Correlation between Malocclusion and Mandibular Fractures: An Experimental Study Comparing Dynamic Finite Element Models and Clinical Case Studies
Abstract
1. Introduction
2. Materials and Method
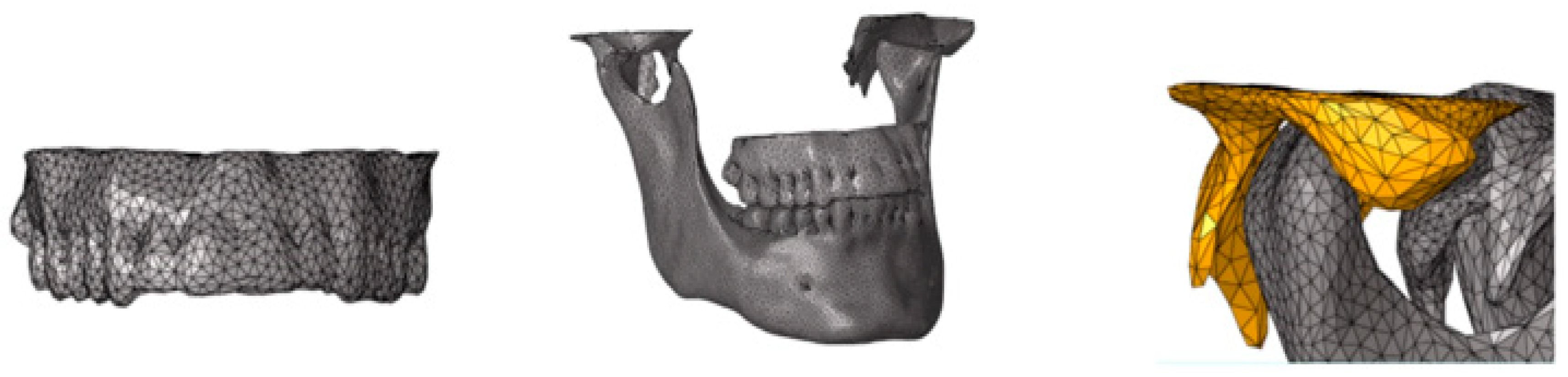
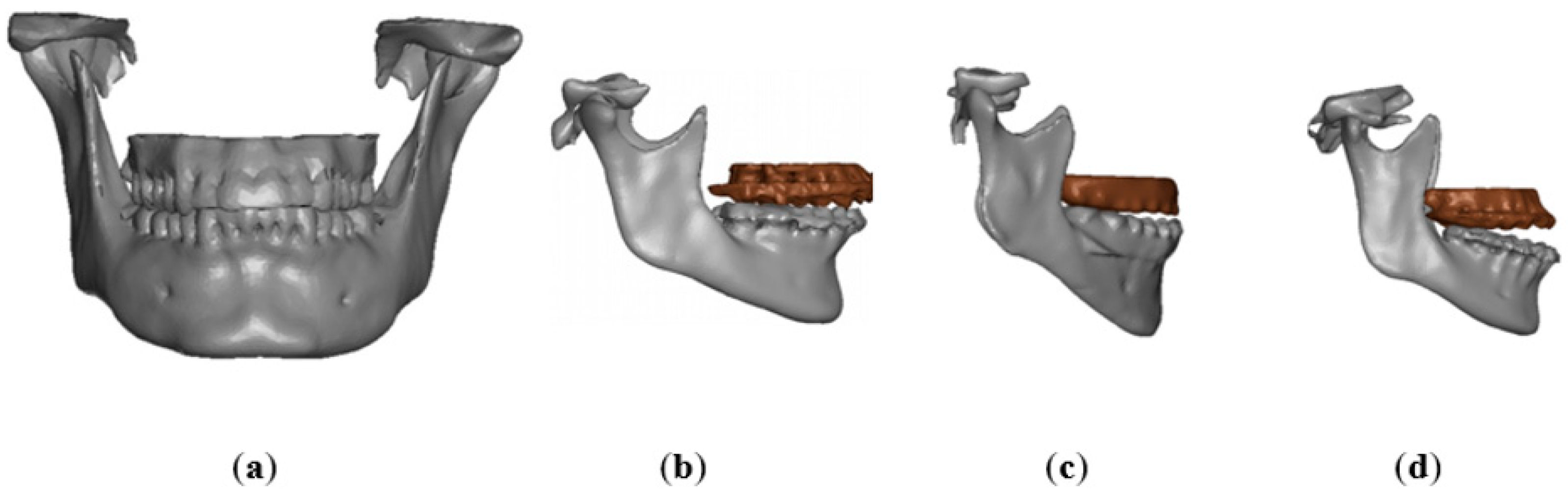
2.1. Finite Element Model
2.2. Virtual Simulation
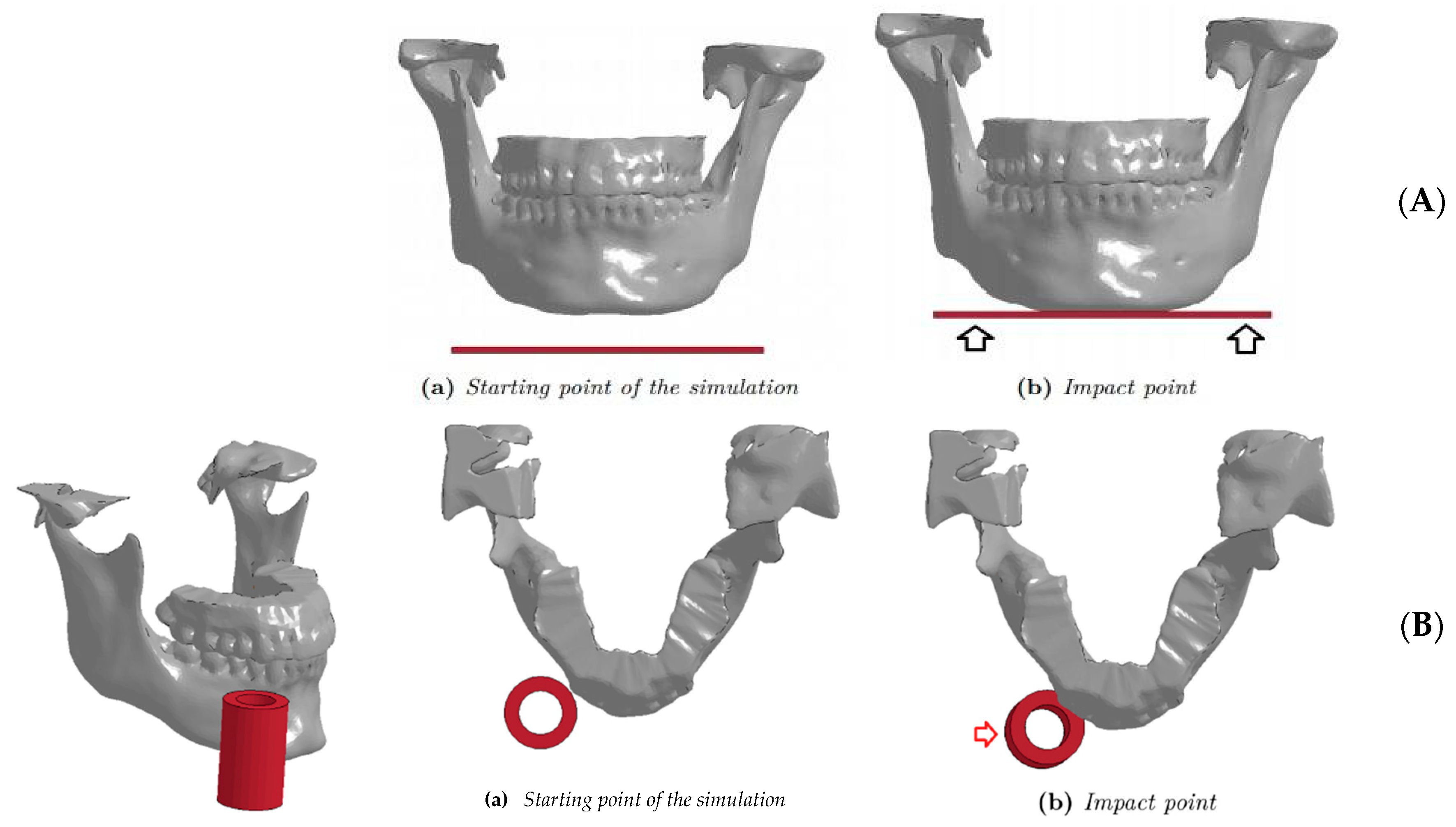
- The first (vertical) impact simulates a fall to the ground, with direct involvement of the submental region (Figure 4A). A surface was created to collide with the submental region with different speeds (1.5, 2.5, 3.5 and 4.5 m/s). A fall on the ground at 4 m/s is considered critical for the human head [21,22,23].
- 2.
- The second (lateral) impact applied to the parasymphyseal region (Figure 4B), simulating a punch or a similar mechanism of injury. A 20 × 40 × 5 mm3 cylindrical impacting object was chosen, made by a material that responded to ELASTIC laws with Young’s modulus to avoid deformations of the cylinder during the impact (20 GPa) (Table 1). It was decided to simulate an impact corresponding to 2 m/s and 5 m/s, as these values in the literature correlated to loss of consciousness [21,22,23,24,25,26,27,28,29].
2.3. Clinical Sample
2.4. Statistical Analysis on Clinical Sample
3. Results
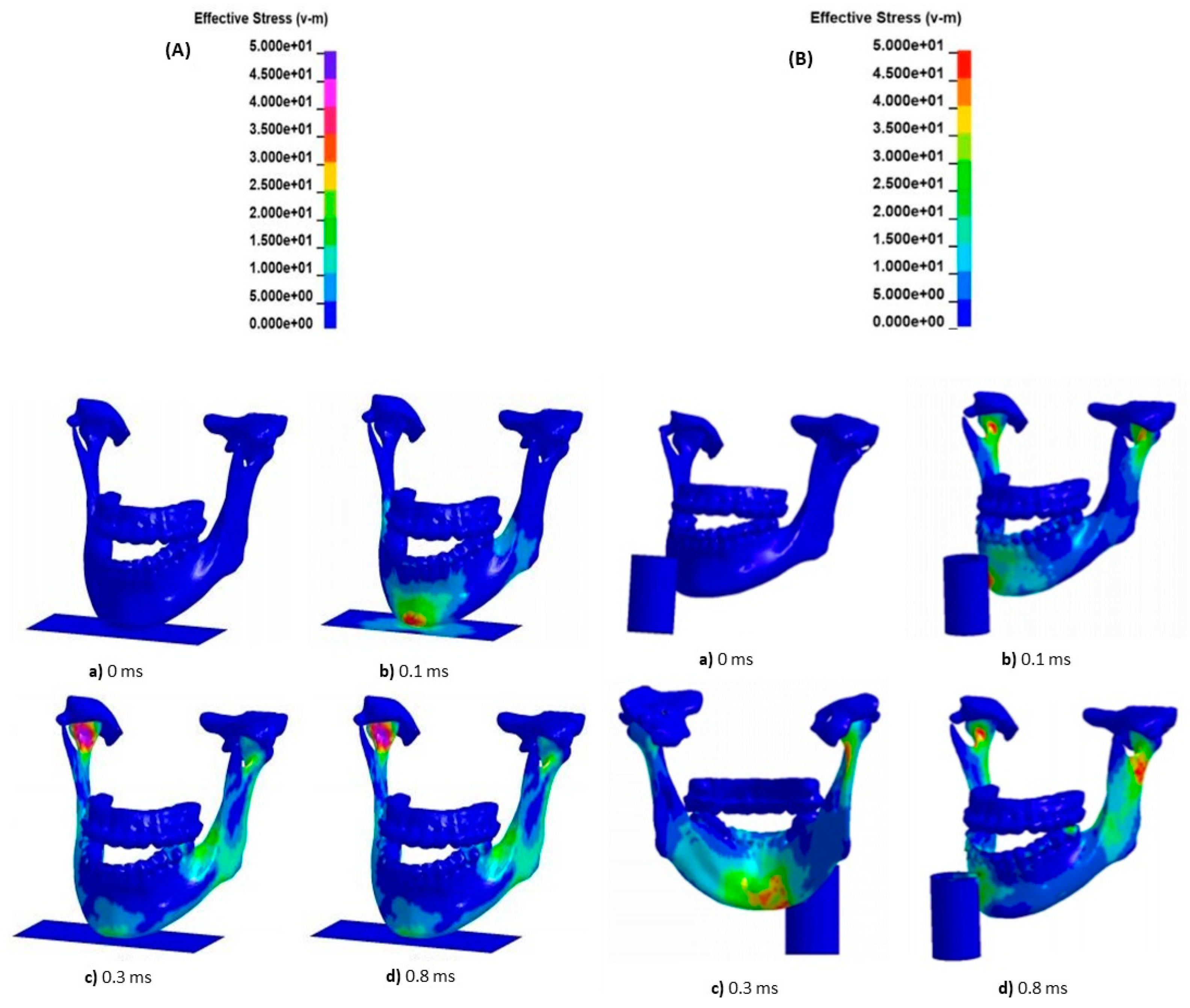
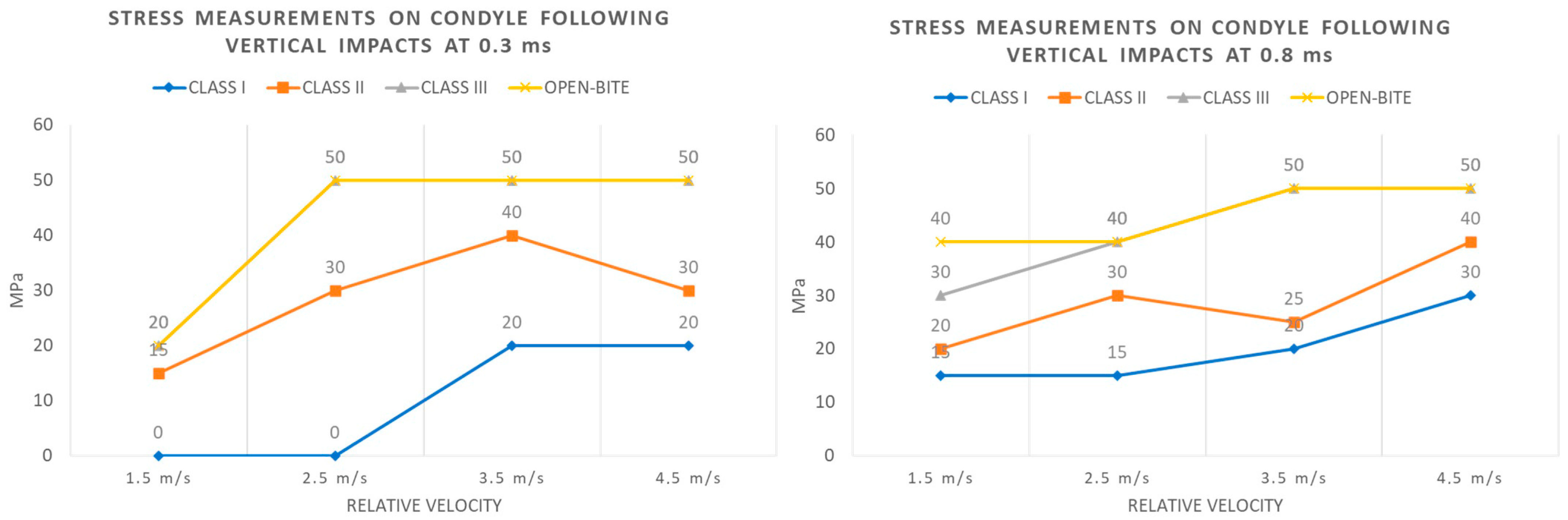
3.1. Vertical Impact on FEM Model
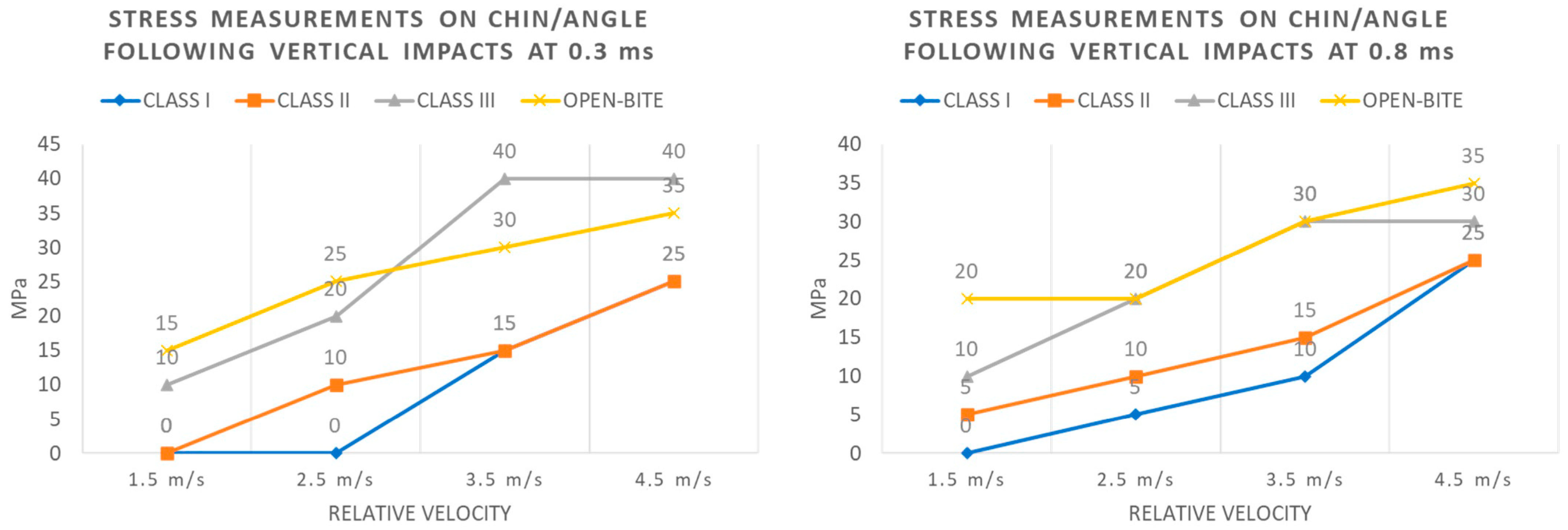
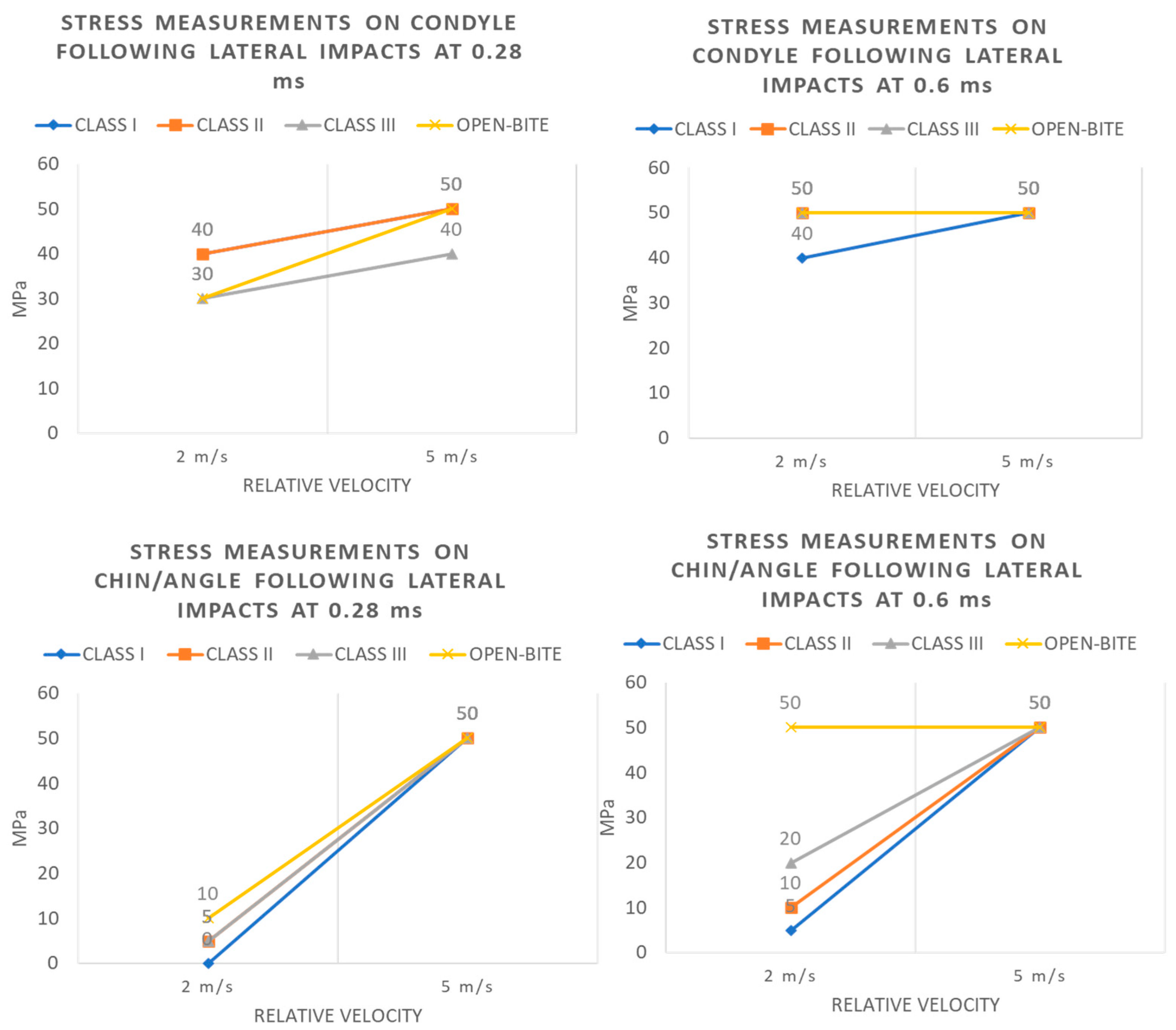
3.2. Lateral Impact on FEM Model (Table 3)
3.3. Comparative Analysis of the Sample
3.4. Quantitative Analysis by Comprehensive Facial Injury (CFI) Score of Mandibular Fractures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wusiman, P.; Maimaitituerxun, B.; Guli Saimaiti, A.; Moming, A. Epidemiology and Pattern of Oral and Maxillofacial Trauma. J. Craniofacial Surg. 2020, 31, e517–e520. [Google Scholar] [CrossRef]
- Granieri, S.S.; Reitano, E.E.; Bindi, F.F.; Renzi, F.F.; Sammartano, F.F.; Cimbanassi, S.S.; Gupta, S.S.; Chiara, O.O. Motorcycle-related trauma:effects of age and site of injuries on mortality. A single-center, retrospective study. World J. Emerg. Surg. 2020, 15, 18. [Google Scholar] [CrossRef]
- McCarty, J.C.; Herrera-Escobar, J.P.; Gadkaree, S.K.; El Moheb, M.; Kaafarani, H.M.A.; Velmahos, G.; Salim, A.; Nehra, D.; Caterson, E.J. Long-Term Functional Outcomes of Trauma Patients with Facial Injuries. J. Craniofacial Surg. 2021, 32, 2584–2587. [Google Scholar] [CrossRef]
- Canzi, G.; De Ponti, E.; Filippi, A.; Bozzetti, A.; Sozzi, D.; Novelli, G. The burden of facial trauma on mortality in patients with multiple injuries: A single-center analysis of 1862 motorcycle accidents. J. Cranio-Maxillofac. Surg. 2022, 50, 146–149. [Google Scholar] [CrossRef]
- Verbruggen, K.; Halewyck, S. Long-term Complications after facial trauma: Literature review. B-ENT 2016, 26, 47–58. [Google Scholar]
- Morris, C.; Bebeau, N.P.; Brockhoff, H.; Tandon, R.; Tiwana, P. Mandibular fractures: An analysis of the epidemiology and patterns of injury in 4,143 fractures. J. Oral Maxillofac. Surg. 2015, 73, 951.e1–951.e12. [Google Scholar] [CrossRef] [PubMed]
- Saravanan, T.; Balaguhan, B.; Venkatesh, A.; Geethapriya, N.; Goldpearlinmary Karthick, A. Prevalence of mandibular fractures. Indian J. Dent. Res. 2020, 31, 971–974. [Google Scholar] [CrossRef]
- Gassner, R.; Tuli, T.; Hächl, O.; Rudisch, A.; Ulmer, H. Cranio-maxillofacial trauma: A 10-year review of 9,543 cases with 21,067 injuries. J. Cranio-Maxillofac. Surg. 2003, 31, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Nishimoto, R.N.; Dodson, T.B.; Lang, M.S. Is the Mandible Injury Severity Score a Valid Measure of Mandibular Injury Severity? J. Oral Maxillofac. Surg. 2019, 77, 1023–1030. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E., 3rd; Price, C. Treatment protocol for fractures of the atrophic mandible. J. Oral Maxillofac. Surg. 2008, 66, 421–435. [Google Scholar] [CrossRef]
- Beret, M.; Nicot, R.; Roland-Billecart, T.; Ramdane, N.; Ferri, J.; Schlund, M. Impacted lower third molar relationship with mandibular angle fracture complications. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, 149–154. [Google Scholar] [CrossRef]
- Ribeiro, P.D., Jr.; Senko, R.A.; Momesso, N.R.; Izidoro, J.H.; Padovan, L.E.M.; Viswanath, A. Occlusal Instability Results in Increased Complication Rates After Treatment of Mandibular Fractures. J. Oral Maxillofac. Surg. 2020, 78, 1163.e1–1163.e7. [Google Scholar] [CrossRef]
- Karagah, A.; Tabrizi, R.; Pourahmadali, F.; Alizadeh, A.; Tofangchiha, M.; Patini, R. Correlation of radiomorphometric indices of the mandible and mandibular angle fractures. Heliyon 2022, 8, e10549. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, P.; Bera, R.N.; Chauhan, N. Magnitude of Gonial Angle Influence on the Commonness of Mandibular Angle Fractures. Ann. Maxillofac. Surg. 2020, 10, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Samieirad, S.; Eshghpour, M.; Dashti, R.; Tohidi, E.; Javan, A.R.; Mianbandi, V. Correlation Between Lower Third Molar Impaction Types and Mandibular Angle and Condylar Fractures: A Retrospective Study. J. Oral Maxillofac. Surg. 2019, 77, 556–564. [Google Scholar] [CrossRef]
- Strait, D.S.; Wang, Q.; Dechow, P.C.; Ross, C.F.; Richmond, B.G.; Spencer, M.A.; Patel, B.A. Modeling elastic properties in finite-element analysis: How much precision is needed to produce an accurate model? Anat. Rec. A Discov. Mol. Cell Evol. Biol. 2005, 283, 275–287. [Google Scholar] [CrossRef]
- Canzi, G.; De Ponti, E.; Novelli, G.; Mazzoleni, F.; Chiara, O.; Bozzetti, A.; Sozzi, D. The CFI score: Validation of a new comprehensive severity scoring system for facial injuries. J. Cranio-Maxillofac. Surg. 2019, 47, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Canzi, G.; De Ponti, E.; Fossati, C.; Novelli, G.; Cimbanassi, S.; Bozzetti, A.; Sozzi, D. Understanding the relevance of comprehensive facial injury (CFI) score: Statistical analysis of overall surgical time and length of stay outcomes. J. Cranio-Maxillofac. Surg. 2019, 47, 1456–1463. [Google Scholar] [CrossRef]
- Canzi, G.; Aseni, P.; De Ponti, E.; Cimbanassi, S.; Sammartano, F.; Novelli, G.; Sozzi, D. The Comprehensive Facial Injury (CFI) Score Is an Early Predictor of the Management for Mild, Moderate and Severe Facial Trauma. J. Clin. Med. 2022, 11, 3281. [Google Scholar] [CrossRef]
- Vincent, A.G.; Ducic, Y.; Kellman, R. Fractures of the Mandibular Condyle. Facial Plast. Surg. 2019, 35, 623–626. [Google Scholar] [CrossRef]
- Singh, A.; Ganpule, S.G.; Khan, M.K.; Iqbal, M.A. Measurement of brain simulant strains in head surrogate under impact loading. Biomech. Model. Mechanobiol. 2021, 20, 2319–2334. [Google Scholar] [CrossRef]
- Allison, M.A.; Kang, Y.S.; Bolte, J.H., 4th; Maltese, M.R.; Arbogast, K.B. Validation of a helmet-based system to measure head impact biomechanics in ice hockey. Med. Sci. Sports Exerc. 2014, 46, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Iwamoto, M.; Nakahira, Y. Development and Validation of the Total Human Model for Safety (THUMS) Version 5 Containing Multiple 1D Muscles for Estimating Occupant Motions with Muscle Activation During Side Impacts. Stapp Car Crash J. 2015, 59, 53–90. [Google Scholar] [CrossRef]
- Kuhn, F.; Clausing, R.J.; Stiller, A.; Fonseca Ulloa, C.A.; Foelsch, C.; Rickert, M.; Jahnke, A. Determination of E-modulus of cancellous bone derived from human humeri and validation of plotted single trabeculae: Development of a standardized humerus bone model. J. Orthop. 2022, 33, 48–54. [Google Scholar] [CrossRef]
- Huempfner-Hierl, H.; Schaller, A.; Hierl, T. Maxillofacial fractures and craniocerebral injuries—Stress propagation from face to neurocranium in a finite element analysis. Scand. J. Trauma Resusc. Emerg. Med. 2015, 23, 35. [Google Scholar] [CrossRef][Green Version]
- Stojsih, S.; Boitano, M.; Wilhelm, M.; Bir, C. A prospective study of punch biomechanics and cognitive function for amateur boxers. Br. J. Sports Med. 2010, 44, 725–730. [Google Scholar] [CrossRef]
- Yamamoto, K.; Matsusue, Y.; Horita, S.; Murakami, K.; Sugiura, T.; Kirita, T. Maxillofacial Fractures Associated with Interpersonal Violence. J. Craniofacial Surg. 2019, 30, e312–e315. [Google Scholar] [CrossRef] [PubMed]
- Rees, C.D.; Spiller, P.; Blancher, A.; Moore-Medlin, T.; Bundrick, P.; Hamiter, M.; Samra, N.; Nathan, C.O. Assessment of Facial Injury by “Slock” in Incarcerated Patients. J. Correct. Health Care 2022, 28, 345–348. [Google Scholar] [CrossRef]
- Cournoyer, J.; Hoshizaki, T.B. Head dynamic response and brain tissue deformation for boxing punches with and without loss of consciousness. Clin. Biomech. 2019, 67, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Gibstein, A.R.; Chen, K.; Nakfoor, B.; Gargano, F.; Bradley, J.P. Mandibular Subcondylar Fracture: Improved Functional Outcomes in Selected Patients with Open Treatment. Plast. Reconstr. Surg. 2021, 148, 398e–406e. [Google Scholar] [CrossRef]
- Rikhotso, R.E.; Reyneke, J.P.; Nel, M. Does Open Reduction and Internal Fixation Yield Better Outcomes Over Closed Reduction of Mandibular Condylar Fractures? J. Oral Maxillofac. Surg. 2022, 80, 1641–1654. [Google Scholar] [CrossRef]
- Nys, M.; Van Cleemput, T.; Dormaar, J.T.; Politis, C. Long-term Complications of Isolated and Combined Condylar Fractures: A Retrospective Study. Craniomaxillofacial Trauma Reconstr. 2022, 15, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Mohanty, S.; Chaudhary, Z.; Sharma, P.; Kumar, J.; Verma, A. Does Mandibular Condylar Morphology After Fracture Healing Predict Functional Outcomes in Patients Treated with Closed Reduction? J. Oral Maxillofac. Surg. 2022, 80, 691–699. [Google Scholar] [CrossRef] [PubMed]
- Rajan, R.; Verma, D.K.; Borle, R.M.; Yadav, A. Relationship between fracture of mandibular condyle and absence of unerupted mandibular third molar-a retrospective study. Oral Maxillofac. Surg. 2016, 20, 191–194. [Google Scholar] [CrossRef] [PubMed]
- Venkatachalam, V.; Pandiarajan, R. Does the Impacted Mandibular Third Molar Increase the Risk of Angle Fracture to Prevent the Incidence of Condylar Fracture?—A Retrospective Analysis. Ann. Maxillofac. Surg. 2022, 12, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Revanth Kumar, S.; Sinha, R.; Uppada, U.K.; Ramakrishna Reddy, B.V.; Paul, D. Mandibular Third Molar Position Influencing the Condylar and Angular Fracture Patterns. J. Maxillofac. Oral Surg. 2015, 14, 956–961. [Google Scholar] [CrossRef]
- Bottlang, M.; DiGiacomo, G.; Tsai, S.; Madey, S. Effect of helmet design on impact performance of industrial safety helmets. Heliyon 2022, 8, e09962. [Google Scholar] [CrossRef]
- Novelli, G.; Moretti, M.; De Ponti, E.; Bozzetti, A.; Sozzi, D.; Canzi, G. Analysis of Different Safety Devices in the Prevention of Motorcycle-Related Craniofacial Trauma—A Retrospective Study. Ann. Maxillofac. Surg. 2021, 11, 293–297. [Google Scholar] [CrossRef]
- Colangeli, W.; Cordaro, R.; Boschetti, C.E.; Apice, C.; Novembre, D.; Lo Faro, C.; Cristofaro, M.G. Protective Effects of Helmet Type on Facial Injuries. J. Craniofacial Surg. 2021, 32, 1591–1595. [Google Scholar] [CrossRef]
- Lucci, C.; Piantini, S.; Savino, G.; Pierini, M. Motorcycle helmet selection and usage for improved safety: A systematic review on the protective effects of helmet type and fastening. Traffic Inj. Prev. 2021, 22, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.C.; Rivara, F.P.; Thompson, R. Helmets for preventing head and facial injuries in bicyclists. Cochrane Database Syst. Rev. 2000, 1999, CD001855. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.K.; Kumar, V.; Ganguly, R.; Patel, J.; Daga, D. Helmet shielding effect in mandibular fractures during road traffic accident. Natl. J. Maxillofac. Surg. 2021, 12, 56–61. [Google Scholar] [CrossRef] [PubMed]


| Pressure (GPa) | Density (ton/mm3) | Poisson | Yield (MPa) | LS-DYNA Card | |
|---|---|---|---|---|---|
| Cortical | 13.7 | 1.7 × 10−9 | 0.3 | 50 | 024 PIECEWISE LINEAR PLASTICITY |
| Trabecular | 1.37 | 7.0 × 10−10 | 0.3 | 1.8 | 024 PIECEWISE LINEAR PLASTICITY |
| Plate (100 × 50 × 2 mm3) | 70 | 2.7 × 10−9 | 0.3 | - | 001 ELASTIC |
| Cylinder (20 × 40 × 5 mm3) | 20 | 2.7 × 10−9 | 0.3 | - | 001 ELASTIC |
| Dentoskeletal Morphology | Number and Percentage |
|---|---|
| Class I | 31 (13.9%) |
| Class II | 85 (38.1%) |
| Class III | 41 (18.4%) |
| Open Bite/Poor Occlusal Contact (POC) | 66 (29.6%) |
| 233 (100%) |
| Occlusion | 0.0 ms | 0.3 ms | 0.8 ms | 3.5 ms | ||||
|---|---|---|---|---|---|---|---|---|
| Condyle | Chin/Angle | Condyle | Chin/Angle | Condyle | Chin/Angle | Condyle | Chin/Angle | |
| Speed 1.5 m/s | ||||||||
| Class I | 0 MPa | 0 MPa | 0 MPa | 0 MPa | 15 MPa | 0 MPa | 10 MPa | 0 MPa |
| Class II | 0 MPa | 0 MPa | 15 MPa | 0 MPa | 20 MPa | 5 MPa | 5 MPa | 0 MPa |
| Class III | 0 MPa | 0 MPa | 20 MPa | 10 MPa | 30 MPa | 10 MPa | 10 MPa | 5 MPa |
| Open-Bite | 0 MPa | 0 MPa | 20 MPa | 15 MPa | 40 MPa | 20 MPa | 10 MPa | 10 MPa |
| Speed 2.5 m/s | ||||||||
| Class I | 0 MPa | 0 MPa | 0 MPa | 0 MPa | 15 MPa | 5 MPa | 15 MPa | 0 MPa |
| Class II | 0 MPa | 0 MPa | 30 MPa | 10 MPa | 30 MPa | 10 MPa | 10 MPa | 0 MPa |
| Class III | 0 MPa | 0 MPa | >50 MPa | 20 MPa | 40 MPa | 20 MPa | 20 MPa | 15 MPa |
| Open-Bite | 0 MPa | 0 MPa | >50 MPa | 25 MPa | 40 MPa | 20 MPa | 25 MPa | 15 MPa |
| Speed 3.5 m/s | ||||||||
| Class I | 0 MPa | 0 MPa | 20 MPa | <15 MPa | 20 MPa | 10 MPa | 10 MPa | 5 MPa |
| Class II | 0 MPa | 0 MPa | 40 MPa | 15 MPa | 25 MPa | 15MPa | 20 MPa | 10 MPa |
| Class III | 0 MPa | 0 MPa | >50 MPa | 40 MPa | >50 MPa | 30 MPa | 25 MPa | 20 MPa |
| Open-Bite | 0 MPa | 0 MPa | >50 MPa | 30 MPa | >50 MPa | 30 MPa | 30 MPa | 20 MPa |
| Speed 4.5 m/s | ||||||||
| Class I | 0 MPa | 0 MPa | 20 MPa | 25 MPa | 30 MPa | 25 MPa | 15 MPa | 25 MPa |
| Class II | 0 MPa | 0 MPa | 30 MPa | 25 MPa | 40 MPa | 25 MPa | 15 MPa | 25 MPa |
| Class III | 0 MPa | 0 MPa | >50 MPa | 40 MPa | >50 MPa | 30 MPa | 30 MPa | 25 MPa |
| Open-Bite | 0 MPa | 0 MPa | >50 MPa | 35 MPa | >50 MPa | 35 MPa | 30 MPa | 25 MPa |
| Occlusion | Time | |||||||
|---|---|---|---|---|---|---|---|---|
| 0.0 ms | 0.28 ms | 0.6 ms | 1.2 ms | |||||
| Speed 2 m/s | ||||||||
| Condyle | Chin/Angle | Condyle | Chin/Angle | Condyle | Chin/Angle | Condyle | Chin/Angle | |
| Class I | 0 MPa | 0 MPa | 40 MPa | 0 MPa | 50 MPa | 5 MPa | 50 MPa | 20 MPa |
| Class II | 0 MPa | 0 MPa | 40 MPa | 5 MPa | 50 MPa | 10 MPa | 50 MPa | 15 MPa |
| Class III | 0 MPa | 0 MPa | 30 MPa | 5 MPa | 50 MPa | 20 MPa | 50 MPa | 40 MPa |
| Open-Bite | 0 MPa | 0 MPa | 30 MPa | 10 MPa | 50 MPa | 20 MPa | 50 MPa | 30 MPa |
| Speed 5 m/s | ||||||||
| Class I | 0 MPa | 0 MPa | 50 MPa | 50 MPa | 50 MPa | |||
| Class II | 0 MPa | 0 MPa | 30 MPa | 50 MPa | 50 MPa | |||
| Class III | 0 MPa | 0 MPa | 40 MPa | 50 MPa | 50 MPa | |||
| Open-Bite | 0 MPa | 0 MPa | 50 MPa | 50 MPa | 50 MPa | |||
| Fracture type | |
| Non displaced | 85 (38.1%) |
| Displaced | 108 (48.4%) |
| Displaced/Non displaced | 30 (13.5%) |
| Numbers of Foci | |
| Unifocal | 102 (45.7%) |
| Bifocal | 89 (39.9%) |
| Trifocal | 32 (14.4%) |
| Cause | |
| Accidental Fall | 50 (22.4%) |
| Aggression | 56 (25.1%) |
| Syncope | 34 (15.3%) |
| Sportive Trauma | 31 (13.9%) |
| Traffic trauma (bike/car) | 37 (16.6%) |
| Bicycle | 15 (6.7%) |
| Total | 223 (100%) |
| Unifocal | Bifocal | Trifocal | |
|---|---|---|---|
| Class I | 16 (51.6%) | 13 (41.9%) | 2 (6.5%) |
| (15.7%) | (14.5%) | (6.2%) | |
| Class II | 33 (38.8%) | 36 (42.4%) | 16 (18.8%) |
| (32.4%) | (40.5%) | (50.0%) | |
| Class III | 17 (41.5%) | 16 (39.0%) | 8 (19.5%) |
| (16.6%) | (18.0%) | (25.0%) | |
| Open/POC | 36 (54.6%) | 24 (36.4%) | 6 (9.0%) |
| (35.3%) | (27.0%) | (18.8%) |
| Non Displaced | Non Displaced/Displaced | Displaced | |
|---|---|---|---|
| Class I | 22 (71.0%) | 4 (12.9%) | 5 (16.1%) |
| (25.9%) | (13.3%) | (4.6%) | |
| Class II | 33 (38.8%) | 12 (14.1%) | 40 (47.1%) |
| (38.8%) | (40.0%) | (37.0%) | |
| Class III | 12 (29.3%) | 9 (22.0%) | 20 (48.8%) |
| (14.1%) | (30.0%) | (18.5%) | |
| Open/POC | 18 (27.3%) | 5 (7.6%) | 43 (65.2%) |
| (21.2%) | (16.7%) | (39.8%) |
| Class I | Class II | Class III | Open Bite/POC | Total | |
|---|---|---|---|---|---|
| Unifocal Non-Displaced | 16 | 11 | 8 | 15 | 50 |
| 32.00% | 22.00% | 16.00% | 30.00% | 100.00% | |
| 51.61% | 12.94% | 19.51% | 22.73% | 22.42% | |
| Unifocal Displaced | 0 | 22 | 9 | 21 | 52 |
| 0.00% | 42.31% | 17.31% | 40.38% | 100.00% | |
| 0.00% | 25.88% | 21.95% | 31.82% | 23.32% | |
| Bifocal Non-Displaced | 5 | 18 | 4 | 3 | 30 |
| 16.67% | 60.00% | 13.33% | 10.00% | 100.00% | |
| 16.13% | 21.18% | 9.76% | 4.55% | 13.45% | |
| Bifocal Non-Displaced/Displaced | 4 | 6 | 4 | 4 | 18 |
| 22.22% | 33.33% | 22.22% | 22.22% | 100.00% | |
| 12.90% | 7.06% | 9.76% | 6.06% | 8.07% | |
| Bifocal Displaced | 4 | 12 | 8 | 17 | 41 |
| 9.76% | 29.27% | 19.51% | 41.46% | 100.00% | |
| 12.90% | 14.12% | 19.51% | 25.76% | 18.39% | |
| Trifocal Non-Displaced | 1 | 4 | 0 | 0 | 5 |
| 20.00% | 80.00% | 0.00% | 0.00% | 100% | |
| 3.23% | 4.71% | 0.00% | 0.00% | 2.24% | |
| Trifocal Non-Displaced/Displaced | 0 | 6 | 5 | 1 | 12 |
| 0.00% | 50.00% | 41.67% | 8.33% | 100.00% | |
| 0.00% | 7.06% | 12.20% | 1.52% | 5.38% | |
| Trifocal Displaced | 1 | 6 | 3 | 5 | 15 |
| 6.67% | 40.00% | 20.00% | 33.33% | 100.00% | |
| 3.23% | 7.06% | 7.32% | 7.58% | 6.73% | |
| Total | 31 | 85 | 41 | 66 | 223 |
| 13.90% | 38.12% | 18.39% | 29.60% | 100.00% | |
| 100.00% | 100.00% | 100.00% | 100.00% | 100.00% |
| CFI Score (Mean) | |
|---|---|
| Class I | 3.29 |
| Class II | 4.69 |
| Class III | 5.29 |
| Open Bite/Poc | 5.37 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Novelli, G.; Filippi, A.; Cartocci, A.; Mirabella, S.; Talarico, M.; De Ponti, E.; Meazzini, M.C.; Sozzi, D.; Canzi, G.; Anghileri, M. Correlation between Malocclusion and Mandibular Fractures: An Experimental Study Comparing Dynamic Finite Element Models and Clinical Case Studies. Bioengineering 2024, 11, 274. https://doi.org/10.3390/bioengineering11030274
Novelli G, Filippi A, Cartocci A, Mirabella S, Talarico M, De Ponti E, Meazzini MC, Sozzi D, Canzi G, Anghileri M. Correlation between Malocclusion and Mandibular Fractures: An Experimental Study Comparing Dynamic Finite Element Models and Clinical Case Studies. Bioengineering. 2024; 11(3):274. https://doi.org/10.3390/bioengineering11030274
Chicago/Turabian StyleNovelli, Giorgio, Andrea Filippi, Andrea Cartocci, Sergio Mirabella, Marco Talarico, Elena De Ponti, Maria Costanza Meazzini, Davide Sozzi, Gabriele Canzi, and Marco Anghileri. 2024. "Correlation between Malocclusion and Mandibular Fractures: An Experimental Study Comparing Dynamic Finite Element Models and Clinical Case Studies" Bioengineering 11, no. 3: 274. https://doi.org/10.3390/bioengineering11030274
APA StyleNovelli, G., Filippi, A., Cartocci, A., Mirabella, S., Talarico, M., De Ponti, E., Meazzini, M. C., Sozzi, D., Canzi, G., & Anghileri, M. (2024). Correlation between Malocclusion and Mandibular Fractures: An Experimental Study Comparing Dynamic Finite Element Models and Clinical Case Studies. Bioengineering, 11(3), 274. https://doi.org/10.3390/bioengineering11030274









