A Review of Evidence for a Therapeutic Application of Traditional Japanese Kampo Medicine for Oral Diseases/Disorders
Abstract
1. Introduction
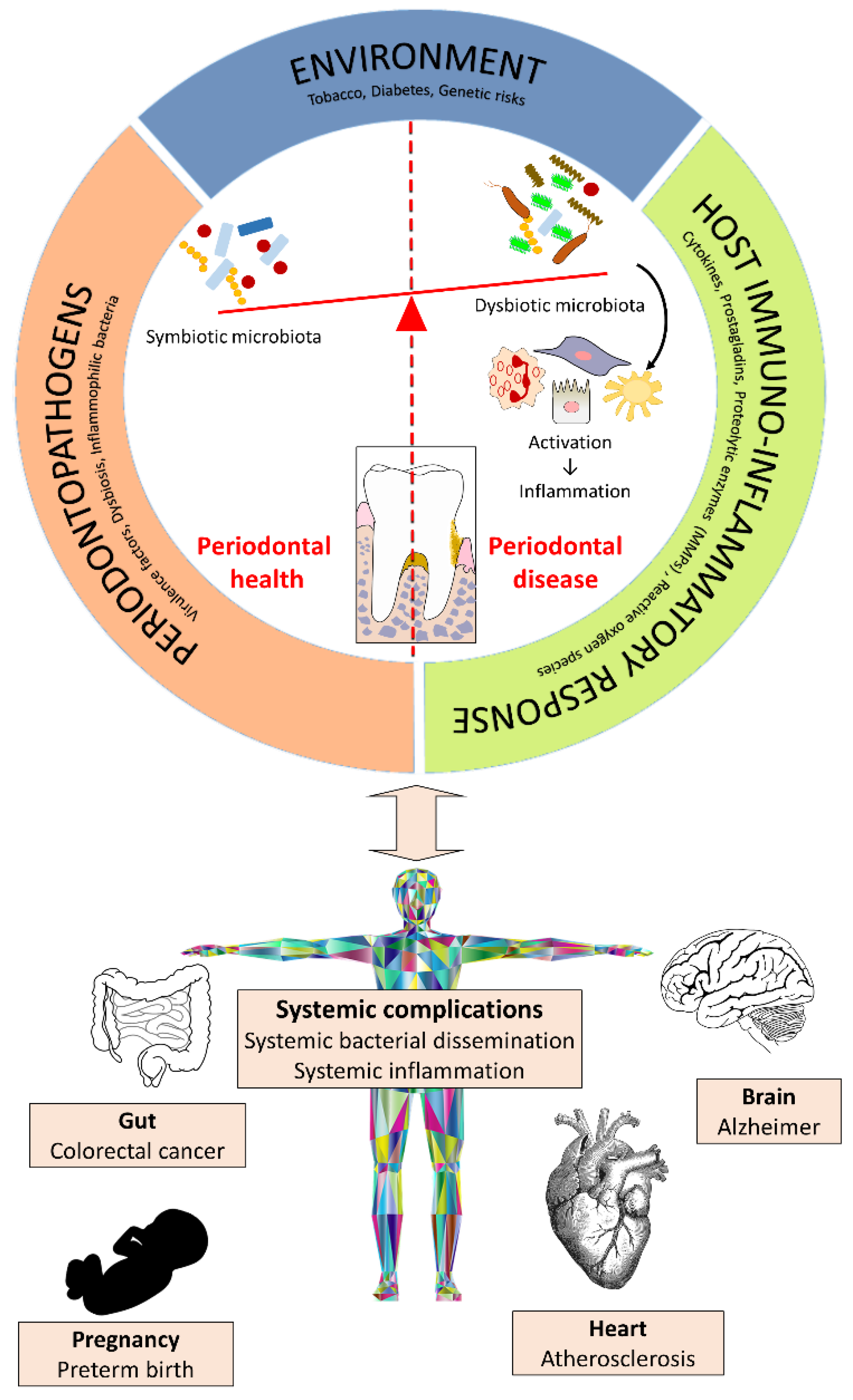
2. Kampo Medicines and Periodontal Disease
2.1. Effect on Periodontopathogenic Bacteria
2.2. Effect on the Host Inflammatory Response and Bone Resorption
2.3. Effect on Wound Healing
2.4. Effect on the Innate Immunity of Epithelial Cells
3. Kampo Medicines and Oral Mucositis
4. Kampo Medicines and Xerostomia
5. Kampo Medicines and Drug-Induced Gingival Overgrowth
6. Conclusions
Acknowledgments
Conflicts of Interest
References
- Motoo, Y.; Seki, T.; Tsutani, K. Traditional Japanese medicine, Kampo: Its history and current status. Chin. J. Integr. Med. 2011, 17, 85–87. [Google Scholar] [CrossRef] [PubMed]
- Yu, F.; Takahashi, T.; Moriya, J.; Kawaura, K.; Yamakawa, J.; Kusaka, K.; Itoh, T.; Morimoto, S.; Yamaguchi, N.; Kanda, T. Traditional Chinese medicine and Kampo: A review from the distant past for the future. J. Int. Med. Res. 2006, 34, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Ono, N. Medical insurance in Japan. J. Kampo Acupunct. Integr. Med. 2005, 1, 70–84. [Google Scholar]
- Tsuruoka, K.; Tsuruoka, Y.; Kajii, E. Complementary medicine education in Japanese medical schools: A survey. Complement. Ther. Med. 2001, 9, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, K.; Matsuura, K.; Gao, P.; Hottenbacher, L.; Tokunaga, H.; Nishimura, K.; Imazu, Y.; Reissenweber, H.; Witt, C.M. Traditional Japanese Kampo medicine: Clinical research between modernity and traditional medicine—The state of research and methodological suggestions for the future. Evid. Based Complement. Altern. Med. 2011, 2011, 513842. [Google Scholar] [CrossRef] [PubMed]
- Yamada, K. Quality of life in patients treated with Kampo medicine: A complementary alternative to modern medicine. J. Altern. Complement. Med. 2006, 12, 799–803. [Google Scholar] [CrossRef] [PubMed]
- Japanese Ministry of Health, Labour and Welfare. The Japanese Pharmacopoeia, 15th ed.; Pharmaceuticals and Medical Devices Agency: Tokyo, Japan, 2006.
- Saito, H. Regulation of herbal medicines in Japan. Pharmacol. Res. 2000, 41, 515–519. [Google Scholar] [CrossRef] [PubMed]
- Keisetsu, O. Kampo: A Clinical Guide to Theory and Practice; Churchill Livingstone Elsevier: London, UK, 2010; 164p. [Google Scholar]
- Goto, S. Manufacturing process for the prescriptions of Kampo Medicine. J. Kampo Acupunct. Integr. Med. 2005, 1, 51–55. [Google Scholar]
- Yasui, H. Clinical applications of Kampo Medicine. J. Kampo Acupunct. Integr. Med. 2005, 1, 15–50. [Google Scholar]
- Larsen, T.; Fiehn, N.E. Dental biofilm infections—An update. APMIS 2017, 125, 376–384. [Google Scholar] [CrossRef] [PubMed]
- Pihlstrom, B.L.; Michalowicz, B.S.; Johnson, N.W. Periodontal diseases. Lancet 2005, 366, 1809–1820. [Google Scholar] [CrossRef]
- Berezow, A.B.; Darveau, R.O. Microbial shift and periodontitis. Periodontol. 2000 2011, 55, 36–47. [Google Scholar] [CrossRef] [PubMed]
- Garlet, G.P. Destructive and protective roles of cytokines in periodontitis: A reappraisal from host defense and tissue destruction viewpoints. J. Dent. Res. 2010, 89, 1349–1363. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.C.; Lerner, U.H.; Teng, Y.T. Cytokine responses against periodontal infection: Protective and destructive roles. Periodontol. 2000 2010, 52, 163–206. [Google Scholar] [CrossRef] [PubMed]
- Genco, R.J.; Borgnakke, W.S. Risks factors for periodontal disease. Periodontol. 2000 2013, 62, 59–94. [Google Scholar] [CrossRef] [PubMed]
- Otomo-Corgel, J.; Pucher, J.J.; Rethman, M.P.; Reynolds, M.A. State of the science: Chronic periodontitis and systemic health. J. Evid. Based Dent. Pract. 2012, 12, 20–28. [Google Scholar] [CrossRef]
- Yang, H.W.; Huang, Y.F.; Chou, M.Y. Occurrence of Porphyromonas gingivalis and Tannerella forsythensis in periodontally diseased and healthy subjects. J. Periodontol. 2004, 75, 1077–1083. [Google Scholar] [CrossRef] [PubMed]
- Bostanci, N.; Belibasakis, G.N. Porphyromonas gingivalis: An invasive and evasive opportunistic oral pathogen. FEMS Microbiol. Lett. 2012, 333, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Liao, J.; Zhao, L.; Yoshioka, M.; Hinode, D.; Grenier, D. Effects of Japanese traditional herbal medicines (Kampo) on growth and virulence properties of Porphyromonas gingivalis and viability of oral epithelial cells. Pharm. Biol. 2013, 51, 1538–1544. [Google Scholar] [CrossRef] [PubMed]
- Fournier-Larente, J.; Azelmat, J.; Yoshioka, M.; Hinode, D.; Grenier, D. The Daiokanzoto (TJ-84) Kampo formulation reduces virulence factor gene expression in Porphyromonas gingivalis and possesses anti-inflammatory and anti-protease activities. PLoS ONE 2016, 11, 2. [Google Scholar] [CrossRef] [PubMed]
- Ximenez-Fyvie, L.A.; Haffajee, A.D.; Socransky, S.S. Comparison of the microbiota of supra- and subgingival plaque in health and periodontitis. J. Clin. Periodontol. 2000, 27, 648–657. [Google Scholar] [CrossRef] [PubMed]
- Kolenbrander, P.E.; Palmer, R.J.; Rickard, A.H.; Jakubovics, N.S.; Chalmers, N.I.; Diaz, P.I. Bacterial interactions and successions during plaque development. Periodontol. 2000 2006, 42, 47–79. [Google Scholar] [CrossRef] [PubMed]
- Socransky, S.S.; Haffajee, A.D.; Cugini, M.A.; Smith, C.; Kent, R.L. Microbial complexes in subgingival plaque. J. Clin. Periodontol. 1988, 25, 134–144. [Google Scholar] [CrossRef]
- Liao, J.; Azelmat, J.; Zhao, L.; Yoshioka, M.; Hinode, D.; Grenier, D. The Kampo medicine Rokumigan possesses antibiofilm, anti-inflammatory, and wound healing properties. BioMed Res. Int. 2014, 2014, 436206. [Google Scholar] [CrossRef] [PubMed]
- Fukamachi, H.; Matsumoto, C.; Omiya, Y.; Arimoto, T.; Morisali, H.; Kataoka, H.; Kadena, M.; Funatsu, T.; Fukutake, M.; Kase, Y.; et al. Effects of Hangeshashinto on growth of oral microorganisms. Evid. Based Complement. Altern. Med. 2015, 2015, 512947. [Google Scholar] [CrossRef] [PubMed]
- Hassell, T.M. Tissues and cells of the periodontium. Periodontol. 2000 1993, 3, 9–38. [Google Scholar] [CrossRef] [PubMed]
- Takashiba, S.; Naruishi, K.; Murayama, Y. Perspective of cytokine regulation for periodontal treatment: Fibroblast biology. J. Periodontol. 2003, 74, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, G.A.; Miozza, V.A.; Delgado, A.; Busch, L. Salivary IL-1β and PGE2 as biomarkers of periodontal status, before and after periodontal treatment. J. Clin. Periodontol. 2013, 40, 1112–1117. [Google Scholar] [CrossRef] [PubMed]
- Ara, T.; Maeda, Y.; Fujinami, Y.; Imamura, Y.; Hattori, T.; Wang, P.L. Preventive effects of a Kampo medicine, Shosaikoto, on inflammatory responses in LPS-treated human fibroblasts. Biol. Pharm. Bull. 2008, 31, 1141–1144. [Google Scholar] [CrossRef] [PubMed]
- Ara, T.; Honjo, K.; Fujinami, Y.; Hattori, T.; Imamura, Y.; Wang, P.L. Preventive effects of a Kampo medicine, Orento on inflammatory responses in lipopolysaccharide treated human gingival fibroblasts. Biol. Pharm. Bull. 2010, 33, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Irwin, C.R.; Myrillas, T.T. The role of IL-6 in the pathogenesis of periodontal disease. Oral Dis. 1998, 4, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Ishimi, Y.; Miyaura, C.; Jin, C.H.; Akatsu, T.; Abe, E.; Nakamura, Y.; Yamaguchi, A.; Yoshiki, S.; Matsuda, T.; Hirano, T.; et al. IL-6 is produced by osteoblasts and induces bone resorption. J. Immunol. 1990, 145, 3297–3303. [Google Scholar] [PubMed]
- Shim, K.S.; Ma, C.J.; Kim, D.S.; Ma, J.Y. Yukmijihwang-tang inhibits receptor activator for nuclear factor-κB ligand-induced osteoclast differentiation. J. Med. Food 2011, 14, 1439–1447. [Google Scholar] [CrossRef] [PubMed]
- Horie, N.; Hashimoto, K.; Hino, S.; Kato, T.; Shimoyama, T.; Kaneko, T.; Kusama, K.; Sakagami, H. Anti-inflammatory potential of Rikkosan based on IL-1β network through macrophages to oral tissue cells. In Vivo 2014, 28, 563–569. [Google Scholar] [PubMed]
- Gamonal, J.; Acevedo, A.; Bascones, A.; Jorge, O.; Silva, A. Characterization of cellular infiltrate, detection of chemokine receptor CCR5 and interleukin-8 and RANTES chemokines in adult periodontitis. J. Periodontal Res. 2001, 36, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Takada, Y.; Boriek, A.M.; Aggarwal, B.B. Nuclear factor-kappaB: Its role in health and disease. J. Mol. Med. 2004, 82, 434–448. [Google Scholar] [CrossRef] [PubMed]
- Souza, J.A.; Rossa, C.; Garlet, G.P.; Nogueira, A.V.; Cirelli, J.A. Modulation of host cell signaling pathways as a therapeutic approach in periodontal disease. J. Appl. Oral Sci. 2012, 20, 128–138. [Google Scholar] [CrossRef] [PubMed]
- Hosseinzadeh, H.; Nassiri-Asl, M. Pharmacological effects of Glycyrrhiza spp. and its bioactive constituents: Update and review. Phytother. Res. 2015, 29, 1868–1886. [Google Scholar] [CrossRef] [PubMed]
- Sapna, G.; Gokul, S.; Bagri-Manjrekar, K. Matrix metalloproteinases and periodontal diseases. Oral Dis. 2014, 20, 538–550. [Google Scholar] [CrossRef] [PubMed]
- Teng, Y.T.; Sodek, J.; McCulloch, C.A. Gingival crevicular fluid gelatinase and its relationship to periodontal disease in human subjects. J. Periodontal Res. 1992, 27, 544–552. [Google Scholar] [CrossRef] [PubMed]
- Kubota, T.; Nomura, T.; Takahashi, T.; Hara, K. Expression of mRNA for matrix metalloproteinases and tissue inhibitors of metalloproteinases in periodontitis-affected human gingival tissue. Arch. Oral Biol. 1996, 41, 253–262. [Google Scholar] [CrossRef]
- Takeda, O.; Toyama, T.; Watanabe, K.; Sato, T.; Sasaguri, K.; Akimoto, S.; Sato, S.; Kawata, T.; Hamada, N. Ameliorating effects of Juzentaihoto on restraint stress and P. gingivalis-induced alveolar bone loss. Arch. Oral Biol. 2014, 59, 1130–1138. [Google Scholar] [CrossRef] [PubMed]
- Wikesjo, U.M.; Selvig, K.A. Periodontal wound healing and regeneration. Periodontol. 2000 1999, 19, 21–39. [Google Scholar] [CrossRef] [PubMed]
- Groeger, S.E.; Meyle, J. Epithelial barrier and oral bacterial infection. Periodontol. 2000 2015, 69, 46–67. [Google Scholar] [CrossRef] [PubMed]
- Gursoy, U.K.; Könönen, E. Understanding the roles of gingival beta-defensins. J. Oral Microbiol. 2012, 4, 15127. [Google Scholar] [CrossRef] [PubMed]
- Hiroshima, Y.; Bando, M.; Kataoka, M.; Shinohara, Y.; Herzberg, M.C.; Ross, K.F.; Inagaki, Y.; Nagata, T.; Kido, J. Shosaikoto increases calprotectin expression in human oral epithelial cells. J. Periodontal Res. 2010, 45, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Hiroshima, Y.; Bando, M.; Inagaki, Y.; Kido, R.; Kataoka, M.; Nagata, T.; Kido, J. Effect of Hangeshashinto on calprotectin expression in human oral epithelial cells. Odontology 2016, 104, 152–162. [Google Scholar] [CrossRef] [PubMed]
- Al-Ansari, S.; Zecha, J.A.E.M.; Barasch, A.; De Lange, J.; Rozema, F.R.; Raber-Durlacher, J.E. Oral mucositis induced by anticancer therapies. Curr. Oral Health Rep. 2015, 2, 202–211. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, K.; Yoshioka, M.; Okamura, H.; Moriyama, S.; Kawazoe, K.; Grenier, D.; Hinode, D. Preventive effect of Daiokanzoto (TJ-84) on 5-fluorouracil-induced human gingival cell death through the inhibition of reactive oxygen species production. PLoS ONE 2014, 9, e112689. [Google Scholar] [CrossRef] [PubMed]
- Kono, T.; Satomi, M.; Chisato, N.; Ebisawa, Y.; Suno, M.; Asama, T.; Karasaki, H.; Matsubara, K.; Furukawa, H. Topical application of Hangeshashinto (TJ-14) in the treatment of chemotherapy-induced oral mucositis. World J. Oncol. 2010, 1, 232–235. [Google Scholar] [PubMed]
- Yamashita, T.; Araki, K.; Tomifuji, M.; Kamide, D.; Tanaka, Y.; Shiotani, A. A traditional Japanese medicine—Hangeshashinto (TJ-14)—Alleviates chemoradiation-induced mucositis and improves rates of treatment completion. Support. Care Cancer 2015, 23, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Kono, T.; Kaneko, A.; Matsumoto, C.; Miyagi, C.; Ohbuchi, K.; Mizuhara, Y.; Miyano, K.; Uezono, Y. Multitargeted effects of Hangeshashinto for treatment of chemotherapy-induced oral mucositis on inducible prostaglandin E2 production in human oral keratinocytes. Integr. Cancer Ther. 2014, 13, 435–445. [Google Scholar] [CrossRef] [PubMed]
- Kamide, D.; Yamashita, T.; Araki, K.; Tomifuji, M.; Shiotani, A. Hangeshashinto (TJ-14) prevents radiation-induced mucositis by suppressing cyclooxygenase-2 expression and chemotaxis of inflammatory cells. Clin. Transl. Oncol. 2017, 19, 1329–1336. [Google Scholar] [CrossRef] [PubMed]
- Napenas, J.J.; Brennan, M.T.; Fox, P.C. Diagnosis and treatment of xerostomia (dry mouth). Odontology 2009, 97, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Yanagi, Y.; Yasuda, M.; Hashida, K.; Kadokura, Y.; Yamamoto, T.; Suzaki, H. Mechanism of salivary secretion enhancement by Byakkokaninjinto. Biol. Pharm. Bull. 2008, 31, 431–435. [Google Scholar] [CrossRef] [PubMed]
- Sakaguchi, M.; Goto, K.; Ichiki, H.; Hattori, N.; Iizuka, A.; Yamamoto, M.; Takeda, S.; Ishige, A.; Aburada, M.; Yasuda, M.; et al. Effects of Byakkokaninjinto on salivary secretion and bladder function in rats. J. Ethnopharmacol. 2005, 102, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Ara, T.; Hattori, T.; Imamura, Y.; Wang, P.L. Development of novel therapy for oral diseases using kampo medicines. J. Oral Biosci. 2010, 52, 100–106. [Google Scholar] [CrossRef]
- Trackman, P.C.; Kantarci, A. Molecular and clinical aspects of drug-induced gingival overgrowth. J. Dent. Res. 2015, 94, 540–546. [Google Scholar] [CrossRef] [PubMed]
- Awazu, M.; Fujita, H.; Omori, S.; Hida, M. The herbal medicine Saireito inhibits proliferation of rat mesangial cells. Nephron 2002, 92, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Hattori, T.; Tanaka, J.; Kikuchi, M.; Suetsugu, Y.; Matsunaga, S.; Nakazono, Y.; Wang, P.L. Inhibition of nifedipine-induced proliferation of cultured human gingival fibroblasts by Saireito, a Chinese herbal medicine. J. Oral Biosci. 2006, 48, 126–131. [Google Scholar] [CrossRef]
| Name of Kampo | Type of Studies | Disease/Disorder | Effect of Kampo | Reference |
|---|---|---|---|---|
| Byakkokaninjinto (TJ-34) | In vivo (animal) | Xerostomia |
| [57,58] |
| Daijokito (TJ-133) | In vitro | Periodontal disease |
| [21] |
| Daiokanzoto (TJ-84) | In vitro | Periodontal disease |
| [21] |
| [22] | ||||
| [22] | ||||
| [22] | ||||
| [22] | ||||
| In vitro | Oral mucositis |
| [51] | |
| Goreisan (TJ-17) | In vivo (animal) | Xerostomia |
| [59] |
| Hangeshashinto (TJ-14) | In vitro | Periodontal disease |
| [49] |
| [49] | |||
| In vivo (human) | Oral mucositis |
| [27] | |
| In vitro | Oral mucositis |
| [52,53] | |
| [54,55] | |||
| Inchinkoto (TJ-135) | In vitro | Periodontal disease |
| [21] |
| Juzentaihoto (TJ-48) | In vitro | Periodontal disease |
| [44] |
| In vivo (animal) | Periodontal disease |
| [44] | |
| Keishikashakuyakudaioto (TJ-134) | In vitro | Periodontal disease |
| [21] |
| Mashiningan (TJ-126) | In vitro | Periodontal disease |
| [21] |
| Orento (TJ-120) | In vitro | Periodontal disease |
| [32] |
| Rikkosan (TJ-110) | In vitro | Periodontal disease |
| [36] |
| [36] | |||
| Rokumigan (TJ-87) | In vitro | Periodontal disease |
| [26] |
| [26] | |||
| [26] | |||
| Saireito (TJ-114) | In vitro | Drug-induced gingival overgrowth |
| [62] |
| [62] | |||
| Saoshashinto (TJ-113) | In vitro | Periodontal disease |
| [21] |
| Shosaikoto (TJ-9) | In vitro | Periodontal disease |
| [31] |
| [48] | |||
| Tokakujokito (TJ-61) | In vitro | Periodontal disease |
| [21] |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Veilleux, M.-P.; Moriyama, S.; Yoshioka, M.; Hinode, D.; Grenier, D. A Review of Evidence for a Therapeutic Application of Traditional Japanese Kampo Medicine for Oral Diseases/Disorders. Medicines 2018, 5, 35. https://doi.org/10.3390/medicines5020035
Veilleux M-P, Moriyama S, Yoshioka M, Hinode D, Grenier D. A Review of Evidence for a Therapeutic Application of Traditional Japanese Kampo Medicine for Oral Diseases/Disorders. Medicines. 2018; 5(2):35. https://doi.org/10.3390/medicines5020035
Chicago/Turabian StyleVeilleux, Marie-Pier, Satomi Moriyama, Masami Yoshioka, Daisuke Hinode, and Daniel Grenier. 2018. "A Review of Evidence for a Therapeutic Application of Traditional Japanese Kampo Medicine for Oral Diseases/Disorders" Medicines 5, no. 2: 35. https://doi.org/10.3390/medicines5020035
APA StyleVeilleux, M.-P., Moriyama, S., Yoshioka, M., Hinode, D., & Grenier, D. (2018). A Review of Evidence for a Therapeutic Application of Traditional Japanese Kampo Medicine for Oral Diseases/Disorders. Medicines, 5(2), 35. https://doi.org/10.3390/medicines5020035