Overground Robotic Gait Trainer mTPAD Improves Gait Symmetry and Weight Bearing in Stroke Survivors
Abstract
1. Introduction
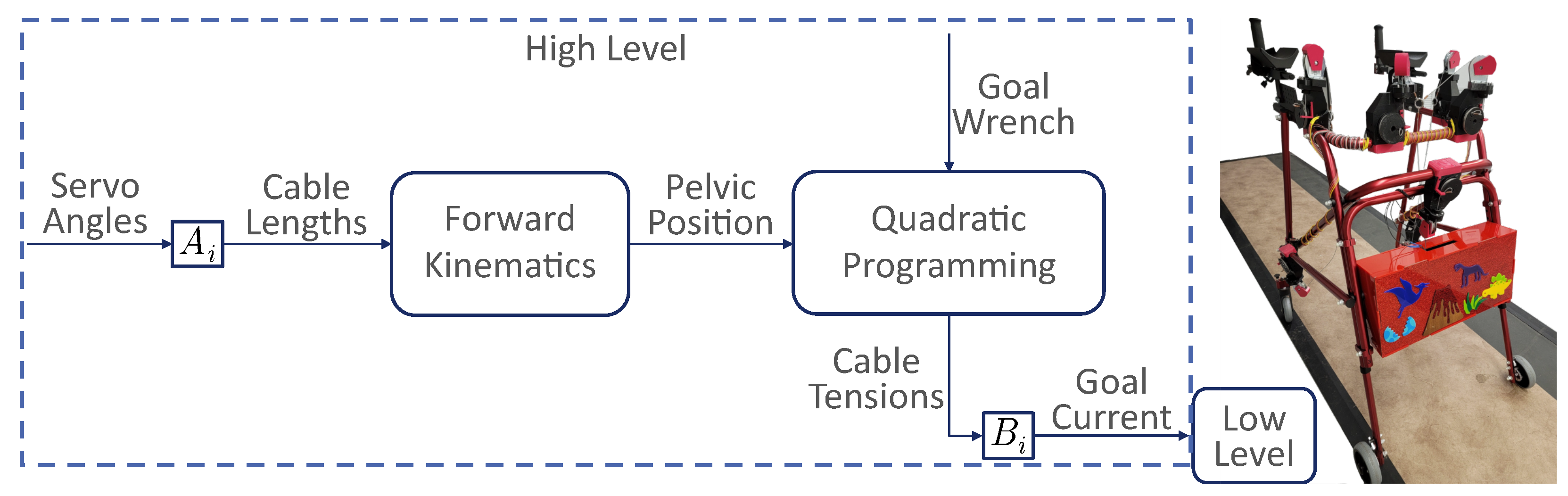
2. mTPAD Asymmetric Controller
2.1. mTPAD
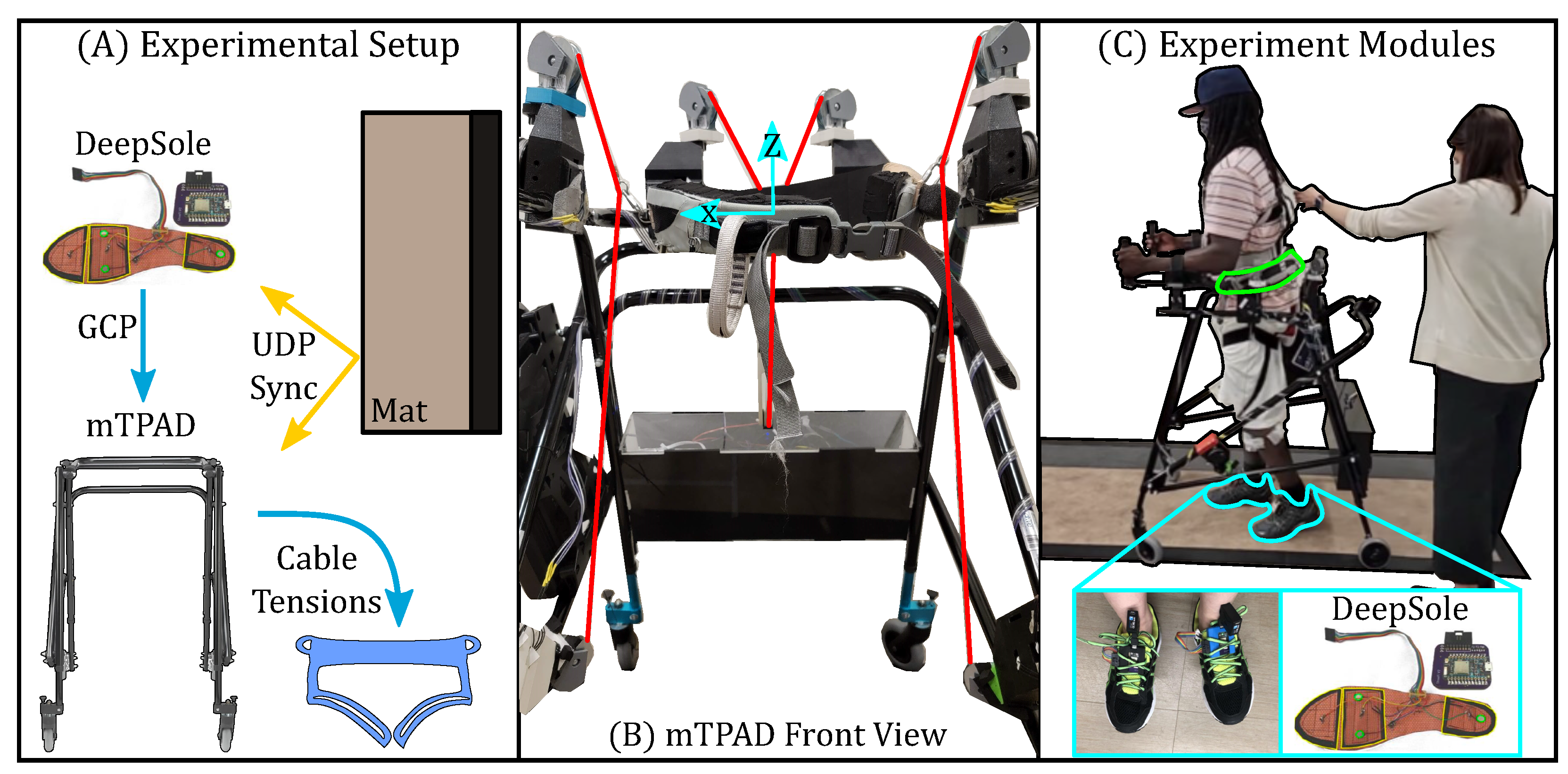
2.2. DeepSole System
2.3. Gait Phase Prediction
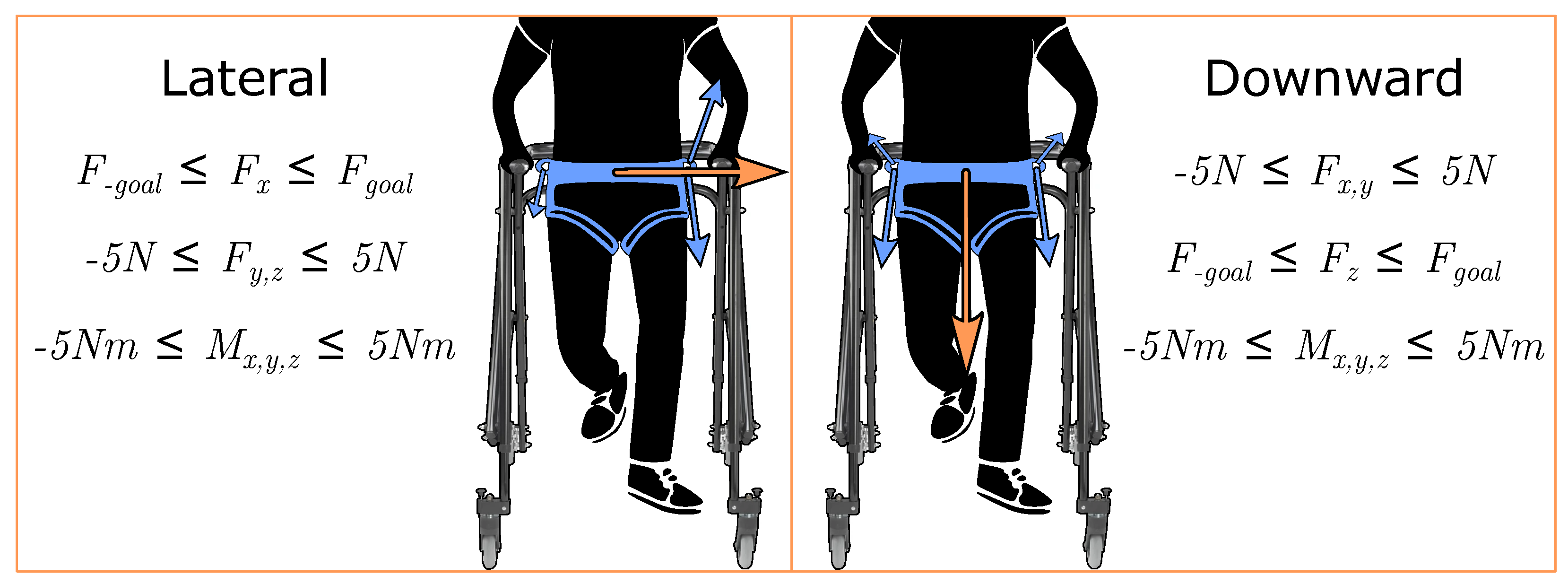
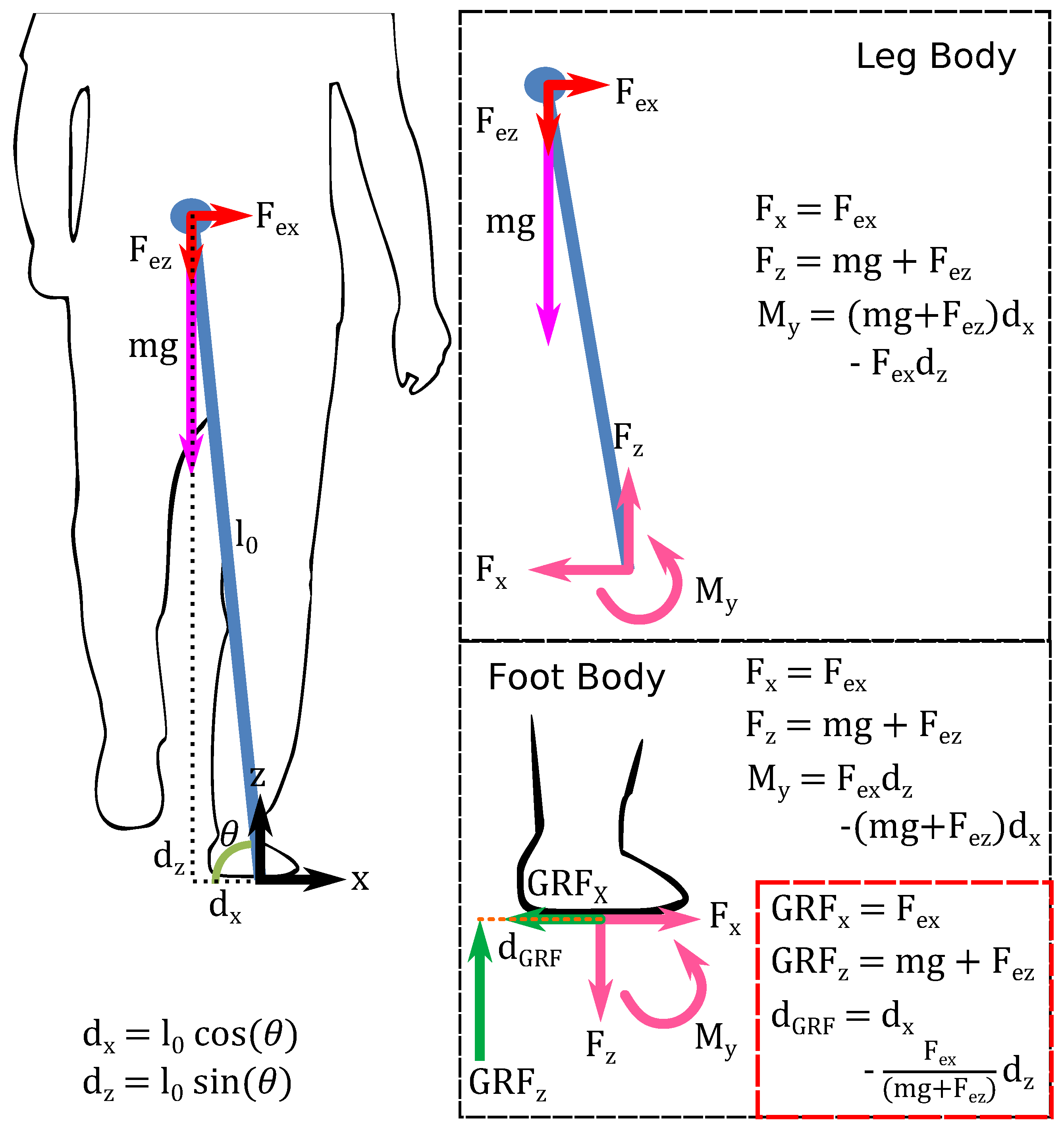
3. Frontal Plane Pelvic Forces Characterization
3.1. Experimental Setup
3.2. Protocol
3.3. Segmentation
3.4. Cyclogram and CISP
3.5. Foot Pressure
3.6. Statistical Analysis
4. Results
4.1. Frontal Plane Force Application
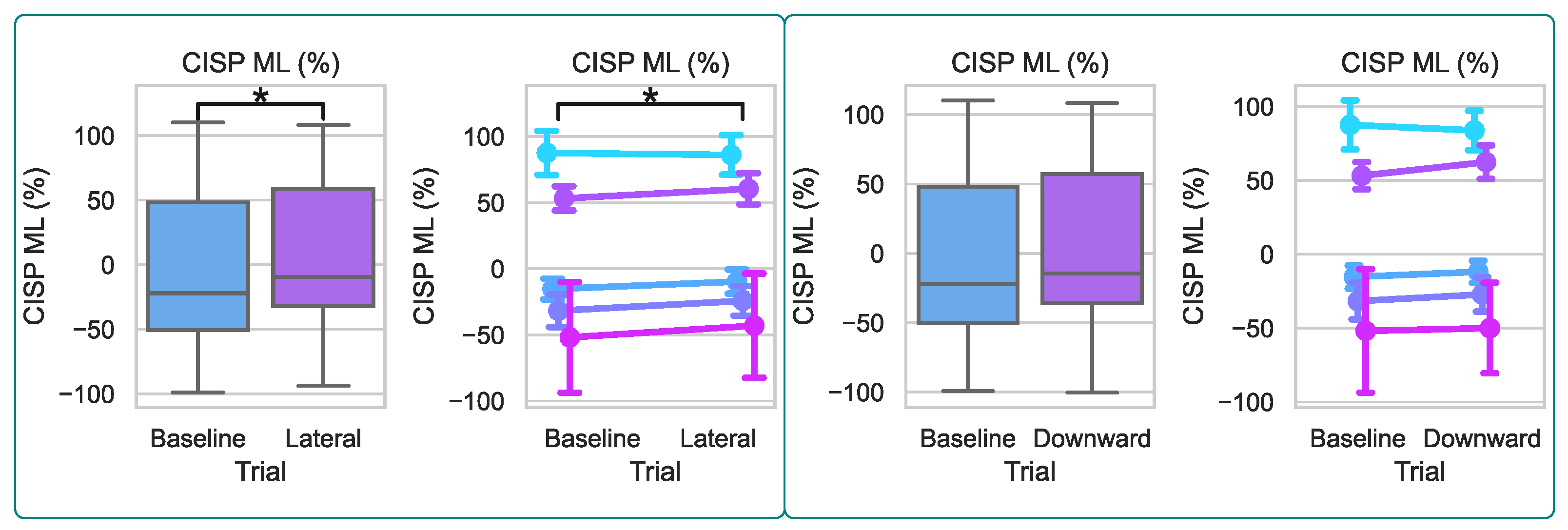
4.2. Cyclogram and CISP
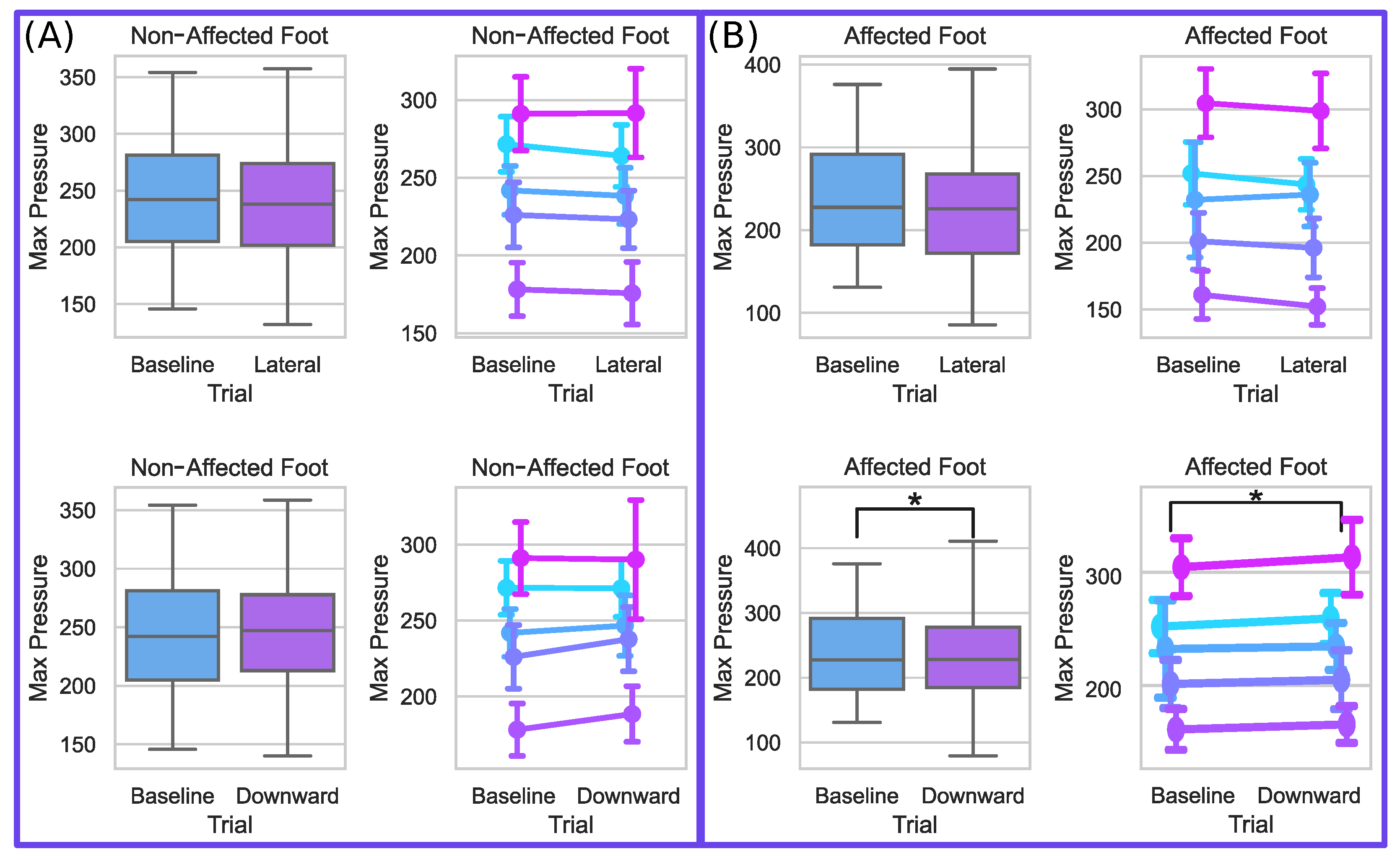
4.3. Foot Pressures
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| mTPAD | Mobile Tethered Pelvic Assist Device |
| GRF | Ground Reaction Force |
| COP | Center of Pressure |
| SS | Single Stance |
| FES | Functional Electrical Stimulation |
| 10MWT | 10-Meter Walk Test |
| DOF(s) | Degree(s) of Freedom |
| IMU | Inertial Measurement Unit |
| UDP | User Datagram Packet |
| RNN | Recurrent Neural Network |
| ERM | Encoder–Decoder RNN |
| ML | Mediolateral |
| AP | Anteroposterior |
| COM | Center of Mass |
| CISP | COP Intersection Point |
| TTL | Transistor–Transistor Logic |
| IRB | International Review Board |
| SW | Step Width |
| Af | Affected |
| Naf | Non-Affected |
| B | Baseline |
| L | Lateral |
| D | Downward |
| sEMG | Surface Electromyography |
| mTPAD | mobile Tethered Pelvic Assist Device |
| PKMAS | ProtoKinetics Movement Analysis Software |
| UDP | User Datagram Protocol |
| COP | Center of Pressure |
| SS | Single Stance |
| AP | Anterior–Posterior |
| CISP | Cyclogram Intersection Point |
| iEMG | Integrated Surface Electromyography |
| ML | Mediolateral |
| rmANOVA | Repeated Measures Analysis of Variance |
| BR | Brachioradialis |
| ND | Nondominant |
| D | Dominant |
| NF | No Force |
| F | Force |
References
- Kuriakose, D.; Xiao, Z. Pathophysiology and treatment of stroke: Present status and future perspectives. Int. J. Mol. Sci. 2020, 21, 7609. [Google Scholar] [CrossRef] [PubMed]
- Kelly-Hayes, M.; Beiser, A.; Kase, C.S.; Scaramucci, A.; D’Agostino, R.B.; Wolf, P.A. The influence of gender and age on disability following ischemic stroke: The Framingham study. J. Stroke Cerebrovasc. Dis. 2003, 12, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Arene, N.; Hidler, J. Understanding motor impairment in the paretic lower limb after a stroke: A review of the literature. Top. Stroke Rehabil. 2009, 16, 346–356. [Google Scholar] [CrossRef] [PubMed]
- Gray, V.; Rice, C.L.; Garland, S.J. Factors that influence muscle weakness following stroke and their clinical implications: A critical review. Physiother. Can. 2012, 64, 415–426. [Google Scholar] [CrossRef]
- Den Otter, A.; Geurts, A.; Mulder, T.; Duysens, J. Abnormalities in the temporal patterning of lower extremity muscle activity in hemiparetic gait. Gait Posture 2007, 25, 342–352. [Google Scholar] [CrossRef]
- Winter, D.A. Kinematic and kinetic patterns in human gait: Variability and compensating effects. Hum. Mov. Sci. 1984, 3, 51–76. [Google Scholar] [CrossRef]
- Lee, D.H.; Chang, W.N.; Jeon, H.J. Comparison of ground reaction force during gait between the nonparetic side in hemiparetic patients and the dominant side in healthy subjects. J. Exerc. Rehabil. 2020, 16, 344. [Google Scholar] [CrossRef]
- Bowden, M.G.; Balasubramanian, C.K.; Neptune, R.R.; Kautz, S.A. Anterior-posterior ground reaction forces as a measure of paretic leg contribution in hemiparetic walking. Stroke 2006, 37, 872–876. [Google Scholar] [CrossRef]
- Hsiao, H.; Gray, V.L.; Creath, R.A.; Binder-Macleod, S.A.; Rogers, M.W. Control of lateral weight transfer is associated with walking speed in individuals post-stroke. J. Biomech. 2017, 60, 72–78. [Google Scholar] [CrossRef]
- Roelker, S.A.; Bowden, M.G.; Kautz, S.A.; Neptune, R.R. Paretic propulsion as a measure of walking performance and functional motor recovery post-stroke: A review. Gait Posture 2019, 68, 6–14. [Google Scholar] [CrossRef]
- Boehm, W.L.; Gruben, K.G. Post-stroke walking behaviors consistent with altered ground reaction force direction control advise new approaches to research and therapy. Transl. Stroke Res. 2016, 7, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Lugade, V.; Kaufman, K. Center of pressure trajectory during gait: A comparison of four foot positions. Gait Posture 2014, 40, 719–722. [Google Scholar] [CrossRef] [PubMed]
- Nolan, K.J.; Yarossi, M.; Mclaughlin, P. Changes in center of pressure displacement with the use of a foot drop stimulator in individuals with stroke. Clin. Biomech. 2015, 30, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.; Kim, W.S. Anterior-posterior displacement of center of pressure measured by insole foot pressure measurement system in subacute recovery stage of post-stroke hemiplegia. Technol. Health Care 2018, 26, 649–657. [Google Scholar] [CrossRef]
- Chisholm, A.E.; Perry, S.D.; McIlroy, W.E. Inter-limb centre of pressure symmetry during gait among stroke survivors. Gait Posture 2011, 33, 238–243. [Google Scholar] [CrossRef]
- Wong, A.M.; Pei, Y.C.; Hong, W.H.; Chung, C.Y.; Lau, Y.C.; Chen, C.P. Foot contact pattern analysis in hemiplegic stroke patients: An implication for neurologic status determination. Arch. Phys. Med. Rehabil. 2004, 85, 1625–1630. [Google Scholar] [CrossRef]
- Roerdink, M.; De Haart, M.; Daffertshofer, A.; Donker, S.F.; Geurts, A.; Beek, P. Dynamical structure of center-of-pressure trajectories in patients recovering from stroke. Exp. Brain Res. 2006, 174, 256–269. [Google Scholar] [CrossRef] [PubMed]
- Treger, I.; Mizrachi, N.; Melzer, I. Open-loop and closed-loop control of posture: Stabilogram-diffusion analysis of center-of-pressure trajectories among people with stroke. J. Clin. Neurosci. 2020, 78, 313–316. [Google Scholar] [CrossRef]
- Stinear, C.M.; Lang, C.E.; Zeiler, S.; Byblow, W.D. Advances and challenges in stroke rehabilitation. Lancet Neurol. 2020, 19, 348–360. [Google Scholar] [CrossRef]
- Ribeiro, T.S.; Regalado, I.C.R.; da Silva, S.T.; de Oliveira Sousa, C.; de Figueiredo, K.M.O.B.; Lindquist, A.R.R. Effects of Load Addition During Gait Training on Weight-Bearing and Temporal Asymmetry After Stroke: A Randomized Clinical Trial. Am. J. Phys. Med. Rehabil. 2020, 99, 250–256. [Google Scholar] [CrossRef]
- Cha, Y.J.; Kim, J.D.; Choi, Y.R.; Kim, N.H.; Son, S.M. Effects of gait training with auditory feedback on walking and balancing ability in adults after hemiplegic stroke: A preliminary, randomized, controlled study. Int. J. Rehabil. Res. 2018, 41, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Gelaw, A.Y.; Janakiraman, B.; Teshome, A.; Ravichandran, H. Effectiveness of treadmill assisted gait training in stroke survivors: A systematic review and meta-analysis. Glob. Epidemiol. 2019, 1, 100012. [Google Scholar] [CrossRef]
- Mehrholz, J.; Thomas, S.; Elsner, B. Treadmill training and body weight support for walking after stroke. Cochrane Database Syst. Rev. 2017, 8, CD002840. [Google Scholar] [CrossRef] [PubMed]
- Maranesi, E.; Riccardi, G.R.; Di Donna, V.; Di Rosa, M.; Fabbietti, P.; Luzi, R.; Pranno, L.; Lattanzio, F.; Bevilacqua, R. Effectiveness of intervention based on end-effector gait trainer in older patients with stroke: A systematic review. J. Am. Med. Dir. Assoc. 2020, 21, 1036–1044. [Google Scholar] [CrossRef]
- Manuli, A.; Maggio, M.G.; Latella, D.; Cannavò, A.; Balletta, T.; De Luca, R.; Naro, A.; Calabrò, R.S. Can robotic gait rehabilitation plus Virtual Reality affect cognitive and behavioural outcomes in patients with chronic stroke? A randomized controlled trial involving three different protocols. J. Stroke Cerebrovasc. Dis. 2020, 29, 104994. [Google Scholar] [CrossRef]
- Moucheboeuf, G.; Griffier, R.; Gasq, D.; Glize, B.; Bouyer, L.; Dehail, P.; Cassoudesalle, H. Effects of robotic gait training after stroke: A meta-analysis. Ann. Phys. Rehabil. Med. 2020, 63, 518–534. [Google Scholar] [CrossRef]
- Kim, H.; Park, G.; Shin, J.H.; You, J.H. Neuroplastic effects of end-effector robotic gait training for hemiparetic stroke: A randomised controlled trial. Sci. Rep. 2020, 10, 12461. [Google Scholar] [CrossRef]
- Choi, W. Effects of robot-assisted gait training with body weight support on gait and balance in stroke patients. Int. J. Environ. Res. Public Health 2022, 19, 5814. [Google Scholar] [CrossRef]
- Bruni, M.F.; Melegari, C.; De Cola, M.C.; Bramanti, A.; Bramanti, P.; Calabrò, R.S. What does best evidence tell us about robotic gait rehabilitation in stroke patients: A systematic review and meta-analysis. J. Clin. Neurosci. 2018, 48, 11–17. [Google Scholar] [CrossRef]
- Tedla, J.S.; Dixit, S.; Gular, K.; Abohashrh, M. Robotic-assisted gait training effect on function and gait speed in subacute and chronic stroke population: A systematic review and meta-analysis of randomized controlled trials. Eur. Neurol. 2019, 81, 103–111. [Google Scholar] [CrossRef]
- Alingh, J.; Fleerkotte, B.; Groen, B.; Rietman, J.; Weerdesteyn, V.; van Asseldonk, E.; Geurts, A.; Buurke, J. Effect of assist-as-needed robotic gait training on the gait pattern post stroke: A randomized controlled trial. J. Neuroeng. Rehabil. 2021, 18, 26. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, J.; Truijen, S.; Van Criekinge, T.; Saeys, W. Feasibility and effectiveness of repetitive gait training early after stroke: A systematic review and meta-analysis. J. Rehabil. Med. 2019, 51, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Louie, D.R.; Eng, J.J. Powered robotic exoskeletons in post-stroke rehabilitation of gait: A scoping review. J. Neuroeng. Rehabil. 2016, 13, 53. [Google Scholar] [CrossRef] [PubMed]
- Degami, A.; Taki, S.; Imura, T.; Iwamoto, Y.; Imada, N.; Tanaka, R.; Urakawa, S.; Inagawa, T.; Araki, H.; Araki, O. Early Initiation of exoskeletal robotic gait training improves functional outcomes in the patients with stroke: A retrospective observational Study. Eur. Neurol. 2023, 86, 121–127. [Google Scholar] [CrossRef]
- Tanaka, H.; Nankaku, M.; Nishikawa, T.; Hosoe, T.; Yonezawa, H.; Mori, H.; Kikuchi, T.; Nishi, H.; Takagi, Y.; Miyamoto, S.; et al. Spatiotemporal gait characteristic changes with gait training using the hybrid assistive limb for chronic stroke patients. Gait Posture 2019, 71, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Bang, D.H.; Shin, W.S. Effects of robot-assisted gait training on spatiotemporal gait parameters and balance in patients with chronic stroke: A randomized controlled pilot trial. NeuroRehabilitation 2016, 38, 343–349. [Google Scholar] [CrossRef]
- Krishnan, C.; Ranganathan, R.; Kantak, S.S.; Dhaher, Y.Y.; Rymer, W.Z. Active robotic training improves locomotor function in a stroke survivor. J. Neuroeng. Rehabil. 2012, 9, 57. [Google Scholar] [CrossRef]
- Alingh, J.; Groen, B.; Kamphuis, J.; Geurts, A.; Weerdesteyn, V. Task-specific training for improving propulsion symmetry and gait speed in people in the chronic phase after stroke: A proof-of-concept study. J. Neuroeng. Rehabil. 2021, 18, 69. [Google Scholar] [CrossRef]
- Yeung, L.F.; Ockenfeld, C.; Pang, M.K.; Wai, H.W.; Soo, O.Y.; Li, S.W.; Tong, K.Y. Randomized controlled trial of robot-assisted gait training with dorsiflexion assistance on chronic stroke patients wearing ankle-foot-orthosis. J. Neuroeng. Rehabil. 2018, 15, 51. [Google Scholar] [CrossRef]
- Bishop, L.; Khan, M.; Martelli, D.; Quinn, L.; Stein, J.; Agrawal, S. Exploration of two training paradigms using forced induced weight shifting with the tethered pelvic assist device to reduce asymmetry in individuals after stroke. Am. J. Phys. Med. Rehabil. 2017, 96, S135–S140. [Google Scholar] [CrossRef]
- Bishop, L.; Omofuma, I.; Stein, J.; Agrawal, S.; Quinn, L. Treadmill-Based Locomotor Training With Robotic Pelvic Assist and Visual Feedback: A Feasibility Study. J. Neurol. Phys. Ther. 2020, 44, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Lorusso, M.; Tramontano, M.; Casciello, M.; Pece, A.; Smania, N.; Morone, G.; Tamburella, F. Efficacy of Overground Robotic Gait Training on Balance in Stroke Survivors: A Systematic Review and Meta-Analysis. Brain Sci. 2022, 12, 713. [Google Scholar] [CrossRef] [PubMed]
- Nedergård, H.; Arumugam, A.; Sandlund, M.; Bråndal, A.; Häger, C.K. Effect of robotic-assisted gait training on objective biomechanical measures of gait in persons post-stroke: A systematic review and meta-analysis. J. Neuroeng. Rehabil. 2021, 18, 64. [Google Scholar] [CrossRef] [PubMed]
- Stramel, D.M.; Agrawal, S.K. Validation of a forward kinematics based controller for a mobile tethered pelvic assist device to augment pelvic forces during walking. In Proceedings of the 2020 IEEE International Conference on Robotics and Automation (ICRA), Paris, France, 31 May–31 August 2020; pp. 10133–10139. [Google Scholar]
- Stramel, D.M.; Prado, A.; Roy, S.H.; Kim, H.; Agrawal, S.K. Effects of Timed Frontal Plane Pelvic Moments during Overground Walking with a Mobile TPAD System. IEEE Trans. Neural Syst. Rehabil. Eng. 2023, 31, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Prado, A.; Cao, X.; Ding, X.; Agrawal, S.K. Prediction of gait cycle percentage using instrumented shoes with artificial neural networks. In Proceedings of the 2020 IEEE International Conference on Robotics and Automation (ICRA), Paris, France, 31 May–31 August 2020; pp. 2834–2840. [Google Scholar]
- Viteckova, S.; Kutilek, P.; Svoboda, Z.; Krupicka, R.; Kauler, J.; Szabo, Z. Gait symmetry measures: A review of current and prospective methods. Biomed. Signal Process. Control 2018, 42, 89–100. [Google Scholar] [CrossRef]
- Lynall, R.C.; Zukowski, L.A.; Plummer, P.; Mihalik, J.P. Reliability and validity of the protokinetics movement analysis software in measuring center of pressure during walking. Gait Posture 2017, 52, 308–311. [Google Scholar] [CrossRef]
- Seabold, S.; Perktold, J. Statsmodels: Econometric and statistical modeling with python. In Proceedings of the 9th Python in Science Conference, Austin, TX, USA, 28 June–3 July 2010; Volume 57, pp. 10–25080. [Google Scholar]
- Stramel, D.M.; Agrawal, S.K. Assessing Changes in Human Gait with a Mobile Tethered Pelvic Assist Device (mTPAD) in Transparent Mode with Hand Holding Conditions. In Proceedings of the 2022 9th IEEE RAS/EMBS International Conference for Biomedical Robotics and Biomechatronics (BioRob), Seoul, Republic of Korea, 21–24 August 2022; pp. 1–6. [Google Scholar]




| Participant | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| BodyWeight (kg) | 79.4 | 76.2 | 68.0 | 52.2 | 94.3 |
| Lateral (BW%) | 4% | 10% | 6% | 8% | 8% |
| Lateral Force (N) | 31.1 | 74.7 | 40.0 | 40.9 | 74.0 |
| Downward (BW%) | 6% | 10% | 10% | 10% | 8% |
| Downward Force (N) | 46.7 | 74.7 | 66.7 | 51.2 | 74.0 |
| Participant | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Baseline (B) SW (cm) | 5.1 | 8.6 | 3.6 | 13.2 | 13.3 |
| Lateral (L) SW (cm) | 6.1 | 9.4 | 4.8 | 15.4 | 12.7 |
| Downward (D) SW (cm) | 4.9 | 9.0 | 5.8 | 14.2 | 11.9 |
| B Af SS COP Dist. (cm) | 1.8 | 7.4 | 6.4 | 5.2 | 1.8 |
| L Af SS COP Dist. (cm) | 1.7 | 8.3 | 7.1 | 4.5 | 1.8 |
| D Af SS COP Dist. (cm) | 1.8 | 8.6 | 6.7 | 4.1 | 2.6 |
| B Naf SS COP Dist. (cm) | 12.2 | 11.0 | 14.9 | 13.7 | 3.3 |
| L Naf SS COP Dist. (cm) | 11.8 | 10.9 | 14.1 | 13.1 | 4.1 |
| D Naf SS COP Dist. (cm) | 12.5 | 11.4 | 14.4 | 12.7 | 3.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stramel, D.M.; Winterbottom, L.; Stein, J.; Agrawal, S.K. Overground Robotic Gait Trainer mTPAD Improves Gait Symmetry and Weight Bearing in Stroke Survivors. Bioengineering 2023, 10, 698. https://doi.org/10.3390/bioengineering10060698
Stramel DM, Winterbottom L, Stein J, Agrawal SK. Overground Robotic Gait Trainer mTPAD Improves Gait Symmetry and Weight Bearing in Stroke Survivors. Bioengineering. 2023; 10(6):698. https://doi.org/10.3390/bioengineering10060698
Chicago/Turabian StyleStramel, Danielle Marie, Lauren Winterbottom, Joel Stein, and Sunil K. Agrawal. 2023. "Overground Robotic Gait Trainer mTPAD Improves Gait Symmetry and Weight Bearing in Stroke Survivors" Bioengineering 10, no. 6: 698. https://doi.org/10.3390/bioengineering10060698
APA StyleStramel, D. M., Winterbottom, L., Stein, J., & Agrawal, S. K. (2023). Overground Robotic Gait Trainer mTPAD Improves Gait Symmetry and Weight Bearing in Stroke Survivors. Bioengineering, 10(6), 698. https://doi.org/10.3390/bioengineering10060698







