Analysis of Final Year Veterinary Students’ Telephone Communication Skills at a Veterinary Teaching Hospital
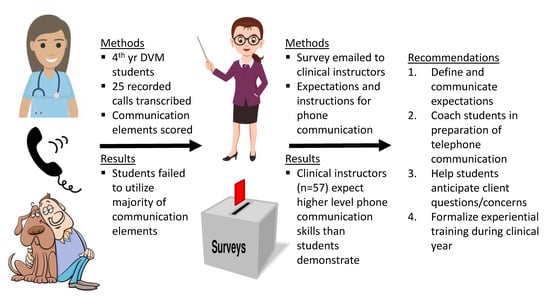
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
Current North Carolina State University (NCSU) Communication Training Curriculum
2.2. Data Collection
2.2.1. Authentic Student-Client Telephone Communication
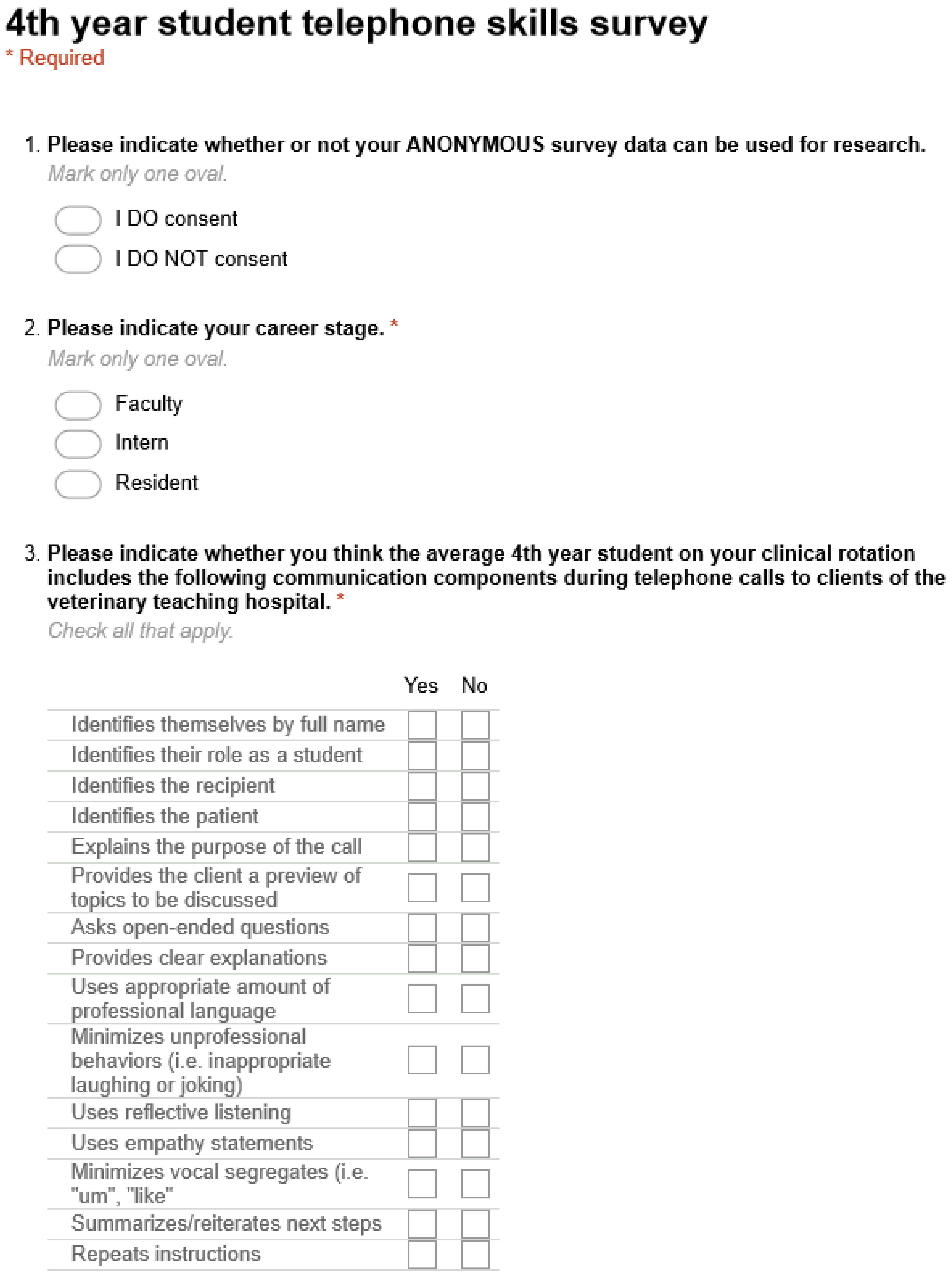
2.2.2. Educator Questionnaire
2.3. Data Analysis
2.4. Ethical Considerations
3. Results
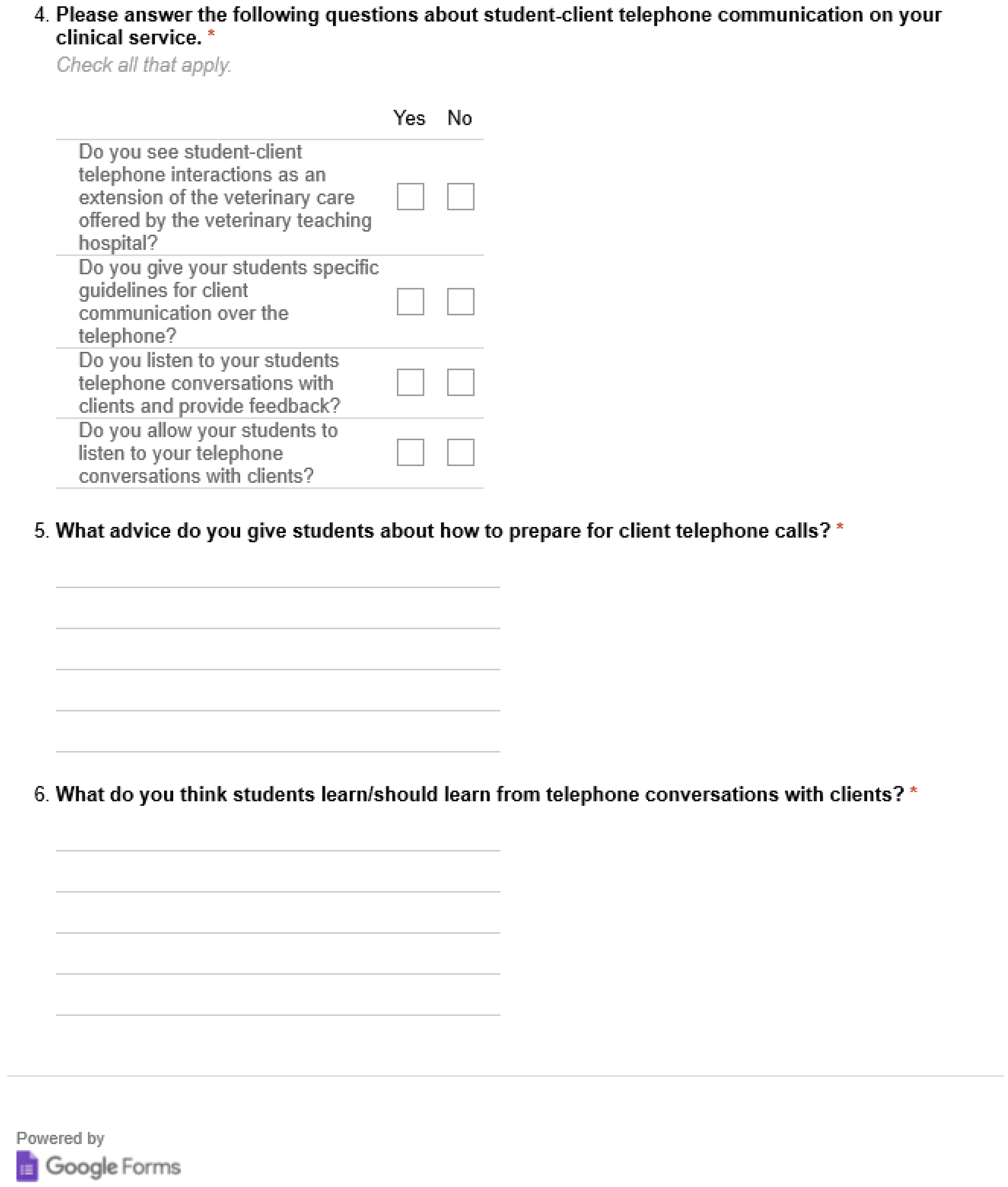
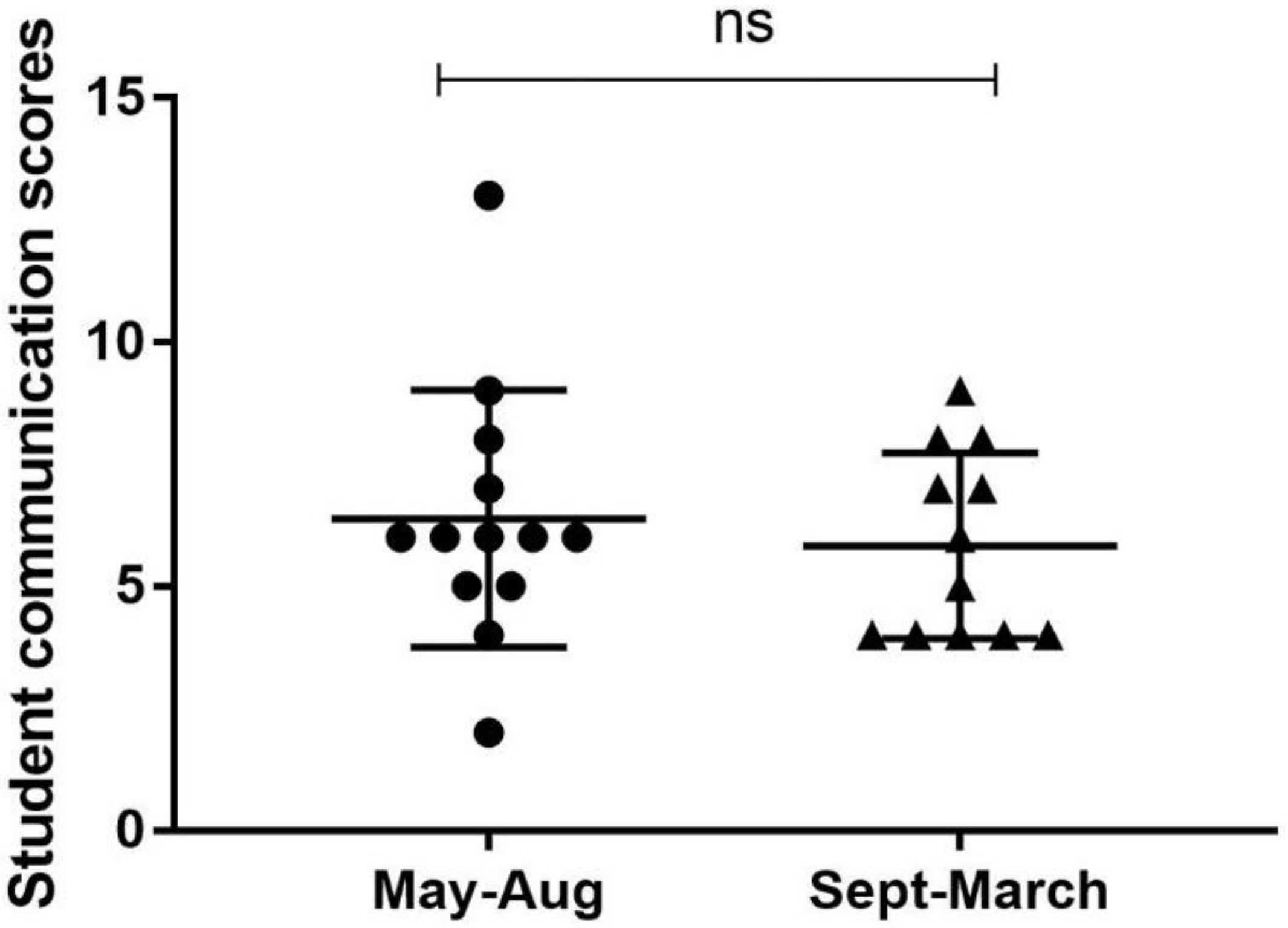
3.1. Analysis of Authentic, Recorded Student-Client Telephone Communications
3.2. Quantitative and Qualitative Analysis of Veterinary Educator Survey Responses
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Student: | Service: | Call Length: |
|---|---|---|
| Missing/No | Item to Be Coded | Completed/Yes |
| Identify self by full name | ||
| Identify role | ||
| Identify recipient | ||
| Identify patient | ||
| Explains purpose of call | ||
| Provides preview | ||
| Clear explanations | ||
| Professional language | ||
| Unprofessional behaviors (Laughing) | ||
| Vocal segregates (ums) | ||
| Reflective listening | ||
| Interruptions | ||
| Empathy | ||
| Open-ended questions | ||
| Summarize/reiterate next steps | ||
| Repeat instructions |
Appendix B
References
- LeBlanc, T.W. Communication skills training in the twenty-first century. AMA J. Ethics 2015, 17, 140–143. [Google Scholar] [PubMed]
- Whitcomb, M.E. Communication and professionalism. Patient Educ. Couns. 2000, 41, 137–144. [Google Scholar] [CrossRef]
- Shaw, J.R. Four core communication skills of highly effective practitioners. Vet. Clin. N. Am. Small Anim. Pract. 2006, 36, 385–396. [Google Scholar] [CrossRef]
- Lloyd, J.W.; King, L.J.; Klausner, J.S.; Harris, D. National workshop on core competencies for success in the veterinary profession. J. Vet. Med. Educ. 2003, 30, 280–284. [Google Scholar] [CrossRef] [PubMed]
- Roter, D.L.; Stewart, M.; Putnam, S.M.; Lipkin, M.; Stiles, W.; Inui, T.S. Communication patterns of primary care physicians. JAMA 1997, 277, 350–356. [Google Scholar] [CrossRef]
- Langewitz, W.A.; Eich, P.; Kiss, A.; Wössmer, B. Improving communication skills—A randomized controlled behaviorally oriented intervention study for residents in internal medicine. Psychosom. Med. 1998, 60, 268–276. [Google Scholar] [CrossRef] [PubMed]
- Langewitz, W. [The more the patient knows the better his or her position?]. Ther. Umsch. 2007, 64, 585–587. [Google Scholar] [CrossRef]
- Jenkins, V.; Fallowfield, L. Can communication skills training alter physicians’ beliefs and behavior in clinics? J. Clin. Oncol. 2002, 20, 765–769. [Google Scholar]
- Royal, K.D.; Sheats, M.K.; Kedrowicz, A.A. Readability Evaluations of Veterinary Client Handouts and Implications for Patient Care. Top. Companion Anim. Med. 2018. [Google Scholar] [CrossRef]
- Tuisku, O.A.; Ilves, M.K.; Lylykangas, J.K.; Surakka, V.V.; Ainasoja, M.; Rytövuori, S.E.; Ruohonen, M.J. Emotional responses of clients to veterinarian communication style during a vaccination visit in companion animal practice. J. Am. Vet. Med. Assoc. 2018, 252, 1120–1132. [Google Scholar] [CrossRef]
- Coe, J.B.; Adams, C.L.; Bonnett, B.N. A focus group study of veterinarians’ and pet owners’ perceptions of veterinarian-client communication in companion animal practice. J. Am. Vet. Med. Assoc. 2008, 233, 1072–1080. [Google Scholar] [CrossRef] [PubMed]
- Aaronson, E.L.; White, B.A.; Black, L.; Brown, D.F.; Benzer, T.; Castagna, A.; Raja, A.S.; Sonis, J.; Mort, E. Training to Improve Communication Quality: An Efficient Interdisciplinary Experience for Emergency Department Clinicians. Am. J. Med. Qual. 2018. [Google Scholar] [CrossRef] [PubMed]
- Abdoolraheem, M.Y.; Zeina, M. A perspective on simulated patients’ and patient-educators’ teaching of communication skills. Med. Educ. 2018, 52, 1097. [Google Scholar] [CrossRef] [PubMed]
- Abughosh, S.; Wang, X.; Serna, O.; Esse, T.; Mann, A.; Masilamani, S.; Holstad, M.M.; Essien, E.J.; Fleming, M. A Motivational Interviewing Intervention by Pharmacy Students to Improve Medication Adherence. J. Manag. Care Spec. Pharm. 2017, 23, 549–560. [Google Scholar] [CrossRef] [PubMed]
- Chichirez, C.M.; Purcărea, V.L. Interpersonal communication in healthcare. J. Med. Life 2018, 11, 119–122. [Google Scholar] [PubMed]
- DeBlasio, D.; Real, F.J.; Ollberding, N.J.; Klein, M.D. Provision of Parent Feedback via the Communication Assessment Tool: Does It Improve Resident Communication Skills? Acad. Pediatr. 2018. [Google Scholar] [CrossRef] [PubMed]
- Denvir, P.M.; Cardone, K.E.; Parker, W.M.; Cerulli, J. “How do I say that?”: Using communication principles to enhance medication therapy management instruction. Curr Pharm. Teach. Learn. 2018, 10, 185–194. [Google Scholar] [CrossRef]
- Gené, E.; Olmedo, L.; Pascual, M.; Azagra, R.; Elorduy, M.; Virumbrales, M. [Evaluation of clinical communication skills in medical students with simulated patients]. Rev. Med. Chile 2018, 146, 160–167. [Google Scholar] [CrossRef]
- Haugland, V.L.; Reime, M.H. Scenario-based simulation training as a method to increase nursing students’ competence in demanding situations in dementia care. A mixed method study. Nurse Educ. Pract. 2018. [Google Scholar] [CrossRef]
- Koehler, T.C.; Bok, H.; Westerman, M.; Jaarsma, D. Developing a competency framework for pharmacy technicians: Perspectives from the field. Res. Soc. Adm. Pharm. 2018. [Google Scholar] [CrossRef]
- MacDonald-Wicks, L.; Levett-Jones, T. Effective teaching of communication to health professional undergraduate and postgraduate students: A Systematic Review. JBI Libr. Syst. Rev. 2012, 10, 1–12. [Google Scholar] [CrossRef]
- Niglio de Figueiredo, M.; Krippeit, L.; Ihorst, G.; Sattel, H.; Bylund, C.L.; Joos, A.; Bengel, J.; Lahmann, C.; Fritzsche, K.; Wuensch, A. ComOn-Coaching: The effect of a varied number of coaching sessions on transfer into clinical practice following communication skills training in oncology: Results of a randomized controlled trial. PLoS ONE 2018, 13, e0205315. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, K.R.E.; Trovo, M.M.; Risso, A.C.M.D.; Braga, E.M. The teaching approach on communicative skills in different teaching methodologies. Rev. Bras. Enferm. 2018, 71, 2447–2453. [Google Scholar] [CrossRef] [PubMed]
- Shen, L.; Zeng, H.; Jin, X.; Yang, J.; Shang, S.; Zhang, Y. An Innovative Evaluation in Fundamental Nursing Curriculum for Novice Nursing Students: An Observational Research. J. Prof. Nurs. 2018, 34, 412–416. [Google Scholar] [CrossRef] [PubMed]
- Teramachi, H.; Ino, Y.; Sugita, I.; Nishio, Y.; Yoshida, A.; Hayashi, Y.; Esaki, H.; Saito, K.; Noguchi, Y.; Iguchi, K.; et al. Evaluating communication skills after long-term practical training among Japanese pharmacy students. Curr. Pharm. Teach. Learn. 2018, 10, 446–452. [Google Scholar] [CrossRef] [PubMed]
- Vogel, D.; Meyer, M.; Harendza, S. Verbal and non-verbal communication skills including empathy during history taking of undergraduate medical students. BMC Med. Educ. 2018, 18, 157. [Google Scholar] [CrossRef] [PubMed]
- Webb, L. Exploring the characteristics of effective communicators in healthcare. Nurs. Stand. 2018. [Google Scholar] [CrossRef]
- Carson, C.A. Nonverbal communication in veterinary practice. Vet. Clin. N. Am. Small Anim. Pract. 2007, 37, 49–63. [Google Scholar] [CrossRef]
- Adams, C.L.; Kurtz, S.M. Building on existing models from human medical education to develop a communication curriculum in veterinary medicine. J. Vet. Med. Educ. 2006, 33, 28–37. [Google Scholar] [CrossRef]
- Shaw, J.R.; Adams, C.L.; Bonnett, B.N. What can veterinarians learn from studies of physician-patient communication about veterinarian-client-patient communication? J. Am. Vet. Med. Assoc. 2004, 224, 676–684. [Google Scholar] [CrossRef]
- Shaw, J.R.; Bonnett, B.N.; Adams, C.L.; Roter, D.L. Veterinarian-client-patient communication patterns used during clinical appointments in companion animal practice. J. Am. Vet. Med. Assoc. 2006, 228, 714–721. [Google Scholar] [CrossRef] [PubMed]
- Cornell, K.K.; Kopcha, M. Client-veterinarian communication: Skills for client centered dialogue and shared decision making. Vet. Clin. N. Am. Small Anim. Pract. 2007, 37, 37–47, abstract vii. [Google Scholar] [CrossRef] [PubMed]
- Radecki, S.E.; Neville, R.E.; Girard, R.A. Telephone patient management by primary care physicians. Med. Care 1989, 27, 817–822. [Google Scholar] [CrossRef] [PubMed]
- Car, J.; Sheikh, A. Telephone consultations. BMJ 2003, 326, 966–969. [Google Scholar] [CrossRef] [PubMed]
- Morony, S.; Weir, K.; Duncan, G.; Biggs, J.; Nutbeam, D.; Mccaffery, K.J. Enhancing communication skills for telehealth: Development and implementation of a Teach-Back intervention for a national maternal and child health helpline in Australia. BMC Health Serv. Res. 2018, 18, 162. [Google Scholar] [CrossRef]
- Reisman, A.B.; Brown, K.E. Preventing communication errors in telephone medicine. J. Gen. Intern. Med. 2005, 20, 959–963. [Google Scholar] [CrossRef]
- Kosower, E.; Inkelis, S.H.; Seidel, J.S. Telephone T.A.L.K.: A telephone communication program. Pediatr. Emerg. Care 1991, 7, 76–79. [Google Scholar] [CrossRef]
- Grevemeyer, B.; Betance, L.; Artemiou, E. A Telephone Communication Skills Exercise for Veterinary Students: Experiences, Challenges, and Opportunities. J. Vet. Med. Educ. 2016, 43, 126–134. [Google Scholar] [CrossRef]
- Cary, J.A.; Farnsworth, K.D.; Kurtz, S. Telephone communication in emergency cases: A training program for veterinary students. J. Vet. Med. Educ. 2010, 37, 130–135. [Google Scholar] [CrossRef]
- Molgaard, L.K.; Hodgson, J.L.; Bok, H.G.J.; Chaney, K.P.; Ilkiw, J.E.; Matthew, S.M.; May, S.A.; Read, E.K.; Rush, B.R.; Salisbury, S.K. Competency-Based Veterinary Education: Part 1—CBVE Framework; Association of American Veterinary Medical Colleges: Washington, DC, USA, 2018. [Google Scholar]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Corbin, J.M. The Corbin and Strauss Chronic Illness Trajectory model: An update. Sch. Inq. Nurs. Pract. 1998, 12, 33–41. [Google Scholar] [PubMed]
- Reedy, G.B. Using Cognitive Load Theory to Inform Simulation Design and Practice. Clin. Simul. Nurs. 2015, 11, 355–360. [Google Scholar] [CrossRef]
- Kurtz, S.M. Doctor-patient communication: Principles and practices. Can. J. Neurol. Sci. 2002, 29 (Suppl. 2), S23–S29. [Google Scholar] [CrossRef] [PubMed]
| Communication Categories | Students | Clinical Educators | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | ||||||
| n | % | n | % | n | % | n | % | p-Value | |
| Identify self by name | 3 | 12.0 | 22 | 88.0 | 38 | 66.7 | 19 | 33.3 | 0.000 * |
| Identify role | 3 | 12.0 | 22 | 88.0 | 52 | 91.2 | 5 | 8.8 | 0.000 * |
| Identify recipient | 14 | 56.0 | 11 | 44.0 | 37 | 64.9 | 20 | 35.1 | 0.300 |
| Identify patient | 22 | 88.0 | 3 | 12.0 | 27 | 100.0 | 0 | 0 | 0.026 † |
| Explain purpose of call | 20 | 80.0 | 5 | 20.0 | 53 | 93.0 | 4 | 7.0 | 0.092 |
| Provide preview | 25 | 100.0 | 0 | 0 | 13 | 22.8 | 44 | 77.2 | 0.005 † |
| Clear explanations | 9 | 36.0 | 16 | 64.0 | 41 | 71.9 | 16 | 28.1 | 0.002 * |
| Professional language | 17 | 68.0 | 8 | 32.0 | 40 | 70.2 | 17 | 29.8 | 0.520 |
| Unprofessional behaviors | 9 | 36.0 | 16 | 64.0 | 51 | 89.5 | 6 | 10.5 | 0.000 * |
| Vocal segregates | 22 | 88.0 | 3 | 12.0 | 23 | 40.4 | 34 | 59.6 | 0.000 * |
| Reflective listening | 9 | 36.0 | 16 | 64.0 | 26 | 45.6 | 31 | 54.4 | 0.286 |
| Open-ended questions | 2 | 8.0 | 23 | 92.0 | 30 | 52.6 | 27 | 47.4 | 0.000 * |
| Summarize next steps | 13 | 52.0 | 12 | 48.0 | 28 | 49.1 | 29 | 50.9 | 0.500 |
| Repeat instructions | 9 | 36.0 | 16 | 64.0 | 26 | 45.6 | 31 | 54.4 | 0.286 |
| Use empathy statements | 5 | 20.0 | 20 | 80.0 | 46 | 80.7 | 11 | 19.3 | 0.000 * |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sheats, M.K.; Hammond, S.; Kedrowicz, A.A. Analysis of Final Year Veterinary Students’ Telephone Communication Skills at a Veterinary Teaching Hospital. Vet. Sci. 2018, 5, 99. https://doi.org/10.3390/vetsci5040099
Sheats MK, Hammond S, Kedrowicz AA. Analysis of Final Year Veterinary Students’ Telephone Communication Skills at a Veterinary Teaching Hospital. Veterinary Sciences. 2018; 5(4):99. https://doi.org/10.3390/vetsci5040099
Chicago/Turabian StyleSheats, M. Katie, Sarah Hammond, and April A. Kedrowicz. 2018. "Analysis of Final Year Veterinary Students’ Telephone Communication Skills at a Veterinary Teaching Hospital" Veterinary Sciences 5, no. 4: 99. https://doi.org/10.3390/vetsci5040099
APA StyleSheats, M. K., Hammond, S., & Kedrowicz, A. A. (2018). Analysis of Final Year Veterinary Students’ Telephone Communication Skills at a Veterinary Teaching Hospital. Veterinary Sciences, 5(4), 99. https://doi.org/10.3390/vetsci5040099