PosturAll: A Posture Assessment Software for Children
Abstract
:1. Introduction
2. Materials and Methods
2.1. Software Improvement
2.2. Software Optimization
2.3. Data Acquisition
2.3.1. Description of Participants
2.3.2. Materials and Experimental Setup
2.3.3. Technical Validation
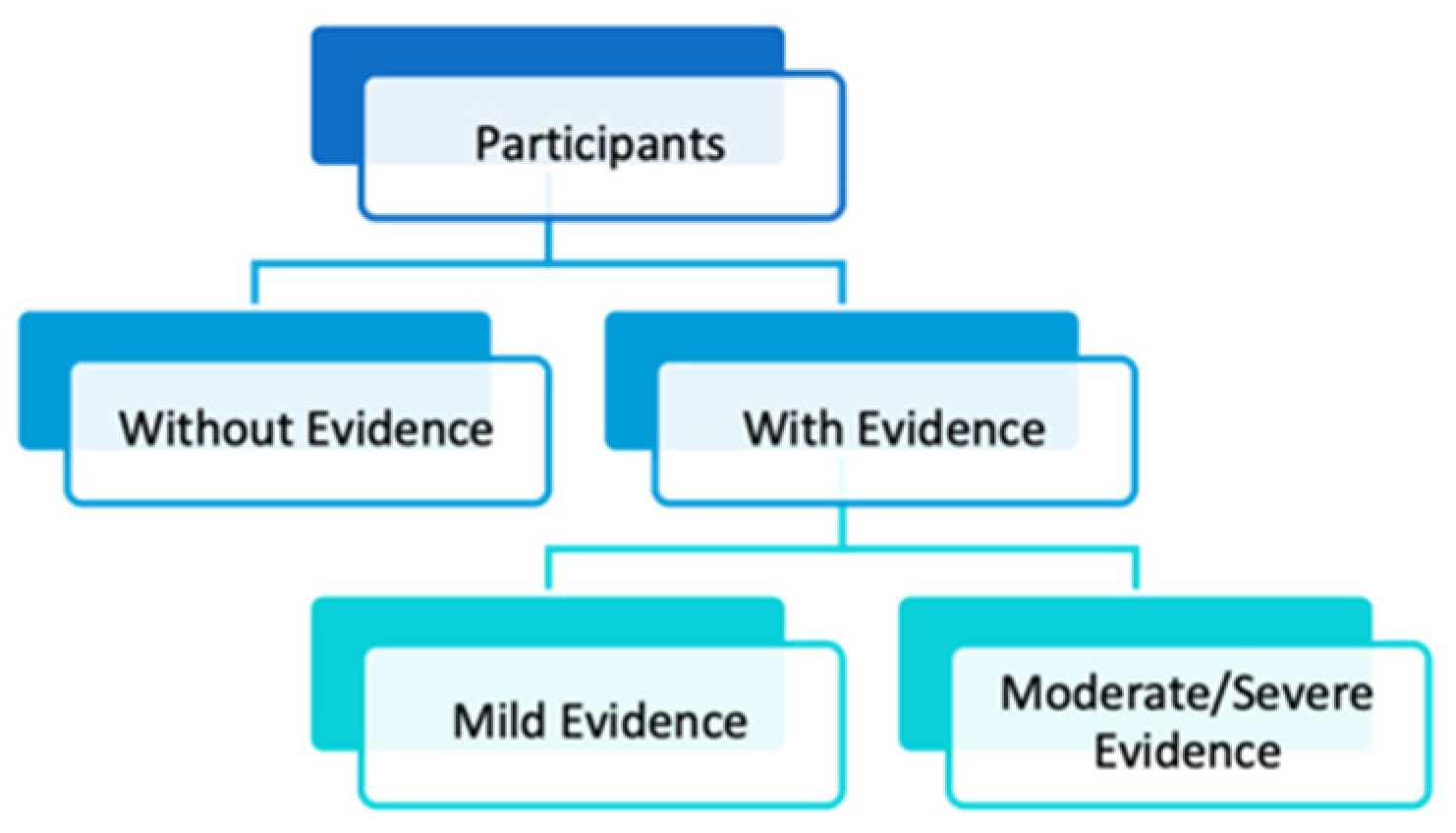
2.4. Classification
3. Results
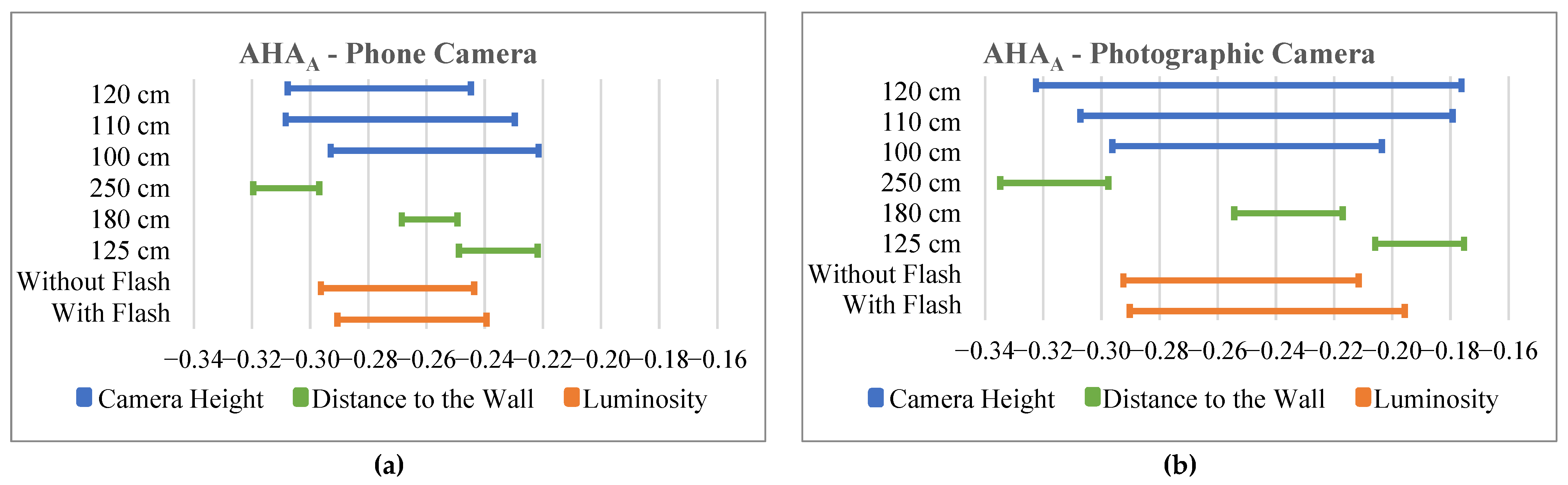
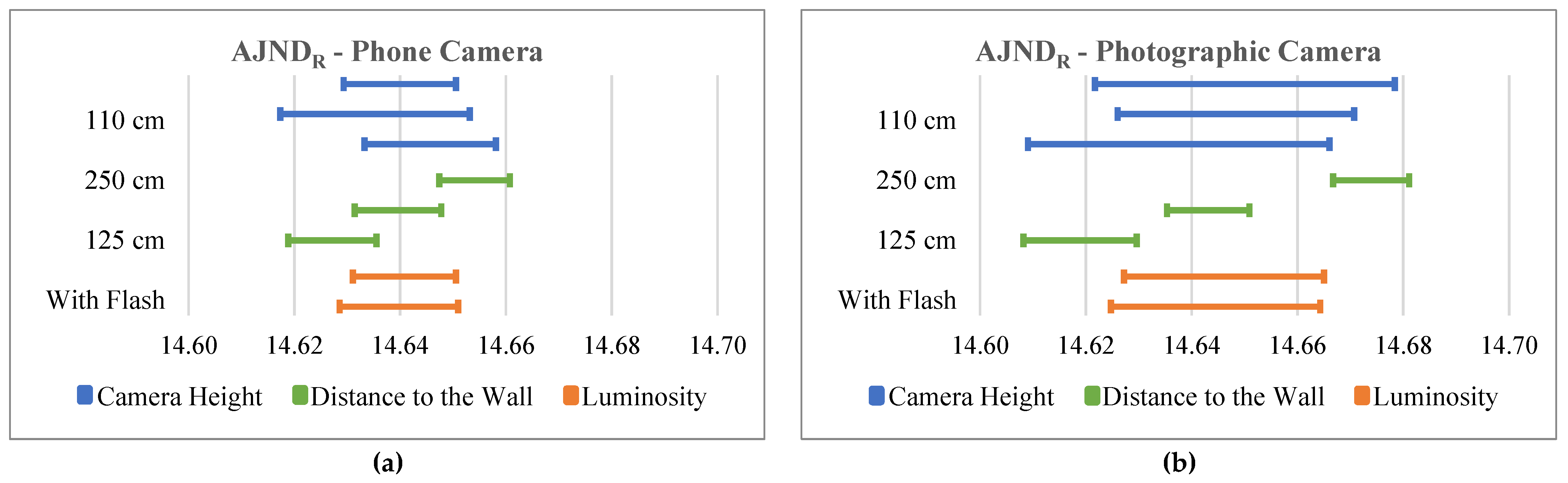
3.1. Software Optimization
3.2. Comparison with the Contemplas Software
3.3. Classification
3.3.1. Feature Selection
3.3.2. Classification Performance
4. Discussion
4.1. Software Optimization
4.2. Comparison with the Contemplas Software
4.3. Classification
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AADL | Left Acromion–ASIS Distance |
| AADR | Right Acromion–ASIS Distance |
| AHAA | Acromions Horizontal Alignment in Anterior View |
| AHAP | Acromions Horizontal Alignment in Posterior View |
| AJNDL | Left Acromion–Jugular Notch Distance |
| AJNDR | Right Acromion–Jugular Notch Distance |
| AKLAL | Left Knee Lateral Angle in Anterior View |
| AKLAR | Right Knee Lateral Angle in Anterior View |
| ALAL | Left Ankle Lateral Angle |
| ALAR | Right Ankle Lateral Angle |
| ALLLL | Left Lower Limb Length in Anterior View |
| ALLLR | Right Lower Limb Length in Anterior View |
| APDL | Left Acromion–PSIS Distance |
| APDR | Right Acromion–PSIS Distance |
| ASA | Acromions–Sternum Angle |
| ASISHA | ASISs Horizontal Alignment |
| ASISLAL | ASISs–Left Leg Angle |
| ASISLAR | ASISs–Right Leg Angle |
| AVA | Acromions–Vertebral Column Angle |
| KAL | Knee Angle in Left Lateral View |
| KAR | Knee Angle in Right Lateral View |
| LFAL | Leg–Foot Angle in Left Lateral View |
| LFAR | Leg–Foot Angle in Right Lateral View |
| LLA | Lumbar Lordosis Lateral Angle |
| LLCL | Lumbar Lordosis Curvature in Left Lateral View |
| LLCR | Lumbar Lordosis Curvature in Right Lateral View |
| PKLAL | Left Knee Lateral Angle in Posterior View |
| PKLAR | Right Knee Lateral Angle in Posterior View |
| PLAL | Pelvis–Leg Angle in Left Lateral View |
| PLAR | Pelvis–Leg Angle in Right Lateral View |
| PLLLL | Left Lower Limb Length in Posterior View |
| PLLLR | Right Lower Limb Length in Posterior View |
| PSISHA | PSISs Horizontal Alignment |
| PSISLAL | PSISs–Left Leg Angle |
| PSISLAR | PSISs–Right Leg Angle |
| TKA | Thoracic Kyphosis Lateral Angle |
| TKCL | Thoracic Kyphosis Curvature in Left Lateral View |
| TKCR | Thoracic Kyphosis Curvature in Right Lateral View |
References
- Latalski, M.; Bylina, J.; Fatyga, M.; Repko, M.; Filipovic, M.; Jarosz, M.J.; Borowicz, K.B.; Matuszewski, Ł.; Trzpis, T. Risk factors of postural defects in children at school age. Ann. Agric. Environ. Med. AAEM 2013, 20, 583–587. [Google Scholar] [PubMed]
- Pinho, M.E.R.C.; Vaz, M.A.P.; Arezes, P.M.F.M.; Campos, J.C.R.; De Magalhães, A.P.B. Lesões músculo-esqueléticas relacionadas com as atividades desportivas em crianças e adolescentes: Uma revisão das questões emergentes. Motricidade 2013, 9, 31–48. [Google Scholar] [CrossRef] [PubMed]
- Minghelli, B.; Oliveira, R.; Nunes, C. Postural habits and weight of backpacks of Portuguese adolescents: Are they associated with scoliosis and low back pain? Work 2016, 54, 197–208. [Google Scholar] [CrossRef] [PubMed]
- Galozzi, P.; Maghini, I.; Bakdounes, L.; Ferlito, E.; Lazzari, V.; Ermani, M.; Chia, M.; Gatti, D.; Masiero, S.; Punzi, L. Prevalence of low back pain and its effect on health-related quality of life in 409 scholar adolescents from the Veneto region. Reumatismo 2019, 71, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Dianat, I.; Sorkhi, N.; Pourhossein, A.; Alipour, A.; Asghari-Jafarabadi, M. Neck, shoulder and low back pain in secondary schoolchildren in relation to schoolbag carriage: Should the recommended weight limits be gender-specific? Appl. Ergon. 2014, 45, 437–442. [Google Scholar] [CrossRef]
- Houghton, K.M. Review for the generalist: Evaluation of low back pain in children and adolescents. Pediatr. Rheumatol. Online J. 2010, 8, 28. [Google Scholar] [CrossRef]
- Jones, G.T. Epidemiology of low back pain in children and adolescents. Arch. Dis. Child. 2005, 90, 312–316. [Google Scholar] [CrossRef]
- Barreto, T.W.; Lin, K.W. Noninvasive Treatments for Low Back Pain. Am. Fam. Physician 2017, 96, 324–327. [Google Scholar]
- Froud, R.; Patterson, S.; Eldridge, S.; Seale, C.; Pincus, T.; Rajendran, D.; Fossum, C.; Underwood, M. A systematic review and meta-synthesis of the impact of low back pain on people’s lives. BMC Musculoskelet. Disord. 2014, 15, 50. [Google Scholar] [CrossRef]
- Coelho, L.; Almeida, V.; Oliveira, R. Lombalgia nos adolescentes: Identificação de factores de risco psicossociais. Estud. Epidemiológico Região Gd. Lisb. 2005, 23, 81–90. [Google Scholar]
- O’Sullivan, P.; Smith, A.; Beales, D.; Straker, L. Understanding Adolescent Low Back Pain from a Multidimensional Perspective: Implications for Management. J. Orthop. Sports Phys. Ther. 2017, 47, 741–751. [Google Scholar] [CrossRef] [PubMed]
- Dorner, T.E.; Crevenna, R. Preventive aspects regarding back pain. Wien. Med. Wochenschr. 2016, 166, 15–21. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, J.; Stuart, E.; Rodenberg, R. Musculoskeletal Low Back Pain in School-aged Children: A Review. JAMA Pediatr. 2017, 171, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Minghelli, B. Musculoskeletal spine pain in adolescents: Epidemiology of non-specific neck and low back pain and risk factors. J. Orthop. Sci. 2020, 25, 776–780. [Google Scholar] [CrossRef]
- Watson, K.D.; Papageorgiou, A.C.; Jones, G.T.; Taylor, S.; Symmons, D.P.M.; Silman, A.J.; Macfarlane, G.J. Low back pain in schoolchildren: Occurrence and characteristics. Pain 2002, 97, 87–92. [Google Scholar] [CrossRef]
- Fritz, J.M.; Clifford, S.N. Low back pain in adolescents: A comparison of clinical outcomes in sports participants and nonparticipants. J. Athl. Train. 2010, 45, 61–66. [Google Scholar] [CrossRef]
- Siivola, S.M.; Levoska, S.; Latvala, K.; Hoskio, E.; Vanharanta, H.; Keinänen-Kiukaanniemi, S. Predictive Factors for Neck and Shoulder Pain: A Longitudinal Study in Young Adults. Spine 2004, 29, 1662–1669. [Google Scholar] [CrossRef]
- Hestbaek, L.; Leboeuf-Yde, C.; Kyvik, K.O.; Manniche, C. The course of low back pain from adolescence to adulthood: Eight-year follow-up of 9600 twins. Spine 2006, 31, 468–472. [Google Scholar] [CrossRef]
- Breivik, H.; Collett, B.; Ventafridda, V.; Cohen, R.; Gallacher, D. Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. Eur. J. Pain 2006, 10, 287–333. [Google Scholar] [CrossRef]
- Lee, S.; Shim, J. The effects of backpack loads and spinal stabilization exercises on the dynamic foot pressure of elementary school children with idiopathic scoliosis. J. Phys. Ther. Sci. 2015, 27, 2257–2260. [Google Scholar] [CrossRef]
- Bozkurt, S.; Kayalar, G.; Tezel, N.; Güler, T.; Kesikburun, B.; Denizli, M.; Tan, S.; Yilmaz, H. Hypermobility Frequency in School Children: Relationship with Idiopathic Scoliosis, Age, Sex and Musculoskeletal Problems. Arch. Rheumatol. 2019, 34, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Ghanem, I.; Rizkallah, M. Adolescent idiopathic scoliosis for the primary care physician: Frequently asked questions. Curr. Opin. Pediatr. 2019, 31, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Gieysztor, E.Z.; Sadowska, L.; Choińska, A.M.; Paprocka-Borowicz, M. Trunk rotation due to persistence of primitive reflexes in early school-age children. Adv. Clin. Exp. Med. 2018, 27, 363–366. [Google Scholar] [CrossRef]
- Kenanidis, E.; Athanasiadis, D.I.; Geropoulos, G.; Kakoulidis, P.; Potoupnis, M.; Tsiridis, E. Does the sternum play a role in the aetiopathogenesis of adolescent idiopathic scoliosis? Preliminary data of a new theory. Hippokratia 2018, 22, 173–177. [Google Scholar] [PubMed]
- Konieczny, M.R.; Senyurt, H.; Krauspe, R. Epidemiology of adolescent idiopathic scoliosis. J. Child. Orthop. 2013, 7, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Horne, J.P.; Flannery, R.; Usman, S. Adolescent idiopathic scoliosis: Diagnosis and management. Am. Fam. Physician 2014, 89, 193–198. [Google Scholar]
- Jada, A.; Mackel, C.E.; Hwang, S.W.; Samdani, A.F.; Stephen, J.H.; Bennett, J.T.; Baaj, A.A. Evaluation and management of adolescent idiopathic scoliosis: A review. Neurosurg. Focus 2017, 43, E2. [Google Scholar] [CrossRef] [PubMed]
- Gelalis, I.D.; Ristanis, S.; Nikolopoulos, A.; Politis, A.; Rigas, C.; Xenakis, T. Loading rate patterns in scoliotic children during gait: The impact of the schoolbag carriage and the importance of its position. Eur. Spine J. 2012, 21, 1936–1941. [Google Scholar] [CrossRef]
- Mahaudens, P.; Detrembleur, C.; Mousny, M.; Banse, X. Gait in adolescent idiopathic scoliosis: Energy cost analysis. Eur. Spine J. 2009, 18, 1160–1168. [Google Scholar] [CrossRef]
- Minghelli, B.; Oliveira, R.; Nunes, C. Non-specific low back pain in adolescents from the south of Portugal: Prevalence and associated factors. J. Orthop. Sci. 2014, 19, 883–892. [Google Scholar] [CrossRef]
- Dianat, I.; Javadivala, Z.; Allahverdipour, H. School Bag Weight and the Occurrence of Shoulder, Hand/Wrist and Low Back Symptoms among Iranian Elementary Schoolchildren. Health Promot. Perspect. 2011, 1, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Koch, C.; Hänsel, F. Non-specific Low Back Pain and Postural Control During Quiet Standing—A Systematic Review. Front. Psychol. 2019, 10, 586. [Google Scholar] [CrossRef] [PubMed]
- Brumagne, S.; Janssens, L.; Knapen, S.; Claeys, K.; Suuden-Johanson, E. Persons with recurrent low back pain exhibit a rigid postural control strategy. Eur. Spine J. 2008, 17, 1177–1184. [Google Scholar] [CrossRef] [PubMed]
- García-Soidán, J.L.; Leirós-Rodríguez, R.; Romo-Pérez, V.; García-Liñeira, J. Accelerometric Assessment of Postural Balance in Children: A Systematic Review. Diagnostics 2020, 11, 8. [Google Scholar] [CrossRef] [PubMed]
- Yu, Q.; Huo, Y.; Chen, M.; Zhang, Z.; Li, Z.; Luo, H.; Liang, Z.; Wang, C.; Lo, W.L.A. A Study on the Relationship between Postural Control and Pain-Related Clinical Outcomes in Patients with Chronic Nonspecific Low Back Pain. Pain Res. Manag. 2021, 2021, 9054152. [Google Scholar] [CrossRef]
- Gur, G.; Dilek, B.; Ayhan, C.; Simsek, E.; Aras, O.; Aksoy, S.; Yakut, Y. Effect of a spinal brace on postural control in different sensory conditions in adolescent idiopathic scoliosis: A preliminary analysis. Gait Posture 2015, 41, 93–99. [Google Scholar] [CrossRef]
- Beaulieu, M.; Toulotte, C.; Gatto, L.; Rivard, C.-H.; Teasdale, N.; Simoneau, M.; Allard, P. Postural imbalance in non-treated adolescent idiopathic scoliosis at different periods of progression. Eur. Spine J. 2009, 18, 38–44. [Google Scholar] [CrossRef]
- Gauchard, G.C.; Lascombes, P.; Kuhnast, M.; Perrin, P.P. Influence of Different Types of Progressive Idiopathic Scoliosis on Static and Dynamic Postural Control. Spine 2001, 26, 1052–1058. [Google Scholar] [CrossRef]
- Dagenais, S.; Caro, J.; Haldeman, S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008, 8, 8–20. [Google Scholar] [CrossRef]
- EuroStat Persons Reporting a Chronic Disease, by Disease, Sex, Age and Educational Attainment Level. Available online: https://ec.europa.eu/eurostat/databrowser/view/HLTH{\_}EHIS{\_}CD1E{\_}{\_}custom{\_}6017590/default/table?lang=en (accessed on 28 March 2023).
- Instituto Nacional de Estatística (INE). Acidentes de Trabalho e Problemas de Saúde Relacionados com o Trabalho—Módulo ad hoc do Inquérito ao Emprego 2.o trimestre de 2020. 2020. Available online: https://www.ine.pt/ngt_server/attachfileu.jsp?look_parentBoui=462695067&att_display=n&att_download=y (accessed on 21 January 2021).
- Gunzburg, R.; Balagué, F.; Nordin, M.; Szpalski, M.; Duyck, D.; Bull, D.; Mélot, C. Low back pain in a population of school children. Eur. Spine J. 1999, 8, 439–443. [Google Scholar] [CrossRef]
- Shah, S.A.; Saller, J. Evaluation and Diagnosis of Back Pain in Children and Adolescents. J. Am. Acad. Orthop. Surg. 2016, 24, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.P. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin. Proc. 2015, 90, 284–299. [Google Scholar] [CrossRef]
- Hébert-Losier, K.; Abd Rahman, F. Reliability of postural measures in elite badminton players using Posture Pro 8. Physiother. Theory Pract. 2018, 34, 483–494. [Google Scholar] [CrossRef] [PubMed]
- Toelle, T.R.; Utpadel-Fischler, D.A.; Haas, K.-K.; Priebe, J.A. App-based multidisciplinary back pain treatment versus combined physiotherapy plus online education: A randomized controlled trial. NPJ Digit. Med. 2019, 2, 34. [Google Scholar] [CrossRef]
- Huber, S.; Priebe, J.A.; Baumann, K.-M.; Plidschun, A.; Schiessl, C.; Tölle, T.R. Treatment of Low Back Pain with a Digital Multidisciplinary Pain Treatment App: Short-Term Results. JMIR Rehabil. Assist. Technol. 2017, 4, e11. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, U.-V.; von Jan, U. Safe, sound and desirable: Development of mHealth apps under the stress of rapid life cycles. mHealth 2017, 3, 27. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, E.A.G.; Duarte, M.; Maldonado, E.P.; Burke, T.N.; Marques, A.P. Postural assessment software (PAS/SAPO): Validation and reliabiliy. Clinics 2010, 65, 675–681. [Google Scholar] [CrossRef]
- Ferreira, E.A.; Duarte, M.; Maldonado, E.P.; Bersanetti, A.A.; Marques, A.P. Quantitative assessment of postural alignment in young adults based on photographs of anterior, posterior, and lateral views. J. Manip. Physiol. Ther. 2011, 34, 371–380. [Google Scholar] [CrossRef]
- Ming, A.; Ma, H. A blob detector in color images. In Proceedings of the 6th ACM International Conference on Image and Video Retrieval—CIVR ’07, Amsterdam, The Netherlands, 9–11 July 2007; ACM Press: New York, NY, USA, 2007; pp. 364–370. [Google Scholar] [CrossRef]
- Lindeberg, T. Detecting salient blob-like image structures and their scales with a scale-space primal sketch: A method for focus-of-attention. Int. J. Comput. Vis. 1993, 11, 283–318. [Google Scholar] [CrossRef]
- Bradski, G. The OpenCV Library: SimpleBlobDetector Class Reference. Available online: https://docs.opencv.org/4.5.1/d0/d7a/classcv_1_1SimpleBlobDetector.html (accessed on 7 January 2021).
- Baíllo, A.; Chacón, J.E. Statistical outline of animal home ranges: An application of set estimation. Handb. Stat. 2021, 44, 3–37. [Google Scholar] [CrossRef]
- Stark, R.M.; Morris, C.C. Finite Mathematics: Models and Applications; Wiley: Hoboken, NJ, USA, 2015; Available online: https://books.google.pt/books?id=ZgJyCgAAQBAJ (accessed on 12 May 2022).
- CONTEMPLAS GmbH CONTEMPLAS—Professional Motion Analysis Software. 2022. Available online: https://contemplas.com/en/motion-analysis/ (accessed on 5 March 2022).
- Bee Wah, Y.; Mohd Razali, N. Power comparisons of Shapiro-Wilk, Kolmogorov-Smirnov, Lilliefors and Anderson-Darling tests. J. Stat. Model. Anal. 2011, 2, 21–33. [Google Scholar]
- Rosner, B. Fundamentals of Biostatistics; Cengage Learning: Boston, MA, USA, 2015; Available online: https://books.google.pt/books?id=yn4yBgAAQBAJ (accessed on 16 May 2022).
- Lakens, D. Equivalence Tests. Soc. Psychol. Personal. Sci. 2017, 8, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Streiner, D.L. Unicorns Do Exist: A Tutorial on “Proving” the Null Hypothesis. Can. J. Psychiatry 2003, 48, 756–761. [Google Scholar] [CrossRef] [PubMed]
- Altay, O.; Ulas, M. Prediction of the autism spectrum disorder diagnosis with linear discriminant analysis classifier and K-nearest neighbor in children. In Proceedings of the 2018 6th International Symposium on Digital Forensic and Security (ISDFS), Antalya, Turkey, 22–25 March 2018; pp. 1–4. [Google Scholar] [CrossRef]
- Berrar, D. Cross-Validation. In Encyclopedia of Bioinformatics and Computational Biology; Elsevier: Amsterdam, The Netherlands, 2019; pp. 542–545. [Google Scholar] [CrossRef]
- Anguita, D.; Ghelardoni, L.; Ghio, A.; Oneto, L.; Ridella, S. The ‘K’ in K-fold Cross Validation. In Proceedings of the ESANN 2012 European Symposium on Artificial Neural Networks, Computational Intelligence and Machine Learning, Bruges, Belgium, 25–27 April 2012; pp. 25–27. [Google Scholar]
- Palshikar, A. What distinguishes binary from multi-class intrusion detection systems: Observations from experiments. Int. J. Inf. Manag. Data Insights 2022, 2, 100125. [Google Scholar] [CrossRef]
- Sáez, J.A.; Galar, M.; Luengo, J.; Herrera, F. Analyzing the presence of noise in multi-class problems: Alleviating its influence with the One-vs-One decomposition. Knowl. Inf. Syst. 2014, 38, 179–206. [Google Scholar] [CrossRef]
- Lorena, A.C.; De Carvalho, A.C.P.L.F.; Gama, J.M.P. A review on the combination of binary classifiers in multiclass problems. Artif. Intell. Rev. 2008, 30, 19–37. [Google Scholar] [CrossRef]
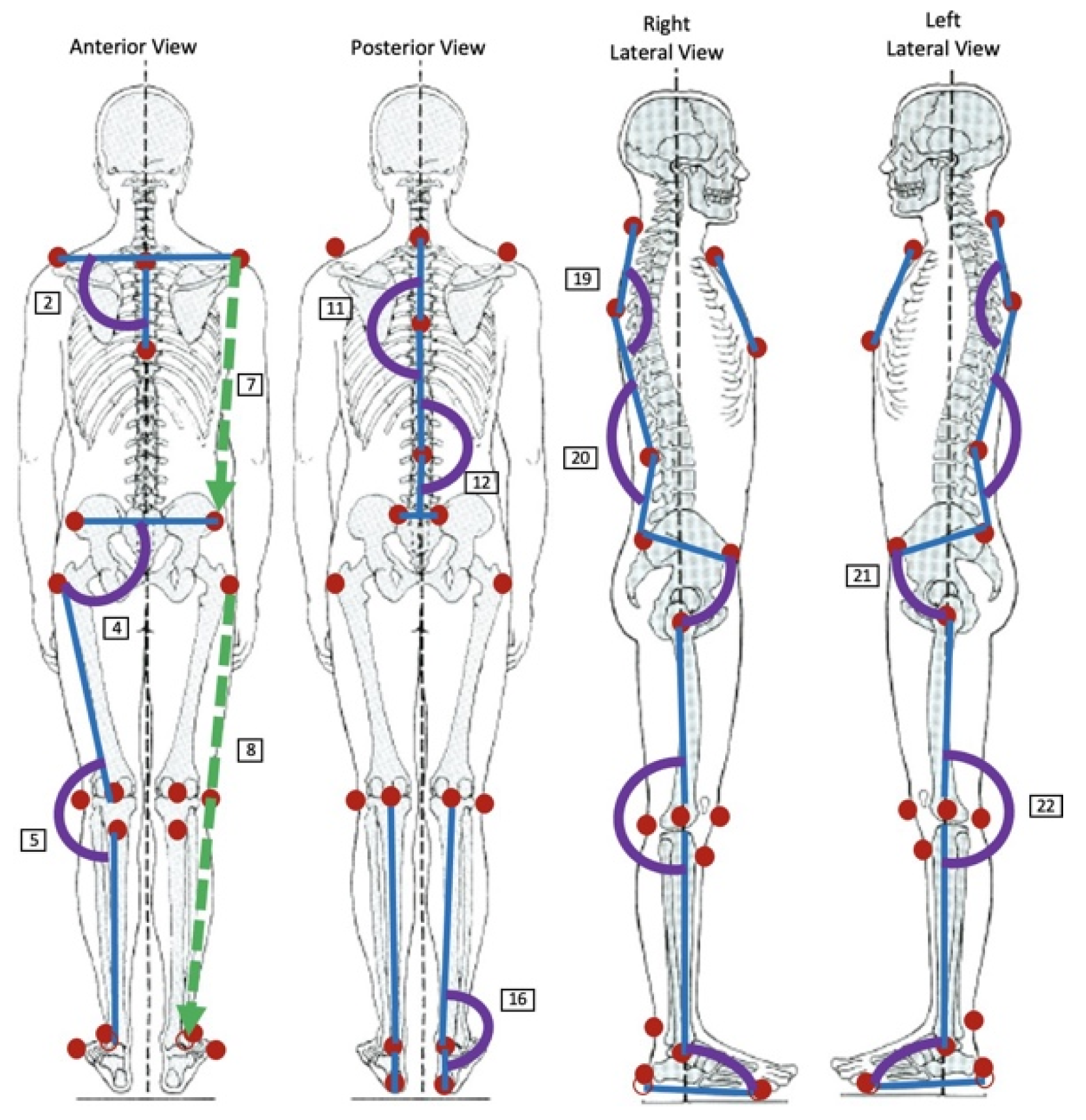
| Parameter | Description of Anatomical Landmarks Used | |
|---|---|---|
| Anterior | 1. Acromions Horizontal Alignment (AHAA) | Angle between the two acromions and a horizontal line |
| 2. Acromions–Sternum Angle (ASA) | Angle between the jugular notch and the xiphoid appendix and the two acromions’ line | |
| 3. ASISs Horizontal Alignment (ASISHA) | Angle between the two ASISs and a horizontal line | |
| 4. ASISs–Leg Angle (ASISLAL; ASISLAR) | Angle between the trochanter and patella and the line of the two ASIS’s line | |
| 5. Knee Lateral Angle (AKLAL; AKLAR) | Angle between the line of the trochanter and the patella and the line of the tibial tuberosity and the lateral malleolus | |
| 6. Acromion–Jugular Notch Distance (AJNDL; AJNDR) | Distance between the jugular notch and each acromion | |
| 7. Acromion–ASIS Distance (AADL; AADR) | Distance between the acromion and the ASIS of the same side | |
| 8. Lower Limb Length (ALLLL; ALLLR) | Distance between the trochanter and the lateral malleolus of the same side | |
| Posterior | 9. Acromions Horizontal Alignment (AHAP) | Angle between the two acromions and a horizontal line |
| 10. Acromions-Vertebral Column Angle (AVA) | Angle between the C7 and the most prominent point of thoracic kyphosis and the line of the two acromions | |
| 11. Thoracic Kyphosis Lateral Angle (TKA) | Angle between C7, the most prominent point of thoracic kyphosis and the deepest point of lumbar lordosis | |
| 12. Lumbar Lordosis Lateral Angle (LLA) | Angle between the most prominent point of thoracic kyphosis and the deepest point of lumbar lordosis and the midpoint of the PSISs | |
| 13. PSISs Horizontal Alignment (PSISHA) | Angle between the two PSISs and the horizontal line | |
| 14. PSISs-Leg Angle (PSISLAL; PSISLAR) | Angle between the trochanter and popliteal fossa and the line of the two PSISs | |
| 15. Knee Lateral Angle (PKLAL; PKLAR) | Angle between the trochanter and the popliteal fossa and the posterior midpoint between the lateral and medial malleolus | |
| 16. Ankle Lateral Angle (ALAL; ALAR) | Angle between the popliteal fossa, the posterior midpoint between the lateral and the medial malleoli and the calcaneus | |
| 17. Acromion-PSIS Distance (APDL; APDR) | Distance between the acromion and the PSIS of the same side | |
| 18. Lower Limb Length (PLLLL; PLLLR) | Distance between the trochanter and the calcaneus of the same side | |
| Lateral | 19. Thoracic Kyphosis Curvature (TKCL; TKCR) | Angle between C7, the most prominent point of thoracic kyphosis and the deepest point of lumbar lordosis |
| 20. Lumbar Lordosis Curvature (LLCL; LLCR) | Angle between the most prominent point of thoracic kyphosis, the deepest point of lumbar lordosis and the PSIS | |
| 21. Pelvis–Leg Angle (PLAL; PLAR) | Angle between the line of the ASIS and the PSIS and the line of the trochanter and the lateral femoral condyle | |
| 22. Knee Angle (KAL; KAR) | Angle between the trochanter, the lateral femoral condyle and the lateral malleolus | |
| 23. Leg–Foot Angle (LFAL; LFAR) | Angle between the line of the trochanter and the lateral femoral condyle and the line of the calcaneus and the fifth metatarsal |
| Marker Size | Detection Rate |
|---|---|
| 40 mm—Ping-Pong Ball | 75.2% |
| 20 mm—Styrofoam Ball | 64.8% |
| Marker Color | Success Rate |
|---|---|
| White | 64.8% |
| Yellow | 89.9% |
| Orange | 95.4% |
| Red | 93.9% |
| Blue | 94.2% |
| Green | 96.7% |
| Age | Biological Gender (F/M) | Height (cm) | Weight (kg) |
|---|---|---|---|
| 20.9 ± 4.5 | 39/18 | 166.4 ± 9.3 | 69.4 ± 16.3 |
| ALLLL | PSISHA | |||
|---|---|---|---|---|
| Before removing the outliers | Mean ± Standard Deviation | Our Software | 68.65 ± 5.25 | 0.58 ± 2.72 |
| Contemplas | 68.62 ± 5.25 | 0.55 ± 2.70 | ||
| Values Range | Our Software | [58.35; 80.05] | [−9.90; 5.04] | |
| Contemplas | [58.5; 80.0] | [−9.8; 5.1] | ||
| p-Value | 0.058 | 0.047 | ||
| Statistically Significant α = 0.05/α = 0.1 | No/Yes | Yes/Yes | ||
| After removing the outliers | Mean ± Standard Deviation | Our Software | 68.64 ± 5.3 | -0.58 ± 2.76 |
| Contemplas | 68.62 ± 5.3 | -0.56 ± 2.74 | ||
| Values Range | Our Software | [58.35; 80.05] | [−9.9; 5.04] | |
| Contemplas | [58.5; 80.0] | [−9.8; 5.1] | ||
| p-Value | 0.01 | 0.02 | ||
| Statistically Significant α = 0.05/α = 0.1 | No/No | No/No | ||
| ALLLL | PSISHA | ||
|---|---|---|---|
| ΔL = −0.01 ΔU = 0.01 | p-Value | 0.89 | 0.91 |
| Statistically Significant /α = 0.1 | No/No | No/No | |
| ΔL = −0.05 ΔU = 0.05 | p-Value | 0.05 | 0.07 |
| Statistically Significant /α = 0.1 | No/Yes | No/Yes | |
| ΔL = −0.06 ΔU = 0.06 | p-Value | 0.01 | 0.02 |
| Statistically Significant /α = 0.1 | Yes/Yes | Yes/Yes |
| Train/Test Split Validation (70%Train/30%Test) | 10-Fold Cross-Validation | |||||||||||
| Multiclass | ||||||||||||
| LDA | k = 3 | k = 4 | k = 5 | k = 6 | k = 9 | LDA | k = 4 | k = 5 | k = 6 | k = 8 | k = 12 | |
| Accuracy | 50% | 55.56% | 55.56% | 55.56% | 55.56% | 61.11% | 56.14% | 59.65% | 59.65% | 57.89% | 59.65% | 56.14% |
| F1-Score “Without Evidence” | 36.36% | 53.33% | 53.33% | 53.33% | 53.33% | 66.67% | 43.75% | 58.82% | 57.89% | 57.89% | 57.89% | 58.82% |
| F1-Score “Mild Evidence” | 57.14% | 76.92% | 76.92% | 76.92% | 76.92% | 70.59% | 65.38% | 65.38% | 64% | 62.75% | 66.67% | 63.33% |
| F1-Score “Moderate/ Severe Evidence” | 54.55% | 25% | 25% | 25% | 25% | 28.57% | 53.33% | 50% | 53.85% | 48% | 48% | 30% |
| Binary—Level 1 | ||||||||||||
| LDA | k = 9 | k = 13 | k = 14 | k = 15 | k = 17 | LDA | k = 8 | k = 9 | k = 10 | k = 17 | k = 21 | |
| Accuracy | 72.22% | 77.78% | 77.78% | 77.78% | 83.33% | 77.78% | 63.16% | 77.19% | 77.19% | 77.19% | 77.19% | 77.19% |
| F1-Score “With Evidence” | 80% | 84.62% | 84.62% | 83.33% | 88.89% | 85.71% | 74.07% | 83.12% | 83.54% | 83.12% | 85.39% | 86.02% |
| F1-Score “Without Evidence” | 54.55% | 60% | 60% | 66.67% | 66.67% | 50% | 36.36% | 64.86% | 62.86% | 64.86% | 48% | 38.1% |
| Binary—Level 2 | ||||||||||||
| LDA | k = 6 | k = 7 | k = 9 | k = 10 | k = 11 | LDA | k = 3 | k = 4 | k = 5 | k = 6 | k = 9 | |
| Accuracy | 76.92% | 92.31% | 92.31% | 84.62% | 84.62% | 84.62% | 60.98% | 70.73% | 70.73% | 70.73% | 73.17% | 73.17% |
| F1-Score “Mild Evidence” | 84.21% | 94.74% | 94.74% | 90% | 90% | 90% | 69.23% | 76.92% | 79.31% | 78.57% | 81.36% | 81.36% |
| F1-Score “Moderate/ Severe Evidence” | 57.14% | 85.71% | 85.71% | 66.67% | 66.67% | 66.67% | 46.67% | 60% | 50% | 53.85% | 52.17% | 52.17% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neves, A.B.; Martins, R.; Matela, N.; Atalaia, T. PosturAll: A Posture Assessment Software for Children. Bioengineering 2023, 10, 1171. https://doi.org/10.3390/bioengineering10101171
Neves AB, Martins R, Matela N, Atalaia T. PosturAll: A Posture Assessment Software for Children. Bioengineering. 2023; 10(10):1171. https://doi.org/10.3390/bioengineering10101171
Chicago/Turabian StyleNeves, Ana Beatriz, Rodrigo Martins, Nuno Matela, and Tiago Atalaia. 2023. "PosturAll: A Posture Assessment Software for Children" Bioengineering 10, no. 10: 1171. https://doi.org/10.3390/bioengineering10101171
APA StyleNeves, A. B., Martins, R., Matela, N., & Atalaia, T. (2023). PosturAll: A Posture Assessment Software for Children. Bioengineering, 10(10), 1171. https://doi.org/10.3390/bioengineering10101171









