Available online: https://brechacero.com/haiti-desarrolla-plataforma-de-telemedicina/ (accessed on 14 June 2025).
- Yarak, S.; Evandro, I.; Seron, E.; Torres Pisa, I. A teledermatologia na prática médica. Rev. Bras. Educ. Med. 2017, 41, 346–355. [Google Scholar] [CrossRef]
- González-Villalobos, C.; Santana-Chávez, L. Práctica clínico-quirúrgica: Experiencia en el programa Telederma de una unidad de medicina familiar. Rev. Med. Inst. Mex. Seguro Soc. 2011, 49, 407–411. [Google Scholar][Green Version]
- Organización Panamericana de la Salud (OPS). Guía de Intervención Humanitaria mhGAP [Internet]. 2016. Available online: https://iris.paho.org/bitstream/handle/10665.2/28413/9789275319031_spa.pdf (accessed on 14 June 2025).
- Global Action Fund for Fungal Infections (GAFFI). Antifungal Echinocandins Added to the WHO’s Essential Medicines List [Internet]. 2021. Available online: https://gaffi.org/antifungal-echinocandins-added-to-the-whos-essential-medicines-list/ (accessed on 14 June 2025).
- World Health Organization (WHO). WHO Model List of Essential Medicines, 23rd List, 2023 [Internet]. 2023. Available online: https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2023.02 (accessed on 14 June 2025).
- Ndyetukira, J.F.; Kwizera, R.; Ahimbisibwe, C.; Namujju, C.; Meya, D.B. Using single-dose liposomal amphotericin B for cryptococcal meningitis induction therapy: Nurse pearls and practical perspectives. Wellcome Open Res. 2024, 9, 253. [Google Scholar] [CrossRef] [PubMed]
- Clancy, C.J.; Nguyen, M.H. Emergence of Candida auris: An international call to arms. Clin. Infect. Dis. 2017, 64, 141–143. [Google Scholar] [CrossRef] [PubMed]
- Spruijtenburg, B.; Baqueiro, C.C.S.Z.; Colombo, A.L.; Meijer, E.F.J.; de Almeida, J.N.; Berrio, I.; Fernández, N.B.; Chaves, G.M.; Meis, J.F.; de Groot, T.; et al. Short tandem repeat genotyping and antifungal susceptibility testing of Latin American Candida tropicalis isolates. J. Fungi 2023, 9, 112. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.Y.; Chuang, Y.C.; Wu, U.I.; Sun, H.Y.; Wang, J.T.; Sheng, W.H.; Chen, Y.-C.; Chang, S.-C. Mechanisms of azole resistance and trailing in Candida tropicalis bloodstream isolates. J. Fungi 2021, 7, 603. [Google Scholar] [CrossRef]
- Bonilla-Oviedo, D. Candida en la Mira: Vigilancia de Aislamientos Resistentes en Colombia (Julio–Noviembre 2024) [Internet]. 2025. Available online: https://repositorio.uniandes.edu.co/entities/publication/7dcb6f4f-ad7b-463b-bb0b-f3198ad1e7cf (accessed on 14 June 2025).
- Ministério da Saúde de Brasil. Acceso y Costos de Antifúngicos en Hospitales Terciarios (2021); [Informe interno] No publicado; Ministério da Saúde de Brasil: Brasília, Brazil, 2021.
- Rosenthal, V.D.; Bat-Erdene, I.; Gupta, D.; Belkebir, S.; Rajhans, P.; Zand, F.; Myatra, S.N.; Afeef, M.; Tanzi, V.L.; Muralidharan, S.; et al. International Nosocomial Infection Control Consortium (INICC) report, data summary of 45 countries for 2012–2017: Device-associated module. Am. J. Infect. Control 2020, 48, 423–432. [Google Scholar] [CrossRef]
- Frías-De-León, M.G.; Hernández-Castro, R.; Conde-Cuevas, E.; García-Coronel, I.H.; Vázquez-Aceituno, V.A.; Soriano-Ursúa, M.A.; Farfán-García, E.D.; Ocharán-Hernández, E.; Rodríguez-Cerdeira, C.; Arenas, R.; et al. Candida glabrata antifungal resistance and virulence factors, a perfect pathogenic combination. Pharmaceutics 2021, 13, 1529. [Google Scholar] [CrossRef]
- Ministerio de Salud (Colombia). Informe de Brotes de Candida Auris en Campamentos de Desplazados (2022); [Informe interno] No publicado; Ministerio de Salud (Colombia): Bogotá, Colombia, 2022.
- Pan American Health Organization (PAHO). Epidemiological Updates: Candida Auris Outbreaks in Health Care Services (3 October 2016). Epidemiological Alert [Internet]. 2016. Available online: https://iris.paho.org/handle/10665.2/50649 (accessed on 14 June 2025).
- Ministerio de Salud (Colombia). Acceso a Antifúngicos en Poblaciones Desplazadas y Migrantes (2021); [Informe interno] No publicado; Ministerio de Salud (Colombia): Bogotá, Colombia, 2021.
- Ministério da Saúde de Brasil. Disponibilidad de Antifúngicos en Campamentos y Clínicas Móviles (2019); [Informe interno] No publicado; Ministério da Saúde de Brasil: Brasília, Brazil, 2019.
- Huang, Y.C.; Lin, T.-Y.; Leu, H.S.; Peng, H.L.; Wu, J.-H.; Chang, H.Y. Outbreak of Candida parapsilosis fungemia in neonatal intensive care units: Clinical implications and genotyping analysis. Infection 1999, 27, 97–102. [Google Scholar] [CrossRef]
- Pinhati, H.M.S.; Casulari, L.A.; Souza, A.C.R.; Siqueira, R.A.; Damasceno, C.M.G.; Colombo, A.L. Outbreak of candidemia caused by fluconazole-resistant Candida parapsilosis strains in an intensive care unit. BMC Infect. Dis. 2016, 16, 398. [Google Scholar] [CrossRef]
- Berkow, E.L.; Lockhart, S.R. Fluconazole resistance in Candida species: A current perspective. Infect. Drug Resist. 2017, 10, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Thomaz, D.Y.; Del Negro, G.M.B.; Ribeiro, L.B.; da Silva, M.; Carvalho, G.O.M.H.; Camargo, C.H.; de Almeida, J.N.; Motta, A.L.; Siciliano, R.F.; Sejas, O.N.E.; et al. A Brazilian inter-hospital candidemia outbreak caused by fluconazole-resistant Candida parapsilosis in the COVID-19 era. J. Fungi 2022, 8, 122. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Salud (Colombia). Barreras y Desafíos en el Acceso a Tratamientos Antimicóticos en Zonas Rurales y Fronterizas; [Informe interno] No publicado; Ministerio de Salud (Colombia): Bogotá, Colombia, 2020.
- Ministerio de Salud (México). Acceso a Consultas y Diagnósticos Especializados Para Candidiasis en Poblaciones Vulnerables; [Informe interno] No publicado; Ministerio de Salud (México): Ciudad de México, Mexico, 2019.
- Ministerio de Salud (El Salvador). Mortalidad por Candidemia en Población Desplazada y General en Hospitales Públicos; [Informe interno] No publicado; Ministerio de Salud (El Salvador): San Salvador, El Salvador, 2021. [Google Scholar]
- Ministerio de Salud (El Salvador). Morbimortalidad de Candidiasis Mucocutánea en Pacientes con VIH y Diabetes en Contexto de Desplazamiento; [Informe interno] No publicado; Ministerio de Salud (El Salvador): San Salvador, El Salvador, 2021. [Google Scholar]
- Harding, E.; Beckworth, C.; Fesselet, J.F.; Lenglet, A.; Lako, R.; Valadez, J.J. Using lot quality assurance sampling to assess access to water, sanitation and hygiene services in a refugee camp setting in South Sudan: A feasibility study. BMC Public Health 2017, 17, 630. [Google Scholar] [CrossRef]
- Médecins Sans Frontières (MSF). Informe de Actividades de MSF México–Centroamérica 2022; MSF: Ciudad de México, Mexico, 2022. [Google Scholar]
- Fouad, F.M.; Sparrow, A.; Tarakji, A.; Alameddine, M.; El-Jardali, F.; Coutts, A.P.; El Arnaout, N.; Karroum, L.B.; Jawad, M.; Roborgh, S.; et al. Health workers and the weaponisation of health care in Syria: A preliminary inquiry for The Lancet–American University of Beirut Commission on Syria. Lancet 2017, 390, 2516–2526. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Rapid Grey Literature Evidence Review to Support the Guideline on Emergency Risk Communication [Internet]. 2017. Available online: https://www.who.int/publications/m/item/rapid-grey-literature (accessed on 14 June 2025).
- Human Rights Watch (HRW). Informe Mundial 2022: COLOMBIA [Internet]. 2022. Available online: https://www.hrw.org/es/world-report/2022/country-chapters/colombia (accessed on 14 June 2025).
- Ministerio de Salud (Colombia). Desplazamiento Forzado Del Personal Sanitario en Contextos de Violencia; [Informe interno] No publicado; Ministerio de Salud (Colombia): Bogotá, Colombia, 2021. [Google Scholar]
- Moreno Páez, L.F.; Cortes Mendoza, L. Estudio de Utilización de Antibióticos en Una IPS de Atención Médica Domiciliaria de la Ciudad de BOGOTÁ Durante la Prestación de Servicio Médico a Pacientes Mayores de 18 Años Desde Marzo de 2020. Tesis [Internet]. 2022. Available online: https://repository.udca.edu.co/server/api/core/bitstreams/95e506d0-a0d2-46d6-b2d7-53548928c620/content (accessed on 14 June 2025).
- Human Rights Watch (HRW). México—Country Page [Internet]. 2025. Available online: https://www.hrw.org/es/americas/mexico (accessed on 14 June 2025).
- Secretaría de Salud (México). Informe Sobre Interrupción de Cadenas de Suministro de Medicamentos en Zonas de Violencia; [Informe interno] No publicado; Secretaría de Salud (México): Ciudad de México, Mexico, 2021. [Google Scholar]
- Akinosoglou, K.; Livieratos, A.; Asimos, K.; Donders, F.; Donders, G.G.G. Fluconazole-resistant vulvovaginal candidosis: An update on current management. Pharmaceutics 2024, 16, 1555. [Google Scholar] [CrossRef]
- Pan American Health Organization (PAHO). Haiti; Pan American Health Organization: Washington, DC, USA, 2025; Available online: https://www.paho.org/fr/haiti (accessed on 14 June 2025).
- International Organization for Migration (IOM). El Salvador Crisis Response Plan 2023–2025. [Internet]. 2023. Available online: https://crisisresponse.iom.int/response/el-salvador-crisis-response-plan-2023-2025 (accessed on 14 June 2025).
- UNHCR. Situación de El Salvador, Guatemala y Honduras | Enfoque Global [Internet]. 2024. Available online: https://reporting.unhcr.org/operational/situations/el-salvador-guatemala-and-honduras-situation (accessed on 13 June 2025).
- UNICEF. UNICEF El Salvador [Internet]. Available online: https://www.unicef.org/elsalvador/ (accessed on 14 June 2025).
- Alberto, S.; Rodríguez, M.; Noemy, I.; Medrano, M.; Carolina, B.; Tobías, M. Prevalencia de Infecciones Vaginales en Mujeres. [Informe interno], No publicado. 2024. [Google Scholar]
- Kim, S.H.; Mun, S.J.; Kang, J.S.; Moon, C.; Kim, H.T.; Lee, H.Y. Multifaceted evaluation of antibiotic therapy as a factor associated with candidemia in non-neutropenic patients. J. Fungi 2023, 9, 134. [Google Scholar] [CrossRef]
- Unidad para las Víctimas de Colombia. Registro Nacional de Desplazados Internos; UV: Bogotá, Colombia, 2023. [Google Scholar]
- Ombelet, S.; Barbé, B.; Affolabi, D.; Ronat, J.B.; Lompo, P.; Lunguya, O.; Jacobs, J.; Hardy, L. Best practices of blood cultures in low- and middle-income countries. Front. Med. 2019, 6, 26. [Google Scholar] [CrossRef]
- Ministerio de Salud (Colombia). Seguimiento a la Situación de Salud de la Población Migrante Procedente de Venezuela, Para el Período Comprendido Entre el 1 de Marzo de 2017 y el 31 de Diciembre de 2022; Informe interno; Ministerio de Salud: Bogotá, Colombia, 2022.
- Ministério da Saúde de Brasil. Violencia Urbana y Desabastecimiento en Regiones Amazónicas: Impacto en Infecciones Fúngicas; [Informe interno] No publicado; Ministério da Saúde de Brasil: Brasília, Brazil, 2022.
- Agência Nacional de Vigilância Sanitária. Resistência aos Antimicrobianos é Coisa Séria! Informe Público; Anvisa: Brasília, Brazil, 2024. [Google Scholar]
- Pan American Health Organization (PAHO). Informe Anual OPS 2022; PAHO: Washington, DC, USA, 2022. [Google Scholar]
- Seguro Integral de Salud (Perú). Cobertura de Antifúngicos: Fluconazol, Equinocandinas y Anfotericina B Liposomal; Informe interno; SIS: Lima, Perú, 2023. [Google Scholar]
- Villaseca, R.; Ovalle, A.; Amaya, F.; Labra, B.; Escalona, N.; Lizana, P.; Montoya, M.J.; Martínez, E.L.Y.M.A. Infecciones vaginales en un centro de salud familiar de la Región Metropolitana, Chile. Rev. Chil. Infectol. 2015, 32, 30–36. [Google Scholar] [CrossRef]
- Martinez Rosado, L.L.; Cardona-Arias, J.A. Infecciones fúngicas en un hospital público de referencia para la atención de personas con VIH/SIDA, Medellín 2013–2017. Med. UIS 2020, 33, 17–24. [Google Scholar][Green Version]
- Organización Panamericana de la Salud (OPS). Sistemas de Laboratorio; Pan American Health Organization: Washington, DC, USA; Available online: https://www.paho.org/es/temas/sistemas-laboratorio (accessed on 14 June 2025).
- Pineda-Murillo, J.; Cortés-Figueroa, Á.; Uribarren-Berrueta, T.d.N.J.; Castañón-Olivares, L.R. Candidosis vaginal: Revisión de la literatura y situación de México y otros países latinoamericanos. Rev. Med. Risaralda. 2017, 23, 38–44. [Google Scholar][Green Version]
- Lynch, T.; Peirano, G.; Lloyd, T.; Read, R.; Carter, J.; Chu, A.; Shaman, J.A.; Jarvis, J.P.; Diamond, E.; Ijaz, U.Z.; et al. Molecular diagnosis of vaginitis: Comparing quantitative PCR and microbiome profiling approaches to current microscopy scoring. J. Clin. Microbiol. 2019, 57, e00300-19. [Google Scholar] [CrossRef]
- CVSP/OPS. Identificación y Sensibilidad a Los Antifúngicos en Levaduras del Género Candida [Internet]. 2021. Available online: https://campus.paho.org/es/curso/Candida-Metodos-Identificacion-Sensibilidad (accessed on 14 June 2025).
- Boonsilp, S.; Homkaew, A.; Phumisantiphong, U.; Nutalai, D.; Wongsuk, T. Species distribution, antifungal susceptibility, and molecular epidemiology of candida species causing candidemia in a tertiary care hospital in Bangkok, Thailand. J. Fungi 2021, 7, 577. [Google Scholar] [CrossRef]
- Instituto Nacional de Salud (Colombia). Manual de Procedimientos Técnicos para el Diagnóstico Micológico; Instituto Nacional de Salud: Bogotá, Colombia, 2019; Available online: https://hdl.handle.net/20.500.14196/915 (accessed on 14 June 2025).
- World Health Organization (WHO). WHO Releases First-Ever List of Health-Threatening Fungi [Internet]. 2022. Available online: https://www.who.int/es/news/item/25-10-2022-who-releases-first-ever-list-of-health-threatening-fungi (accessed on 14 June 2025).
- Donders, G.; Sziller, I.O.; Paavonen, J.; Hay, P.; de Seta, F.; Bohbot, J.M.; Kotarski, J.; Vives, J.A.; Szabo, B.; Cepuliené, R.; et al. Management of recurrent vulvovaginal candidosis: Narrative review of the literature and European expert panel opinion. Front. Cell. Infect. Microbiol. 2022, 12, 934353. [Google Scholar] [CrossRef]
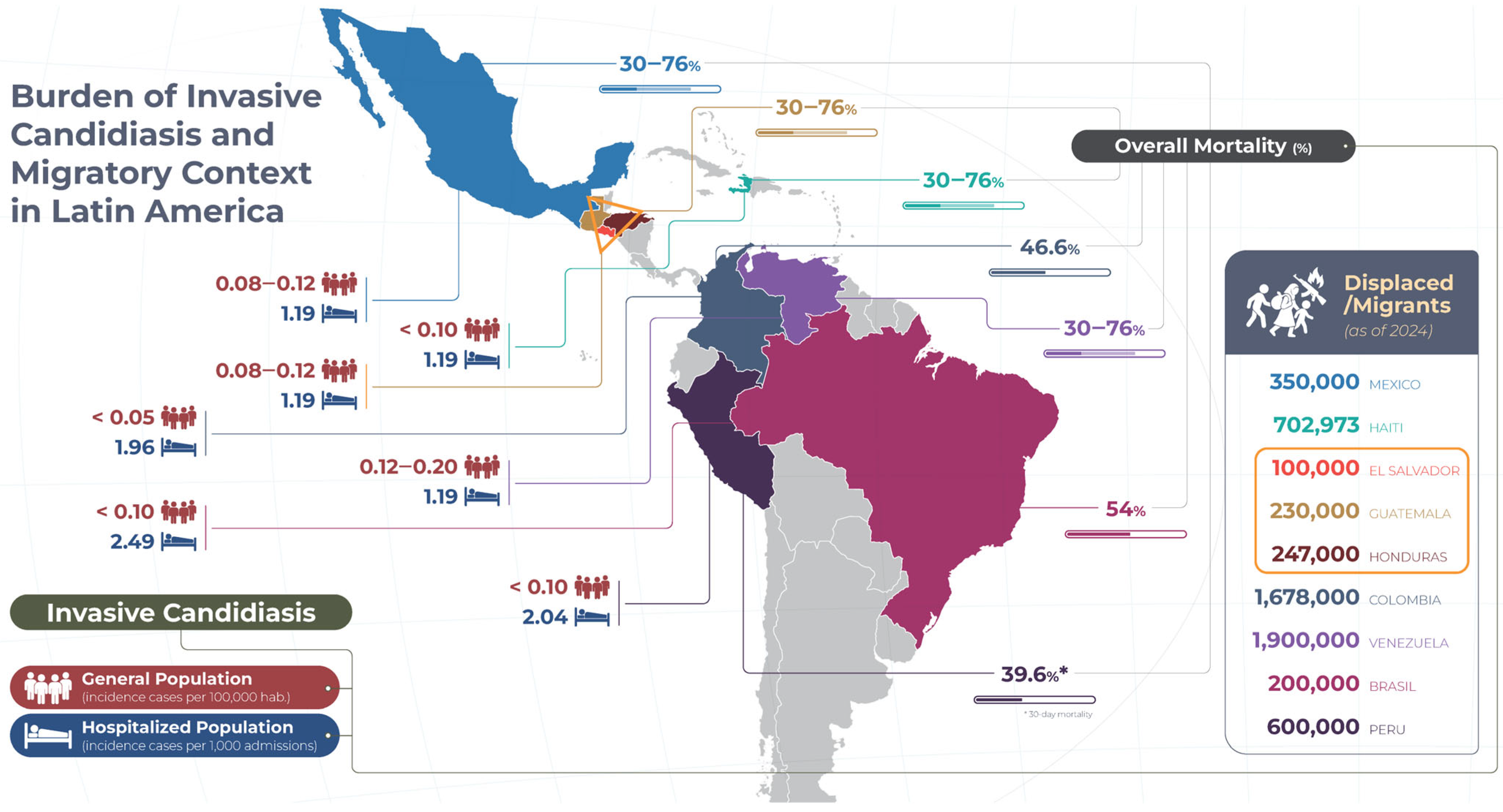
| Country | Type of Conflict/Violence | Key Period | Internally Displaced Persons/Migrants-Refugees (Estimates) | Key Findings |
|---|---|---|---|---|
| Mexico | Drug trafficking and violence by criminal groups | 2006–2020 | –/127,796 1 |
|
| Haiti | Political instability, gang violence, and natural disasters | 2004–2020 | 702,973/350,000 2 |
|
| El Salvador | Gang violence (MS-13, Barrio 18) | 2000–2020 | 513,000/234,000 3 |
|
| Guatemala | Civil war (1960–1996) and post-conflict violence | 1960–1996/2000–2020 |
| |
| Honduras | Gang violence and organized crime | 2000–2020 |
| |
| Colombia | Internal armed conflict (FARC, paramilitaries) | 2000–2020 | 6,900,000/3,000,000 + 2,900,000 4 |
|
| Venezuela | Sociopolitical crisis and high levels of street violence | 2014–2020 | –/7,770,000 5 |
|
| Brazil | Urban violence and organized crime (favelas, militias) | 2000–2020 | –/790,000 6 |
|
| Peru | Internal conflict (Sendero Luminoso (Shining Path) and State response) | 1980–2000 | –/Not available |
|
| Country | Main Risk Factors for IC | Common Conditions and Fungal Risk General Population | Common Conditions and Fungal Risk Displaced/Migrant Population * | Comments |
|---|---|---|---|---|
| Mexico | - CVC—Broad-spectrum antibiotics—TPN—Colonization by Candida | - Infant malnutrition (13%)—HIV/AIDS (0.3%)—TB (22/100,000) - Fungal risk: 1.19‰ (regional mean). Associated with CVC and TPN | - Malnutrition and anemia in Central American migrants—COPD in rural displaced - Fungal risk: probable aspergillosis and candidemia in detention centers | The high rotation in shelters and the presence of wet soils increase the exposure to fungal spores. |
| Haiti | - Broad-spectrum antibiotics—CVC—TPN | - Severe malnutrition (22%)—Epidemics of cholera and diarrhea - Fungal risk: post-breakout mucocutaneous mycoses; limited data on IC | - Critical post-disaster malnutrition—Cholera outbreaks in camps - Fungal risk: probable increase in mucocutaneous and systemic candidiasis | Sanitary collapse and lack of available antifungals limit the management of deep infections. |
| Central America Northern Triangle (El Salvador. Guatemala. Honduras) | - Broad-spectrum antibiotics—CVC—TPN—Invasive procedures | - Chronic malnutrition (25–30%)—TB (≈100/100,000)—Trauma and violence - Fungal risk: skin cysts and candidemia in municipal ICUs | - Malnutrition in rural displaced persons—TB in informal camps - Fungal risk: IC in burns and associated with CVC | The insecurity and dispersion of the population make prevention and timely treatment interventions difficult. |
| Colombia | - Broad-spectrum antibiotics (OR 5.6)—CVC (OR 4.7)—TPN (OR 4.6)—Colonization by Candida | - Chronic malnutrition (10.5%)—HIV/AIDS (0.4%)—TB (21/100,000) - Fungal risk: candidemia associated with CVC. TPN. and antibiotics (OR 5.6) | - Acute and chronic malnutrition—HIV/AIDS (~0.5%)—Elevated risk for pulmonary and extrapulmonary TB - Fungal risk: similar to the general hospitalized. aggravated by overcrowding and malnutrition | The combination of malnutrition and overcrowding enhances immunosuppression. increasing susceptibility to HF. |
| Venezuela | Same as Colombia. but with scarce local data | - Infant malnutrition (11.3%)—Diabetes (8%)—TB (17/100,000) - Fungal risk: similar to Latin America, with local under-registration | - Malnutrition due to food crisis—Chronic diseases (diabetes, HTN)—TB in returnees - Fungal risk: possible delay in diagnosis, with poor surveillance | The humanitarian crisis hinders timely access to antifungal diagnosis and treatment. |
| Brazil | - CVC—Broad-spectrum antibiotics—TPN—Recent surgery | - Infant malnutrition (7.4%)—HIV/AIDS (0.4%)—TB (32/100,000) - Fungal risk: outbreaks of candidemia in the ICU; increased isolates of N. glabratus | - Moderate malnutrition in Haitian refugees—HIV/AIDS in urban displaced persons—CKD (dialysis) in Haitian refugees—Chronic kidney disease (dialysis) in Haitian refugees - Fungal risk: elevated in dialysis and ICU patients | Migration from Haiti generates social stress and hinders the continuity of antifungal treatments. |
| Peru | - Broad-spectrum antibiotics—CVC—Recent surgery—MV—TPN | - Infant malnutrition (12%)—TB (119/100 000)—HIV/AIDS (0.3%) - Fungal risk: incidence of 2.04‰ in ICU; mortality 39.6% | - Malnutrition in rural displaced persons—Extrapulmonary TB—TB-HIV co-infection in migrants - Fungal risk: similar to general inpatients | Internal-urban displacement delays seeking care, increasing fungal complications. |
| Country | IC Burden (Incidence; Mortality) | Diagnosis and Treatment General Population | Diagnosis and Treatment Displaced/Migrant Population | Comments |
|---|---|---|---|---|
| Mexico | 1.19‰; 30–76% (regional mean) | Diagnosis:—Cultures and stains (48–72 h)-BDG/AGA (3 national institutes)-MALDI-TOF (5 high-complexity hospitals) Treatment:—FCZ-Standard AmB—L-AmB (limited)-Echinocandins (available, irregular distribution) | Diagnosis:—Cultures and stains in large hospitals—BDG and MALDI-TOF almost absent at the second level Treatment:—FCZ-D-AmB-Echinocandins (very limited access) | Existing national protocol, but uneven distribution of reagents and drugs delays the management of migrants and displaced persons. |
| Haiti | 1.19‰; 30–76% (regional mean) | Diagnosis:—Cultures in 2 central laboratories (48–72 h)-No BDG, PCR, or MALDI-TOF. Treatment:—Generic AmB—FCZ (ONG) | Diagnosis:—Clinical (lack of specialized laboratories) Treatment:—AmB-FCZ-Echinocandins (not available) | Healthcare collapse and dependence on NGOs leave displaced persons without timely diagnosis and appropriate treatment. |
| Central America Northern Triangle (El Salvador, Guatemala, Honduras) | 1.19‰; 30–76% (regional mean) | Diagnosis:—Local cultures—No BDG, PCR, or MALDI-TOF Treatment:—D-AmB-FCZ-ITZ-Echinocandins (not included in the public service) | Diagnosis:—Clinical and primary cultures—No immunological/molecular testing Treatment:—AmB-FCZ-Echinocandins (not accessible) | Lack of training and equipment in local laboratories; diagnostic delays increase mortality among displaced persons. |
| Colombia | 1.19‰; 30–76% (regional mean) | Diagnosis:—Cultures and stains (48–72 h)-BDG (reference)-MALDI-TOF (large hospitals) Treatment:—D-AmB, L-AmB (limited)-FCZ, ITZ-Echinocandins (expensive, scarce) | Diagnosis: Cultures and stains (reference)—No BDG/MALDI-TOF in primary care Treatment:—AmB-FCZ-Echinocandins (not accessible) | Delays in diagnosis and lack of echinocandins in the public system increase mortality in displaced persons. |
| Venezuela | 1.19‰; 30–76% (regional mean) | Diagnosis:—Cultures (very slow)—No BDG nor MALDI-TOF Treatment:—Generic AmB—FCZ (unstable stock) | Diagnosis:—Predominantly clinical—No immunological/molecular testing Treatment:—AmB-FCZ-Echinocandins (not available) | Chronic shortage of reagents and antifungals aggravates delays in displaced persons. |
| Brazil | 2.49‰; 54% | Diagnosis:—Cultures and stains (48–72 h)—BDG (2–3 reference laboratories)—MALDI-TOF (large hospitals) Treatment:—AmB (including liposomal)—FCZ, VCZ, echinocandins | Diagnosis:—Cultures/stains in urban centers-Little BDG/MALDI-TOF outside of capitals—PCR almost null Treatment:—D-AmB-FCZ-Echinocandins (limited) | Large health centers offer adequate care, but rural refugees and displaced persons are almost completely lacking these options. |
| Peru | 2.04‰; 39.6% (30 days) | Diagnosis:—Cultures (48–72 h)-BDG (2 laboratories in Lima)-MALDI-TOF (1 university center) Treatment:—D-AmB, L-AmB (limited stock)—FCZ, ITZ, echinocandins (irregular stock) | Diagnosis:—Cultures—Outside Lima without BDG/MALDI-TOF/PCR Treatment:—AmB-FCZ-Echinocandins (virtually inaccessible) | Concentration of resources in Lima leaves displaced persons from the interior of the country with almost insurmountable barriers to diagnosis and treatment. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rivas-Pinedo, P.; Motta, J.C.; Gutierrez, J.M.O. Invasive Candidiasis in Contexts of Armed Conflict, High Violence, and Forced Displacement in Latin America and the Caribbean (2005–2025). J. Fungi 2025, 11, 583. https://doi.org/10.3390/jof11080583
Rivas-Pinedo P, Motta JC, Gutierrez JMO. Invasive Candidiasis in Contexts of Armed Conflict, High Violence, and Forced Displacement in Latin America and the Caribbean (2005–2025). Journal of Fungi. 2025; 11(8):583. https://doi.org/10.3390/jof11080583
Chicago/Turabian StyleRivas-Pinedo, Pilar, Juan Camilo Motta, and Jose Millan Onate Gutierrez. 2025. "Invasive Candidiasis in Contexts of Armed Conflict, High Violence, and Forced Displacement in Latin America and the Caribbean (2005–2025)" Journal of Fungi 11, no. 8: 583. https://doi.org/10.3390/jof11080583
APA StyleRivas-Pinedo, P., Motta, J. C., & Gutierrez, J. M. O. (2025). Invasive Candidiasis in Contexts of Armed Conflict, High Violence, and Forced Displacement in Latin America and the Caribbean (2005–2025). Journal of Fungi, 11(8), 583. https://doi.org/10.3390/jof11080583






