Effect of Different Landing Heights and Loads on Ankle Inversion Proprioception during Landing in Individuals with and without Chronic Ankle Instability
Abstract
1. Introduction
2. Materials and Methods
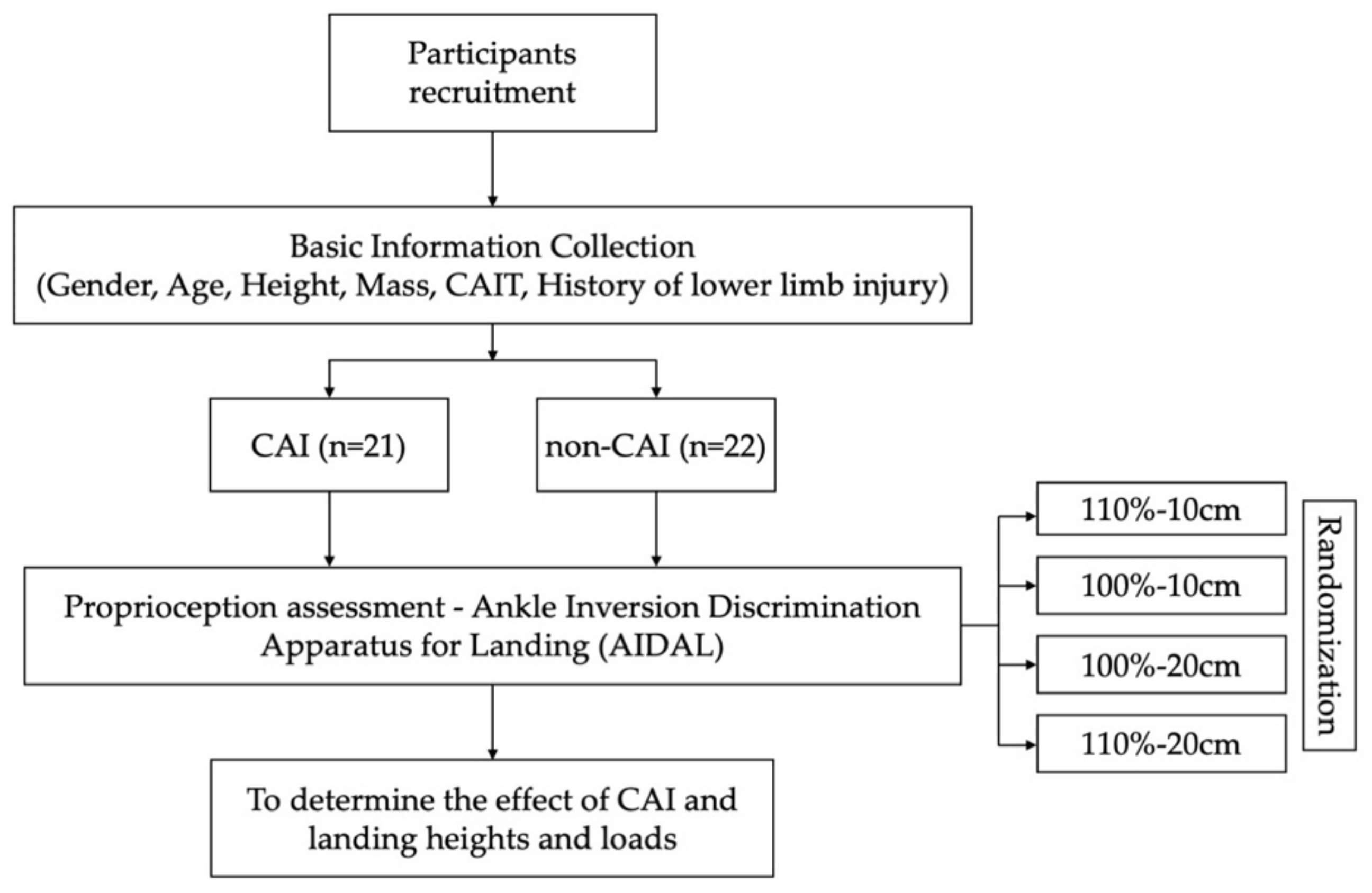
2.1. Study Design
2.2. Participants
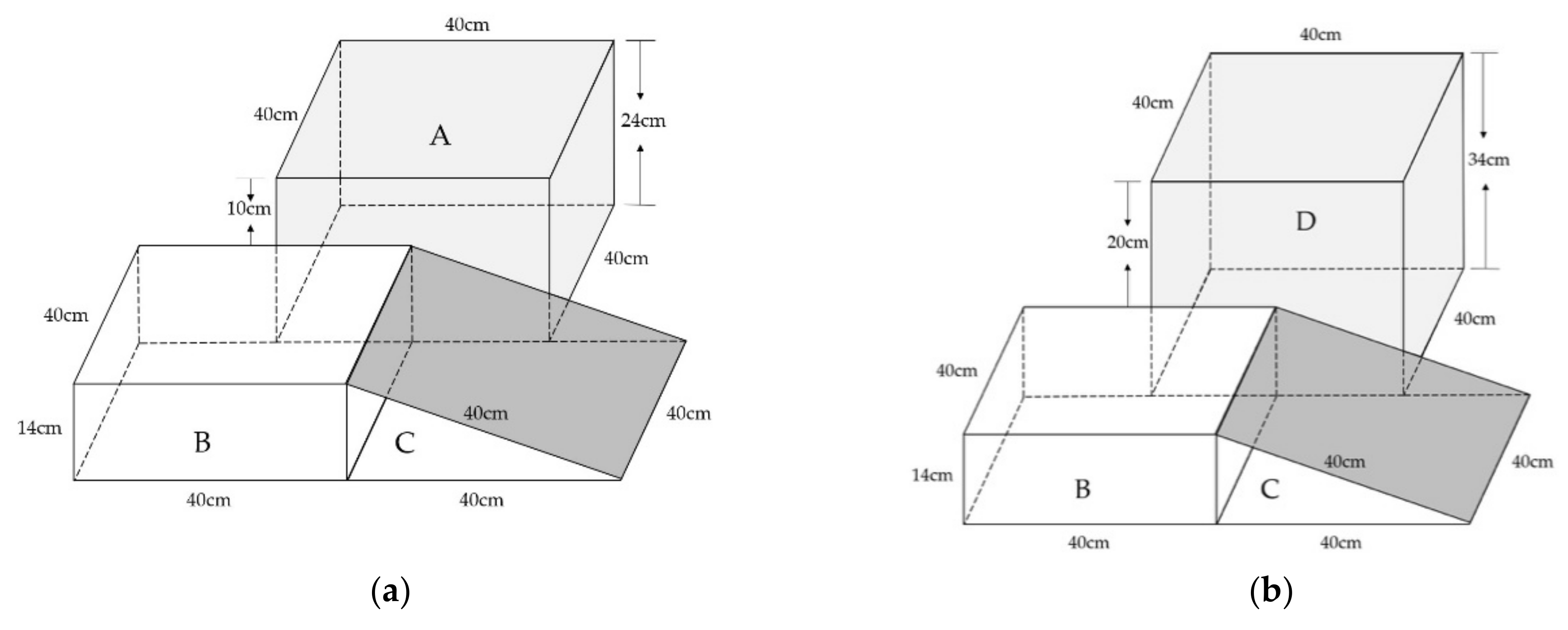
2.3. Apparatus
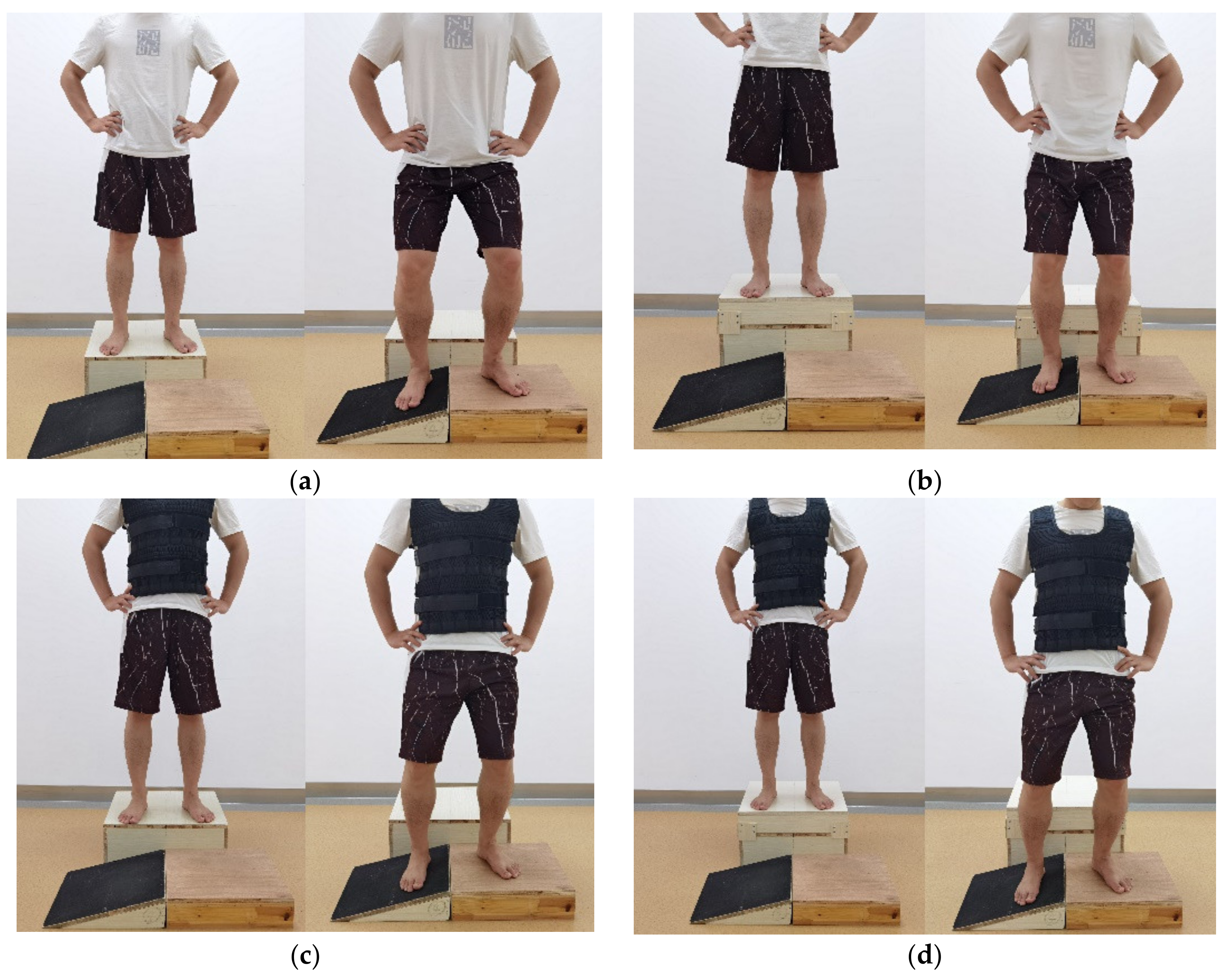
2.4. Procedures
2.5. Data Analysis
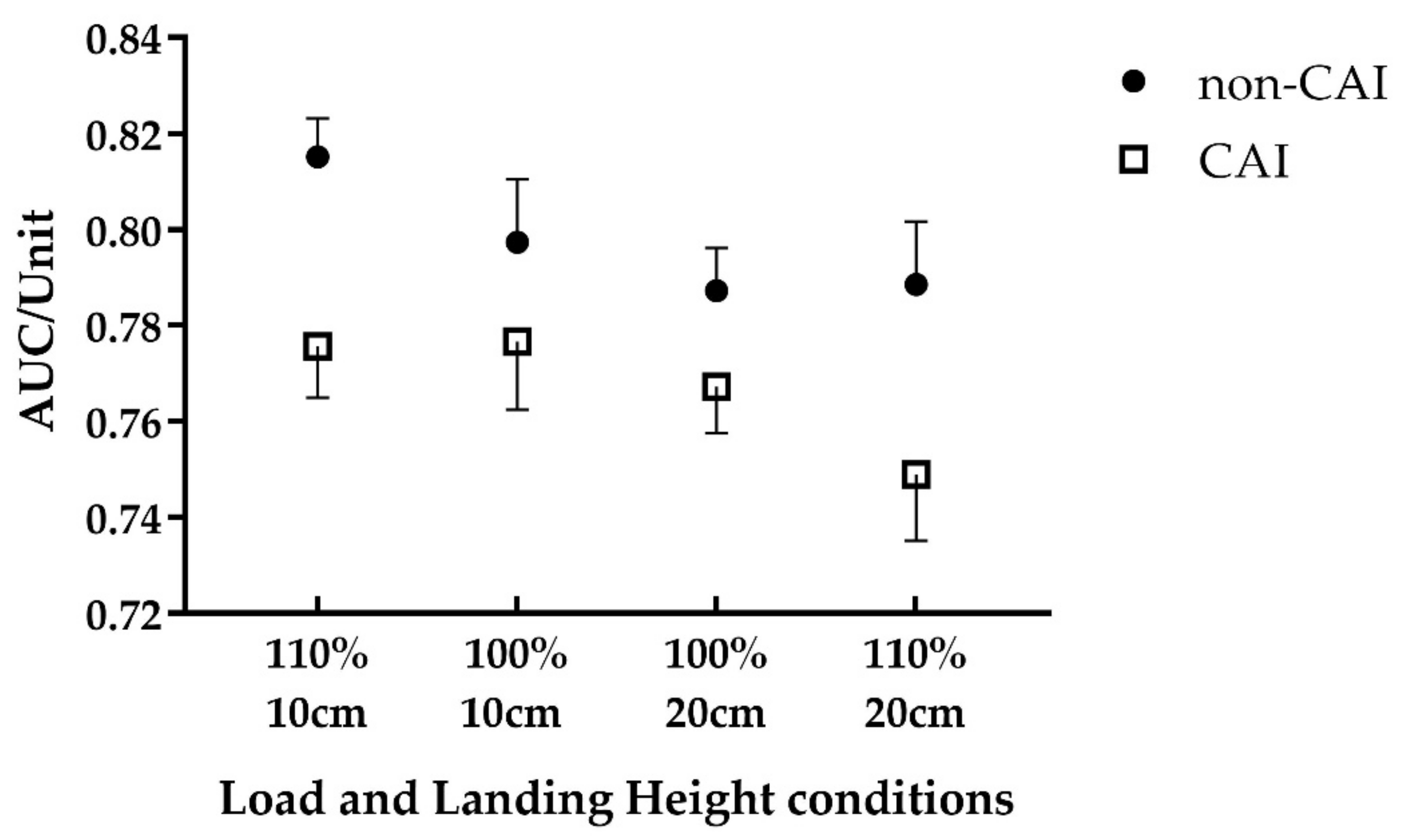
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fong, D.T.; Hong, Y.; Chan, L.K.; Yung, P.S.; Chan, K.M. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007, 37, 73–94. [Google Scholar] [CrossRef] [PubMed]
- Lytle, J.B.; Parikh, K.B.; Tarakemeh, A.; Vopat, B.G.; Mulcahey, M.K. Epidemiology of Foot and Ankle Injuries in NCAA Jumping Athletes in the United States During 2009–2014. Orthop. J. Sports Med. 2021, 9, 2325967121998052. [Google Scholar] [CrossRef] [PubMed]
- Waterman, B.R.; Owens, B.D.; Davey, S.; Zacchilli, M.A.; Belmont, P.J.J.J., Jr. The epidemiology of ankle sprains in the United States. J. Bone Jt. Surg. Am. 2010, 92, 2279–2284. [Google Scholar] [CrossRef]
- McKay, G.D.; Goldie, P.A.; Payne, W.R.; Oakes, B.W. Ankle injuries in basketball: Injury rate and risk factors. Br. J. Sports Med. 2001, 35, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.-Z.; Lin, Y.-A.; Tai, W.-H.; Chen, C.-Y. Influence of Landing in Neuromuscular Control and Ground Reaction Force with Ankle Instability: A Narrative Review. Bioengineering 2022, 9, 68. [Google Scholar] [CrossRef] [PubMed]
- Panagiotakis, E.; Mok, K.M.; Fong, D.T.; Bull, A.M.J. Biomechanical analysis of ankle ligamentous sprain injury cases from televised basketball games: Understanding when, how and why ligament failure occurs. J. Sci. Med. Sport 2017, 20, 1057–1061. [Google Scholar] [CrossRef]
- Fong, D.T.; Chan, Y.Y.; Mok, K.M.; Yung, P.S.; Chan, K.M. Understanding acute ankle ligamentous sprain injury in sports. Sports Med. Arthrosc. Rehabil. Ther. Technol. 2009, 1, 14. [Google Scholar] [CrossRef]
- Doherty, C.; Bleakley, C.; Delahunt, E.; Holden, S. Treatment and prevention of acute and recurrent ankle sprain: An overview of systematic reviews with meta-analysis. Br. J. Sports Med. 2017, 51, 113–125. [Google Scholar] [CrossRef]
- Han, J.; Waddington, G.; Adams, R.; Anson, J.; Liu, Y. Assessing proprioception: A critical review of methods. J. Sport Health Sci. 2016, 5, 80–90. [Google Scholar] [CrossRef]
- Xue, X.; Ma, T.; Li, Q.; Song, Y.; Hua, Y. Chronic ankle instability is associated with proprioception deficits: A systematic review and meta-analysis. J. Sport Health Sci. 2021, 10, 182–191. [Google Scholar] [CrossRef]
- Kazemi, K.; Arab, A.M.; Abdollahi, I.; López-López, D.; Calvo-Lobo, C. Electromiography comparison of distal and proximal lower limb muscle activity patterns during external perturbation in subjects with and without functional ankle instability. Hum. Mov. Sci. 2017, 55, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Yang, Z.; Adams, R.; Ganderton, C.; Witchalls, J.; Waddington, G. Ankle inversion proprioception measured during landing in individuals with and without chronic ankle instability. J. Sci. Med. Sport 2021, 24, 665–669. [Google Scholar] [CrossRef]
- Hunt, K.J.; Hurwit, D.; Robell, K.; Gatewood, C.; Botser, I.B.; Matheson, G. Incidence and Epidemiology of Foot and Ankle Injuries in Elite Collegiate Athletes. Am. J. Sports Med. 2017, 45, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Nordin, A.D.; Dufek, J.S. Lower extremity variability changes with drop-landing height manipulations. Res. Sports Med. 2017, 25, 144–155. [Google Scholar] [CrossRef] [PubMed]
- Wang, I.L.; Chen, Y.M.; Zhang, K.K.; Li, Y.G.; Su, Y.; Wu, C.; Ho, C.S. Influences of Different Drop Height Training on Lower Extremity Kinematics and Stiffness during Repetitive Drop Jump. Appl. Bionics Biomech. 2021, 2021, 5551199. [Google Scholar] [CrossRef] [PubMed]
- Wang, I.L.; Wang, S.Y.; Wang, L.I. Sex differences in lower extremity stiffness and kinematics alterations during double-legged drop landings with changes in drop height. Sports Biomech. 2015, 14, 404–412. [Google Scholar] [CrossRef]
- Gribble, P.A.; Bleakley, C.M.; Caulfield, B.M.; Docherty, C.L.; Fourchet, F.; Fong, D.T.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; McKeon, P.O.; et al. 2016 consensus statement of the International Ankle Consortium: Prevalence, impact and long-term consequences of lateral ankle sprains. Br. J. Sports Med. 2016, 50, 1493–1495. [Google Scholar] [CrossRef]
- Hopkins, J.T.; Brown, T.N.; Christensen, L.; Palmieri-Smith, R.M. Deficits in peroneal latency and electromechanical delay in patients with functional ankle instability. J. Orthop. Res. 2009, 27, 1541–1546. [Google Scholar] [CrossRef]
- Fong, D.T.; Hong, Y.; Shima, Y.; Krosshaug, T.; Yung, P.S.; Chan, K.M. Biomechanics of supination ankle sprain: A case report of an accidental injury event in the laboratory. Am. J. Sports Med. 2009, 37, 822–827. [Google Scholar] [CrossRef]
- Wojciechowska-Maszkowska, B.; Borzucka, D. Characteristics of Standing Postural Control in Women under Additional Load. Int. J. Environ. Res. Public Health 2020, 17, 490. [Google Scholar] [CrossRef]
- Jammes, Y.; Ferrand, E.; Fraud, C.; Boussuges, A.; Weber, J.P. Adding body load modifies the vibratory sensation of the foot sole and affects the postural control. Mil. Med. Res. 2018, 5, 28. [Google Scholar] [CrossRef] [PubMed]
- Bullock-Saxton, J.E.; Wong, W.J.; Hogan, N. The influence of age on weight-bearing joint reposition sense of the knee. Exp. Brain Res. 2001, 136, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Anson, J.; Waddington, G.; Adams, R.; Liu, Y. The Role of Ankle Proprioception for Balance Control in relation to Sports Performance and Injury. Biomed. Res. Int. 2015, 2015, 842804. [Google Scholar] [CrossRef] [PubMed]
- Simpson, J.D.; Stewart, E.M.; Macias, D.M.; Chander, H.; Knight, A.C. Individuals with chronic ankle instability exhibit dynamic postural stability deficits and altered unilateral landing biomechanics: A systematic review. Phys. Ther. Sport 2019, 37, 210–219. [Google Scholar] [CrossRef]
- Vuurberg, G.; Hoorntje, A.; Wink, L.M.; van der Doelen, B.F.W.; van den Bekerom, M.P.; Dekker, R.; van Dijk, C.N.; Krips, R.; Loogman, M.C.M.; Ridderikhof, M.L.; et al. Diagnosis, treatment and prevention of ankle sprains: Update of an evidence-based clinical guideline. Br. J. Sports Med. 2018, 52, 956. [Google Scholar] [CrossRef]
- Hertel, J.; Corbett, R.O. An Updated Model of Chronic Ankle Instability. J. Athl. Train. 2019, 54, 572–588. [Google Scholar] [CrossRef]
- Morales, C.R.; Lobo, C.C.; Sanz, D.R.; Corbalán, I.S.; Ruiz, B.R.; López, D.L. The concurrent validity and reliability of the Leg Motion system for measuring ankle dorsiflexion range of motion in older adults. PeerJ 2017, 5, e2820. [Google Scholar] [CrossRef]
- Cruz-Díaz, D.; Vega, R.L.; Osuna-Pérez, M.C.; Hita-Contreras, F.; Martínez-Amat, A. Effects of joint mobilization on chronic ankle instability: A randomized controlled trial. Disabil. Rehabil. 2015, 37, 601–610. [Google Scholar] [CrossRef]
- Romero-Morales, C.; López-López, S.; Bravo-Aguilar, M.; Cerezo-Téllez, E.; Benito-de Pedro, M.; López, D.L.; Lobo, C.C. Ultrasonography Comparison of the Plantar Fascia and Tibialis Anterior in People with and Without Lateral Ankle Sprain: A Case-Control Study. J. Manip. Physiol. Ther. 2020, 43, 799–805. [Google Scholar] [CrossRef]
- Delahunt, E.; Bleakley, C.M.; Bossard, D.S.; Caulfield, B.M.; Docherty, C.L.; Doherty, C.; Fourchet, F.; Fong, D.T.; Hertel, J.; Hiller, C.E.; et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the International Ankle Consortium. Br. J. Sports Med. 2018, 52, 1304–1310. [Google Scholar] [CrossRef]
- Kaminski, T.W.; Knight, C.; Glutting, J.; Thomas, S.; Swanik, C.; Rosen, A. Differences in Lateral Drop Jumps from an Unknown Height Among Individuals With Functional Ankle Instability. J. Athl. Train. 2013, 48, 773–781. [Google Scholar] [CrossRef]
- Lin, J.Z.; Lin, Y.A.; Lee, H.J. Are Landing Biomechanics Altered in Elite Athletes with Chronic Ankle Instability. J. Sports Sci. Med. 2019, 18, 653–662. [Google Scholar] [PubMed]
- DeJong, A.F.; Koldenhoven, R.M.; Hertel, J. Hip biomechanical alterations during walking in chronic ankle instability patients: A cross-correlation analysis. Sports Biomech. 2022, 21, 460–471. [Google Scholar] [CrossRef] [PubMed]
- Jeon, K.; Kim, K.; Kang, N. Leg stiffness control during drop landing movement in individuals with mechanical and functional ankle disabilities. Sports Biomech. 2022, 21, 1093–1106. [Google Scholar] [CrossRef] [PubMed]
- Refshauge, K.M.; Kilbreath, S.L.; Raymond, J. The effect of recurrent ankle inversion sprain and taping on proprioception at the ankle. Med. Sci. Sports Exerc. 2000, 32, 10–15. [Google Scholar] [CrossRef]
- Rosen, A.B.; Yentes, J.M.; McGrath, M.L.; Maerlender, A.C.; Myers, S.A.; Mukherjee, M. Alterations in cortical activation among individuals with chronic ankle instability during single-limb postural control. J. Athl. Train. 2019, 54, 718–726. [Google Scholar] [CrossRef] [PubMed]
- Koren, Y.; Parmet, Y.; Bar-Haim, S. Treading on the unknown increases prefrontal activity: A pilot fNIRS study. Gait Posture 2019, 69, 96–100. [Google Scholar] [CrossRef]
- Stuart, S.; Vitorio, R.; Morris, R.; Martini, D.N.; Fino, P.C.; Mancini, M. Cortical activity during walking and balance tasks in older adults and in people with Parkinson’s disease: A structured review. Maturitas 2018, 113, 53–72. [Google Scholar] [CrossRef]
- Gribble, P.A.; Delahunt, E.; Bleakley, C.; Caulfield, B.; Docherty, C.; Fourchet, F.; Fong, D.T.; Hertel, J.; Hiller, C.; Kaminski, T.; et al. Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the International Ankle Consortium. Br. J. Sports Med. 2014, 48, 1014–1018. [Google Scholar] [CrossRef]
- Hiller, C.E.; Refshauge, K.M.; Bundy, A.C.; Herbert, R.D.; Kilbreath, S.L. The Cumberland ankle instability tool: A report of validity and reliability testing. Arch. Phys. Med. Rehabil. 2006, 87, 1235–1241. [Google Scholar] [CrossRef]
- Witchalls, J.B.; Waddington, G.; Adams, R.; Blanch, P. Chronic ankle instability affects learning rate during repeated proprioception testing. Phys. Ther. Sport 2014, 15, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Watabe, T.; Takabayashi, T.; Tokunaga, Y.; Watanabe, T.; Kubo, M. Copers exhibit altered ankle and trunk kinematics compared to the individuals with chronic ankle instability during single-leg landing. Sports Biomech. 2022, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Yu, P.; Mei, Q.; Xiang, L.; Fernandez, J.; Gu, Y. Differences in the locomotion biomechanics and dynamic postural control between individuals with chronic ankle instability and copers: A systematic review. Sports Biomech. 2022, 21, 531–549. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Palmieri-Smith, R.; Kipp, K. Peak Forces and Force Generating Capacities of Lower Extremity Muscles During Dynamic Tasks in People With and Without Chronic Ankle Instability. Sports Biomech. 2022, 21, 487–500. [Google Scholar] [CrossRef] [PubMed]
- Waddington, G.; Adams, R. Football boot insoles and sensitivity to extent of ankle inversion movement. Br. J. Sports Med. 2003, 37, 170–174, discussion 175. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Luan, L.; Adams, R.; Witchalls, J.; Newman, P.; Tirosh, O.; Waddington, G. Can therapeutic exercises improve proprioception in chronic ankle instability? A systematic review and network meta-analysis. Arch. Phys. Med. Rehabil. 2022, 103, 2232–2244. [Google Scholar] [CrossRef]
- Watanabe, K.; Koshino, Y.; Ishida, T.; Samukawa, M.; Tohyama, H. Energy dissipation during single-leg landing from three heights in individuals with and without chronic ankle instability. Sports Biomech. 2022, 21, 408–427. [Google Scholar] [CrossRef]
- Goble, D.J. Proprioceptive acuity assessment via joint position matching: From basic science to general practice. Phys. Ther. 2010, 90, 1176–1184. [Google Scholar] [CrossRef]
- Faisal, A.A.; Selen, L.P.; Wolpert, D.M. Noise in the nervous system. Nat. Rev. Neurosci. 2008, 9, 292–303. [Google Scholar] [CrossRef]
- Han, J.; Adams, R.; Waddington, G.; Han, C.J.S.; Research, M. Proprioceptive accuracy after uni-joint and multi-joint patterns of arm-raising movements directed to overhead targets. Somatosens. Mot. Res. 2021, 38, 127–132. [Google Scholar] [CrossRef]
- Symes, M.; Waddington, G.; Adams, R. Depth of ankle inversion and discrimination of foot positions. Percept. Mot. Ski. 2010, 111, 475–484. [Google Scholar] [CrossRef] [PubMed]
- Fong, D.T.; Ha, S.C.; Mok, K.M.; Chan, C.W.; Chan, K.M. Kinematics analysis of ankle inversion ligamentous sprain injuries in sports: Five cases from televised tennis competitions. Am. J. Sports Med. 2012, 40, 2627–2632. [Google Scholar] [CrossRef] [PubMed]
- Weerakkody, N.; Blouin, J.; Taylor, J.; Gandevia, S.C. Local subcutaneous and muscle pain impairs detection of passive movements at the human thumb. J. Physiol. 2008, 586, 3183–3193. [Google Scholar] [CrossRef]
- Han, J.; Adams, R.; Waddington, G. “Imposed” and “obtained” ankle proprioception across the life span—Commentary on Djajadikarta et al. J. Appl. Physiol. 2020, 129, 533–534. [Google Scholar] [CrossRef] [PubMed]
- Lephart, S.M.; Pincivero, D.M.; Giraldo, J.L.; Fu, F.H. The role of proprioception in the management and rehabilitation of athletic injuries. Am. J. Sports Med. 1997, 25, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Waddington, G.; Adams, R. Discrimination of active plantarflexion and inversion movements after ankle injury. Aust. J. Physiother. 1999, 45, 7–13. [Google Scholar] [CrossRef]
- Lu, J.; Wu, Z.; Adams, R.; Han, J.; Cai, B. Sex differences in the relationship of hip strength and functional performance to chronic ankle instability scores. J. Orthop. Surg. Res. 2022, 17, 173. [Google Scholar] [CrossRef]
| Characteristic | Group | Difference between Groups | |
|---|---|---|---|
| CAI | Non-CAI | ||
| N | 21 | 22 | - |
| Gender | M10 F11 | M11 F11 | - |
| Age (y) | 23.4 ± 3.2 | 24.1 ± 2.1 | t = −0.804, p = 0.426 |
| Height (cm) | 171.3 ± 8.2 | 169.1 ± 6.3 | t = 0.972, p = 0.337 |
| Mass (kg) | 65.6 ± 11.6 | 64.6 ± 9.0 | t = 0.268, p = 0.790 |
| CAIT score | 15.6 ± 4.9 | 28.6 ± 1.8 | t = −11.606, p = 0.000 |
| F | p | Partial η2 | |
|---|---|---|---|
| 10 cm vs. 20 cm | 7.216 | 0.010 * | 0.150 |
| CAI vs. Non-CAI | 6.120 | 0.018 * | 0.130 |
| 100% vs. 110% | <0.001 | 0.995 | <0.001 |
| Height × Load | 1.874 | 0.178 | 0.044 |
| Height × CAI | <0.001 | 0.984 | <0.001 |
| Load × CAI | 2.244 | 0.142 | 0.052 |
| Height × Load × CAI | 0.001 | 0.972 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, M.; Zhang, T.; Yu, R.; Ganderton, C.; Adams, R.; Han, J. Effect of Different Landing Heights and Loads on Ankle Inversion Proprioception during Landing in Individuals with and without Chronic Ankle Instability. Bioengineering 2022, 9, 743. https://doi.org/10.3390/bioengineering9120743
Kang M, Zhang T, Yu R, Ganderton C, Adams R, Han J. Effect of Different Landing Heights and Loads on Ankle Inversion Proprioception during Landing in Individuals with and without Chronic Ankle Instability. Bioengineering. 2022; 9(12):743. https://doi.org/10.3390/bioengineering9120743
Chicago/Turabian StyleKang, Ming, Tongzhou Zhang, Ruoni Yu, Charlotte Ganderton, Roger Adams, and Jia Han. 2022. "Effect of Different Landing Heights and Loads on Ankle Inversion Proprioception during Landing in Individuals with and without Chronic Ankle Instability" Bioengineering 9, no. 12: 743. https://doi.org/10.3390/bioengineering9120743
APA StyleKang, M., Zhang, T., Yu, R., Ganderton, C., Adams, R., & Han, J. (2022). Effect of Different Landing Heights and Loads on Ankle Inversion Proprioception during Landing in Individuals with and without Chronic Ankle Instability. Bioengineering, 9(12), 743. https://doi.org/10.3390/bioengineering9120743








