Effect of Abutment Screw Design on Torque Loss Under Cyclic Fatigue Loading: A Comparison of TSIII and KSIII Implant Systems
Abstract
1. Introduction
2. Materials and Methods
2.1. Implant Systems and Abutments
2.2. Sample Size and Grouping
2.3. Torque Application and Measurement of Initial Removal Torque (T1)
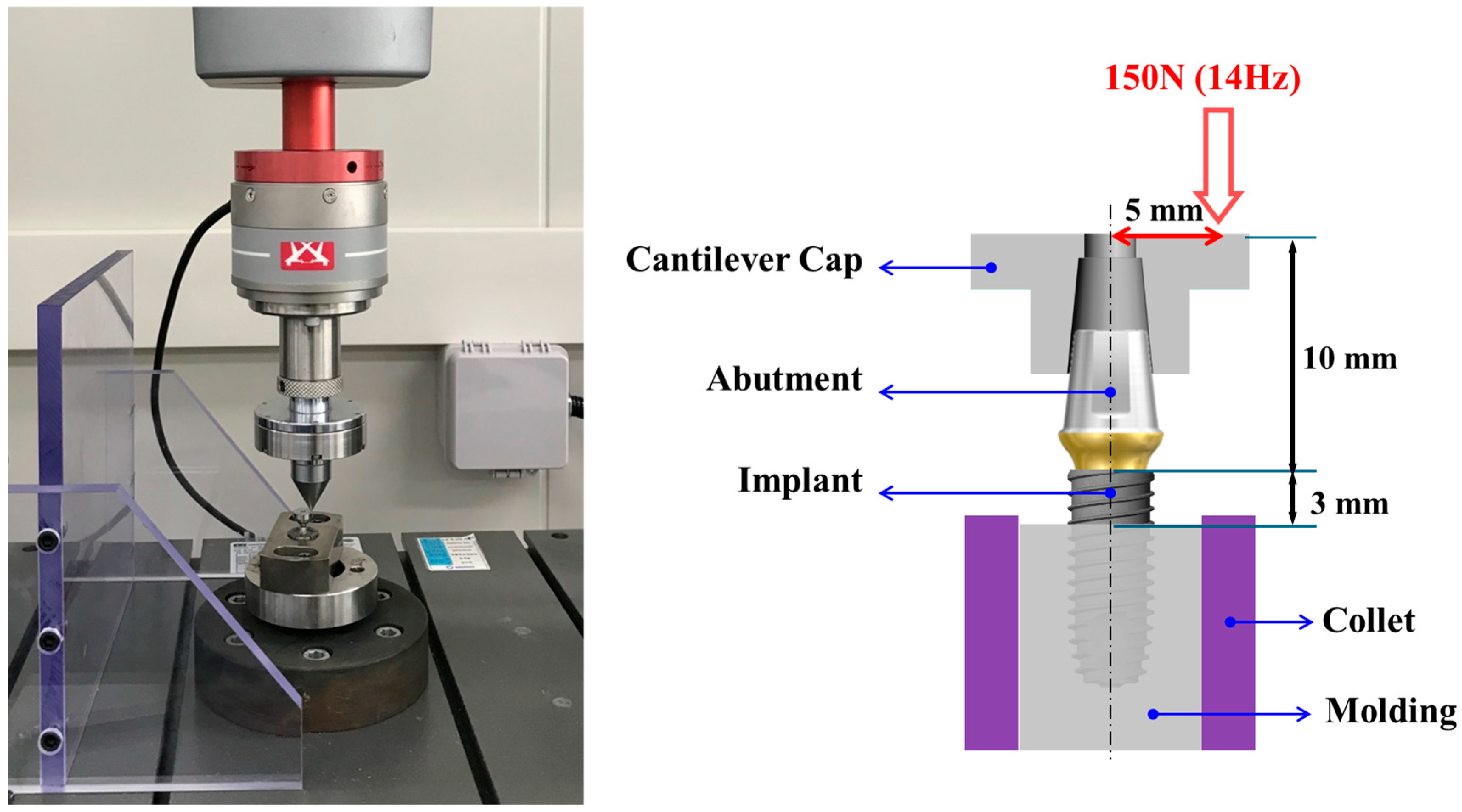
2.4. Fatigue Loading Protocol
2.5. Measurement of Post-Fatigue Removal Torque (T2) and Torque Loss Rate
2.6. Statistical Analysis
3. Results
3.1. Initial Removal Torque (T1)
3.2. Post-Fatigue Removal Torque (T2)
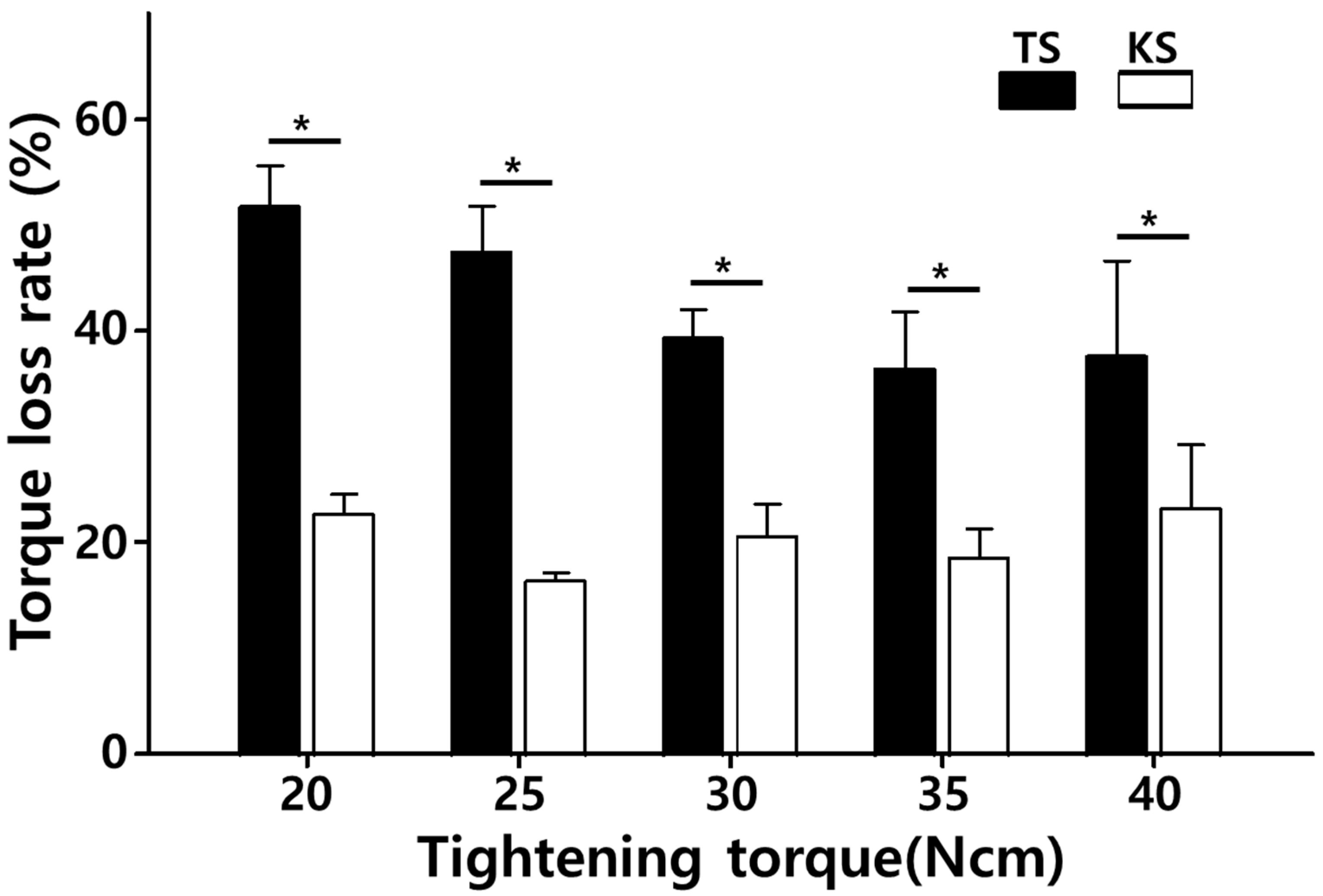
3.3. Torque Loss Rate (%)
4. Discussion
4.1. Comparison with Literature
4.2. Tightening Torque and Retightening
4.3. Biomechanical and Clinical Implications
4.4. Limitations and Future Directions
5. Conclusions
- (1)
- The KSIII system consistently demonstrated lower torque loss rates (<25%) than the TSIII system (>35%), regardless of tightening torque, indicating superior mechanical stability of the implant–abutment complex.
- (2)
- For both systems, this torque level (35 Ncm) minimized preload loss while avoiding the increased loss observed at lower (20–25 Ncm) or excessively high (40 Ncm) values.
- (3)
- By maintaining preload more effectively, the KSIII system may reduce the risk of screw loosening, enhance prosthetic stability, and lower the frequency of maintenance visits in clinical settings.
- (4)
- Results are based on short-term fatigue testing and cannot fully replicate the oral environment. Long-term cyclic loading, thermomechanical aging, and clinical trials are required to confirm whether these biomechanical advantages translate into reduced complication rates in patients.
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wittneben, J.G.; Buser, D.; Salvi, G.E.; Bürgin, W.; Hicklin, S.; Brägger, U. Complication and failure rates with implant-supported prostheses. Clin. Implant Dent. Relat. Res. 2014, 16, 356–364. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Brägger, U.; Lang, N.P.; Zwahlen, M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin. Oral Implant. Res. 2007, 18, 97–113. [Google Scholar] [CrossRef]
- Jung, R.E.; Zembic, A.; Pjetursson, B.E.; Zwahlen, M.; Thomaet, D.S. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin. Oral Implant. Res. 2012, 23, 2–21. [Google Scholar] [CrossRef]
- Goodacre, C.J.; Bernal, G.; Rungcharassaeng, K.; Kan, J.Y.K. Clinical complications with implants. J. Prosthet. Dent. 2003, 90, 121–132. [Google Scholar] [CrossRef]
- Schwarz, F.; Derks, J.; Monje, A.; Wang, H.L. Peri-implantitis. J. Clin. Periodontol. 2018, 45 (Suppl. 20), S246–S266. [Google Scholar] [CrossRef]
- Martin, W.C.; Woody, R.D.; Miller, A.W. Implant abutment screw rotations and preloads for four different screw materials and surfaces. J. Prosthet. Dent. 2001, 86, 24–32. [Google Scholar] [CrossRef]
- Bulaqi, H.A.; Mashhadi, M.M.; Geramipanah, F.; Safari, H.; Paknejad, M. Effect of the coefficient of friction and tightening speed on the preload induced at the dental implant complex with the finite element method. J. Prosthet. Dent. 2015, 113, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Haack, J.E.; Sakaguchi, R.L.; Sun, T.; Coffey, J.P. Elongation and preload stress in dental implant abutment screws. Int. J. Oral Maxillofac. Implant. 1995, 10, 529–536. [Google Scholar]
- Sagheb, K.; Görgen, G.I.; Döll, S.; Schmidtmann, I.; Wentaschek, S. Preload and friction in an implant-abutment-screw complex including a carbon-coated titanium alloy abutment screw: An in vitro study. Int. J. Implant Dent. 2023, 9, 8. [Google Scholar] [CrossRef]
- Varvara, G.; Sinjari, B.; Caputi, S.; Scarano, A.; Piattelli, M. The Relationship Between Time of Retightening and Preload Loss of Abutment Screws for Two Different Implant Designs: An In Vitro Study. J. Oral Implantol. 2020, 46, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Sun, M.; Shui, Y.; Zhang, Y.; Ma, R.; Zhao, Y.; Chen, H.; Yu, P.; Li, T.; Wu, T.; Yu, H. Influence of Abutment Screw-Tightening Methods on the Screw Joint: Immediate and Long-Term Stability. Int. J. Dent. 2024, 2024, 5768318. [Google Scholar] [CrossRef]
- Kwon, J.H.; Son, Y.H.; Han, C.H.; Kim, S. Accuracy of implant impressions without impression copings: A three-dimensional analysis. J. Prosthet. Dent. 2011, 105, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Coelho, L.; Mendes, J.M.; Mendes, J.; Aroso, C.; Silva, A.S.; Manzanares-Céspedes, M. Preload and Removal Torque of Two Different Prosthetic Screw Coatings—A Laboratory Study. Materials 2024, 17, 1414. [Google Scholar] [CrossRef]
- Merz, B.R.; Hunenbar, S.; Belser, U.C. Mechanics of the implant-abutment connection: An 8-degree taper compared to a butt joint connection. Int. J. Oral Maxillofac. Implant. 2000, 15, 519–526. [Google Scholar]
- Hung, H.C.; Huang, C.S.; Pan, Y.H. The compressive strength of implant-abutment complex with different connection designs. J. Dent. Sci. 2019, 14, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Binon, P.P. The effect of implant/abutment hexagonal misfit on screw joint stability. Int. J. Prosthodont. 1996, 9, 149–160. [Google Scholar]
- Angermair, J.; Iglhaut, G.; Meyenberg, K.; Wiest, W.; Rack, A.; Zabler, S.; Fretwurst, T.; Nelson, K.; Kernen, F. In vitro assessment of internal implant-abutment connections with different cone angles under static loading using synchrotron-based radiation. BMC Oral Health 2024, 24, 396. [Google Scholar] [CrossRef]
- Camps-Font, O.; Rubianes-Porta, L.; Valmaseda-Castellón, E.; Jung, R.E.; Gay-Escoda, C.; Figueiredo, R. Comparison of external, internal flat-to-flat, and conical implant abutment connections for implant-supported prostheses: A systematic review and network meta-analysis of randomized clinical trials. J. Prosthet. Dent. 2023, 130, 327–340. [Google Scholar] [CrossRef]
- Soleimani, M.; Żmudzki, J.; Pakieta, W.; Jaśkowska, A.; Krasny, K. Dental Implant Abutment Screw Loss: Presentation of 10 Cases. J. Funct. Biomater. 2024, 15, 96. [Google Scholar] [CrossRef]
- Levartovsky, S.; Ronen, G.; Raz, P.; Beitlitum, I. Effect of Fluid Contamination on Reverse Torque of Healing Abutments in Two Implant Connection Systems: In Vitro Study. Clin. Implant Dent. Relat. Res. 2025, 27, e70056. [Google Scholar] [CrossRef] [PubMed]
- Tsuge, T.; Hagiwara, Y. Influence of lateral-oblique cyclic loading on abutment screw loosening of internal and external hexagon implants. Dent. Mater. J. 2009, 28, 373–381. [Google Scholar] [CrossRef]
- Kim, W.H.; Song, E.S.; Ju, K.W.; Lim, D.; Han, D.-W.; Jung, T.-G.; Jeong, Y.-H.; Lee, J.-H.; Kim, B. Mechanical Assessment of Fatigue Characteristics between Single- and Multi-Directional Cyclic Loading Modes on a Dental Implant System. Materials 2020, 13, 1545. [Google Scholar] [CrossRef]
- Kwan, J.C. An In Vitro Study of Torque Application in Abutment Screw Tightening at the Implant-Abutment Junction in Simulated Osseointegrated Implants. Int. J. Oral Maxillofac. Implant. 2025, 1–27. [Google Scholar] [CrossRef] [PubMed]
- ISO 14801; Dentistry—Implants—Dynamic Fatigue Test for Endosseous Dental Implants. International Organization for Standardization: Geneva, Switzerland, 2016.
- Satpathy, M.; Duan, Y.; Betts, L.; Priddy, M.; Griggs, J.A. Effect of Bone Remodeling on Dental Implant Fatigue Limit Predicted Using 3D Finite Element Analysis. J. Dent. Oral. Epidemiol. 2022, 2, 10-54289. [Google Scholar] [CrossRef]
- Bickford, J.H. Introduction to the Design and Behavior of Bolted Joints, 3rd ed.; CRC Press: Boca Raton, FL, USA, 2008; pp. 213–267. [Google Scholar]
- Tonin, B.S.H.; He, Y.; Ye, N.; Chew, H.P.; Fok, A. Effects of tightening torque on screw stress and formation of implant-abutment microgaps: A finite element analysis. J. Prosthet. Dent. 2022, 127, 882–889. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.H.; Wu, Y.L.; Chen, H.S.; Lin, C.P.; Wu, A.Y.J. Reverse Torque Value of Angulated Screw Channel Abutment before and after Cyclic Loading: An In Vitro Study. J. Funct. Biomater. 2023, 14, 124. [Google Scholar] [CrossRef]
- Tallarico, M.; Lee, S.-Y.; Cho, Y.-J.; Noh, K.-T.; Chikahiro, O.; Aguirre, F.; Uzgur, R.; Noè, G.; Cervino, G.; Cicciù, M. Prosthetic Guidelines to Prevent Implant Fracture and Peri-Implantitis: A Consensus Statement from the Osstem Implant Community. Prosthesis 2025, 7, 65. [Google Scholar] [CrossRef]
- Manfredini, M.; Poli, P.P.; Giboli, L.; Beretta, M.; Maiorana, C.; Pellegrini, M. Clinical Factors on Dental Implant Fractures: A Systematic Review. Dent. J. 2024, 12, 200. [Google Scholar] [CrossRef]
- Fernández-Asián, I.; García-Rubio, C.; Serrera-Figallo, M.-Á.; Torres-Lagares, D.; Gutiérrez-Pérez, J.-L. Relationship Between Implant Connection and Mechanical Complications/Fracture: A Systematic Review. Bioengineering 2025, 12, 333. [Google Scholar] [CrossRef]

| Tightening Torque (Ncm) | TSIII (Mean ± SD) | KSIII (Mean ± SD) | p-Value |
|---|---|---|---|
| 20 | 16.4 ± 0.3 | 18.2 ± 0.3 | 0.002 |
| 25 | 19.3 ± 0.3 | 20.8 ± 0.3 | 0.004 |
| 30 | 23.1 ± 0.7 | 27.1 ± 0.2 | <0.001 |
| 35 | 30.3 ± 0.3 | 33.1 ± 0.3 | 0.001 |
| 40 | 29.3 ± 1.1 | 32.2 ± 0.6 | 0.006 |
| Tightening Torque (Ncm) | TSIII (Mean ± SD) | KSIII (Mean ± SD) | p-Value |
|---|---|---|---|
| 20 | 7.9 ± 0.2 | 14.0 ± 0.4 | <0.001 |
| 25 | 10.1 ± 0.5 | 17.4 ± 0.2 | <0.001 |
| 30 | 14.0 ± 0.6 | 21.5 ± 0.4 | <0.001 |
| 35 | 19.2 ± 0.6 | 26.9 ± 0.5 | 0.002 |
| 40 | 18.1 ± 0.7 | 24.7 ± 0.8 | 0.003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-T.; Lee, J.-C.; Han, D.-W.; Kim, B. Effect of Abutment Screw Design on Torque Loss Under Cyclic Fatigue Loading: A Comparison of TSIII and KSIII Implant Systems. Bioengineering 2025, 12, 1131. https://doi.org/10.3390/bioengineering12101131
Lee J-T, Lee J-C, Han D-W, Kim B. Effect of Abutment Screw Design on Torque Loss Under Cyclic Fatigue Loading: A Comparison of TSIII and KSIII Implant Systems. Bioengineering. 2025; 12(10):1131. https://doi.org/10.3390/bioengineering12101131
Chicago/Turabian StyleLee, Jung-Tae, Jae-Chang Lee, Dong-Wook Han, and Bongju Kim. 2025. "Effect of Abutment Screw Design on Torque Loss Under Cyclic Fatigue Loading: A Comparison of TSIII and KSIII Implant Systems" Bioengineering 12, no. 10: 1131. https://doi.org/10.3390/bioengineering12101131
APA StyleLee, J.-T., Lee, J.-C., Han, D.-W., & Kim, B. (2025). Effect of Abutment Screw Design on Torque Loss Under Cyclic Fatigue Loading: A Comparison of TSIII and KSIII Implant Systems. Bioengineering, 12(10), 1131. https://doi.org/10.3390/bioengineering12101131









