Opposite Interactive Effects of Heat Wave and Cold Spell with Fine Particulate Matter on Pneumonia Mortality
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Study Design
2.3. Exposure Assessment
2.4. Statistical Analysis
3. Results
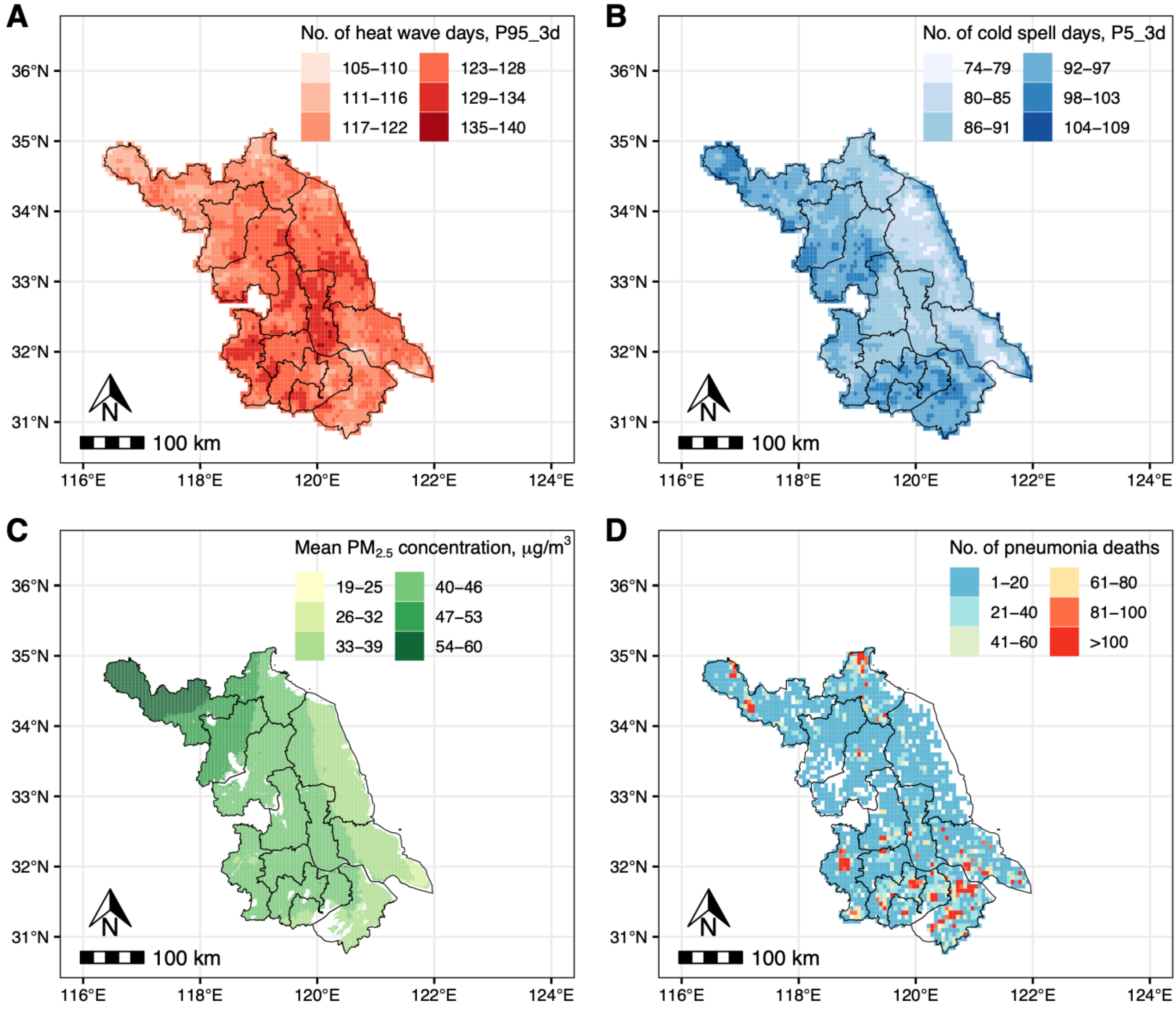
3.1. Descriptive Statistics
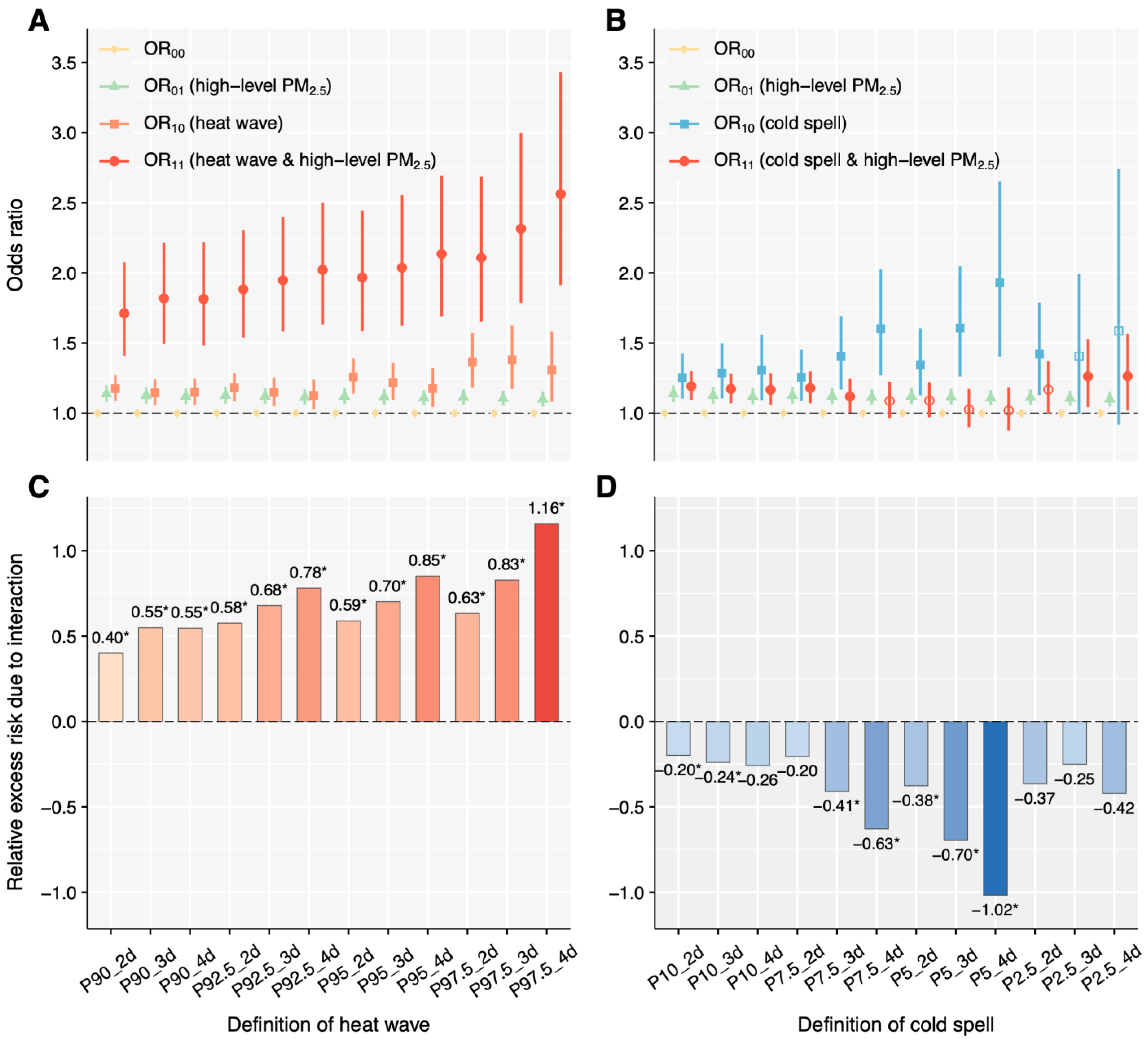
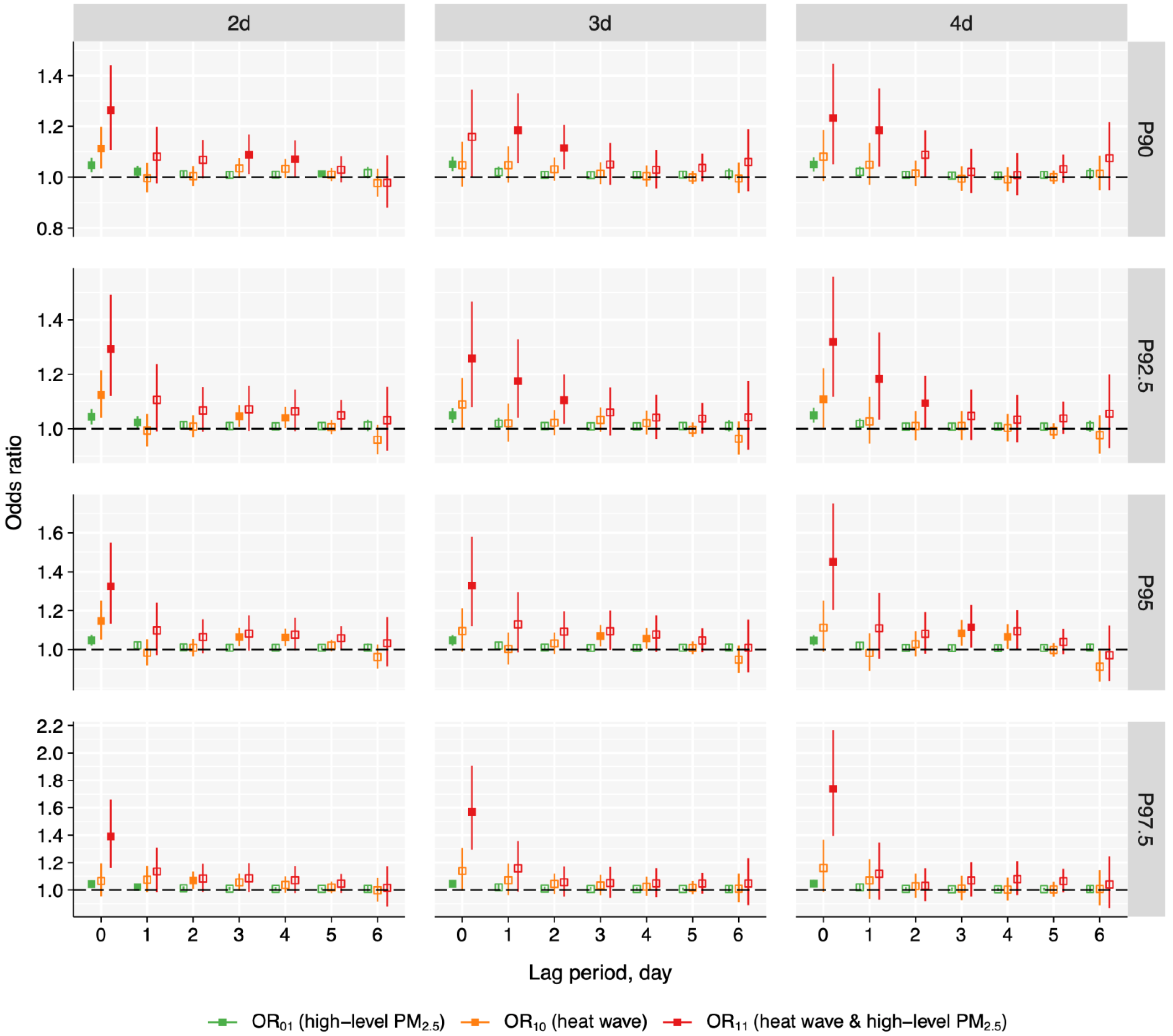
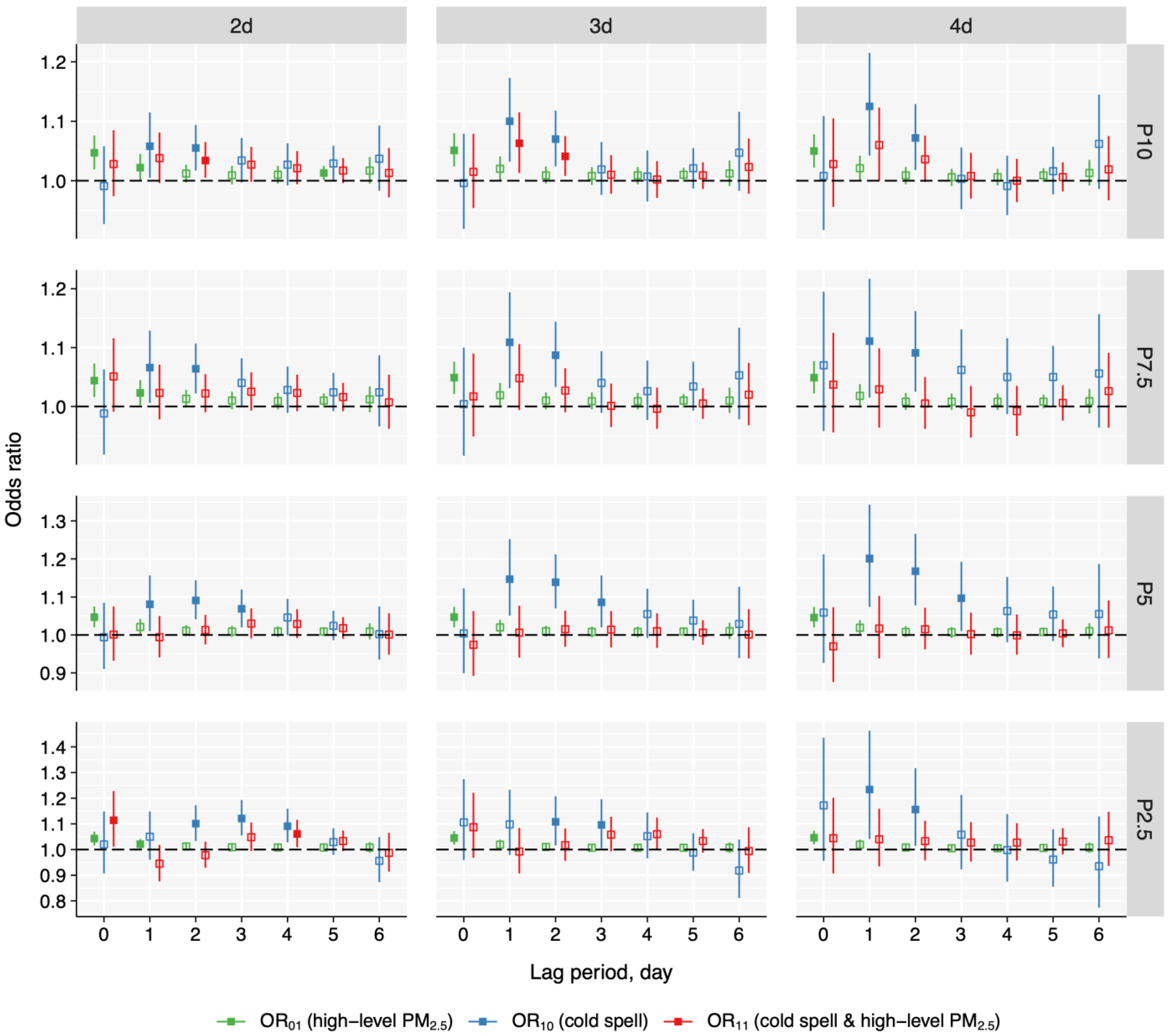
3.2. Exposure–Response Analysis
3.3. Interactive Effects
3.4. Stratified Analysis
3.5. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| GBD | Global Burden of Diseases, Injuries, and Risk Factors Study |
| LRI | lower respiratory infections |
| YLLs | years of life lost |
| ETEs | extreme temperature events |
| PM2.5 | fine particulate matter |
| ICD-10 | International Statistical Classification of Diseases and Related Health Problems |
| HI | heat index |
| O3 | ozone |
| CHAP | ChinaHighAirPollutants |
| R2 | cross-validated coefficients of determination |
| RMSE | root-mean-square deviations |
| DLNM | distributed lag nonlinear model |
| df | degrees of freedom |
| OR | odds ratio |
| CI | confidence interval |
| RERI | relative excess risk due to interaction |
| AP | attributable proportion due to interaction |
| S | synergy index |
| eCI | empirical confidence interval |
| WHO | World Health Organization |
| AQGs | air quality guidelines |
References
- Cilloniz, C.; Dela Cruz, C.; Curioso, W.H.; Vidal, C.H. World pneumonia day 2023: The rising global threat of pneumonia and what we must do about it. Eur. Respir. J. 2023, 62, 2301672. [Google Scholar] [CrossRef]
- Global, regional, and national incidence and mortality burden of non-COVID-19 lower respiratory infections and aetiologies, 1990-2021: A systematic analysis from the Global Burden of Disease Study 2021. Lancet Infect. Dis. 2024, 24, 974–1002. [CrossRef]
- Fan, G.; Zhou, Y.; Zhou, F.; Yu, Z.; Gu, X.; Zhang, X.; Liu, Z.; Zhou, M.; Cao, B. The mortality and years of life lost for community-acquired pneumonia before and during COVID-19 pandemic in China. Lancet Reg. Health West. Pac. 2024, 42, 100968. [Google Scholar] [CrossRef]
- Marangu, D.; Zar, H.J. Childhood pneumonia in low-and-middle-income countries: An update. Paediatr. Respir. Rev. 2019, 32, 3–9. [Google Scholar] [CrossRef]
- Xu, R.; Sun, H.; Zhong, Z.; Zheng, Y.; Liu, T.; Li, Y.; Liu, L.; Luo, L.; Wang, S.; Lv, Z.; et al. Ozone, heat wave, and cardiovascular disease mortality: A population-based case-crossover study. Environ. Sci. Technol. 2024, 58, 171–181. [Google Scholar] [CrossRef]
- Xu, R.; Huang, S.; Shi, C.; Wang, R.; Liu, T.; Li, Y.; Zheng, Y.; Lv, Z.; Wei, J.; Sun, H.; et al. Extreme temperature events, fine particulate matter, and myocardial infarction mortality. Circulation 2023, 148, 312–323. [Google Scholar] [CrossRef]
- Zhang, Q.; Meng, X.; Shi, S.; Kan, L.; Chen, R.; Kan, H. Overview of particulate air pollution and human health in China: Evidence, challenges, and opportunities. Innovation 2022, 3, 100312. [Google Scholar] [CrossRef]
- Luo, H.; Zhang, Q.; Niu, Y.; Kan, H.; Chen, R. Fine particulate matter and cardiorespiratory health in China: A systematic review and meta-analysis of epidemiological studies. J. Environ. Sci. 2023, 123, 306–316. [Google Scholar] [CrossRef]
- Bowe, B.; Xie, Y.; Yan, Y.; Al-Aly, Z. Burden of cause-specific mortality associated with PM2.5 air pollution in the United States. JAMA Netw. Open 2019, 2, e1915834. [Google Scholar] [CrossRef]
- Chen, H.; Zhao, L.; Cheng, L.; Zhang, Y.; Wang, H.; Gu, K.; Bao, J.; Yang, J.; Liu, Z.; Huang, J.; et al. Projections of heatwave-attributable mortality under climate change and future population scenarios in China. Lancet Reg. Health West. Pac. 2022, 28, 100582. [Google Scholar] [CrossRef]
- He, C.; Yin, P.; Liu, Z.; Huang, J.; Chen, Y.; Gao, X.; Xu, Y.; Wang, C.; Cai, W.; Gong, P.; et al. Projections of excess deaths related to cold spells under climate and population change scenarios: A nationwide time series modeling study. Environ. Int. 2023, 178, 108034. [Google Scholar] [CrossRef]
- Rahman, M.M.; McConnell, R.; Schlaerth, H.; Ko, J.; Silva, S.; Lurmann, F.W.; Palinkas, L.; Johnston, J.; Hurlburt, M.; Yin, H.; et al. The effects of coexposure to extremes of heat and particulate air pollution on mortality in california: Implications for climate change. Am. J. Respir. Crit. Care Med. 2022, 206, 1117–1127. [Google Scholar] [CrossRef]
- Zhang, Y.; He, Q.; Tong, X.; Yin, P.; Liu, Y.; Meng, X.; Gao, Y.; Shi, S.; Li, X.; Kan, H.; et al. Differential associations of fine and coarse particulate air pollution with cause-specific pneumonia mortality: A nationwide, individual-level, case-crossover study. Environ. Res. 2024, 252, 119054. [Google Scholar] [CrossRef]
- Sun, S.; Tian, L.; Cao, W.; Lai, P.C.; Wong, P.P.Y.; Lee, R.S.; Mason, T.G.; Krämer, A.; Wong, C.M. Urban climate modified short-term association of air pollution with pneumonia mortality in Hong Kong. Sci. Total Environ. 2019, 646, 618–624. [Google Scholar] [CrossRef]
- Liu, Y.; Pan, J.; Zhang, H.; Shi, C.; Li, G.; Peng, Z.; Ma, J.; Zhou, Y.; Zhang, L. Short-term exposure to ambient air pollution and asthma mortality. Am. J. Respir. Crit. Care Med. 2019, 200, 24–32. [Google Scholar] [CrossRef]
- Zhao, B.; Johnston, F.H.; Salimi, F.; Kurabayashi, M.; Negishi, K. Short-term exposure to ambient fine particulate matter and out-of-hospital cardiac arrest: A nationwide case-crossover study in Japan. Lancet Planet. Health 2020, 4, e15–e23. [Google Scholar] [CrossRef]
- Liu, T.; Shi, C.; Wei, J.; Xu, R.; Li, Y.; Wang, R.; Lu, W.; Liu, L.; Zhong, C.; Zhong, Z.; et al. Extreme temperature events and dementia mortality in Chinese adults: A population-based, case-crossover study. Int. J. Epidemiol. 2024, 53, dyad119. [Google Scholar] [CrossRef]
- Carracedo-Martínez, E.; Taracido, M.; Tobias, A.; Saez, M.; Figueiras, A. Case-crossover analysis of air pollution health effects: A systematic review of methodology and application. Environ. Health Perspect. 2010, 118, 1173–1182. [Google Scholar] [CrossRef]
- Liu, J.; Shi, C.; Sun, S.; Liang, J.; Yang, Z.-L. Improving land surface hydrological simulations in China using CLDAS meteorological forcing data. J. Meteorol. Res. 2019, 33, 1194–1206. [Google Scholar] [CrossRef]
- Han, S.; Liu, B.C.; Shi, C.X.; Liu, Y.; Qiu, M.J.; Sun, S. Evaluation of CLDAS and GLDAS datasets for near-surface air temperature over major land areas of China. Sustainability 2020, 12, 4311. [Google Scholar] [CrossRef]
- Tie, R.; Shi, C.; Wan, G.; Hu, X.; Kang, L.; Ge, L. CLDASSD: Reconstructing fine textures of the temperature field using super-resolution technology. Adv. Atmos. Sci. 2022, 39, 117–130. [Google Scholar] [CrossRef]
- Anderson, G.B.; Bell, M.L.; Peng, R.D. Methods to calculate the heat index as an exposure metric in environmental health research. Environ. Health Perspect. 2013, 121, 1111–1119. [Google Scholar] [CrossRef]
- Chiu, K.C.; Hsieh, M.S.; Huang, Y.T.; Liu, C.Y. Exposure to ambient temperature and heat index in relation to DNA methylation age: A population-based study in Taiwan. Environ. Int. 2024, 186, 108581. [Google Scholar] [CrossRef]
- Steadman, R.G. Norms of apparent temperature in Australia. Aust. Met. Mag. 1994, 43, 1–16. [Google Scholar]
- Guo, Y.; Gasparrini, A.; Armstrong, B.G.; Tawatsupa, B.; Tobias, A.; Lavigne, E.; Coelho, M.; Pan, X.; Kim, H.; Hashizume, M.; et al. Heat wave and mortality: A multicountry, multicommunity study. Environ. Health Perspect. 2017, 125, 087006. [Google Scholar] [CrossRef]
- Jiang, Y.; Yi, S.; Gao, C.; Chen, Y.; Chen, J.; Fu, X.; Yang, L.; Kong, X.; Chen, M.; Kan, H.; et al. Cold spells and the onset of acute myocardial infarction: A nationwide case-crossover study in 323 Chinese cities. Environ. Health Perspect. 2023, 131, 87016. [Google Scholar] [CrossRef]
- Wei, J.; Li, Z.Q.; Li, K.; Dickerson, R.R.; Pinker, R.T.; Wang, J.; Liu, X.; Sun, L.; Xue, W.H.; Cribb, M. Full-coverage mapping and spatiotemporal variations of ground-level ozone (O3) pollution from 2013 to 2020 across China. Remote Sens. Environ. 2022, 270, 112775. [Google Scholar] [CrossRef]
- Wei, J.; Li, Z.Q.; Lyapustin, A.; Sun, L.; Peng, Y.R.; Xue, W.H.; Su, T.N.; Cribb, M. Reconstructing 1-km-resolution high-quality PM2.5 data records from 2000 to 2018 in China: Spatiotemporal variations and policy implications. Remote Sens. Environ. 2021, 252, 112136. [Google Scholar] [CrossRef]
- Gasparrini, A. Modeling exposure-lag-response associations with distributed lag non-linear models. Stat. Med. 2014, 33, 881–899. [Google Scholar] [CrossRef]
- Jiang, S.; Tong, X.; Yu, K.; Yin, P.; Shi, S.; Meng, X.; Chen, R.; Zhou, M.; Kan, H.; Niu, Y.; et al. Ambient particulate matter and chronic obstructive pulmonary disease mortality: A nationwide, individual-level, case-crossover study in China. eBioMedicine 2024, 107, 105270. [Google Scholar] [CrossRef]
- Knol, M.J.; VanderWeele, T.J. Recommendations for presenting analyses of effect modification and interaction. Int. J. Epidemiol. 2012, 41, 514–520. [Google Scholar] [CrossRef]
- Knol, M.J.; VanderWeele, T.J.; Groenwold, R.H.; Klungel, O.H.; Rovers, M.M.; Grobbee, D.E. Estimating measures of interaction on an additive scale for preventive exposures. Eur. J. Epidemiol. 2011, 26, 433–438. [Google Scholar] [CrossRef]
- Knol, M.J.; van der Tweel, I.; Grobbee, D.E.; Numans, M.E.; Geerlings, M.I. Estimating interaction on an additive scale between continuous determinants in a logistic regression model. Int. J. Epidemiol. 2007, 36, 1111–1118. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Leone, M. Attributable risk from distributed lag models. BMC Med. Res. Methodol. 2014, 14, 55. [Google Scholar] [CrossRef]
- Altman, D.G.; Bland, J.M. Interaction revisited: The difference between two estimates. BMJ 2003, 326, 219. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.; Li, M.; Wang, Y.; Cui, L.; Li, T. Acute effects of low temperatures and cold waves on elderly infectious pneumonia mortality—Jinan city, Shandong province, China, 2014–2022. China CDC Wkly. 2024, 6, 77–82. [Google Scholar] [CrossRef]
- Wilson, L.A.; Morgan, G.G.; Hanigan, I.C.; Johnston, F.H.; Abu-Rayya, H.; Broome, R.; Gaskin, C.; Jalaludin, B. The impact of heat on mortality and morbidity in the greater metropolitan sydney region: A case crossover analysis. Environ. Health 2013, 12, 98. [Google Scholar] [CrossRef]
- Huang, C.; Cheng, J.; Phung, D.; Tawatsupa, B.; Hu, W.; Xu, Z. Mortality burden attributable to heatwaves in Thailand: A systematic assessment incorporating evidence-based lag structure. Environ. Int. 2018, 121, 41–50. [Google Scholar] [CrossRef]
- Qiu, H.; Tian, L.; Ho, K.F.; Yu, I.T.; Thach, T.Q.; Wong, C.M. Who is more vulnerable to death from extremely cold temperatures? a case-only approach in Hong Kong with a temperate climate. Int. J. Biometeorol. 2016, 60, 711–717. [Google Scholar] [CrossRef]
- Ma, C.; Yang, J.; Nakayama, S.F.; Iwai-Shimada, M.; Jung, C.R.; Sun, X.L.; Honda, Y. Cold spells and cause-specific mortality in 47 Japanese prefectures: A systematic evaluation. Environ. Health Perspect. 2021, 129, 67001. [Google Scholar] [CrossRef]
- Ran, J.; Sun, S.; Han, L.; Zhao, S.; Chen, D.; Guo, F.; Li, J.; Qiu, H.; Lei, Y.; Tian, L. Fine particulate matter and cause-specific mortality in the Hong Kong elder patients with chronic kidney disease. Chemosphere 2020, 247, 125913. [Google Scholar] [CrossRef]
- Zhou, H.; Geng, H.; Dong, C.; Bai, T. The short-term harvesting effects of ambient particulate matter on mortality in Taiyuan elderly residents: A time-series analysis with a generalized additive distributed lag model. Ecotoxicol. Environ. Saf. 2021, 207, 111235. [Google Scholar] [CrossRef] [PubMed]
- He, Q.; Liu, Y.; Yin, P.; Gao, Y.; Kan, H.; Zhou, M.; Chen, R.; Li, Y. Differentiating the impacts of ambient temperature on pneumonia mortality of various infectious causes: A nationwide, individual-level, case-crossover study. eBioMedicine 2023, 98, 104854. [Google Scholar] [CrossRef]
- Rai, M.; Stafoggia, M.; de’Donato, F.; Scortichini, M.; Zafeiratou, S.; Vazquez Fernandez, L.; Zhang, S.; Katsouyanni, K.; Samoli, E.; Rao, S.; et al. Heat-related cardiorespiratory mortality: Effect modification by air pollution across 482 cities from 24 countries. Environ. Int. 2023, 174, 107825. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Wang, Y.; Zhang, T.; Wang, P.; Huang, L.; Guo, Y. Exploring health effects under specific causes of mortality based on 90 definitions of PM2.5 and cold spell combined exposure in Shanghai, China. Environ. Sci. Technol. 2023, 57, 2423–2434. [Google Scholar] [CrossRef]
- Ning, Z.; He, S.; Liu, Q.; Ma, H.; Ma, C.; Wu, J.; Ma, Y.; Zhang, Y. Effects of the interaction between cold spells and fine particulate matter on mortality risk in Xining: A case-crossover study at high altitude. Front. Public Health. 2024, 12, 1414945. [Google Scholar] [CrossRef]
- Pompilio, A.; Di Bonaventura, G. Ambient air pollution and respiratory bacterial infections, a troubling association: Epidemiology, underlying mechanisms, and future challenges. Crit. Rev. Microbiol. 2020, 46, 600–630. [Google Scholar] [CrossRef]
- Lepeule, J.; Litonjua, A.A.; Gasparrini, A.; Koutrakis, P.; Sparrow, D.; Vokonas, P.S.; Schwartz, J. Lung function association with outdoor temperature and relative humidity and its interaction with air pollution in the elderly. Environ. Res. 2018, 165, 110–117. [Google Scholar] [CrossRef]
- Cao, C.; Jiang, W.; Wang, B.; Fang, J.; Lang, J.; Tian, G.; Jiang, J.; Zhu, T.F. Inhalable microorganisms in Beijing’s PM2.5 and PM10 pollutants during a severe smog event. Environ. Sci. Technol. 2014, 48, 1499–1507. [Google Scholar] [CrossRef]
- Moriyama, M.; Hugentobler, W.J.; Iwasaki, A. Seasonality of respiratory viral infections. Annu. Rev. Virol. 2020, 7, 83–101. [Google Scholar] [CrossRef] [PubMed]
- Tucker, P.; Gilliland, J. The effect of season and weather on physical activity: A systematic review. Public Health 2007, 121, 909–922. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Zhou, K.; Yang, S. Regional difference of household electricity consumption: An empirical study of Jiangsu, China. J. Clean. Prod. 2018, 171, 1415–1428. [Google Scholar] [CrossRef]
- Watkinson, W.P.; Campen, M.J.; Wichers, L.B.; Nolan, J.P.; Costa, D.L. Cardiac and thermoregulatory responses to inhaled pollutants in healthy and compromised rodents: Modulation via interaction with environmental factors. Environ. Res. 2003, 92, 35–47. [Google Scholar] [CrossRef]
- Rocholl, M.; Ludewig, M.; John, S.M.; Bitzer, E.M.; Wilke, A. Outdoor workers’ perceptions of skin cancer risk and attitudes to sun-protective measures: A qualitative study. J. Occup. Health 2020, 62, e12083. [Google Scholar] [CrossRef]
- Castellani, J.W.; Young, A.J. Human physiological responses to cold exposure: Acute responses and acclimatization to prolonged exposure. Auton. Neurosci. 2016, 196, 63–74. [Google Scholar] [CrossRef]
- Ji, L.; Laouadi, A.; Wang, L.; Lacasse, M. Development of a bioheat model for older people under hot and cold exposures. Build. Simul. 2022, 15, 1815–1829. [Google Scholar] [CrossRef]
- Wagner, J.A.; Horvath, S.M. Influences of age and gender on human thermoregulatory responses to cold exposures. J. Appl. Physiol. 1985, 58, 180–186. [Google Scholar] [CrossRef]
- Yin, C.; Yang, Y.; Chen, X.; Yue, X.; Liu, Y.; Xin, Y. Global near real-time daily apparent temperature and heat wave dataset. Geosci. J. 2023, 10, 231–245. [Google Scholar] [CrossRef]
- Zeger, S.L.; Thomas, D.; Dominici, F.; Samet, J.M.; Schwartz, J.; Dockery, D.; Cohen, A. Exposure measurement error in time-series studies of air pollution: Concepts and consequences. Environ. Health Perspect. 2000, 108, 419–426. [Google Scholar] [CrossRef]

| Characteristic | N (%) |
|---|---|
| Pneumonia deaths (case days), n | 50,196 |
| Control days, n | 169,721 |
| Age, mean (SD) | 81.9 (15.3) |
| ≤80, n (%) | 14,316 (28.5) |
| >80, n (%) | 35,880 (71.5) |
| Sex, n (%) | |
| Men | 26,269 (52.3) |
| Women | 23,925 (47.7) |
| Unknown | 2 (0) |
| Season at death, n (%) | |
| Spring (March to May) | 12,549 (25.0) |
| Summer (June to August) | 10,299 (20.5) |
| Autumn (September to November) | 10,763 (21.4) |
| Winter (December to February) | 16,585 (33.0) |
| Exposure | On Case Days | On Control Days | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | P25 | P50 | P75 | Mean | P25 | P50 | P75 | |
| PM2.5 (μg/m3) | 49.0 | 26.4 | 40.8 | 62.2 | 48.5 | 26.1 | 40.0 | 61.6 |
| O3 (μg/m3) | 103.1 | 68.4 | 94.1 | 132.1 | 102.8 | 68.2 | 94.1 | 131.9 |
| Heat index (°C) | 15.7 | 5.6 | 14.2 | 24.0 | 15.7 | 5.7 | 14.4 | 24.0 |
| Heat Wave | Cold Spell | PM2.5 2 | |||
|---|---|---|---|---|---|
| Definition | OR (95% CI) | Definition | OR (95% CI) | Definition | OR (95% CI) |
| P90_2d | 1.23 (1.15, 1.32) | P10_2d | 1.10 (1.04, 1.17) | P90/10_2d | 1.016 (1.009, 1.024) |
| P90_3d | 1.22 (1.14, 1.31) | P10_3d | 1.10 (1.04, 1.17) | P90/10_3d | 1.016 (1.008, 1.023) |
| P90_4d | 1.23 (1.14, 1.32) | P10_4d | 1.10 (1.03, 1.18) | P90/10_4d | 1.015 (1.008, 1.023) |
| P92.5_2d | 1.27 (1.18, 1.36) | P7.5_2d | 1.11 (1.04, 1.18) | P92.5/7.5_2d | 1.016 (1.008, 1.023) |
| P92.5_3d | 1.25 (1.16, 1.35) | P7.5_3d | 1.10 (1.02, 1.18) | P92.5/7.5_3d | 1.015 (1.007, 1.022) |
| P92.5_4d | 1.25 (1.16, 1.36) | P7.5_4d | 1.11 (1.02, 1.20) | P92.5/7.5_4d | 1.014 (1.007, 1.022) |
| P95_2d | 1.36 (1.25, 1.48) | P5_2d | 1.08 (1.002, 1.17) | P95/5_2d | 1.015 (1.007, 1.022) |
| P95_3d | 1.35 (1.24, 1.48) | P5_3d | 1.08 (0.99, 1.18) | P95/5_3d | 1.014 (1.007, 1.021) |
| P95_4d | 1.35 (1.22, 1.48) | P5_4d | 1.11 (1.002, 1.22) | P95/5_4d | 1.013 (1.006, 1.021) |
| P97.5_2d | 1.53 (1.36, 1.71) | P2.5_2d | 1.16 (1.04, 1.28) | P97.5/2.5_2d | 1.014 (1.007, 1.022) |
| P97.5_3d | 1.60 (1.40, 1.81) | P2.5_3d | 1.17 (1.03, 1.33) | P97.5/2.5_3d | 1.014 (1.007, 1.022) |
| P97.5_4d | 1.59 (1.38, 1.84) | P2.5_4d | 1.18 (1.01, 1.38) | P97.5/2.5_4d | 1.013 (1.006, 1.021) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zheng, Y.; Xu, R.; Chen, Y.; Li, Y.; Bi, Y.; Jia, X.; Wang, S.; Luo, L.; Wei, J.; Wang, R.; et al. Opposite Interactive Effects of Heat Wave and Cold Spell with Fine Particulate Matter on Pneumonia Mortality. Toxics 2025, 13, 702. https://doi.org/10.3390/toxics13080702
Zheng Y, Xu R, Chen Y, Li Y, Bi Y, Jia X, Wang S, Luo L, Wei J, Wang R, et al. Opposite Interactive Effects of Heat Wave and Cold Spell with Fine Particulate Matter on Pneumonia Mortality. Toxics. 2025; 13(8):702. https://doi.org/10.3390/toxics13080702
Chicago/Turabian StyleZheng, Yi, Ruijun Xu, Yuling Chen, Yingxin Li, Yuxin Bi, Xiaohong Jia, Sirong Wang, Lu Luo, Jing Wei, Rui Wang, and et al. 2025. "Opposite Interactive Effects of Heat Wave and Cold Spell with Fine Particulate Matter on Pneumonia Mortality" Toxics 13, no. 8: 702. https://doi.org/10.3390/toxics13080702
APA StyleZheng, Y., Xu, R., Chen, Y., Li, Y., Bi, Y., Jia, X., Wang, S., Luo, L., Wei, J., Wang, R., Shi, C., Lv, Z., Huang, S., Chen, G., Sun, H., Sun, B., Feng, N., & Liu, Y. (2025). Opposite Interactive Effects of Heat Wave and Cold Spell with Fine Particulate Matter on Pneumonia Mortality. Toxics, 13(8), 702. https://doi.org/10.3390/toxics13080702









