Effectiveness of Raw, Natural Medical Cannabis Flower for Treating Insomnia under Naturalistic Conditions
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Outcomes
2.3. Statistical Analysis
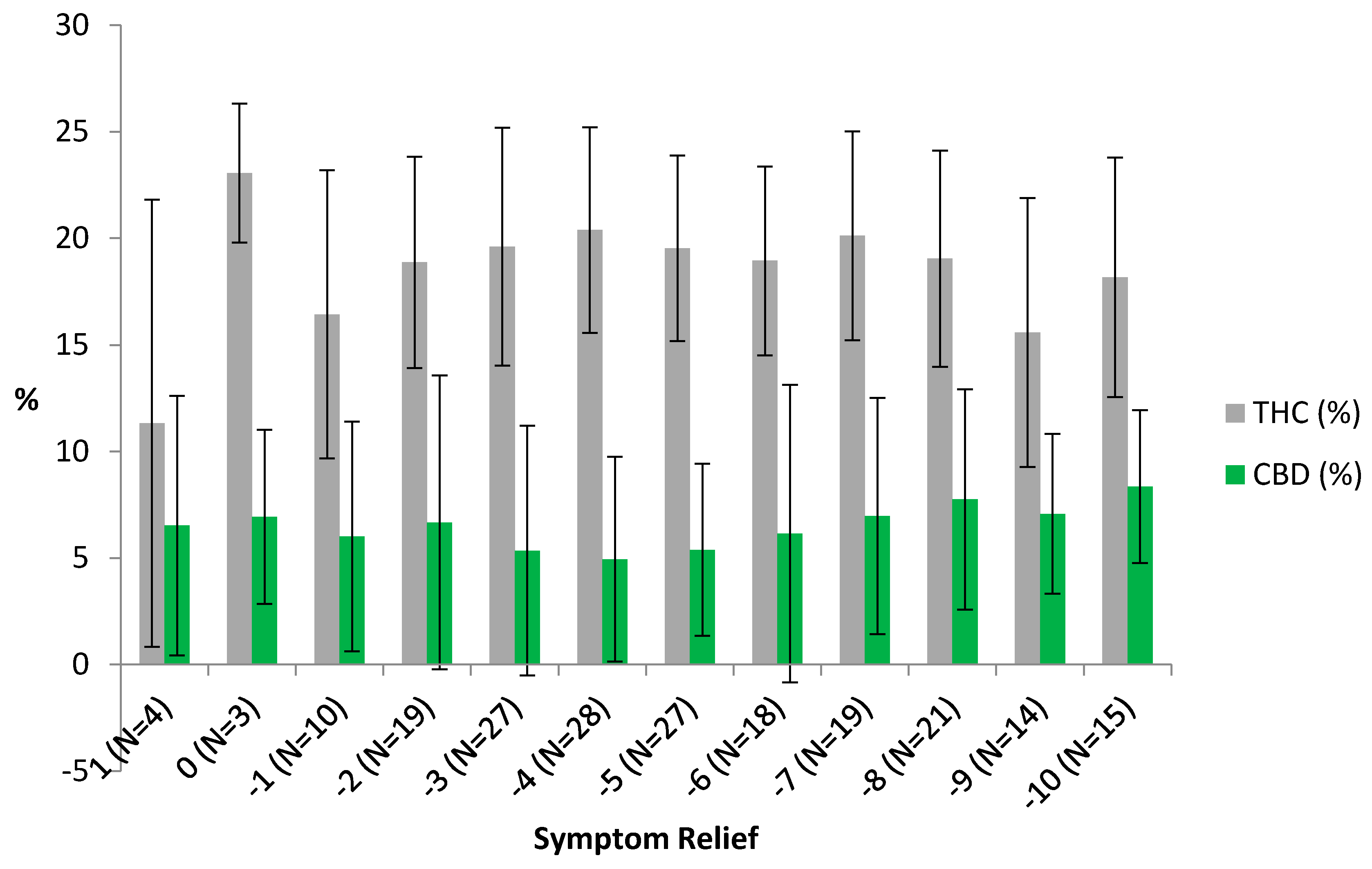
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Abraham, O.; Pu, J.; Schleiden, L.J.; Albert, S.M. Factors contributing to poor satisfaction with sleep and healthcare seeking behavior in older adults. Sleep Health 2017, 3, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control. Available online: https://www.cdc.gov/sleep/data_statistics.html (accessed on 15 March 2018).
- Ellis, J.G.; Perlis, M.L.; Neale, L.F.; Espie, C.A.; Bastien, C.H. The natural history of insomnia: Focus on prevalence and incidence of acute insomnia. J. Psychiatr. Res. 2012, 46, 1278–1285. [Google Scholar] [CrossRef] [PubMed]
- Ohayon, M.M. Epidemiology of insomnia: What we know and what we still need to learn. Sleep Med. Rev. 2002, 6, 97–111. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.; Youn, S.; Yi, K.; Park, B.; Lee, S. Sleeping pill administration time and patient subjective satisfaction. J. Clin. Sleep Med. 2016, 12, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Morin, C.M.; Benca, R. Chronic insomnia. Lancet 2012, 379, 1129–1141. [Google Scholar] [CrossRef]
- Fitzgerald, T.; Vietri, J. Residual effects of sleep medications are commonly reported and associated with impaired patient-reported outcomes among insomnia patients in the United States. Sleep Disord. 2015, 2015, 607148. [Google Scholar] [CrossRef] [PubMed]
- Auld, F.; Maschauer, E.L.; Morrison, I.; Skene, D.J.; Riha, R.L. Evidence for the efficacy of melatonin in the treatment of primary adult sleep disorders. Sleep Med. Rev. 2017, 34, 10–22. [Google Scholar] [CrossRef] [PubMed]
- Bent, S.; Padula, A.; Moore, D.; Patterson, M.; Mehling, W. Valerian for Sleep: A Systematic Review and Meta-Analysis. Am. J. Med. 2006, 119, 1005–1012. [Google Scholar] [CrossRef] [PubMed]
- Pragst, F.; Herre, S.; Bakdash, A. Poisonings with diphenhydramine—A survey of 69 clinical and 55 death cases. Forensic Sci. Int. 2006, 161, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Radovanovic, D.; Meier, P.J.; Guirguis, M.; Lorent, J.P.; Kupferscchmidt, H. Dose-dependent toxicity of diphenhydramine overdose. Hum. Exp. Toxicol. 2000, 19, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Gray, S.L.; Anderson, M.L.; Dublin, S.; Hanlon, J.T.; Hubbard, R.; Walker, R.; Yu, O.; Crane, P.K.; Larson, E.B. Cumulative Use of Strong Anticholinergics and Incident Dementia A Prospective Cohort Study. JAMA Intern. Med. 2015, 175, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Bonn-Miller, M.O.; Babson, K.A.; Vandrey, R. Using cannabis to help you sleep: Heightened frequency of medical cannabis use among those with PTSD. Drug Alcohol Depend. 2014, 136, 162–165. [Google Scholar] [CrossRef] [PubMed]
- Bradford, A.C.; Bradford, W.D. Medical marijuana laws reduce prescription medication use in Medicare Part D. Health Aff. 2016, 35, 1230–1236. [Google Scholar] [CrossRef] [PubMed]
- Piper, B.J. Substitution of medical cannabis for pharmaceutical agents for pain, anxiety, and sleep. J. Psychopharmacol. 2017, 31, 569–575. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on the Health Effects of Marijuana. An Evidence Review and Research Agenda. In The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research; National Academies Press: Washington, DC, USA, 2017. [Google Scholar]
- Babson, K.A. Cannabis, Cannabinoids, and Sleep: A Review of the Literature. Curr. Psychiatry Rep. 2017, 19, 23. [Google Scholar] [CrossRef] [PubMed]
- Chagas, M.H.N.; Eckeli, A.L.; Zuardi, A.W.; Pena-Pereira, M.A.; Sobreira-Neto, M.A.; Sobreira, E.T.; Camilo, M.R.; Bergamaschi, M.M.; Schenck, C.H.; Hallak, J.E.C.; et al. Cannabidiol can improve complex sleep-related behaviours associated with rapid eye movement sleep behaviour disorder in Parkinson’s disease patients: A case series. J. Clin. Pharm. Ther. 2014, 39, 564–566. [Google Scholar] [CrossRef] [PubMed]
- Feinberg, I.; Jones, R.; Walker, J.M.; Cavness, C.; March, J. Effects of high dosage delta-9-tetrahydrocannabinol on sleep patterns in man. Clin. Pharmacol. Ther. 1975, 17, 458–466. [Google Scholar] [CrossRef] [PubMed]
- Gates, P.J.; Albertella, L.; Copeland, J. The effects of cannabinoid administration on sleep: A systematic review of human studies. Sleep Med. Rev. 2014, 18, 477–487. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, A.N.; Turner, C.; Stone, B.M.; Robson, P.J. Effect of Delta-9-tetrahydrocannabinol and cannabidiol on nocturnal sleep and early-morning behavior in young adults. J. Clin. Psychopharmacol. 2004, 24, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.F.; Wolff, R.F.; Deshpande, S.; Nisio, M.D.; Duffy, S.; Hernandez, A.V.; Keurentjes, J.C.; Lang, S.; Misso, K.; Ryder, S.; et al. Cannabinoids for Medical Use: A Systematic Review and Meta-analysis. JAMA 2015, 313, 2456–2473. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.D.; Takeshi, S.; Rainero, I.; Maj, M.C.; Kukkonen, J.P. Orexin receptor multimerization versus functional interactions: Neuropharmacological implications for opioid and cannabinoid signalling and pharmacogenetics. Pharmaceuticals 2017, 10, 79. [Google Scholar] [CrossRef] [PubMed]
- Stith, S.S.; Vigil, J.M.V. Federal barriers to Cannabis research. Science 2016, 352, 1182. [Google Scholar] [CrossRef] [PubMed]
- Releaf App. Available online: https://Releaf®appcom/ (accessed on 18 April 2018).
- Mintel. OTC Sleep Aids US, MARCH 2017. 2017. Available online: http://academic.mintel.com.libproxy.unm.edu/sinatra/oxygen_academic/attachment/id=793087&seq=1 (accessed on 15 March 2018).
- Belendiuk, K.A.; Babson, K.A.; Vandrey, R.; Bonn-Miller, M.O. Cannabis types and cannabinoid concentration preference among sleep-disturbed medicinal cannabis users. Addict. Behav. 2015, 50, 178–181. [Google Scholar] [CrossRef] [PubMed]
- Fontanella, C.A.; Campo, J.V.; Phillips, G.S.; Hiance-Steelesmith, D.L.; Sweeney, H.A.; Tam, K.; Lehrer, D.; Klein, R.; Hurst, M. Benzodiazepine use and risk of mortality among patients with schizophrenia: A retrospective longitudinal study. J. Clin. Psychiatry 2016, 77, 661–667. [Google Scholar] [CrossRef] [PubMed]
- Nakafero, G.; Sanders, R.D.; Nguyen-Van-Tam, J.S.; Myles, P.R. The association between benzodiazepines and influenza-like illness-related pneumonia and mortality: A survival analysis using UK Primary Care data. Pharmacoepidemiol. Drug Saf. 2016, 25, 1263–1273. [Google Scholar] [CrossRef] [PubMed]
- Weich, S.; Pearce, H.L.; Croft, P.; Singh, S.; Crome, I.; Bashford, J.; Frisher, M. Effect of anxiolytic and hypnotic drug prescriptions on mortality hazards: Retrospective cohort study. Bmj 2014. [Google Scholar] [CrossRef] [PubMed]
- Śledziński, P.; Zeyland, J.; Słomski, R.; Nowak, A. The current state and future perspectives of cannabinoids in cancer biology. Cancer Med. 2018, 7, 765–775. [Google Scholar] [CrossRef] [PubMed]
- Burstein, S. Cannabidiol (CBD) and its analogs: A review of their effects on inflammation. Bioorg. Med. Chem. 2015, 23, 1377–1385. [Google Scholar] [CrossRef] [PubMed]
- McPartland, J.M.; Duncan, M.; Di Marzo, V.; Pertwee, R.G. Are cannabidiol and Δ9-tetrahydrocannabivarin negative modulators of the endocannabinoid system? A systematic review. Br. J. Pharmacol. 2015, 172, 737–753. [Google Scholar] [CrossRef] [PubMed]
- Norman, J.; Anderson, S. Novel class of medications, orexin receptor antagonists, in the treatment of insomnia—Critical appraisal of suvorexant. Nat. Sci. Sleep 2016, 8, 239–247. [Google Scholar] [PubMed]
- Scammell, T.; Winrow, C. Orexin receptors: Pharmacology and therapeutic opportunities. Annu. Rev. Pharmacol. Toxicol. 2011, 51, 243–266. [Google Scholar] [CrossRef] [PubMed]
- Flores, Á.; Julià-Hernández, M.; Maldonado, R.; Berrendero, F.; Flores, Á.; Julià-Hernández, M. Involvement of the orexin/hypocretin system in the pharmacological effects induced by Δ(9)-tetrahydrocannabinol. Br. J. Pharmacol. 2016, 173, 1381–1392. [Google Scholar] [CrossRef] [PubMed]
- Pertwee, R.G. The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: Δ9-tetrahydrocannabinol, cannabidiol and Δ9-tetrahydrocannabivarin. Br. J. Pharmacol. 2008, 153, 199–215. [Google Scholar] [CrossRef] [PubMed]
- Bonn-Miller, M.O.; Loflin, M.J.E.; Thomas, B.F.; Marcu, J.P.; Hyke, T.; Vandrey, R. Labeling accuracy of cannabidiol extracts sold online. JAMA 2017, 318, 1708–1709. [Google Scholar] [CrossRef] [PubMed]
- Haroutounian, S.; Ratz, Y.; Ginosar, Y.; Furmanov, K.; Saifi, F.; Meidan, R.; Davidson, E. The effect of medicinal cannabis on pain and quality-of-life outcomes in chronic pain: A prospective open-label study. Clin. J. Pain 2016, 32, 1036–1043. [Google Scholar] [CrossRef] [PubMed]
- Stith, S.S.; Vigil, J.M.; Adams, I.M.; Reeve, A.P. Effects of legal access to cannabis on Scheduled II-V drug prescriptions. J. Am. Med. Dir. Assoc. 2018, 19, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Vigil, J.M.; Stith, S.S.; Adams, I.M.; Reeve, A.P. Associations between medical cannabis and prescription opioid use in chronic pain patients: A preliminary cohort study. PLoS ONE 2017, 12, e0187795. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean | Std. Dev | Minimum | Maximum |
|---|---|---|---|---|
| Panel A: Subtypes (983 sessions, 378 users) | ||||
| Hybrid | 0.33 | 0.47 | 0 | 1 |
| C. indica | 0.60 | 0.49 | 0 | 1 |
| C. sativa | 0.06 | 0.24 | 0 | 1 |
| Panel B: Combustion Method (996 sessions, 385 users) | ||||
| Joint | 0.13 | 0.34 | 0 | 1 |
| Pipe | 0.38 | 0.48 | 0 | 1 |
| Vape | 0.49 | 0.50 | 0 | 1 |
| Panel C: THC (353 sessions, 143 users) | ||||
| % THC | 0.19 | 0.54 | 0.02 | 0.35 |
| THC < 10% | 0.05 | 0.22 | 0 | 1 |
| THC 10–19% | 0.50 | 0.50 | 0 | 1 |
| THC 20–34% | 0.45 | 0.50 | 0 | 1 |
| Panel D: CBD (119 sessions, 281 users) | ||||
| % CBD | 0.60 | 0.54 | 0 | 0.30 |
| CBD 0% | 0.19 | 0.39 | 0 | 1 |
| CBD 1–9% | 0.51 | 0.50 | 0 | 1 |
| CBD 10–34% | 0.30 | 0.46 | 0 | 1 |
| Panel E: Outcome and Control Variables (1056 sessions, 409 users) | ||||
| Symptom Change | −4.5 | 2.7 | −10 | 9 |
| Starting Symptom Level | 6.6 | 2.1 | 1 | 10 |
| Ending Symptom Level | 2.2 | 2.1 | 0 | 10 |
| Panel F: Side Effects (1215 sessions, 359 users) | ||||
| Any Negative Side Effect | 0.57 | 0.50 | 0 | 1 |
| % of Negative Side Effects | 0.10 | 0.13 | 0 | 1 |
| Any Positive Side Effect | 0.95 | 0.23 | 0 | 1 |
| % of Positive Side Effects | 0.21 | 0.15 | 0 | 1 |
| Any Context-Specific Side Effect | 0.86 | 0.35 | 0 | 1 |
| % of Context-Specific Side Effects | 0.24 | 0.19 | 0 | 1 |
| Variable | (1) | (2) | (3) | (4) |
|---|---|---|---|---|
| Panel A: Subtypes, omitted category = hybrid | ||||
| C. indica | −0.227 | 0.176 | ||
| (0.214) | (0.220) | |||
| C. sativa | −0.214 | 2.481 * | ||
| (0.492) | (1.445) | |||
| Panel B: Combustion Method, omitted category = joint | ||||
| Pipe | −0.715 | −1.686 ** | ||
| (0.563) | (0.758) | |||
| Vape | −0.823 | −1.560 ** | ||
| (0.583) | (0.782) | |||
| Panel C: THC and CBD | ||||
| THC (%) | −4.759 | −4.280 | ||
| (2.978) | (3.761) | |||
| CBD (%) | −3.828 *** | −5.232 * | ||
| (1.121) | (2.841) | |||
| Starting Symptom Level | −0.763 *** | −0.781 *** | −0.951 *** | −0.873 *** |
| (0.058) | (0.056) | (0.095) | (0.092) | |
| Constant | 0.603 * | 1.318 ** | 2.599 *** | 3.100 *** |
| (0.362) | (0.617) | (0.920) | (1.115) | |
| Observations | 983 | 996 | 205 | 195 |
| R-squared | 0.341 | 0.337 | 0.562 | 0.613 |
| Number of users | 378 | 385 | 90 | 83 |
| Variable | (1) | (2) | (3) | (4) | (5) | (6) |
|---|---|---|---|---|---|---|
| Negative | % of Negative | Positive | % of Positive | Context-Specific | % of Context-Specific | |
| C. indica | −0.034 | 0.001 | 0.037 | −0.035 ** | −0.004 | −0.013 |
| (0.026) | (0.011) | (0.036) | (0.015) | (0.039) | (0.022) | |
| C. sativa | 0.478 *** | 0.105 *** | −0.349 | −0.002 | −0.236 | −0.018 |
| (0.152) | (0.028) | (0.277) | (0.088) | (0.309) | (0.131) | |
| Pipe | −0.042 | −0.044 | 0.025 | 0.116 ** | 0.917 *** | 0.252 *** |
| (0.122) | (0.038) | (0.022) | (0.050) | (0.075) | (0.050) | |
| Vape | −0.484 *** | −0.067 * | 0.034 | 0.135 *** | 0.993 *** | 0.248 *** |
| (0.144) | (0.037) | (0.026) | (0.049) | (0.083) | (0.063) | |
| THC (%) | −0.136 | −0.002 | 0.031 | −0.200 | 0.808 | 0.506 |
| (0.810) | (0.093) | (0.077) | (0.304) | (0.586) | (0.455) | |
| CBD (%) | 0.525 | 0.239 | 0.163 | −0.008 | −1.101 ** | −0.006 |
| (1.263) | (0.159) | (0.142) | (0.154) | (0.496) | (0.241) | |
| Starting Symptom Level | 0.074 *** | 0.012 *** | −0.002 | 0.012 *** | 0.030 | 0.004 |
| (0.025) | (0.004) | (0.002) | (0.004) | (0.021) | (0.009) | |
| Constant | 0.388 | 0.035 | 0.955 *** | 0.084 | −0.297 * | −0.105 |
| (0.329) | (0.055) | (0.035) | (0.092) | (0.155) | (0.096) | |
| Observations | 170 | 170 | 170 | 170 | 170 | 170 |
| R-squared | 0.128 | 0.165 | 0.382 | 0.123 | 0.355 | 0.101 |
| N Users | 70 | 70 | 70 | 70 | 70 | 70 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vigil, J.M.; Stith, S.S.; Diviant, J.P.; Brockelman, F.; Keeling, K.; Hall, B. Effectiveness of Raw, Natural Medical Cannabis Flower for Treating Insomnia under Naturalistic Conditions. Medicines 2018, 5, 75. https://doi.org/10.3390/medicines5030075
Vigil JM, Stith SS, Diviant JP, Brockelman F, Keeling K, Hall B. Effectiveness of Raw, Natural Medical Cannabis Flower for Treating Insomnia under Naturalistic Conditions. Medicines. 2018; 5(3):75. https://doi.org/10.3390/medicines5030075
Chicago/Turabian StyleVigil, Jacob M., Sarah S. Stith, Jegason P. Diviant, Franco Brockelman, Keenan Keeling, and Branden Hall. 2018. "Effectiveness of Raw, Natural Medical Cannabis Flower for Treating Insomnia under Naturalistic Conditions" Medicines 5, no. 3: 75. https://doi.org/10.3390/medicines5030075
APA StyleVigil, J. M., Stith, S. S., Diviant, J. P., Brockelman, F., Keeling, K., & Hall, B. (2018). Effectiveness of Raw, Natural Medical Cannabis Flower for Treating Insomnia under Naturalistic Conditions. Medicines, 5(3), 75. https://doi.org/10.3390/medicines5030075





