Microendoscopic Dorsal Laminectomy for Multi-Level Cervical Intervertebral Disc Protrusions in Dogs
Abstract
:1. Introduction
2. Materials and Methods
2.1. Case Enrollment
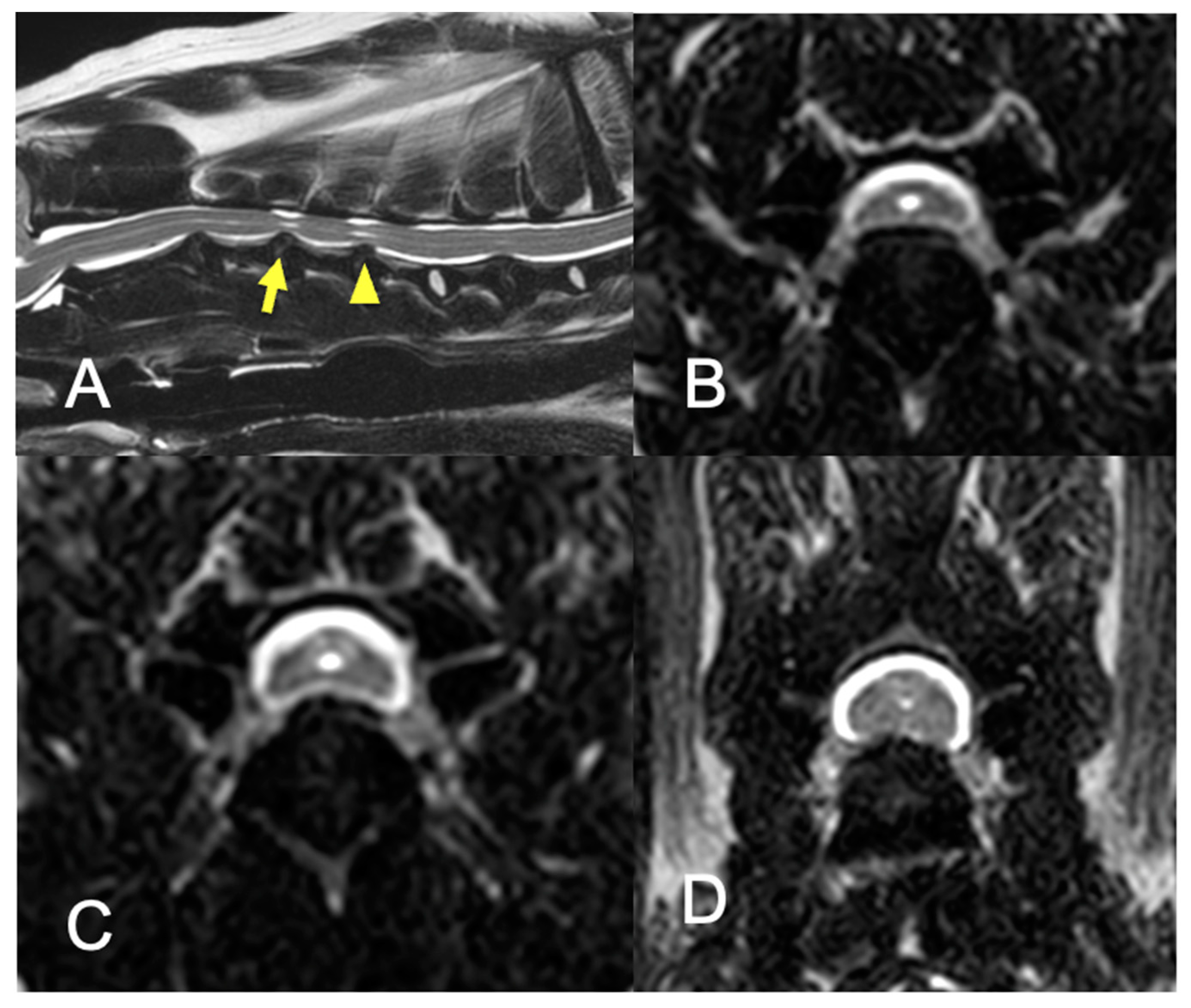
2.2. Imaging
2.3. Clinical Information and Follow-Up Evaluation
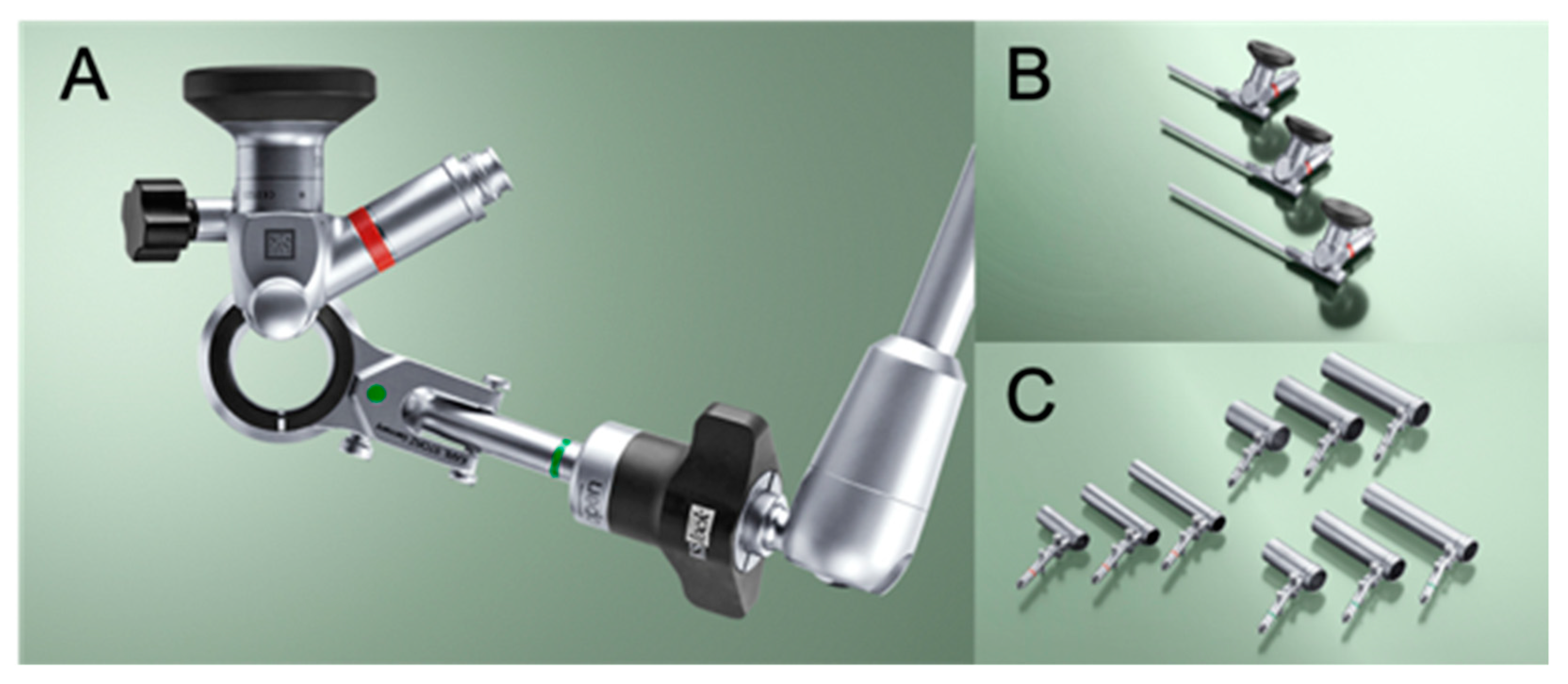
2.4. Surgical Procedure
2.5. Post-Operative Management
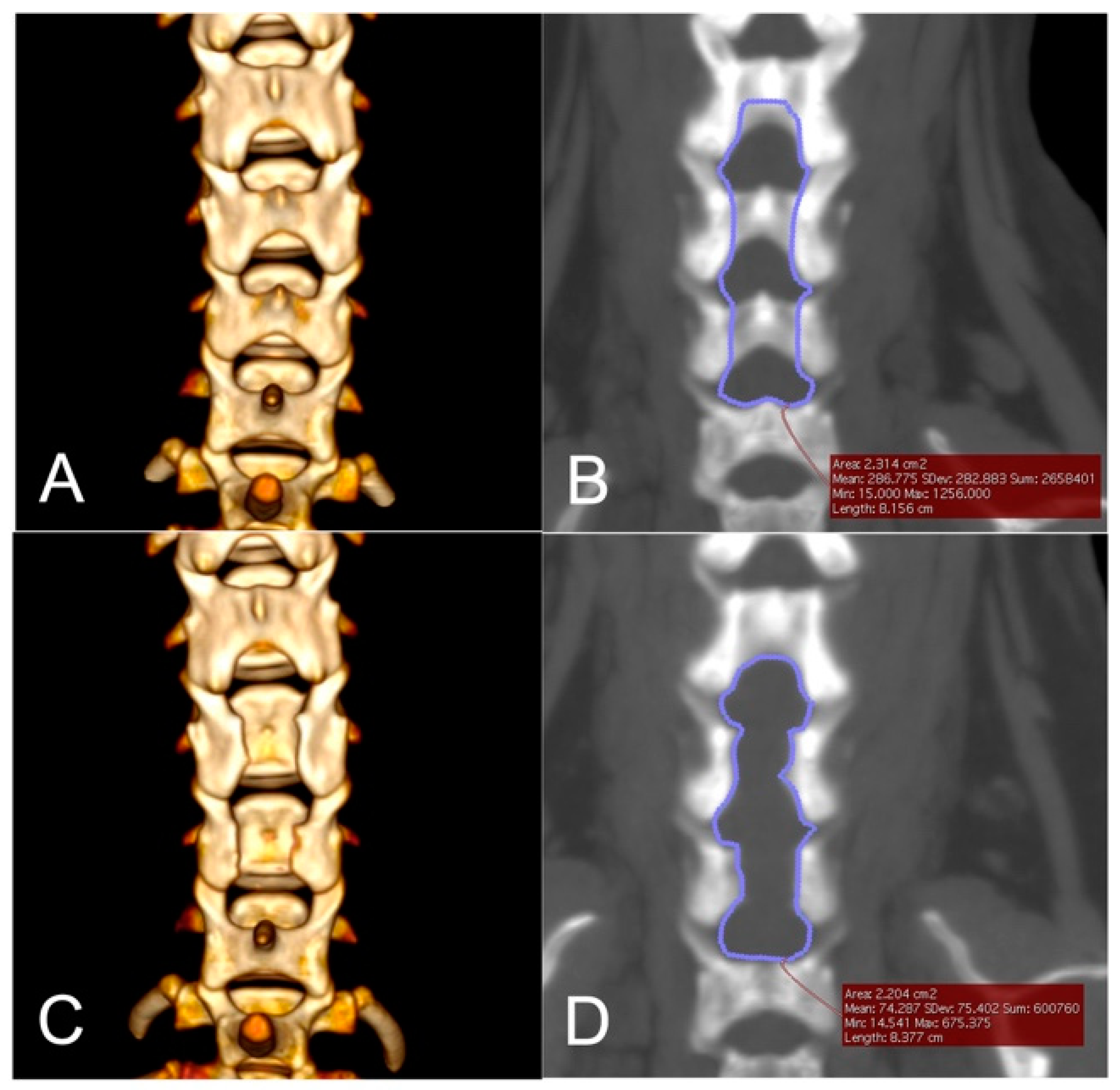
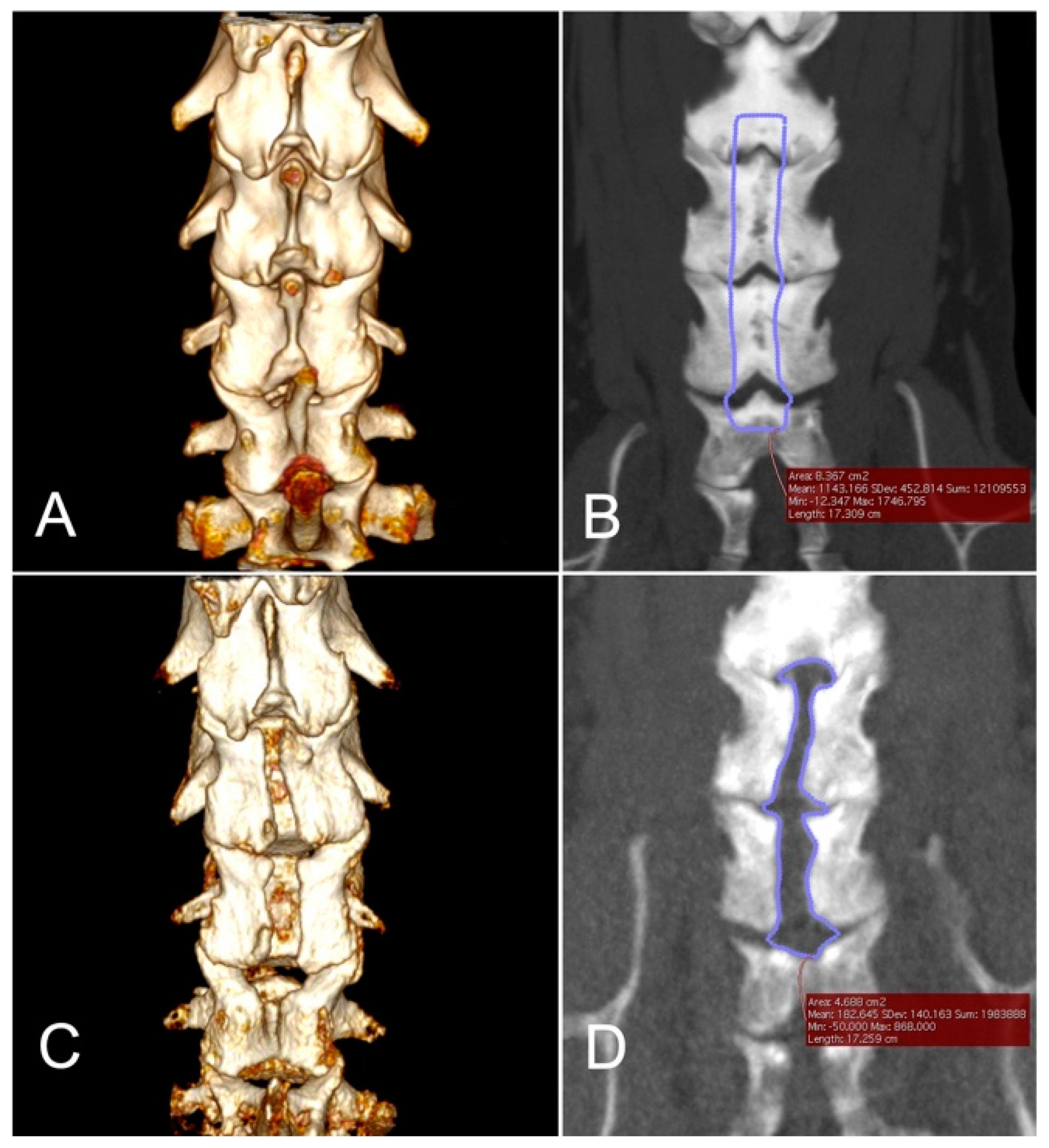
2.6. Imaging Analyses
3. Results
3.1. Case Population
3.2. Surgery and Intraoperative Complications
3.3. Postoperative Complications and Clinical Outcomes
3.4. Morphometric Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brisson, B.A. Intervertebral disc disease in dogs. Vet. Clin. N. Am. Small Anim. Pract. 2010, 40, 829–858. [Google Scholar] [CrossRef]
- Sharp, N. (Ed.) Cervical disk disease. In Small Animal Spinal Disorders Diagnosis and Surgery, 2nd ed.; Elsevier Mosby: Edinburgh, UK, 2005; pp. 93–120. [Google Scholar]
- Gill, P.J.; Lippincott, C.L.; Anderson, S.M. Dorsal laminectomy in the treatment of cervical intervertebral disk disease in small dogs: A retrospective study of 30 cases. J. Am. Anim. Hosp. Assoc. 1996, 32, 77–80. [Google Scholar] [CrossRef]
- Tanaka, H.; Nakayama, M.; Takase, K. Usefulness of hemilaminectomy for cervical intervertebral disk disease in small dogs. J. Vet. Med. Sci. 2005, 67, 679–683. [Google Scholar] [CrossRef] [Green Version]
- De Risio, L.; Munana, K.; Murray, M.; Olby, N.; Sharp, N.J.; Cuddon, P. Dorsal laminectomy for caudal cervical spondylomyelopathy: Postoperative recovery and long-term follow-up in 20 dogs. Vet. Surg. 2002, 31, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Taylor-Brown, F.E.; Cardy, T.J.; Liebel, F.X.; Garosi, L.; Kenny, P.J.; Volk, H.A.; De Decker, S. Risk factors for early post-operative neurological deterioration in dogs undergoing a cervical dorsal laminectomy or hemilaminectomy: 100 cases (2002–2014). Vet. J. 2015, 206, 327–331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hermantin, F.U.; Peters, T.; Quartararo, L.; Kambin, P. A prospective, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J. Bone Joint Surg. Am. 1999, 81, 958–965. [Google Scholar] [CrossRef]
- McGirt, M.J.; Parker, S.L.; Mummaneni, P.; Knightly, J.; Pfortmiller, D.; Foley, K.; Asher, A.L. Is the use of minimally invasive fusion technologies associated with improved outcomes after elective interbody lumbar fusion? Analysis of a nationwide prospective patient-reported outcomes registry. Spine J. 2017, 17, 922–932. [Google Scholar] [CrossRef]
- Rahman, M.; Summers, L.E.; Richter, B.; Mimran, R.I.; Jacob, R.P. Comparison of techniques for decompressive lumbar laminectomy: The minimally invasive versus the “classic” open approach. Minim. Invasive Neurosurg. 2008, 51, 100–105. [Google Scholar] [CrossRef]
- Park, Y.; Ha, J.W. Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine 2007, 32, 537–543. [Google Scholar] [CrossRef]
- Wang, H.; Zhou, Y.; Li, C.; Liu, J.; Xiang, L. Comparison of Open Versus Percutaneous Pedicle Screw Fixation Using the Sextant System in the Treatment of Traumatic Thoracolumbar Fractures. Clin. Spine Surg. 2017, 30, E239–E246. [Google Scholar] [CrossRef] [PubMed]
- Franke, J.; Greiner-Perth, R.; Boehm, H.; Mahlfeld, K.; Grasshoff, H.; Allam, Y.; Awiszus, F. Comparison of a minimally invasive procedure versus standard microscopic discotomy: A prospective randomised controlled clinical trial. Eur. Spine J. 2009, 18, 992–1000. [Google Scholar] [CrossRef] [Green Version]
- Fessler, R.G.; Khoo, L.T. Minimally invasive cervical microendoscopic foraminotomy: An initial clinical experience. Neurosurgery 2002, 51, S37–S45. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.T.; Kim, Y.B. Comparison between open procedure and tubular retractor assisted procedure for cervical radiculopathy: Results of a randomized controlled study. J. Korean Med. Sci. 2009, 24, 649–653. [Google Scholar] [CrossRef]
- Ruetten, S.; Komp, M.; Merk, H.; Godolias, G. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: A prospective, randomized, controlled study. Spine 2008, 33, 940–948. [Google Scholar] [CrossRef] [Green Version]
- Lockwood, A.A.; Griffon, D.J.; Gordon-Evans, W.; Matheson, J.A.; Barthelemy, N.; Schaeffer, D.J. Comparison of two minimally invasive approaches to the thoracolumbar spinal canal in dogs. Vet. Surg. 2014, 43, 209–221. [Google Scholar] [CrossRef]
- Carozzo, C.; Maitre, P.; Genevois, J.P.; Gabanou, P.A.; Fau, D.; Viguier, E. Endoscope-assisted thoracolumbar lateral corpectomy. Vet. Surg. 2011, 40, 738–742. [Google Scholar] [CrossRef]
- Drury, A.G.; Monnet, E.; Packer, R.A.; Marolf, A.J. Determination of surgical exposure obtained with integrated endoscopic thoracolumbar hemilaminectomy in large-breed cadaveric dogs. Vet. Surg. 2019, 48, O52–O58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hwang, Y.H.; Lee, H.C.; Lee, J.H. Operative Techniques and Preliminary Outcomes Following Percutaneous Endoscopic Thoracolumbar Pediculectomy in Dogs. Vet. Surg. 2016, 45, O84–O94. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.S.; Hwang, Y.H.; Lee, H.C.; Lee, J.H. Operative techniques of percutaneous endoscopic mini-hemilaminectomy using a uniportal approach in dogs. J. Vet. Med. Sci. 2017, 79, 1532–1539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leperlier, D.; Manassero, M.; Blot, S.; Thibaud, J.L.; Viateau, V. Minimally invasive video-assisted cervical ventral slot in dogs. A cadaveric study and report of 10 clinical cases. Vet. Comp. Orthop. Traumatol. 2011, 24, 50–56. [Google Scholar]
- Dent, B.T.; Fosgate, G.T.; Hettlich, B.F. Minimally invasive approach to lumbosacral decompression in a cadaveric canine model. N. Z. Vet. J. 2016, 64, 71–75. [Google Scholar] [CrossRef] [Green Version]
- Wood, B.C.; Lanz, O.I.; Jones, J.C.; Shires, P.K. Endoscopic-assisted lumbosacral foraminotomy in the dog. Vet. Surg. 2004, 33, 221–231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmied, O.; Golini, L.; Steffen, F. Effectiveness of cervical hemilaminectomy in canine Hansen Type I and Type II disc disease: A retrospective study. J. Am. Anim. Hosp. Assoc. 2011, 47, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Jeffery, N.D.; Olby, N.J.; Moore, S.A.; Canine Spinal Cord Injury, C. Clinical Trial Design-A Review-With Emphasis on Acute Intervertebral Disc Herniation. Front. Vet. Sci. 2020, 7, 583. [Google Scholar] [CrossRef]
- Bruecker, K.A.; Seim, H.B.; Withrow, S.J. Clinical evaluation of three surgical methods for treatment of caudal cervical spondylomyelopathy of dogs. Vet. Surg. 1989, 18, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Fitch, R.B.; Kerwin, S.C.; Hosgood, G. Caudal cervical intervertebral disk disease in the small dog: Role of distraction and stabilization in ventral slot decompression. J. Am. Anim. Hosp. Assoc. 2000, 36, 68–74. [Google Scholar] [CrossRef]
- Lemarié, R.J.; Kerwin, S.C.; Partington, B.P.; Hosgood, G. Vertebral subluxation following ventral cervical decompression in the dog. J. Am. Anim. Hosp. Assoc. 2000, 36, 348–358. [Google Scholar] [CrossRef]
- Guo, S.; Lu, D.; Pfeiffer, S.; Pfeiffer, D.U. Non-ambulatory dogs with cervical intervertebral disc herniation: Single versus multiple ventral slot decompression. Aust. Vet. J. 2020, 98, 148–155. [Google Scholar] [CrossRef] [PubMed]
- da Costa, R.C. Cervical spondylomyelopathy (wobbler syndrome) in dogs. Vet. Clin. N. Am. Small Anim. Pract. 2010, 40, 881–913. [Google Scholar] [CrossRef]
- Gasper, J.A.; Rylander, H.; Stenglein, J.L.; Waller, K.R. Osseous-associated cervical spondylomyelopathy in dogs: 27 cases (2000–2012). J. Am. Vet. Med. Assoc. 2014, 244, 1309–1318. [Google Scholar] [CrossRef] [PubMed]
- De Decker, S.; De Risio, L.; Lowrie, M.; Mauler, D.; Beltran, E.; Giedja, A.; Kenny, P.J.; Gielen, I.; Garosi, L.; Volk, H. Cervical vertebral stenosis associated with a vertebral arch anomaly in the Basset Hound. J. Vet. Intern. Med. 2012, 26, 1374–1382. [Google Scholar] [CrossRef]
- Guevar, J.; Zidan, N.; Durand, A.; Olby, N.J. Minimally invasive spine surgery in dogs: Evaluation of the safety and feasibility of a thoracolumbar approach to the spinal cord. Vet. Surg. 2020, 49 (Suppl. 1), O76–O85. [Google Scholar] [CrossRef]
- Marappan, K.; Jothi, R.; Paul Raj, S. Microendoscopic discectomy (MED) for lumbar disc herniation: Comparison of learning curve of the surgery and outcome with other established case studies. J. Spine Surg. 2018, 4, 630–637. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Merchant, Z.; Kire, N.; Patel, J.; Patel, A.; Kundnani, V. Learning Curve of Microendoscopic Discectomy in Single-Level Prolapsed Intervertebral Disc in 120 Patients. Glob. Spine J. 2020, 10, 571–577. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Righesso, O.; Falavigna, A.; Avanzi, O. Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: Results of a randomized controlled trial. Neurosurgery 2007, 61, 545–549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakagawa, H.; Kamimura, M.; Uchiyama, S.; Takahara, K.; Itsubo, T.; Miyasaka, T. Microendoscopic discectomy (MED) for lumbar disc prolapse. J. Clin. Neurosci. 2003, 10, 231–235. [Google Scholar] [CrossRef]
- Schizas, C.; Tsiridis, E.; Saksena, J. Microendoscopic discectomy compared with standard microsurgical discectomy for treatment of uncontained or large contained disc herniations. Neurosurgery 2005, 57, 357–360. [Google Scholar] [CrossRef] [Green Version]

| Case No. | Breed | Body Weight at Surgery (kg) | Sex | Age at Surgery (month) | Duration of Clinical Signs(days) | Locations of IVDH | Prior Medication |
|---|---|---|---|---|---|---|---|
| 1 | Chihuahua | 3.2 | CM | 84 | 180 | C4–5, C5–6, C6–7 | prednisolone 0.3 mg/kg q24 |
| 2 | Chihuahua | 2.62 | CM | 124 | 14 | C4–5, C5–6, C6–7 | none |
| 3 | Whippet | 11.6 | M | 118 | 120 | C5–6, C6–7 | none |
| 4 | Doberman Pinscher | 30.4 | SF | 108 | 21 | C4–5, C5–6, C6–7 | prednisolone 0.5 mg/kg q24 |
| 5 | Yorkshire Terrier | 3.55 | CM | 143 | 330 | C5–6, C7–T1 | prednisolone 0.5 mg/kg q24 |
| 6 | Yorkshire Terrier | 4 | SF | 124 | 14 | C3–4, C4–5 | prednisolone 0.6 mg/kg q48 |
| 7 | Toy Poodle | 4.3 | F | 142 | 30 | C5–6, C6–7, C7–T1 | prednisolone 0.5 mg/kg q24 |
| 8 | Pomeranian | 2.9 | SF | 118 | 30 | C3–4, C6–7, C7–T1 | none |
| Case No. | Locations of Laminectomy | Total Surgery Time (min) | Size of Tubular Retractor (mm) | Size of Skin Incision (mm) | Laminectomy Size | ||
|---|---|---|---|---|---|---|---|
| Planned Area (cm2) | Actual Area (cm2) | Actual/Planned (%) | |||||
| 1 | 142 | 15 × 40 | 26.19 | 2.176 | 2.002 | 92.00 | |
| 2 | C4, C5, C6 | 125 | 15 × 40 | 26.5 | 2.314 | 2.204 | 95.25 |
| 3 | C5, C6, C7 | 189 | 19 × 40 | 19.1 | 3.552 | 2.682 | 75.51 |
| 4 | C4, C5, C6, C7 | 324 * | 19 × 70 | NA | 8.367 | 4.688 | 56.03 |
| 5 | C5, C6, C7 | 113 | 15 × 40 | 30.24 | NA | NA | NA |
| 6 | C3, C4, C5 | 217 | 15 × 40 | 17.91 | 1.559 | 1.374 | 88.13 |
| 7 | C5, C6, C7 | 107 | 15 × 40 | 34.62 | 1.993 | 1.919 | 96.29 |
| 8 | C6, C7 | 236 ** | 15 × 40 | 23.4 | 1.519 | 1.774 | 116.79 |
| Case No. | Neurological Grade (Post-Op Day) | In-Hospital Follow Up Evaluation (Days) | ||||
|---|---|---|---|---|---|---|
| Presentation | Discharge | 1st Visit Post-Surgery | Last Visit Post-Surgery | Telephone Interview | ||
| 1 | 3 | 3 (2) | 2 (42) | NA | 0 (898) | 42 |
| 2 | 2 | 2 (3) | 1 (17) | NA | 0 (1024) | 17 |
| 3 | 3 | 3 (3) | 1 (25) | NA | 1 (437) | 25 |
| 4 | 3 | 4 (3) | 2 (15) | 1 (92) | 1 (284) | 15, 43, 92 |
| 5 | 4 | 4 (3) | NA | NA | 1 (668) | NA |
| 6 | 4 | 4 (2) | 4 (10) | 1 (88) | 1 (521) | 10, 22, 63, 88 |
| 7 | 3 | 4 (4) | 2 (16) | NA | 1 (495) | 16 |
| 8 | 4 | 4 (3) | 2 (17) | NA | 1 (88) | 17 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamishina, H.; Nakano, Y.; Nakata, K.; Kimura, S.; Nozue, Y.; Drury, A.G.; Maeda, S. Microendoscopic Dorsal Laminectomy for Multi-Level Cervical Intervertebral Disc Protrusions in Dogs. Vet. Sci. 2022, 9, 18. https://doi.org/10.3390/vetsci9010018
Kamishina H, Nakano Y, Nakata K, Kimura S, Nozue Y, Drury AG, Maeda S. Microendoscopic Dorsal Laminectomy for Multi-Level Cervical Intervertebral Disc Protrusions in Dogs. Veterinary Sciences. 2022; 9(1):18. https://doi.org/10.3390/vetsci9010018
Chicago/Turabian StyleKamishina, Hiroaki, Yukiko Nakano, Kohei Nakata, Shintaro Kimura, Yuta Nozue, Adam G. Drury, and Sadatoshi Maeda. 2022. "Microendoscopic Dorsal Laminectomy for Multi-Level Cervical Intervertebral Disc Protrusions in Dogs" Veterinary Sciences 9, no. 1: 18. https://doi.org/10.3390/vetsci9010018
APA StyleKamishina, H., Nakano, Y., Nakata, K., Kimura, S., Nozue, Y., Drury, A. G., & Maeda, S. (2022). Microendoscopic Dorsal Laminectomy for Multi-Level Cervical Intervertebral Disc Protrusions in Dogs. Veterinary Sciences, 9(1), 18. https://doi.org/10.3390/vetsci9010018






