A Finite Element Analysis Study of Edentulous Model with Complete Denture to Simulate Masticatory Movement
Abstract
1. Introduction
2. Materials and Methods
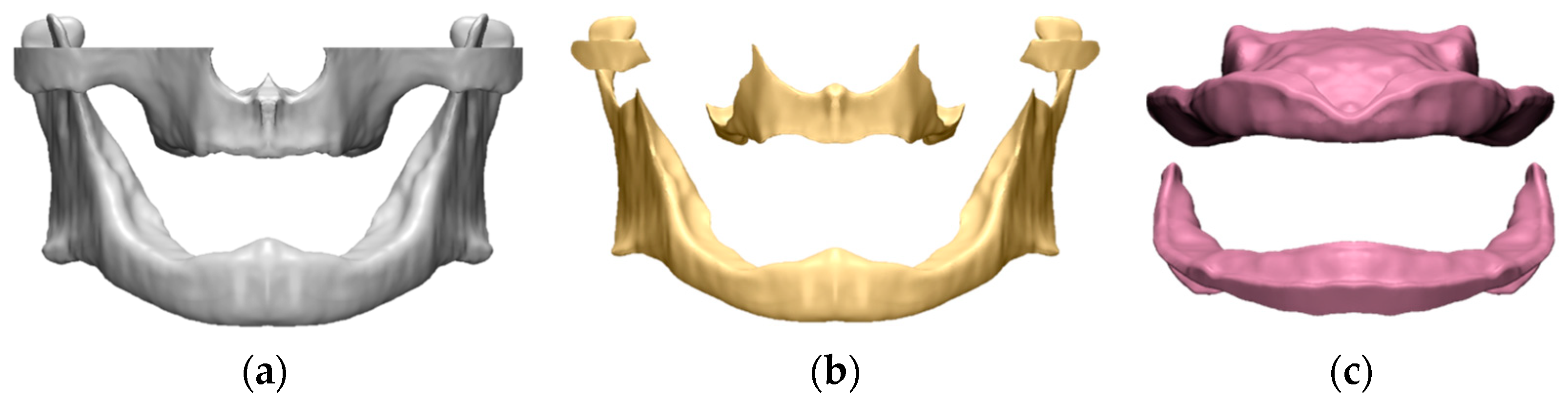
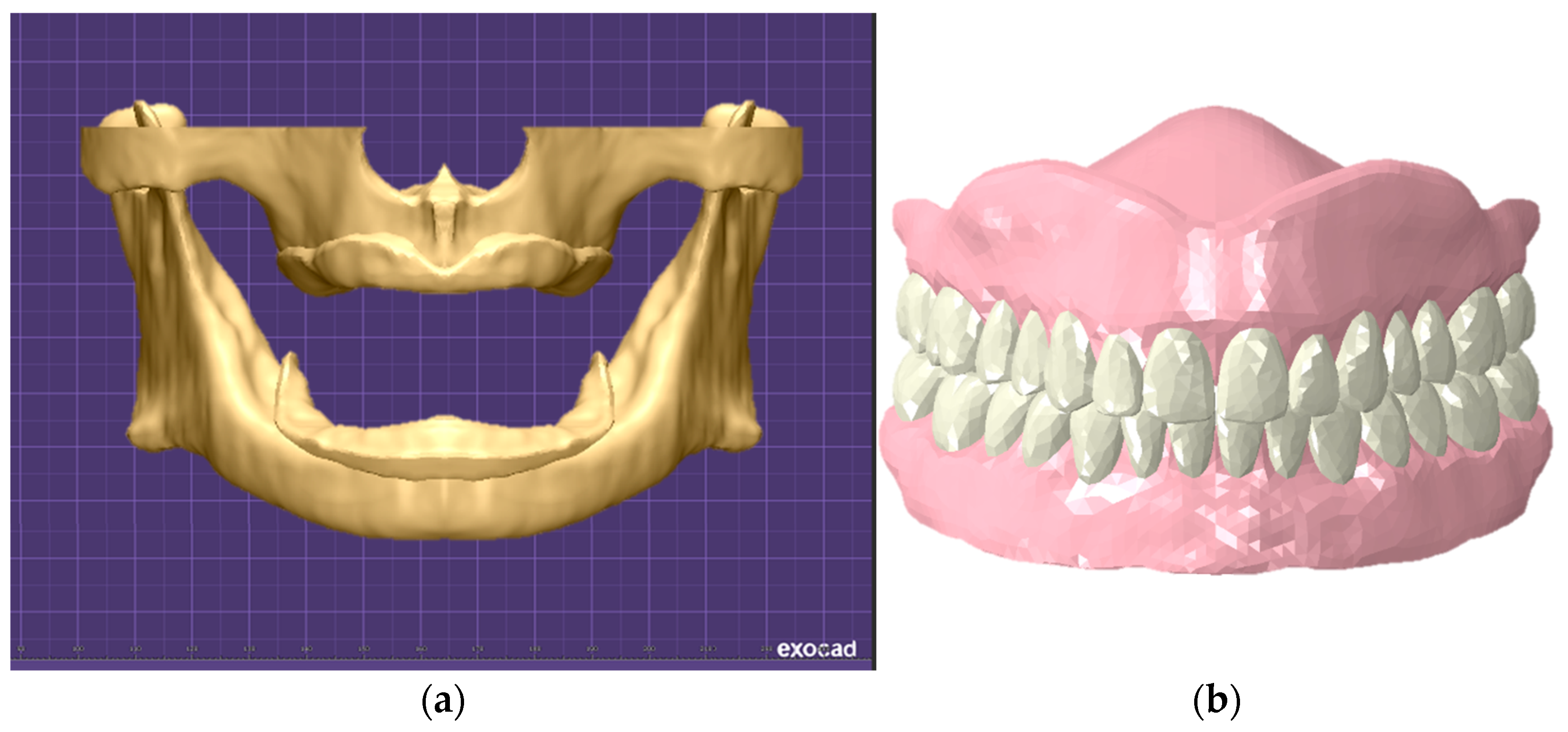
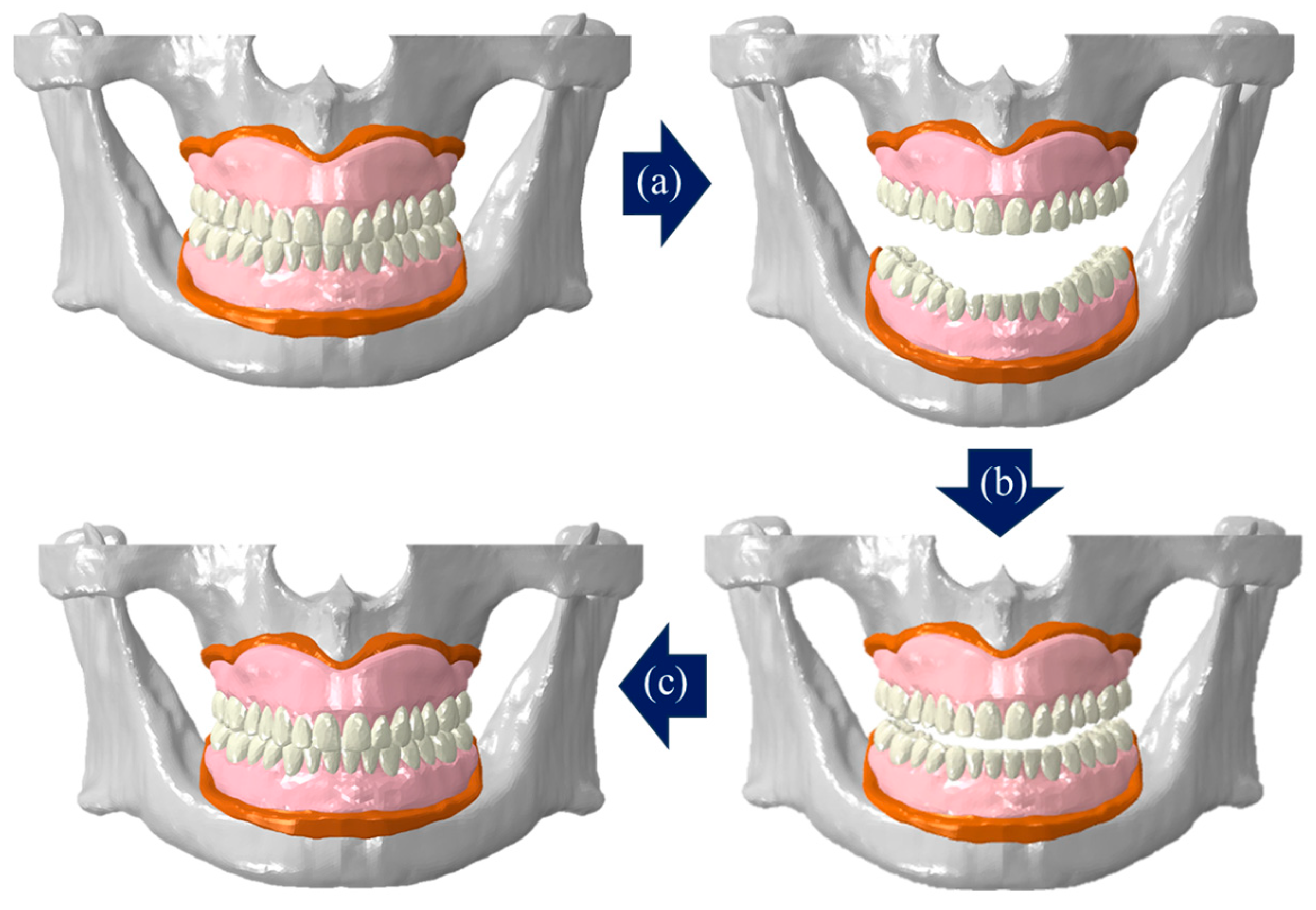
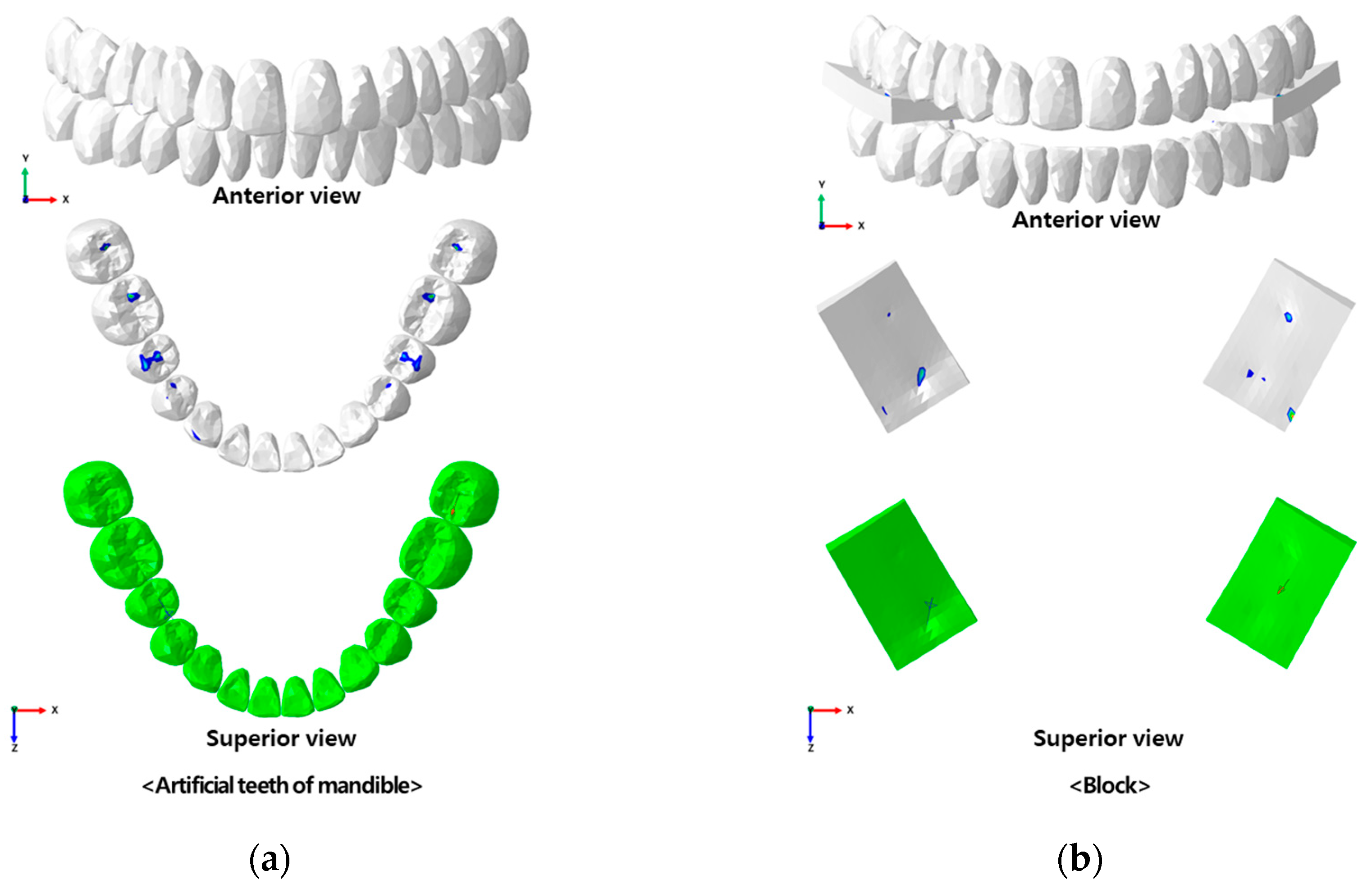
2.1. Construction of Edentulous Alveolar Bone-Gingiva and Complete Denture FE Model
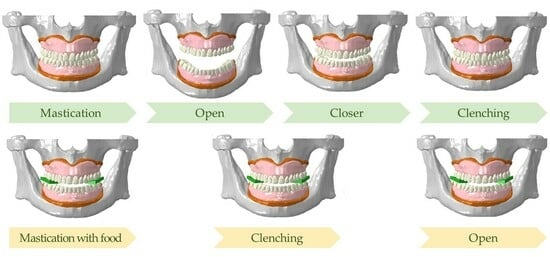
2.2. Validation of the Constructed FE Model
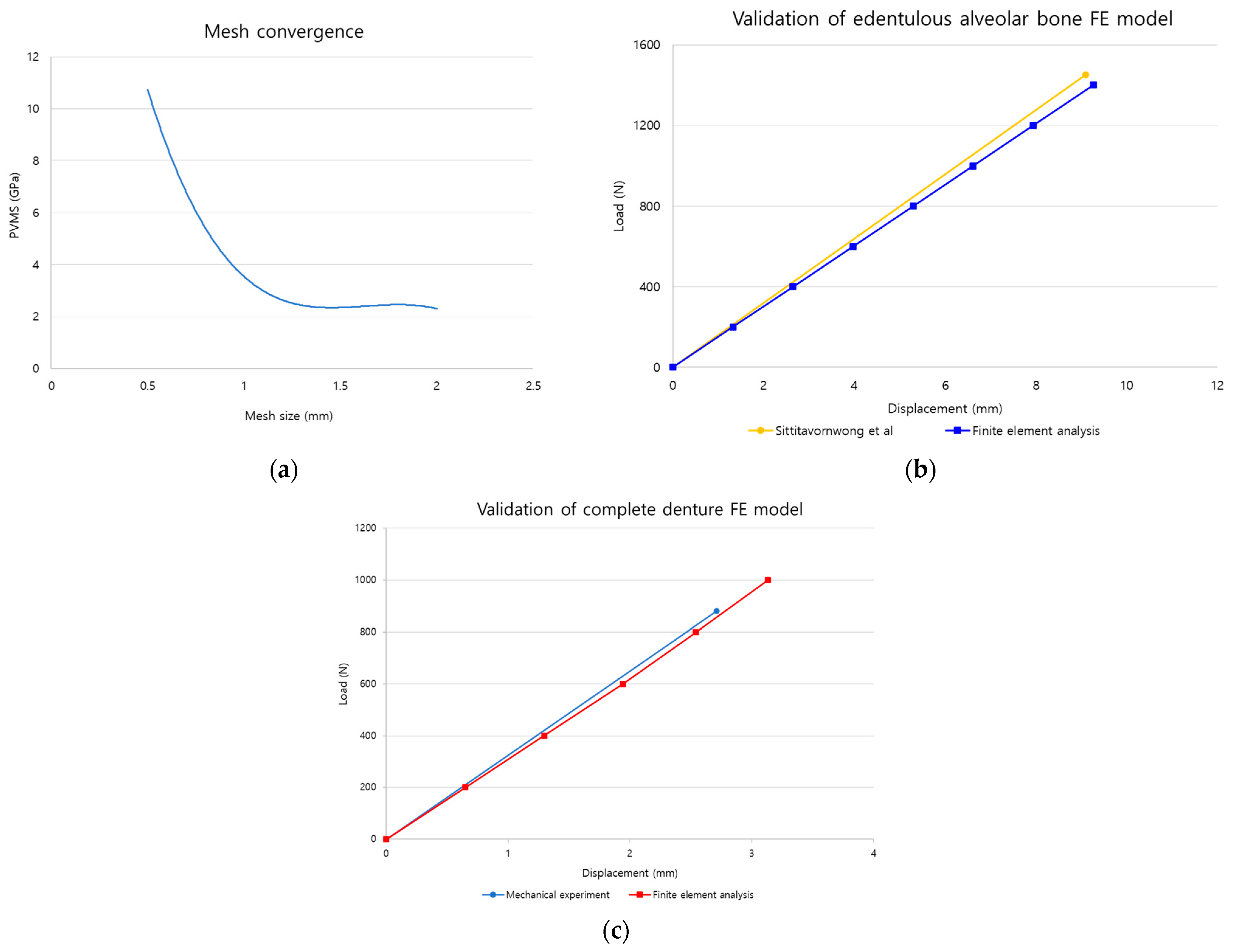
2.2.1. Mesh Convergence
2.2.2. Edentulous Alveolar Bone Model
2.2.3. Complete Denture Model
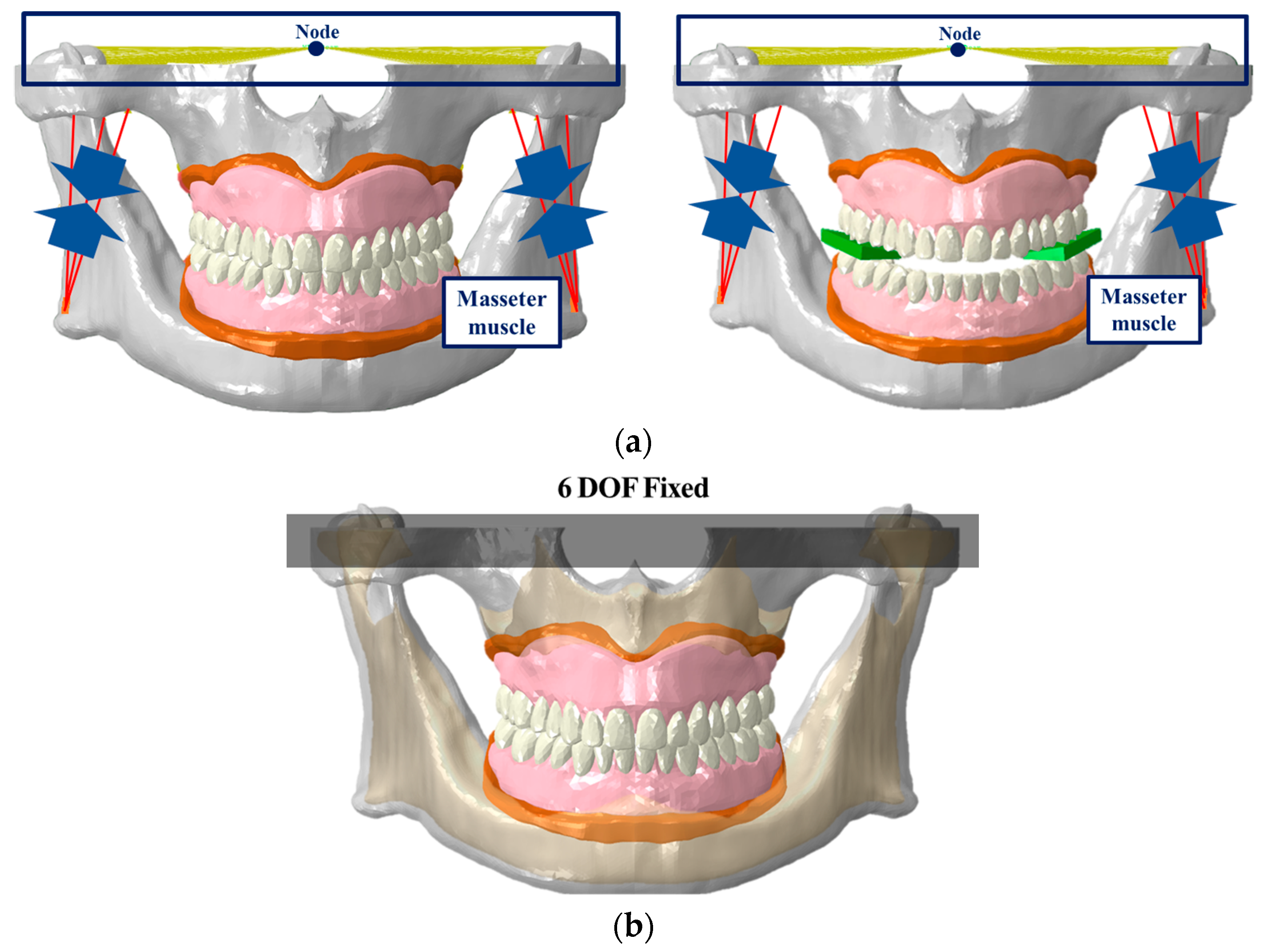
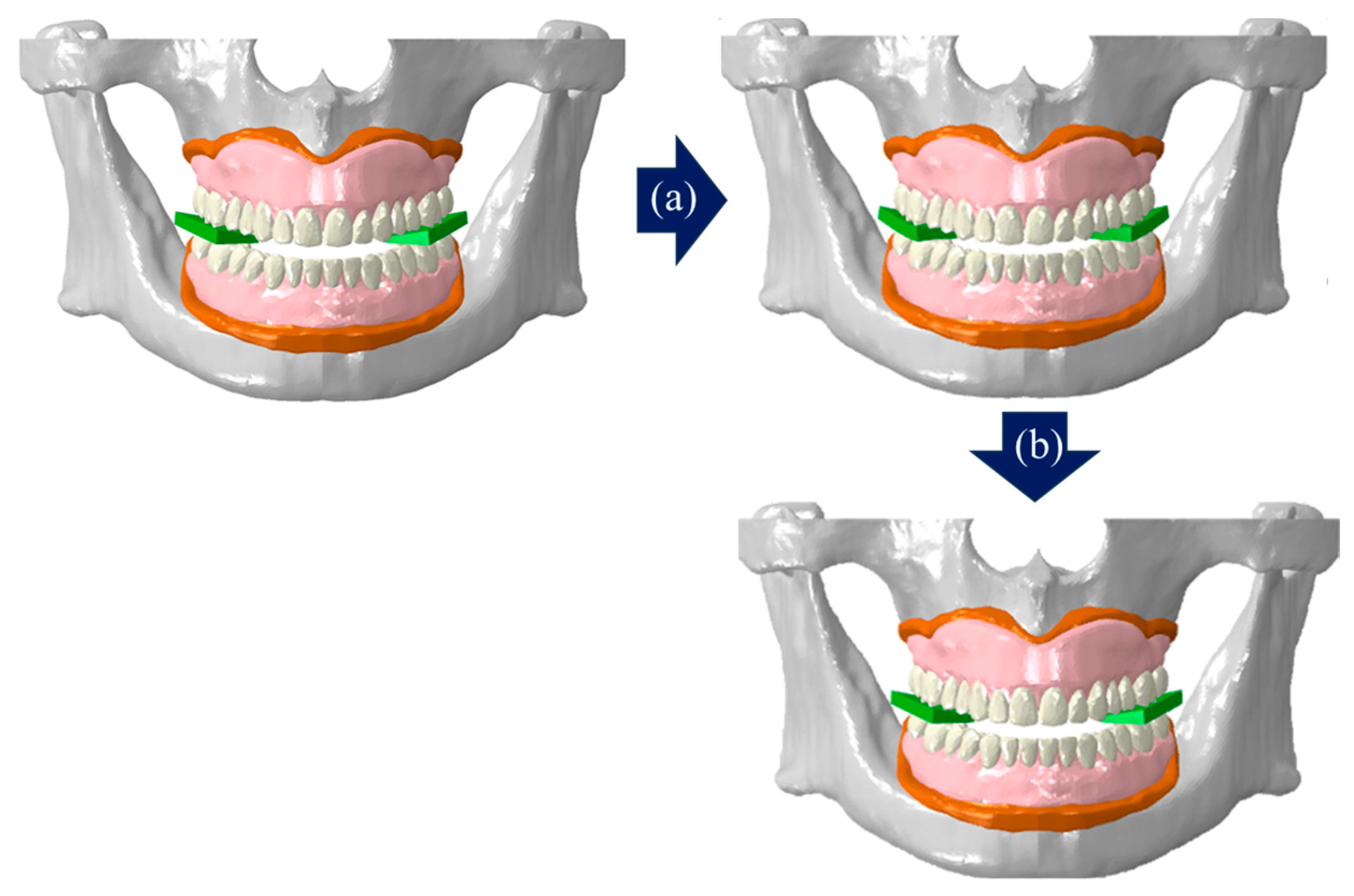
2.3. Loading and Boundary Conditions
3. Results
3.1. Validation of the Edentulous Alveolar Bone and Complete Denture FE Model
3.1.1. Mesh Convergence
3.1.2. Edentulous Alveolar Bone Model
3.1.3. Complete Denture Model
3.2. Implementation of Mastication Movement
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jung, Y.; Lee, J.; Hong, S.J.; Noh, K.; Kim, H.S.; Pae, A. Fabrication of complete dentures by conventional method and CAD/CAM milling: A case report. J. Korean Acad. Prosthodont. 2019, 57, 296–303. [Google Scholar] [CrossRef]
- Yim, S.H.; Kim, J.H. Esthetically improved complete denture by gingival shade alteration: A case report. J. Korean Acad. Prosthodont. 2014, 52, 239–245. [Google Scholar] [CrossRef]
- Park, M.; Park, S.W.; Lim, H.P.; Park, C.; Yun, K.D. Fabrication of mandibular suction denture for complete edentulous patient: A case report. J. Korean Acad. Prosthodont. 2020, 58, 257–267. [Google Scholar] [CrossRef]
- Koide, K. Designing Complete Denture, 5th ed.; Ishiyaku Publishers, Inc.: Tokyo, Japan, 2019. [Google Scholar]
- Lee, S.M.; Yoo, K.H. Three-dimensional photoelastic stress analysis of occlusions of complete denture supported by shape memory implants. J. Dent. Implant. Res. 1992, 11, 51–67. [Google Scholar]
- Preoteasa, E.; Preoteasa, C.T.; Iosif, L.; Magureanu, C.M.; Imre, M. Denture and overdenture complications. In Emerging Trends in Oral Health Sciences and Dentistry; IntechOpen: London, UK, 2015; pp. 193–226. [Google Scholar]
- Lee, J.S.; Song, Y.G.; Cho, I.H. The Effect of Reinforcing Materials on the Transverse Strength of Denture Base Resin. J. Dent. Rehabil. Appl. Sci. 2012, 28, 327–337. [Google Scholar]
- Lee, J.I.; Jo, J.Y.; Yun, M.J.; Jeon, Y.C.; Jeong, C.M.; Huh, J.B. Comparison of metal wire reinforcement and glass fiber reinforcement in repaired maxillary complete denture. J. Korean Acad. Prosthodont. 2013, 51, 284–291. [Google Scholar] [CrossRef]
- Özkan, Y.K. Post Insertion Problems in Complete Dentures. In Complete Denture Prosthodontics: Treatment and Problem Solving; Springer International Publishing AG, Part of Nature: Berlin/Heidelberg, Germany, 2018; pp. 145–195. [Google Scholar]
- Kim, Y.J.; Song, Y.G. Comparative analysis of case series for the prosthetic rehabilitation of edentulous patients using suction denture. J. Korean Acad. Prosthodont. 2019, 57, 389–396. [Google Scholar] [CrossRef]
- Cheng, Y.Y.; Cheung, W.L.; Chow, T.W. Strain analysis of maxillary complete denture with three-dimensional finite element method. J. Prosthet. Dent. 2010, 103, 309–318. [Google Scholar] [CrossRef]
- Takayama, Y.; Yamada, T.; Araki, O.; Seki, T.; Kawasaki, T. The dynamic behaviour of a lower complete denture during unilateral loads: Analysis using the finite element method. J. Oral Rehabil. 2001, 28, 1064–1074. [Google Scholar] [CrossRef]
- Shrivastava, R.; Chaturvedi, S.; Verma, A.K.; Ali, M.; Nagendra, A.; Chaturvedi, M. Stress distribution under commercial denture liners-a finite element and clinical analysis. J. Clin. Diagn. Res. JCDR 2016, 10, ZC14. [Google Scholar] [CrossRef]
- Żmudzki, J.; Chladek, G.; Malara, P. Use of finite element analysis for the assessment of biomechanical factors related to pain sensation beneath complete dentures during mastication. J. Prosthet. Dent. 2018, 120, 934–941. [Google Scholar] [CrossRef] [PubMed]
- Jung, B.T.; Kim, W.H.; Kim, B.; Lee, J.H. Biomechanical integrity of hydroxyapatite/poly-l-lactide fixation system in mandibular body reconstruction with deep circumflex iliac artery free flap. J. Mater. Res. Technol. 2022, 18, 4662–4671. [Google Scholar] [CrossRef]
- Kim, W.H.; Hong, K.; Lim, D.; Lee, J.H.; Jung, Y.J.; Kim, B. Optimal position of attachment for removable thermoplastic aligner on the lower canine using finite element analysis. Materials 2020, 13, 3369. [Google Scholar] [CrossRef] [PubMed]
- Koblar, D.; Škofic, J.; Boltežar, M. Evaluation of the young’s modulus of rubber-like materials bonded to rigid surfaces with respect to Poisson’s ratio. Stroj. Vestn. J. Mech. Eng. 2014, 60, 506–511. [Google Scholar] [CrossRef]
- Hussein, L.A. 3D finite element analysis of the influence of different soft lining materials with variable thicknesses on stress transmitted to underlying mucosa. Int. J. Adv. Res. 2014, 2, 896–905. [Google Scholar]
- Baldini, A.; Bruzzesi, G.; Zaffe, D.; Giacopini, M.; Strozzi, A.; De Pol, A. Biomechanical aspects in dental replacements. WIT Trans. State Art Sci. Eng. 2008, 35, 197–243. [Google Scholar]
- Lima, J.B.G.; Orsi, I.A.; Borie, E.; Lima, J.H.F.; Noritomi, P.Y. Analysis of stress on mucosa and basal bone underlying complete dentures with different reliner material thicknesses: A three-dimensional finite element study. J. Oral Rehabil. 2013, 40, 767–773. [Google Scholar] [CrossRef]
- Daas, M.; Dubois, G.; Bonnet, A.S.; Lipinski, P.; Rignon-Bret, C. A complete finite element model of a mandibular implant-retained overdenture with two implants: Comparison between rigid and resilient attachment configurations. Med. Eng. Phys. 2008, 30, 218–225. [Google Scholar] [CrossRef]
- Barão, V.A.R.; Delben, J.A.; Lima, J.; Cabral, T.; Assunção, W.G. Comparison of different designs of implant-retained overdentures and fixed full-arch implant-supported prosthesis on stress distribution in edentulous mandible–a computed tomography-based three-dimensional finite element analysis. J. Biomech. 2013, 46, 1312–1320. [Google Scholar] [CrossRef]
- Christensen, L.V.; Tran, K.T.; Mohamed, S.E. Gum chewing and jaw muscle fatigue and pains. J. Oral Rehabil. 1996, 23, 424–437. [Google Scholar] [CrossRef]
- Kim, W.H. Biomechanical Diagnostic Guideline for Temporomandibular Joint Movement Disorders. Ph.D. Dissertation, Sejong University, Seoul, Republic of Korea, 2022; p. 93. [Google Scholar]
- Langenbach, G.E.J.; Hannam, A.G. The role of passive muscle tensions in a three-dimensional dynamic model of the human jaw. Arch. Oral Biol. 1999, 44, 557–573. [Google Scholar] [CrossRef]
- Sittitavornwong, S.; Ashley, D.; Denson, D.; Walma, D.C.; Potter, S.; Lin, C.P.; Freind, J. Assessment of the integrity of Adult human mandibular angle. Craniomaxillofac. Trauma Reconstr. Open 2019, 3, s-0038. [Google Scholar] [CrossRef]
- Hedzelek, W.; Gajdus, P. Comparison of mechanical strength of palatal denture bases made from various plastic materials. Int. J. Prosthodont. 2006, 19, 193. [Google Scholar] [PubMed]
- Yu, S.H.; Cho, H.W.; Oh, S.; Bae, J.M. Effects of glass fiber mesh with different fiber content and structures on the compressive properties of complete dentures. J. Prosthet. Dent. 2015, 113, 636–644. [Google Scholar] [CrossRef] [PubMed]
- Jadhav, S.S.; Sanyal, P.K.; Tewary, S.; Guru, R.; Joshi, S.; Kore, A. Comparison of Mechanical Strength of Palatal Denture Base using Four Mesh Designs on Shallow Palatal Vault Configuration: An in vitro Study. Int. J. Prev. Clin. Dent. Res. 2017, 4, 201–209. [Google Scholar] [CrossRef]
- Ortún-Terrazas, J.; Cegoñino, J.; Del Palomar, A.P. In silico study of cuspid’periodontal ligament damage under parafunctional and traumatic conditions of whole-mouth occlusions. A patient-specific evaluation. Comput. Methods Programs Biomed. 2020, 184, 105107. [Google Scholar] [CrossRef] [PubMed]
- Duanmu, Z.; Liu, L.; Deng, Q.; Ren, Y.; Wang, M. Development of a biomechanical model for dynamic occlusal stress analysis. Int. J. Oral Sci. 2021, 13, 29. [Google Scholar] [CrossRef]
- Jahadakbar, A.; Shayesteh Moghaddam, N.; Amerinatanzi, A.; Dean, D.; Karaca, H.E.; Elahinia, M. Finite element simulation and additive manufacturing of stiffness-matched niti fixation hardware for mandibular reconstruction surgery. Bioengineering 2016, 3, 36. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-H.; Seo, J.-H.; Park, S.-W.; Kim, W.-G.; Jung, T.-G.; Lee, S.-J. A Finite Element Analysis Study of Edentulous Model with Complete Denture to Simulate Masticatory Movement. Bioengineering 2024, 11, 336. https://doi.org/10.3390/bioengineering11040336
Lee J-H, Seo J-H, Park S-W, Kim W-G, Jung T-G, Lee S-J. A Finite Element Analysis Study of Edentulous Model with Complete Denture to Simulate Masticatory Movement. Bioengineering. 2024; 11(4):336. https://doi.org/10.3390/bioengineering11040336
Chicago/Turabian StyleLee, Jeong-Hyeon, Jeong-Hee Seo, Shin-Wook Park, Won-Gi Kim, Tae-Gon Jung, and Sung-Jae Lee. 2024. "A Finite Element Analysis Study of Edentulous Model with Complete Denture to Simulate Masticatory Movement" Bioengineering 11, no. 4: 336. https://doi.org/10.3390/bioengineering11040336
APA StyleLee, J.-H., Seo, J.-H., Park, S.-W., Kim, W.-G., Jung, T.-G., & Lee, S.-J. (2024). A Finite Element Analysis Study of Edentulous Model with Complete Denture to Simulate Masticatory Movement. Bioengineering, 11(4), 336. https://doi.org/10.3390/bioengineering11040336