Effective Veterinary Clinical Teaching in a Variety of Teaching Settings
Abstract
1. Introduction
- Accreditation/Regulatory Requirements (e.g., AAVMC, EAEVE, RCVS, VSAAC)
- Alternative approaches for learners refusing clinical teaching with live animals, which is a growing concern
- Animal rights activism
- Availability of animal models in Lab skills in order to avoid the use of live animals
- Caseload per clinical instructor
- Demand for exposure to different settings
- Departmental pressure
- Following the example from other areas of the OneHealth initiative
- Increasing learner numbers
- Increasing specialization at university veterinary hospitals
- Interruptions to delivery (e.g., Covid-19 pandemic)
- Minimal access to live animals, including restrictions on availability of shelter animals
- Staff shortages
- Main differences between clinical teaching in three types of learning settings, (clinical, traditional academic, and work-based learning) related to the delivery of the ‘exposure to practice’;
- Main differences between cases seen/solved in the three types of learning settings
- Structuring clinical teaching for high efficacy;
- Potential clinical teaching methods to minimize the impact of the types of learning setting on learning outcomes.
2. Main Differences between Clinical Teaching Settings
3. Main Differences between Cases Seen/Solved
4. Structuring Clinical Teaching for High Efficacy
5. Potential Strategies to Minimize the Impact of Alternative Settings and Approaches on Learner Outcomes
- Clinical teaching skills of instructors;
- Teaching settings;
- Time spent per site, and in total, on experiential learning.
5.1. Clinical Teaching Skills of Instructors
- Training of instructors in both delivery of clinical teaching and pedagogy-based approaches. Trained clinical instructors are better at delivering clinical teaching and are usually more satisfied [4,15,40,41,42]. Currently, veterinary instructors rarely, if ever, receive official training in clinical teaching, and there are no standardized requirements. This has been identified as an important gap in both veterinary [43,44] and human medical education [15,41,44,45,46,47]. Veterinary schools should provide opportunities to all professional staff for training in education, particularly staff delivering clinical teaching. In some geographical areas, on-line courses in general education become attractive [47,48]. However, it is recognized that general training may not be attractive or satisfying for veterinary clinical educators. Discipline teaching is preferred [47,49]. Indeed, some schools have developed discipline-specific, context-relevant partial programs to complete the clinical instructor development program [49], including the school at which we teach.
- Official recognition of clinical instructors. Official recognition of clinical instructors may take the form of being given title-holder status or, even better, a special qualification as a clinical instructor, after completing a specified training course/module/curriculum [35]. Training can be managed at departmental level, and it is easy to achieve.
- Promotion and career advancement of clinical instructors. The possibility of promotion of clinical instructors within a university setting is limited [16,41,50]. This is often due to the lack of a research component by many of the clinical instructors [51,52,53]. Promotion is primarily managed at the university, not departmental, level using the same rigid requirements as traditional academics. This makes the recognition by promotion and career advancements of clinical instructors more difficult and limited [50]. Therefore, for promotion and career advancement of clinical instructors, universities must consider having a special track for clinical instructors in veterinary medicine. Indeed, career progression is important also in partner clinics and this is an important area that needs to be addressed by the industry.
5.2. Strategies to Improve Clinical Teaching in Different Teaching Settings
5.2.1. Traditional Academic Settings
- Case-based learning (CBL). The CBL is a clinical teaching method usually applicable for earlier stages of the learner’s development. However, skillfully used, it is also suitable in advanced learning. The advantage of the CBL is it is a less time-consuming approach to delivery of clinical teaching. The role of the clinical instructor, who is the ‘expert in the field’ is to correct, direct, and provide feedback [55].
- ○
- Incorporation of simulation models within a case-based scenario rather than a practical class only, e.g., when using a bovine venipuncture simulation model, the scenario would look like: “A cow presented with progressively decreasing milk yield and exercise intolerance”. The scenario should guide learners to gather additional information
- ■
- Obtain health interview information from the client (for teaching purposes it should be available on request in a full format or summarized but without interpretations);
- ■
- Clinical examination results of the patient (for teaching purposes it should be available on request in a full format or summarized but without interpretations);
- ■
- Findings should indicate a clinical anemia. To confirm the anemia, the learners would hopefully arrive at the need to collect a blood sample;
- ■
- At that moment learners can be allowed to approach the model and carry out the skill;
- ■
- These points are summarized in Figure 2.

- Day One competencies (graduate attributes) addressed. Learners prefer seeing practice that is closer to what they will be seeing in their future clinical practice. Therefore, experiential learning should include diverse cases, particularly those that are common in general practice [13,19]. Learners prefer community-based clinical encounters, but with this approach only, there is often a lack of continuity of care. Thus, a variety of teaching settings are the preferred option.
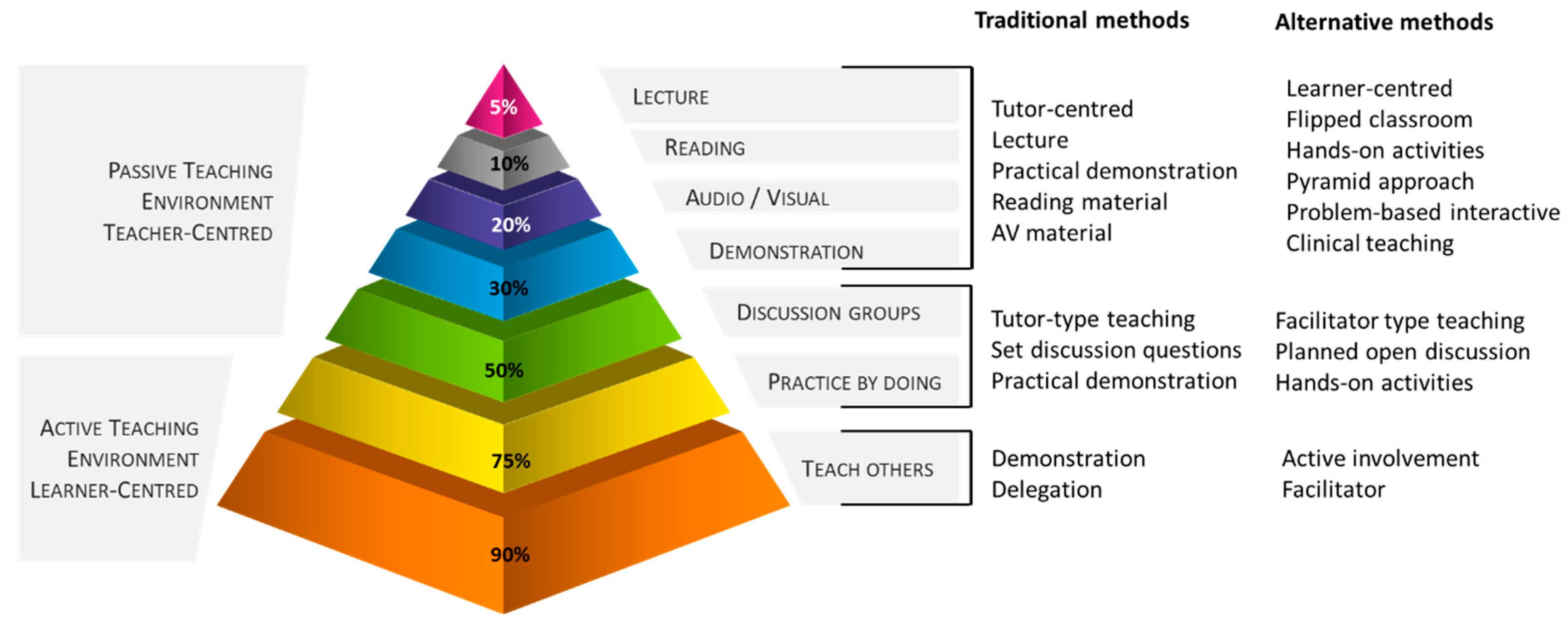
- Elements of ‘teach-others’. ‘Teaching’ others significantly increased knowledge retention and capacity to implement experience from one-to-another clinical situation in the future [30,34,56] (Figure 3). Teach-others learning may be used during discussion with the client, when implementing peer-assisted learning [14], or utilizing mini-lecture discussions [30]. Indeed, peer-assisted learning may also be a valuable tool for feedback on performance, frequently accepted as less confronting than when provided by the clinical instructor [14,31,55]. It is worth noting that peer-based feedback only is not preferred, as learners appreciate expert opinion on their performance and progress. Hence, a combination of peer- and expert-feedback is needed.
- Psychomotor activity within the case-solving. For example, use of simulation models rather than only presenting a case for solving.
- ○
- Simulation in a variety of forms should be utilized as much as possible, including but not restricted to [57,58,59,60,61]:
- ■
- High-fidelity examination simulators;
- ■
- Single-task models (e.g., skin suturing model, model for venipuncture);
- ■
- Standardized patient encounters;
- ■
- Virtual reality models (e.g., ‘haptic cow/horse’).
- Team-based learning (TBL). Although TBL is a teaching method aimed at delivery of clinical teaching to early stages of development of learners in veterinary and medical sciences, it is assumed to be very suitable for clinical teaching in advanced years [32,55,62]. Team-based learning clinical teaching has been praised for three elements of clinical teaching, inclusion of development of clinical reasoning, team work from learner’s perspective [31], and time efficiency. It usually consists of in-contact activities of 2 h duration, but preparation time is required. For efficacy, TBL should be properly executed, namely learners should be carefully allocated to groups. There should be a proper pre-activity preparation (e.g., readings, pre-recorded lectures) and individual- and group-level testing should be incorporated (i.e., readiness assurance tests), followed by immediate feedback on performance. Use of the four S approach (significant problem, same problem, specific choice and simultaneous reporting) during the activity is relevant for reflection, clinical reasoning and problem-solving [31,55,62,63].
- Combination of any of the above proposed strategies.
5.2.2. Clinical Setting
- Elements of ‘teach-others’.
- Case-based learning (e.g., rounds presentation/s). Case based discussions and enquiries are a great learning opportunity for learners [19]. However, this activity should not be limited to presentation and interpretation of facts only. It should stimulate development of clinical reasoning and other analytical skills [54,64]. For stimulation of the deep learning in learners, provided the learner has been asked to present rounds, the presentation should consider a type of a case critique where the learner explains what, why and how it could be improved in the particular clinical encounter.
- Day One competencies (graduate attributes) addressed. Minimize administrative load of learners [3].
- Use of clinical teaching models such as the Five Microskills Model. The use of clinical teaching models stimulates discussion and enquiries related to the clinical encounter that are particularly useful in the development of clinical reasoning of learners, yet with minimal time requirements of the clinical instructor in a busy practice [11,19].
- Using clinical instructor/s with a relevant clinical experience (e.g., avoiding the use of interns) [3].
5.2.3. Work-Based Learning
- Involvement in the clinical encounter. Learners may be involved by brief teaching models (e.g., Five Microskills [11]) or a formative assessments (e.g., grand rounds presentation/s).
- Day One competencies (graduate attributes) addressed [13].
- Portfolio-based learning can be utilized to stimulate the learner to engage with the clinical exposure [64]. However, for a deep learning, at least part of the records in the portfolio should include elements of displaying clinical reasoning and other analytical skills [64]. A properly designed portfolio should also include some elements of reflection [64]. Alternatives to a full learning portfolio, encompassing only particular portion/s, may be more appropriate and less demanding on the learner and the clinical instructor.
5.3. Strategies to Improve Clinical Teaching Changing the Time Spent in Exposure to Practice
6. Conclusions
Funding
Conflicts of Interest
Glossary
| Case-based learning | solving of an authentic clinical case using clinical reasoning skills, particularly useful in developing learners’ reflection and analytical skills through peer-learning approach and activation of prior knowledge. Learner-centered approach to learning. |
| Clinical encounter | any physical or virtual contact with a veterinary patient and client (e.g., owner, employee of an enterprise) with a primary responsibility to carry out clinical assessment or activity. |
| Clinical instructor | in addition to the regular veterinary practitioner’s duties, a clinical instructor should fulfil roles of assessor, facilitator, mentor, preceptor, role-model, supervisor, and teacher of veterinary learners in a clinical teaching environment. Apprentice/intern in the upper years, Resident, Veterinary educator/teacher, Veterinary practitioner. |
| Clinical reasoning | process during which a learner collects information, process it, comes to an understanding of the problem presented during a clinical encounter, and prepares a management plan, followed by evaluation of the outcome and self-reflection. Common synonyms include clinical acumen, clinical critical thinking, clinical decision-making, clinical judgment, clinical problem-solving, and clinical rationale. |
| Clinical teaching | form of an interpersonal communication between a clinical instructor and a learner that involves a physical or virtual clinical encounter. |
| Deep learning | aiming for mastery of essential academic content; thinking critically and solving complex problems; working collaboratively and communicating effectively; having an academic mindset; and being empowered through self-directed learning. |
| Portfolio-based learning | record of examples of learner’s work, including but not limited to case log, activity log and similar, with some elements of demonstration of reflective and clinical reasoning skills used for learning and assessment purposes. Learner-centered approach to learning. |
| Proper learning or a safe learning environment | an environment in which a learner feels safe, relaxed, and willing to take risks in pursuing a goal; enhances self-esteem and encourages exploration. |
| Self-directed learning | learners take charge of their own learning process by identifying learning needs, goals, and strategies and evaluating learning performances and outcomes. Learner-centered approach to learning. |
| Team-based learning | solving of an authentic clinical case using clinical reasoning skills. Particularly useful in developing basic science concepts through peer-learning approach (learning occurs within a team but also between teams when activity carried out concurrently with more than one team) and activation of prior knowledge. Learner-centered approach to learning. |
| Work-based learning | educational method that immerses the learners in the workplace. Usually, learners have to complete typical tasks for the workplace and satisfy school accreditation requirements, e.g., the American Association of Veterinary Medical Colleges and The Royal College of Veterinary Surgeons (where applicable). |
References
- Oaks, J.L.; Gilbert, M.; Virani, M.Z.; Watson, R.T.; Meteyer, C.U.; Rideout, B.A.; Shivaprasad, H.L.; Ahmed, S.; Iqbal Chaudhry, M.J.; Arshad, M.; et al. Diclofenac residues as the cause of vulture population decline in pakistan. Nature 2004, 427, 630–633. [Google Scholar] [CrossRef]
- Ogada, D.L.; Keesing, F.; Virani, M.Z. Dropping dead: Causes and consequences of vulture population declines worldwide: Worldwide decline of vultures. Ann. N. Y. Acad. Sci. 2012, 1249, 57–71. [Google Scholar] [CrossRef] [PubMed]
- Conner, B.J.; Behar-Horenstein, L.S.; Su, Y. Comparison of two clinical teaching models for veterinary emergency and critical care instruction. J. Vet. Med. Educ. 2016, 43, 58–63. [Google Scholar] [CrossRef]
- Boerboom, T.B.B.; Dolmans, D.H.J.M.; Jaarsma, A.D.C.; Muijtjens, A.M.M.; Van Beukelen, P.; Scherpbier, A.J.J.A. Exploring the validity and reliability of a questionnaire for evaluating veterinary clinical teachers’ supervisory skills during clinical rotations. Med. Teach. 2011, 33, e84–e91. [Google Scholar] [CrossRef]
- Ash, J.K.; Walters, L.K.; Prideaux, D.J.; Wilson, I.G. The context of clinical teaching and learning in australia. Med. J. Aust. 2012, 196, 475. [Google Scholar] [CrossRef]
- McCobb, E.; Rozanski, E.A.; Malcolm, E.L.; Wolfus, G.; Rush, J.E. A novel model for teaching primary care in a community practice setting: Tufts at tech community veterinary clinic. J. Vet. Med. Educ. 2018, 45, 99–107. [Google Scholar] [CrossRef]
- Smith, B.P.; Walsh, D.A. Teaching the art of clinical practice: The veterinary medical teaching hospital, private practice, and other externships. J. Vet. Med. Educ. 2003, 30, 203–206. [Google Scholar] [CrossRef]
- Barron, D.; Khosa, D.; Jones-Bitton, A. Experiential learning in primary care: Impact on veterinary students’ communication confidence. J. Exp. Educ. 2017, 40, 349–365. [Google Scholar] [CrossRef]
- Adams, C.L.; Ladner, L. Implementing a simulated client program: Bridging the gap between theory and practice. J. Vet. Med. Educ. 2004, 31, 138–145. [Google Scholar] [CrossRef]
- Kolb, D.A. Experiential Learning: Experience as the Source of Learning and Development; FT Press: Upper Saddle River, NJ, USA, 2014. [Google Scholar]
- Carr, A.N.; Kirkwood, R.N.; Petrovski, K.R. Using the five-microskills method in veterinary medicine clinical teaching. Vet. Sci. 2021, 8, 89. [Google Scholar] [CrossRef]
- Parsell, G.; Bligh, J. Recent perspectives on clinical teaching. Med. Educ. 2001, 35, 409–414. [Google Scholar] [CrossRef]
- Molgaard, L.K.; Chaney, K.P.; Bok, H.G.J.; Read, E.K.; Hodgson, J.L.; Salisbury, S.K.; Rush, B.R.; Ilkiw, J.E.; May, S.A.; Danielson, J.A.; et al. Development of core entrustable professional activities linked to a competency-based veterinary education framework. Med. Teach. 2019, 41, 1404–1410. [Google Scholar] [CrossRef]
- Sevenhuysen, S.; Skinner, E.H.; Farlie, M.K.; Raitman, L.; Nickson, W.; Keating, J.L.; Maloney, S.; Molloy, E.; Haines, T.P. Educators and students prefer traditional clinical education to a peer-assisted learning model, despite similar student performance outcomes: A randomised trial. J. Physiother. 2014, 60, 209–216. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McNeil, B.; Jakubisin Konicki, A. Insights on the clinical teaching needs of nurse practitioner preceptors. J. Nurse Pract. 2021, 17, 105–111. [Google Scholar] [CrossRef]
- Stark, P. Teaching and learning in the clinical setting: A qualitative study of the perceptions of students and teachers. Med. Educ. 2003, 37, 975–982. [Google Scholar] [CrossRef] [PubMed]
- Masters, P.A.; Nester, C. A study of primary care teaching comparing academic and community-based settings. J. Gen. Intern. Med. 2001, 16, 9–13. [Google Scholar] [CrossRef]
- Mor, S.M.; Norris, J.M.; Bosward, K.L.; Toribio, J.A.L.M.L.; Ward, M.P.; Gongora, J.; Vost, M.; Higgins, P.C.; McGreevy, P.D.; White, P.J.; et al. One health in our backyard: Design and evaluation of an experiential learning experience for veterinary medical students. One Health 2018, 5, 57–64. [Google Scholar] [CrossRef]
- Horner, P.; Hunukumbure, D.; Fox, J.; Leedham-Green, K. Outpatient learning perspectives at a uk hospital. Clin. Teach. 2020, 17, 680–687. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, A.; Allister, R.; Humphrey, D.; Moore, K.; Greenberg, K.; Greenberg, N. An evaluation of a veterinary-specific mental health service. Occup. Med. 2020, 70, 169–175. [Google Scholar] [CrossRef]
- Nahar, V.K.; Davis, R.E.; Dunn, C.; Layman, B.; Johnson, E.C.; Dascanio, J.J.; Johnson, J.W.; Sharma, M. The prevalence and demographic correlates of stress, anxiety, and depression among veterinary students in the southeastern united states. Res. Vet. Sci. 2019, 125, 370–373. [Google Scholar] [CrossRef]
- Ladyshewsky, R. Clinical Teaching; HERDSA: Canberra, Australia, 1995. [Google Scholar]
- Beck, J.B.; Long, M.; Ryan, M.S. Into the unknown: Helping learners become more comfortable with diagnostic uncertainty. Pediatrics 2020, 146, e2020027300. [Google Scholar] [CrossRef]
- Chinai, S.A.; Guth, T.; Lovell, E.; Epter, M. Taking advantage of the teachable moment: A review of learner-centered clinical teaching models. West. J. Emerg. Med. 2018, 19, 28–34. [Google Scholar] [CrossRef]
- Geyman, J.P. The practicing family physician as a teacher and learner in a family practice residency. J. Assoc. Hosp. Med. Educ. 1976, 1, 30–32. [Google Scholar]
- Hopkins, L.M.D.; Hampton, B.S.M.D.; Abbott, J.F.M.D.; Buery-Joyner, S.D.M.D.; Craig, L.B.M.D.; Dalrymple, J.L.M.D.; Forstein, D.A.D.O.; Graziano, S.C.M.D.; McKenzie, M.L.M.D.; Pradham, A.M.D.; et al. To the point: Medical education, technology, and the millennial learner. Am. J. Obstet. Gynecol. 2017, 218, 188–192. [Google Scholar] [CrossRef]
- Cantillon, P.; Wood, D.; Yardley, S. ABC of Learning and Teaching in Medicine, 3rd ed.; Wiley Blackwell: Hoboken, NJ, USA, 2017. [Google Scholar]
- Murad, M.H.; Coto-Yglesias, F.; Varkey, P.; Prokop, L.J.; Murad, A.L. The effectiveness of self-directed learning in health professions education: A systematic review. Med. Educ. 2010, 44, 1057–1068. [Google Scholar] [CrossRef] [PubMed]
- Otto, P.B. Finding an answer in questioning strategies. Sci. Child. 1991, 28, 44–47. [Google Scholar]
- Taylor, D.C.M.; Hamdy, H. Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83. Med. Teach. 2013, 35, e1561–e1572. [Google Scholar] [CrossRef]
- Burgess, A.; Bleasel, J.; Haq, I.; Roberts, C.; Garsia, R.; Robertson, T.; Mellis, C. Team-based learning (tbl) in the medical curriculum: Better than pbl? BMC Med. Educ. 2017, 17, 243. [Google Scholar] [CrossRef] [PubMed]
- Bate, E.; Hommes, J.; Duvivier, R.; Taylor, D.C.M. Problem-based learning (PBL): Getting the most out of your students—Their roles and responsibilities: AMEE Guide No. 84. Med. Teach. 2014, 36, 1–12. [Google Scholar] [CrossRef]
- Ownby, K.; Schumann, R.; Dune, L.; Kohne, D. A comparison of a traditional clinical experience to a precepted clinical experience for baccalaureate-seeking nursing students in their second semester. Nurs. Res. Pract. 2012, 2012, 276506. [Google Scholar] [CrossRef][Green Version]
- Lockyer, J.M.; Hodgson, C.S.; Lee, T.; Faremo, S.; Fisher, B.; Dafoe, W.; Yiu, V.; Violato, C. Clinical teaching as part of continuing professional development: Does teaching enhance clinical performance? Med. Teach. 2016, 38, 815–822. [Google Scholar] [CrossRef] [PubMed]
- Claeys, M.; Deplaecie, M.; Vanderplancke, T.; Delbaere, I.; Myny, D.; Beeckman, D.; Verhaeghe, S. The difference in learning culture and learning performance between a traditional clinical placement, a dedicated education unit and work-based learning. Nurse Educ. Today 2015, 35, e70–e77. [Google Scholar] [CrossRef]
- Bowker, M.H. Teaching students to ask questions instead of answering them. Thought Action 2010, 26, 127–134. [Google Scholar]
- Nguyen, K.A.; Lucas, C.; Leadbeatter, D. Student generation and peer review of examination questions in the dental curriculum: Enhancing student engagement and learning. Eur. J. Dent. Educ. 2020, 24, 548–558. [Google Scholar] [CrossRef]
- Hendricson, W.D.; Andrieu, S.C.; Chadwick, G.; Chmar, J.E.; Cole, J.R.; George, M.C.; Glickman, G.N.; Glover, J.F.; Goldberg, J.S.; Haden, N.K.; et al. Educational strategies associated with development of problem-solving, critical thinking, and self-directed learning. J. Dent. Educ. 2006, 70, 925–936. [Google Scholar] [PubMed]
- Petrovski, K.; McArthur, M. The art and science of consultations in bovine medicine: Use of modified calgary—Cambridge guides. Maced. Vet. Rev. 2015, 38, 137–147. [Google Scholar] [CrossRef]
- Adelung, M.; Prol, L.; Calabrese, J.; Guenther, L.A.; Copes, A. Teaching the teacher: Improving supervisory roles for clinical educators using interprofessional workshops. J. Allied Health 2021, 50, 9–13. [Google Scholar]
- Ramani, S. Twelve tips to promote excellence in medical teaching. Med. Teach. 2006, 28, 19–23. [Google Scholar] [CrossRef]
- O’Toole, J.K.; Klein, M.D.; McLinden, D.; Sucharew, H.; DeWitt, T.G. A pilot study of the creation and implementation of a teaching development assessment tool. J. Grad. Med. Educ. 2015, 7, 638–642. [Google Scholar] [CrossRef]
- Humm, K.R.; May, S.A. Clinical reasoning by veterinary students in the first-opinion setting: Is it encouraged? Is it practiced? J. Vet. Med. Educ. 2018, 45, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Steinert, Y.; Mann, K.V. Faculty development: Principles and practices. J. Vet. Med. Educ. 2006, 33, 317–324. [Google Scholar] [CrossRef]
- Boillat, M.; Bethune, C.; Ohle, E.; Razack, S.; Steinert, Y. Twelve tips for using the objective structured teaching exercise for faculty development. Med. Teach. 2012, 34, 269–273. [Google Scholar] [CrossRef]
- Houston, T.K.; Ferenchick, G.S.; Clark, J.M.; Bowen, J.L.; Branch, W.T.; Alguire, P.; Esham, R.H.; Clayton, C.P.; Kern, D.E. Faculty development needs. J. Gen. Intern. Med. 2004, 19, 375–379. [Google Scholar] [CrossRef][Green Version]
- Burgess, A.; van Diggele, C.; Mellis, C. Faculty development for junior health professionals. Clin. Teach. 2019, 16, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Burgess, A.; Bansal, A.; Clarke, A.; Ayton, T.; van Diggele, C.; Clark, T.; Matar, E. Clinical teacher training for health professionals: From blended to online and (maybe) back again? Clin. Teach. 2021, 18, 630–640. [Google Scholar] [CrossRef]
- Marschner, C.B.; Dahl, K.; Langebæk, R. Creating a pedagogical development program for veterinary clinical teachers: A discipline-specific, context-relevant, bottom-up initiative. J. Vet. Med. Educ. 2021, 48, 129–135. [Google Scholar] [CrossRef]
- Jacobs, C.K.; Everard, K.M.; Cronholm, P.F. Promotion of clinical educators: A critical need in academic family medicine. Fam. Med. 2020, 52, 631–634. [Google Scholar] [CrossRef]
- Deiorio, N.M.; Carney, P.A.; Kahl, L.E.; Bonura, E.M.; Juve, A.M. Coaching: A new model for academic and career achievement. Med. Educ. Online 2016, 21, 33480. [Google Scholar] [CrossRef] [PubMed]
- McAndrew, M.; Motwaly, S.; Kamens, T.E. Long-term follow-up of a dental faculty development program. J. Dent. Educ. 2013, 77, 716–722. [Google Scholar] [CrossRef] [PubMed]
- Ranieri, V.; Barratt, H.; Fulop, N.; Rees, G. Factors that influence career progression among postdoctoral clinical academics: A scoping review of the literature. BMJ Open 2016, 6, e013523. [Google Scholar] [CrossRef] [PubMed]
- Hashemiparast, M.; Negarandeh, R.; Theofanidis, D. Exploring the barriers of utilizing theoretical knowledge in clinical settings: A qualitative study. Int. J. Nurs. Sci. 2019, 6, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Burgess, A.; Matar, E.; Roberts, C.; Haq, I.; Wynter, L.; Singer, J.; Kalman, E.; Bleasel, J. Scaffolding medical student knowledge and skills: Team-based learning (TBL) and case-based learning (CBL). BMC Med. Educ. 2021, 21, 238. [Google Scholar] [CrossRef]
- Churchill, R.; Godinho, S.; Johnson, N.F.; Keddie, A.; Letts, W.J.; Lowe, K.; Mackay, J.; McGill, M.; Moss, J.; Nagel, M.C.; et al. Teaching: Making a Difference, 4th ed.; Wiley: Milton, Australia, 2019. [Google Scholar]
- Issenberg, S.B.; McGaghie, W.C.; Petrusa, E.R.; Gordon, D.L.; Scalese, R.J. Features and uses of high-fidelity medical simulations that lead to effective learning: A beme systematic review. Med. Teach. 2005, 27, 10–28. [Google Scholar] [CrossRef]
- Issenberg, S.B.; Scalese, R.J. Simulation in health care education. Perspect. Biol. Med. 2008, 51, 31–46. [Google Scholar] [CrossRef]
- Multak, N.; Newell, K.; Spear, S.; Scalese, R.J.; Barry Issenberg, S. A multi-institutional study using simulation to teach cardiopulmonary physical examination and diagnosis skills to physician assistant students. J. Physician Assist. Educ. 2015, 26, 70–76. [Google Scholar] [CrossRef]
- Scalese, R.J.; Issenberg, S.B. Effective use of simulations for the teaching and acquisition of veterinary professional and clinical skills. J. Vet. Med. Educ. 2005, 32, 461–467. [Google Scholar] [CrossRef]
- Ferreira, M.F.; de Araújo Sampaio Lima, R.; de Souza Amaral, R. Practising with an obstetric box and a dummy improves students’ confidence in performing obstetric procedures involving large animals. Vet. Rec. 2021, 188, e57. [Google Scholar] [CrossRef]
- Haidet, P.; Levine, R.E.; Parmelee, D.X.; Crow, S.; Kennedy, F.; Kelly, P.A.; Perkowski, L.; Michaelsen, L.; Richards, B.F. Perspective: Guidelines for reporting team-based learning activities in the medical and health sciences education literature. Acad. Med. 2012, 87, 292–299. [Google Scholar] [CrossRef]
- Ormandy, E. Team-based learning within the veterinary curriculum. Dev. Acad. Pract. 2021, 2021, 1–5. [Google Scholar] [CrossRef]
- Dacre, J.E.; Fox, R.A. How should we be teaching our undergraduates? Ann. Rheum. Dis. 2000, 59, 662–667. [Google Scholar] [CrossRef]
- Schutte, T.; Tichelaar, J.; Donker, E.; Richir, M.C.; Westerman, M.; van Agtmael, M.A. Clarifying learning experiences in student-run clinics: A qualitative study. BMC Med. Educ. 2018, 18, 244. [Google Scholar] [CrossRef]
- Payne, E.; Cobb, K.; Oldham, J.; Remnant, J. Attitudes of uk veterinary students towards careers in the production animal sector: A mixed methods approach. Vet. Rec. 2021, 189, e455. [Google Scholar] [CrossRef]
- Russell, W.M.S.; Burch, R.L. The Principles of Humane Experimental Technique; Methuen: London, UK, 1959. [Google Scholar]
| Parameter | Clinical Settings | Traditional Academic Settings | Work-Based Learning |
|---|---|---|---|
| Assessment method | Assessment of competency standards, Direct observations, Review of documentation | Assignment, Orals, OSCE 1, Project, Written | Direct observations; Semi-formative |
| Continuous and cumulative | Episodic | Hopefully continuous and cumulative | |
| Consequences of mistakes | Adverse effects on future learning and risk-taking, Adverse effects on the patient and/or client, Failure, Loss of employment opportunities, Loss of self-esteem, Poor grades | Failure, Lost opportunities for a scholarship and early graduation, Poor grades | Adverse effects on future learning and risk-taking, Adverse effects on the patient and/or client, Loss of employment opportunities, Loss of self-esteem, Repeating the activity |
| Emphasis of the learning material | Integration of skills, knowledge and attributes; Involvement of an integrated approach to all three learning domains (cognitive, affective and psychomotor) | Hopefully involves all three learning domains (cognitive, affective and psychomotor) but often in isolation, Knowledge, Theory, Skills; | Integration of cognitive and affective skills ± psychomotor skills |
| Expected outcomes | Each party may have different expectations and concerns. Learner and instructor—Achievement of academic program requirements, Good patient outcome, Happy client Client—Economic return, Improved animal welfare, Recovery of patient | Achievement of academic program requirements | Achievements of the work-based learning objectives |
| Group size | Usually single to few learners | Usually few to many learners | Usually single to few learners |
| Instructor’s responsibilities | Available; Colleague; Counsellor; Demonstrator; Evaluator, Facilitator, Mentor, More personal, Objective, Prepared, Role model, Up to date | Evaluator, Facilitator, Mentor, Less personal, Objective, Prepared, Up to date, Well presented, Work within specified frame | Colleague, Demonstrator, Evaluator, Facilitator, Mentor, More personal Prepared, Up to date, Objective, Role model, ±Available, ±Counsellor |
| Involved parties | Academic supervision, Client, Client’s family, Clinical and Para-clinical staff, Enterprise employees, Institutional supervision, Instructors, Learners, Patient | Instructors, Learners, Librarians, Para-teaching staff, Simulated clients | Academic supervision, Client, and Client’s family, Clinical and Para-clinical staff, Enterprise employees, Institutional supervision, Instructors, Learners, Patient |
| Learner’s responsibilities | Demonstrate problem-solving, clinical reasoning and empathy, Demonstrate professionalism, safe and effective clinical practice, | Participate, Pass assessment tasks, Turn up to activities, Work cooperatively with peers in group activities and assessments | Demonstrate professionalism, Turn up to activity, Work cooperatively |
| Learning happens by | Engagement, Learning through experience and active involvement, Observation, On-going feedback, Peer interaction, Real-life practice, Trial and error | Group work, Learner-centered strategies, Occasional feedback, Reading, Problem-based activities, Simulated practice | Learning through experience, Observation; Occasional feedback |
| Learning setting | Client’s homes or properties, Clinic, Hospital, Other institutions, Private institutions | Animal handling facility, Classroom, Laboratory, Tutorial room | Client’s homes or properties, Clinic, Hospital, Other institutions, Private institutions |
| Main settings | Clinical activities occur in a university clinic or similar setting | Little or no real-time animal contact (mainly theoretical, except practical activities) | Learners placed in a commercial practice |
| Number of instructors involved in clinical teaching | Usually few to many instructors | Usually single to few instructors | Usually single to few instructors |
| Risk of conflict | High | Low | Low to medium |
| Time per clinical encounter | Short to medium | Medium to long | Short |
| Total learner-instructor contact time | Short to medium | Medium to long | Short |
| Parameter | Clinical Settings | Traditional Academic Settings | Work-Based Learning |
|---|---|---|---|
| Instructor’s involvement | Facilitate learner’s dealing with cases; Learner’s assessment | Facilitate case-solving by learners; Learner’s assessment; Provision of feedback | Deal with cases and allow learners to observe ± be involved |
| Instructor’s responsibilities | Create safe learning environment during clinical exposure | Present for solving of a case in safe learning environment | Expose learners to cases |
| Learner’s involvement | Have the role of an ‘intern’ under direct and immediate supervision | Case-solving under direct facilitation | Minimal to restricted |
| Learner’s responsibilities | Deal with cases and observe clinic operations; Prepare case notes | Participate in case-solving | Observe cases and clinic operations |
| Learning environment | Ensuring achievement of learning objectives; ‘Safe’ | Animal handling facility; Classroom; Laboratory; Tutorial room; ± Simulated house call/field environment | Regular clinical practice |
| Learning objectives | Set learning objectives | Instructor-led set learning objectives | Prepared by learner and agreed by instructor (principles of self-directed learning) |
| Type of cases | Few; Need research time, Selection of what comes ‘in the door’, Unpredictable | Few; Clearly selected by the instructor, Predictable, Simulations | Anything that comes ‘in the door’; As many as possible, Unpredictable |
| Strategy | Attributes |
|---|---|
| Clinical encounter | Case-based/Real/Simulated; Carefully selected to allow progression of the learner from ‘simple’ to ‘more complex’; Stimulate teamwork |
| Independent learning | Case of the day/week; Case/Exit/Grand rounds; Question banks; Poster; Project; Report |
| Orientation | Discuss the usual approaches; Find out learners’ expectations/level of knowledge and expertise; Introduce facility; Introduce team; Set time for feedback; Set expectations; Set levels of responsibility |
| Planning | Debriefing after dealing with client/patient; Levels of responsibility when dealing with client/patient; How/What/When/Where/Who/Why when dealing with client/patient; Responsibility for veterinary medical records |
| Reflection | Debriefing on every case; What went well; What could be improved |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carr, A.N.; Kirkwood, R.N.; Petrovski, K.R. Effective Veterinary Clinical Teaching in a Variety of Teaching Settings. Vet. Sci. 2022, 9, 17. https://doi.org/10.3390/vetsci9010017
Carr AN, Kirkwood RN, Petrovski KR. Effective Veterinary Clinical Teaching in a Variety of Teaching Settings. Veterinary Sciences. 2022; 9(1):17. https://doi.org/10.3390/vetsci9010017
Chicago/Turabian StyleCarr, Amanda Nichole (Mandi), Roy Neville Kirkwood, and Kiro Risto Petrovski. 2022. "Effective Veterinary Clinical Teaching in a Variety of Teaching Settings" Veterinary Sciences 9, no. 1: 17. https://doi.org/10.3390/vetsci9010017
APA StyleCarr, A. N., Kirkwood, R. N., & Petrovski, K. R. (2022). Effective Veterinary Clinical Teaching in a Variety of Teaching Settings. Veterinary Sciences, 9(1), 17. https://doi.org/10.3390/vetsci9010017







