Pharmacokinetics, Milk Residues, and Toxicological Evaluation of a Single High Dose of Meloxicam Administered at 30 mg/kg per os to Lactating Dairy Cattle
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Experimental Animals
2.2. Housing and Husbandry
2.3. Meloxicam Administration
2.4. Sample Collection
2.5. Milk Sample Preparation
2.6. Plasma Sample Preparation
2.7. Determination of Meloxicam Concentrations by LC-MS
2.8. Noncompartmental Pharmacokinetic Analysis
2.9. Statistical Analysis
3. Results
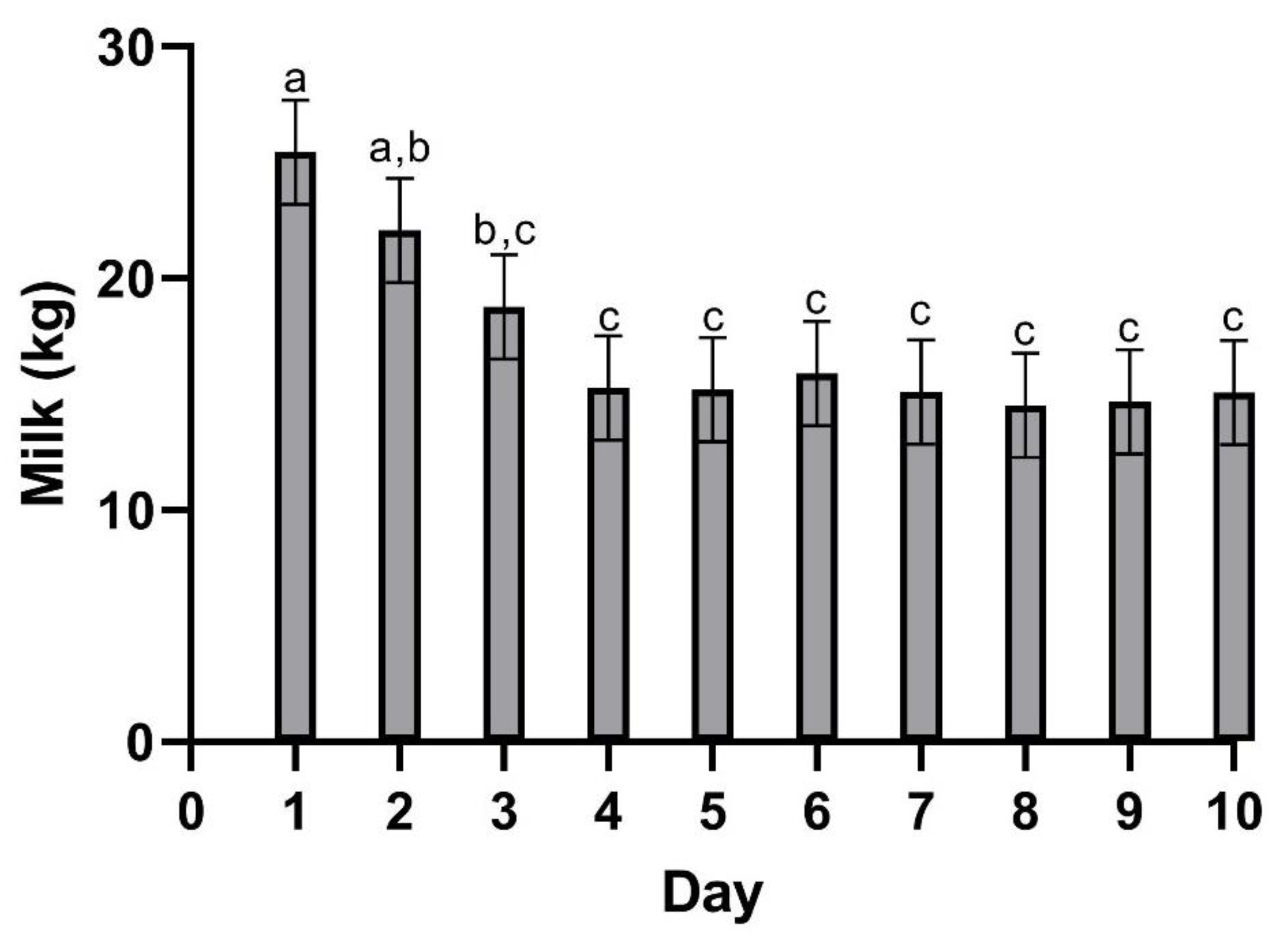
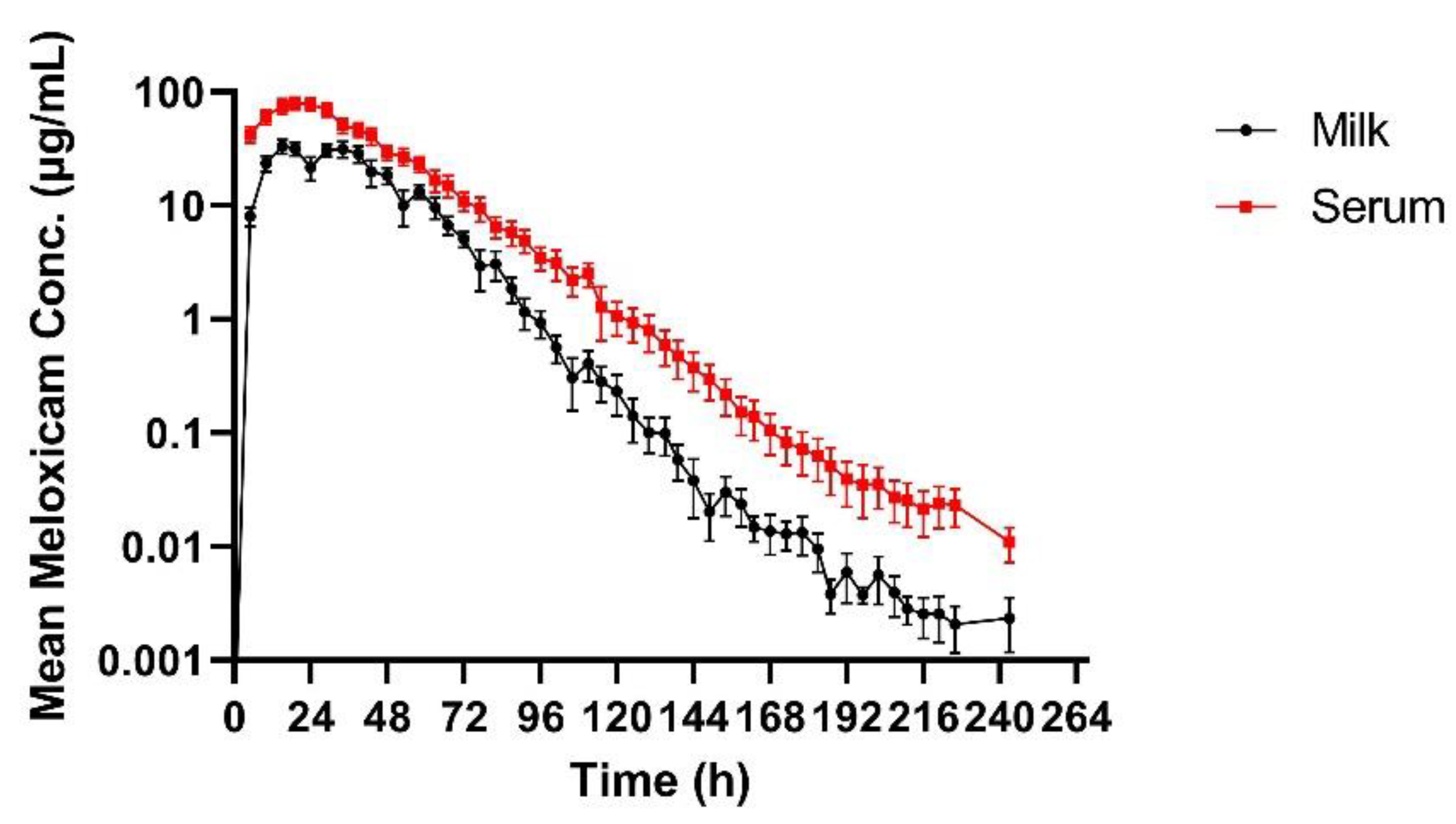
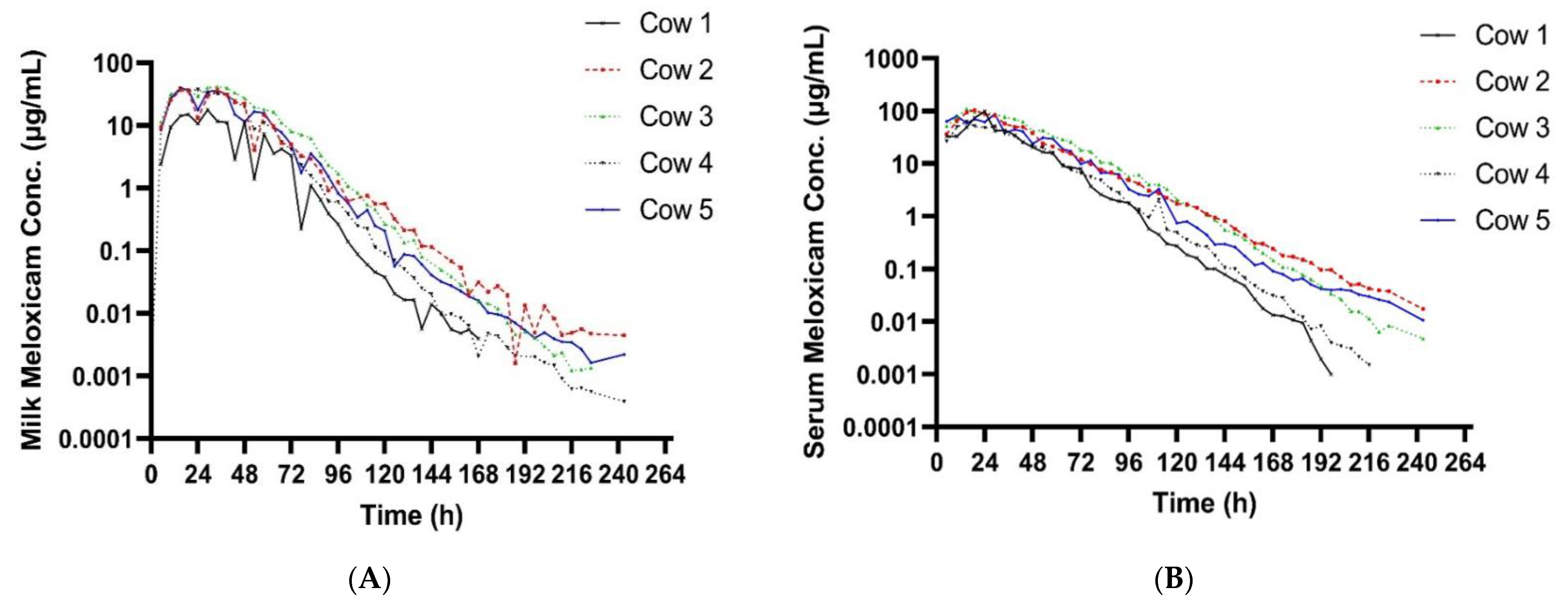
3.1. Milk
3.2. Plasma
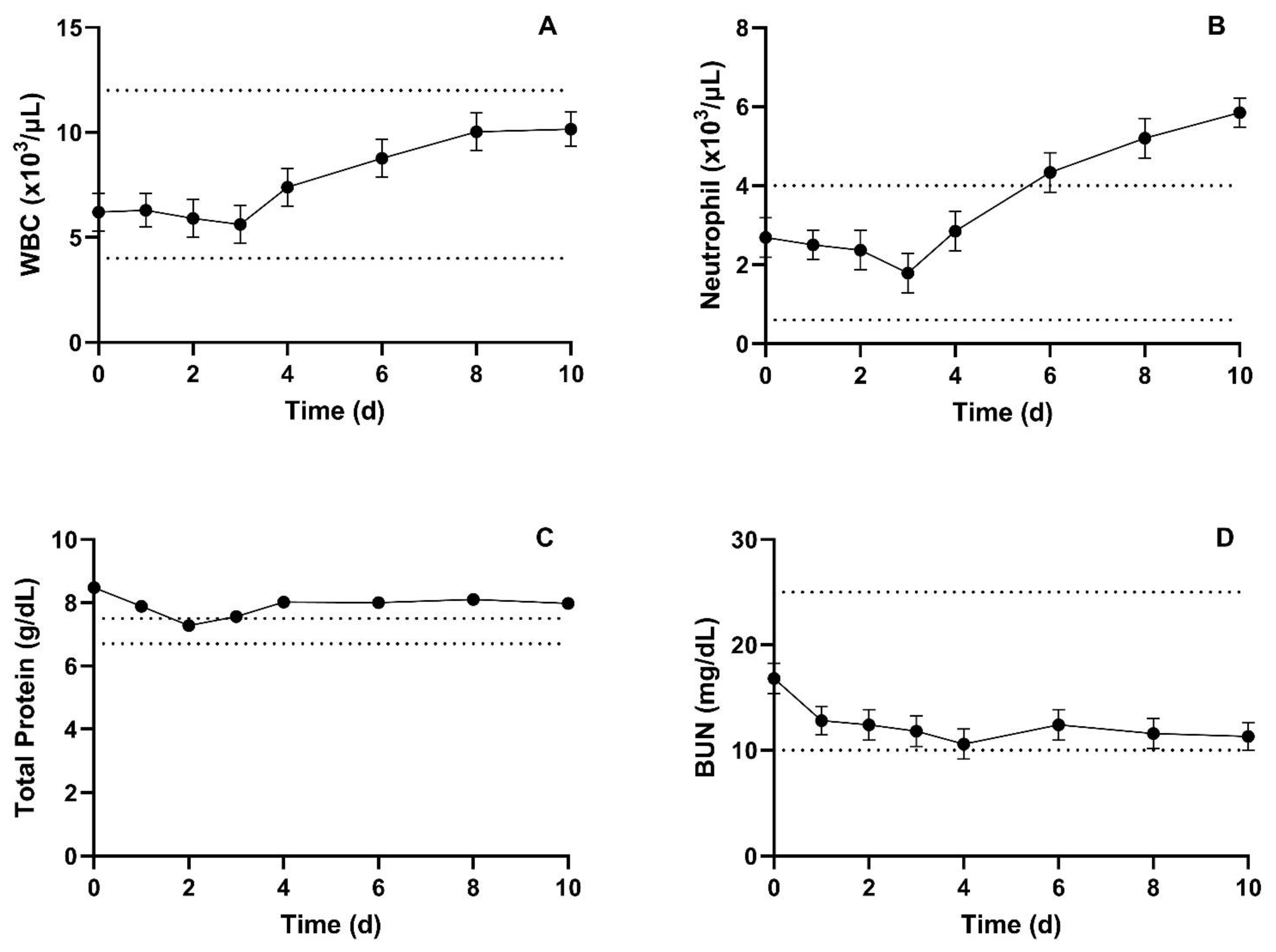
3.3. Complete Blood Counts and Blood Chemistry
3.4. Fecal Occult Blood
3.5. Urine Analysis
3.6. Necropsy Findings
3.7. Histological Examination
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- EMEA. Committee for Veterinary Medical Products: Meloxicam Summary Report (2); European Medicines Agency: Amsterdam, The Netherlands, 1999.
- Todd, C.G.; Millman, S.T.; McKnight, D.R.; Duffield, T.F.; Leslie, K.E. Nonsteroidal anti-inflammatory drug therapy for neonatal calf diarrhea complex: Effects on calf performance1. J. Anim. Sci. 2010, 88, 2019–2028. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Olson, M.E.; Ralston, B.; Burwash, L.; Matheson-Bird, H.; Allan, N.D. Efficacy of oral meloxicam suspension for prevention of pain and inflammation following band and surgical castration in calves. BMC Vet. Res. 2016, 12, 102. [Google Scholar] [CrossRef][Green Version]
- Barrier, A.C.; Coombs, T.M.; Dwyer, C.M.; Haskell, M.J.; Goby, L. Administration of a NSAID (meloxicam) affects lying behaviour after caesarean section in beef cows. Appl. Anim. Behav. Sci. 2014, 155, 28–33. [Google Scholar] [CrossRef]
- Robles, I.; Arruda, A.G.; Nixon, E.; Johnstone, E.; Wagner, B.; Edwards-Callaway, L.; Baynes, R.; Coetzee, J.; Pairis-Garcia, M. Producer and Veterinarian Perspectives towards Pain Management Practices in the US Cattle Industry. Animals 2021, 11, 209. [Google Scholar] [CrossRef]
- Lees, P. Analgesic, Antiinflammatory, Antipyretic Drugs. In Veterinary Pharmacology and Therapeutics, 9th ed.; Jim, E., Riviere, M.G.P., Eds.; Blackwell Publishing: Hoboken, NJ, USA, 2009; pp. 457–492. [Google Scholar]
- Kim, J.; Cannon, B.A.; Freeman, L.E.; Tan, S.; Knych, H.K.; Kendall, L.V. High-dose Meloxicam Provides Improved Analgesia in Female CD1 Mice: A Pharmacokinetic and Efficacy Study. J. Am. Assoc. Lab. Anim. Sci. 2023, 62, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Kendall, L.V.; Bailey, A.L.; Singh, B.; McGee, W. Toxic Effects of High-dose Meloxicam and Carprofen on Female CD1 Mice. J. Am. Assoc. Lab. Anim. Sci. 2022, 61, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Sarfaty, A.E.; Zeiss, C.J.; Willis, A.D.; Harris, J.M.; Smith, P.C. Concentration-dependent Toxicity after Subcutaneous Administration of Meloxicam to C57BL/6N Mice (Mus musculus). J. Am. Assoc. Lab. Anim. Sci. 2019, 58, 802–809. [Google Scholar] [CrossRef]
- Bharani, S.P.; Naik, A.K.; Parija, S.C.; Panda, S.K. Meloxicam induced toxicopathology studies in Wistar rats. Indian J. Anim. Res. 2020, 54, 363–366. [Google Scholar] [CrossRef]
- Ingrao, J.C.; Johnson, R.; Tor, E.; Gu, Y.; Litman, M.; Turner, P.V. Aqueous stability and oral pharmacokinetics of meloxicam and carprofen in male C57BL/6 mice. J. Am. Assoc. Lab. Anim. Sci. 2013, 52, 553–559. [Google Scholar]
- Summa, N.M.; Guzman, D.S.; Larrat, S.; Troncy, E.; Bird, D.M.; Lair, S.; Fitzgerald, G. Evaluation of High Dosages of Oral Meloxicam in American Kestrels (Falco sparverius). J. Avian. Med. Surg. 2017, 31, 108–116. [Google Scholar] [CrossRef]
- Waelchli, R.O.; Thun, R.; Stocker, H. Effect of flunixin meglumine on placental expulsion in dairy cattle after a caesarean. Vet. Rec. 1999, 144, 702–703. [Google Scholar] [CrossRef] [PubMed]
- Newby, N.C.; Renaud, D.; Tremblay, R.; Duffield, T.F. Evaluation of the effects of treating dairy cows with meloxicam at calving on retained fetal membranes risk. Can. Vet. J. 2014, 55, 1196–1199. [Google Scholar] [PubMed]
- Hirsch, A.C.; Philipp, H. Effects of meloxicam on reproduction parameters in dairy cattle. J. Vet. Pharmacol. Ther. 2009, 32, 566–570. [Google Scholar] [CrossRef]
- Bates, J.L. Transmammary-Delivered Meloxicam in Piglets Undergoing Castration and Tail Docking: Impact on Pharmacokinetics and Pain Biomarkers. Master’s Thesis, Iowa State University, Ames, IA, USA, 2015. [Google Scholar]
- McLean, M.K.; Khan, S.A. Toxicology of Frequently Encountered Nonsteroidal Anti-inflammatory Drugs in Dogs and Cats: An Update. Vet. Clin. Small Anim. Pract. 2018, 48, 969–984. [Google Scholar] [CrossRef] [PubMed]
- Bates, J.L.; Karriker, L.A.; Stock, M.L.; Pertzborn, K.M.; Baldwin, L.G.; Wulf, L.W.; Lee, C.J.; Wang, C.; Coetzee, J.F. Impact of transmammary-delivered meloxicam on biomarkers of pain and distress in piglets after castration and tail docking. PLoS ONE 2014, 9, e113678. [Google Scholar] [CrossRef] [PubMed]
- Gorden, P.J.; Burchard, M.; Ydstie, J.A.; Kleinhenz, M.D.; Wulf, L.W.; Rajewski, S.J.; Wang, C.; Gehring, R.; Mochel, J.P.; Coetzee, J.F. Comparison of milk and plasma pharmacokinetics of meloxicam in postpartum versus mid-lactation Holstein cows. J. Vet. Pharmacol. Ther. 2018, 41, 463–468. [Google Scholar] [CrossRef]
- Malreddy, P.R.; Coetzee, J.F.; Kukanich, B.; Gehring, R. Pharmacokinetics and milk secretion of gabapentin and meloxicam co-administered orally in Holstein-Friesian cows. J. Vet. Pharmacol. Ther. 2013, 36, 14–20. [Google Scholar] [CrossRef][Green Version]
- Coetzee, J.F.; KuKanich, B.; Mosher, R.; Allen, P.S. Pharmacokinetics of intravenous and oral meloxicam in ruminant calves. Vet. Ther. 2009, 10, E1–E8. [Google Scholar]
- Warner, R.; Ydstie, J.A.; Wulf, L.W.; Gehring, R.; Coetzee, J.F.; Mochel, J.P.; Gorden, P.J. Comparative Pharmacokinetics of Meloxicam Between Healthy Post-partum vs. Mid-lactation Dairy Cattle. Front. Vet. Sci. 2020, 7, 548. [Google Scholar] [CrossRef]
- Shock, D.; Roche, S.; Olson, M. A Comparative Pharmacokinetic Analysis of Oral and Subcutaneous Meloxicam Administered to Postpartum Dairy Cows. Vet. Sci. 2019, 6, 73. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Igarza, L.; Soraci, A.; Auza, N.; Zeballos, H. Some Pharmacokinetic Parameters of R-(-)- and S-(+)-Ketoprofen: The Influence of Age and Differing Physiological Status in Dairy Cattle. Vet. Res. Commun. 2004, 28, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Volner, Z.; Nouws, J.F.; Kozjek, F.; van Ginneken, C.A.; Primozic, S. Age-dependent pharmacokinetics of phenylbutazone in calves. Vet. Q. 1990, 12, 98–102. [Google Scholar] [CrossRef]
- Kissell, L.W.; Brinson, P.D.; Gehring, R.; Tell, L.A.; Wetzlich, S.E.; Baynes, R.E.; Riviere, J.E.; Smith, G.W. Pharmacokinetics and tissue elimination of flunixin in veal calves. Am. J. Vet. Res. 2016, 77, 634–640. [Google Scholar] [CrossRef][Green Version]
- Roder, J.D. Analgesics. In Clinical Veterinary Toxicology; Plumlee, K.H., Ed.; Mosby: St. Louis, MO, USA, 2004; pp. 282–284. [Google Scholar]
- Beasely, V. Analgesic Nephropathy in Nephrotoxic Organic Compounds. In Veterinary Toxicology; International Veterinary Information Service: Ithaca, NY, USA, 1999. [Google Scholar]
- Lehmann, H.A.; Baumeister, M.; Lützen, L.; Wiegleb, J. Meloxicam: A toxicology overview. Inflammopharmacology 1996, 4, 105–123. [Google Scholar] [CrossRef]
- Walton, S.; Ryan, K.A.; Davis, J.L.; Acierno, M. Treatment of meloxicam overdose in a dog via therapeutic plasma exchange. J. Vet. Emerg. Crit. Care 2017, 27, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Kreuder, A.J.; Coetzee, J.F.; Wulf, L.W.; Schleining, J.A.; KuKanich, B.; Layman, L.L.; Plummer, P.J. Bioavailability and pharmacokinetics of oral meloxicam in llamas. BMC Vet. Res. 2012, 8, 85. [Google Scholar] [CrossRef] [PubMed][Green Version]
| Study Day | −1 | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Catheter | X | |||||||||||
| Drug administration | X | |||||||||||
| CBC/Chem | X | X | X | X | X | X | X | X | X | X | X | X |
| Plasma Drug | X | X | X | X | X | X | X | X | X | X | X | |
| Milk Drug | X | X | X | X | X | X | X | X | X | X | X | |
| Physical Exam | X | X | X | X | X | X | X | X | X | X | X | X |
| Urinalysis | X | X | X | X | X | X | X | X | X | X | X | X |
| Fecal blood | X | X | X | X | X | X | X | X | X | X | X | X |
| Euthanasia | X |
| Parameter | Unit | Mean | SD | Median | Range |
|---|---|---|---|---|---|
| λz | 1/h | 0.060 | 1.130 | 0.060 | 0.05–0.07 |
| λz-HL | h | 12.230 | 1.130 | 11.600 | 10.59–14.40 |
| AUC0-last | h × µg/mL | 1360.71 | 1.580 | 1553.23 | 621.102–2035.769 |
| AUC0-∞ | h × µg/mL | 1360.77 | 1.580 | 1553.28 | 621.162–2035.791 |
| AUCextrap | % | 0.002 | 3.590 | 0.003 | 0.0004–0.01 |
| Cmax | µg/mL | 33.4 | 1.43 | 39.0 | 17.704–41.393 |
| Tmax | h | 23.740 | 1.530 | 29.000 | 15–34 |
| Parameter | Unit | Mean | SD | Median | Range |
|---|---|---|---|---|---|
| λz | 1/h | 0.050 | 1.204 | 0.052 | 0.04–0.061 |
| λz-HL | h | 13.79 | 1.20 | 13.41 | 11.328–17.422 |
| Tmax | h | 19.71 | 1.34 | 19.00 | 15–29 |
| Cmax | µg/mL | 91.061 | 1.248 | 98.164 | 63.10–110.578 |
| CL/F | mL/h/kg | 9.09 | 1.3 | 8.5 | 6.283–12.716 |
| AUC0–∞ AUClast | h × µg/mL h × µg/mL | 3301.30 3301.16 | 1.342 1.342 | 3509.40 3509.16 | 2359.279–4775.071 2359.278–4774.979 |
| AUC extrap | % | 0.001 | 8.646 | 0.002 | 0–0.011 |
| AUMC0–∞ | h2 × µg/mL | 109,842.0 | 1.4 | 117,505 | 75,845–172,426 |
| MRT0–∞ | h | 33.27 | 1.07 | 33.48 | 30.515–36.11 |
| Vz/F | ml/kg | 181 | 1 | 194 | 121.542–217.102 |
| Parameter | Days after Meloxicam Administration at 30 mg/kg PO | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| (Ref Range) | Baseline | 1 | 2 | 3 | 4 | 6 | 8 | 10 | p-Value |
| WBC × 103/uL (4–12) | 6.20 c (0.90) | 6.29 c (0.81) | 5.9 c (0.89) | 5.62 c (0.89) | 7.39 bc (0.89) | 8.77 ab (0.89) | 10.03 a (0.89) | 10.16 a (0.90) | <0.001 |
| RBC × 106/uL (5–10) | 6.40 a (0.25) | 5.57 b (0.24) | 5.34 b (0.25) | 5.48 b (0.25) | 5.66 b (0.25) | 5.55 b (0.25) | 5.6 b (0.25) | 5.49 b (0.24) | 0.26 |
| Hemoglobin g/dL (5–15) | 11.98 a (0.61) | 9.97 b (0.58) | 9.66 b (0.61) | 9.8 b (0.61) | 10.2 b (0.61) | 10.02 b (0.61) | 10.24 b (0.61) | 9.73 b (0.58) | 0.30 |
| Hematocrit % (24–46) | 32.9 a (1.64) | 27.33 b (1.57) | 26.34 b (1.64) | 27.12 b (1.64) | 27.88 b (1.64) | 27.40 b (1.64) | 27.64 b (1.64) | 27.01 b (1.57) | 0.29 |
| MCV fl (40–60) | 51.20 a (1.62) | 49.04 a (1.56) | 49.26 a (1.62) | 49.36 a (1.62) | 49.16 a (1.62) | 49.3 a (1.62) | 49.28 a (1.62) | 49.26 a (1.56) | 0.99 |
| MCH pg (11–17) | * 18.60 a (0.61) | * 17.91 a (0.58) | * 18.06 a (0.61) | * 17.88 a (0.61) | * 18.00 a (0.61) | * 18.02 a (0.61) | * 18.26 a (0.61) | * 17.75 a (0.58) | 0.99 |
| MCHC g/dL (30–36) | * 36.38 ab (0.28) | * 36.56 ab (0.23) | * 36.68 ab (0.28) | * 36.22 ab (0.28) | * 36.58 ab (0.28) | * 36.58 ab (0.28) | * 37.04 a (0.28) | * 36.02 b (0.23) | 0.04 |
| Platelets × 103/uL (100–800) | 472.4 ab (44.34) | 450.9 ab (41.99) | 419.6 b (44.34) | 435.8 ab (44.34) | 492.8 ab (44.34) | 452.2 ab (44.34) | 494.4 ab (44.34) | 511.4 a (41.99) | 0.78 |
| Neutrophils × 103/uL (0.6–4.0) | 2.69 bc (0.50) | 2.5 bc (0.37) | 2.37 bc (0.50) | 1.79 c (0.50) | 2.85 bc (0.50) | * 4.34 ab (0.50) | * 5.20 a (0.50) | * 5.85 a (0.37) | <0.001 |
| Lymphocytes × 103/uL (2.5–7.5) | 2.74 b (0.75) | 3.22 ab (0.73) | 2.81 b (0.75) | 3.12 ab (0.75) | 3.84 ab (0.75) | 3.49 ab (0.75) | 4.00 a (0.75) | 3.49 ab (0.73) | 0.98 |
| Monocytes × 103/uL (0.03–0.85) | 0.348 a (0.07) | 0.165 a (0.05) | 0.156 a (0.07) | 0.218 a (0.07) | 0.216 a (0.07) | 0.308 a (0.07) | 0.368 a (0.07) | 0.294 a (0.05) | 0.24 |
| Eosinophils × 103/uL (0.0–2.4) | 0.338 a (0.18) | 0.374 a (0.16) | 0.506 a (0.18) | 0.298 a (0.18) | 0.420 a (0.18) | 0.598 a (0.18) | 0.418 a (0.18) | 0.388 a (0.16) | 0.96 |
| Basophils × 103/uL (0.0–0.2) | 0.082 a (0.07) | 0.021 a (0.05) | 0.050 a (0.07) | 0.024 a (0.07) | 0.058 a (0.07) | 0.012 a (0.07) | 0.054 a (0.07) | * 0.221 a (0.05) | 0.02 |
| RDW % (8–15) | * 17.78 a (0.47) | * 17.63 a (0.46) | * 17.52 a (0.47) | * 17.44 a (0.47) | * 17.34 a (0.47) | * 17.5 a (0.47) | * 17.52 a (0.47) | * 17.46 a (0.46) | 0.99 |
| Plasma Protein g/dL (6.9–7.7) | * 8.76 a (0.22) | * 8.33 abc (0.17) | 7.64 c (0.22) | * 7.86 bc (0.22) | * 8.48 abc (0.22) | * 8.32 abc (0.22) | * 8.6 ab (0.22) | * 8.63 ab (0.17) | 0.02 |
| Fibrinogen mg/dL (100–500) | * 540 ab (77.82) | 490 b (64.60) | 440 b (77.82) | 460 b (77.82) | * 520 ab (77.82) | * 560 ab (77.82) | * 620 ab (77.82) | * 720 a (64.60) | 0.12 |
| Parameter | Days after Meloxicam Administration at 30 mg/kg PO | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| (Ref. Range) | Baseline | 1 | 2 | 3 | 4 | 6 | 8 | 10 | p-Value |
| Sodium mEq/L (132–152) | 142 a (0.92) | 140 a (0.75) | 140.2 a (0.92) | 139.6 a (0.92) | 141.4 a (0.92) | 140.6 a (0.92) | 140.6 a (0.92) | 140.5 a (0.75) | 0.21 |
| Potassium mEq/L (3.9–5.8) | 4.5 a (0.12) | 3.96 bc (0.09) | * 3.8 c (0.12) | 3.94 bc (0.12) | 4.2 abc (0.12) | 4.22 abc (0.12) | 4.36 ab (0.12) | 4.28 ab (0.09) | 0.01 |
| Chloride mEq/L (100–115) | 100.6 b (1.40) | 102.8 ab (1.22) | 105.2 a (1.40) | 103.8 ab (1.40) | 102 ab (1.40) | 102.2 ab (1.40) | 101.2 ab (1.40) | 102.8 ab (1.22) | 0.60 |
| Bicarbonate mEq/L (21–31) | 29 a (1.13) | 28.5 a (0.87) | 26.8 a (1.13) | 27.2 a (1.13) | *31.2 a (1.13) | 30 a (1.13) | 29.4 a (1.13) | 29.5 a (0.87) | 0.18 |
| Calcium mg/dL (8.0–11.4) | 9.14 ab (0.27) | 8.98 ab (0.22) | 8.44 b (0.27) | 8.78 ab (0.27) | 9.64 a (0.27) | 9.06 ab (0.27) | 9.4 ab (0.27) | 9.52 a (0.22) | 0.06 |
| Phosphorus mg/dL (5.6–8.0) | 6.88 a (0.68) | 7.21 a (0.47) | 7.66 a (0.68) | 6.18 a (0.68) | 6.38 a (0.68) | 6.34 a (0.68) | 5.82 a (0.68) | 5.75 a (0.47) | 0.15 |
| BUN mg/dL (10–25) | 16.8 a (1.45) | 12.8 b (1.33) | 12.4 b (1.45) | 11.8 b (1.45) | 10.6 b (1.45) | 12.4 b (1.45) | 11.6 b (1.45) | 11.3 b (1.33) | 0.19 |
| Creatinine mg/dL (0.1–1.8) | 1.38 a (0.14) | 1.21 b (0.13) | 1.14 b (0.14) | 1.12 b (0.14) | 1.14 b (0.14) | 1.14 b (0.14) | 1.2 ab (0.14) | 1.16 b (0.13) | 0.97 |
| Glucose md/dL (40–100) | 70.4 ab (3.95) | 72.2 a (3.48) | 63.6 ab (3.95) | 65.4 ab (3.95) | 64 ab (3.95) | 62.4 ab (3.95) | 59.6 b (3.95) | 67.6 ab (3.48) | 0.30 |
| Total Protein g/dL (6.7–7.5) | * 8.48 a (0.16) | * 7.89 ab (0.12) | 7.28 c (0.16) | * 7.56 bc (0.16) | * 8.02 ab (0.16) | * 8.00 ab (0.16) | * 8.10 ab (0.16) | * 7.98 ab (0.12) | 0.002 |
| Albumin g/dL (2.5–3.8) | 3.38 a (0.10) | 2.93 bc (0.09) | 2.66 c (0.10) | 2.72 bc (0.10) | 2.94 bc (0.10) | 2.9 bc (0.10) | 2.98 b (0.10) | 2.9 bc (0.09) | 0.003 |
| AST U/L (55–125) | 98.8 a (11.74) | 95.3 a (10.53) | 76.2 a (11.74) | 83.8 a (11.74) | 90.6 a (11.74) | 84.6 a (11.74) | 82.8 a (11.74) | 74.6 a (10.53) | 0.71 |
| CK U/L (1–350) | 265.8 a (121) | 327.7 a (99) | 258.8 a (121) | 248 a (121) | 98 a (121) | 91.6 a (121) | 81.4 a (121) | 64.7 a (99) | 0.55 |
| ALP U/L (25–250) | 104.4 a (16.95) | 78 ab (15.86) | 63.8 b (16.95) | 65 b (16.95) | 72 ab (16.95) | 64.6 b (16.95) | 72.8 ab (16.95) | 60.3 b (15.86) | 0.7 |
| GGT U/L (1–50) | * 57.4 ab (8.59) | * 58.1 a (8.46) | * 50.6 ab (8.59) | 49.4 b (8.59) | * 55.8 ab (8.59) | * 54.4 ab (8.59) | * 56 ab (8.59) | * 52.4 ab (8.46) | 0.99 |
| Total Bilirubin mg/dL (0.1–1.6) | 0.42 a (0.04) | 0.338 ab (0.03) | 0.146 c (0.04) | 0.186 c (0.04) | 0.222 bc (0.04) | 0.274 abc (0.04) | 0.284 abc (0.04) | 0.291 abc (0.03) | 0.001 |
| Anion Gap (14–21) | 17 a (0.96) | * 12.7 b (0.71) | * 12.2 b (0.96) | * 12.6 b (0.96) | * 12.4 b (0.96) | * 12.6 b (0.96) | 14.4 ab (0.96) | * 12.4 b (0.71) | 0.01 |
| Lipemic Indice | 20 a (0) | 20 a (0) | 20 a (0) | 20 a (0) | 20 a (0) | 20 a (0) | 20 a (0) | 20 a (0) | |
| Hemolytic Indice | 32 a (3.94) | 22.3 ab (2.72) | 18.2 ab (3.94) | 15 ab (3.94) | 18.6 ab (3.94) | 15.8 ab (3.94) | 17.8 ab (3.94) | 15.1 b (2.72) | 0.01 |
| Icteric Indice | 3.8 a (0.15) | 3.5 ab (0.12) | 2.8 c (0.15) | 2.8 c (0.15) | 3 bc (0.15) | 3 bc (0.15) | 3 bc (0.15) | 3 bc (0.12) | |
| Animal ID | Parameter | Baseline | 1 | 2 | 3 | 4 | 6 | 8 | 10 |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Sp. Gravity | 1.034 | 1.04 | 1.046 | 1.047 | 1.042 | 1.036 | 1.038 | 1.032 |
| pH | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | |
| Protein | 3 | 3 | 3 | 3 | 1 | 1 | 2 | 2 | |
| Leukocytes | 1 | 1 | 1 | 0.5 | 1 | 0.5 | 0.5 | 1 | |
| 2 | Sp. Gravity | 1.013 | 1.021 | N/A | 1.023 | 1.02 | 1.016 | 1.015 | 1.015 |
| pH | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | |
| Protein | 1 | 1 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | |
| Leukocytes | 0 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | |
| 3 | Sp. Gravity | 1.035 | 1.03 | 1.044 | 1.05 | 1.046 | 1.031 | 1.027 | 1.025 |
| pH | 8.5 | 8 | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | |
| Protein | 0.5 | 0.5 | 1 | 0.5 | 1 | 2 | 0.5 | 0.5 | |
| Leukocytes | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | |
| 4 | Sp. Gravity | 1.026 | 1.045 | 1.043 | 1.037 | 1.036 | 1.027 | 1.029 | 1.028 |
| pH | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | |
| Protein | 1 | 1 | 0.5 | 3 | 1 | 1 | 1 | 1 | |
| Leukocytes | 1 | 1 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | |
| 5 | Sp. Gravity | 1.039 | 1.03 | 1.039 | 1.04 | 1.03 | 1.037 | 1.03 | 1.027 |
| pH | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | 8.5 | |
| Protein | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Leukocytes | 1 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fritz, S.A.; Ensley, S.M.; Lawrence, J.R.; Van Engen, N.; Lin, Z.; Kleinhenz, M.D.; Wulf, L.W.; Rice, S.; Gorden, P.J.; Peterson, J.; et al. Pharmacokinetics, Milk Residues, and Toxicological Evaluation of a Single High Dose of Meloxicam Administered at 30 mg/kg per os to Lactating Dairy Cattle. Vet. Sci. 2023, 10, 301. https://doi.org/10.3390/vetsci10040301
Fritz SA, Ensley SM, Lawrence JR, Van Engen N, Lin Z, Kleinhenz MD, Wulf LW, Rice S, Gorden PJ, Peterson J, et al. Pharmacokinetics, Milk Residues, and Toxicological Evaluation of a Single High Dose of Meloxicam Administered at 30 mg/kg per os to Lactating Dairy Cattle. Veterinary Sciences. 2023; 10(4):301. https://doi.org/10.3390/vetsci10040301
Chicago/Turabian StyleFritz, Scott A., Steve M. Ensley, Jay R. Lawrence, Nicholas Van Engen, Zhoumeng Lin, Michael D. Kleinhenz, Larry W. Wulf, Somchai Rice, Patrick J. Gorden, Jackie Peterson, and et al. 2023. "Pharmacokinetics, Milk Residues, and Toxicological Evaluation of a Single High Dose of Meloxicam Administered at 30 mg/kg per os to Lactating Dairy Cattle" Veterinary Sciences 10, no. 4: 301. https://doi.org/10.3390/vetsci10040301
APA StyleFritz, S. A., Ensley, S. M., Lawrence, J. R., Van Engen, N., Lin, Z., Kleinhenz, M. D., Wulf, L. W., Rice, S., Gorden, P. J., Peterson, J., & Coetzee, J. F. (2023). Pharmacokinetics, Milk Residues, and Toxicological Evaluation of a Single High Dose of Meloxicam Administered at 30 mg/kg per os to Lactating Dairy Cattle. Veterinary Sciences, 10(4), 301. https://doi.org/10.3390/vetsci10040301








