Internet Mindfulness Meditation Intervention (IMMI) Improves Depression Symptoms in Older Adults
Abstract
1. Introduction
2. Materials and Methods
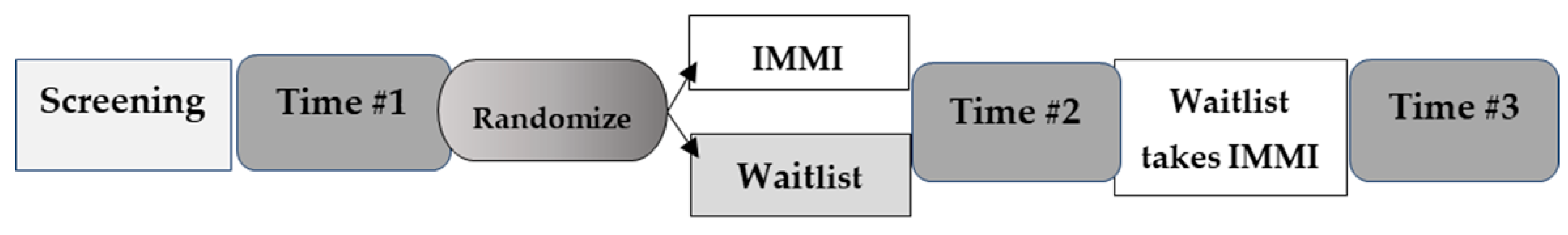
2.1. Study Overview
2.2. Participants
2.3. Procedures
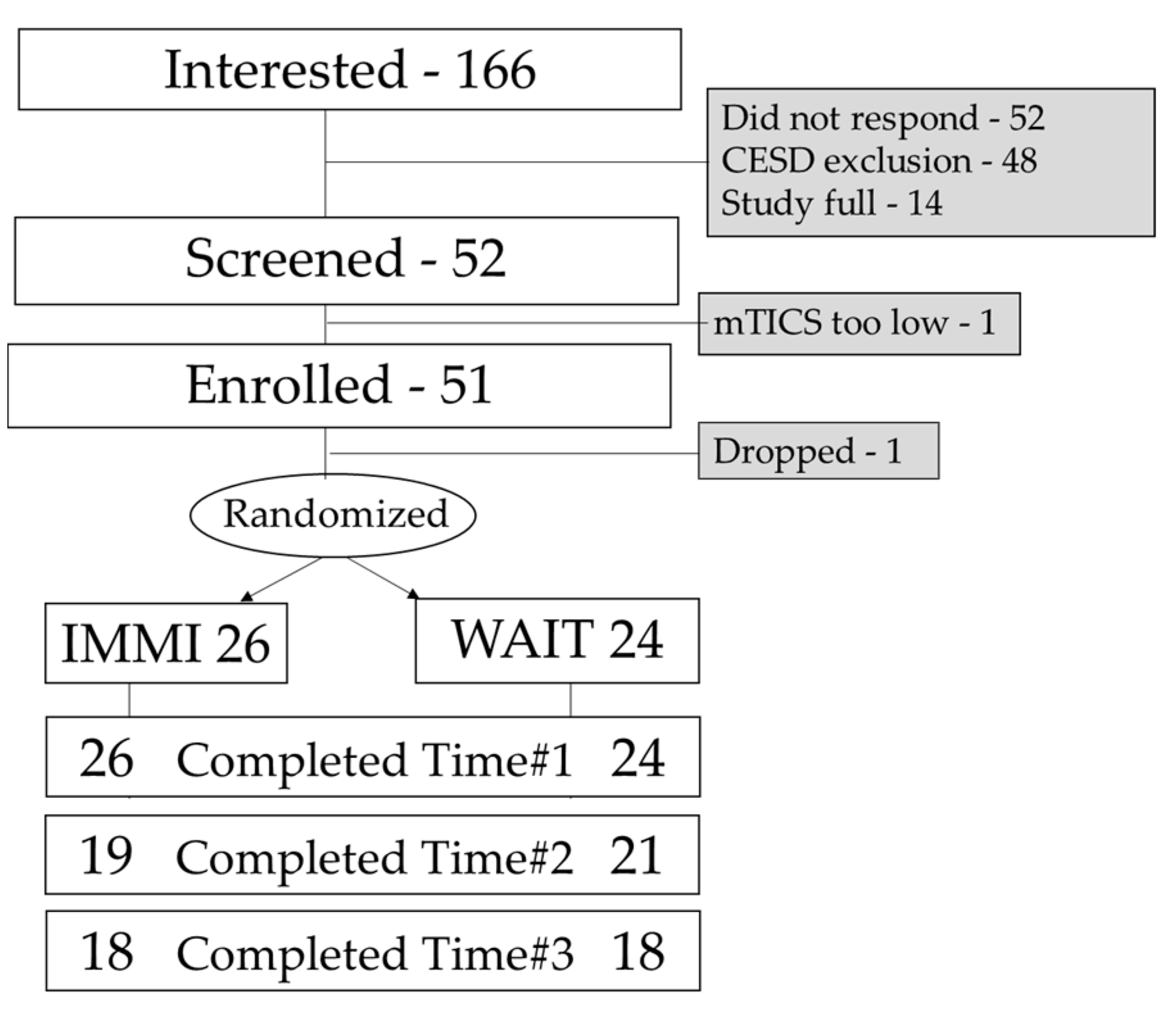
2.3.1. Recruitment
2.3.2. Screening
2.3.3. Time #1
2.3.4. Intervention Period
IMMI
Waitlist
2.3.5. Time #2 and #3
2.4. Measures (in Alphabetical Order)
2.5. Statistical Analysis
3. Results
3.1. Recruitment
3.2. Participant Characteristics
3.3. Adherence
3.4. Participant Satisfaction
“I was dealing with the death of my mother just before starting this program. I realized that I was angry with her and myself. I know that the mindful practices helped me to see this. I was able to give myself and my mother’s memories more gentleness and more of an open heart and mind. Thank you!”
“I had surgery in the middle of my time. I was very fortunate that I was in the program. I did continue to keep up my meditation practice, though I got behind on the written work …. I am very glad I was chosen to participate and thank you for what you are trying to achieve. I believe the results will play a big part in the lives of older people.”
“My father died with me at his side in a local hospital two or three weeks into this program (i.e., in the middle), and my family immediately informed me that his house, where I had been living, needed to be emptied, vacated, and placed for sale within a month and a half. This set of circumstances, along with an apparently missing will, contributed to a break for my participation in this program.”
“My mom was recently diagnosed with advanced cancer, so I felt sadder than my norm the past two weeks. My answers to some questions may reflect that. Although, I believe mindfulness has helped with this as well.”
“During the time of the study my sister-in-law died and my son’s non-cancerous brain tumor has returned, so the program was especially helpful in sitting with difficult situations and compassion meditation.”
“It helped me appreciate few feelings felt during meditation in the past, and look positively for meditation.”
“I have become more focused on what I am doing instead of operating on “automatic Pilot” as I did so much of the time.”
“I was so pleased with how the program had so many types of meditation to choose from and I found a couple that suited me and I am able to continue the practice on my own. The tools I learned have helped me immensely in redirecting my energies to a more positive and healthy direction. Thank you.”
“There was a noticeable decrease in depressing thoughts and stressful times.”
“I feel my sleep issues have greatly improved and I am very grateful to have been able to be a part of this study! Thank you!”
“Listening to the guided meditations has become an everyday practice.”
“I’m happy to have incorporated mediation into my daily life.”
“The program met my goal of exploring again the benefits of meditative practice”.
“It was my fault that I wasn’t able to participate as fully as I would have liked. But I did gain some tools and insights.”
“I am the worst participant ever. Such good intentions gone bad over Thanksgiving and Christmas with extensive travel and 11 grandchildren and severe flu throughout.”
“I’ve done a MBSR workshop series (in 2001), have read Full Catastrophe Living several times and used to meditate similar to this program. So, the training videos were boring to me. I was hoping for something less rudimentary but it helped me to be reminded of techniques I’ve not recalled and to have the structure to bring these back into my life. I had a friend from Holland visit week 5 and that was a big commitment that made me skip a few days of meditation. Is it necessary to have the woman in the video repeat simple info over and over? That was annoying. Then the workbook said the same thing w/o much more elaboration so I felt like it was geared to a child rather than an intelligent educated adult.”
“online program glitches and voice microphone issues, audio, programming glitches, some aspects of program can be improved”
“The program seems kind of jumbled up. Maybe there needs to be bullet points of all the things you are supposed to do in the week. Maybe it was just the fire which made it difficult to get all the work done. The program definitely needs some work, not too user friendly if the material is new to the participant.”
“I appreciate your efforts, it did not impress me and it was confusing at times.”
“good ideas, a few practices that have been useful, but the actual session were too cumbersome, too much narration, not a calming presentation. the amount of verbal content became work to listen to. most similar audio programs are more subtle, mellow, etc.”
3.5. Mood and Related Symptoms
4. Discussion
4.1. Summary
4.2. Patient Characteristics
4.3. Adherence
4.4. Participant Satisfaction
4.5. Mood and Related Outcomes
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Mitchell, P.B.; Harvey, S.B. Depression and the older medical patient—When and how to intervene. Maturitas 2014, 79, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Ellison, J.M.; Kyomen, H.H.; Harper, D.G. Depression in later life: An overview with treatment recommendations. Psychiatr. Clin. N. Am. 2012, 35, 203–229. [Google Scholar] [CrossRef] [PubMed]
- Oken, B.S.; Chamine, I.; Wakeland, W. A systems approach to stress, stressors and resilience in humans. Behav. Brain Res. 2015, 282, 144–154. [Google Scholar] [CrossRef] [PubMed]
- Aziz, R.; Steffens, D.C. What are the causes of late-life depression? Psychiatr. Clin. N. Am. 2013, 36, 497–516. [Google Scholar] [CrossRef] [PubMed]
- Wahbeh, H.; Elsas, S.M.; Oken, B.S. Mind-body interventions: Applications in neurology. Neurology 2008, 70, 2321–2328. [Google Scholar] [CrossRef] [PubMed]
- Goyal, M.; Singh, S.; Sibinga, E.M.; Gould, N.F.; Rowland-Seymour, A.; Sharma, R.; Berger, Z.; Sleicher, D.; Maron, D.D.; Shihab, H.M.; et al. Meditation Programs for Psychological Stress and Well-being: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2014. [Google Scholar] [CrossRef] [PubMed]
- Khoury, B.; Lecomte, T.; Fortin, G.; Masse, M.; Therien, P.; Bouchard, V.; Chapleau, M.A.; Paquin, K.; Hofmann, S.G. Mindfulness-based therapy: A comprehensive meta-analysis. Clin. Psychol. Rev. 2013, 33, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Chi, X.; Bo, A.; Liu, T.; Zhang, P.; Chi, I. Effects of Mindfulness-Based Stress Reduction on Depression in Adolescents and Young Adults: A Systematic Review and Meta-Analysis. Front. Psychol. 2018, 9, 1034. [Google Scholar] [CrossRef] [PubMed]
- MacKenzie, M.B.; Abbott, K.A.; Kocovski, N.L. Mindfulness-based cognitive therapy in patients with depression: Current perspectives. Neuropsychiatr. Dis. Treat. 2018, 14, 1599–1605. [Google Scholar] [CrossRef] [PubMed]
- Hazlett-Stevens, H.; Singer, J.; Chong, A. Mindfulness-Based Stress Reduction and Mindfulness-Based Cognitive Therapy with Older Adults: A Qualitative Review of Randomized Controlled Outcome Research. Clin. Gerontol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Wahbeh, H.; Svalina, M.N.; Oken, B.S. Group, One-on-One, or Internet? Preferences for Mindfulness Meditation Delivery Format and their Predictors. Open Med. J. 2014, 1, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Wahbeh, H.; Oken, B.S. Internet Mindfulness Meditation Intervention for the General Public: Pilot Randomized Controlled Trial. JMIR Ment. Health 2016, 3, e37. [Google Scholar] [CrossRef] [PubMed]
- Wahbeh, H.; Goodrich, E.; Oken, B.S. Internet mindfulness meditation for cognition and mood in older adults: A pilot study. Altern. Ther. Health Med. 2016, 22, 44–53. [Google Scholar] [PubMed]
- Neuendorf, R.; Wahbeh, H.; Chamine, I.; Yu, J.; Hutchison, K.; Oken, B.S. The Effects of Mind-Body Interventions on Sleep Quality: A Systematic Review. Evid. Based Complement. Altern. Med. 2015, 2015, 902708. [Google Scholar] [CrossRef] [PubMed]
- Kohout, F.J.; Berkman, L.F.; Evans, D.A.; Cornoni-Huntley, J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J. Aging Health 1993, 5, 179–193. [Google Scholar] [CrossRef] [PubMed]
- Welsh, K.A.; Breitner, J.C.; Magruder, K.M. Detection of dementia in the elderly using telephone screening of cognitive status. Neuropsychiatry Neuropsychol. Behav. Neurol. 1993, 6, 103–110. [Google Scholar]
- Brandt, J.; Welsh, K.A.; Breitner, J.C.; Folstein, M.F.; Helms, M.; Christian, J.C. Hereditary influences on cognitive functioning in older men. A study of 4000 twin pairs. Arch. Neurol. 1993, 50, 599–603. [Google Scholar] [CrossRef] [PubMed]
- Wahbeh, H.; Lane, J.B.; Goodrich, E.; Miller, M.; Oken, B.S. One-on-one Mindfulness Meditation Trainings in a Research Setting. Mindfulness (N. Y.) 2012, 5, 88–99. [Google Scholar] [CrossRef] [PubMed]
- Wahbeh, H.; Zwickey, H.; Oken, B.S. One method for objective adherence measurement in mind-body medicine. J. Altern. Complement. Med. 2011, 17, 175–177. [Google Scholar] [CrossRef] [PubMed]
- Attkisson, C.; Zwick, R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Eval. Program. Plan. 1982, 5, 233–237. [Google Scholar] [CrossRef]
- Idler, E.L.; Musick, M.A.; Ellison, C.G.; George, L.K.; Krause, N.; Ory, M.G.; Pargament, K.I.; Powell, L.H.; Underwood, L.G.; Williams, D.R. Measuring multiple dimensions of religion and spirituality for health research: Conceptual background and findings from the 1998 General Social Survey. Res. Aging 2003, 25, 327–365. [Google Scholar] [CrossRef]
- Fetzer Institute. Multidimensional Measurement of Religiousness/Spirituality for Use in Health Research: A Report of the Fetzer Institute/National Institute on Aging Working Group; John E. Fetzer Institute: Kalamazoo, MI, USA, 2003. [Google Scholar]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Amat, S.; Subhan, M.; Jaafar, W.M.W.; Mahmud, Z.; Johari, K.S.K. Evaluation and psychometric status of the brief resilience scale in a sample of Malaysian international students. Asian Soc. Sci. 2014, 10, 240. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Maljanian, R.; Goethe, J. Screening for depression in clinical practice: Reliability and validity of a five-item subset of the CES-Depression. Percept. Mot. Skills 2003, 97, 855–861. [Google Scholar] [CrossRef] [PubMed]
- Radloff, L.S. The CES-D scale: A self report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Baer, R.A.; Smith, G.T.; Lykins, E.; Button, D.; Krietemeyer, J.; Sauer, S.; Walsh, E.; Duggan, D.; Williams, J.M. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment 2008, 15, 329–342. [Google Scholar] [CrossRef] [PubMed]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Cleeland, C.S. Brief Pain Inventory—Short Form© Interactive Performance Technologies, LLC; Pain Research Group: Waltham, MA, USA, 1991. [Google Scholar]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 386–396. [Google Scholar] [CrossRef]
- Pocock, S.J.; Simon, R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics 1975, 31, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.; Xia, J.; Xu, D.; Gao, D.; Yan, Y. A generic minimization random allocation and blinding system on web. J. Biomed. Inform. 2006, 39, 706–719. [Google Scholar] [CrossRef] [PubMed]
- Benjamini, Y.; Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B (Methodol.) 1995, 57, 289–300. [Google Scholar]
- Center for Economic Development 2016 Sonoma County Economic and Demographic Profile. Available online: http://sonomaedb.org/WorkArea/DownloadAsset.aspx?id=2147520797 (accessed on 1 October 2018).
- Barnes, P.M.; Powell-Griner, E.; McFann, K.; Nahin, R.L. Complementary and alternative medicine use among adults: United States, 2002. Adv. Data 2004, 343, 1–19. [Google Scholar] [CrossRef]
- Parsons, C.E.; Crane, C.; Parsons, L.J.; Fjorback, L.O.; Kuyken, W. Home practice in Mindfulness-Based Cognitive Therapy and Mindfulness-Based Stress Reduction: A systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behav. Res. Ther. 2017, 95, 29–41. [Google Scholar] [CrossRef] [PubMed]
- Cavanagh, K.; Churchard, A.; O’Hanlon, P.; Mundy, T.; Votolato, P.; Jones, F.; Gu, J.; Strauss, C. A Randomised Controlled Trial of a Brief Online Mindfulness-Based Intervention in a Non-clinical Population: Replication and Extension. Mindfulness (N. Y.) 2018, 9, 1191–1205. [Google Scholar] [CrossRef] [PubMed]
- Pew Research Center. Technology Use Among Seniors. Available online: http://www.pewinternet.org/2017/05/17/technology-use-among-seniors/ (accessed on 1 October 2018).
- Oken, B.S.; Wahbeh, H.; Goodrich, E.; Klee, D.; Memmott, T.; Miller, M.; Fu, R. Meditation in Stressed Older Adults: Improvements in self-rated mental health not paralleled by improvements in cognitive function or physiological measures. Mindfulness (N. Y.) 2017, 8, 627–638. [Google Scholar] [CrossRef] [PubMed]
- Grecucci, A.; Pappaianni, E.; Siugzdaite, R.; Theuninck, A.; Job, R. Mindful Emotion Regulation: Exploring the Neurocognitive Mechanisms behind Mindfulness. Biomed. Res. Int. 2015, 2015, 670724. [Google Scholar] [CrossRef] [PubMed]
- Chiesa, A.; Anselmi, R.; Serretti, A. Psychological mechanisms of mindfulness-based interventions: What do we know? Holist. Nurs. Pract. 2014, 28, 124–148. [Google Scholar] [CrossRef] [PubMed]
- Garland, S.N.; Zhou, E.S.; Gonzalez, B.D.; Rodriguez, N. The Quest for Mindful Sleep: A Critical Synthesis of the Impact of Mindfulness-Based Interventions for Insomnia. Curr. Sleep Med. Rep. 2016, 2, 142–151. [Google Scholar] [CrossRef] [PubMed]
- Zeidan, F.; Adler-Neal, A.L.; Wells, R.E.; Stagnaro, E.; May, L.M.; Eisenach, J.C.; McHaffie, J.G.; Coghill, R.C. Mindfulness-Meditation-Based Pain Relief Is Not Mediated by Endogenous Opioids. J. Neurosci. 2016, 36, 3391–3397. [Google Scholar] [CrossRef] [PubMed]
- Zeidan, F.; Grant, J.A.; Brown, C.A.; McHaffie, J.G.; Coghill, R.C. Mindfulness meditation-related pain relief: Evidence for unique brain mechanisms in the regulation of pain. Neurosci. Lett. 2012, 520, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Gu, Q.; Hou, J.C.; Fang, X.M. Mindfulness Meditation for Primary Headache Pain: A Meta-Analysis. Chin. Med. J. (Engl.) 2018, 131, 829–838. [Google Scholar] [CrossRef] [PubMed]
- Hilton, L.; Hempel, S.; Ewing, B.A.; Apaydin, E.; Xenakis, L.; Newberry, S.; Colaiaco, B.; Maher, A.R.; Shanman, R.M.; Sorbero, M.E.; et al. Mindfulness Meditation for Chronic Pain: Systematic Review and Meta-analysis. Ann. Behav. Med. 2017, 51, 199–213. [Google Scholar] [CrossRef] [PubMed]
- Ball, E.F.; Nur Shafina Muhammad Sharizan, E.; Franklin, G.; Rogozinska, E. Does mindfulness meditation improve chronic pain? A systematic review. Curr. Opin. Obstet. Gynecol. 2017, 29, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Langer, N. The Importance of Spirituality in Later Life. Gerontol. Geriatr. Educ. 2000, 20, 41–50. [Google Scholar] [CrossRef]
- Hosseini, S.; Chaurasia, A.; Oremus, M. The Effect of Religion and Spirituality on Cognitive Function: A Systematic Review. Gerontologist 2017. [Google Scholar] [CrossRef] [PubMed]
- Oken, B.S. Placebo effect: Clinical perspectives and potential mechanisms. In Complementary Therapies in Neurology; Oken, B.S., Ed.; Parthenon Publishing Group: New York, NY, USA, 2004. [Google Scholar]
- Kinser, P.A.; Robins, J.L. Control group design: Enhancing rigor in research of mind-body therapies for depression. Evid. Based Complement. Altern. Med. 2013, 2013, 140467. [Google Scholar] [CrossRef] [PubMed]
| Variable | IMMI (n = 26) | Waitlist (n = 24) | Statistics |
|---|---|---|---|
| Age | 48.6 ± 6.1 | 46.9 ± 6.3 | F(1, 49) = 0.95, p = 0.34 |
| Gender (Female) | 21 (81%) | 19 (79%) | X2 = 0.02, p = 0.89 |
| Race (Caucasian) | 21 (81%) | 21 (88%) | X2 = 1.92, p = 0.75 |
| Relationship Couple | 13 (62%) | 8 (33%) | X2 = 3.98, p = 0.05 |
| Single | 10 (38%) | 16 (67%) | |
| Education (years) | 16.7 ± 2.9 | 16.7 ± 2.5 | F(1, 49) = 0.00, p = 0.97 |
| Income $0–24,999 | 5 (19%) | 6(25%) | X2 = 5.6, p = 0.20 |
| 25,000–49,999 | 3 (12%) | 6(25%) | |
| 50,000–74,999 | 4 (15%) | 2 (8%) | |
| 75,000–99,999 | 3 (12%) | 6 (25%) | |
| 100,000 & up | 11 (42%) | 4 (17%) | |
| Depression | 20.23 ± 7.8 | 22.5 ± 6.6 | F(1, 49) = 1.18, p = 0.28 |
| mTICS | 38.2 ± 3.8 | 39.9 ± 3.5 | F(1, 49) = 2.11, p = 0.16 |
| Outcome | IMMI | Waitlist | Statistics | ||
|---|---|---|---|---|---|
| Time #1 | Time #2 | Time #1 | Time #2 | ||
| Depression | 20.2 ± 7.8 | 15.1 ± 6.3 | 22.5 ± 6.6 | 22.5 ± 6.1 | F(1, 39) = 13.6, p < 0.00005 * |
| Perceived Stress | 19.0 ± 6.2 | 13.4 ± 5.2 | 20.4 ± 5.0 | 19.0 ± 5.0 | F(1, 39) = 13.58, p = 0.0007 * |
| Sleep Disturbance | 13.3 ± 6.3 | 9.3 ± 6.0 | 12.3 ± 4.5 | 12.9 ± 4.4 | F(1, 39) = 13.15, p = 0.0009 * |
| Mindfulness | 3.1 ± 0.4 | 3.0 ± 0.4 | 3.0 ± 0.3 | 3.1 ± 0.3 | F(1, 39) = 1.19, p = 0.28 |
| Pain Interference | 2.5 ± 2.6 | 1.4 ± 1.7 | 2.1 ± 1.7 | 1.5 ± 1.5 | F(1, 39) = 2.49, p = 0.12 |
| Pain Severity | 2.3 ± 1.9 | 1.2 ± 1.7 | 1.7 ± 1.3 | 1.8 ± 1.4 | F(1, 39) = 4.31, p = 0.05 * |
| Resilience | 2.0 ± 0.3 | 2.1 ± 0.3 | 2.1 ± 0.2 | 2.1 ± 0.3 | F(1, 39) = 0.55, p = 0.46 |
| Spirituality | 23.0 ± 7.5 | 24.6 ± 8.2 | 19.1 ± 6.8 | 19.8 ± 7.5 | F(1, 39) = 1.87, p = 0.18 |
| Outcome | Before | After | Statistics |
|---|---|---|---|
| Depression | 22.8 ± 5 | 18.7 ± 6.6 | t(37) = 4.6, p = 0.0001 * |
| Perceived Stress | 19 ± 5.7 | 14.1 ± 6 | t(37) = 4.27, p = 0.0001 * |
| Sleep Disturbance | 13.1 ± 5.5 | 8.3 ± 5.8 | t(37) = 5.63, p < 0.00005 * |
| Mindfulness | 3.1 ± 0.3 | 3.0 ± 0.3 | z(37) = 1.52, p = 0.13 |
| Pain Interference | 2.1 ± 2.2 | 1.4 ± 1.8 | z(37) = 2.95, p = 0.003 * |
| Pain Severity | 2.1 ± 1.7 | 1.5 ± 1.7 | z(37) = 1.74, p = 0.08 |
| Resilience | 2.0 ± 0.3 | 2.1 ± 0.2 | z(37) = −1.12, p = 0.27 |
| Spirituality | 21.6 ± 7.6 | 23.4 ± 8.4 | t(37) = −2.47, p = 0.018 * |
| Outcome | Time #1 (n = 26) | Time #2 (n = 19) | Time #3 (n = 18) | Statistics |
|---|---|---|---|---|
| Depression | 22.5 a ± 5.7 a | 18.5 a ± 5.2 | 18.6 ± 8.9 a | F(2, 62) = 5.95, p < 0.00005 * |
| Perceived Stress | 19.0 d ± 6.2 d | 13.4 d ± 5.2 | 11.9 ± 6.1 d | F(2, 62) = 23.3, p < 0.00005 * |
| Sleep Disturbance | 13.3 b ± 6.3 b | 9.3 b ± 6.0 | 9.3 ± 6.3 b | F(2, 62) = 9.22, p = 0.0006 * |
| Mindfulness | 3.1 ± 0.4 | 3.0 ± 0.4 | 3.0 ± 0.4 | F(2, 62) = 0.88, p = 0.42 |
| Pain Interference | 2.5 b ± 2.6 | 1.4 b ± 1.7 | 1.8 ± 2.5 | F(2, 62) = 4.83, p = 0.01 * |
| Pain Severity | 2.3 ± 1.9 | 1.2 ± 1.7 | 1.8 ± 2.7 | F(2, 62) = 2.63, p = 0.09 |
| Resilience | 2.0 ± 0.3 | 2.1 ± 0.3 | 1.9 ± 0.3 | F(2, 62) = 3.05, p = 0.06 |
| Spirituality | 23.0 b ± 7.5 | 24.6 ± 8.2 | 25.8 b ± 7.4 | F(2, 62) = 5.29, p = 0.0098 * |
© 2018 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wahbeh, H. Internet Mindfulness Meditation Intervention (IMMI) Improves Depression Symptoms in Older Adults. Medicines 2018, 5, 119. https://doi.org/10.3390/medicines5040119
Wahbeh H. Internet Mindfulness Meditation Intervention (IMMI) Improves Depression Symptoms in Older Adults. Medicines. 2018; 5(4):119. https://doi.org/10.3390/medicines5040119
Chicago/Turabian StyleWahbeh, Helané. 2018. "Internet Mindfulness Meditation Intervention (IMMI) Improves Depression Symptoms in Older Adults" Medicines 5, no. 4: 119. https://doi.org/10.3390/medicines5040119
APA StyleWahbeh, H. (2018). Internet Mindfulness Meditation Intervention (IMMI) Improves Depression Symptoms in Older Adults. Medicines, 5(4), 119. https://doi.org/10.3390/medicines5040119




