Mechanisms and Clinical Implications of Endothelial Dysfunction in Arterial Hypertension
Abstract
1. Introduction
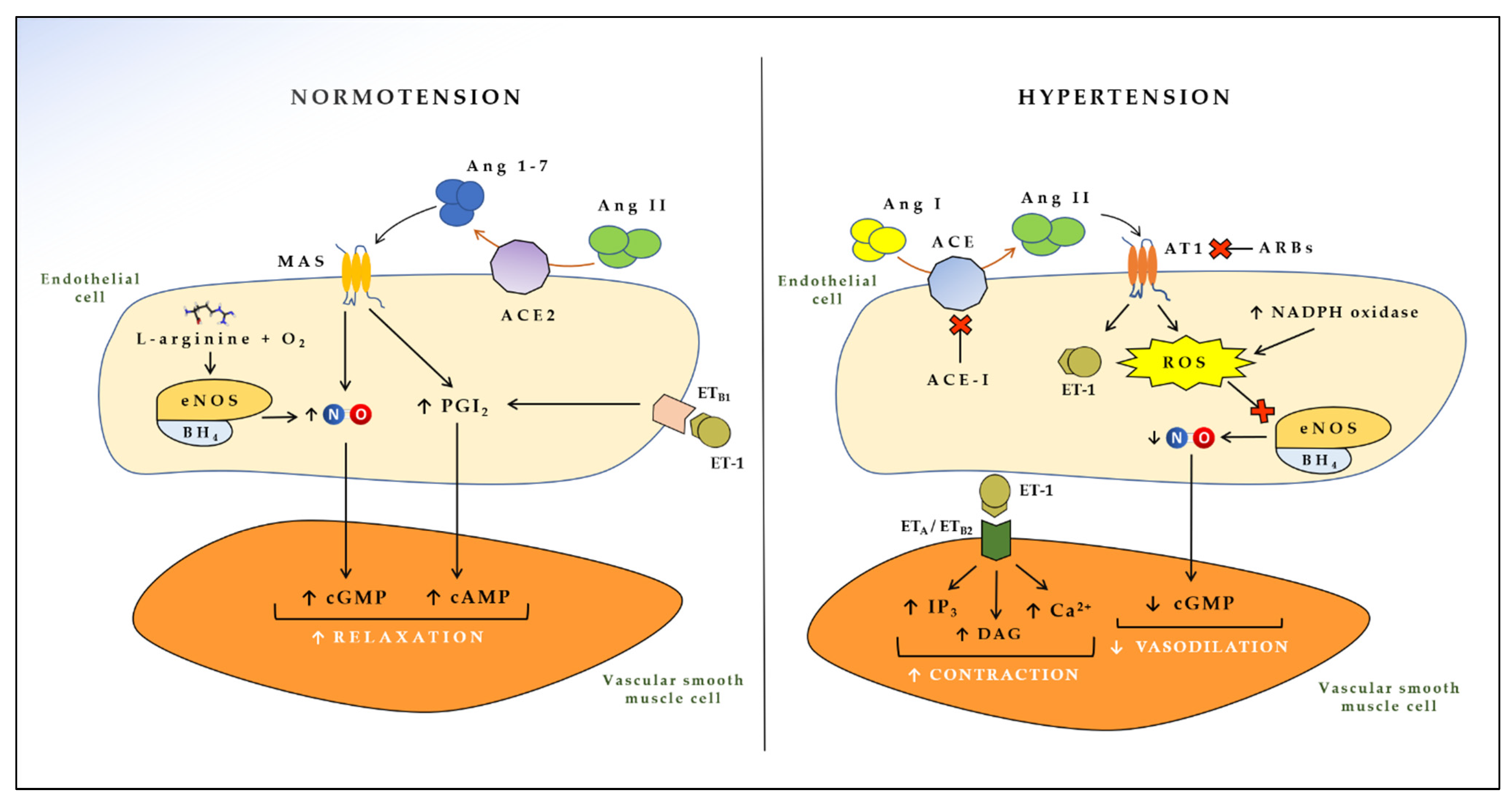
2. Endothelial Cell Mediators in the Pathogenesis of Arterial Hypertension
2.1. Endothelial-Derived Vasoactive Mediators
2.2. Extracellular Vesicles in the Cross-Talk between Endothelial and Smooth Muscle Cells
3. Endothelial Dysfunction, Hypertension, and Cardiovascular Risk
4. Endothelial Function Evaluation
4.1. Laboratory Methods
4.2. Clinical Methods
5. Therapeutic Targets for Endothelial Dysfunction in Hypertension
5.1. ACE Inhibitors and Angiotensin II Receptor Blockers
5.2. Calcium-Channel Blockers
5.3. β-Blockers
5.4. Other Cardiovascular Therapies
5.5. Antioxidants and Nutraceutical Strategies
5.6. Exercise and Rehabilitation
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Oparil, S.; Acelajado, M.C.; Bakris, G.L.; Berlowitz, D.R.; Cifkova, R.; Dominiczak, A.F.; Grassi, G.; Jordan, J.; Poulter, N.R.; Rodgers, A.; et al. Hypertension. Nat. Rev. Dis Prim. 2018, 4, 18014. [Google Scholar] [CrossRef] [PubMed]
- Unger, T.; Borghi, C.; Charchar, F.; Khan, N.A.; Poulter, N.R.; Prabhakaran, D.; Ramirez, A.; Schlaich, M.; Stergiou, G.S.; Tomaszewski, M.; et al. 2020 International Society of Hypertension global hypertension practice guidelines. J. Hypertens 2020, 38, 982–1004. [Google Scholar] [CrossRef]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Konukoglu, D.; Uzun, H. Endothelial dysfunction and hypertension. Adv. Exp. Med. Biol. 2017, 956, 511–540. [Google Scholar] [CrossRef] [PubMed]
- Ambrosino, P.; Grassi, G.; Maniscalco, M. Endothelial dysfunction: From a pathophysiological mechanism to a potential therapeutic target. Biomedicines 2021, 10, 78. [Google Scholar] [CrossRef]
- Gokce, N.; Holbrook, M.; Duffy, S.J.; Demissie, S.; Cupples, L.A.; Biegelsen, E.; Keaney, J.F., Jr.; Loscalzo, J.; Vita, J.A. Effects of race and hypertension on flow-mediated and nitroglycerin-mediated dilation of the brachial artery. Hypertension 2001, 38, 1349–1354. [Google Scholar] [CrossRef]
- Gonzalez, M.A.; Selwyn, A.P. Endothelial function, inflammation, and prognosis in cardiovascular disease. Am. J. Med. 2003, 115 (Suppl. 8A), 99S–106S. [Google Scholar] [CrossRef]
- Furchgott, R.F. Role of endothelium in responses of vascular smooth muscle. Circ. Res. 1983, 53, 557–573. [Google Scholar] [CrossRef]
- Harrison, D.G.; Cai, H. Endothelial control of vasomotion and nitric oxide production. Cardiol. Clin. 2003, 21, 289–302. [Google Scholar] [CrossRef]
- Arnold, W.P.; Mittal, C.K.; Katsuki, S.; Murad, F. Nitric oxide activates guanylate cyclase and increases guanosine 3’:5’-cyclic monophosphate levels in various tissue preparations. Proc. Natl. Acad. Sci. USA 1977, 74, 3203–3207. [Google Scholar] [CrossRef]
- Forstermann, U.; Munzel, T. Endothelial nitric oxide synthase in vascular disease: From marvel to menace. Circulation 2006, 113, 1708–1714. [Google Scholar] [CrossRef] [PubMed]
- da Silva, G.M.; da Silva, M.C.; Nascimento, D.V.G.; Lima Silva, E.M.; Gouvea, F.F.F.; de Franca Lopes, L.G.; Araujo, A.V.; Ferraz Pereira, K.N.; de Queiroz, T.M. Nitric oxide as a central molecule in hypertension: Focus on the vasorelaxant activity of new nitric oxide donors. Biology 2021, 10, 1041. [Google Scholar] [CrossRef] [PubMed]
- Gallo, G.; Volpe, M.; Savoia, C. Endothelial dysfunction in hypertension: Current concepts and clinical implications. Front. Med. (Lausanne) 2021, 8, 798958. [Google Scholar] [CrossRef]
- Brandes, R.P. Endothelial dysfunction and hypertension. Hypertension 2014, 64, 924–928. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Larson, M.G.; Keyes, M.J.; Mitchell, G.F.; Vasan, R.S.; Keaney, J.F., Jr.; Lehman, B.T.; Fan, S.; Osypiuk, E.; Vita, J.A. Clinical correlates and heritability of flow-mediated dilation in the community: The Framingham heart study. Circulation 2004, 109, 613–619. [Google Scholar] [CrossRef]
- Ambrosino, P.; Lupoli, R.; Iervolino, S.; De Felice, A.; Pappone, N.; Storino, A.; Di Minno, M.N.D. Clinical assessment of endothelial function in patients with chronic obstructive pulmonary disease: A systematic review with meta-analysis. Intern. Emerg. Med. 2017, 12, 877–885. [Google Scholar] [CrossRef]
- Karbach, S.; Wenzel, P.; Waisman, A.; Munzel, T.; Daiber, A. eNOS uncoupling in cardiovascular diseases—The role of oxidative stress and inflammation. Curr. Pharm. Des. 2014, 20, 3579–3594. [Google Scholar] [CrossRef]
- Korsager Larsen, M.; Matchkov, V.V. Hypertension and physical exercise: The role of oxidative stress. Medicina (Kaunas) 2016, 52, 19–27. [Google Scholar] [CrossRef]
- Sedeek, M.; Hebert, R.L.; Kennedy, C.R.; Burns, K.D.; Touyz, R.M. Molecular mechanisms of hypertension: Role of Nox family NADPH oxidases. Curr. Opin. Nephrol. Hypertens. 2009, 18, 122–127. [Google Scholar] [CrossRef]
- Griendling, K.K.; Camargo, L.L.; Rios, F.J.; Alves-Lopes, R.; Montezano, A.C.; Touyz, R.M. Oxidative Stress and Hypertension. Circ. Res. 2021, 128, 993–1020. [Google Scholar] [CrossRef]
- Shanahan, C.M.; Furmanik, M. Endoplasmic reticulum stress in arterial smooth muscle cells: A novel regulator of vascular disease. Curr. Cardiol. Rev. 2017, 13, 94–105. [Google Scholar] [CrossRef] [PubMed]
- Ochoa, C.D.; Wu, R.F.; Terada, L.S. ROS signaling and ER stress in cardiovascular disease. Mol. Asp. Med. 2018, 63, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.Y.; Lee, T.H. Antioxidant enzymes as redox-based biomarkers: A brief review. BMB Rep. 2015, 48, 200–208. [Google Scholar] [CrossRef]
- Montezano, A.C.; Dulak-Lis, M.; Tsiropoulou, S.; Harvey, A.; Briones, A.M.; Touyz, R.M. Oxidative stress and human hypertension: Vascular mechanisms, biomarkers, and novel therapies. Can. J. Cardiol. 2015, 31, 631–641. [Google Scholar] [CrossRef]
- Suzuki, H.; Chen, G.; Yamamoto, Y. Endothelium-derived hyperpolarizing factor (EDHF). Jpn. Circ. J. 1992, 56, 170–174. [Google Scholar] [CrossRef]
- Oyama, J.; Node, K. Endothelium-derived hyperpolarizing factor and hypertension. Hypertens. Res. 2013, 36, 852–853. [Google Scholar] [CrossRef]
- Kelly, J.J.; Whitworth, J.A. Endothelin-1 as a mediator in cardiovascular disease. Clin. Exp. Pharmacol. Physiol. 1999, 26, 158–161. [Google Scholar] [CrossRef]
- Kostov, K. The causal relationship between endothelin-1 and hypertension: Focusing on endothelial dysfunction, arterial stiffness, vascular remodeling, and blood pressure regulation. Life 2021, 11, 986. [Google Scholar] [CrossRef]
- Adam, L.P.; Milio, L.; Brengle, B.; Hathaway, D.R. Myosin light chain and caldesmon phosphorylation in arterial muscle stimulated with endothelin-1. J. Mol. Cell. Cardiol. 1990, 22, 1017–1023. [Google Scholar] [CrossRef]
- Chen, M.; Lin, Y.Q.; Xie, S.L.; Wang, J.F. Mitogen-activated protein kinase in endothelin-1-induced cardiac differentiation of mouse embryonic stem cells. J. Cell. Biochem. 2010, 111, 1619–1628. [Google Scholar] [CrossRef]
- Rafnsson, A.; Matic, L.P.; Lengquist, M.; Mahdi, A.; Shemyakin, A.; Paulsson-Berne, G.; Hansson, G.K.; Gabrielsen, A.; Hedin, U.; Yang, J.; et al. Endothelin-1 increases expression and activity of arginase 2 via ETB receptors and is co-expressed with arginase 2 in human atherosclerotic plaques. Atherosclerosis 2020, 292, 215–223. [Google Scholar] [CrossRef]
- Davenport, A.P.; Hyndman, K.A.; Dhaun, N.; Southan, C.; Kohan, D.E.; Pollock, J.S.; Pollock, D.M.; Webb, D.J.; Maguire, J.J. Endothelin. Pharmacol. Rev. 2016, 68, 357–418. [Google Scholar] [CrossRef]
- Kiowski, W.; Luscher, T.F.; Linder, L.; Buhler, F.R. Endothelin-1-induced vasoconstriction in humans. Reversal by calcium channel blockade but not by nitrovasodilators or endothelium-derived relaxing factor. Circulation 1991, 83, 469–475. [Google Scholar] [CrossRef]
- Shreenivas, S.; Oparil, S. The role of endothelin-1 in human hypertension. Clin. Hemorheol. Microcirc. 2007, 37, 157–178. [Google Scholar]
- Schiffrin, E.L. Role of endothelin-1 in hypertension and vascular disease. Am. J. Hypertens. 2001, 14, 83S–89S. [Google Scholar] [CrossRef]
- Schiffrin, E.L. Vascular remodeling in hypertension: Mechanisms and treatment. Hypertension 2012, 59, 367–374. [Google Scholar] [CrossRef]
- Mulvany, M.J. Vascular remodelling in hypertension. Eur. Hear. J. 1993, 14 (Suppl. C), 2–4. [Google Scholar] [CrossRef]
- Idris-Khodja, N.; Ouerd, S.; Trindade, M.; Gornitsky, J.; Rehman, A.; Barhoumi, T.; Offermanns, S.; Gonzalez, F.J.; Neves, M.F.; Paradis, P.; et al. Vascular smooth muscle cell peroxisome proliferator-activated receptor gamma protects against endothelin-1-induced oxidative stress and inflammation. J. Hypertens. 2017, 35, 1390–1401. [Google Scholar] [CrossRef]
- Wallace, K.B.; Bailie, M.D.; Hook, J.B. Development of angiotensin-converting enzyme in fetal rat lungs. Am. J. Physiol. 1979, 236, R57–R60. [Google Scholar] [CrossRef]
- Khurana, V.; Goswami, B. Angiotensin converting enzyme (ACE). Clin. Chim. Acta 2022, 524, 113–122. [Google Scholar] [CrossRef]
- Navar, L.G.; Harrison-Bernard, L.M.; Imig, J.D.; Cervenka, L.; Mitchell, K.D. Renal responses to AT1 receptor blockade. Am. J. Hypertens. 2000, 13, 45S–54S. [Google Scholar] [CrossRef][Green Version]
- Thomas, W.G. Regulation of angiotensin II type 1 (AT1) receptor function. Regul. Pept. 1999, 79, 9–23. [Google Scholar] [CrossRef]
- Nickenig, G.; Bohm, M. Interaction between insulin and AT1 receptor. Relevance for hypertension and arteriosclerosis. Basic Res. Cardiol. 1998, 93 (Suppl. 2), 135–139. [Google Scholar] [CrossRef]
- Carey, R.M. Update on the role of the AT2 receptor. Curr. Opin. Nephrol. Hypertens. 2005, 14, 67–71. [Google Scholar] [CrossRef]
- Siragy, H.M. The role of the AT2 receptor in hypertension. Am. J. Hypertens. 2000, 13, 62S–67S. [Google Scholar] [CrossRef]
- Scialo, F.; Vitale, M.; Daniele, A.; Nigro, E.; Perrotta, F.; Gelzo, M.; Iadevaia, C.; Cerqua, F.S.; Costigliola, A.; Allocca, V.; et al. SARS-CoV-2: One year in the pandemic. What have we learned, the new vaccine era and the threat of SARS-CoV-2 variants. Biomedicines 2021, 9, 611. [Google Scholar] [CrossRef]
- Scialo, F.; Daniele, A.; Amato, F.; Pastore, L.; Matera, M.G.; Cazzola, M.; Castaldo, G.; Bianco, A. ACE2: The major cell entry receptor for SARS-CoV-2. Lung 2020, 198, 867–877. [Google Scholar] [CrossRef]
- Perrotta, F.; Matera, M.G.; Cazzola, M.; Bianco, A. Severe respiratory SARS-CoV2 infection: Does ACE2 receptor matter? Respir. Med. 2020, 168, 105996. [Google Scholar] [CrossRef]
- van Niel, G.; D’Angelo, G.; Raposo, G. Shedding light on the cell biology of extracellular vesicles. Nat. Rev. Mol. Cell Biol 2018, 19, 213–228. [Google Scholar] [CrossRef]
- Raposo, G.; Stoorvogel, W. Extracellular vesicles: Exosomes, microvesicles, and friends. J. Cell Biol. 2013, 200, 373–383. [Google Scholar] [CrossRef]
- Jeppesen, D.K.; Fenix, A.M.; Franklin, J.L.; Higginbotham, J.N.; Zhang, Q.; Zimmerman, L.J.; Liebler, D.C.; Ping, J.; Liu, Q.; Evans, R.; et al. Reassessment of exosome composition. Cell 2019, 177, 428–445.e18. [Google Scholar] [CrossRef]
- Santavanond, J.P.; Rutter, S.F.; Atkin-Smith, G.K.; Poon, I.K.H. Apoptotic bodies: Mechanism of formation, isolation and functional relevance. Subcell. Biochem. 2021, 97, 61–88. [Google Scholar] [CrossRef]
- Mathiesen, A.; Hamilton, T.; Carter, N.; Brown, M.; McPheat, W.; Dobrian, A. Endothelial extracellular vesicles: From keepers of health to messengers of disease. Int. J. Mol. Sci. 2021, 22, 4640. [Google Scholar] [CrossRef]
- Liu, Z.Z.; Jose, P.A.; Yang, J.; Zeng, C. Importance of extracellular vesicles in hypertension. Exp. Biol. Med. (Maywood) 2021, 246, 342–353. [Google Scholar] [CrossRef]
- Good, M.E.; Musante, L.; La Salvia, S.; Howell, N.L.; Carey, R.M.; Le, T.H.; Isakson, B.E.; Erdbrugger, U. Circulating extracellular vesicles in normotension restrain vasodilation in resistance arteries. Hypertension 2020, 75, 218–228. [Google Scholar] [CrossRef]
- Otani, K.; Yokoya, M.; Kodama, T.; Hori, K.; Matsumoto, K.; Okada, M.; Yamawaki, H. Plasma exosomes regulate systemic blood pressure in rats. Biochem. Biophys. Res. Commun. 2018, 503, 776–783. [Google Scholar] [CrossRef]
- Sansone, R.; Baaken, M.; Horn, P.; Schuler, D.; Westenfeld, R.; Amabile, N.; Kelm, M.; Heiss, C. Endothelial microparticles and vascular parameters in subjects with and without arterial hypertension and coronary artery disease. Data Br. 2018, 19, 495–500. [Google Scholar] [CrossRef]
- Sun, Y.; Wang, Q.; Yang, G.; Lin, C.; Zhang, Y.; Yang, P. Weight and prognosis for influenza A(H1N1)pdm09 infection during the pandemic period between 2009 and 2011: A systematic review of observational studies with meta-analysis. Infect. Dis. (Lond) 2016, 48, 813–822. [Google Scholar] [CrossRef]
- Perez-Hernandez, J.; Riffo-Campos, A.L.; Ortega, A.; Martinez-Arroyo, O.; Perez-Gil, D.; Olivares, D.; Solaz, E.; Martinez, F.; Martinez-Hervas, S.; Chaves, F.J.; et al. Urinary- and plasma-derived exosomes reveal a distinct MicroRNA signature associated with albuminuria in hypertension. Hypertension 2021, 77, 960–971. [Google Scholar] [CrossRef]
- Wang, C.; Xing, C.; Li, Z.; Liu, Y.; Li, Q.; Wang, Y.; Hu, J.; Yuan, L.; Yang, G. Bioinspired therapeutic platform based on extracellular vesicles for prevention of arterial wall remodeling in hypertension. Bioact. Mater. 2022, 8, 494–504. [Google Scholar] [CrossRef]
- Quick, S.; Moss, J.; Rajani, R.M.; Williams, A. A vessel for change: Endothelial dysfunction in cerebral small vessel disease. Trends Neurosci. 2021, 44, 289–305. [Google Scholar] [CrossRef] [PubMed]
- Berry, C.; Sidik, N.; Pereira, A.C.; Ford, T.J.; Touyz, R.M.; Kaski, J.C.; Hainsworth, A.H. Small-Vessel disease in the heart and brain: Current knowledge, unmet therapeutic need, and future directions. J. Am. Hear. Assoc. 2019, 8, e011104. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Brown, J.M.; Bajaj, N.S.; Chandra, A.; Divakaran, S.; Weber, B.; Bibbo, C.F.; Hainer, J.; Taqueti, V.R.; Dorbala, S.; et al. Hypertensive coronary microvascular dysfunction: A subclinical marker of end organ damage and heart failure. Eur Hear. J. 2020, 41, 2366–2375. [Google Scholar] [CrossRef] [PubMed]
- Toya, T.; Sara, J.D.; Scharf, E.L.; Ahmad, A.; Nardi, V.; Ozcan, I.; Lerman, L.O.; Lerman, A. Impact of peripheral microvascular endothelial dysfunction on white matter hyperintensity. J. Am. Hear. Assoc. 2021, 10, e021066. [Google Scholar] [CrossRef] [PubMed]
- Toya, T.; Sara, J.D.; Ahmad, A.; Nardi, V.; Taher, R.; Lerman, L.O.; Lerman, A. Incremental prognostic impact of peripheral microvascular endothelial dysfunction on the development of ischemic stroke. J. Am. Hear. Assoc. 2020, 9, e015703. [Google Scholar] [CrossRef]
- Nezu, T.; Hosomi, N.; Aoki, S.; Kubo, S.; Araki, M.; Mukai, T.; Takahashi, T.; Maruyama, H.; Higashi, Y.; Matsumoto, M. Endothelial dysfunction is associated with the severity of cerebral small vessel disease. Hypertens. Res. 2015, 38, 291–297. [Google Scholar] [CrossRef]
- Serne, E.H.; de Jongh, R.T.; Eringa, E.C.; RG, I.J.; Stehouwer, C.D. Microvascular dysfunction: A potential pathophysiological role in the metabolic syndrome. Hypertension 2007, 50, 204–211. [Google Scholar] [CrossRef]
- Quyyumi, A.A.; Patel, R.S. Endothelial dysfunction and hypertension: Cause or effect? Hypertension 2010, 55, 1092–1094. [Google Scholar] [CrossRef]
- Schachinger, V.; Britten, M.B.; Zeiher, A.M. Prognostic impact of coronary vasodilator dysfunction on adverse long-term outcome of coronary heart disease. Circulation 2000, 101, 1899–1906. [Google Scholar] [CrossRef]
- Yeboah, J.; Folsom, A.R.; Burke, G.L.; Johnson, C.; Polak, J.F.; Post, W.; Lima, J.A.; Crouse, J.R.; Herrington, D.M. Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: The multi-ethnic study of atherosclerosis. Circulation 2009, 120, 502–509. [Google Scholar] [CrossRef]
- Gokce, N.; Keaney, J.F., Jr.; Hunter, L.M.; Watkins, M.T.; Menzoian, J.O.; Vita, J.A. Risk stratification for postoperative cardiovascular events via noninvasive assessment of endothelial function: A prospective study. Circulation 2002, 105, 1567–1572. [Google Scholar] [CrossRef] [PubMed]
- Shimbo, D.; Muntner, P.; Mann, D.; Viera, A.J.; Homma, S.; Polak, J.F.; Barr, R.G.; Herrington, D.; Shea, S. Endothelial dysfunction and the risk of hypertension: The multi-ethnic study of atherosclerosis. Hypertension 2010, 55, 1210–1216. [Google Scholar] [CrossRef] [PubMed]
- Sciacqua, A.; Scozzafava, A.; Pujia, A.; Maio, R.; Borrello, F.; Andreozzi, F.; Vatrano, M.; Cassano, S.; Perticone, M.; Sesti, G.; et al. Interaction between vascular dysfunction and cardiac mass increases the risk of cardiovascular outcomes in essential hypertension. Eur. Hear. J. 2005, 26, 921–927. [Google Scholar] [CrossRef] [PubMed]
- van Oort, S.; Beulens, J.W.J.; van Ballegooijen, A.J.; Grobbee, D.E.; Larsson, S.C. Association of cardiovascular risk factors and lifestyle behaviors with hypertension: A mendelian randomization study. Hypertension 2020, 76, 1971–1979. [Google Scholar] [CrossRef]
- Sander, M.; Chavoshan, B.; Victor, R.G. A large blood pressure-raising effect of nitric oxide synthase inhibition in humans. Hypertension 1999, 33, 937–942. [Google Scholar] [CrossRef]
- Juonala, M.; Viikari, J.S.; Ronnemaa, T.; Helenius, H.; Taittonen, L.; Raitakari, O.T. Elevated blood pressure in adolescent boys predicts endothelial dysfunction: The cardiovascular risk in young Finns study. Hypertension 2006, 48, 424–430. [Google Scholar] [CrossRef]
- Rossi, R.; Chiurlia, E.; Nuzzo, A.; Cioni, E.; Origliani, G.; Modena, M.G. Flow-mediated vasodilation and the risk of developing hypertension in healthy postmenopausal women. J. Am. Coll. Cardiol 2004, 44, 1636–1640. [Google Scholar] [CrossRef]
- Salmito, F.T.; de Oliveira Neves, F.M.; Meneses, G.C.; de Almeida Leitao, R.; Martins, A.M.; Liborio, A.B. Glycocalyx injury in adults with nephrotic syndrome: Association with endothelial function. Clin. Chim. Acta 2015, 447, 55–58. [Google Scholar] [CrossRef]
- Sabatier, F.; Camoin-Jau, L.; Anfosso, F.; Sampol, J.; Dignat-George, F. Circulating endothelial cells, microparticles and progenitors: Key players towards the definition of vascular competence. J. Cell Mol. Med. 2009, 13, 454–471. [Google Scholar] [CrossRef]
- Klonizakis, M.; Manning, G.; Donnelly, R. Assessment of lower limb microcirculation: Exploring the reproducibility and clinical application of laser Doppler techniques. Ski. Pharm. Physiol 2011, 24, 136–143. [Google Scholar] [CrossRef]
- Rubinshtein, R.; Kuvin, J.T.; Soffler, M.; Lennon, R.J.; Lavi, S.; Nelson, R.E.; Pumper, G.M.; Lerman, L.O.; Lerman, A. Assessment of endothelial function by non-invasive peripheral arterial tonometry predicts late cardiovascular adverse events. Eur. Hear. J. 2010, 31, 1142–1148. [Google Scholar] [CrossRef]
- Flammer, A.J.; Anderson, T.; Celermajer, D.S.; Creager, M.A.; Deanfield, J.; Ganz, P.; Hamburg, N.M.; Luscher, T.F.; Shechter, M.; Taddei, S.; et al. The assessment of endothelial function: From research into clinical practice. Circulation 2012, 126, 753–767. [Google Scholar] [CrossRef]
- Corretti, M.C.; Anderson, T.J.; Benjamin, E.J.; Celermajer, D.; Charbonneau, F.; Creager, M.A.; Deanfield, J.; Drexler, H.; Gerhard-Herman, M.; Herrington, D.; et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: A report of the International Brachial Artery Reactivity Task Force. J. Am. Coll. Cardiol. 2002, 39, 257–265. [Google Scholar] [CrossRef]
- Holder, S.M.; Bruno, R.M.; Shkredova, D.A.; Dawson, E.A.; Jones, H.; Hopkins, N.D.; Hopman, M.T.E.; Bailey, T.G.; Coombes, J.S.; Askew, C.D.; et al. Reference intervals for brachial artery flow-mediated dilation and the relation with cardiovascular risk factors. Hypertension 2021, 77, 1469–1480. [Google Scholar] [CrossRef]
- Greyling, A.; van Mil, A.C.; Zock, P.L.; Green, D.J.; Ghiadoni, L.; Thijssen, D.H.; TIFN International Working Group on Flow Mediated Dilation. Adherence to guidelines strongly improves reproducibility of brachial artery flow-mediated dilation. Atherosclerosis 2016, 248, 196–202. [Google Scholar] [CrossRef]
- Daiber, A.; Steven, S.; Weber, A.; Shuvaev, V.V.; Muzykantov, V.R.; Laher, I.; Li, H.; Lamas, S.; Munzel, T. Targeting vascular (endothelial) dysfunction. Br. J. Pharmacol. 2017, 174, 1591–1619. [Google Scholar] [CrossRef]
- Nagele, M.P.; Haubner, B.; Tanner, F.C.; Ruschitzka, F.; Flammer, A.J. Endothelial dysfunction in COVID-19: Current findings and therapeutic implications. Atherosclerosis 2020, 314, 58–62. [Google Scholar] [CrossRef]
- Yong, J.; Tian, J.; Yang, X.; Xing, H.; He, Y.; Song, X. Effects of oral drugs on coronary microvascular function in patients without significant stenosis of epicardial coronary arteries: A systematic review and meta-analysis of coronary flow reserve. Front. Cardiovasc. Med. 2020, 7, 580419. [Google Scholar] [CrossRef]
- Bakris, G.; Ali, W.; Parati, G. ACC/AHA versus ESC/ESH on hypertension guidelines: JACC guideline comparison. J. Am. Coll. Cardiol. 2019, 73, 3018–3026. [Google Scholar] [CrossRef]
- Juggi, J.S.; Koenig-Berard, E.; Van Gilst, W.H. Cardioprotection by angiotensin-converting enzyme (ACE) inhibitors. Can. J. Cardiol. 1993, 9, 336–352. [Google Scholar]
- Matoba, S.; Tatsumi, T.; Keira, N.; Kawahara, A.; Akashi, K.; Kobara, M.; Asayama, J.; Nakagawa, M. Cardioprotective effect of angiotensin-converting enzyme inhibition against hypoxia/reoxygenation injury in cultured rat cardiac myocytes. Circulation 1999, 99, 817–822. [Google Scholar] [CrossRef]
- Shahin, Y.; Khan, J.A.; Samuel, N.; Chetter, I. Angiotensin converting enzyme inhibitors effect on endothelial dysfunction: A meta-analysis of randomised controlled trials. Atherosclerosis 2011, 216, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Napoleone, E.; Di Santo, A.; Camera, M.; Tremoli, E.; Lorenzet, R. Angiotensin-converting enzyme inhibitors downregulate tissue factor synthesis in monocytes. Circ. Res. 2000, 86, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.; Channon, K.M.; Antoniades, C. Therapeutic strategies targeting endothelial function in humans: Clinical implications. Curr. Vasc. Pharmacol. 2012, 10, 77–93. [Google Scholar] [CrossRef] [PubMed]
- Erdos, E.G.; Tan, F.; Skidgel, R.A. Angiotensin I-converting enzyme inhibitors are allosteric enhancers of kinin B1 and B2 receptor function. Hypertension 2010, 55, 214–220. [Google Scholar] [CrossRef]
- Li, K.; Zemmrich, C.; Bramlage, P.; Persson, A.B.; Sacirovic, M.; Ritter, O.; Buschmann, E.; Buschmann, I.; Hillmeister, P. Effect of ACEI and ARB treatment on nitric oxide-dependent endothelial function. Vasa 2021, 50, 413–422. [Google Scholar] [CrossRef]
- Radenkovic, M.; Stojanovic, M.; Prostran, M. Calcium channel blockers in restoration of endothelial function: Systematic review and meta-analysis of randomized controlled trials. Curr. Med. Chem. 2019, 26, 5579–5595. [Google Scholar] [CrossRef]
- Mancini, G.B.; Henry, G.C.; Macaya, C.; O’Neill, B.J.; Pucillo, A.L.; Carere, R.G.; Wargovich, T.J.; Mudra, H.; Luscher, T.F.; Klibaner, M.I.; et al. Angiotensin-converting enzyme inhibition with quinapril improves endothelial vasomotor dysfunction in patients with coronary artery disease. The TREND (trial on reversing endothelial dysfunction) study. Circulation 1996, 94, 258–265. [Google Scholar] [CrossRef]
- Chiesa, S.T.; Marcovecchio, M.L.; Benitez-Aguirre, P.; Cameron, F.J.; Craig, M.E.; Couper, J.J.; Davis, E.A.; Dalton, R.N.; Daneman, D.; Donaghue, K.C.; et al. Vascular effects of ACE (angiotensin-converting enzyme) inhibitors and statins in adolescents with type 1 diabetes. Hypertension 2020, 76, 1734–1743. [Google Scholar] [CrossRef]
- Schmieder, R.E.; Delles, C.; Mimran, A.; Fauvel, J.P.; Ruilope, L.M. Impact of telmisartan versus ramipril on renal endothelial function in patients with hypertension and type 2 diabetes. Diabetes Care 2007, 30, 1351–1356. [Google Scholar] [CrossRef]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L., Jr.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T., Jr.; et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA 2003, 289, 2560–2572. [Google Scholar] [CrossRef] [PubMed]
- Mohler, E.R., 3rd; Herrington, D.; Ouyang, P.; Mangano, C.; Ritter, S.; Davis, P.; Purkayastha, D.; Gatlin, M.; Vogel, R.A.; Investigators, E. A randomized, double-blind trial comparing the effects of amlodipine besylate/benazepril HCl vs amlodipine on endothelial function and blood pressure. J. Clin. Hypertens. (Greenwich) 2006, 8, 692–698. [Google Scholar] [CrossRef] [PubMed]
- Frielingsdorf, J.; Seiler, C.; Kaufmann, P.; Vassalli, G.; Suter, T.; Hess, O.M. Normalization of abnormal coronary vasomotion by calcium antagonists in patients with hypertension. Circulation 1996, 93, 1380–1387. [Google Scholar] [CrossRef] [PubMed]
- Yasu, T.; Kobayashi, M.; Mutoh, A.; Yamakawa, K.; Momomura, S.; Ueda, S. Dihydropyridine calcium channel blockers inhibit non-esterified-fatty-acid-induced endothelial and rheological dysfunction. Clin. Sci. 2013, 125, 247–255. [Google Scholar] [CrossRef]
- Napoli, C.; Salomone, S.; Godfraind, T.; Palinski, W.; Capuzzi, D.M.; Palumbo, G.; D’Armiento, F.P.; Donzelli, R.; de Nigris, F.; Capizzi, R.L.; et al. 1,4-Dihydropyridine calcium channel blockers inhibit plasma and LDL oxidation and formation of oxidation-specific epitopes in the arterial wall and prolong survival in stroke-prone spontaneously hypertensive rats. Stroke 1999, 30, 1907–1915. [Google Scholar] [CrossRef]
- Ruschitzka, F.T.; Noll, G.; Luscher, T.F. Combination of ACE inhibitors and calcium antagonists: A logical approach. J. Cardiovasc. Pharmacol. 1998, 31 (Suppl. 2), S5–S16. [Google Scholar] [CrossRef]
- Tiryaki, O.; Usalan, C.; Buyukhatipoglu, H.; Sayiner, Z.A.; Kilisli, H. Effects of lisinopril, irbesartan, and amlodipine on the thrombogenic variables in the early and late stages of the treatment in hypertensive patients. Clin. Exp. Hypertens. 2012, 34, 145–152. [Google Scholar] [CrossRef]
- Wiysonge, C.S.; Bradley, H.A.; Volmink, J.; Mayosi, B.M.; Opie, L.H. Beta-blockers for hypertension. Cochrane Database Syst. Rev. 2017, 2017, CD002003. [Google Scholar] [CrossRef]
- Ong, P.; Athanasiadis, A.; Sechtem, U. Pharmacotherapy for coronary microvascular dysfunction. Eur. Hear. J.-Cardiovasc. Pharm. 2015, 1, 65–71. [Google Scholar] [CrossRef]
- Gomes, A.; Costa, D.; Lima, J.L.; Fernandes, E. Antioxidant activity of beta-blockers: An effect mediated by scavenging reactive oxygen and nitrogen species? Bioorganic Med. Chem. 2006, 14, 4568–4577. [Google Scholar] [CrossRef]
- Pedersen, M.E.; Cockcroft, J.R. The vasodilatory beta-blockers. Curr. Hypertens. Rep. 2007, 9, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Kalinowski, L.; Dobrucki, L.W.; Szczepanska-Konkel, M.; Jankowski, M.; Martyniec, L.; Angielski, S.; Malinski, T. Third-generation beta-blockers stimulate nitric oxide release from endothelial cells through ATP efflux: A novel mechanism for antihypertensive action. Circulation 2003, 107, 2747–2752. [Google Scholar] [CrossRef]
- Zepeda, R.J.; Castillo, R.; Rodrigo, R.; Prieto, J.C.; Aramburu, I.; Brugere, S.; Galdames, K.; Noriega, V.; Miranda, H.F. Effect of carvedilol and nebivolol on oxidative stress-related parameters and endothelial function in patients with essential hypertension. Basic Clin. Pharmacol. Toxicol. 2012, 111, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z. The metabolic syndrome. Lancet 2005, 365, 1415–1428. [Google Scholar] [CrossRef]
- Antoniades, C.; Bakogiannis, C.; Leeson, P.; Guzik, T.J.; Zhang, M.H.; Tousoulis, D.; Antonopoulos, A.S.; Demosthenous, M.; Marinou, K.; Hale, A.; et al. Rapid, direct effects of statin treatment on arterial redox state and nitric oxide bioavailability in human atherosclerosis via tetrahydrobiopterin-mediated endothelial nitric oxide synthase coupling. Circulation 2011, 124, 335–345. [Google Scholar] [CrossRef]
- Liu, A.; Wu, Q.; Guo, J.; Ares, I.; Rodriguez, J.L.; Martinez-Larranaga, M.R.; Yuan, Z.; Anadon, A.; Wang, X.; Martinez, M.A. Statins: Adverse reactions, oxidative stress and metabolic interactions. Pharmacol. Ther. 2019, 195, 54–84. [Google Scholar] [CrossRef] [PubMed]
- Di Minno, M.N.; Ambrosino, P.; Peluso, R.; Di Minno, A.; Lupoli, R.; Dentali, F.; Ca, R.S.G. Lipid profile changes in patients with rheumatic diseases receiving a treatment with TNF-alpha blockers: A meta-analysis of prospective studies. Ann. Med. 2014, 46, 73–83. [Google Scholar] [CrossRef]
- Martinez-Gonzalez, J.; Badimon, L. Influence of statin use on endothelial function: From bench to clinics. Curr. Pharm. Des. 2007, 13, 1771–1786. [Google Scholar] [CrossRef]
- Takagi, H.; Yamamoto, H.; Iwata, K.; Goto, S.N.; Umemoto, T. Low-density lipoprotein-independent improvement of flow-mediated dilatation with atorvastatin: A meta-analysis and meta-regression of randomized controlled trials. Int. J. Cardiol. 2012, 158, 285–289. [Google Scholar] [CrossRef]
- Zinellu, A.; Mangoni, A.A. Systematic review and meta-analysis of the effect of statins on circulating E-selectin, L-selectin, and P-selectin. Biomedicines 2021, 9, 1707. [Google Scholar] [CrossRef]
- Zinellu, A.; Mangoni, A.A. An updated systematic review and meta-analysis of the effect of statins on asymmetric dimethylarginine. Nitric Oxide 2022, 120, 26–37. [Google Scholar] [CrossRef]
- Maruhashi, T.; Higashi, Y. Pathophysiological association between diabetes mellitus and endothelial dysfunction. Antioxidants 2021, 10, 1306. [Google Scholar] [CrossRef] [PubMed]
- Stojanovic, M.; Prostran, M.; Radenkovic, M. Thiazolidinediones improve flow-mediated dilation: A meta-analysis of randomized clinical trials. Eur. J. Clin. Pharmacol. 2016, 72, 385–398. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, S.; Jinnouchi, H.; Kurinami, N.; Hieshima, K.; Yoshida, A.; Jinnouchi, K.; Nishimura, H.; Suzuki, T.; Miyamoto, F.; Kajiwara, K.; et al. The SGLT2 inhibitor dapagliflozin significantly improves the peripheral microvascular endothelial function in patients with uncontrolled type 2 diabetes mellitus. Intern. Med. 2018, 57, 2147–2156. [Google Scholar] [CrossRef] [PubMed]
- Nafisa, A.; Gray, S.G.; Cao, Y.; Wang, T.; Xu, S.; Wattoo, F.H.; Barras, M.; Cohen, N.; Kamato, D.; Little, P.J. Endothelial function and dysfunction: Impact of metformin. Pharmacol. Ther. 2018, 192, 150–162. [Google Scholar] [CrossRef]
- Androulakis, E.; Norrington, K.; Bakogiannis, C.; Lioudaki, E.; Siasos, G.; Tousoulis, D. The impact of antiplatelet treatment on endothelial function. Curr. Pharm. Des. 2016, 22, 4512–4518. [Google Scholar] [CrossRef]
- Lee, S.J.; Lee, J.S.; Choi, M.H.; Lee, S.E.; Shin, D.H.; Hong, J.M. Cilostazol improves endothelial function in acute cerebral ischemia patients: A double-blind placebo controlled trial with flow-mediated dilation technique. BMC Neurol. 2017, 17, 169. [Google Scholar] [CrossRef]
- Shi, M.Q.; Su, F.F.; Xu, X.; Liu, X.T.; Wang, H.T.; Zhang, W.; Li, X.; Lian, C.; Zheng, Q.S.; Feng, Z.C. Cilostazol suppresses angiotensin II-induced apoptosis in endothelial cells. Mol. Med. Rep. 2016, 13, 2597–2605. [Google Scholar] [CrossRef]
- Chao, T.H.; Chen, I.C.; Lee, C.H.; Chen, J.Y.; Tsai, W.C.; Li, Y.H.; Tseng, S.Y.; Tsai, L.M.; Tseng, W.K. Cilostazol enhances mobilization of circulating endothelial progenitor cells and improves endothelium-dependent function in patients at high risk of cardiovascular disease. Angiology 2016, 67, 638–646. [Google Scholar] [CrossRef]
- Suzuki, K.; Uchida, K.; Nakanishi, N.; Hattori, Y. Cilostazol activates AMP-activated protein kinase and restores endothelial function in diabetes. Am. J. Hypertens. 2008, 21, 451–457. [Google Scholar] [CrossRef]
- Warnholtz, A.; Mollnau, H.; Oelze, M.; Wendt, M.; Munzel, T. Antioxidants and endothelial dysfunction in hyperlipidemia. Curr. Hypertens. Rep. 2001, 3, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Dodd, S.; Dean, O.; Copolov, D.L.; Malhi, G.S.; Berk, M. N-acetylcysteine for antioxidant therapy: Pharmacology and clinical utility. Expert Opin. Biol. Ther. 2008, 8, 1955–1962. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Miao, N.J.; Xu, J.L.; Gan, X.X.; Xu, D.; Zhou, L.; Xue, H.; Zhang, W.; Lu, L.M. N-acetylcysteine alleviates angiotensin II-mediated renal fibrosis in mouse obstructed kidneys. Acta Pharmacol. Sin. 2016, 37, 637–644. [Google Scholar] [CrossRef]
- Ruiz, F.J.; Salom, M.G.; Ingles, A.C.; Quesada, T.; Vicente, E.; Carbonell, L.F. N-acetyl-L-cysteine potentiates depressor response to captopril and enalaprilat in SHRs. Am. J. Physiol. 1994, 267, R767–R772. [Google Scholar] [CrossRef] [PubMed]
- Fang, X.; Liu, L.; Zhou, S.; Zhu, M.; Wang, B. Nacetylcysteine inhibits atherosclerosis by correcting glutathionedependent methylglyoxal elimination and dicarbonyl/oxidative stress in the aorta of diabetic mice. Mol. Med. Rep. 2021, 23, 291. [Google Scholar] [CrossRef]
- Sahin, G.; Yalcin, A.U.; Akcar, N. Effect of N-acetylcysteine on endothelial dysfunction in dialysis patients. Blood Purif. 2007, 25, 309–315. [Google Scholar] [CrossRef]
- Miner, S.E.; Cole, D.E.; Evrovski, J.; Forrest, Q.; Hutchison, S.J.; Holmes, K.; Ross, H.J. N-acetylcysteine neither lowers plasma homocysteine concentrations nor improves brachial artery endothelial function in cardiac transplant recipients. Can. J. Cardiol. 2002, 18, 503–507. [Google Scholar]
- Kim, D.H.; Meza, C.A.; Clarke, H.; Kim, J.S.; Hickner, R.C. Vitamin D and endothelial function. Nutrients 2020, 12, 575. [Google Scholar] [CrossRef]
- Chiu, H.F.; Venkatakrishnan, K.; Golovinskaia, O.; Wang, C.K. Impact of micronutrients on hypertension: Evidence from clinical trials with a special focus on meta-analysis. Nutrients 2021, 13, 588. [Google Scholar] [CrossRef]
- Ran, L.; Zhao, W.; Tan, X.; Wang, H.; Mizuno, K.; Takagi, K.; Zhao, Y.; Bu, H. Association between serum vitamin C and the blood pressure: A systematic review and meta-analysis of observational studies. Cardiovasc. Ther. 2020, 2020, 4940673. [Google Scholar] [CrossRef]
- Guan, Y.; Dai, P.; Wang, H. Effects of vitamin C supplementation on essential hypertension: A systematic review and meta-analysis. Medicine (Baltimore) 2020, 99, e19274. [Google Scholar] [CrossRef] [PubMed]
- Tousoulis, D.; Antoniades, C.; Vassiliadou, C.; Toutouza, M.; Pitsavos, C.; Tentolouris, C.; Trikas, A.; Stefanadis, C. Effects of combined administration of low dose atorvastatin and vitamin E on inflammatory markers and endothelial function in patients with heart failure. Eur. J. Hear. Fail. 2005, 7, 1126–1132. [Google Scholar] [CrossRef] [PubMed]
- Emami, M.R.; Safabakhsh, M.; Alizadeh, S.; Asbaghi, O.; Khosroshahi, M.Z. Effect of vitamin E supplementation on blood pressure: A systematic review and meta-analysis. J. Hum. Hypertens. 2019, 33, 499–507. [Google Scholar] [CrossRef] [PubMed]
- Gates, P.E.; Boucher, M.L.; Silver, A.E.; Monahan, K.D.; Seals, D.R. Impaired flow-mediated dilation with age is not explained by L-arginine bioavailability or endothelial asymmetric dimethylarginine protein expression. J. Appl. Physiol. 2007, 102, 63–71. [Google Scholar] [CrossRef]
- Shiraseb, F.; Asbaghi, O.; Bagheri, R.; Wong, A.; Figueroa, A.; Mirzaei, K. The effect of L-arginine supplementation on blood pressure in adults: A systematic review and dose-response meta-analysis of randomized clinical trials. Adv. Nutr. Int. Rev. J. 2021. [Google Scholar] [CrossRef] [PubMed]
- Whyte, J. Rehabilitation effectiveness: The state of the science and a hope for the future. Am. J. Phys. Med. Rehabil. 2007, 86, 835–837. [Google Scholar] [CrossRef]
- Kachur, S.; Lavie, C.J.; Morera, R.; Ozemek, C.; Milani, R.V. Exercise training and cardiac rehabilitation in cardiovascular disease. Expert Rev. Cardiovasc. Ther. 2019, 17, 585–596. [Google Scholar] [CrossRef]
- Stucki, G.; Kroeling, P. Physical therapy and rehabilitation in the management of rheumatic disorders. Best Pr. Res. Clin. Rheumatol. 2000, 14, 751–771. [Google Scholar] [CrossRef]
- Sahin, H.; Varol, Y.; Naz, I.; Aksel, N.; Tuksavul, F.; Ozsoz, A. The effect of pulmonary rehabilitation on COPD exacerbation frequency per year. Clin. Respir. J. 2018, 12, 165–174. [Google Scholar] [CrossRef]
- McCarthy, B.; Casey, D.; Devane, D.; Murphy, K.; Murphy, E.; Lacasse, Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2015, 2, CD003793. [Google Scholar] [CrossRef]
- Anderson, L.; Thompson, D.R.; Oldridge, N.; Zwisler, A.D.; Rees, K.; Martin, N.; Taylor, R.S. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst. Rev. 2016, 1, CD001800. [Google Scholar] [CrossRef]
- Heran, B.S.; Chen, J.M.; Ebrahim, S.; Moxham, T.; Oldridge, N.; Rees, K.; Thompson, D.R.; Taylor, R.S. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst. Rev. 2011, CD001800. [Google Scholar] [CrossRef]
- Smith, E.E.; Markus, H.S. New treatment approaches to modify the course of cerebral small vessel diseases. Stroke 2020, 51, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Soares, R.N.; Murias, J.M.; Saccone, F.; Puga, L.; Moreno, G.; Resnik, M.; De Roia, G.F. Effects of a rehabilitation program on microvascular function of CHD patients assessed by near-infrared spectroscopy. Physiol. Rep. 2019, 7, e14145. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, K.; Ohta, T.; Zhang, J.; Hashimoto, S.; Tanaka, H. Influence of age and gender on exercise training-induced blood pressure reduction in systemic hypertension. Am. J. Cardiol. 1999, 84, 192–196. [Google Scholar] [CrossRef]
- Sinoway, L.I.; Musch, T.I.; Minotti, J.R.; Zelis, R. Enhanced maximal metabolic vasodilatation in the dominant forearms of tennis players. J. Appl. Physiol. 1986, 61, 673–678. [Google Scholar] [CrossRef] [PubMed]
- Mehra, V.M.; Gaalema, D.E.; Pakosh, M.; Grace, S.L. Systematic review of cardiac rehabilitation guidelines: Quality and scope. Eur. J. Prev. Cardiol. 2020, 27, 912–928. [Google Scholar] [CrossRef]
- Tanaka, S.; Sanuki, Y.; Ozumi, K.; Harada, T.; Tasaki, H. Heart failure with preserved vs reduced ejection fraction following cardiac rehabilitation: Impact of endothelial function. Hear. Vessel. 2018, 33, 886–892. [Google Scholar] [CrossRef]
- Legallois, D.; Belin, A.; Nesterov, S.V.; Milliez, P.; Parienti, J.J.; Knuuti, J.; Abbas, A.; Tirel, O.; Agostini, D.; Manrique, A. Cardiac rehabilitation improves coronary endothelial function in patients with heart failure due to dilated cardiomyopathy: A positron emission tomography study. Eur. J. Prev. Cardiol. 2016, 23, 129–136. [Google Scholar] [CrossRef]
- Cesari, F.; Marcucci, R.; Gori, A.M.; Burgisser, C.; Francini, S.; Sofi, F.; Gensini, G.F.; Abbate, R.; Fattirolli, F. Impact of a cardiac rehabilitation program and inflammatory state on endothelial progenitor cells in acute coronary syndrome patients. Int. J. Cardiol. 2013, 167, 1854–1859. [Google Scholar] [CrossRef]
- Guo, Y.; Ledesma, R.A.; Peng, R.; Liu, Q.; Xu, D. The beneficial effects of cardiac rehabilitation on the function and levels of endothelial progenitor cells. Hear. Lung Circ. 2017, 26, 10–17. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Merlo, C.; Bernardi, E.; Bellotti, F.; Pomidori, L.; Cogo, A. Supervised exercise training improves endothelial function in COPD patients: A method to reduce cardiovascular risk? ERJ Open Res. 2020, 6. [Google Scholar] [CrossRef] [PubMed]
- Ross, M.D.; Malone, E.; Florida-James, G. Vascular ageing and exercise: Focus on cellular reparative processes. Oxidative Med. Cell. Longev. 2016, 2016, 3583956. [Google Scholar] [CrossRef] [PubMed]
- Finks, S.W.; Rumbak, M.J.; Self, T.H. Treating hypertension in chronic obstructive pulmonary disease. N. Engl. J. Med. 2020, 382, 353–363. [Google Scholar] [CrossRef] [PubMed]
- Slivnick, J.; Lampert, B.C. Hypertension and Heart Failure. Hear. Fail. Clin. 2019, 15, 531–541. [Google Scholar] [CrossRef] [PubMed]
- Ambrosino, P.; Molino, A.; Calcaterra, I.; Formisano, R.; Stufano, S.; Spedicato, G.A.; Motta, A.; Papa, A.; Di Minno, M.N.D.; Maniscalco, M. Clinical assessment of endothelial function in convalescent COVID-19 patients undergoing multidisciplinary pulmonary rehabilitation. Biomedicines 2021, 9, 614. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ambrosino, P.; Bachetti, T.; D’Anna, S.E.; Galloway, B.; Bianco, A.; D’Agnano, V.; Papa, A.; Motta, A.; Perrotta, F.; Maniscalco, M. Mechanisms and Clinical Implications of Endothelial Dysfunction in Arterial Hypertension. J. Cardiovasc. Dev. Dis. 2022, 9, 136. https://doi.org/10.3390/jcdd9050136
Ambrosino P, Bachetti T, D’Anna SE, Galloway B, Bianco A, D’Agnano V, Papa A, Motta A, Perrotta F, Maniscalco M. Mechanisms and Clinical Implications of Endothelial Dysfunction in Arterial Hypertension. Journal of Cardiovascular Development and Disease. 2022; 9(5):136. https://doi.org/10.3390/jcdd9050136
Chicago/Turabian StyleAmbrosino, Pasquale, Tiziana Bachetti, Silvestro Ennio D’Anna, Brurya Galloway, Andrea Bianco, Vito D’Agnano, Antimo Papa, Andrea Motta, Fabio Perrotta, and Mauro Maniscalco. 2022. "Mechanisms and Clinical Implications of Endothelial Dysfunction in Arterial Hypertension" Journal of Cardiovascular Development and Disease 9, no. 5: 136. https://doi.org/10.3390/jcdd9050136
APA StyleAmbrosino, P., Bachetti, T., D’Anna, S. E., Galloway, B., Bianco, A., D’Agnano, V., Papa, A., Motta, A., Perrotta, F., & Maniscalco, M. (2022). Mechanisms and Clinical Implications of Endothelial Dysfunction in Arterial Hypertension. Journal of Cardiovascular Development and Disease, 9(5), 136. https://doi.org/10.3390/jcdd9050136










