Comparative Biomechanical Strategies of Running Gait Among Healthy and Recently Injured Pediatric and Adult Runners
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
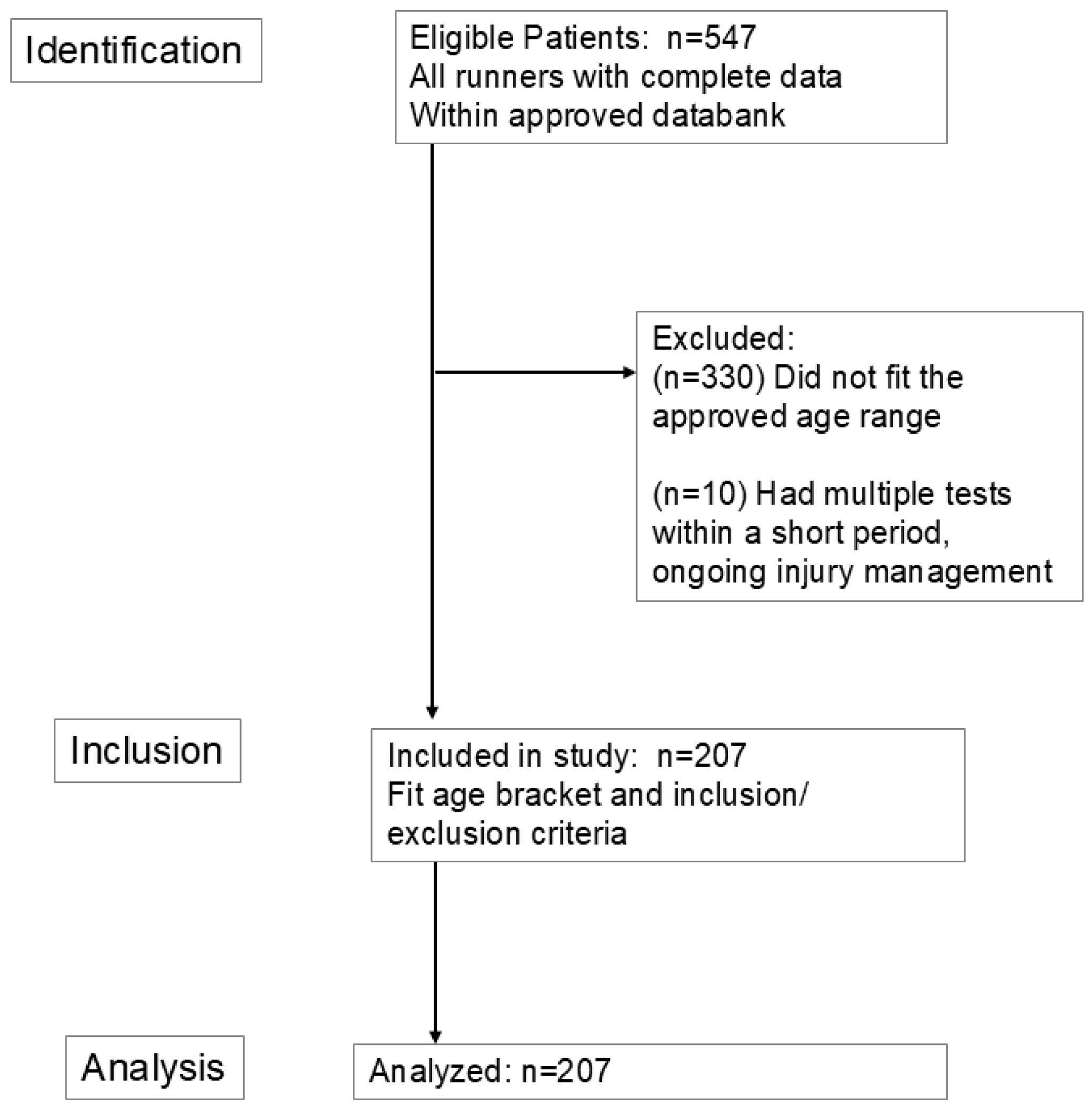
2.3. Participants
2.4. Participant Characteristics
2.5. Data Sources and Measurements
2.6. Statistical Analyses
3. Results
3.1. Characteristics
3.2. Temporal Spatial Parameters
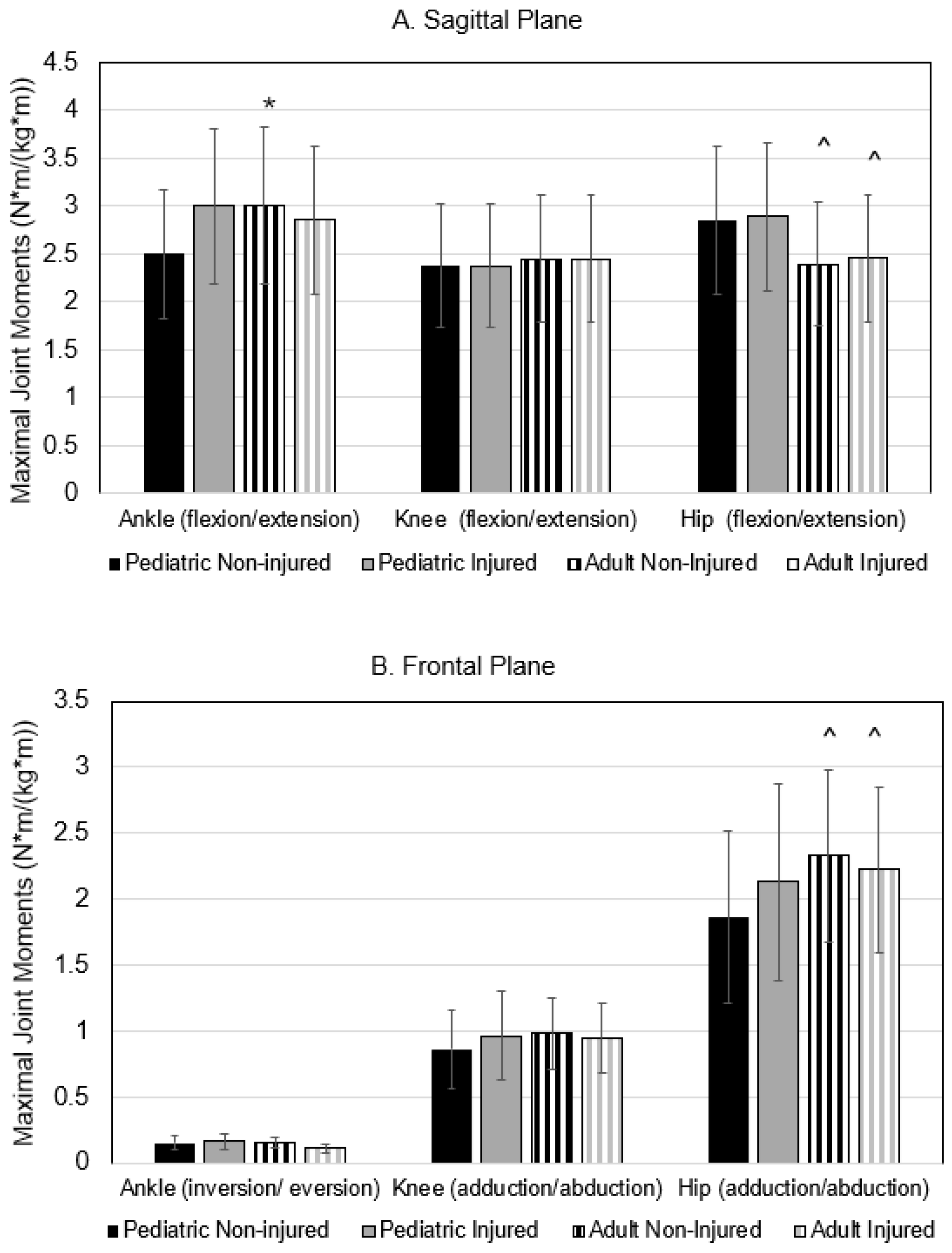
3.3. Kinetic Parameters and Leg Stiffness
3.4. Kinematic Parameters
4. Discussion
4.1. Age-Related Running Differences
4.2. Injury-Related Running Differences
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| GC | gait cycle |
| GRF | ground reaction force |
| VALR | vertical average load rate |
| LR | load rate |
| COM | center of mass |
| Kvert | vertical leg stiffness |
| M-L | medial lateral |
| BMI | body mass index |
References
- NFHS. National Federation of State High School Associations; High School Athletics Participation Survey: Indianapolis, IN, USA, 2021. [Google Scholar]
- Running USA. Running USA 2022 Global Runner Survey; Running USA: San Diego, CA, USA, 2022. [Google Scholar]
- Statista Running and Jogging Participation in the U.S. 2010–2023. Artic. ID Did-18259-1. 2024. Available online: https://www.statista.com/study/18259/running-and-jogging/ (accessed on 15 August 2024).
- Van Middelkoop, M.; Kolkman, J.; Van Ochten, J.; Bierma-Zeinstra, S.; Koes, B. Prevalence and Incidence of Lower Extremity Injuries in Male Marathon Runners. Scand. J. Med. Sci. Sports 2008, 18, 140–144. [Google Scholar] [CrossRef]
- Hollander, K.; Johnson, C.D.; Outerleys, J.; Davis, I.S. Multifactorial Determinants of Running Injury Locations in 550 Injured Recreational Runners. Med. Sci. Sports Exerc. 2021, 53, 102–107. [Google Scholar] [CrossRef]
- van Gent, R.N.; Siem, D.; van Middelkoop, M.; van Os, A.G.; Bierma-Zeinstra, S.M.A.; Koes, B.W. Incidence and Determinants of Lower Extremity Running Injuries in Long Distance Runners: A Systematic Review. Br. J. Sports Med. 2007, 41, 469–480; discussion 480. [Google Scholar] [CrossRef] [PubMed]
- DeJong Lempke, A.F.; Whitney, K.E.; Collins, S.E.; d’Hemecourt, P.A.; Meehan Iii, W.P. Biomechanical Running Gait Assessments across Prevalent Adolescent Musculoskeletal Injuries. Gait Posture 2022, 96, 123–129. [Google Scholar] [CrossRef] [PubMed]
- McSweeney, S.C.; Grävare Silbernagel, K.; Gruber, A.H.; Heiderscheit, B.C.; Krabak, B.J.; Rauh, M.J.; Tenforde, A.S.; Wearing, S.C.; Zech, A.; Hollander, K. Adolescent Running Biomechanics-Implications for Injury Prevention and Rehabilitation. Front. Sports Act. Living 2021, 3, 689846. [Google Scholar] [CrossRef]
- Close, E.L.; Garcia, M.C.; Bazett-Jones, D.M. Pre-Pubertal Runners Demonstrate Greater Variability in Running Kinematics than Post-Pubertal Runners. Gait Posture 2024, 107, 136–140. [Google Scholar] [CrossRef]
- Schepens, B.; Willems, P.A.; Cavagna, G.A. The Mechanics of Running in Children. J. Physiol. 1998, 509 Pt 3, 927–940. [Google Scholar] [CrossRef]
- Garcia, M.C.; Heiderscheit, B.C.; Kraus, E.A.; Norte, G.E.; Murray, A.M.; Bazett-Jones, D.M. Preferred Temporal-Spatial Parameters, Physical Maturation, and Sex Are Related to Vertical and Braking Forces in Adolescent Long-Distance Runners. Sports Biomech. 2024, 23, 3224–3234. [Google Scholar] [CrossRef]
- Clarke, L. The Effect of Physical Growth on Gait Stability in Adolescent Athletes; Temple University: Philadelphia, PA, USA, 2022. [Google Scholar]
- Cesar, G.M.; Sigward, S.M. Dynamic Stability during Running Gait Termination: Differences in Strategies between Children and Adults to Control Forward Momentum. Hum. Mov. Sci. 2015, 43, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Cartón-Llorente, A.; Cardiel-Sánchez, S.; Molina-Molina, A.; Ráfales-Perucha, A.; Rubio-Peirotén, A. Bilateral Asymmetry of Spatiotemporal Running Gait Parameters in U14 Athletes at Different Speeds. Sports 2024, 12, 117. [Google Scholar] [CrossRef]
- Krahenbuhl, G.S.; Williams, T.J. Running Economy: Changes with Age during Childhood and Adolescence. Med. Sci. Sports Exerc. 1992, 24, 462–466. [Google Scholar] [CrossRef]
- Vincent, H.K.; Popp, R.; Cicilioni, O.; Vincent, K.R.; Pezzullo, L.; Martenson, M.; Nixon, R.M. Reference Biomechanical Parameters and Natural Asymmetry among Runners across the Age Spectrum without a History of Running-Related Injuries. Front. Sports Act. Living 2025, 7, 1560756. [Google Scholar] [CrossRef]
- DeJong Lempke, A.F.; Hunt, D.L.; Dawkins, C.; Stracciolini, A.; Kocher, M.S.; d’Hemecourt, P.A.; Whitney, K.E. Adolescent and Young Adult Hip and Knee Strength Profiles Relate to Running Gait Biomechanics. Phys. Ther. Sport Off. J. Assoc. Chart. Physiother. Sports Med. 2023, 64, 48–54. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Morgan, D.W.; Martin, P.E.; Krahenbuhl, G.S.; Baldini, F.D. Variability in Running Economy and Mechanics among Trained Male Runners. Med. Sci. Sports Exerc. 1991, 23, 378. [Google Scholar] [CrossRef] [PubMed]
- Vincent, H.K.; Vincent, K.R. Evaluation of the Injured Runner. In Clinical Care of the Runner: Assessment, Biomechanical Principles, and Injury Management; Elsevier: Toronto, ON, Canada, 2020; pp. 19–26. [Google Scholar]
- Madsen, A.; Sharififar, S.; Oberhaus, J.; Vincent, K.R.; Vincent, H.K. Anxiety State Impact on Recovery of Runners with Lower Extremity Injuries. PLoS ONE 2022, 17, e0278444. [Google Scholar] [CrossRef]
- Vincent, H.K.; Massengill, C.; Harris, A.; Chen, C.; Wasser, J.G.; Bruner, M.; Vincent, K.R. Cadence Impact on Cardiopulmonary, Metabolic and Biomechanical Loading during Downhill Running. Gait Posture 2019, 71, 186–191. [Google Scholar] [CrossRef]
- Kadaba, M.P.; Ramakrishnan, H.K.; Wootten, M.E. Measurement of Lower Extremity Kinematics during Level Walking. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 1990, 8, 383–392. [Google Scholar] [CrossRef] [PubMed]
- de Leva, P. Joint Center Longitudinal Positions Computed from a Selected Subset of Chandler’s Data. J. Biomech. 1996, 29, 1231–1233. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Cui, C.; Zhou, Z.; Zheng, Z.; Yan, S.; Liu, H.; Qu, F.; Zhang, K. Effect of Midsole Hardness and Surface Type Cushioning on Landing Impact in Heel-Strike Runners. J. Biomech. 2024, 165, 111996. [Google Scholar] [CrossRef]
- Vincent, H.K.; Kilgore, J.E.; Chen, C.; Bruner, M.; Horodyski, M.; Vincent, K.R. Impact of Body Mass Index on Biomechanics of Recreational Runners. PM R 2020, 12, 1106–1112. [Google Scholar] [CrossRef]
- Drozda, D.; Thompson, Z.; Vincent, K.R.; Nixon, R.M.; Bolling, J.; Vincent, H.K. Gait Signatures of Endurance Runners with Low Back Pain: A Case Controlled Cross Sectional Study. Gait Posture 2024, 113, 184–190. [Google Scholar] [CrossRef]
- Tenforde, A.S.; Ruder, M.C.; Jamison, S.T.; Singh, P.P.; Davis, I.S. Is Symmetry of Loading Improved for Injured Runners during Novice Barefoot Running? Gait Posture 2018, 62, 317–320. [Google Scholar] [CrossRef]
- Furlong, L.-A.M.; Egginton, N.L. Kinetic Asymmetry during Running at Preferred and Nonpreferred Speeds. Med. Sci. Sports Exerc. 2018, 50, 1241–1248. [Google Scholar] [CrossRef] [PubMed]
- Clark, K.P.; Ryan, L.J.; Weyand, P.G. A General Relationship Links Gait Mechanics and Running Ground Reaction Forces. J. Exp. Biol. 2017, 220, 247–258. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.D.; Tenforde, A.S.; Outerleys, J.; Reilly, J.; Davis, I.S. Impact-Related Ground Reaction Forces Are More Strongly Associated with Some Running Injuries than Others. Am. J. Sports Med. 2020, 48, 3072–3080. [Google Scholar] [CrossRef]
- Davis, J.J.; Gruber, A.H. Leg Stiffness, Joint Stiffness, and Running-Related Injury: Evidence from a Prospective Cohort Study. Orthop. J. Sports Med. 2021, 9, 23259671211011213. [Google Scholar] [CrossRef]
- Gruber, A.H. The “Impacts Cause Injury” Hypothesis: Running in Circles or Making New Strides? J. Biomech. 2023, 156, 111694. [Google Scholar] [CrossRef] [PubMed]
- Sancho, I.; Malliaras, P.; Barton, C.; Willy, R.W.; Morrissey, D. Biomechanical Alterations in Individuals with Achilles Tendinopathy during Running and Hopping: A Systematic Review with Meta-Analysis. Gait Posture 2019, 73, 189–201. [Google Scholar] [CrossRef]
- Zhang, H.; Peng, W.; Qin, C.; Miao, Y.; Zhou, F.; Ma, Y.; Gao, Y. Lower Leg Muscle Stiffness on Two-Dimensional Shear Wave Elastography in Subjects with Medial Tibial Stress Syndrome. J. Ultrasound Med. Off. J. Am. Inst. Ultrasound Med. 2022, 41, 1633–1642. [Google Scholar] [CrossRef]
- Blyton, S.J.; Snodgrass, S.J.; Pizzari, T.; Birse, S.M.; Likens, A.D.; Edwards, S. The Impact of Previous Musculoskeletal Injury on Running Gait Variability: A Systematic Review. Gait Posture 2023, 101, 124–133. [Google Scholar] [CrossRef] [PubMed]
- Peng, L.; Seay, A.N.; Montero, C.; Barnes, L.L.; Vincent, K.R.; Conrad, B.P.; Chen, C.; Vincent, H.K. Metabolic, Cardiopulmonary, and Gait Profiles of Recently Injured and Noninjured Runners. PM R 2015, 7, 26–33. [Google Scholar] [CrossRef] [PubMed]
- McSweeney, S.; Reed, L.F.; Wearing, S.C. Vertical Ground Reaction Forces during Gait in Children with and without Calcaneal Apophysitis. Gait Posture 2019, 71, 126–130. [Google Scholar] [CrossRef]
- Vincent, H.K.; Vincent, K.R. Healthy Running Habits for the Distance Runner: Clinical Utility of the American College of Sports Medicine Infographic. Curr. Sports Med. Rep. 2022, 21, 463–469. [Google Scholar] [CrossRef]
- Anderson, L.M.; Bonanno, D.R.; Hart, H.F.; Barton, C.J. What Are the Benefits and Risks Associated with Changing Foot Strike Pattern During Running? A Systematic Review and Meta-Analysis of Injury, Running Economy, and Biomechanics. Sports Med. 2020, 50, 885–917. [Google Scholar] [CrossRef]
- Peterson, J.R.; Sanders, C.R.; Reynolds, N.S.; Alford, C.A.; Platt, M.J.; Parr, J.J.; Twum, F.; Burns, J.R.; Dolbow, D.R. Running Cadence and the Influence on Frontal Plane Knee Deviations. Clin. Pract. 2024, 14, 2491–2498. [Google Scholar] [CrossRef] [PubMed]
- Zandbergen, M.A.; Marotta, L.; Bulthuis, R.; Buurke, J.H.; Veltink, P.H.; Reenalda, J. Effects of Level Running-Induced Fatigue on Running Kinematics: A Systematic Review and Meta-Analysis. Gait Posture 2023, 99, 60–75. [Google Scholar] [CrossRef] [PubMed]

| Pediatric | Adult | |||||
|---|---|---|---|---|---|---|
| Variable | Non-Injured (n = 23) | Injured (n = 96) | Non-Injured (n = 13) | Injured (n = 75) | p | η2 or Φ |
| Female (%) | 47.8 | 43.8 | 76.9 | 58.7 | 0.012 | 0.017 |
| Age (yr) | 14.7 ± 1.7 | 15.1 ± 1.3 | 30.2 ± 3.3 | 29.4 ± 3.5 | <0.001 | 0.009 |
| Height (cm) | 167.9 ± 8.9 | 167.7 ± 9.9 | 168.7 ± 8.5 | 171.1 ± 9.2 | 0.455 | 0.003 |
| Weight (kg) | 57.3 ± 11.8 | 56.8 ± 10.4 | 66.0 ± 10.3 | 69.1 ± 16.3 | 0.464 | 0.003 |
| BMI (kg/m2) | 20.2 ± 3.4 | 20.1 ± 2.6 | 23.2 ± 2.6 | 23.2 ± 3.3 | 0.933 | 0.001 |
| Running history | ||||||
| Weekly runs (#) | 5.4 ± 3.7 | 4.6 ± 1.8 | 4.3 ± 1.7 | 3.7 ± 2.1 | 0.831 | 0.001 |
| Volume (km/wk) | 32.6 ± 21.4 | 34.6 ± 24.0 | 47.3 ± 34.1 | 32.8 ± 29.0 | 0.129 | 0.012 |
| Speedwork (% yes) | 47.8 | 55.9 | 30.0 | 50.7 | 0.469 | 0.394 |
| Competing (% yes) | 60.9 | 68.7 | 61.5 | 46.7 | 0.023 | 0.023 |
| Shoe wear | ||||||
| Heel height (cm) | 33.1 ± 4.1 | 32.5 ± 7.1 | 31.4 ± 5.7 | 30.1 ± 8.1 | 0.864 | 0.001 |
| Heel-to-toe drop (mm) | 9.3 ± 2.1 | 8.2 ± 3.3 | 5.6 ± 3.1 | 7.7 ± 3.5 | 0.042 | 0.023 |
| Weight (oz) | 9.2 ± 1.5 | 9.0 ± 1.3 | 8.3 ± 1.4 | 8.8 ± 1.5 | 0.239 | 0.008 |
| Cross training practices (%) | ||||||
| Strength training | ||||||
| Lower body | 34.8 | 55.2 | 76.9 | 70.7 | 0.004 | 0.003 |
| Upper body | 34.8 | 60.4 | 76.9 | 72.0 | 0.013 | 0.011 |
| Swimming | 8.7 | 34.4 | 15.4 | 33.3 | 0.879 | 0.844 |
| Cycling | 13.0 | 46.9 | 38.5 | 54.7 | 0.093 | 0.088 |
| Yoga/Pilates | 13.0 | 10.4 | 23.1 | 25.3 | 0.009 | 0.008 |
| Foot strike (%) | ||||||
| Rearfoot | 87.0 | 78.1 | 46.2 | 68.0 | ||
| Midfoot | 13.0 | 18.8 | 46.2 | 25.3 | ||
| Forefoot | 0.0 | 3.1 | 7.7 | 6.7 | 0.042 | 0.042 |
| Injury type (%) | ||||||
| Bone | --- | 61.5 | --- | 47.3 | 0.050 | 0.046 |
| Soft tissue | --- | 48.1 | --- | 68.0 | 0.025 | 0.020 |
| Pediatric | Adult | p | η2 | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | Non-Injured (n = 23) | Injured (n = 96) | Non-Injured (n = 13) | Injured (n = 75) | Injury | Age | Intxn | |
| Velocity (km/h) | 11.1 ± 1.8 | 10.7 ± 2.2 | 9.9 ± 1.7 | 10.0 ± 1.7 | 0.602 | 0.012 | 0.503 | 0.002 |
| Cadence (step/min) | 168 ± 11 | 170 ± 12 | 173 ± 12 | 167 ± 9 | 0.518 | 0.386 | 0.044 | 0.020 |
| COM vertical displacement (cm) | 9.5 ± 1.3 | 9.6 ± 1.6 | 9.2 ± 1.1 | 9.8 ± 1.3 | 0.262 | 0.836 | 0.405 | 0.004 |
| COM M-L displacement (cm) | 2.4 ± 0.6 | 2.5 ± 0.7 | 2.8 ± 0.7 | 2.8 ± 0.9 | 0.450 | 0.176 | 0.953 | 0.001 |
| Step length (m) | 1.02 ± 0.11 | 0.99 ± 0.18 | 0.91 ± 0.12 | 0.93 ± 0.16 | 0.722 | 0.281 | 0.583 | 0.00 |
| Stride length (m) | 1.5 ± 0.2 | 1.5 ± 0.3 | 1.4 ± 0.2 | 1.4 ± 0.2 | 0.447 | 0.280 | 0.273 | 0.007 |
| Stride width (cm) | 7.6 ± 2.2 | 7.6 ± 2.9 | 9.4 ± 2.3 | 9.1 ± 4.5 | 0.730 | 0.042 | 0.884 | 0.001 |
| Stance time (% GC) | 42.9 ± 3.7 | 42.3 ± 4.5 | 44.3 ± 3.1 | 44.4 ± 3.7 | 0.753 | 0.026 | 0.688 | 0.001 |
| Stance time variance (SD) | 0.005 ± 0.002 | 0.004 ± 0.001 | 0.003 ± 0.001 | 0.004 ± 0.002 | 0.557 | <0.001 | 0.002 | 0.056 |
| Swing time, average (% GC) | 57.1 ± 3.7 | 57.6 ± 4.7 | 55.5 ± 3.1 | 55.4 ± 4.1 | 0.853 | 0.022 | 0.761 | 0.001 |
| Swing time variance (SD) | 0.010 ± 0.003 | 0.008 ± 0.003 | 0.005 ± 0.001 | 0.007 ± 0.002 | 0.465 | <0.001 | 0.045 | 0.030 |
| Pediatric | Adult | p | η2 | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | Non-Injured (n = 23) | Injured (n = 96) | Non-Injured (n = 13) | Injured (n = 75) | Injury | Age | Intxn | |
| vertical GRF (BW) | ||||||||
| Left | 2.4 ± 0.2 | 2.6 ± 0.3 | 2.7 ± 0.5 | 2.4 ± 0.3 | 0.279 | 0.754 | 0.037 | 0.021 |
| Right | 2.5 ± 0.3 | 2.5 ± 0.3 | 2.6 ± 0.4 | 2.4 ± 0.3 | 0.417 | 0.911 | 0.013 | 0.120 |
| VALR (BW/s) | ||||||||
| Left | 73.1 ± 28.5 | 73.4 ± 27.9 | 58.7 ± 29.1 | 66.3 ± 25.5 | 0.315 | 0.022 | 0.337 | 0.005 |
| Right | 70.7 ± 21.5 | 75.1 ± 25.7 | 58.3 ± 29.0 | 66.8 ± 24.6 | 0.128 | 0.021 | 0.525 | 0.002 |
| Kvert (N/cm) | 148 ± 28 | 154 ± 35 | 184 ± 46 | 168 ± 33 | 0.318 | 0.017 | 0.309 | 0.006 |
| Pediatric | Adult | p | η2 | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | Non-Injured (n = 23) | Injured (n = 96) | Non-Injured (n = 13) | Injured (n = 75) | Injury | Age | Intxn | |
| Sagittal | ||||||||
| Ankle | 53.1 ± 4.7 | 48.6 ± 7.4 | 46.7 ± 6.1 | 48.1 ± 7.8 | 0.325 | 0.015 | 0.036 | 0.027 |
| Knee | 85.9 ± 11.1 | 91.2 ± 12.3 | 82.7 ± 9.5 | 86.2 ± 14.3 | 0.079 | 0.098 | 0.778 | 0.001 |
| Hip | 57.9 ± 6.6 | 58.2 ± 9.9 | 52.4 ± 6.8 | 55.1 ± 8.7 | 0.312 | 0.276 | 0.967 | 0.001 |
| Pelvis | 8.1 ± 1.9 | 8.4 ± 2.3 | 9.0 ± 0.1 | 8.7 ± 2.3 | 0.983 | 0.146 | 0.532 | 0.002 |
| Frontal | ||||||||
| Ankle | 17.2 ± 4.2 | 15.4 ± 4.6 | 14.2 ± 5.6 | 15.2 ±5.3 | 0.484 | 0.181 | 0.251 | 0.008 |
| Knee | 10.1 ± 3.2 | 10.6 ± 3.7 | 10.4 ± 3.3 | 11.2 ± 5.3 | 0.544 | 0.514 | 0.940 | 0.001 |
| Hip | 20.6 ± 4.0 | 19.3 ± 5.3 | 20.3 ± 5.4 | 21.7 ± 5.7 | 0.900 | 0.395 | 0.172 | 0.011 |
| Pelvis | 10.5 ± 2.6 | 11.5 ± 2.9 | 11.3 ± 2.6 | 12.5 ± 3.4 | 0.044 | 0.180 | 0.655 | 0.001 |
| Transverse | ||||||||
| Ankle | 12.5 ± 3.2 | 13.0 ± 3.1 | 11.7 ± 3.5 | 11.2 ±3.2 | 0.960 | 0.037 | 0.477 | 0.003 |
| Knee | 16.8 ± 3.6 | 19.9 ± 5.4 | 20.0 ± 5.4 | 18.1 ± 2.4 | 0.109 | 0.014 | 0.111 | 0.016 |
| Hip | 17.0 ± 6.2 | 17.0 ± 5.0 | 16.0 ± 5.5 | 18.2 ± 6.9 | 0.943 | 0.127 | 0.124 | 0.014 |
| Pelvis | 17.3 ± 4.4 | 14.4 ± 5.3 | 12.0 ± 4.3 | 13.8 ± 4.8 | 0.472 | 0.005 | 0.036 | 0.027 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Verble, C.; Nixon, R.M.; Pezzullo, L.; Martenson, M.; Vincent, K.R.; Vincent, H.K. Comparative Biomechanical Strategies of Running Gait Among Healthy and Recently Injured Pediatric and Adult Runners. Bioengineering 2025, 12, 937. https://doi.org/10.3390/bioengineering12090937
Verble C, Nixon RM, Pezzullo L, Martenson M, Vincent KR, Vincent HK. Comparative Biomechanical Strategies of Running Gait Among Healthy and Recently Injured Pediatric and Adult Runners. Bioengineering. 2025; 12(9):937. https://doi.org/10.3390/bioengineering12090937
Chicago/Turabian StyleVerble, Cole, Ryan M. Nixon, Lydia Pezzullo, Matthew Martenson, Kevin R. Vincent, and Heather K. Vincent. 2025. "Comparative Biomechanical Strategies of Running Gait Among Healthy and Recently Injured Pediatric and Adult Runners" Bioengineering 12, no. 9: 937. https://doi.org/10.3390/bioengineering12090937
APA StyleVerble, C., Nixon, R. M., Pezzullo, L., Martenson, M., Vincent, K. R., & Vincent, H. K. (2025). Comparative Biomechanical Strategies of Running Gait Among Healthy and Recently Injured Pediatric and Adult Runners. Bioengineering, 12(9), 937. https://doi.org/10.3390/bioengineering12090937






