Cardiovascular Effect of Epoprostenol and Intravenous Cardiac Drugs for Acute Heart Failure on Canine Pulmonary Hypertension
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Study Protocol
2.3. Right Heart Catheterization
2.4. Echocardiography
2.5. Statistical Analysis
3. Results
3.1. Epoprostenol Administration
3.2. Dobutamine Administration
3.3. Dopamine Administration
3.4. Pimobendan Administration
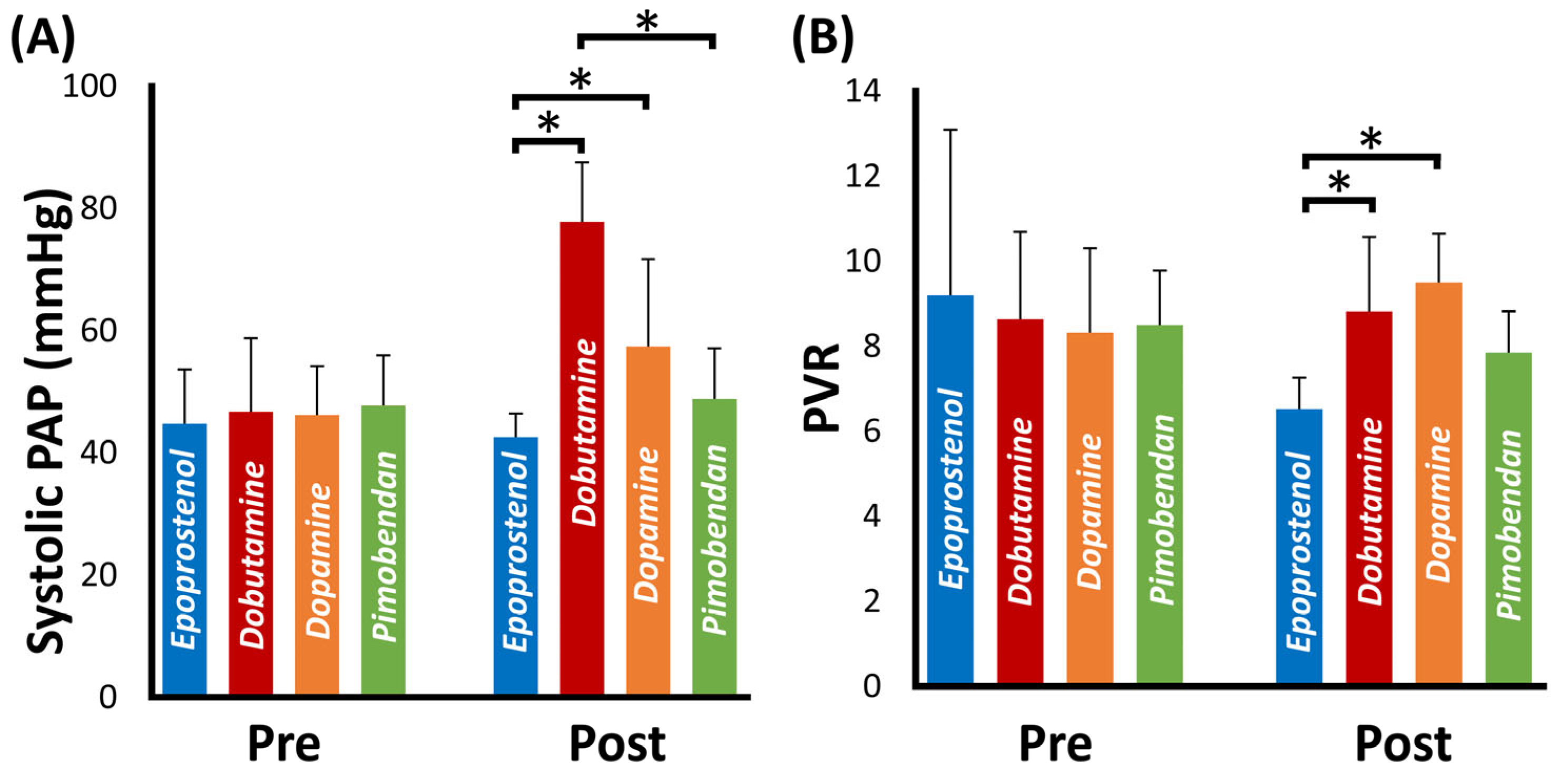
3.5. Comparison of the Hemodynamical Effect of Each Cardiac Drug
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Reinero, C.; Visser, L.C.; Kellihan, H.B.; Masseau, I.; Rozanski, E.; Clercx, C.; Williams, K.; Abbott, J.A.; Borgarelli, M.; Scansen, B.A. ACVIM Consensus Statement Guidelines for the Diagnosis, Classification, Treatment, and Monitoring of Pulmonary Hypertension in Dogs. J. Vet. Intern. Med. 2020, 34, 549–573. [Google Scholar] [CrossRef]
- Johnson, L.; Boon, J.; Orton, E.C. Clinical Characteristics of 53 Dogs with Doppler-Derived Evidence of Pulmonary Hypertension: 1992–1996. J. Vet. Intern. Med. 1999, 13, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Borgarelli, M.; Abbott, J.A.; Braz-Ruivo, L.; Chiavegato, D.; Crosara, S.; Lamb, K.; Ljungvall, I.; Poggi, M.; Santilli, R.A.; Haggstrom, J. Prevalence and Prognostic Importance of Pulmonary Hypertension in Dogs with Myxomatous Mitral Valve Disease. J. Vet. Intern. Med. 2015, 29, 569–574. [Google Scholar] [CrossRef]
- Jaffey, J.A.; Wiggen, K.; Leach, S.B.; Masseau, I.; Girens, R.E.; Reinero, C.R. Pulmonary Hypertension Secondary to Respiratory Disease and/or Hypoxia in Dogs: Clinical Features, Diagnostic Testing and Survival. Vet. J. 2019, 251, 105347. [Google Scholar] [CrossRef] [PubMed]
- Morita, T.; Nakamura, K.; Osuga, T.; Kawamoto, S.; Miki, S.; Sasaoka, K.; Takiguchi, M. Acute Effects of Intravenous Pimobendan Administration in Dog Models of Chronic Precapillary Pulmonary Hypertension. J. Vet. Cardiol. 2020, 32, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Enokizono, M.; Mandour, A.S.; Komeda, S.; Goya, S.; Takeuchi, A.; Katoh, K.; Yairo, A.; Yilmaz, Z.; Shimada, K.; Tanaka, R. Hemodynamic Effect of Pimobendan Following Intramuscular and Intravenous Administration in Healthy Dogs: A Pilot Study. Front. Vet. Sci. 2022, 9, 1422. [Google Scholar] [CrossRef]
- Galiè, N.; Humbert, M.; Vachiery, J.L.; Gibbs, S.; Lang, I.; Torbicki, A.; Simonneau, G.; Peacock, A.; Vonk Noordegraaf, A.; Beghetti, M.; et al. 2015 ESC/ERS Guidelines for the Diagnosis and Treatment of Pulmonary Hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endor. Eur. Heart J. 2016, 37, 67–119. [Google Scholar] [CrossRef] [PubMed]
- Degering, J.; Egenlauf, B.; Harutyunova, S.; Benjamin, N.; Salkić, A.; Xanthouli, P.; Eichstaedt, C.A.; Seeger, R.; Sitbon, O.; Grünig, E. Tolerability, Safety and Survival in Patients with Severe Pulmonary Arterial Hypertension Treated with Intravenous Epoprostenol (Veletri®): A Prospective, 6-Months, Open Label, Observational, Non-Interventional Study. Respir. Res. 2023, 24, 18. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, C.; Amar, D.; Boucly, A.; Savale, L.; Jaïs, X.; Chaumais, M.C.; Montani, D.; Humbert, M.; Simonneau, G.; Sitbon, O. Comparative Safety and Tolerability of Prostacyclins in Pulmonary Hypertension. Drug Saf. 2016, 39, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Koh, E.; Morimoto, S.; Jiang, B.; Inoue, T.; Nabata, T.; Kitano, S.; Yasuda, O.; Fukuo, K.; Ogihara, T. Effects of Beraprost Sodium, a Stable Analogue of Prostacyclin, on Hyperplasia, Hypertrophy and Glycosaminoglycan Synthesis of Rat Aortic Smooth Muscle Cells. Artery 1993, 20, 242–252. [Google Scholar] [PubMed]
- Nishio, S.; Matsuura, H.; Kanai, N.; Fukatsu, Y.; Hirano, T.; Nishikawa, N.; Kameoka, K.; Umetsu, T. The In Vitro and Ex Vivo Antiplatelet Effect of TRK-100, a Stable Prostacyclin Analog, in Several Species. Jpn. J. Pharmacol. 1988, 47, 1–10. [Google Scholar] [CrossRef]
- Akiba, T.; Miyazaki, M.; Toda, N. Vasodilator Actions of TRK-100, a New Prostaglandin I2 Analogue. Br. J. Pharmacol. 1986, 89, 703–711. [Google Scholar] [CrossRef] [PubMed]
- Tamura, M.; Kurumatani, H.; Matsushita, T. Comparative Effects of Beraprost, a Stable Analogue of Prostacyclin, with PGE1, Nitroglycerin and Nifedipine on Canine Model of Vasoconstrictive Pulmonary Hypertension. Prostaglandins Leukot. Essent. Fat. Acids 2001, 64, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, R.; Yuchi, Y.; Saito, T.; Teshima, T.; Matsumoto, H.; Koyama, H. Investigation of Beraprost Sodium on Cardiac Function and Hemodynamics in Canine Models of Chronic Pulmonary Hypertension. Front. Vet. Sci. 2022, 9, 451. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, R.; Yuchi, Y.; Saito, T.; Yasumura, Y.; Teshima, T.; Matsumoto, H.; Koyama, H. Beraprost Sodium for Pulmonary Hypertension in Dogs: Effect on Hemodynamics and Cardiac Function. Animals 2022, 12, 2078. [Google Scholar] [CrossRef]
- Yuchi, Y.; Suzuki, R.; Kanno, H.; Teshima, T.; Matsumoto, H.; Koyama, H. Right Ventricular Myocardial Adaptation Assessed by Two-Dimensional Speckle Tracking Echocardiography in Canine Models of Chronic Pulmonary Hypertension. Front. Vet. Sci. 2021, 8, 727155. [Google Scholar] [CrossRef]
- Yoshida, T.; Mandour, A.S.; Matsuura, K.; Shimada, K.; El-Husseiny, H.M.; Hamabe, L.; Yilmaz, Z.; Uemura, A.; Tanaka, R. Changes in the Pulmonary Artery Wave Reflection in Dogs with Experimentally-Induced Acute Pulmonary Embolism and the Effect of Vasodilator. Animals 2021, 11, 1977. [Google Scholar] [CrossRef] [PubMed]
- Barst, R.J.; Rubin, L.J.; Long, W.A.; McGoon, M.D.; Rich, S.; Badesch, D.B.; Groves, B.M.; Tapson, V.F.; Bourge, R.C.; Brundage, B.H.; et al. A Comparison of Continuous Intravenous Epoprostenol (Prostacyclin) with Conventional Therapy for Primary Pulmonary Hypertension. N. Engl. J. Med. 1996, 334, 296–301. [Google Scholar] [CrossRef]
- Yoshida, T.; Matsuura, K.; Mandour, A.S.; Aboshi, Y.; Yamada, S.; Yotsuida, H.; Hasegawa, M.; Cheng, C.J.; Yaginuma, Y.; Watanabe, M.; et al. Hemodynamic Effects of Protamine Infusion in Dogs with Myxomatous Mitral Valve Disease Undergoing Mitral Valvuloplasty. Vet. Sci. 2022, 9, 178. [Google Scholar] [CrossRef]
- Schiller, N.B.; Shah, P.M.; Crawford, M.; DeMaria, A.; Devereux, R.; Feigenbaum, H.; Gutgesell, H.; Reichek, N.; Sahn, D.; Schnittger, I. Recommendations for Quantitation of the Left Ventricle by Two-Dimensional Echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J. Am. Soc. Echocardiogr. 1989, 2, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Scollan, K.F.; Stieger-Vanegas, S.M.; David Sisson, D. Assessment of Left Ventricular Volume and Function in Healthy Dogs by Use of One-, Two-, and Three-Dimensional Echocardiography versus Multidetector Computed Tomography. Am. J. Vet. Res. 2016, 77, 1211–1219. [Google Scholar] [CrossRef]
- Lewis, J.F.; Kuo, L.C.; Nelson, J.G.; Limacher, M.C.; Quinones, M.A. Pulsed Doppler Echocardiographic Determination of Stroke Volume and Cardiac Output: Clinical Validation of Two New Methods Using the Apical Window. Circulation 1984, 70, 425–431. [Google Scholar] [CrossRef]
- Gentile-Solomon, J.M.; Abbott, J.A. Conventional Echocardiographic Assessment of the Canine Right Heart: Reference Intervals and Repeatability. J. Vet. Cardiol. 2016, 18, 234–247. [Google Scholar] [CrossRef] [PubMed]
- Rudski, L.G.; Lai, W.W.; Afilalo, J.; Hua, L.; Handschumacher, M.D.; Chandrasekaran, K.; Solomon, S.D.; Louie, E.K.; Schiller, N.B. Guidelines for the Echocardiographic Assessment of the Right Heart in Adults: A Report from the American Society of Echocardiography Endorsed by the European Association of Echocardiography, a Registered Branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J. Am. Soc. Echocardiogr. 2010, 23, 685–713. [Google Scholar] [CrossRef]
- Yuchi, Y.; Suzuki, R.; Teshima, T.; Matsumoto, H.; Koyama, H. Utility of Tricuspid Annular Plane Systolic Excursion Normalized by Right Ventricular Size Indices in Dogs with Postcapillary Pulmonary Hypertension. J. Vet. Intern. Med. 2021, 35, 107–119. [Google Scholar] [CrossRef]
- Visser, L.C.; Sintov, D.J.; Oldach, M.S. Evaluation of Tricuspid Annular Plane Systolic Excursion Measured by Two-Dimensional Echocardiography in Healthy Dogs: Repeatability, Reference Intervals, and Comparison with M-Mode Assessment. J. Vet. Cardiol. 2018, 20, 165–174. [Google Scholar] [CrossRef] [PubMed]
- Visser, L.C.; Scansen, B.A.; Schober, K.E.; Bonagura, J.D. Echocardiographic Assessment of Right Ventricular Systolic Function in Conscious Healthy Dogs: Repeatability and Reference Intervals. J. Vet. Cardiol. 2015, 17, 83–96. [Google Scholar] [CrossRef] [PubMed]
- Acierno, M.J.; Brown, S.; Coleman, A.E.; Jepson, R.E.; Papich, M.; Stepien, R.L.; Syme, H.M. ACVIM Consensus Statement: Guidelines for the Identification, Evaluation, and Management of Systemic Hypertension in Dogs and Cats. J. Vet. Intern. Med. 2018, 32, 1803–1822. [Google Scholar] [CrossRef] [PubMed]
- Hamabe, L.; Shimada, K.; Mandour, A.S.; Yoshida, T.; Hirose, M.; Hendawy, H.; El-Husseiny, H.M.; Tanaka, R. Evaluation of Left Ventricular Function in Healthy Retrievers Using Standard and 2D Speckle-Tracking Echocardiography. Vet. Sci. 2022, 9, 529. [Google Scholar] [CrossRef] [PubMed]
- Yuchi, Y.; Suzuki, R.; Teshima, T.; Matsumoto, H.; Koyama, H. Right Ventricular Systolic and Diastolic Function Assessed by Two-Dimensional Speckle Tracking Echocardiography in Dogs with Myxomatous Mitral Valve Disease. J. Vet. Med. Sci. 2021, 83, 1918–1927. [Google Scholar] [CrossRef] [PubMed]
- Kanda, Y. Investigation of the Freely Available Easy-to-Use Software “EZR” for Medical Statistics. Bone Marrow Transpl. 2013, 48, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Kerbaul, F.; Rondelet, B.; Demester, J.P.; Fesler, P.; Huez, S.; Naeije, R.; Brimioulle, S. Effects of Levosimendan versus Dobutamine on Pressure Load-Induced Right Ventricular Failure. Crit. Care Med. 2006, 34, 2814–2819. [Google Scholar] [CrossRef]
| Variables | Baseline | Epoprostenol (ng/kg/min) | p * | ||||
|---|---|---|---|---|---|---|---|
| 2 | 5 | 10 | 15 | 20 | |||
| Mean PAWP (mmHg) | 7.2 ± 2.3 | 7.3 ± 1.9 | 6.9 ± 2.0 | 6.6 ± 2.0 | 6.6 ± 1.7 | 6.7 ± 1.9 | 0.72 |
| Systolic PAP (mmHg) | 44.8 ± 8.9 | 44.2 ± 10.1 | 45.9 ± 9.7 | 44.6 ± 9.6 | 43.2 ± 5.9 | 42.6 ± 3.9 | 0.14 |
| Mean PAP (mmHg) | 34 ± 8.8 | 33.9 ± 7.7 | 34.3 ± 7.8 | 35.6 ± 10.2 | 31.8 ± 5.5 | 31.5 ± 2.9 | 0.09 |
| Diastolic PAP (mmHg) | 24.8 ± 8.3 | 25.7 ± 6.7 | 25.2 ± 6.5 | 25.7 ± 7.7 | 22.7 ± 6.4 | 22.5 ± 4.2 | 0.12 |
| Systolic RVP (mmHg) | 46.4 ± 12.4 | 44.2 ± 12 | 43.5 ± 8.8 | 43.2 ± 9.4 | 42.8 ± 7 | 42.4 ± 7.3 | 0.02 |
| Diastolic RVP (mmHg) | 2.1 ± 1.4 | 1.7 ± 1.5 | 1.0 ± 1.9 | 0.8 ± 1.8 | 0.4 ± 1.9 | 1.2 ± 2.0 | 0.64 |
| RV dP/dtmax (mmHg/s) | 324 ± 52 | 340 ± 109 | 383 ± 94 | 384 ± 122 | 441 ± 103 a | 476 ± 119 a,b | 0.03 |
| RV dP/dtmin (mmHg/s) | −374 ± 61 | −359 ± 114 | −437 ± 144 | −424 ± 131 | −505 ± 173 | −540 ± 193 | 0.40 |
| RV CO (L/min/m2) | 2.7 ± 0.7 | 2.9 ± 0.9 | 3.2 ± 0.6 | 3.3 ± 0.6 | 3.7 ± 0.6 a | 3.8 ± 0.6 a,b,d | <0.01 |
| RV SV (mL/m2) | 31.6 ± 6.9 | 33.5 ± 6.5 | 35.2 ± 5.8 | 33.0 ± 4.1 | 34.8 ± 5.7 a,b | 33.9 ± 5.1 a,b,c | <0.01 |
| Systolic SAP (mmHg) | 108 ± 10 | 109 ± 13 | 100 ± 11 | 99 ± 10 | 100 ± 8 | 103 ± 12 | 0.64 |
| Mean SAP (mmHg) | 75 ± 10 | 73 ± 12 | 71 ± 9 | 69 ± 8 | 69 ± 7 | 72 ± 12 | 0.81 |
| PVR | 10.2 ± 3.9 | 9.7 ± 4.0 | 8.6 ± 2.4 | 8.7 ± 2.8 | 6.8 ± 1.4 a | 6.5 ± 0.7 a,b | <0.01 |
| SVR | 17.5 ± 3.6 | 16.6 ± 3.5 | 14.8 ± 1.7 | 13.4 ± 0.8 | 13.0 ± 1.4 c | 12.8 ± 2.5 a,c | <0.01 |
| LVEDVI (mL/m2) | 68.5 ± 10.7 | 70.3 ± 10.0 | 72.3 ± 12.9 | 71.8 ± 12.6 | 73.8 ± 10.2 | 71.4 ± 12.6 | 0.20 |
| LVESVI (mL/m2) | 37.6 ± 7.3 | 37.5 ± 6.2 | 39.7 ± 8.6 | 37.6 ± 9.3 | 36.3 ± 6.3 | 35.9 ± 7.4 | 0.39 |
| Ejection fraction (%) | 45.5 ± 3.5 | 46.6 ± 4.2 | 45.5 ± 2.6 | 48.2 ± 4.0 | 51.1 ± 2.5 a,c | 50.0 ± 3.5 a,c | 0.02 |
| LV SV (mL/m2) | 48.8 ± 7.3 | 48.2 ± 6.3 | 49.7 ± 6.6 | 50.6 ± 5.7 | 52.2 ± 4.2 | 53.8 ± 7.5 a,b,c | <0.01 |
| LV CO (L/min/m2) | 4.4 ± 1 | 4.6 ± 1.1 | 4.9 ± 0.8 | 5.2 ± 0.8 | 5.4 ± 0.7 | 5.7 ± 0.6 a,b,c | <0.01 |
| RVEDA index (cm2/kg0.624) | 1.5 ± 0.1 | 1.6 ± 0.2 | 1.6 ± 0.1 | 1.6 ± 0.1 | 1.6 ± 0.2 | 1.6 ± 0.1 | 0.13 |
| RVESA index (cm2/kg0.628) | 1.0 ± 0.1 | 1.1 ± 0.1 | 1.0 ± 0.1 | 1.0 ± 0.1 | 1.0 ± 0.1 | 1.0 ± 0.1 | 0.16 |
| RV FACn (%/kg−0.097) | 39.3 ± 4.4 | 40.1 ± 6.1 | 46.2 ± 3.8 | 47.3 ± 3.4 | 46.7 ± 2.9 | 49.4 ± 4.9 | <0.01 |
| TAPSEn (mm/kg0.284) | 4.5 ± 0.6 | 4.9 ± 1.2 | 5.2 ± 1.0 | 5.6 ± 0.9 | 5.7 ± 1.1 | 5.8 ± 0.8 a,b | <0.01 |
| LV-SL (%) | 12.1 ± 2.1 | 12.6 ± 2.1 | 12.7 ± 1.9 | 13.3 ± 2.2 | 13.6 ± 1.5 a | 14.5 ± 1.5 a,b,c | <0.01 |
| LV-SC (%) | 14.0 ± 1.8 | 14.6 ± 1.8 | 14.8 ± 2.3 | 15.3 ± 2.2 | 16.1 ± 1.5 a | 16.6 ± 2.4 a,b,c | <0.01 |
| RV-SL (%) | 17.5 ± 3.6 | 17.8 ± 3.2 | 19.3 ± 3.4 | 20.1 ± 3.2 | 21.2 ± 1.8 a,b | 22.5 ± 2.5 a,b | <0.01 |
| Variables | Baseline | Dobutamine (µg/kg/min) | p * | |
|---|---|---|---|---|
| 5 | 10 | |||
| Mean PAWP (mmHg) | 7.4 ± 1.9 | 6.9 ± 2.0 | 7.0 ± 1.6 | 0.14 |
| Systolic PAP (mmHg) | 46.8 ± 12.0 | 65.2 ± 12.3 a | 77.8 ± 9.8 a,b | <0.01 |
| Mean PAP (mmHg) | 35.2 ± 9.1 | 43.3 ± 11.6 a | 53.9 ± 7.6 a,b | <0.01 |
| Diastolic PAP (mmHg) | 25.5 ± 7.3 | 28.8 ± 11.0 | 38.6 ± 6.9 a,b | <0.01 |
| Systolic RVP (mmHg) | 46.8 ± 12.9 | 69.4 ± 19.1 a | 77.9 ± 16.4 a | <0.01 |
| Diastolic RVP (mmHg) | 4.1 ± 4.6 | 5.2 ± 5.6 | 4.2 ± 7.6 | 0.74 |
| RV dP/dtmax (mmHg/s) | 434 ± 96 | 648 ± 254 a | 890 ± 390 a | <0.01 |
| RV dP/dtmin (mmHg/s) | −459 ± 112 | −746 ± 289 a | −923 ± 350 a,b | <0.01 |
| RV CO (L/min/m2) | 3.2 ± 0.6 | 3.9 ± 1.2 | 5.5 ± 1.3 a,b | <0.01 |
| RV SV (mL/m2) | 32.7 ± 3.1 | 44.0 ± 6.9 a | 46.2 ± 6.9 a | <0.01 |
| Systolic SAP (mmHg) | 110 ± 14 | 129 ± 15 a | 127 ± 12 a | <0.01 |
| Mean SAP (mmHg) | 76 ± 15 | 83 ± 16 | 85 ± 12 | 0.11 |
| PVR | 8.6 ± 2.1 | 9.5 ± 1.8 a | 8.8 ± 1.8 | 0.03 |
| SVR | 16.1 ± 3.3 | 17.2 ± 4.2 | 13.0 ± 2.4 | 0.09 |
| LVEDVI (mL/m2) | 72.5 ± 11.1 | 77.4 ± 12.2 | 73.0 ± 14.8 | 0.45 |
| LVESVI (mL/m2) | 41.0 ± 8.5 | 33.8 ± 7.0 a | 28.4 ± 7.1 a,b | <0.01 |
| Ejection fraction (%) | 43.9 ± 3.6 | 56.6 ± 3.3 a | 61.4 ± 3.3 a,b | <0.01 |
| LV SV (mL/m2) | 48.1 ± 7.9 | 61.3 ± 12.7 a | 64.2 ± 11.0 a | <0.01 |
| LV CO (L/min/m2) | 4.8 ± 1.1 | 5.1 ± 1.6 | 6.4 ± 1.6 a | 0.02 |
| RVEDA index (cm2/kg0.624) | 1.5 ± 0.1 | 1.6 ± 0.1 | 1.5 ± 0.2 | 0.96 |
| RVESA index (cm2/kg0.628) | 1.0 ± 0.1 | 0.9 ± 0.2 | 0.8 ± 0.1 a | 0.03 |
| RV FACn (%/kg−0.097) | 44.3 ± 6.6 | 54.1 ± 7.3 | 58.0 ± 5.5 a | 0.02 |
| TAPSEn (mm/kg0.284) | 5.2 ± 1.0 | 6.5 ± 0.9 a | 6.8 ± 0.5 a | <0.01 |
| LV-SL (%) | 12.8 ± 1.9 | 15.9 ± 1.9 a | 17.3 ± 1.5 a | <0.01 |
| LV-SC (%) | 17.0 ± 2.6 | 25.2 ± 2.3 a | 29.4 ± 1.9 a,b | <0.01 |
| RV-SL (%) | 15.2 ± 2.4 | 21.8 ± 2.2 a | 25.0 ± 1.3 a,b | <0.01 |
| Variables | Baseline | Dopamine (µg/kg/min) | p * | |
|---|---|---|---|---|
| 3 | 5 | |||
| Mean PAWP (mmHg) | 7.7 ± 1.9 | 6.9 ± 2.3 | 6.4 ± 2.1 | 0.13 |
| Systolic PAP (mmHg) | 49.3 ± 7.9 | 51.4 ± 9.9 | 57.4 ± 14.3 a | 0.04 |
| Mean PAP (mmHg) | 36.8 ± 7.1 | 36.2 ± 6.5 | 39.7 ± 6.0 | 0.12 |
| Diastolic PAP (mmHg) | 29.3 ± 4.5 | 25.1 ± 4.7 | 25.0 ± 6.4 | 0.06 |
| Systolic RVP (mmHg) | 47.4 ± 8.1 | 51.7 ± 12.6 a | 55.4 ± 13.2 a | 0.03 |
| Diastolic RVP (mmHg) | 4.9 ± 4.4 | 3.5 ± 4.3 a | 2.3 ± 3.7 a | <0.01 |
| RV dP/dtmax (mmHg/s) | 409 ± 127 | 511 ± 208 a | 499 ± 196 a | 0.04 |
| RV dP/dtmin (mmHg/s) | −432 ± 126 | −536 ± 204 | −553 ± 203 a | 0.02 |
| RV CO (L/min/m2) | 3.5 ± 0.3 | 3.6 ± 0.7 | 3.5 ± 0.7 | 0.94 |
| RV SV (mL/m2) | 33.0 ± 4.1 | 41.1 ± 7.2 a | 46.8 ± 7.6 a | <0.01 |
| Systolic SAP (mmHg) | 108 ± 10 | 110 ± 14 | 126 ± 10 a | 0.01 |
| Mean SAP (mmHg) | 75 ± 11 | 72 ± 11 | 75 ± 11 | 0.74 |
| PVR | 8.3 ± 2.0 | 8.3 ± 1.7 | 9.5 ± 1.2 a | 0.04 |
| SVR | 12.6 ± 0.9 | 14.4 ± 1.6 | 15.4 ± 1.4 a | 0.04 |
| LVEDVI (mL/m2) | 69.9 ± 11.6 | 70.7 ± 9.1 | 74.5 ± 8.5 | 0.12 |
| LVESVI (mL/m2) | 37.2 ± 8.5 | 34.4 ± 6.3 | 33.3 ± 7.6 | 0.11 |
| Ejection fraction (%) | 47.4 ± 4.3 | 51.7 ± 2.8 a | 55.7 ± 5.8 a | <0.01 |
| LV SV (mL/m2) | 49.9 ± 4.9 | 55.0 ± 5.7 | 62.2 ± 5.5 a | <0.01 |
| LV CO (L/min/m2) | 5.5 ± 0.5 | 5.0 ± 0.6 | 5.3 ± 1.1 | 0.38 |
| RVEDA index (cm2/kg0.624) | 1.6 ± 0.1 | 1.5 ± 0.2 | 1.6 ± 0.1 | 0.09 |
| RVESA index (cm2/kg0.628) | 1.1 ± 0.1 | 1.0 ± 0.1 | 0.9 ± 0.1 a | 0.04 |
| RV FACn (%/kg−0.097) | 39.8 ± 2.9 | 45.2 ± 2.8 | 53.7 ± 5.2 a,b | <0.01 |
| TAPSEn (mm/kg0.284) | 4.9 ± 0.8 | 5.3 ± 0.6 | 6.4 ± 0.9 a,b | <0.01 |
| LV-SL (%) | 12.6 ± 2.4 | 13.7 ± 1.4 | 16.2 ± 2.4 a,b | <0.01 |
| LV-SC (%) | 14.9 ± 1.2 | 19.6 ± 3.2 a | 22.3 ± 2.0 a | <0.01 |
| RV-SL (%) | 17.5 ± 2.0 | 21.5 ± 2.9 a | 25.1 ± 2.3 a,b | <0.01 |
| Variables | Pimobendan (0.15 mg/kg) | p * | |
|---|---|---|---|
| Pre | Post | ||
| Mean PAWP (mmHg) | 7.4 ± 2.1 | 6.9 ± 1.8 | 0.35 |
| Systolic PAP (mmHg) | 47.8 ± 8.2 | 48.9 ± 8.2 | 0.53 |
| Mean PAP (mmHg) | 37.1 ± 5.5 | 37.5 ± 6.5 | 0.75 |
| Diastolic PAP (mmHg) | 28.2 ± 4.4 | 28.0 ± 5.3 | 0.86 |
| Systolic RVP (mmHg) | 44.7 ± 5.1 | 50.4 ± 10.3 | 0.04 |
| Diastolic RVP (mmHg) | 4.2 ± 4.3 | 1.8 ± 2.7 | 0.06 |
| RV dP/dtmax (mmHg/s) | 397 ± 124 | 480 ± 118 | 0.04 |
| RV dP/dtmin (mmHg/s) | −418 ± 104 | −512 ± 123 | 0.04 |
| RV CO (L/min/m2) | 3.5 ± 0.3 | 3.9 ± 0.4 | 0.03 |
| RV SV (mL/m2) | 34.4 ± 2.6 | 38.5 ± 3.5 | 0.01 |
| Systolic SAP (mmHg) | 109 ± 9 | 107 ± 8 | 0.82 |
| Mean SAP (mmHg) | 71 ± 3 | 70 ± 3 | 0.95 |
| PVR | 8.5 ± 1.3 | 7.8 ± 1.0 | 0.06 |
| SVR | 13.3 ± 2.2 | 11.6 ± 3.0 | 0.03 |
| LVEDVI (mL/m2) | 73.4 ± 9.4 | 73.0 ± 10.1 | 0.60 |
| LVESVI (mL/m2) | 38.8 ± 6.5 | 34.1 ± 6.7 | <0.01 |
| Ejection fraction (%) | 47.4 ± 3.4 | 53.6 ± 3.2 | <0.01 |
| LV SV (mL/m2) | 54.0 ± 6.9 | 61.3 ± 7.8 | <0.01 |
| LV CO (L/min/m2) | 5.5 ± 0.9 | 6.4 ± 1.3 | 0.04 |
| RVEDA index (cm2/kg0.624) | 1.6 ± 0.2 | 1.5 ± 0.1 | 0.45 |
| RVESA index (cm2/kg0.628) | 1.1 ± 0.2 | 0.9 ± 0.1 | 0.04 |
| RV FACn (%/kg−0.097) | 42.0 ± 6.1 | 49.9 ± 5.3 | <0.01 |
| TAPSEn (mm/kg0.284) | 5.4 ± 0.8 | 6.0 ± 0.5 | 0.07 |
| LV-SL (%) | 13.9 ± 1.8 | 15.5 ± 2.1 | <0.01 |
| LV-SC (%) | 16.2 ± 1.9 | 19.5 ± 1.1 | <0.01 |
| RV-SL (%) | 19.2 ± 2.9 | 23.0 ± 1.7 | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yuchi, Y.; Suzuki, R.; Satomi, S.; Saito, T.; Teshima, T.; Matsumoto, H. Cardiovascular Effect of Epoprostenol and Intravenous Cardiac Drugs for Acute Heart Failure on Canine Pulmonary Hypertension. Vet. Sci. 2023, 10, 302. https://doi.org/10.3390/vetsci10040302
Yuchi Y, Suzuki R, Satomi S, Saito T, Teshima T, Matsumoto H. Cardiovascular Effect of Epoprostenol and Intravenous Cardiac Drugs for Acute Heart Failure on Canine Pulmonary Hypertension. Veterinary Sciences. 2023; 10(4):302. https://doi.org/10.3390/vetsci10040302
Chicago/Turabian StyleYuchi, Yunosuke, Ryohei Suzuki, Shuji Satomi, Takahiro Saito, Takahiro Teshima, and Hirotaka Matsumoto. 2023. "Cardiovascular Effect of Epoprostenol and Intravenous Cardiac Drugs for Acute Heart Failure on Canine Pulmonary Hypertension" Veterinary Sciences 10, no. 4: 302. https://doi.org/10.3390/vetsci10040302
APA StyleYuchi, Y., Suzuki, R., Satomi, S., Saito, T., Teshima, T., & Matsumoto, H. (2023). Cardiovascular Effect of Epoprostenol and Intravenous Cardiac Drugs for Acute Heart Failure on Canine Pulmonary Hypertension. Veterinary Sciences, 10(4), 302. https://doi.org/10.3390/vetsci10040302







