The Role of AI in Hospitals and Clinics: Transforming Healthcare in the 21st Century
Abstract
1. Introduction
2. AI in Clinical Decision-Making
2.1. AI Algorithms for Diagnosis and Prognosis
- Machine learning (ML): ML algorithms learn from data to make predictions or decisions without being explicitly programmed for the task [18]. In healthcare, supervised learning algorithms have been instrumental in developing predictive models for patient outcomes based on historical data [19]. Unsupervised learning, on the other hand, is used to identify patterns or clusters within data, useful in discovering novel disease subtypes [20]. Reinforcement learning, where algorithms learn to make sequences of decisions by trial and error, has potential in personalized treatment optimization [21].
- Deep learning (DL): A subset of ML, deep learning uses neural networks with multiple layers (hence “deep”) to analyze complex data structures. Convolutional Neural Networks (CNNs) are particularly effective in processing imaging data, making them invaluable for diagnosing diseases from medical images like X-rays or MRIs [22]. Some other advanced CNN architectures include Residual Network (ResNet), Inception, Visual Geometry Group (VGG), and Graph Convolutional Networks (GCNs), each with its own strengths and applications in image analysis, classification, and graph data processing [23]. Recurrent Neural Networks (RNNs), known for their ability to handle sequential data, are used for analyzing time-series data, such as physiological signals collected during patient monitoring, to predict health deteriorations or outcomes over time [24]. For instance, Long Short-Term Memory (LSTM) networks, a sophisticated variant of RNNs, have been extensively utilized in the detection of sleep apnea using polysomnography data [25]. Additionally, Transformer models, such as BERT (Bidirectional Encoder Representations from Transformers) and GPT (Generative Pre-trained Transformer), offer revolutionary approaches to processing natural language in clinical notes, enabling more accurate extraction of patient information and insights. Generative Adversarial Networks (GANs) [26] and conditional diffusion models [27] have emerged as a powerful tool for generating synthetic medical images for training without privacy concerns, while Graph Neural Networks (GNNs) are unlocking new possibilities in modeling complex biological and health-related networks, from predicting protein interactions to understanding disease pathways.
- 3.
- Natural language processing (NLP): NLP algorithms allow computers to understand and interpret human language. In healthcare, NLP is used to extract meaningful information from unstructured data sources like clinical notes or the research literature, aiding in both diagnostic processes and the aggregation of knowledge for prognosis estimation [33]. An example of such a language model is the GatorTron [34]. It is a large-scale Transformer-based NLP model tailored for the healthcare domain. It utilizes the Transformer architecture, known for its efficiency in handling sequence-to-sequence tasks and its ability to process large datasets, to interpret and analyze electronic health records. With its 8.9 billion parameters, GatorTron is trained on over 90 billion words of clinical text, making it a highly advanced model for extracting and understanding complex medical information from unstructured data sources.
2.2. Case Studies of AI in Detecting Diseases
- Cancer detection: One of the most groundbreaking applications of AI is in the early detection of cancer. A notable case study involves the use of deep learning algorithms in the analysis of mammograms for breast cancer detection. Research has shown that AI can identify patterns in mammographic images that are indicative of cancerous growths, often with greater accuracy than traditional methods. A notable study published in the journal Nature reported the development of an AI model by Google Health [35]. This model was trained on a large dataset of mammograms and demonstrated the ability to detect breast cancer more accurately than human radiologists. The AI system showed a reduction in both false positives and false negatives, key factors in cancer diagnostics. This progress in AI technology is significant because early detection of breast cancer can dramatically improve prognosis and treatment outcomes.
- Diabetes management: AI’s role in managing and detecting diabetes, particularly through machine learning algorithms, is a significant area of improvement in healthcare. These algorithms can analyze patient data to predict the onset and progression of diabetes and its complications, as demonstrated in different studies.In one study, several supervised classification algorithms were applied to predict and classify eight diabetes complications, including metabolic syndrome, dyslipidemia, neuropathy, nephropathy, diabetic foot, hypertension, obesity, and retinopathy [36]. The dataset utilized in this study comprises 79 input attributes, including results of medical tests and demographic information collected from 884 patients. The performance of the models was evaluated using the accuracy and F1 score, reaching a maximum of 97.8% and 97.7%, respectively. Among different classifiers, random forest (RF), Adaboost, and XGBoost achieved the best performance. This high level of accuracy demonstrates the potential of machine learning in effectively predicting diabetes complications.Another study focused on evaluating the efficacy of machine learning algorithms in predicting complications and poor glycemic control in nonadherent type 2 diabetes patients [37]. This real-world study used data from 800 type 2 diabetes patients, of which 165 met the inclusion criteria. Different machine learning algorithms were used to develop prediction models, with the predictive performance assessed using the area under the curve. The highest performance scores for predicting various complications such as diabetic nephropathy, neuropathy, angiopathy, and eye disease were 90.2%, 85.9%, 88.9%, and 83.2%, showcasing the effectiveness of these models.
- Heart disease prediction: The prediction of heart disease using AI represents a significant advancement in cardiovascular healthcare. This application not only aims to predict the occurrence of heart disease but also attempts to determine its severity, a crucial factor in effective treatment and management.One innovative study in this area focused on a machine learning-based prediction model that performs both binary and multiple classifications of heart disease [38]. The model, known as Fuzzy-GBDT, integrates fuzzy logic with a gradient boosting decision tree to streamline data complexity and improve prediction accuracy. Additionally, to avoid overfitting, the model incorporates a bagging technique, enhancing its capability to classify the severity of heart disease. The evaluation results of this model show excellent accuracy and stability in predicting heart disease, demonstrating its potential as a valuable tool in healthcare.Another interesting study introduces a cutting-edge healthcare system that employs ensemble deep learning coupled with feature fusion approaches [39]. This system is designed to overcome the limitations of traditional machine learning models that struggle with high-dimensional datasets. It achieves this by integrating sensor data with electronic medical records, creating a more holistic dataset for heart disease prediction. The system uses the information gain technique to streamline this dataset, focusing on the most relevant features and thereby reducing computational complexity. A key aspect of this model is the application of conditional probability for precise feature weighting, enhancing the overall performance of the system. Impressively, this ensemble deep learning model achieved an accuracy of 98.5%, outperforming existing models and illustrating its efficacy in heart disease prediction.
- AI in neurological disorders: The integration of AI, particularly deep learning (DL), in neurology has opened new avenues for the diagnosis and management of neurological disorders. The recent literature reveals significant progress in employing AI for the early detection and more accurate diagnosis of various conditions, including AD.One area of notable advancement is the use of deep learning in neuroimaging studies. DL’s ability to process and learn from raw data through complex, nonlinear transformations makes it well suited for identifying the subtle and diffuse alterations characteristic of many neurological and psychiatric disorders. Research in this domain has shown that DL can be a powerful tool in the ongoing search for biomarkers of such conditions, offering potential breakthroughs in understanding and diagnosing brain-based disorders [40].Furthering this progress, a comprehensive review of deep learning techniques in the prognosis of a range of neuropsychiatric and neurological disorders, such as stroke, Alzheimer’s, Parkinson’s, epilepsy, autism, migraine, cerebral palsy, and multiple sclerosis, has underscored deep learning’s versatility in addressing real-life challenges across various domains, including disease diagnosis [41]. In the specific case of Alzheimer’s Disease (AD), the most common cause of dementia, deep learning has shown promise in enhancing diagnosis accuracy. Utilizing Convolutional Neural Networks (CNNs), researchers have developed frameworks for detecting AD characteristics from Magnetic Resonance Imaging (MRI) data [42]. By considering different stages of dementia and creating high-resolution disease probability maps, these models provide intuitive visualizations of individual AD risk. This approach, especially when addressing class imbalance in datasets, has achieved high accuracy, surpassing existing methods. The adaptation of such models to extensive datasets like the Alzheimer’s Disease Neuroimaging Initiative (ADNI) further validates their effectiveness in predicting AD classes.
- Key insights: These case studies highlight AI’s significant role in advancing disease detection across multiple medical disciplines, offering accurate and timely diagnoses, often through non-invasive methods. However, as AI technology continues to evolve, there is a critical need for addressing challenges such as data privacy, algorithmic transparency, and ensuring equitable access to these technologies. Future developments should focus on creating more robust AI systems that can handle diverse datasets, thereby reducing potential biases in diagnosis. Additionally, integrating AI with traditional diagnostic methods and enhancing interdisciplinary collaboration among technologists, clinicians, and patients will be key to harnessing AI’s full potential in disease detection and management.
2.3. The Role of AI in Personalized Medicine
- Tailoring treatments to genetic profiles: One of the most significant applications of AI in personalized medicine is in the field of genomics. AI algorithms can analyze vast genomic datasets to identify mutations and variations that might influence an individual’s response to certain treatments. For example, in oncology, AI helps in identifying specific genetic markers that are susceptible to targeted cancer therapies. This approach increases the efficacy of the treatment and minimizes the risk of adverse reactions, ensuring a more effective and safer treatment plan for the patient.A prime example of this application is a study focusing on nonmuscle invasive urothelial carcinoma, a type of bladder cancer known for its high recurrence risk [43]. In this study, researchers employed a machine learning algorithm to analyze genomic data from patients at their initial presentation. They aimed to identify genes most predictive of recurrence within five years following transurethral resection of the bladder tumor. The study involved whole-genome profiling of 112 frozen nonmuscle invasive urothelial carcinoma specimens using Human WG-6 BeadChips. A genetic programming algorithm was then applied to evolve classifier mathematical models for outcome prediction. The process involved cross-validation-based resampling and assessing gene use frequencies to pinpoint the most prognostic genes. These genes were subsequently combined into rules within a voting algorithm to predict the likelihood of cancer recurrence. Of the genes analyzed, 21 were identified as predictive of recurrence. Further validation through the quantitative polymerase chain reaction was conducted on a subset of 100 patients. The results were promising: a five-gene combined rule using the voting algorithm showed 77% sensitivity and 85% specificity in predicting recurrence in the training set. Additionally, a three-gene rule was developed, offering 80% sensitivity and 90% specificity in the training set for recurrence prediction.
- Predictive analytics in drug development: AI also plays a crucial role in drug development, particularly in predicting how different patients will respond to a drug. By analyzing historical data from clinical trials and patient records, AI models can predict the effectiveness of drugs on various demographic groups [44,45]. This predictive power is invaluable in designing clinical trials and in developing drugs that are more effective for specific patient populationsIn recent years, AI has made remarkable strides in drug development. Exscientia introduced the first AI-designed drug molecule for clinical trials in early 2020 [46]. DeepMind’s AlphaFold then achieved a breakthrough in July 2021 by predicting structures for over 330,000 proteins, including the entire human genome. In 2022, Insilico Medicine started Phase I trials for an AI-discovered molecule, a process significantly faster and more cost-effective than traditional methods. By 2023, AbSci had innovated in creating antibodies using generative AI, and Insilico Medicine saw an AI-designed drug receive FDA Orphan Drug Designation, with Phase II trials planned shortly thereafter. These milestones mark a transformative era in AI-driven drug discovery.AI’s application extends to the identification of novel proteins or genes as potential disease targets, with systems capable of predicting the 3D structures of these targets using deep learning [47]. AI is also revolutionizing molecular simulations and the prediction of drug properties such as toxicity and bioactivity, enabling high-fidelity simulations that can be run entirely in silico [44]. Moreover, AI is shifting the paradigm of traditional drug discovery from screening large libraries of molecules to generating novel drug molecules from scratch [48]. This approach can enhance the efficiency of the drug discovery process and can lead to the development of novel therapies.
- 3.
- Customizing treatment plans: AI systems are adept at integrating and analyzing various types of health data—from clinical records and lab results to lifestyle information and environmental factors. This capability allows healthcare providers to create more refined and comprehensive treatment plans [49]. For instance, in managing chronic diseases like diabetes, AI can analyze data from wearable devices, diet logs, and blood sugar readings to recommend personalized lifestyle and medication adjustments for better disease management [50].
- 4.
- AI in mental health: In the field of mental health, AI is used to personalize treatment approaches. By monitoring patterns in speech [51], behavior [52], and social media activity [53,54], AI tools can help in identifying the onset of mental health issues and suggest interventions tailored to the individual’s unique situation. This personalized approach is crucial in mental health, where treatment efficacy can vary significantly from person to person.
- 5.
- Key insights: While the integration of AI into personalized medicine offers transformative potential, it also presents a spectrum of challenges that must be addressed. Beyond data privacy and algorithmic bias, significant concerns include interoperability and data integration across diverse healthcare systems [56], ensuring AI systems are compliant with regulatory and ethical standards, and establishing their clinical validity and reliability [57].
3. AI in Hospital Operations and Management
3.1. AI for Hospital Logistics and Resource Management
- Inventory management: AI systems are being used to predictively manage inventory in hospitals [60,61]. By analyzing usage patterns, patient inflow, and other relevant data, AI can forecast the need for medical supplies, medications, and equipment. This predictive capability ensures that hospitals maintain optimal stock levels, reducing wastage and ensuring the availability of critical supplies when needed.
- Facility management: AI also contributes to the efficient management of hospital facilities. For example, AI-powered systems can control heating, ventilation, and air conditioning (HVAC) systems more efficiently, reducing energy costs while maintaining a comfortable environment for patients and staff [62]. Additionally, AI can help in the predictive maintenance of hospital equipment, identifying potential issues before they lead to breakdowns, thus minimizing downtime and repair costs [63].
- Resource allocation: One of the most substantial applications of AI in hospital management is in the optimization of resource allocation [64]. AI algorithms can analyze complex datasets, including patient admissions, staff availability, and operational capacities, to optimize the allocation of human and material resources. This includes scheduling surgeries and medical procedures in a manner that maximizes the utilization of operating rooms and medical staff, while minimizing patient wait times [65].
- Supply chain optimization: AI enhances supply chain operations in hospitals by analyzing trends and automating ordering processes [66,67]. It can anticipate supply chain disruptions and suggest alternative solutions, ensuring that the hospital’s operations are not affected by external supply chain challenges. In emergency situations or during health crises, AI systems play a crucial role in managing logistics and resources [68]. They can quickly analyze the situation, predict the resources required, and assist in the efficient distribution of these resources where they are needed most.
3.2. Automating Administrative Tasks with AI
- Patient data management: AI plays an important role in managing vast amounts of patient data [69]. AI systems can organize, categorize, and process patient records, appointments, and treatment histories with high efficiency and accuracy. These systems can also extract relevant information from unstructured data, such as doctor’s notes, making it easier for healthcare providers to access and analyze patient information. For example, a study utilized AI and natural language processing (NLP) to analyze electronic medical records (EMRs), focusing on uncoded consultation notes for disease prediction [70]. Techniques like bag of words and topic modeling were applied, along with a method to match notes with a medical ontology. This approach was particularly tested for colorectal cancer. The study found that the ontology-based method significantly enhanced predictive performance, with an AUC of 0.870, surpassing traditional benchmarks. This highlights AI’s potential in extracting useful information from EMR’s unstructured data, improving disease prediction accuracy.
- Billing and claims processing: AI algorithms can also be used to automate billing and insurance claims processing. They can quickly analyze and process claims data, identify errors or inconsistencies, and ensure that billing is accurate and compliant with relevant regulations [71]. This not only speeds up the reimbursement process but also reduces the likelihood of billing errors, leading to improved financial operations and patient satisfaction. For example, a study in the insurance sector utilized machine learning to improve loss reserve estimation accuracy, crucial for financial statements [72]. Moving away from traditional macro-level models, this approach used individual claims data, integrating details about policies, policyholders, and claims. The method addressed the challenge of right-censored variables by creating tailored datasets for training and evaluating the algorithms. Compared to the conventional chain ladder method, this AI-driven approach showed notable improvements in accuracy, evidenced by a real case study with a Dutch loan insurance portfolio.
- Scheduling appointments: AI-driven scheduling systems are revolutionizing the way appointments are managed in healthcare settings [73]. These systems can analyze patterns in appointment bookings and cancellations to optimize the scheduling of patients. By predicting peak times and adjusting appointments accordingly, AI helps in reducing wait times and improving patient flow. For example, a project aimed at reducing outpatient MRI no-shows effectively utilized AI predictive analytics [74]. In this quality improvement initiative, over 32,000 anonymized outpatient MRI appointment records were analyzed using machine learning techniques, specifically an XGBoost model, a decision tree-based ensemble algorithm. This approach achieved notable results; the model’s predictive accuracy was demonstrated by an ROC AUC of 0.746 and an optimized F1 score of 0.708. When implemented alongside a practical intervention of telephone call reminders for patients identified as high-risk for no-shows, the no-show rate decreased from 19.3% to 15.9% over six months. In another study, a data-driven approach was used to optimize appointment scheduling and sequencing, especially in environments with uncertain service durations and customer punctuality [75]. Leveraging a novel method based on infinite-server queues, the study developed scalable solutions suitable for complex systems with numerous jobs and servers. Tested using a comprehensive dataset from a cancer center’s infusion unit, this approach significantly improved operational efficiency. The results showed a consistent reduction in costs—combining waiting times and overtime—by 15% to 40%, demonstrating the effectiveness of AI-based strategies in optimizing appointment scheduling.
- Document management and processing: AI technologies are adept at automating the processing of various documents, including consent forms, admission forms, and medical reports [76]. By using natural language processing (NLP) and machine learning, AI can quickly parse through documents, extract relevant information, and categorize them appropriately. This automation reduces the administrative burden on staff and speeds up document processing.
- Automated communication and reminders: A notable application of AI in healthcare is the optimization of information extraction from electronic health records (EHRs), particularly from scanned documents. A study demonstrated this by successfully extracting sleep apnea indicators from scanned sleep study reports using a combination of image preprocessing techniques and natural language processing (NLP) [77]. By employing methods like gray-scaling and OCR with Tesseract, followed by analysis through advanced models like ClinicalBERT, the study achieved high accuracy rates (over 90%) in identifying key health metrics.
- Automated communication and reminders: AI-powered chatbots and virtual assistants are increasingly used for patient communication. They can handle routine inquiries, provide information about services, and send reminders for upcoming appointments or medication schedules. This not only enhances patient engagement but also frees up staff to focus on more critical tasks.An example of this application is seen in the ChronologyMD project [78], which utilized AI to improve eHealth communication programs. The project addressed major deficiencies in existing eHealth communication strategies, which often failed to fully engage audiences and sometimes even negatively impacted the delivery of crucial health information. By strategically employing AI, the ChronologyMD project succeeded in making health communication more engaging, relevant, and actionable. Additionally, it led to increased exposure to relevant messages, reduced the workload of healthcare staff, and improved the overall efficiency of the program while minimizing costs.
- Data security and compliance: AI systems contribute significantly to data security and compliance in healthcare [79]. They can monitor and analyze data access patterns to detect and prevent unauthorized access or breaches. Additionally, AI can ensure that administrative processes are compliant with healthcare regulations, such as HIPAA, thereby safeguarding patient privacy.Building on this, recent research has explored the role of AI in ensuring compliance with the General Data Protection Regulation (GDPR), crucial for data controllers [80]. This study aimed to bridge gaps in compliance checking through a two-pronged approach: firstly, by conceptualizing a framework for document-centric compliance checking in the data supply chain, and secondly, by developing methods to automate the compliance checking of privacy policies. The study tested a two-module system, where the first module uses natural language processing (NLP) to extract data practices from privacy policies, and the second module encodes GDPR rules to ensure the inclusion of all mandatory information. The results demonstrated that this text-to-text approach was more effective than local classifiers, capable of extracting both broad and specific information with a single model. The system’s effectiveness was validated on a dataset of 30 privacy policies, annotated by legal experts.
3.3. AI in Patient Flow and Scheduling Optimization
- Optimizing patient flow: AI algorithms are particularly adept at analyzing patterns in patient admissions, discharges, and transfers, enabling more efficient patient flow throughout the hospital [65,81]. By predicting high-demand periods, AI can assist in preemptively allocating resources such as beds, staff, and equipment to meet patient needs. For instance, AI systems can forecast daily or seasonal fluctuations in patient admissions, allowing hospitals to adjust staffing levels and bed availability accordingly [82]. This proactive approach reduces bottlenecks, minimizes wait times, and enhances the overall patient experience.
- Dynamic scheduling systems: AI-driven scheduling systems revolutionize the way appointments and procedures are organized. These systems can analyze multiple variables, including healthcare provider availability, patient preferences, and urgency of care, to create optimal schedules. By doing so, they reduce appointment no-shows and last-minute cancellations, maximizing the utilization of healthcare professionals’ time. Moreover, these AI systems can adapt in real time to changes, such as emergency cases, by rescheduling non-urgent appointments without significant disruptions [83].In a study aimed at improving outpatient department efficiency and patient satisfaction, researchers developed an innovative appointment scheduling system based on a Markov decision process model, incorporating patient preferences to maximize satisfaction [84]. Adaptive dynamic programming algorithms were utilized to overcome the complexity of scheduling, dynamically adjusting to patient preferences and continuously improving appointment decisions. The system’s performance was evaluated through various experiments, which demonstrated optimal convergence behavior and accuracy.
- Reducing waiting times: One of the critical benefits of AI in patient flow is the reduction in waiting times in emergency departments and outpatient clinics. AI can predict patient inflow and identify potential delays, allowing hospital staff to take proactive measures to manage patient wait times effectively [85,86]. For emergency departments, this means better triage processes and quicker allocation of patients to the appropriate care.Utilizing machine learning algorithms, a recent study predicted patient waiting times before consultation and throughput time in an outpatient clinic, aiming to enhance patient satisfaction by providing more accurate wait time information [87]. The study employed random forest and XGBoost algorithms, analyzing input variables such as gender, day and time of visit, and consultation session. The study achieved high accuracy (86–93%) in predicting wait and throughput times in an outpatient clinic using machine learning models with novel input variables.
- Enhancing patient experience: AI systems can also improve the overall patient experience by providing accurate information about appointment times, wait periods, and treatment schedules [88]. This transparency helps in managing patient expectations and reduces anxiety associated with medical appointments and procedures.In a recent study, a machine learning model was developed to predict patient responses to the “Doctor Communications” domain of the Hospital Consumer Assessment of Healthcare Providers and Systems survey, using data from a tertiary care hospital (2016–2020) [89]. The random forest algorithm effectively predicted patient responses about doctors’ courtesy, explanation clarity, and attentiveness. The model achieved an AUC of 88% for these doctor communication survey questions.
- Integrating with telehealth: In the era of digital health, AI in scheduling extends beyond in-person appointments to include telehealth services. AI systems can effectively schedule and manage virtual consultations, ensuring that patients receive timely care without the need to physically visit the healthcare facility, which is particularly beneficial for routine follow-ups or during health crises like pandemics [90].
4. AI in Medical Imaging and Diagnostics
4.1. AI’s Role in Radiology and Pathology
4.2. Enhancing Accuracy and Efficiency in Diagnostic Processes
- Improving diagnostic accuracy: AI algorithms, particularly those based on deep learning, have demonstrated remarkable accuracy in diagnosing diseases from medical images and test results. These systems are trained on vast datasets, allowing them to recognize patterns and anomalies that might be imperceptible to the human eye. For example, in dermatology, AI systems trained on images of skin lesions have shown the ability to detect skin cancers, such as melanoma, with a level of precision comparable to that of experienced dermatologists [104].
- Reducing diagnostic errors: One of the key benefits of AI in diagnostics is its potential to reduce errors [105]. Misdiagnosis and missed diagnoses are significant concerns in medicine, often leading to delayed or inappropriate treatment. AI systems provide a level of consistency and attention to detail that is challenging for humans to maintain over long periods, thus reducing the likelihood of such errors.
- Speeding up diagnostic processes: AI significantly speeds up the diagnostic process. Analyzing medical images or test results, tasks that would take a healthcare professional considerable time, can be performed by AI in a fraction of the time. This rapid analysis is particularly beneficial in urgent care situations, where quick decision-making is critical. For instance, AI algorithms can quickly analyze CT scans of stroke patients to identify blockages or bleeding in the brain, enabling faster initiation of life-saving treatments [106].
- Automated reporting and documentation: AI not only automates reporting and documentation in diagnostic processes [107] but also enhances the quality of these processes. While AI systems generate preliminary reports from image analysis for radiologist review, streamlining workflow and reducing administrative burden, a recent study has furthered this efficiency by consolidating existing ML reporting guidelines [108]. This study, after an extensive review of 192 articles and expert feedback, created a comprehensive checklist encompassing 37 reporting items for prognostic and diagnostic ML studies. This effort in standardizing ML reporting is pivotal in improving the quality and reproducibility of ML modeling studies, complementing AI’s role in simplifying diagnostic reporting.
- Integrating diagnostic data: AI excels in integrating and analyzing data from various sources. In the case of complex diseases, AI can combine information from imaging, laboratory tests, and patient histories to provide a more comprehensive diagnostic insight [109]. This integration is particularly valuable in diagnosing complex conditions like autoimmune diseases or in cases where symptoms are ambiguous.As an example, a scoping review focused on AI techniques for fusing multimodal medical data, particularly EHR with medical imaging, to develop AI methods for various clinical applications [110]. The review analyzed 34 studies, observing a workflow of combining raw data using ML or DL algorithms for clinical outcome predictions. It found that multimodality fusion models generally outperform single-modality models, with early fusion being the most commonly used technique. Neurological disorders were the dominant category studied, and conventional ML models were more frequently used than DL models. This review provides insights into the current state of multimodal medical data fusion in healthcare research.
4.3. The Role of Hardware Acceleration in AI-Powered Diagnostics
- Graphics Processing Units (GPUs): Originally designed for computer graphics rendering, GPUs excel at parallel processing, making them ideal for handling the massive datasets and complex calculations involved in AI algorithms. In the medical image analysis domain, GPUs can be used to accelerate basic image processing operations such as filtering and interpolation. Additionally, GPUs can enhance the operation of different AI algorithms used in medical imaging tasks like image registration, image segmentation, image denoising, and image classification [113].
- Tensor Processing Units (TPUs): Custom-designed chips like TPUs, pioneered by companies like Google, are specifically optimized for high-performance deep learning inference, a key technique used in medical image analysis. TPUs offer significant speed advantages over CPUs for tasks like image recognition and classification. For example, researchers implemented a system for glaucoma diagnosis using both edge TPUs and embedded GPUs [114]. While both achieved fast image segmentation and classification for real-time diagnosis support, the study found that TPUs consumed significantly less energy compared to GPUs. This makes TPUs a more attractive option for battery-powered medical devices used in edge computing scenarios.
- Field-Programmable Gate Arrays (FPGAs): These versatile chips offer flexibility for hardware customization. Unlike pre-designed GPUs and TPUs, FPGAs can be programmed to perform specific AI algorithms, potentially leading to highly optimized solutions for certain diagnostic tasks. However, programming FPGAs requires specialized expertise. For instance, researchers have proposed a MobileNet accelerator designed specifically for FPGAs that focuses on minimizing on-chip memory usage and data transfer, making it ideal for low-power devices [115]. They achieve this by using two configurable modules for different convolution operations and a new cache usage method. Their implementation demonstrates real-time processing with low memory usage, making FPGAs a viable option for running efficient CNNs in auxiliary medical tasks on portable devices.
- Application-Specific Integrated Circuits (ASICs): When dealing with a well-defined AI algorithm in a specific diagnostic application, ASICs can be designed to offer the ultimate performance [116]. Engineered for a single task, ASICs provide unparalleled efficiency and processing speed for that specific function. However, the lack of flexibility limits their application to well-established and unchanging algorithms.
4.4. Examples of AI Systems Used in Imaging
- AI in MRI analysis: AI applications in MRI analysis are versatile, encompassing the detection of brain abnormalities, tumors, strokes, neurodegenerative diseases, musculoskeletal injuries, cardiac conditions, and liver and abdominal organ pathologies, as well as evaluating breast and prostate cancers, demonstrating its broad utility in diagnosing a wide range of medical conditions [122,123]. In addition, deep learning is now playing a key role in accelerating the MRI acquisition process [92].An example of AI application in MRI is an AI system developed for detecting brain abnormalities [118]. This system uses a deep CNN to analyze MRI images and can identify conditions such as tumors, strokes, and neurodegenerative diseases. The AI not only detects these abnormalities but also helps in quantifying the volume of affected areas, which is vital for treatment planning and monitoring disease progression. Another example is the application of AI in the interpretation of breast cancer. CNNs are employed to extract features from MRI breast scans, and alongside classifiers, they effectively detect the presence of cancer, showcasing the potential of AI in enhancing diagnostic accuracy in breast cancer detection [124].AI systems are increasingly used for the automated segmentation of images in radiology [125]. These systems can differentiate and label various anatomical structures in the images, such as organs and tissues, aiding radiologists in diagnosis and in planning surgeries or treatments. For example, a study introduced a 4D deep learning model, combining 3D convolution and LSTM, for the precise segmentation of hepatocellular carcinoma (HCC) lesions in dynamic contrast-enhanced MRI images [126]. Utilizing both spatial and temporal domain information from multi-phase images, the model significantly improved liver tumor segmentation performance, achieving superior metrics compared to existing models and offering a comparable performance to the state-of-the-art nnU-Net model with reduced prediction time.AI is also being adapted for pediatric imaging, addressing the unique challenges presented by the varying sizes and developmental stages of pediatric patients [127]. AI systems in this domain are tailored to recognize and interpret patterns specific to children, aiding in the diagnosis of congenital and developmental conditions. For instance, in pediatric imaging for focal epilepsy, a deep CNN model was introduced, excelling in tract classification and identifying critical white matter pathways with 98% accuracy [128]. This model effectively predicted surgical outcomes and postoperative language changes, showcasing its potential to enhance preoperative evaluations and improve surgical precision in children.
- AI for CT scan interpretation: AI applications in CT scan interpretation span detecting lung nodules, identifying fractures and hemorrhages, assessing stroke severity, and characterizing tumor progression. One innovative AI application in CT imaging is in the rapid identification of pulmonary embolisms [119]. The AI system processes CT pulmonary angiograms to detect blood clots in the lungs with high accuracy, often faster than traditional methods. This speed is critical in emergency situations, where timely intervention can be life-saving. As another example, Google’s AI, in collaboration with researchers from Northwestern University, NYU-Langone Medical Center, and Stanford Medicine, has developed a CT scan model that diagnoses lung cancer with accuracy equal to or surpassing six radiologists [129]. This model analyzes 3D volumetric scans to predict malignancy and detect subtle lung nodules, viewing the lungs as a single 3D object and comparing scans over time to track lesion growth. Tested on over 45,800 de-identified chest CT screenings, it detected 5% more cancer cases and reduced false positives by over 11% compared to traditional radiologist evaluations, demonstrating significant potential for enhancing lung cancer diagnosis.
- AI in X-ray analysis: AI is revolutionizing X-ray analysis across various medical fields. Take mammography, for instance, AI is transforming breast cancer screening by enhancing image analysis for tumor detection, improving accuracy in identifying benign and malignant lesions, and reducing false positives and negatives, thereby streamlining the diagnostic process for early and effective treatment [130]. These systems analyze mammograms to identify signs of cancerous lesions, with some AI models demonstrating the ability to detect cancers that were initially missed by radiologists. By serving as a second reviewer, these AI systems enhance the accuracy of breast cancer screening. A recent study demonstrated that cmAssist™, an AI-based CAD algorithm based on multiple custom deep learning-based networks, significantly enhanced radiologists’ sensitivity in breast cancer detection [120]. Analyzing 122 mammograms with a blend of false negatives and BIRADS 1 and 2 ratings, radiologists showed a notable improvement in cancer detection rates (CDRs) by an average of 27% when using cmAssist, with a minimal increase in false positives. This marked improvement underscores the potential of AI-CAD software in improving accuracy and sensitivity in breast cancer screening.
- AI in ultrasound: AI is significantly impacting various applications of ultrasound. In cardiac imaging, for example, AI systems are used to analyze images from echocardiography scans to assess cardiovascular function [131]. They can measure parameters such as the ejection fraction, which indicates how well the heart is pumping blood, and detect structural abnormalities of the heart. This information is crucial in diagnosing and managing heart diseases. For example, a study evaluating a novel AI for automated left ventricular ejection time calculation in echocardiography showed high accuracy, closely correlating with cardiac MRI results [121]. The AI, which demonstrated lower bias and greater reliability especially in challenging cases, outperformed conventional methods. This algorithm is based on a patented CNN, though specific details of its architecture and training process remain proprietary. This underscores the algorithm’s potential in reducing user-dependent variability and enhancing the clinical utility of echocardiography.
5. AI in Patient Care and Monitoring
5.1. AI-Powered Wearable Devices for Continuous Monitoring
5.2. Virtual Nursing Assistants
5.3. AI in Telemedicine and Remote Patient Engagement
6. Methodologies for Assessing AI Healthcare Solutions
6.1. Validation
- Algorithm validation: The successful integration of AI algorithms into healthcare hinges on their accuracy, reliability, and performance. This necessitates comprehensive testing using diverse datasets [150]. A critical challenge in this process is overfitting, where the algorithm performs well on the training data but fails to generalize to unseen data. To address this, techniques like cross-validation are employed [151]. Cross-validation involves splitting the training data into multiple folds and iteratively training the algorithm on a subset of folds while using the remaining folds for validation. This process helps assess how well the algorithm generalizes to new data and prevents overfitting. Beyond generalizability, AI in healthcare should be adaptable for personalized use. This means the algorithms should continuously learn from individual patient data to enable tailored treatment approaches. Rigorous assessment helps identify strengths, weaknesses, and areas for improvement, ultimately enhancing the reliability of AI-based healthcare solutions. Furthermore, validation on different patient groups is essential to address potential biases in the training data. Biases can lead to unfair and ineffective outcomes for certain demographics. By ensuring the algorithms perform consistently across diverse populations, we can ensure fairness and effectiveness for all.
- Clinical validation: Clinical validation plays a crucial role in assessing the efficacy and safety of AI interventions [152]. Rigorous clinical trials and studies should be conducted to compare AI-based interventions with standard treatments or existing practices. These evaluations can encompass a range of study designs, including randomized controlled trials (RCTs), observational studies, or real-world evidence analyses. Through these studies, researchers can determine the effectiveness of AI technologies in improving patient outcomes and clinical decision-making. Furthermore, defining appropriate outcome measures is essential for assessing the impact of AI interventions on patient outcomes. Outcome measures such as mortality rates, disease progression, quality of life, and healthcare costs can be used to evaluate the effectiveness of AI technologies in improving healthcare delivery.
6.2. Interpretability and Usability
- Active stakeholder involvement: Throughout the development process, actively involving clinicians, patients, and other stakeholders provides valuable insights into their needs and expectations. This collaborative approach fosters a sense of ownership in the solution, leading to higher engagement.
- Iterative development and feedback loops: Developing AI solutions is an iterative process. By incorporating user feedback throughout development cycles, researchers can refine the AI tool to better address user needs. This ongoing feedback loop not only improves usability but also strengthens user confidence and engagement.
- User-friendly interfaces and clear visualizations: Designing clear and user-friendly interfaces is essential for user engagement. This includes presenting AI outputs in a way that is easy to understand and interpret, even for users with limited technical expertise. Additionally, providing clear visualizations of the AI’s reasoning can further enhance user trust and engagement.
6.3. Scalability and Continuous Improvement
- Post-market surveillance: Closely monitoring the performance of AI solutions after deployment in real-world settings to identify any unforeseen issues or areas for improvement [158].
- Performance monitoring: Continuously tracking the effectiveness of the AI tool in achieving its intended outcomes [159]. These data can be used to identify areas where the AI can be further optimized.
- Updating algorithms based on new data and insights: AI algorithms are not static. As new data become available, or as researchers gain a deeper understanding of the underlying problem, the algorithms can be updated to improve their performance and accuracy.
7. Ethical Considerations and Challenges
7.1. Ethical Implications of AI in Healthcare
- Privacy concerns: One of the foremost ethical concerns in AI healthcare is the privacy of patient data. AI systems require access to large datasets of patient information, which raises questions about the security and confidentiality of sensitive health data [160]. Ensuring that patient data used for AI applications are anonymized and securely stored is paramount. There is also a need for transparent policies regarding who has access to these data and for what purposes.
- Informed consent: The issue of informed consent in AI healthcare is complex, necessitating clear communication with patients about the use of their data, especially with AI algorithms that may be challenging for non-experts to grasp. This includes detailing data sharing implications, potential benefits and risks associated with AI-driven healthcare, and the level of human oversight in AI decisions. More details on the use of informed consent forms for AI in medicine with a comprehensive guideline for emergency physicians can be found in [161].
- Bias and fairness: AI systems are only as unbiased as the data they are trained on. There is a risk that AI algorithms may perpetuate existing biases present in healthcare data, leading to unfair treatment outcomes for certain groups [162]. For example, if an AI system is trained predominantly on data from a specific demographic, its accuracy might be lower for patients outside of that demographic. Ensuring that AI systems are developed and trained on diverse datasets is crucial to mitigate these biases. Moreover, the continuous monitoring and auditing of AI systems for biased outcomes are necessary to uphold fairness in healthcare delivery.
- Transparency and accountability: Transparency in AI decision-making processes is a key ethical concern [163]. It is important for healthcare providers and patients to understand how AI systems make their recommendations. This transparency is essential for building trust in AI systems and for accountability [164]. In cases where AI-driven decisions impact patient care, it is crucial to have mechanisms in place to review and understand these decisions, particularly in the event of adverse outcomes. A recent study highlights the need for transparent and accountable AI systems in natural NLP to address the “black box” issue of deep learning models [165]. It introduces the Explaining and Visualizing CNNs for Text Information (EVCT) framework, which offers human-interpretable solutions for text classification with minimal information loss, aligning with recent demands for fairness and transparency in AI-driven decision support systems.
7.2. Challenges in Integrating AI
- Data security concerns: As healthcare AI systems require access to large volumes of sensitive patient data, ensuring the security of these data is paramount [166]. The risk of data breaches and cyberattacks poses a significant concern. These security breaches can lead to the exposure of confidential patient information, resulting in privacy violations and potentially harming the trust between patients and healthcare providers. Implementing robust cybersecurity measures, including encryption, secure data storage solutions, and regular security audits, is crucial to protect patient data [167]. Additionally, educating healthcare staff about data security best practices is essential in safeguarding against breaches.
- Interoperability between systems: Another major challenge in integrating AI into healthcare is the issue of interoperability—the ability of different healthcare IT systems and software applications to communicate, exchange data, and use the information that has been exchanged [168]. Many healthcare systems use a variety of electronic health record (EHR) systems and other digital tools that may not be compatible with one another or with new AI technologies. This lack of interoperability can hinder the seamless exchange of patient data, reducing the effectiveness of AI tools. Developing standardized data formats and communication protocols, as well as encouraging the adoption of interoperable systems, is vital to overcome this challenge [169].
- Integration with existing clinical workflows: Integrating AI into existing clinical workflows can be challenging. Healthcare professionals may need to adjust their workflows to accommodate AI tools, which can be a time-consuming and complex process. Ensuring that AI systems are user-friendly and align with current clinical practices is essential to facilitate their adoption. Training and support for healthcare professionals in using these AI systems are also crucial for successful integration. For example, in a recent study, a three-tiered integration approach of AI-based image analysis into radiology workflows is outlined, focusing on enhancing automation and incorporating radiologist feedback for continuous AI improvement [170]. This approach entails initially visualizing AI outcomes without generating new patient records. It allows for the storage of AI-generated results in institutional systems and equips radiologists with tools to refine AI inferences for periodic retraining. This methodology was exemplified in a case study on brain metastases detection, where radiologist input substantially decreased false positives via iterative retraining with an expanded dataset.
- Data quality and quantity: The effectiveness of AI systems depends heavily on the quality and quantity of the data they are trained on. Inconsistent, incomplete, or inaccurate data can lead to poor AI performance. Ensuring the collection of high-quality, comprehensive patient data is therefore a significant challenge in AI integration [171]. Standardizing data collection methods and ensuring thorough data curation processes are essential steps in addressing this issue.
7.3. Regulatory and Compliance Issues
8. The Future of AI in Healthcare
8.1. Personalized Healthcare Applications
- Personalized medicine: One of the most promising trends in AI healthcare is the move towards more personalized medicine [177]. AI’s ability to analyze vast amounts of genetic, health data, and lifestyle information will enable the development of more precise and effective treatments tailored to individual patient profiles. This personalized approach can improve treatment outcomes and reduce side effects.
- AI-powered tools for health and sleep monitoring: Future research should explore the development and validation of AI-driven tools and algorithms for the diagnosis, monitoring, and management of health issues and sleep disorders [178]. This includes leveraging machine learning to analyze data from wearable devices such as sleep patterns, heart rate variability, and activity levels. These analyses can, for example, help detect abnormalities such as sleep apnea and personalize treatment recommendations based on individual sleep profiles.
- Longevity and aging: By harnessing the power of predictive analytics, AI can explore vast datasets to uncover biomarkers of aging and offer personalized strategies to slow or even reverse the aging process [179]. This includes leveraging AI for genomic interventions, where it could guide the editing of genes associated with aging mechanisms, enhancing cellular repair, resilience, and longevity. The potential of AI extends to the field of drug discovery and repurposing, where it can expedite the identification of compounds with anti-aging effects [180]. Moreover, AI’s integration into healthcare promises a paradigm shift towards preventive medicine, emphasizing early detection and intervention in age-related declines.
8.2. Enhanced Treatment Technologies
- AI in drug discovery and development: AI is poised to play a significant role in accelerating drug discovery and development [181]. By rapidly analyzing molecular and clinical data, AI has the potential to identify potential drug candidates much faster than traditional methods. This acceleration could significantly reduce the time and cost associated with bringing new drugs to market.
- Advanced robotics in surgery and rehabilitation: The use of AI-driven robotics in surgery and rehabilitation is expected to advance further [182]. Robotic systems, guided by AI algorithms, could potentially perform complex surgeries with high precision, reducing risks and improving patient outcomes. In rehabilitation, AI-powered exoskeletons and prosthetics are anticipated to offer greater mobility and independence to patients.
- AI hardware accelerators: As AI applications in healthcare grow, the demand for efficient processing capabilities rises. AI hardware accelerators like GPUs, TPUs, and FPGAs optimize AI model performance, enabling real-time medical data processing with minimal latency. Integrating these accelerators into medical devices promises faster diagnosis, treatment planning, and analysis, thereby enhancing patient care outcomes. Developing dedicated AI hardware accelerators tailored to healthcare needs is a promising future direction for improving the efficiency and accessibility of AI-driven healthcare solutions.
- AI-enhanced medical imaging: Future developments in AI are likely to produce even more advanced medical imaging techniques [183]. These advancements could provide clearer, more detailed images and enable the earlier detection of diseases, potentially even identifying health risks before symptoms appear.
- Integrating AI with IoT and wearables: The integration of AI with the Internet of Things (IoT) and wearable technology is an emerging trend [184]. This combination could lead to real-time health monitoring systems that not only track health data but also provide proactive recommendations and alerts. AI can also be integrated into existing wearable technologies to provide further information regarding health and performance [185].
8.3. Healthcare System Optimization
- Enhancing patient outcomes and system efficiency: The transformative potential of AI in healthcare can revolutionize patient care and system efficiency. Future AI applications aim to detect diseases earlier, customize treatments, and significantly personalize patient care, leading to improved recovery times and reduced mortality rates. AI’s role extends to optimizing healthcare resources, reducing costs, and improving care accessibility, especially for underserved communities [186]. Moreover, AI will support healthcare professionals by augmenting decision-making, promising equitable health improvements and a more efficient healthcare delivery system.
- Global health monitoring systems: The significance of AI in addressing pandemics and global health emergencies is increasingly recognized as crucial [187]. By integrating and analyzing diverse data streams, AI is adept at quickly detecting the emergence of disease outbreaks, projecting their spread, and guiding effective public health interventions. During the COVID-19 pandemic, AI-powered models were used to predict the disease’s trajectory, showcasing the potential of AI in navigating the complexities of pandemic management [188]. Moreover, AI’s capabilities extend to enhancing public health strategies, enabling the expedited development and dissemination of vaccines and therapeutic solutions in times of crisis.
8.4. Data Management
- Addressing data scarcity: The scarcity of labeled data in healthcare poses a significant challenge for AI development, especially in areas like rare disease research where data are inherently limited. A practical solution to this problem is the implementation of semi-supervised and weakly supervised learning techniques [189]. By utilizing a combination of a small set of labeled data and a larger volume of unlabeled data, these methods improve AI’s learning efficiency from minimal information, offering a viable strategy for advancing research and treatment in fields where comprehensive labeled datasets are scarce. However, for certain applications in healthcare, even obtaining a small amount of labeled data can be difficult. In such cases, emerging techniques in the field of machine learning offer intriguing possibilities.Few-shot learning: Few-shot learning requires only a small number of labeled examples for a new concept. This could be beneficial for situations where obtaining even a small amount of labeled data for a rare disease is possible. By learning from these few examples, the model could potentially generalize to similar cases [190,191].Zero-shot learning (ZSL): In theory, ZSL could allow AI models to learn about new diseases or medical conditions even with no labeled data for those specific cases. ZSL leverages existing knowledge and relationships between concepts to make predictions for unseen categories. While ZSL is still under development, it holds promise for healthcare applications where data are extremely limited [192].Meta-learning: This approach focuses on training models to “learn how to learn” efficiently. A meta-learning model could be trained on various healthcare-related tasks with limited datasets for each task. This acquired knowledge about learning itself could then be applied to new, unseen medical problems with minimal data, potentially improving performance [193].
- Ensuring model versatility: Achieving versatility in AI models is essential for their effective application across the diverse landscape of healthcare settings and patient demographics. Techniques such as domain adaptation and transfer learning stand out as effective solutions, enabling AI models trained on one dataset to adjust and perform accurately on another with little need for retraining [194]. This capability is particularly valuable in healthcare, where patient characteristics, disease profiles, and treatment responses can vary widely [195]. By fostering such adaptability, these techniques ensure that AI can be deployed more universally, enhancing its effectiveness and utility for a broad spectrum of patients.
8.5. Ethical Considerations and Trust Building
- Ensuring data privacy: Addressing data privacy concerns in healthcare has become increasingly crucial with the rise in AI applications. An exemplary solution to this challenge is federated learning, a novel AI model training approach that enables algorithms to learn from data stored on local servers across different healthcare institutions without the need for direct data sharing [196]. This method significantly enhances privacy and security and offers a strategic advantage in the healthcare industry where the sensitivity and confidentiality of patient data are of utmost importance.
- Stakeholder acceptance: Ensuring trust and acceptance among stakeholders is critical for the successful integration of AI into healthcare practices [197]. This encompasses not only patients and clinicians but also policymakers, regulatory bodies, healthcare administrators, and other relevant parties. Patients may express concerns regarding the reliability and accountability of AI-driven decision-making processes. Therefore, transparent communication about the role of AI in treatment plans and the potential benefits it offers is essential to foster patient acceptance. Similarly, clinicians may have reservations about entrusting AI algorithms with decision-making responsibilities, fearing loss of autonomy or professional judgment, as well as doubting the accuracy of AI decisions. Establishing comprehensive training programs and collaborative frameworks that empower clinicians to understand and validate AI tools effectively can mitigate these concerns. Furthermore, building trust extends to engaging stakeholders such as policymakers, regulatory bodies, and healthcare administrators. Transparency in AI development and deployment, coupled with clear communication about ethical, legal, and regulatory considerations, is crucial for gaining stakeholder trust. Establishing robust governance frameworks that address these concerns can enhance confidence in AI systems and ensure accountability.
- Building trust with Explainable AI: Explainable AI (XAI) aims to make AI decision-making processes transparent and understandable to humans, a crucial aspect for clinical applications [198]. By providing insights into how AI models arrive at their conclusions, XAI fosters trust among healthcare professionals and patients, ensuring that AI-supported decisions are well informed and ethically sound. This transparency is vital for integrating AI into sensitive healthcare decisions, where understanding the rationale behind AI recommendations can significantly impact patient care and outcomes.
9. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Rajpurkar, P.; Chen, E.; Banerjee, O.; Topol, E.J. AI in health and medicine. Nat. Med. 2022, 28, 31–38. [Google Scholar] [CrossRef] [PubMed]
- McCorduck, P.; Cfe, C. Machines Who Think: A Personal Inquiry into the History and Prospects of Artificial Intelligence; CRC Press: Boca Raton, FL, USA, 2004. [Google Scholar]
- Alpaydin, E. Introduction to Machine Learning; MIT Press: Cambridge, MA, USA, 2020. [Google Scholar]
- Brynjolfsson, E.; McAfee, A. The Second Machine Age: Work, Progress, and Prosperity in a Time of Brilliant Technologies; WW Norton & Company: New York, NY, USA, 2014. [Google Scholar]
- Russell, S.J.; Norvig, P. Artificial Intelligence a Modern Approach; Pearson: London, UK, 2010. [Google Scholar]
- LeCun, Y.; Bengio, Y.; Hinton, G. Deep learning. Nature 2015, 521, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Preininger, A. AI in health: State of the art, challenges, and future directions. Yearb. Med. Inform. 2019, 28, 16–26. [Google Scholar] [CrossRef] [PubMed]
- DuBois, K.N. Deep medicine: How artificial intelligence can make healthcare human again. Perspect. Sci. Christ. Faith 2019, 71, 199–201. [Google Scholar]
- Davenport, T.H. The AI Advantage: How to Put the Artificial Intelligence Revolution to Work; MIT Press: Cambridge, MA, USA, 2018. [Google Scholar]
- Kaur, S.; Singla, J.; Nkenyereye, L.; Jha, S.; Prashar, D.; Joshi, G.P.; El-Sappagh, S.; Islam, M.S.; Islam, S.R. Medical diagnostic systems using artificial intelligence (ai) algorithms: Principles and perspectives. IEEE Access 2020, 8, 228049–228069. [Google Scholar] [CrossRef]
- Cortez, N. Digital Health: Scaling Healthcare to the World; Springer: Cham, Switzerland, 2018; pp. 249–269. [Google Scholar]
- Hosny, A.; Parmar, C.; Quackenbush, J.; Schwartz, L.H.; Aerts, H.J. Artificial intelligence in radiology. Nat. Rev. Cancer 2018, 18, 500–510. [Google Scholar] [CrossRef] [PubMed]
- Kagiyama, N.; Shrestha, S.; Farjo, P.D.; Sengupta, P.P. Artificial intelligence: Practical primer for clinical research in cardiovascular disease. J. Am. Heart Assoc. 2019, 8, e012788. [Google Scholar] [CrossRef] [PubMed]
- Bardhan, I.; Chen, H.; Karahanna, E. Connecting systems, data, and people: A multidisciplinary research roadmap for chronic disease management. MIS Q. 2020, 44, 185–200. [Google Scholar]
- Huang, S.; Yang, J.; Fong, S.; Zhao, Q. Artificial intelligence in cancer diagnosis and prognosis: Opportunities and challenges. Cancer Lett. 2020, 471, 61–71. [Google Scholar] [CrossRef]
- Binhowemel, S.; Alfakhri, M.; AlReshaid, K.; Alyani, A. Role of Artificial Intelligence in Diabetes Research Diagnosis and Prognosis: A Narrative Review. J. Health Inform. Dev. Ctries. 2023, 17, 1–12. [Google Scholar]
- Guan, Z.; Li, H.; Liu, R.; Cai, C.; Liu, Y.; Li, J.; Wang, X.; Huang, S.; Wu, L.; Liu, D. Artificial intelligence in diabetes management: Advancements, opportunities, and challenges. Cell Rep. Med. 2023, 4, 101213. [Google Scholar] [CrossRef] [PubMed]
- Waring, J.; Lindvall, C.; Umeton, R. Automated machine learning: Review of the state-of-the-art and opportunities for healthcare. Artif. Intell. Med. 2020, 104, 101822. [Google Scholar] [CrossRef] [PubMed]
- Eloranta, S.; Boman, M. Predictive models for clinical decision making: Deep dives in practical machine learning. J. Intern. Med. 2022, 292, 278–295. [Google Scholar] [CrossRef] [PubMed]
- Nezamabadi, K.; Sardaripour, N.; Haghi, B.; Forouzanfar, M. Unsupervised ECG analysis: A review. IEEE Rev. Biomed. Eng. 2022, 16, 208–224. [Google Scholar] [CrossRef] [PubMed]
- Coronato, A.; Naeem, M.; De Pietro, G.; Paragliola, G. Reinforcement learning for intelligent healthcare applications: A survey. Artif. Intell. Med. 2020, 109, 101964. [Google Scholar] [CrossRef] [PubMed]
- Sarvamangala, D.; Kulkarni, R.V. Convolutional neural networks in medical image understanding: A survey. Evol. Intell. 2022, 15, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Zhang, L.; Du, M.; Bo, J.; Liu, H.; Ren, L.; Li, X.; Deen, M.J. A comparative analysis of eleven neural networks architectures for small datasets of lung images of COVID-19 patients toward improved clinical decisions. Comput. Biol. Med. 2021, 139, 104887. [Google Scholar] [CrossRef] [PubMed]
- Rim, B.; Sung, N.-J.; Min, S.; Hong, M. Deep learning in physiological signal data: A survey. Sensors 2020, 20, 969. [Google Scholar] [CrossRef] [PubMed]
- Bahrami, M.; Forouzanfar, M. Sleep apnea detection from single-lead ECG: A comprehensive analysis of machine learning and deep learning algorithms. IEEE Trans. Instrum. Meas. 2022, 71, 4003011. [Google Scholar] [CrossRef]
- Yi, X.; Walia, E.; Babyn, P. Generative adversarial network in medical imaging: A review. Med. Image Anal. 2019, 58, 101552. [Google Scholar] [CrossRef]
- Hu, Y.; Kothapalli, S.V.; Gan, W.; Sukstanskii, A.L.; Wu, G.F.; Goyal, M.; Yablonskiy, D.A.; Kamilov, U.S. DiffGEPCI: 3D MRI Synthesis from mGRE Signals using 2.5 D Diffusion Model. arXiv 2023, arXiv:2311.18073. [Google Scholar]
- Wang, J.; Liu, X. Medical image recognition and segmentation of pathological slices of gastric cancer based on Deeplab v3+ neural network. Comput. Methods Programs Biomed. 2021, 207, 106210. [Google Scholar] [CrossRef] [PubMed]
- Nagabushanam, P.; Thomas George, S.; Radha, S. EEG signal classification using LSTM and improved neural network algorithms. Soft Comput. 2020, 24, 9981–10003. [Google Scholar] [CrossRef]
- Kawazoe, Y.; Shibata, D.; Shinohara, E.; Aramaki, E.; Ohe, K. A clinical specific BERT developed using a huge Japanese clinical text corpus. PLoS ONE 2021, 16, e0259763. [Google Scholar] [CrossRef] [PubMed]
- Torfi, A.; Fox, E.A.; Reddy, C.K. Differentially private synthetic medical data generation using convolutional GANs. Inf. Sci. 2022, 586, 485–500. [Google Scholar] [CrossRef]
- Lin, X.; Quan, Z.; Wang, Z.-J.; Ma, T.; Zeng, X. KGNN: Knowledge Graph Neural Network for Drug-Drug Interaction Prediction; IJCAI: Pasadena, CA, USA, 2020; pp. 2739–2745. [Google Scholar]
- Zhou, B.; Yang, G.; Shi, Z.; Ma, S. Natural language processing for smart healthcare. IEEE Rev. Biomed. Eng. 2022, 17, 4–18. [Google Scholar] [CrossRef]
- Yang, X.; Chen, A.; PourNejatian, N.; Shin, H.C.; Smith, K.E.; Parisien, C.; Compas, C.; Martin, C.; Costa, A.B.; Flores, M.G. A large language model for electronic health records. NPJ Digit. Med. 2022, 5, 194. [Google Scholar] [CrossRef] [PubMed]
- McKinney, S.M.; Sieniek, M.; Godbole, V.; Godwin, J.; Antropova, N.; Ashrafian, H.; Back, T.; Chesus, M.; Corrado, G.S.; Darzi, A. International evaluation of an AI system for breast cancer screening. Nature 2020, 577, 89–94. [Google Scholar] [CrossRef]
- Jian, Y.; Pasquier, M.; Sagahyroon, A.; Aloul, F. A machine learning approach to predicting diabetes complications. Healthcare 2021, 9, 1712. [Google Scholar] [CrossRef]
- Fan, Y.; Long, E.; Cai, L.; Cao, Q.; Wu, X.; Tong, R. Machine learning approaches to predict risks of diabetic complications and poor glycemic control in nonadherent type 2 diabetes. Front. Pharmacol. 2021, 12, 665951. [Google Scholar] [CrossRef]
- Yuan, X.; Chen, J.; Zhang, K.; Wu, Y.; Yang, T. A stable AI-based binary and multiple class heart disease prediction model for IoMT. IEEE Trans. Ind. Inform. 2021, 18, 2032–2040. [Google Scholar] [CrossRef]
- Ali, F.; El-Sappagh, S.; Islam, S.R.; Kwak, D.; Ali, A.; Imran, M.; Kwak, K.-S. A smart healthcare monitoring system for heart disease prediction based on ensemble deep learning and feature fusion. Inf. Fusion 2020, 63, 208–222. [Google Scholar] [CrossRef]
- Vieira, S.; Pinaya, W.H.; Mechelli, A. Using deep learning to investigate the neuroimaging correlates of psychiatric and neurological disorders: Methods and applications. Neurosci. Biobehav. Rev. 2017, 74, 58–75. [Google Scholar] [CrossRef] [PubMed]
- Gautam, R.; Sharma, M. Prevalence and diagnosis of neurological disorders using different deep learning techniques: A meta-analysis. J. Med. Syst. 2020, 44, 49. [Google Scholar] [CrossRef] [PubMed]
- Murugan, S.; Venkatesan, C.; Sumithra, M.; Gao, X.-Z.; Elakkiya, B.; Akila, M.; Manoharan, S. DEMNET: A deep learning model for early diagnosis of Alzheimer diseases and dementia from MR images. IEEE Access 2021, 9, 90319–90329. [Google Scholar] [CrossRef]
- Bartsch, G., Jr.; Mitra, A.P.; Mitra, S.A.; Almal, A.A.; Steven, K.E.; Skinner, D.G.; Fry, D.W.; Lenehan, P.F.; Worzel, W.P.; Cote, R.J. Use of artificial intelligence and machine learning algorithms with gene expression profiling to predict recurrent nonmuscle invasive urothelial carcinoma of the bladder. J. Urol. 2016, 195, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Paul, D.; Sanap, G.; Shenoy, S.; Kalyane, D.; Kalia, K.; Tekade, R.K. Artificial intelligence in drug discovery and development. Drug Discov. Today 2021, 26, 80. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Srivastava, D.; Sahu, M.; Tiwari, S.; Ambasta, R.K.; Kumar, P. Artificial intelligence to deep learning: Machine intelligence approach for drug discovery. Mol. Divers. 2021, 25, 1315–1360. [Google Scholar] [CrossRef] [PubMed]
- Hasselgren, C.; Oprea, T.I. Artificial Intelligence for Drug Discovery: Are We There Yet? Annu. Rev. Pharmacol. Toxicol. 2024, 64, 527–550. [Google Scholar] [CrossRef]
- Senior, A.W.; Evans, R.; Jumper, J.; Kirkpatrick, J.; Sifre, L.; Green, T.; Qin, C.; Žídek, A.; Nelson, A.W.; Bridgland, A. Improved protein structure prediction using potentials from deep learning. Nature 2020, 577, 706–710. [Google Scholar] [CrossRef]
- Sadybekov, A.V.; Katritch, V. Computational approaches streamlining drug discovery. Nature 2023, 616, 673–685. [Google Scholar] [CrossRef] [PubMed]
- Bica, I.; Alaa, A.M.; Lambert, C.; Van Der Schaar, M. From real-world patient data to individualized treatment effects using machine learning: Current and future methods to address underlying challenges. Clin. Pharmacol. Ther. 2021, 109, 87–100. [Google Scholar] [CrossRef]
- Vettoretti, M.; Cappon, G.; Facchinetti, A.; Sparacino, G. Advanced diabetes management using artificial intelligence and continuous glucose monitoring sensors. Sensors 2020, 20, 3870. [Google Scholar] [CrossRef] [PubMed]
- Low, D.M.; Bentley, K.H.; Ghosh, S.S. Automated assessment of psychiatric disorders using speech: A systematic review. Laryngoscope Investig. Otolaryngol. 2020, 5, 96–116. [Google Scholar] [CrossRef] [PubMed]
- Graham, S.; Depp, C.; Lee, E.E.; Nebeker, C.; Tu, X.; Kim, H.-C.; Jeste, D.V. Artificial intelligence for mental health and mental illnesses: An overview. Curr. Psychiatry Rep. 2019, 21, 116. [Google Scholar] [CrossRef] [PubMed]
- Nasrullah, S.; Jalali, A. Detection of Types of Mental Illness through the Social Network Using Ensembled Deep Learning Model. Comput. Intell. Neurosci. 2022, 2022, 9404242. [Google Scholar] [CrossRef] [PubMed]
- Guntuku, S.C.; Yaden, D.B.; Kern, M.L.; Ungar, L.H.; Eichstaedt, J.C. Detecting depression and mental illness on social media: An integrative review. Curr. Opin. Behav. Sci. 2017, 18, 43–49. [Google Scholar] [CrossRef]
- Czerwinski, M.; Hernandez, J.; McDuff, D. Building an AI That Feels: AI systems with emotional intelligence could learn faster and be more helpful. IEEE Spectr. 2021, 58, 32–38. [Google Scholar] [CrossRef]
- Torab-Miandoab, A.; Samad-Soltani, T.; Jodati, A.; Rezaei-Hachesu, P. Interoperability of heterogeneous health information systems: A systematic literature review. BMC Med. Inform. Decis. Mak. 2023, 23, 18. [Google Scholar] [CrossRef]
- Díaz-Rodríguez, N.; Del Ser, J.; Coeckelbergh, M.; de Prado, M.L.; Herrera-Viedma, E.; Herrera, F. Connecting the dots in trustworthy Artificial Intelligence: From AI principles, ethics, and key requirements to responsible AI systems and regulation. Inf. Fusion 2023, 99, 101896. [Google Scholar] [CrossRef]
- Gurevich, E.; El Hassan, B.; El Morr, C. In Equity within AI systems: What can health leaders expect? Healthc. Manag. Forum 2023, 36, 119–124. [Google Scholar] [CrossRef]
- Dwivedi, Y.K.; Hughes, L.; Ismagilova, E.; Aarts, G.; Coombs, C.; Crick, T.; Duan, Y.; Dwivedi, R.; Edwards, J.; Eirug, A. Artificial Intelligence (AI): Multidisciplinary perspectives on emerging challenges, opportunities, and agenda for research, practice and policy. Int. J. Inf. Manag. 2021, 57, 101994. [Google Scholar] [CrossRef]
- Jebbor, S.; Raddouane, C.; El Afia, A. A preliminary study for selecting the appropriate AI-based forecasting model for hospital assets demand under disasters. J. Humanit. Logist. Supply Chain Manag. 2022, 12, 1–29. [Google Scholar] [CrossRef]
- Galli, L.; Levato, T.; Schoen, F.; Tigli, L. Prescriptive analytics for inventory management in health care. J. Oper. Res. Soc. 2021, 72, 2211–2224. [Google Scholar] [CrossRef]
- Tien, P.W. Deep Learning-Powered Vision-Based Energy Management System for Next-Gen Built Environment; University of Nottingham: Nottingham, UK, 2023. [Google Scholar]
- Zamzam, A.H.; Hasikin, K.; Wahab, A.K.A. Integrated failure analysis using machine learning predictive system for smart management of medical equipment maintenance. Eng. Appl. Artif. Intell. 2023, 125, 106715. [Google Scholar] [CrossRef]
- Mizan, T.; Taghipour, S. Medical resource allocation planning by integrating machine learning and optimization models. Artif. Intell. Med. 2022, 134, 102430. [Google Scholar] [CrossRef]
- Munavalli, J.R.; Boersma, H.J.; Rao, S.V.; Van Merode, G. Real-time capacity management and patient flow optimization in hospitals using AI methods. Artif. Intell. Data Min. Healthc. 2021, 2021, 55–69. [Google Scholar]
- Adhikari, A.; Joshi, R.; Basu, S. Collaboration and coordination strategies for a multi-level AI-enabled healthcare supply chain under disaster. Int. J. Prod. Res. 2023, 2023, 1–27. [Google Scholar] [CrossRef]
- Samadhiya, A.; Yadav, S.; Kumar, A.; Majumdar, A.; Luthra, S.; Garza-Reyes, J.A.; Upadhyay, A. The influence of artificial intelligence techniques on disruption management: Does supply chain dynamism matter? Technol. Soc. 2023, 75, 102394. [Google Scholar] [CrossRef]
- Sun, W.; Bocchini, P.; Davison, B.D. Applications of artificial intelligence for disaster management. Nat. Hazards 2020, 103, 2631–2689. [Google Scholar] [CrossRef]
- Tang, A.; Tam, R.; Cadrin-Chênevert, A.; Guest, W.; Chong, J.; Barfett, J.; Trump, D.; Noorbakhsh-Sabet, N.; Zand, R.; Zhang, Y. Health information management: Implications of artificial intelligence on healthcare data and information management. Yearb. Med. Inform. 2019, 28, 56–64. [Google Scholar]
- Hoogendoorn, M.; Szolovits, P.; Moons, L.M.; Numans, M.E. Utilizing uncoded consultation notes from electronic medical records for predictive modeling of colorectal cancer. Artif. Intell. Med. 2016, 69, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Thesmar, D.; Sraer, D.; Pinheiro, L.; Dadson, N.; Veliche, R.; Greenberg, P. Combining the power of artificial intelligence with the richness of healthcare claims data: Opportunities and challenges. Pharmacoeconomics 2019, 37, 745–752. [Google Scholar] [CrossRef]
- Baudry, M.; Robert, C.Y. A machine learning approach for individual claims reserving in insurance. Appl. Stoch. Models Bus. Ind. 2019, 35, 1127–1155. [Google Scholar] [CrossRef]
- Samorani, M.; Blount, L.G. Machine learning and medical appointment scheduling: Creating and perpetuating inequalities in access to health care. Am. Public Health Assoc. 2020, 110, 440–441. [Google Scholar] [CrossRef]
- Chong, L.R.; Tsai, K.T.; Lee, L.L.; Foo, S.G.; Chang, P.C. Artificial intelligence predictive analytics in the management of outpatient MRI appointment no-shows. Am. J. Roentgenol. 2020, 215, 1155–1162. [Google Scholar] [CrossRef] [PubMed]
- Mandelbaum, A.; Momčilović, P.; Trichakis, N.; Kadish, S.; Leib, R.; Bunnell, C.A. Data-driven appointment-scheduling under uncertainty: The case of an infusion unit in a cancer center. Manag. Sci. 2020, 66, 243–270. [Google Scholar] [CrossRef]
- Pandey, M.; Arora, M.; Arora, S.; Goyal, C.; Gera, V.K.; Yadav, H. AI-based Integrated Approach for the Development of Intelligent Document Management System (IDMS). Procedia Comput. Sci. 2023, 230, 725–736. [Google Scholar] [CrossRef]
- Hsu, E.; Malagaris, I.; Kuo, Y.-F.; Sultana, R.; Roberts, K. Deep learning-based NLP data pipeline for EHR-scanned document information extraction. JAMIA Open 2022, 5, ooac045. [Google Scholar] [CrossRef]
- Kreps, G.L.; Neuhauser, L. Artificial intelligence and immediacy: Designing health communication to personally engage consumers and providers. Patient Educ. Couns. 2013, 92, 205–210. [Google Scholar] [CrossRef]
- Kingston, J. Using artificial intelligence to support compliance with the general data protection regulation. Artif. Intell. Law 2017, 25, 429–443. [Google Scholar] [CrossRef]
- Hamdani, R.E.; Mustapha, M.; Amariles, D.R.; Troussel, A.; Meeùs, S.; Krasnashchok, K. A combined rule-based and machine learning approach for automated GDPR compliance checking. In Proceedings of the Eighteenth International Conference on Artificial Intelligence and Law, São Paulo, Brazil, 21–25 June 2021; pp. 40–49. [Google Scholar]
- El-Bouri, R.; Taylor, T.; Youssef, A.; Zhu, T.; Clifton, D.A. Machine learning in patient flow: A review. Prog. Biomed. Eng. 2021, 3, 022002. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Asanjan, A.A.; Welles, E.; Gao, X.; Sorooshian, S.; Liu, X. Developing reservoir monthly inflow forecasts using artificial intelligence and climate phenomenon information. Water Resour. Res. 2017, 53, 2786–2812. [Google Scholar] [CrossRef]
- Knight, D.; Aakre, C.A.; Anstine, C.V.; Munipalli, B.; Biazar, P.; Mitri, G.; Valery, J.R.; Brigham, T.; Niazi, S.K.; Perlman, A.I. Artificial Intelligence for Patient Scheduling in the Real-World Health Care Setting: A Metanarrative Review. Health Policy Technol. 2023, 12, 100824. [Google Scholar] [CrossRef]
- Wang, J.; Fung, R.Y. Adaptive dynamic programming algorithms for sequential appointment scheduling with patient preferences. Artif. Intell. Med. 2015, 63, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Tian, D.; Li, W.; Dong, B.; Wang, H.; Yuan, J.; Li, B.; Shi, L.; Lin, X.; Zhao, L. Artificial intelligence-assisted reduction in patients’ waiting time for outpatient process: A retrospective cohort study. BMC Health Serv. Res. 2021, 21, 237. [Google Scholar] [CrossRef]
- Joshi, I. Waiting for deep medicine. Lancet 2019, 393, 1193–1194. [Google Scholar] [CrossRef]
- Joseph, J.; Senith, S.; Kirubaraj, A.A.; Ramson, J.S. Machine Learning for Prediction of Wait Times in Outpatient Clinic. Procedia Comput. Sci. 2022, 215, 230–239. [Google Scholar] [CrossRef]
- Khanbhai, M.; Anyadi, P.; Symons, J.; Flott, K.; Darzi, A.; Mayer, E. Applying natural language processing and machine learning techniques to patient experience feedback: A systematic review. BMJ Health Care Inform. 2021, 28, e100262. [Google Scholar] [CrossRef]
- Bari, V.; Hirsch, J.S.; Narvaez, J.; Sardinia, R.; Bock, K.R.; Oppenheim, M.I.; Meytlis, M. An approach to predicting patient experience through machine learning and social network analysis. J. Am. Med. Inform. Assoc. 2020, 27, 1834–1843. [Google Scholar] [CrossRef]
- Darley, S.; Coulson, T.; Peek, N.; Moschogianis, S.; Van Der Veer, S.N.; Wong, D.C.; Brown, B.C. Understanding how the design and implementation of online consultations affect primary care quality: Systematic review of evidence with recommendations for designers, providers, and researchers. J. Med. Internet Res. 2022, 24, e37436. [Google Scholar] [CrossRef] [PubMed]
- Frid-Adar, M.; Amer, R.; Gozes, O.; Nassar, J.; Greenspan, H. COVID-19 in CXR: From detection and severity scoring to patient disease monitoring. IEEE J. Biomed. Health Inform. 2021, 25, 1892–1903. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Schönlieb, C.-B.; Lio, P.; Leiner, T.; Dragotti, P.L.; Wang, G.; Rueckert, D.; Firmin, D.; Yang, G. AI-based reconstruction for fast MRI—A systematic review and meta-analysis. Proc. IEEE 2022, 110, 224–245. [Google Scholar] [CrossRef]
- Fusco, R.; Grassi, R.; Granata, V.; Setola, S.V.; Grassi, F.; Cozzi, D.; Pecori, B.; Izzo, F.; Petrillo, A. Artificial intelligence and COVID-19 using chest CT scan and chest X-ray images: Machine learning and deep learning approaches for diagnosis and treatment. J. Pers. Med. 2021, 11, 993. [Google Scholar] [CrossRef] [PubMed]
- Panayides, A.S.; Amini, A.; Filipovic, N.D.; Sharma, A.; Tsaftaris, S.A.; Young, A.; Foran, D.; Do, N.; Golemati, S.; Kurc, T. AI in medical imaging informatics: Current challenges and future directions. IEEE J. Biomed. Health Inform. 2020, 24, 1837–1857. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhang, F.; Chen, C.; Wang, S.; Wang, Y.; Yu, Y. Act like a radiologist: Towards reliable multi-view correspondence reasoning for mammogram mass detection. IEEE Trans. Pattern Anal. Mach. Intell. 2021, 44, 5947–5961. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Zhang, Q.; Huang, C.; Shi, C.; Wang, L.; Shi, N.; Fang, C.; Shan, F.; Mei, X.; Shi, J. CT quantification of pneumonia lesions in early days predicts progression to severe illness in a cohort of COVID-19 patients. Theranostics 2020, 10, 5613. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.; Goodman, R.; Patrinely, J.; Stone, C.; Zimmerman, E.; Donald, R.; Chang, S.; Berkowitz, S.; Finn, A.; Jahangir, E. Assessing the accuracy and reliability of AI-generated medical responses: An evaluation of the Chat-GPT model. Res. Sq. 2023, Preprint. [Google Scholar]
- Bera, K.; Braman, N.; Gupta, A.; Velcheti, V.; Madabhushi, A. Predicting cancer outcomes with radiomics and artificial intelligence in radiology. Nat. Rev. Clin. Oncol. 2022, 19, 132–146. [Google Scholar] [CrossRef]
- Lee, R.Y.; Wu, Y.; Goh, D.; Tan, V.; Ng, C.W.; Lim, J.C.T.; Lau, M.C.; Yeong, J.P.S. Application of Artificial Intelligence to in vitro Tumor Modeling and Characterization of the Tumor Microenvironment. Adv. Healthc. Mater. 2023, 12, 2202457. [Google Scholar] [CrossRef]
- Acs, B.; Rantalainen, M.; Hartman, J. Artificial intelligence as the next step towards precision pathology. J. Intern. Med. 2020, 288, 62–81. [Google Scholar] [CrossRef] [PubMed]
- Bera, K.; Schalper, K.A.; Rimm, D.L.; Velcheti, V.; Madabhushi, A. Artificial intelligence in digital pathology—New tools for diagnosis and precision oncology. Nat. Rev. Clin. Oncol. 2019, 16, 703–715. [Google Scholar] [CrossRef] [PubMed]
- Pandey, I.; Misra, V.; Pandey, A.T.; Ramteke, P.W.; Agrawal, R. Artificial intelligence technologies empowering identification of novel diagnostic molecular markers in gastric cancer. Ind. J. Pathol. Microbiol. 2021, 64 (Suppl. S1), S63–S68. [Google Scholar]
- Segura, F.; Segura, P.; Segura, F. Measuring Tumor Aggressiveness Through Artificial Intelligence. J. Asoc. Argent. Ortop. Traumatol. 2023, 88, 653–661. [Google Scholar] [CrossRef]
- Liopyris, K.; Gregoriou, S.; Dias, J.; Stratigos, A.J. Artificial intelligence in dermatology: Challenges and perspectives. Dermatol. Ther. 2022, 12, 2637–2651. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Wasim, S. Prevent medical errors through artificial intelligence: A review. Saudi J. Med. Pharm. Sci. 2023, 9, 419–423. [Google Scholar] [CrossRef]
- Soun, J.; Chow, D.; Nagamine, M.; Takhtawala, R.; Filippi, C.; Yu, W.; Chang, P. Artificial intelligence and acute stroke imaging. Am. J. Neuroradiol. 2021, 42, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Brereton, T.A.; Malik, M.M.; Lifson, M.; Greenwood, J.D.; Peterson, K.J.; Overgaard, S.M. The Role of Artificial Intelligence Model Documentation in Translational Science: Scoping Review. Interact. J. Med. Res. 2023, 12, e45903. [Google Scholar] [CrossRef] [PubMed]
- Klement, W.; El Emam, K. Consolidated reporting guidelines for prognostic and diagnostic machine learning modeling studies: Development and validation. J. Med. Internet Res. 2023, 25, e48763. [Google Scholar] [CrossRef]
- Huang, S.-C.; Pareek, A.; Seyyedi, S.; Banerjee, I.; Lungren, M.P. Fusion of medical imaging and electronic health records using deep learning: A systematic review and implementation guidelines. NPJ Digit. Med. 2020, 3, 136. [Google Scholar] [CrossRef]
- Mohsen, F.; Ali, H.; El Hajj, N.; Shah, Z. Artificial intelligence-based methods for fusion of electronic health records and imaging data. Sci. Rep. 2022, 12, 17981. [Google Scholar] [CrossRef] [PubMed]
- Deng, L.; Li, G.; Han, S.; Shi, L.; Xie, Y. Model compression and hardware acceleration for neural networks: A comprehensive survey. Proc. IEEE 2020, 108, 485–532. [Google Scholar] [CrossRef]
- Alcaín, E.; Fernandez, P.R.; Nieto, R.; Montemayor, A.S.; Vilas, J.; Galiana-Bordera, A.; Martinez-Girones, P.M.; Prieto-de-la-Lastra, C.; Rodriguez-Vila, B.; Bonet, M. Hardware architectures for real-time medical imaging. Electronics 2021, 10, 3118. [Google Scholar] [CrossRef]
- Eklund, A.; Dufort, P.; Forsberg, D.; LaConte, S.M. Medical image processing on the GPU–Past, present and future. Med. Image Anal. 2013, 17, 1073–1094. [Google Scholar] [CrossRef] [PubMed]
- Corral, J.M.R.; Civit-Masot, J.; Luna-Perejón, F.; Díaz-Cano, I.; Morgado-Estévez, A.; Domínguez-Morales, M. Energy efficiency in edge TPU vs. embedded GPU for computer-aided medical imaging segmentation and classification. Eng. Appl. Artif. Intell. 2024, 127, 107298. [Google Scholar] [CrossRef]
- Lin, Y.; Zhang, Y.; Yang, X. A Low Memory Requirement MobileNets Accelerator Based on FPGA for Auxiliary Medical Tasks. Bioengineering 2022, 10, 28. [Google Scholar] [CrossRef] [PubMed]
- Azghadi, M.R.; Lammie, C.; Eshraghian, J.K.; Payvand, M.; Donati, E.; Linares-Barranco, B.; Indiveri, G. Hardware implementation of deep network accelerators towards healthcare and biomedical applications. IEEE Trans. Biomed. Circuits Syst. 2020, 14, 1138–1159. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.; Ye, X.; Chen, R.; Su, F.; Lin, M.; Ma, Y.; Zhu, Y.; Huang, S. Wearable on-device deep learning system for hand gesture recognition based on FPGA accelerator. Math. Biosci. Eng. 2021, 18, 132–153. [Google Scholar] [CrossRef] [PubMed]
- Nayak, D.R.; Dash, R.; Majhi, B. Automated diagnosis of multi-class brain abnormalities using MRI images: A deep convolutional neural network based method. Pattern Recog. Lett. 2020, 138, 385–391. [Google Scholar] [CrossRef]
- Soffer, S.; Klang, E.; Shimon, O.; Barash, Y.; Cahan, N.; Greenspana, H.; Konen, E. Deep learning for pulmonary embolism detection on computed tomography pulmonary angiogram: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 15814. [Google Scholar] [CrossRef]
- Lång, K.; Josefsson, V.; Larsson, A.-M.; Larsson, S.; Högberg, C.; Sartor, H.; Hofvind, S.; Andersson, I.; Rosso, A. Artificial intelligence-supported screen reading versus standard double reading in the Mammography Screening with Artificial Intelligence trial (MASAI): A clinical safety analysis of a randomised, controlled, non-inferiority, single-blinded, screening accuracy study. Lancet Oncol. 2023, 24, 936–944. [Google Scholar] [PubMed]
- Sveric, K.M.; Ulbrich, S.; Dindane, Z.; Winkler, A.; Botan, R.; Mierke, J.; Trausch, A.; Heidrich, F.; Linke, A. Improved assessment of left ventricular ejection fraction using artificial intelligence in echocardiography: A comparative analysis with cardiac magnetic resonance imaging. Int. J. Cardiol. 2024, 394, 131383. [Google Scholar] [CrossRef] [PubMed]
- Khan, P.; Kader, M.F.; Islam, S.R.; Rahman, A.B.; Kamal, M.S.; Toha, M.U.; Kwak, K.-S. Machine learning and deep learning approaches for brain disease diagnosis: Principles and recent advances. IEEE Access 2021, 9, 37622–37655. [Google Scholar] [CrossRef]
- Adam, R.; Dell’Aquila, K.; Hodges, L.; Maldjian, T.; Duong, T.Q. Deep learning applications to breast cancer detection by magnetic resonance imaging: A literature review. Breast Cancer Res. 2023, 25, 87. [Google Scholar] [CrossRef] [PubMed]
- Sheth, D.; Giger, M.L. Artificial intelligence in the interpretation of breast cancer on MRI. J. Magn. Reson. Imaging 2020, 51, 1310–1324. [Google Scholar] [CrossRef]
- McCrindle, B.; Zukotynski, K.; Doyle, T.E.; Noseworthy, M.D. A radiology-focused review of predictive uncertainty for AI interpretability in computer-assisted segmentation. Radiol. Artif. Intell. 2021, 3, e210031. [Google Scholar] [CrossRef] [PubMed]
- Zheng, R.; Wang, Q.; Lv, S.; Li, C.; Wang, C.; Chen, W.; Wang, H. Automatic liver tumor segmentation on dynamic contrast enhanced mri using 4D information: Deep learning model based on 3D convolution and convolutional lstm. IEEE Trans. Med. Imaging 2022, 41, 2965–2976. [Google Scholar] [CrossRef]
- Schalekamp, S.; Klein, W.M.; van Leeuwen, K.G. Current and emerging artificial intelligence applications in chest imaging: A pediatric perspective. Pediatr. Radiol. 2022, 52, 2120–2130. [Google Scholar] [CrossRef]
- Lee, M.-H.; O’Hara, N.; Sonoda, M.; Kuroda, N.; Juhasz, C.; Asano, E.; Dong, M.; Jeong, J.-W. Novel deep learning network analysis of electrical stimulation mapping-driven diffusion MRI tractography to improve preoperative evaluation of pediatric epilepsy. IEEE Trans. Biomed. Eng. 2020, 67, 3151–3162. [Google Scholar] [CrossRef]
- Ardila, D.; Kiraly, A.P.; Bharadwaj, S.; Choi, B.; Reicher, J.J.; Peng, L.; Tse, D.; Etemadi, M.; Ye, W.; Corrado, G. End-to-end lung cancer screening with three-dimensional deep learning on low-dose chest computed tomography. Nat. Med. 2019, 25, 954–961. [Google Scholar] [CrossRef]
- Watanabe, A.T.; Lim, V.; Vu, H.X.; Chim, R.; Weise, E.; Liu, J.; Bradley, W.G.; Comstock, C.E. Improved cancer detection using artificial intelligence: A retrospective evaluation of missed cancers on mammography. J. Digit. Imaging 2019, 32, 625–637. [Google Scholar] [CrossRef] [PubMed]
- Sermesant, M.; Delingette, H.; Cochet, H.; Jais, P.; Ayache, N. Applications of artificial intelligence in cardiovascular imaging. Nat. Rev. Cardiol. 2021, 18, 600–609. [Google Scholar] [CrossRef]
- Nahavandi, D.; Alizadehsani, R.; Khosravi, A.; Acharya, U.R. Application of artificial intelligence in wearable devices: Opportunities and challenges. Comput. Methods Programs Biomed. 2022, 213, 106541. [Google Scholar] [CrossRef]
- Stangl, F.J.; Riedl, R. Measurement of heart rate and heart rate variability with wearable devices: A systematic review. Wirtschaftsinformatik 2022, 2022, 15. [Google Scholar]
- Huang, J.-D.; Wang, J.; Ramsey, E.; Leavey, G.; Chico, T.J.; Condell, J. Applying artificial intelligence to wearable sensor data to diagnose and predict cardiovascular disease: A review. Sensors 2022, 22, 8002. [Google Scholar] [CrossRef] [PubMed]
- Bahrami, M.; Forouzanfar, M. Deep learning forecasts the occurrence of sleep apnea from single-lead ECG. Cardiovasc. Eng. Technol. 2022, 13, 809–815. [Google Scholar] [CrossRef]
- Joeris, A.; Zhu, T.Y.; Lambert, S.; Wood, A.; Jayakumar, P. Real-world patient data: Can they support decision making and patient engagement? Injury 2023, 54, S51–S56. [Google Scholar] [CrossRef]
- Asthana, S.; Megahed, A.; Strong, R. A recommendation system for proactive health monitoring using IoT and wearable technologies. In Proceedings of the 2017 IEEE International Conference on AI & Mobile Services (AIMS), Honolulu, HI, USA, 25–30 June 2017; IEEE: New, York, NY, USA, 2017; pp. 14–21. [Google Scholar]
- Djanian, S.; Bruun, A.; Nielsen, T.D. Sleep classification using Consumer Sleep Technologies and AI: A review of the current landscape. Sleep Med. 2022, 100, 390–403. [Google Scholar] [CrossRef] [PubMed]
- Sabry, F.; Eltaras, T.; Labda, W.; Alzoubi, K.; Malluhi, Q. Machine learning for healthcare wearable devices: The big picture. J. Healthc. Eng. 2022, 2022, 1–25. [Google Scholar] [CrossRef]
- Van Bulck, L.; Couturier, R.; Moons, P. Applications of Artificial Intelligence for Nursing: Has a New Era Arrived? Oxford University Press US: Cary, NC, USA, 2023; Volume 22, pp. e19–e20. [Google Scholar]
- Jadczyk, T.; Wojakowski, W.; Tendera, M.; Henry, T.D.; Egnaczyk, G.; Shreenivas, S. Artificial intelligence can improve patient management at the time of a pandemic: The role of voice technology. J. Med. Internet Res. 2021, 23, e22959. [Google Scholar] [CrossRef]
- Adus, S.; Macklin, J.; Pinto, A. Exploring patient perspectives on how they can and should be engaged in the development of artificial intelligence (AI) applications in health care. BMC Health Serv. Res. 2023, 23, 1163. [Google Scholar] [CrossRef] [PubMed]
- Curtis, R.G.; Bartel, B.; Ferguson, T.; Blake, H.T.; Northcott, C.; Virgara, R.; Maher, C.A. Improving user experience of virtual health assistants: Scoping review. J. Med. Internet Res. 2021, 23, e31737. [Google Scholar] [CrossRef] [PubMed]
- Ye, J.; He, L.; Beestrum, M. Implications for implementation and adoption of telehealth in developing countries: A systematic review of China’s practices and experiences. NPJ Digit. Med. 2023, 6, 174. [Google Scholar] [CrossRef] [PubMed]
- Jeddi, Z.; Bohr, A. Remote patient monitoring using artificial intelligence. In Artificial Intelligence in Healthcare; Elsevier: Amsterdam, The Netherlands, 2020; pp. 203–234. [Google Scholar]
- Shaik, T.; Tao, X.; Higgins, N.; Li, L.; Gururajan, R.; Zhou, X.; Acharya, U.R. Remote patient monitoring using artificial intelligence: Current state, applications, and challenges. Wiley Interdiscip. Rev. Data Min. Knowl. Discov. 2023, 13, e1485. [Google Scholar] [CrossRef]
- Khadija, A.; Zahra, F.F.; Naceur, A. AI-powered health chatbots: Toward a general architecture. Procedia Comput. Sci. 2021, 191, 355–360. [Google Scholar] [CrossRef]
- Görtz, M.; Baumgärtner, K.; Schmid, T.; Muschko, M.; Woessner, P.; Gerlach, A.; Byczkowski, M.; Sültmann, H.; Duensing, S.; Hohenfellner, M. An artificial intelligence-based chatbot for prostate cancer education: Design and patient evaluation study. Digit. Health 2023, 9, 20552076231173304. [Google Scholar] [CrossRef]
- Sharma, S.; Rawal, R.; Shah, D. Addressing the challenges of AI-based telemedicine: Best practices and lessons learned. J. Educ. Health Promot. 2023, 12, 338. [Google Scholar] [CrossRef] [PubMed]
- Maleki, F.; Muthukrishnan, N.; Ovens, K.; Reinhold, C.; Forghani, R. Machine learning algorithm validation: From essentials to advanced applications and implications for regulatory certification and deployment. Neuroimaging Clin. 2020, 30, 433–445. [Google Scholar] [CrossRef] [PubMed]
- Lei, J. Cross-validation with confidence. J. Am. Stat. Assoc. 2020, 115, 1978–1997. [Google Scholar] [CrossRef]
- Ebrahimian, S.; Kalra, M.K.; Agarwal, S.; Bizzo, B.C.; Elkholy, M.; Wald, C.; Allen, B.; Dreyer, K.J. FDA-regulated AI algorithms: Trends, strengths, and gaps of validation studies. Acad. Radiol. 2022, 29, 559–566. [Google Scholar] [CrossRef]
- Linardatos, P.; Papastefanopoulos, V.; Kotsiantis, S. Explainable ai: A review of machine learning interpretability methods. Entropy 2020, 23, 18. [Google Scholar] [CrossRef] [PubMed]
- Davagdorj, K.; Li, M.; Ryu, K.H. Local interpretable model-agnostic explanations of predictive models for hypertension, Advances in Intelligent Information Hiding and Multimedia Signal Processing. In Proceeding of the 16th International Conference on IIHMSP in Conjunction with the 13th International Conference on FITAT, Ho Chi Minh City, Vietnam, 5–7 November 2020; Springer: Berlin/Heidelberg, Germany, 2021; Volume 2, pp. 426–433. [Google Scholar]
- Nohara, Y.; Matsumoto, K.; Soejima, H.; Nakashima, N. Explanation of machine learning models using shapley additive explanation and application for real data in hospital. Comput. Methods Programs Biomed. 2022, 214, 106584. [Google Scholar] [CrossRef] [PubMed]
- Puerta-Beldarrain, M.; Gómez-Carmona, O.; Casado-Mansilla, D.; López-de-Ipiña, D. Human-AI collaboration to promote trust, engagement and adaptation in the process of pro-environmental and health behaviour change. In Proceedings of the International Conference on Ubiquitous Computing and Ambient Intelligence, Córdoba, Spain, 29 November–2 December 2022; Springer: Berlin/Heidelberg, Germany, 2022; pp. 381–392. [Google Scholar]
- Mishra, A. Scalable AI Governance and Ethics. In Scalable AI and Design Patterns: Design, Develop, and Deploy Scalable AI Solutions; Springer: Berlin/Heidelberg, Germany, 2024; pp. 147–165. [Google Scholar]
- Badnjević, A.; Pokvić, L.G.; Deumić, A.; Bećirović, L.S. Post-market surveillance of medical devices: A review. Technol. Health Care 2022, 30, 1315–1329. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Phillips, R.V.; Malenica, I.; Bishara, A.; Hubbard, A.E.; Celi, L.A.; Pirracchio, R. Clinical artificial intelligence quality improvement: Towards continual monitoring and updating of AI algorithms in healthcare. NPJ Digit. Med. 2022, 5, 66. [Google Scholar] [CrossRef] [PubMed]
- Murdoch, B. Privacy and artificial intelligence: Challenges for protecting health information in a new era. BMC Med. Ethics 2021, 22, 122. [Google Scholar] [CrossRef] [PubMed]
- Iserson, K.V. Informed consent for artificial intelligence in emergency medicine: A practical guide. Am. J. Emerg. Med. 2024, 76, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, R.R.; Nakeshimana, A.; Olubeko, O. Addressing fairness, bias, and appropriate use of artificial intelligence and machine learning in global health. Front. Media SA 2021, 3, 561802. [Google Scholar] [CrossRef] [PubMed]
- Smith, H. Clinical AI: Opacity, accountability, responsibility and liability. AI Soc. 2021, 36, 535–545. [Google Scholar] [CrossRef]
- Moltubakk Kempton, A.; Vassilakopoulou, P. Accountability, Transparency and Explainability in AI for Healthcare. 2021. Available online: https://dl.eusset.eu/items/9c739979-ec3f-4510-a02a-553eadee47e2 (accessed on 28 February 2024).
- Kim, B.; Park, J.; Suh, J. Transparency and accountability in AI decision support: Explaining and visualizing convolutional neural networks for text information. Decis. Support Syst. 2020, 134, 113302. [Google Scholar] [CrossRef]
- Carmody, J.; Shringarpure, S.; Van de Venter, G. AI and privacy concerns: A smart meter case study. J. Inf. Commun. Ethics Soc. 2021, 19, 492–505. [Google Scholar] [CrossRef]
- Bandari, V. Enterprise Data Security Measures: A Comparative Review of Effectiveness and Risks Across Different Industries and Organization Types. Int. J. Bus. Intell. Big Data Anal. 2023, 6, 1–11. [Google Scholar]
- Lehne, M.; Sass, J.; Essenwanger, A.; Schepers, J.; Thun, S. Why digital medicine depends on interoperability. NPJ Digit. Med. 2019, 2, 79. [Google Scholar] [CrossRef] [PubMed]
- Perugu, B.; Wadhwa, V.; Kim, J.; Cai, J.; Shin, A.; Gupta, A. Pragmatic Approaches to Interoperability–Surmounting Barriers to Healthcare Data and Information Across Organizations and Political Boundaries. Telehealth Med. Today 2023, 8, 421. [Google Scholar]
- Dikici, E.; Bigelow, M.; Prevedello, L.M.; White, R.D.; Erdal, B.S. Integrating AI into radiology workflow: Levels of research, production, and feedback maturity. J. Med. Imaging 2020, 7, 016502. [Google Scholar] [CrossRef] [PubMed]
- Balagurunathan, Y.; Mitchell, R.; El Naqa, I. Requirements and reliability of AI in the medical context. Phys. Med. 2021, 83, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Schneeberger, D.; Stöger, K.; Holzinger, A. The European Legal Framework for Medical AI, International Cross-Domain Conference for Machine Learning and Knowledge Extraction; Springer: Berlin/Heidelberg, Germany, 2020; pp. 209–226. [Google Scholar]
- Larson, D.B.; Harvey, H.; Rubin, D.L.; Irani, N.; Justin, R.T.; Langlotz, C.P. Regulatory frameworks for development and evaluation of artificial intelligence–based diagnostic imaging algorithms: Summary and recommendations. J. Am. Coll. Radiol. 2021, 18, 413–424. [Google Scholar] [CrossRef]
- Benjamens, S.; Dhunnoo, P.; Meskó, B. The state of artificial intelligence-based FDA-approved medical devices and algorithms: An online database. NPJ Digit. Med. 2020, 3, 118. [Google Scholar] [CrossRef] [PubMed]
- Muehlematter, U.J.; Daniore, P.; Vokinger, K.N. Approval of artificial intelligence and machine learning-based medical devices in the USA and Europe (2015–2020): A comparative analysis. Lancet Digit. Health 2021, 3, e195–e203. [Google Scholar] [CrossRef]
- Baric-Parker, J.; Anderson, E.E. Patient data-sharing for AI: Ethical challenges, catholic solutions. Linacre Q. 2020, 87, 471–481. [Google Scholar] [CrossRef]
- Johnson, K.B.; Wei, W.Q.; Weeraratne, D.; Frisse, M.E.; Misulis, K.; Rhee, K.; Zhao, J.; Snowdon, J.L. Precision medicine, AI, and the future of personalized health care. Clin. Transl. Sci. 2021, 14, 86–93. [Google Scholar] [CrossRef]
- Bandyopadhyay, A.; Goldstein, C. Clinical applications of artificial intelligence in sleep medicine: A sleep clinician’s perspective. Sleep Breath. 2023, 27, 39–55. [Google Scholar] [CrossRef] [PubMed]
- Galkin, F.; Zhavoronkov, A. AI in Longevity. In Artificial Intelligence for Healthy Longevity; Springer: Berlin/Heidelberg, Germany, 2023; pp. 3–13. [Google Scholar]
- Zhavoronkov, A.; Mamoshina, P.; Vanhaelen, Q.; Scheibye-Knudsen, M.; Moskalev, A.; Aliper, A. Artificial intelligence for aging and longevity research: Recent advances and perspectives. Ageing Res. Rev. 2019, 49, 49–66. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Luna, J.; Grisoni, F.; Weskamp, N.; Schneider, G. Artificial intelligence in drug discovery: Recent advances and future perspectives. Expert Opin. Drug Discov. 2021, 16, 949–959. [Google Scholar] [CrossRef] [PubMed]
- Feizi, N.; Tavakoli, M.; Patel, R.V.; Atashzar, S.F. Robotics and ai for teleoperation, tele-assessment, and tele-training for surgery in the era of COVID-19: Existing challenges, and future vision. Front. Robot. AI 2021, 8, 610677. [Google Scholar] [CrossRef] [PubMed]
- Bitencourt, A.; Naranjo, I.D.; Gullo, R.L.; Saccarelli, C.R.; Pinker, K. AI-enhanced breast imaging: Where are we and where are we heading? Eur. J. Radiol. 2021, 142, 109882. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.; Dong, B.; He, T.; Sun, Z.; Zhu, J.; Zhang, Z.; Lee, C. Progress in wearable electronics/photonics—Moving toward the era of artificial intelligence and internet of things. InfoMat 2020, 2, 1131–1162. [Google Scholar] [CrossRef]
- Forghani, N.; Maghooli, K.; Dabanloo, N.J.; Farahani, A.V.; Forouzanfar, M. Intelligent oscillometric system for automatic detection of peripheral arterial disease. IEEE J. Biomed. Health Inform. 2021, 25, 3209–3218. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.-H.; Batarseh, F.A.; Boueiz, A.; Kulkarni, A.; Su, P.-H.; Aman, J. Measuring outcomes in healthcare economics using Artificial Intelligence: With application to resource management. Data Policy 2021, 3, e30. [Google Scholar] [CrossRef] [PubMed]
- Giuste, F.; Shi, W.; Zhu, Y.; Naren, T.; Isgut, M.; Sha, Y.; Tong, L.; Gupte, M.; Wang, M.D. Explainable artificial intelligence methods in combating pandemics: A systematic review. IEEE Rev. Biomed. Eng. 2022, 16, 5–21. [Google Scholar] [CrossRef]
- Cao, L. AI in Combating the COVID-19 Pandemic. IEEE Intell. Syst. 2022, 37, 3–13. [Google Scholar] [CrossRef]
- Gu, X.; Deligianni, F.; Han, J.; Liu, X.; Chen, W.; Yang, G.-Z.; Lo, B. Beyond supervised learning for pervasive healthcare. IEEE Rev. Biomed. Eng. 2023, 17, 42–62. [Google Scholar] [CrossRef] [PubMed]
- Fechter, T.; Baltas, D. One-shot learning for deformable medical image registration and periodic motion tracking. IEEE Trans. Med. Imaging 2020, 39, 2506–2517. [Google Scholar] [CrossRef] [PubMed]
- Feng, R.; Zheng, X.; Gao, T.; Chen, J.; Wang, W.; Chen, D.Z.; Wu, J. Interactive few-shot learning: Limited supervision, better medical image segmentation. IEEE Trans. Med. Imaging 2021, 40, 2575–2588. [Google Scholar] [CrossRef] [PubMed]
- Mahapatra, D.; Bozorgtabar, B.; Ge, Z. Medical image classification using generalized zero shot learning. In Proceedings of the IEEE/CVF International Conference on Computer Vision, Montreal, QC, Canada, 10–17 October 2021; pp. 3344–3353. [Google Scholar]
- Hospedales, T.; Antoniou, A.; Micaelli, P.; Storkey, A. Meta-learning in neural networks: A survey. IEEE Trans. Pattern Anal. Mach. Intell. 2021, 44, 5149–5169. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Soltan, A.A.; Clifton, D.A. Machine learning generalizability across healthcare settings: Insights from multi-site COVID-19 screening. NPJ Digit. Med. 2022, 5, 69. [Google Scholar] [CrossRef] [PubMed]
- Khoshnevisan, F.; Chi, M. Unifying domain adaptation and domain generalization for robust prediction across minority racial groups, Machine Learning and Knowledge Discovery in Databases. In Proceedings of the Research Track: European Conference, ECML PKDD 2021, Bilbao, Spain, 13–17 September 2021; Proceedings, Part I 21. Springer: Berlin/Heidelberg, Germany, 2021; pp. 521–537. [Google Scholar]
- Rieke, N.; Hancox, J.; Li, W.; Milletari, F.; Roth, H.R.; Albarqouni, S.; Bakas, S.; Galtier, M.N.; Landman, B.A.; Maier-Hein, K. The future of digital health with federated learning. NPJ Digit. Med. 2020, 3, 119. [Google Scholar] [CrossRef]
- Hogg, H.D.J.; Al-Zubaidy, M.; Talks, J.; Denniston, A.K.; Kelly, C.J.; Malawana, J.; Papoutsi, C.; Teare, M.D.; A Keane, P.; Beyer, F.R.; et al. Stakeholder perspectives of clinical artificial intelligence implementation: Systematic review of qualitative evidence. J. Med. Internet Res. 2023, 25, e39742. [Google Scholar] [CrossRef]
- Gerlings, J.; Jensen, M.S.; Shollo, A. Explainable ai, but explainable to whom? an exploratory case study of xai in healthcare. In Handbook of Artificial Intelligence in Healthcare: Vol 2: Practicalities and Prospects; Springer: Berlin/Heidelberg, Germany, 2022; pp. 169–198. [Google Scholar]
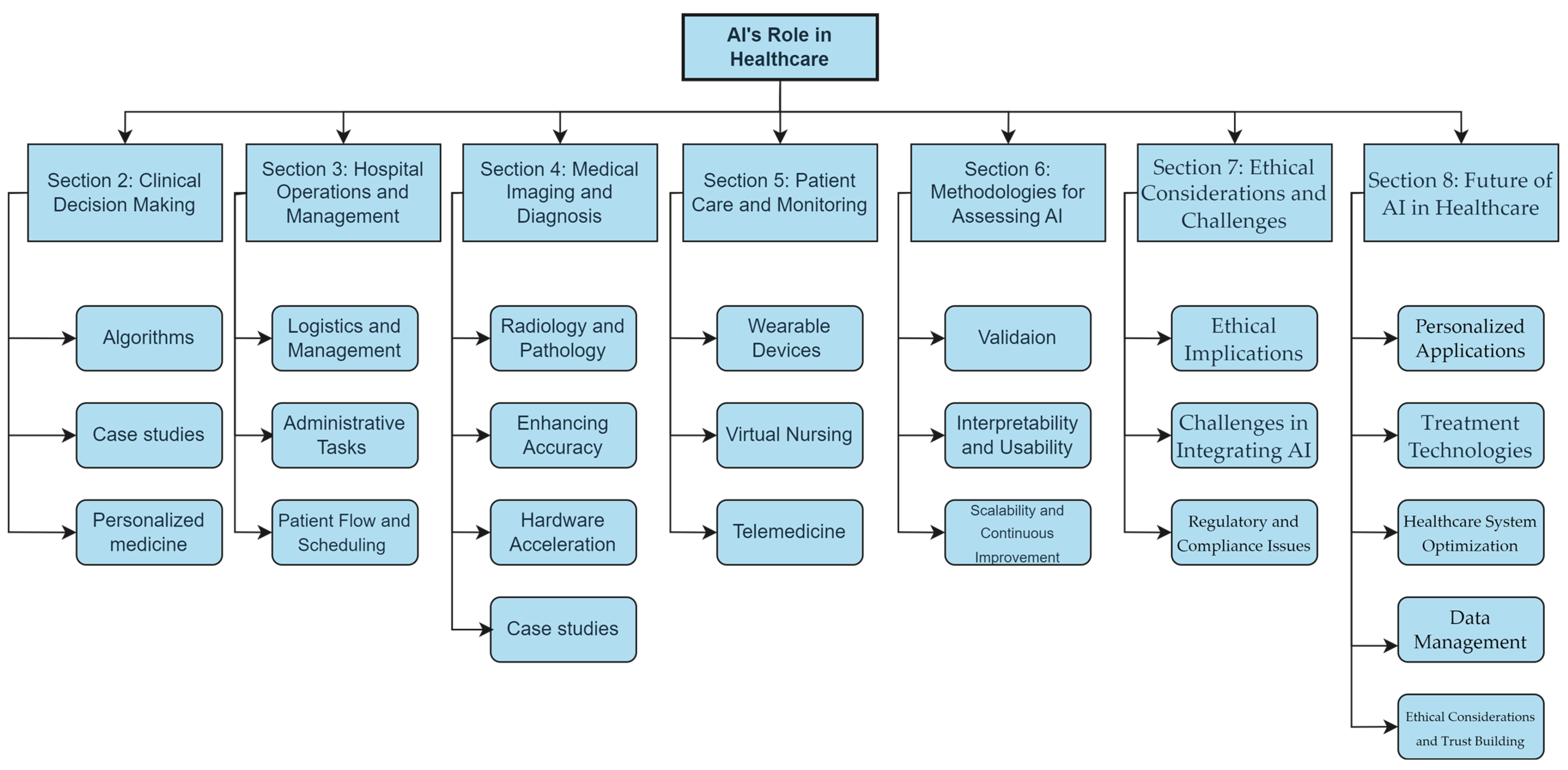
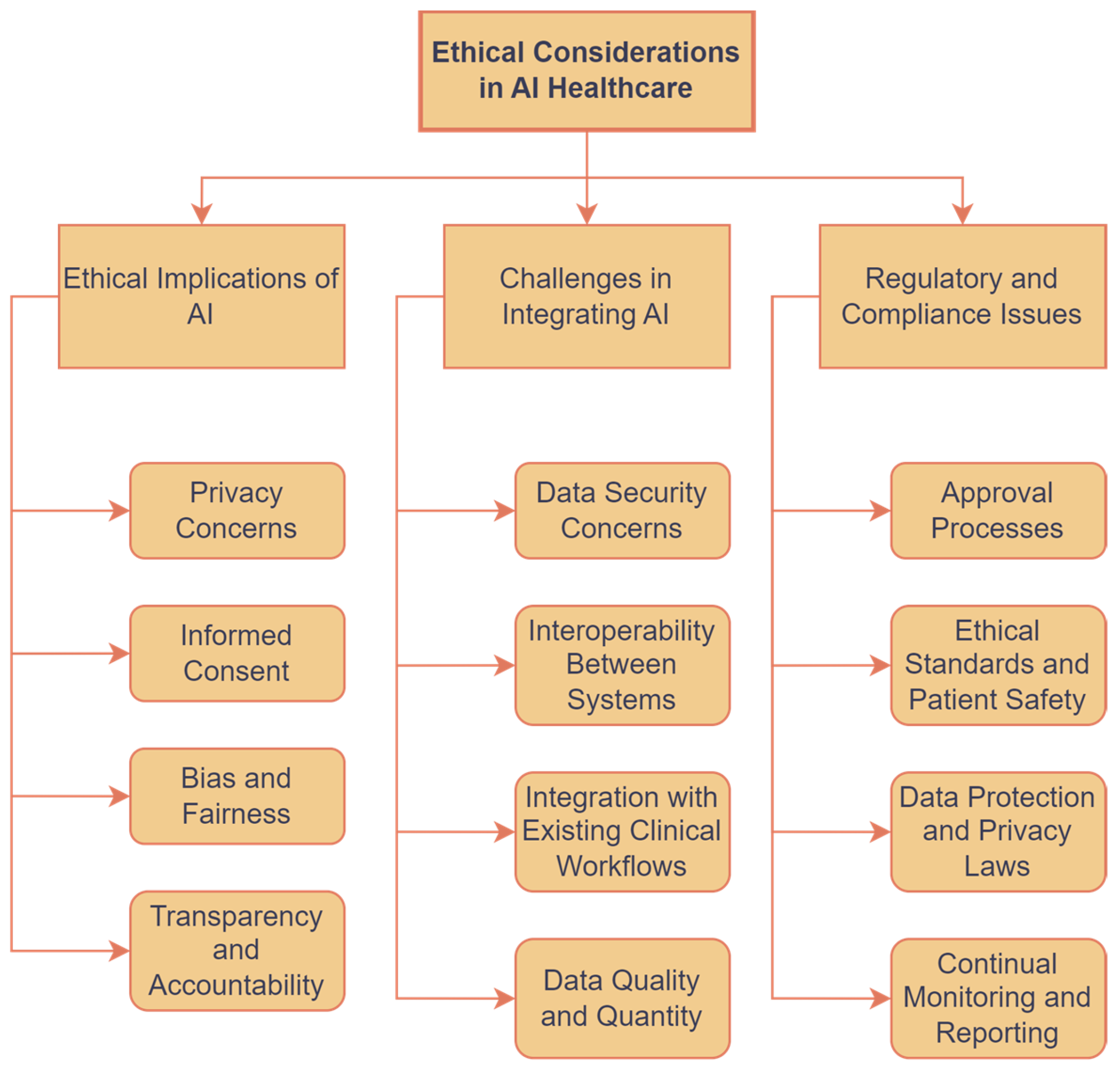
| Algorithm Type | General Application | Limitations | Comments | Example |
|---|---|---|---|---|
| Convolutional Neural Networks (CNNs) | Image recognition and analysis in medical imaging (e.g., X-rays, MRI, CT scans) | Require large labeled datasets and substantial computational resources; can be a “black box” making interpretability difficult | Highly effective for spatial data; state of the art in medical image analysis | Deeplab v3+, a CNN variant for gastric cancer segmentation [28]. Results: 95.76% accuracy, outperforming SegNet/ICNet. |
| Recurrent Neural Networks (RNNs) and Long Short-Term Memory (LSTM) Networks | Analysis of sequential data such as ECG, EEG signals, or patient health records | Prone to overfitting on smaller datasets; long training times; difficulty in parallelizing the tasks | Suited for time-series data; LSTM addresses vanishing gradient problem in RNNs | LSTM for EEG signal classification [29]. Results: 71.3% accuracy, utilizing novel one-dimensional gradient descent activation functions for enhanced performance. |
| Transformer Models (e.g., BERT, GPT) | Natural language processing tasks, including clinical text analysis and patient history summarization | Require significant computational power and memory; pre-training on large datasets is time-consuming | Offer state-of-the-art performance in NLP; enable understanding of context in clinical documentation | Clinical-specific BERT (Transformer) for Japanese text analysis [30]: pre-trained on 120 million texts, achieving 0.773 Masked-LM and 0.975 Next Sentence Prediction accuracy, indicating potential for complex medical NLP tasks. |
| Generative Adversarial Networks (GANs) | Synthetic data generation for training models without compromising patient privacy; augmenting datasets | Training stability issues; generating high-quality data is challenging | Useful in data-limited scenarios; potential in creating realistic medical images for training | Differentially private GAN for synthetic data generation: utilizes convolutional AEs and GANs to produce realistic synthetic medical data, preserving data characteristics and outperforming existing models [31]. |
| Graph Neural Networks (GNNs) | Modeling complex relationships and interactions between health data points (e.g., drug interaction prediction, disease progression modeling) | Complex model architectures that are difficult to interpret; scalability to very large graphs | Effective for data represented as graphs; emerging applications in personalized medicine | Knowledge-GNN for drug–drug interaction prediction: leverages knowledge graphs to capture complex drug relationships and neighborhood information, outperforming conventional models [32]. |
| Aspect | Applications |
|---|---|
| AI for hospital logistics and resource management | Predictive inventory management for medical supplies, medications, and equipment; efficient facility management including HVAC systems and predictive maintenance; optimization of resource allocation for staff and materials; and supply chain optimization and management during emergencies and health crises. |
| Automating administrative tasks with AI | Patient data management including EMRs and unstructured data analysis; billing and claims processing automation for accuracy and compliance; AI-driven scheduling systems for appointments and procedures; document management and processing automation; automated communication and reminders for patient engagement; and data security and compliance monitoring. |
| AI in patient flow and scheduling optimization | Optimization of patient flow through predictive analysis of admissions, discharges, and transfers; dynamic scheduling systems for appointments and procedures, minimizing no-shows and cancellations; reduction in waiting times through better triage processes and real-time patient wait time prediction; and enhancement of patient experience by providing accurate information and integrating with telehealth services for virtual consultations. |
| Imaging Modality | Application | Example of AI System | Impact |
|---|---|---|---|
| MRI | AI applications in MRI analysis encompass detection of brain abnormalities, tumors, strokes, neurodegenerative diseases, and more. AI can analyze images and quantify the volume of affected areas. | An AI system analyzes MRI images to detect brain abnormalities, such as tumors or strokes, and quantifies their volume, aiding in treatment planning [118]. | Improved detection of tumors, strokes, and neurodegenerative diseases; quantification of affected areas aids in treatment planning and disease monitoring. |
| CT | AI in CT scan interpretation includes detecting lung nodules, identifying fractures and hemorrhages, assessing stroke severity, and characterizing tumor progression. AI systems can process CT scans rapidly and accurately, aiding in timely diagnosis. | An AI model diagnoses lung cancer with high accuracy and reduced false positives, improving diagnostic precision [119]. | Faster detection of life-threatening conditions; enhanced accuracy compared to traditional methods; potential to save lives in emergency situations. |
| X-ray | AI applications in X-ray enhance image analysis for tumor detection, improving accuracy and reducing false positives and negatives. AI systems serve as a second reviewer, enhancing the sensitivity of cancer screening. | AI-based CAD algorithms significantly improve radiologists’ sensitivity in breast cancer detection, reducing false negatives and improving cancer detection rates [120]. | Increased sensitivity in detecting breast cancer lesions; reduction in false positives and negatives; enhancement of radiologists’ diagnostic accuracy. |
| Ultrasound | AI aids in analyzing echocardiography scans to assess cardiovascular function and detect structural abnormalities of the heart. AI systems measure parameters such as ejection fraction and aid in diagnosing and managing heart diseases. | A novel AI algorithm accurately calculates left ventricular ejection time in echocardiography, providing reliable metrics for cardiac function assessment [121]. | Accurate assessment of cardiovascular parameters; reduction in user-dependent variability; enhancement of clinical utility in echocardiography. |
| Main Applications | Key Technologies and Applications | Benefits | Challenges |
|---|---|---|---|
| AI-powered wearable devices | Continuous physiological monitoring (heart rate, blood pressure, etc.); early detection of health issues; personalized recommendations for lifestyle changes | Improved patient engagement; proactive health management | Data collection and model deployment; balancing accuracy with wearable device limitations |
| Virtual nursing assistants | 24/7 patient support and health reminders; chronic disease management; patient education and behavior monitoring | Enhanced patient engagement and education; improved treatment plan compliance | Data privacy and information accuracy; ensuring they complement human care |
| AI in telemedicine and remote patient engagement | Advanced diagnostics and consultations; personalized virtual consultations; remote patient monitoring and predictive analytics | Increased healthcare accessibility; proactive chronic condition care | Data privacy, system accuracy, and integration |
| Trend/Application | Potential Impact | Challenges | Future Directions |
|---|---|---|---|
| Personalized medicine | Revolutionizes treatment for diseases with genetic components, significantly improving patient outcomes through customized care plans. | Data privacy, integration into clinical practice, and ensuring equitable access across diverse patient populations. | Expanding personalized medicine to encompass mental health, lifestyle diseases, and integrating real-time health monitoring data for dynamic treatment adjustments. |
| AI-powered tools for health and sleep monitoring | Improved detection and diagnosis of sleep disorders, early identification of potential health issues, personalized treatment, and proactive interventions. | Data privacy, accuracy of predictions, and user acceptance and comfort with interventional technologies. | Designing analysis and intervention technologies to monitor, predict, and manage health issues and sleep disorders; integration with wearable devices and smart home technology, providing real-time adjustments. |
| Longevity and aging | Unlocks new possibilities in aging research, promoting healthier, extended lifespans through AI-driven genomic interventions and predictive analytics for preventive medicine. | Addressing ethical implications of longevity research, ensuring accessibility and fairness in anti-aging treatments. | Leveraging AI for comprehensive health longevity platforms, integrating AI with regenerative medicine, and creating personalized anti-aging treatment plans based on predictive health analytics. |
| AI in drug discovery and development | Reduces time and costs in drug market introduction, enhances the efficacy of new drugs by identifying optimal candidate molecules. | Ensuring the reliability of AI predictions; ethical concerns around automated decision-making in drug development. | Leveraging AI to explore novel drug pathways, improve clinical trial design, and predict patient responses to treatments more accurately. |
| Advanced robotics in surgery and rehabilitation | Improves precision in surgeries and patient outcomes in rehabilitation, potentially reducing recovery times and healthcare costs. | Ethical considerations around autonomy; the need for robust training programs for medical staff on robotic systems. | Developing autonomous surgical robots, enhancing robotic systems with sensory feedback for improved rehabilitation outcomes, and expanding applications in minimally invasive procedures. |
| AI hardware accelerators | Faster diagnoses, treatment planning, and analysis, improved patient care outcomes, and real-time medical data processing. | Integration with medical devices; cost and power consumption of accelerators. | Develop healthcare-specific AI hardware; improve accessibility of AI-driven healthcare. |
| AI-enhanced medical imaging | Enables earlier and more accurate disease detection, potentially even identifying health risks before symptoms appear, thus shifting towards preventive healthcare models. | Balancing the need for patient privacy with the benefits of data sharing for AI training; integrating AI tools with existing healthcare infrastructures. | Developing AI systems capable of cross-modality analysis, improving 3D imaging techniques, and creating predictive models for disease progression based on imaging data. |
| Integrating AI with IoT and wearables | Leads to proactive health management and personalized health recommendations, potentially reducing emergency healthcare interventions. | Addressing data security and ensuring device interoperability across different healthcare systems. | Enhancing predictive analytics for early detection of health anomalies, creating an ecosystem of interconnected devices for holistic health monitoring; unobtrusive health monitoring. |
| Enhancing patient outcomes and system efficiency | Promises significant improvements in patient care through earlier disease detection, customized treatments, and optimized healthcare resource management. | Ensuring equitable improvements across all populations, addressing the digital divide in healthcare access. | Implementing AI-driven health advisories in public health strategies, optimizing healthcare delivery models with predictive resource allocation, and enhancing remote patient monitoring systems. |
| Global health monitoring systems | Strengthens global health security by enabling rapid response to disease outbreaks and guiding public health interventions with data-driven insights. | Integrating diverse data streams in real time, adapting models quickly to emerging health threats. | Developing global AI-powered surveillance systems, enhancing predictive models for epidemic and pandemic forecasting, and creating AI-driven platforms for vaccine and therapeutic development. |
| Addressing data scarcity | Facilitates AI development in under-researched areas, such as rare diseases, by making efficient use of limited data resources. | Creating effective models with sparse data, ensuring the generalizability of findings from limited datasets. | Exploring novel data augmentation techniques, crowdsourcing for data collection, and cross-institutional data sharing initiatives to enrich datasets. Developing advanced techniques based on few-shot leaning. |
| Ensuring model versatility | Allows for the broader application of AI models across varying healthcare settings and patient demographics, improving the universality and accessibility of AI-driven healthcare solutions. | Developing adaptable models that maintain high accuracy across diverse datasets, addressing potential biases in AI training. | Advancing transfer learning and domain adaptation techniques that can be personalized at the point of care. |
| Ensuring data privacy | Enhances privacy and security in healthcare applications, addressing one of the major concerns of digital health data management. | Balancing the utility of data for AI training with stringent privacy requirements, adapting regulations to keep pace with technological advancements. | Developing more advanced privacy-preserving AI techniques, such as secure multi-party computation, federated learning, and advanced encryption methods for health data. |
| Stakeholder acceptance | Successful AI integration in healthcare; improved trust and collaboration. | Concerns about AI reliability and clinician autonomy. | Transparent communication and training programs. |
| Building trust with Explainable AI (XAI) | Enhances the trustworthiness of AI systems among healthcare professionals and patients, ensuring that AI-supported decisions are well informed and ethically sound. | Simplifying complex AI decision-making processes for non-technical stakeholders, ensuring explanations are meaningful and actionable. | Integrating XAI into clinical workflows, developing standards for AI explanations in healthcare, and educating healthcare professionals on interpreting AI decisions. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maleki Varnosfaderani, S.; Forouzanfar, M. The Role of AI in Hospitals and Clinics: Transforming Healthcare in the 21st Century. Bioengineering 2024, 11, 337. https://doi.org/10.3390/bioengineering11040337
Maleki Varnosfaderani S, Forouzanfar M. The Role of AI in Hospitals and Clinics: Transforming Healthcare in the 21st Century. Bioengineering. 2024; 11(4):337. https://doi.org/10.3390/bioengineering11040337
Chicago/Turabian StyleMaleki Varnosfaderani, Shiva, and Mohamad Forouzanfar. 2024. "The Role of AI in Hospitals and Clinics: Transforming Healthcare in the 21st Century" Bioengineering 11, no. 4: 337. https://doi.org/10.3390/bioengineering11040337
APA StyleMaleki Varnosfaderani, S., & Forouzanfar, M. (2024). The Role of AI in Hospitals and Clinics: Transforming Healthcare in the 21st Century. Bioengineering, 11(4), 337. https://doi.org/10.3390/bioengineering11040337







