Single versus Double Plate Fixation in Condylar Neck Fractures: Clinical Results and Biomechanics Simulation
Abstract
1. Introduction
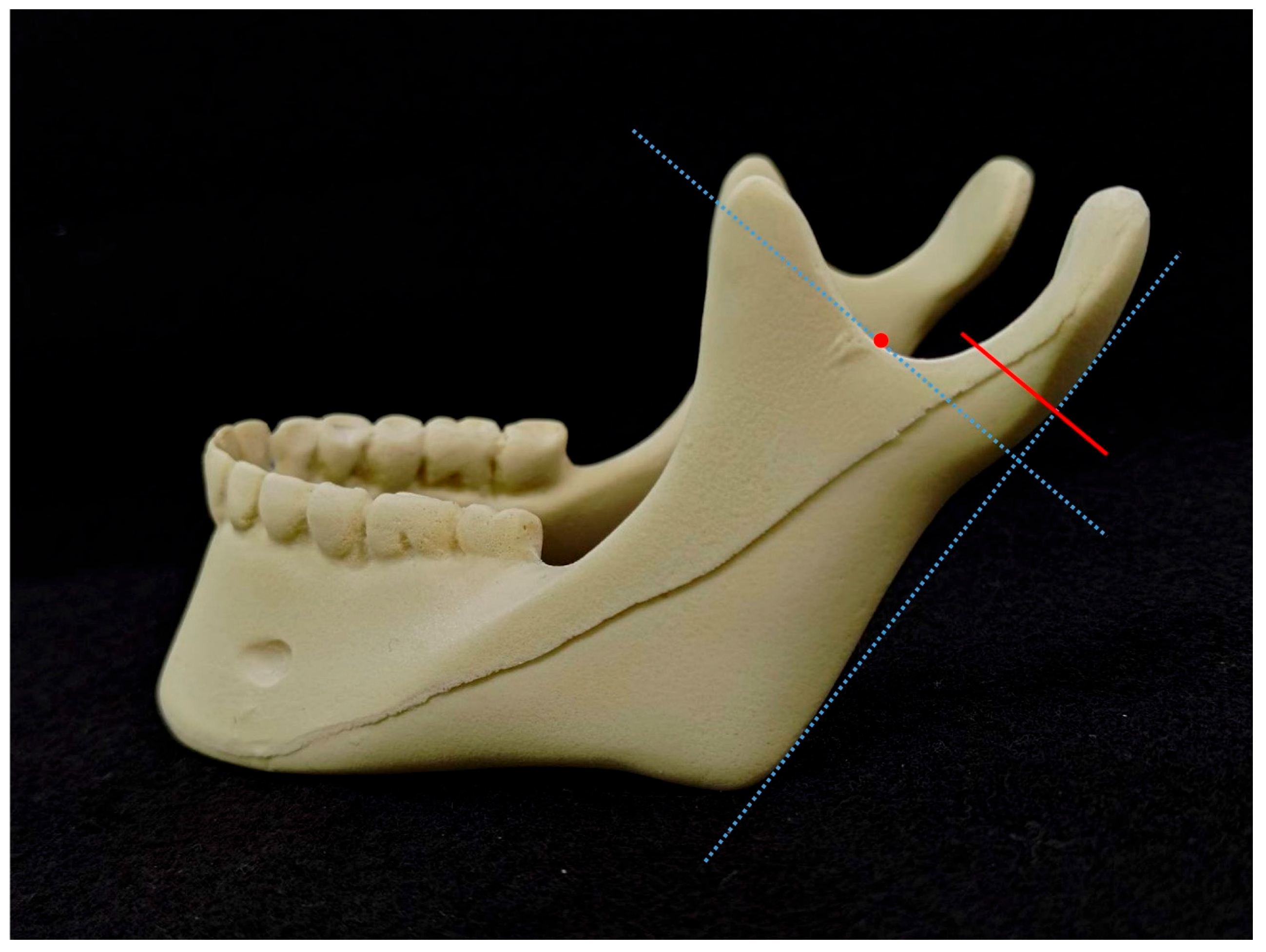
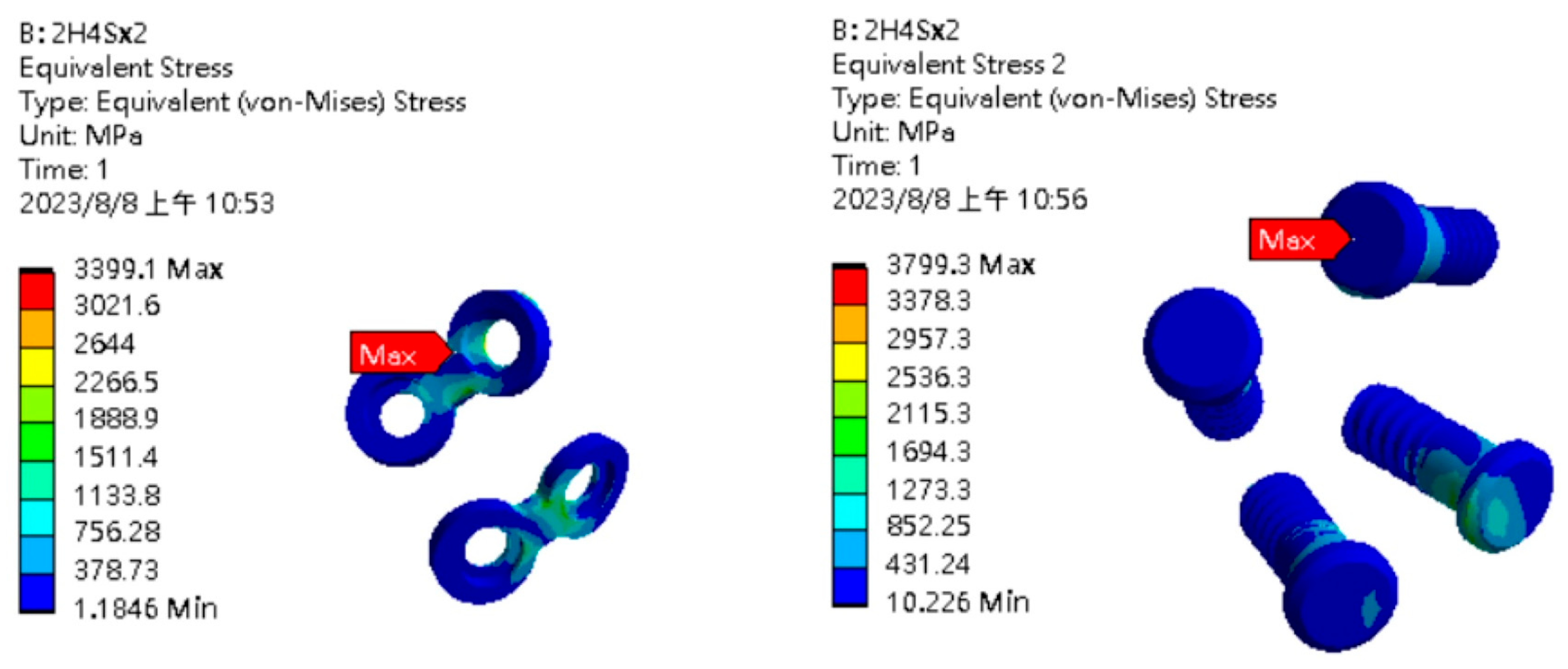
2. Materials and Methods
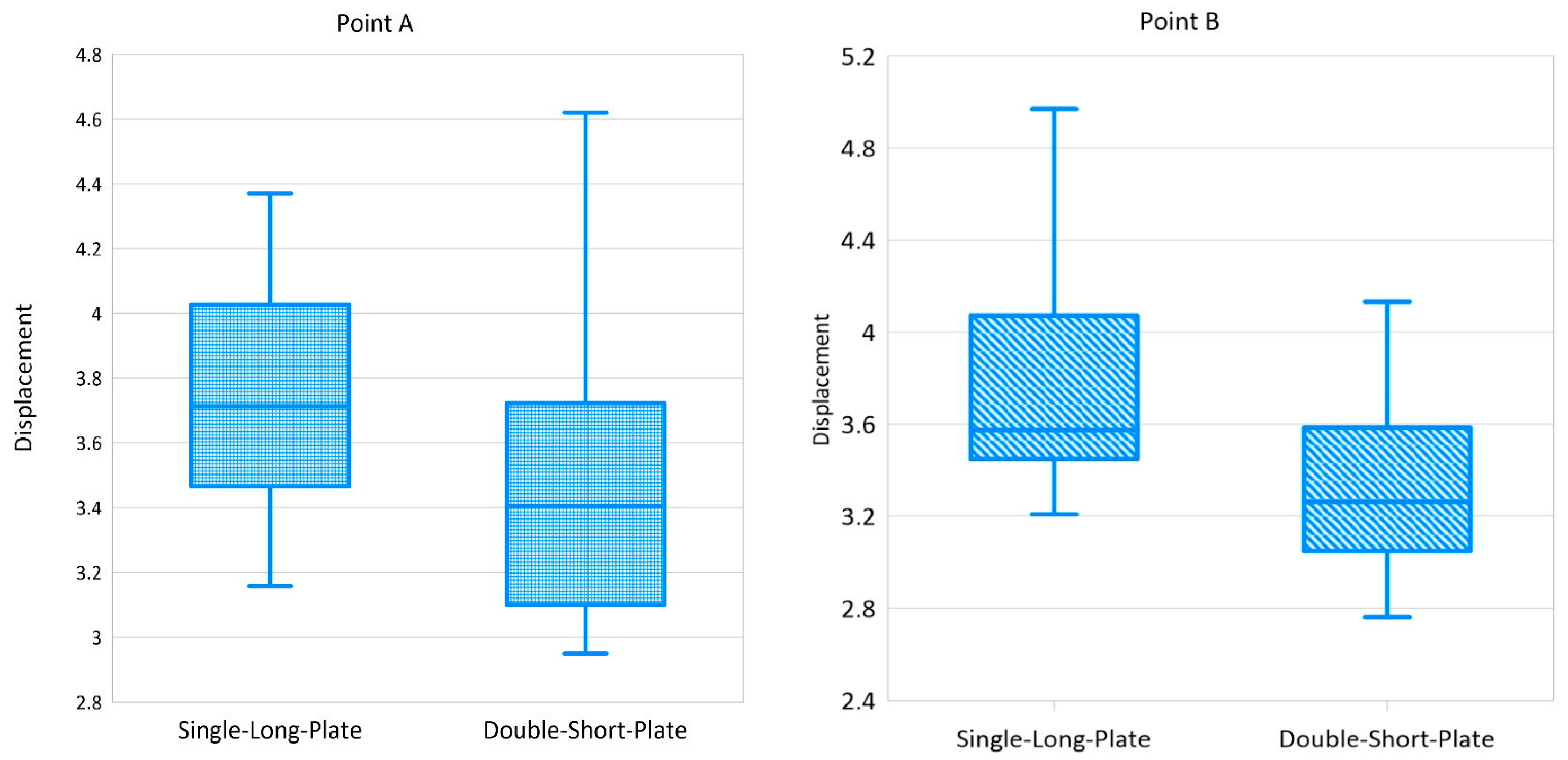
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Throckmorton, G.S.; Ellis, E., 3rd; Hayasaki, H. Masticatory Motion after Surgical or Nonsurgical Treatment for Unilateral Fractures of the Mandibular Condylar Process. J. Oral Maxillofac. Surg. 2004, 62, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E.; Throckmorton, G.S. Treatment of Mandibular Condylar Process Fractures: Biological Considerations. J. Oral Maxillofac. Surg. 2005, 63, 115–134. [Google Scholar] [CrossRef] [PubMed]
- Mooney, S.; Gulati, R.D.; Yusupov, S.; Butts, S.C. Mandibular Condylar Fractures. Facial Plast. Surg. Clin. N. Am. 2022, 30, 85–98. [Google Scholar] [CrossRef] [PubMed]
- Jazayeri, H.E.; Lopez, J.; Khavanin, N.; Xun, H.; Lee, U.K.; Best, D.L.; Reategui, A.; Urata, M.M.; Dorafshar, A.H. Comparative Benefits of Open versus Closed Reduction of Condylar Fractures: A Systematic Review and Meta-Analysis. Plast. Reconstr. Surg. 2023, 151, 664e–672e. [Google Scholar] [CrossRef] [PubMed]
- Tabatabaee, A.; Javanbakht, A.; Mohammadi, K.M.; Shahsavari, P.M.; Dehabadi, F. Comparison of Therapeutic Results of Closed and Open Repair of Mandibular Condylar Fractures. Int. J. Burn. Trauma 2021, 11, 385–390. [Google Scholar]
- Darwich, M.A.; Albogha, M.H.; Abdelmajeed, A.; Darwich, K. Assessment of the Biomechanical Performance of 5 Plating Techniques in Fixation of Mandibular Subcondylar Fracture Using Finite Element Analysis. J. Oral Maxillofac. Surg. 2016, 74, 794.e1–794.e8. [Google Scholar] [CrossRef] [PubMed]
- Çimen, E.; Önder, M.E.; Cambazoğlu, M.; Birant, E. Comparison of Different Fixation Types Used in Unilateral Mandibular Condylar Fractures: An In Vivo Study with New Biomechanical Model. J. Craniofac. Surg. 2016, 27, 1277–1281. [Google Scholar] [CrossRef]
- Marwan, H.; Sawatari, Y. What Is the Most Stable Fixation Technique for Mandibular Condyle Fracture? J. Oral Maxillofac. Surg. 2019, 77, 2522.e1–2522.e12. [Google Scholar] [CrossRef] [PubMed]
- Shih, K.S.; Hsu, C.C. Three-Dimensional Musculoskeletal Model of the Lower Extremity: Integration of Gait Analysis Data with Finite Element Analysis. J. Med. Biol. Eng. 2022, 42, 436–444. [Google Scholar] [CrossRef]
- Chang, L.R.; Hou, Y.P.; Lin, T.S. Is Perpendicular Double Two-Hole Plates Fixation Superior to Single Four-Hole Plate Fixation to Treat Mandibular Symphysis Fracture?—A Finite Element Study. Appl. Sci. 2021, 11, 8629. [Google Scholar] [CrossRef]
- Lin, T.S.; Chiu, T.F.; Hsu, J.T.; Chen, C.C.; Chang, L.R.; Huang, H.L. Biomechanical Evaluation and Factorial Analysis of the 3-Dimensional Printing Self-Designed Metallic Reconstruction Plate for Mandibular Segmental Defect. J. Oral Maxillofac. Surg. 2022, 80, 775–783. [Google Scholar] [CrossRef] [PubMed]
- Calvert, K.L.; Trumble, K.P.; Webster, T.J.; Kirkpatrick, L.A. Characterization of Commercial Rigid Polyurethane Foams Used as Bone Analogs for Implant Testing. J. Mater. Sci. Mater. Med. 2010, 21, 1453–1461. [Google Scholar] [CrossRef]
- Hsu, J.T.; Huang, H.L.; Chang, C.H.; Tsai, M.T.; Hung, W.C.; Fuh, L.J. Relationship of Three-Dimensional Bone-to-Implant Contact to Primary Implant Stability and Peri-Implant Bone Strain in Immediate Loading: Microcomputed Tomographic and in Vitro Analyses. Int. J. Oral Maxillofac. Implants 2013, 28, 367–374. [Google Scholar] [CrossRef]
- Neff, A.; Cornelius, C.P.; Rasse, M.; Torre, D.D.; Audigé, L. The Comprehensive AOCMF Classification System: Condylar Process Fractures–Level 3 Tutorial. Craniomaxillofac. Trauma Reconstr. 2014, 7 (Suppl. S1), S044–S058. [Google Scholar] [CrossRef] [PubMed]
- Verhulp, E.; van Rietbergen, B.; Huiskes, R. A Three-Dimensional Digital Image Correlation Technique for Strain Measurements in Microstructures. J. Biomech. 2004, 37, 1313–1320. [Google Scholar] [CrossRef] [PubMed]
- Zachariades, N.; Mezitis, M.; Mourouzis, C.; Papadakis, D.; Spanou, A. Fractures of the Mandibular Condyle: A Review of 466 Cases. Literature Review, Reflections on Treatment and Proposals. J. Craniomaxillofac. Surg. 2006, 34, 421–432. [Google Scholar] [CrossRef] [PubMed]
- McLeod, N.M.; Keenan, M. Towards a Consensus for Classification of Mandibular Condyle Fractures. J. Cranio-Maxillo-Fac. Surg. 2021, 49, 251–255. [Google Scholar] [CrossRef] [PubMed]
- Loukota, R.A.; Eckelt, U.; De Bont, L.; Rasse, M. Subclassification of Fractures of the Condylar Process of the Mandible. Br. J. Oral Maxillofac. Surg. 2005, 43, 72–73. [Google Scholar] [CrossRef]
- Loukota, R.A.; Neff, A.; Rasse, M. Nomenclature/Classification of Fractures of the Mandibular Condylar Head. Br. J. Oral Maxillofac. Surg. 2010, 48, 477–478. [Google Scholar] [CrossRef]
- MacLennan, W.D. Consideration of 180 cases of typical fractures of the mandibular condylar process. Br. J. Plast. Surg. 1952, 5, 122–128. [Google Scholar] [CrossRef]
- Spiessl, B. Rigid Internal Fixation of Fractures of the Lower Jaw. Reconstr. Surg. Traumatol. 1972, 13, 124–140. [Google Scholar] [PubMed]
- Lindahl, L. Condylar Fractures of the Mandible. I. Classification and Relation to Age, Occlusion, and Concomitant injuries of Teeth and Teeth-Supporting Structures, and Fractures of the Mandibular Body. Int. J. Oral Surg. 1977, 6, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Girhe, V.; Patil, V.; Bhujbal, R.; Singh, R.; Dewang, P.; Vaprani, G. Pre-auricular Transparotid Approach for the Management of Mandibular Condylar Fracture: An Experience of 82 Cases. J. Oral Maxillofac. Surg. 2022, 21, 916–922. [Google Scholar] [CrossRef]
- Bischoff, E.L.; Carmichael, R.; Reddy, L.V. Plating Options for Fixation of Condylar Neck and Base Fractures. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2017, 25, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Chang, L.R.; Chen, C.C.; Jeng, S.F.; Chen, Y.R.; Hwang, L.C.; Lin, T.S. Investigation of a Modified Novel Technique in Bilateral Sagittal Splitting Osteotomy Fixation: Finite Element Analysis and In Vitro Biomechanical Test. BioMed Res. Int. 2020, 2020, 8707389. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.H.; Kim, K.N.; Kim, H.J.; Kim, M.K. Evaluation of Condylar Neck Fracture Plating Techniques. J. Cranio-Maxillo-Fac. Surg. 1999, 27, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.S.; Rehman, S.A.; Ansari, M.K.; Khan, A.A.; Farooq, O.; Khan, A.H. A Comparative Study on evaluation of Role of 1.5 mm Microplates and 2.0 mm Standard Miniplates in Management of Mandibular Fractures Using Bite Force as Indicator of Recommendation. Natl. J. Maxillofac. Surg. 2016, 7, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Patano, A.; Inchingolo, A.M.; Riccaldo, L.; Morolla, R.; Netti, A.; Azzollini, D.; Inchingolo, A.D.; Palermo, A.; Lucchese, A.; et al. Analysis of Mandibular Muscle Variations Following Condylar Fractures: A Systematic Review. J. Clin. Med. 2023, 12, 5925. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.N.A.; Girish, G.; Akarsh, R.; Nikhila, G.; Bhat, P.; Shabadi, N. Comparative Evaluation of Bite Force in Patients Treated for Unilateral Mandibular Condylar Fractures by Open and Closed Methods. Dent. Traumatol. 2022, 38, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, V.; Gupta, H.; Gupta, S.; Ghosh, S. Evaluation of Occlusal Forces Using T Scan Analysis Following Mandibular Fracture Fixation. Natl. J. Maxillofac. Surg. 2023, 14, 35–40. [Google Scholar] [CrossRef]



| Single-Long-Plate | Double-Short-Plate | p Value | |
|---|---|---|---|
| Malocclusion | 11.1% (1/9) | 8.3% (1/12) | p = 1.00 |
| Transient facial palsy | 33.3% (3/9) | 33.3% (4/12) | p = 1.00 |
| Point A | Point B | |||
|---|---|---|---|---|
| Group | Single-Long-Plate | Double-Short-Plate | Single-Long-Plate | Double-Short-Plate |
| Mean | 3.838 | 3.314 | 3.867 | 3.157 |
| S.D. | 0.603 | 0.761 | 0.678 | 0.754 |
| p Value | p = 0.112 | p = 0.043 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, C.-C.; Chiu, T.-H.; Yan, C.-Y.; Hou, Y.-P.; Lin, T.-S. Single versus Double Plate Fixation in Condylar Neck Fractures: Clinical Results and Biomechanics Simulation. Bioengineering 2024, 11, 704. https://doi.org/10.3390/bioengineering11070704
Chen C-C, Chiu T-H, Yan C-Y, Hou Y-P, Lin T-S. Single versus Double Plate Fixation in Condylar Neck Fractures: Clinical Results and Biomechanics Simulation. Bioengineering. 2024; 11(7):704. https://doi.org/10.3390/bioengineering11070704
Chicago/Turabian StyleChen, Chien-Chung, Ting-Han Chiu, Cheng-Yu Yan, Ya-Pei Hou, and Ting-Sheng Lin. 2024. "Single versus Double Plate Fixation in Condylar Neck Fractures: Clinical Results and Biomechanics Simulation" Bioengineering 11, no. 7: 704. https://doi.org/10.3390/bioengineering11070704
APA StyleChen, C.-C., Chiu, T.-H., Yan, C.-Y., Hou, Y.-P., & Lin, T.-S. (2024). Single versus Double Plate Fixation in Condylar Neck Fractures: Clinical Results and Biomechanics Simulation. Bioengineering, 11(7), 704. https://doi.org/10.3390/bioengineering11070704






