Development of a Molecular-Subtype-Associated Immune Prognostic Signature That Can Be Recognized by MRI Radiomics Features in Bladder Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Evaluation of TIICs
2.3. RNA Expression Data-Based Molecular Subtyping
2.4. Molecular-Subtype-Associated IRGs
2.5. IPS Construction and Validation
2.6. Gene Set Enrichment Analysis (GSEA)
2.7. Nomogram Construction
2.8. MRI Protocal
2.9. Region of Interest (ROI) Segmentation and Feature Extraction
2.10. Feature Selection and Radiomics Signature Development
2.11. Statistical Analysis
3. Results
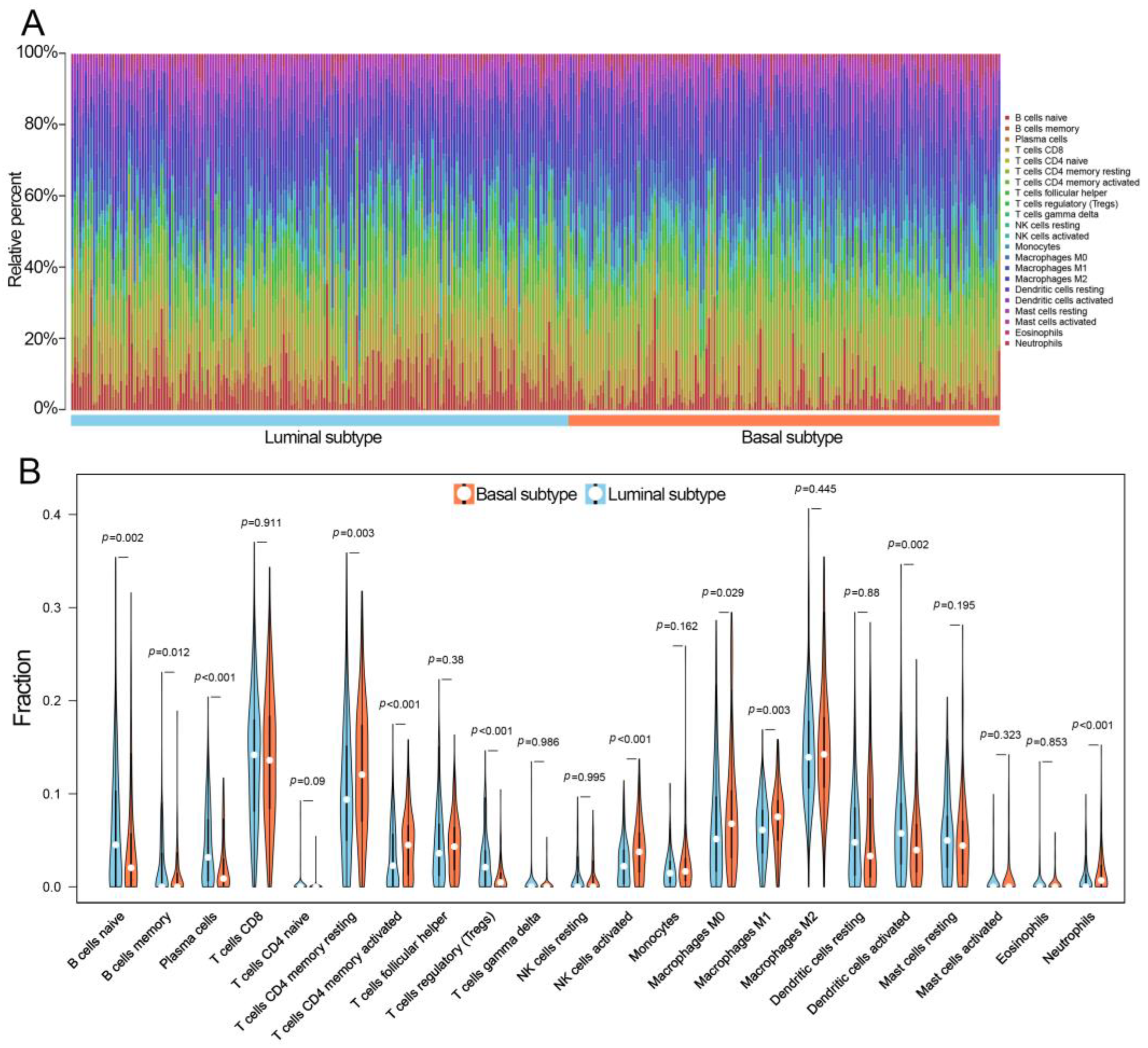
3.1. Comparison of TIICs between Luminal and Basal Subtypes
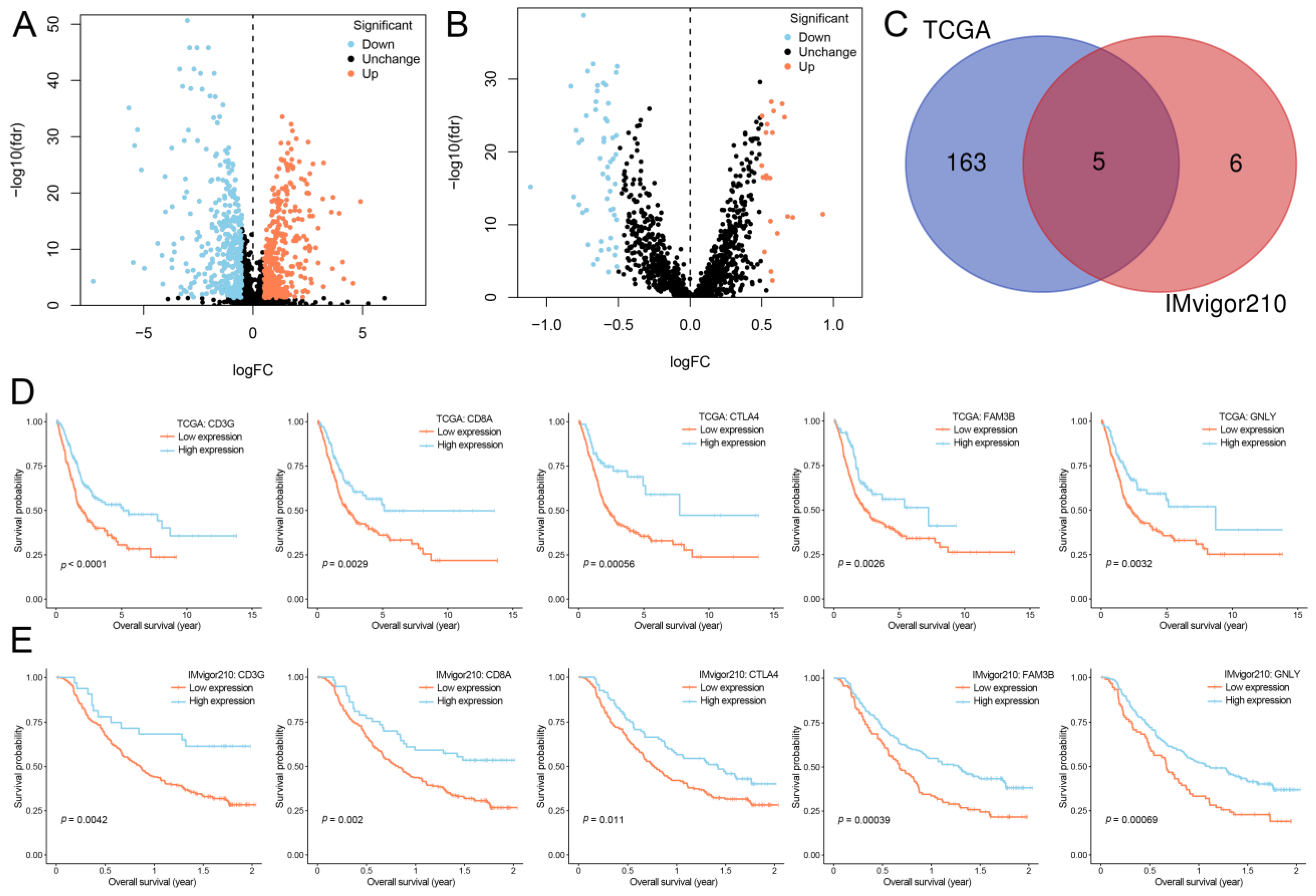
3.2. Selection of IRGs
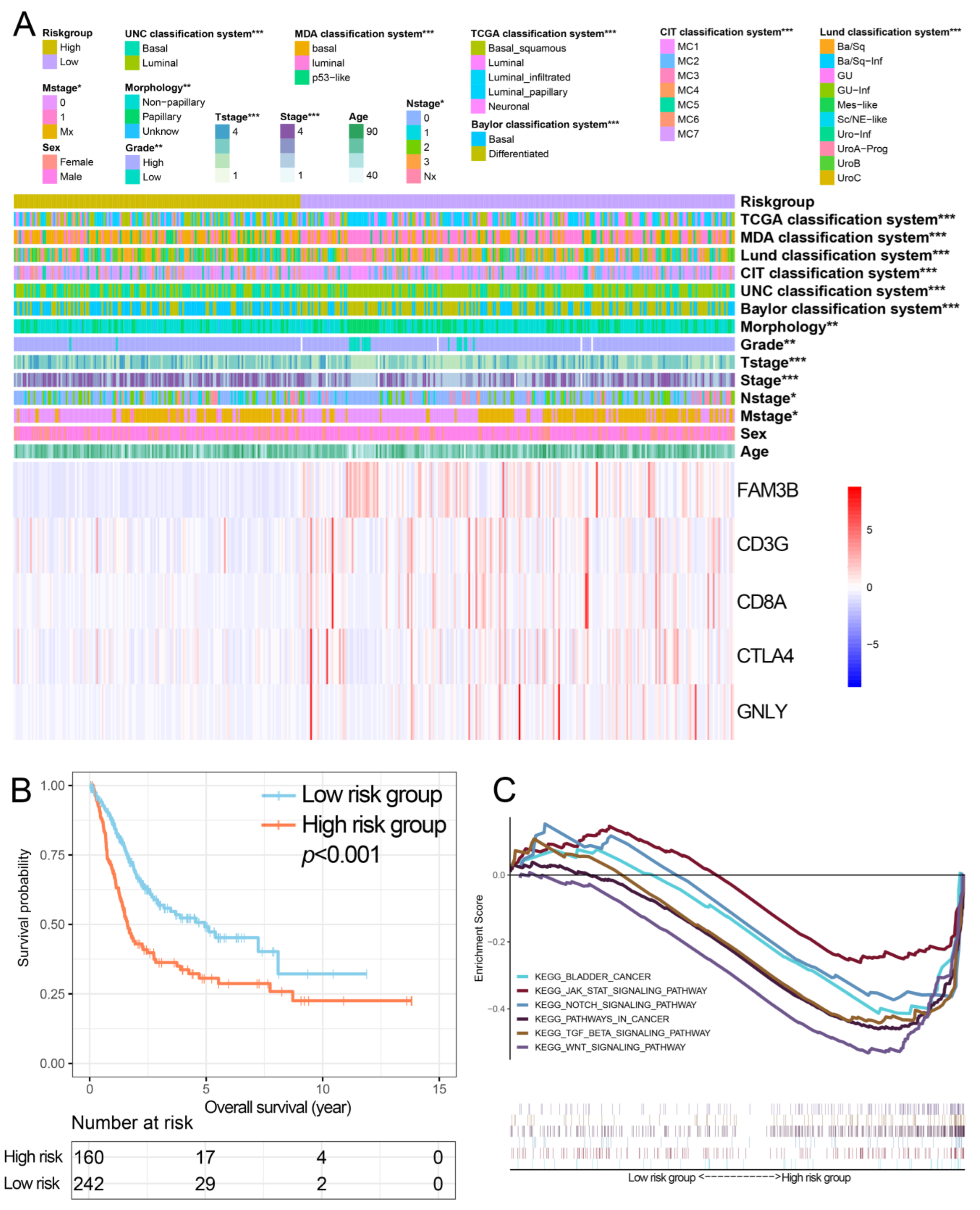
3.3. Construction and Performance of the IPS
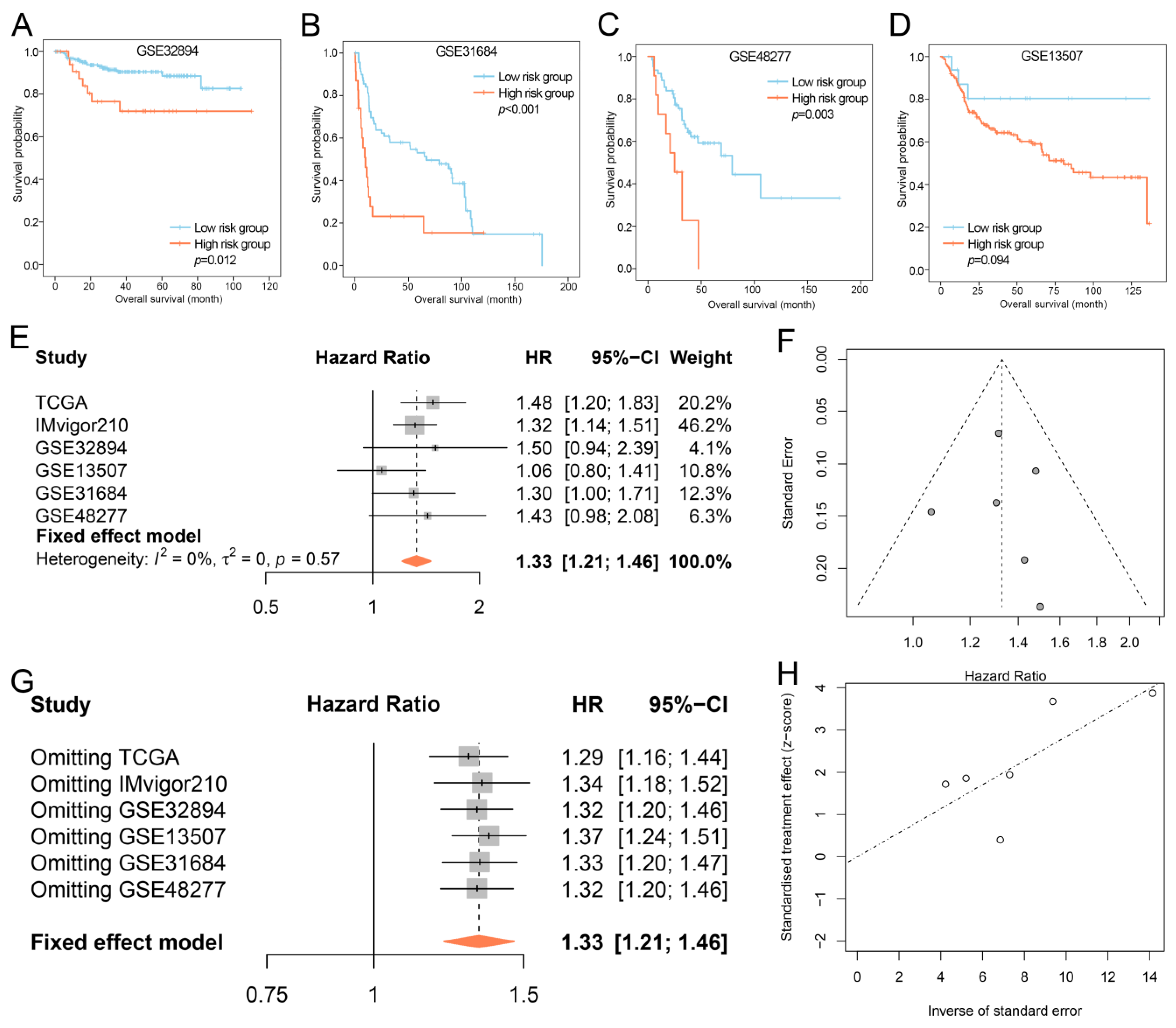
3.4. Validation of the IPS
3.5. Construction of Nomogram
3.6. Radiomics Signature Development and Performance Determination
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BLCA | Bladder cancer |
| TCGA | The Cancer Genome Atlas |
| TIIC | Tumor infiltrating immune cell |
| IPS | Immune prognostic signature |
| GSEA | Functional enrichment analysis |
| LASSO | Least absolute shrinkage and selection operator |
| AUC | Area under the curve |
| NMIBC | Non-muscle invasive bladder cancer |
| MIBC | Muscle-invasive bladder cancer |
| IRGs | Immune-related genes |
| OS | Overall survival |
| PR | Partial response |
| CR | Complete response |
| GEO | Gene Expression Omnibus |
| mRMR | Minimum redundancy maximum relevance |
| ICCs | Intra- and interclass correlation coefficients |
| PPV | Positive predictive value |
| NPV | Negative predictive value |
| CI | Confidence interval |
| MRI | Magnetic resonance imaging |
| DCE | Dynamic contrast-enhanced |
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Balar, A.V.; Galsky, M.D.; Rosenberg, J.E.; Powles, T.; Petrylak, D.P.; Bellmunt, J.; Loriot, Y.; Necchi, A.; Hoffman-Censits, J.; Perez-Gracia, J.L.; et al. Atezolizumab as first-line treatment in cisplatin-ineligible patients with locally advanced and metastatic urothelial carcinoma: A single-arm, multicentre, phase 2 trial. Lancet 2017, 389, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Mariathasan, S.; Turley, S.J.; Nickles, D.; Castiglioni, A.; Yuen, K.; Wang, Y.; Kadel, E.E., III; Koeppen, H.; Astarita, J.L.; Cubas, R.; et al. TGFβ attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature 2018, 554, 544–548. [Google Scholar] [CrossRef] [PubMed]
- Rouanne, M.; Roumiguie, M.; Houede, N.; Masson-Lecomte, A.; Colin, P.; Pignot, G.; Larre, S.; Xylinas, E.; Roupret, M.; Neuzillet, Y. Development of immunotherapy in bladder cancer: Present and future on targeting PD(L)1 and CTLA-4 pathways. World J. Urol. 2018, 36, 1727–1740. [Google Scholar] [CrossRef]
- Damrauer, J.S.; Hoadley, K.A.; Chism, D.D.; Fan, C.; Tiganelli, C.J.; Wobker, S.E.; Yeh, J.J.; Milowsky, M.I.; Iyer, G.; Parker, J.S.; et al. Intrinsic subtypes of high-grade bladder cancer reflect the hallmarks of breast cancer biology. Proc. Natl. Acad. Sci. USA 2014, 111, 3110–3115. [Google Scholar] [CrossRef]
- Choi, W.; Porten, S.; Kim, S.; Willis, D.; Plimack, E.R.; Hoffman-Censits, J.; Roth, B.; Cheng, T.; Tran, M.; Lee, I.L.; et al. Identification of distinct basal and luminal subtypes of muscle-invasive bladder cancer with different sensitivities to frontline chemotherapy. Cancer Cell 2014, 25, 152–165. [Google Scholar] [CrossRef]
- Sjödahl, G.; Lauss, M.; Lövgren, K.; Chebil, G.; Gudjonsson, S.; Veerla, S.; Patschan, O.; Aine, M.; Fernö, M.; Ringnér, M.; et al. A molecular taxonomy for urothelial carcinoma. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2012, 18, 3377–3386. [Google Scholar] [CrossRef]
- Robertson, A.G.; Kim, J.; Al-Ahmadie, H.; Bellmunt, J.; Guo, G.; Cherniack, A.D.; Hinoue, T.; Laird, P.W.; Hoadley, K.A.; Akbani, R.; et al. Comprehensive Molecular Characterization of Muscle-Invasive Bladder Cancer. Cell 2017, 171, 540–556.e25. [Google Scholar] [CrossRef]
- Contreras-Sanz, A.; Roberts, M.E.; Seiler, R.; Black, P.C. Recent progress with next-generation biomarkers in muscle-invasive bladder cancer. Int. J. Urol. 2017, 24, 7–15. [Google Scholar] [CrossRef]
- Fantini, D.; Meeks, J.J. Genomic classification and risk stratification of bladder cancer. World J. Urol. 2019, 37, 1751–1757. [Google Scholar] [CrossRef]
- Zhou, X.; Qiu, S.; Nie, L.; Jin, D.; Jin, K.; Zheng, X.; Yang, L.; Wei, Q. Classification of Muscle-Invasive Bladder Cancer Based on Immunogenomic Profiling. Front. Oncol. 2020, 10, 1429. [Google Scholar] [CrossRef]
- Whiteside, T.L. The tumor microenvironment and its role in promoting tumor growth. Oncogene 2008, 27, 5904–5912. [Google Scholar] [CrossRef]
- Schneider, A.K.; Chevalier, M.F.; Derre, L. The multifaceted immune regulation of bladder cancer. Nat. Rev. Urol. 2019, 16, 613–630. [Google Scholar] [CrossRef]
- Liu, Y.; Cao, X. Immunosuppressive cells in tumor immune escape and metastasis. J. Mol. Med. 2016, 94, 509–522. [Google Scholar] [CrossRef]
- Limkin, E.J.; Sun, R.; Dercle, L.; Zacharaki, E.I.; Robert, C.; Reuzé, S.; Schernberg, A.; Paragios, N.; Deutsch, E.; Ferté, C. Promises and challenges for the implementation of computational medical imaging (radiomics) in oncology. Ann. Oncol. 2017, 28, 1191–1206. [Google Scholar] [CrossRef]
- Gillies, R.J.; Kinahan, P.E.; Hricak, H. Radiomics: Images Are More than Pictures, They Are Data. Radiology 2016, 278, 563–577. [Google Scholar] [CrossRef]
- Ye, F.; Hu, Y.; Gao, J.; Liang, Y.; Liu, Y.; Ou, Y.; Cheng, Z.; Jiang, H. Radiogenomics Map Reveals the Landscape of m6A Methylation Modification Pattern in Bladder Cancer. Front. Immunol. 2021, 12, 722642. [Google Scholar] [CrossRef]
- Tang, X.; Qian, W.L.; Yan, W.F.; Pang, T.; Gong, Y.L.; Yang, Z.G. Radiomic assessment as a method for predicting tumor mutation burden (TMB) of bladder cancer patients: A feasibility study. BMC Cancer 2021, 21, 823. [Google Scholar] [CrossRef]
- Zheng, Z.; Mao, S.; Zhang, W.; Liu, J.; Li, C.; Wang, R.; Yao, X. Dysregulation of the Immune Microenvironment Contributes to Malignant Progression and Has Prognostic Value in Bladder Cancer. Front. Oncol. 2020, 10, 542492. [Google Scholar] [CrossRef]
- Liu, S.; Xu, F.; Xu, T.; Yan, Y.; Yao, X.; Tang, G. Evaluation of Vesical Imaging-Reporting and Data System (VI-RADS) scoring system in predicting muscle invasion of bladder cancer. Transl. Androl. Urol. 2020, 9, 445–451. [Google Scholar] [CrossRef]
- van Griethuysen, J.J.M.; Fedorov, A.; Parmar, C.; Hosny, A.; Aucoin, N.; Narayan, V.; Beets-Tan, R.G.H.; Fillion-Robin, J.C.; Pieper, S.; Aerts, H. Computational Radiomics System to Decode the Radiographic Phenotype. Cancer Res. 2017, 77, e104–e107. [Google Scholar] [CrossRef] [PubMed]
- Peng, H.; Long, F.; Ding, C. Feature selection based on mutual information: Criteria of max-dependency, max-relevance, and min-redundancy. IEEE Trans. Pattern Anal. Mach. Intell. 2005, 27, 1226–1238. [Google Scholar] [CrossRef] [PubMed]
- Tibshirani, R. The lasso method for variable selection in the Cox model. Stat. Med. 1997, 16, 385–395. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed]
- Kitamura, T.; Qian, B.Z.; Pollard, J.W. Immune cell promotion of metastasis. Nat. Rev. Immunol. 2015, 15, 73–86. [Google Scholar] [CrossRef]
- Qian, B.Z.; Pollard, J.W. Macrophage diversity enhances tumor progression and metastasis. Cell 2010, 141, 39–51. [Google Scholar] [CrossRef]
- Ruffell, B.; Coussens, L.M. Macrophages and therapeutic resistance in cancer. Cancer Cell 2015, 27, 462–472. [Google Scholar] [CrossRef]
- Galdiero, M.R.; Garlanda, C.; Jaillon, S.; Marone, G.; Mantovani, A. Tumor associated macrophages and neutrophils in tumor progression. J. Cell Physiol. 2013, 228, 1404–1412. [Google Scholar] [CrossRef]
- Michelet, X.; Dyck, L.; Hogan, A.; Loftus, R.M.; Duquette, D.; Wei, K.; Beyaz, S.; Tavakkoli, A.; Foley, C.; Donnelly, R.; et al. Metabolic reprogramming of natural killer cells in obesity limits antitumor responses. Nat. Immunol. 2018, 19, 1330–1340. [Google Scholar] [CrossRef]
- Necchi, A.; Raggi, D.; Gallina, A.; Ross, J.S.; Fare, E.; Giannatempo, P.; Marandino, L.; Colecchia, M.; Luciano, R.; Bianchi, M.; et al. Impact of Molecular Subtyping and Immune Infiltration on Pathological Response and Outcome Following Neoadjuvant Pembrolizumab in Muscle-invasive Bladder Cancer. Eur. Urol. 2020, 77, 701–710. [Google Scholar] [CrossRef]
- Kamoun, A.; de Reynies, A.; Allory, Y.; Sjodahl, G.; Robertson, A.G.; Seiler, R.; Hoadley, K.A.; Groeneveld, C.S.; Al-Ahmadie, H.; Choi, W.; et al. A Consensus Molecular Classification of Muscle-invasive Bladder Cancer. Eur. Urol. 2020, 77, 420–433. [Google Scholar] [CrossRef]
- Jiang, W.; Zhu, D.; Wang, C.; Zhu, Y. An immune relevant signature for predicting prognoses and immunotherapeutic responses in patients with muscle-invasive bladder cancer (MIBC). Cancer Med. 2020, 9, 2774–2790. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, L.; Yu, M.; Fang, Y.; Qian, K.; Wang, G.; Ju, L.; Xiao, Y.; Wang, X. Immune-related signature predicts the prognosis and immunotherapy benefit in bladder cancer. Cancer Med. 2020, 9, 7729–7741. [Google Scholar] [CrossRef]
- Li, H.; Lu, H.; Cui, W.; Huang, Y.; Jin, X. A TP53-based immune prognostic model for muscle-invasive bladder cancer. Aging 2020, 12, 1929–1946. [Google Scholar] [CrossRef]
- Teft, W.A.; Kirchhof, M.G.; Madrenas, J. A molecular perspective of CTLA-4 function. Annu. Rev. Immunol. 2006, 24, 65–97. [Google Scholar] [CrossRef]
- Lee, K.M.; Chuang, E.; Griffin, M.; Khattri, R.; Hong, D.K.; Zhang, W.; Straus, D.; Samelson, L.E.; Thompson, C.B.; Bluestone, J.A. Molecular basis of T cell inactivation by CTLA-4. Science 1998, 282, 2263–2266. [Google Scholar] [CrossRef]
- Sansom, D.M.; Walker, L.S. The role of CD28 and cytotoxic T-lymphocyte antigen-4 (CTLA-4) in regulatory T-cell biology. Immunol. Rev. 2006, 212, 131–148. [Google Scholar] [CrossRef]
- Topalian, S.L.; Drake, C.G.; Pardoll, D.M. Immune checkpoint blockade: A common denominator approach to cancer therapy. Cancer Cell 2015, 27, 450–461. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Z.; Guo, Y.; Huang, X.; Liu, J.; Wang, R.; Qiu, X.; Liu, S. CD8A as a Prognostic and Immunotherapy Predictive Biomarker Can Be Evaluated by MRI Radiomics Features in Bladder Cancer. Cancers 2022, 14, 4866. [Google Scholar] [CrossRef]
- Tian, Z.; Meng, L.; Long, X.; Diao, T.; Hu, M.; Wang, M.; Liu, M.; Wang, J. Identification and validation of an immune-related gene-based prognostic index for bladder cancer. Am. J. Transl. Res. 2020, 12, 5188–5204. [Google Scholar] [CrossRef]
- Wang, J.; Gu, X.; Cao, L.; Ouyang, Y.; Qi, X.; Wang, Z.; Wang, J. A novel prognostic biomarker CD3G that correlates with the tumor microenvironment in cervical cancer. Front. Oncol. 2022, 12, 979226. [Google Scholar] [CrossRef] [PubMed]
- Berinstein, N.L.; McNamara, M.; Nguyen, A.; Egan, J.; Wolf, G.T. Increased immune infiltration and chemokine receptor expression in head and neck epithelial tumors after neoadjuvant immunotherapy with the IRX-2 regimen. Oncoimmunology 2018, 7, e1423173. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Li, L.; Li, Y.; Qian, Z.; Wu, F.; He, Y.; Jiang, H.; Li, R.; Wang, D.; Zhai, Y.; et al. An MRI radiomics approach to predict survival and tumour-infiltrating macrophages in gliomas. Brain 2022, 145, 1151–1161. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Jiang, Y.; Xiong, W.; Sun, Z.; Chen, C.; Yuan, Q.; Zhou, K.; Han, Z.; Feng, H.; Chen, H.; et al. Noninvasive imaging of the tumor immune microenvironment correlates with response to immunotherapy in gastric cancer. Nat. Commun. 2022, 13, 5095. [Google Scholar] [CrossRef]
- Sun, R.; Limkin, E.J.; Vakalopoulou, M.; Dercle, L.; Champiat, S.; Han, S.R.; Verlingue, L.; Brandao, D.; Lancia, A.; Ammari, S.; et al. A radiomics approach to assess tumour-infiltrating CD8 cells and response to anti-PD-1 or anti-PD-L1 immunotherapy: An imaging biomarker, retrospective multicohort study. Lancet Oncol. 2018, 19, 1180–1191. [Google Scholar] [CrossRef]
- Yacouba, A.; Tidjani Alou, M.; Lagier, J.C.; Dubourg, G.; Raoult, D. Urinary microbiota and bladder cancer: A systematic review and a focus on uropathogens. Semin. Cancer Biol. 2022, 86, 875–884. [Google Scholar] [CrossRef]
- Sun, Q.; Chen, Y.; Liang, C.; Zhao, Y.; Lv, X.; Zou, Y.; Yan, K.; Zheng, H.; Liang, D.; Li, Z.C. Biologic Pathways Underlying Prognostic Radiomics Phenotypes from Paired MRI and RNA Sequencing in Glioblastoma. Radiology 2021, 301, 654–663. [Google Scholar] [CrossRef]
- Ge, L.; Chen, Y.; Yan, C.; Zhao, P.; Zhang, P.; Liu, J. Study Progress of Radiomics With Machine Learning for Precision Medicine in Bladder Cancer Management. Front. Oncol. 2019, 9, 1296. [Google Scholar] [CrossRef]
- Lin, P.; Wen, D.-Y.; Chen, L.; Li, X.; Li, S.-h.; Yan, H.-b.; He, R.-q.; Chen, G.; He, Y.; Yang, H. A radiogenomics signature for predicting the clinical outcome of bladder urothelial carcinoma. Eur. Radiol. 2019, 30, 547–557. [Google Scholar] [CrossRef]





| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Variables | HR (95% CI) | p-Value | HR (95% CI) | p-Value |
| Age | 1.03 (1.02–1.05) | <0.001 | 1.04 (1.02–1.05) | <0.001 |
| Sex | 1.19 (0.86–1.64) | 0.308 | - | - |
| Stage | 1.74 (1.43–2.11) | <0.001 | - | - |
| Grade | 2.89 (0.72–11.68) | 0.136 | - | - |
| T stage | 1.65 (1.33–2.04) | <0.001 | 1.37 (1.05–1.77) | 0.018 |
| M stage | 2.64 (1.29–5.38) | 0.009 | - | - |
| N stage | 1.56 (1.33–1.84) | <0.001 | 1.44 (1.20–1.72) | <0.001 |
| Morphology | 0.68 (0.48–0.97) | 0.031 | - | - |
| IPS | 1.48 (1.20–1.83) | <0.001 | 1.33 (1.06–1.66) | 0.015 |
| Characteristic | Number of Patients (%) | p-Value | |
|---|---|---|---|
| Training Set (n = 77) | Validation Set (n = 34) | ||
| Sex | |||
| Men | 66 (85.7) | 25 (73.5) | 0.124 |
| Women | 11 (14.3) | 9 (26.5) | |
| Age (years) | |||
| <65 | 22 (28.6) | 11 (32.4) | 0.688 |
| ≥65 | 55 (71.4) | 23 (67.6) | |
| Tumor size (cm) | |||
| <3 | 40 (51.9) | 15 (44.1) | 0.447 |
| ≥3 | 37 (48.1) | 19 (55.9) | |
| Number of tumors | |||
| Single | 51 (66.2) | 24 (70.6) | 0.651 |
| Multiple | 26 (33.8) | 10 (29.4) | |
| Pathological grade | |||
| Low-grade | 15 (19.5) | 9 (26.5) | 0.410 |
| High-grade | 62 (80.5) | 25 (73.5) | |
| Clinical T stage | |||
| <T2 | 49 (63.6) | 24 (70.6) | 0.477 |
| ≥T2 | 28 (36.4) | 10 (29.4) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, S.; Chen, H.; Zheng, Z.; He, Y.; Yao, X. Development of a Molecular-Subtype-Associated Immune Prognostic Signature That Can Be Recognized by MRI Radiomics Features in Bladder Cancer. Bioengineering 2023, 10, 318. https://doi.org/10.3390/bioengineering10030318
Liu S, Chen H, Zheng Z, He Y, Yao X. Development of a Molecular-Subtype-Associated Immune Prognostic Signature That Can Be Recognized by MRI Radiomics Features in Bladder Cancer. Bioengineering. 2023; 10(3):318. https://doi.org/10.3390/bioengineering10030318
Chicago/Turabian StyleLiu, Shenghua, Haotian Chen, Zongtai Zheng, Yanyan He, and Xudong Yao. 2023. "Development of a Molecular-Subtype-Associated Immune Prognostic Signature That Can Be Recognized by MRI Radiomics Features in Bladder Cancer" Bioengineering 10, no. 3: 318. https://doi.org/10.3390/bioengineering10030318
APA StyleLiu, S., Chen, H., Zheng, Z., He, Y., & Yao, X. (2023). Development of a Molecular-Subtype-Associated Immune Prognostic Signature That Can Be Recognized by MRI Radiomics Features in Bladder Cancer. Bioengineering, 10(3), 318. https://doi.org/10.3390/bioengineering10030318






