Influence of Microplastics on Manifestations of Experimental Chronic Colitis
Highlights
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Experimental Groups
2.3. Microplastic Consumption Model
2.4. Chronic Colitis Model
2.5. Evaluation of Fluid Intake
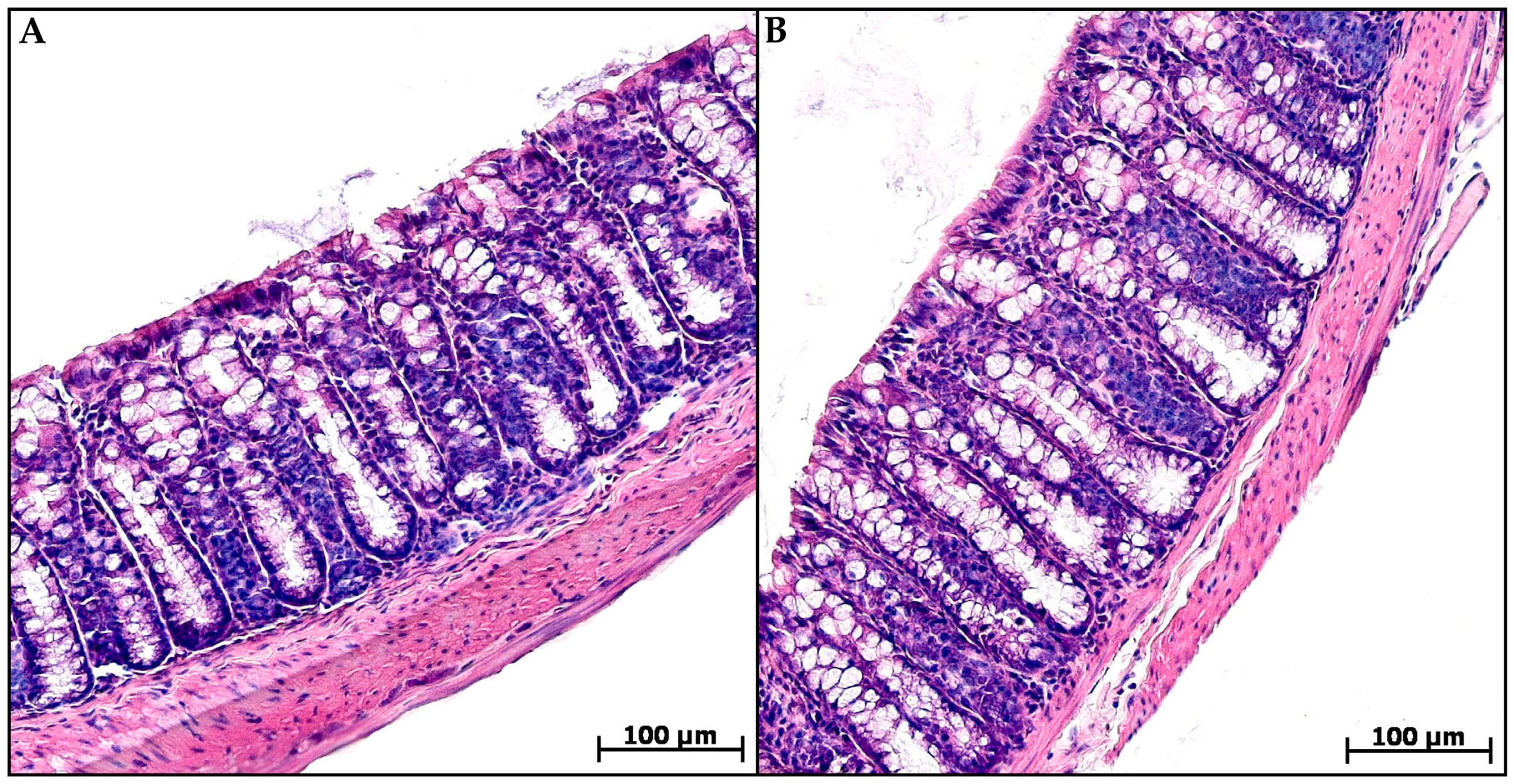
2.6. Histological Study of the Colon
2.6.1. Preparation of Histological Specimens
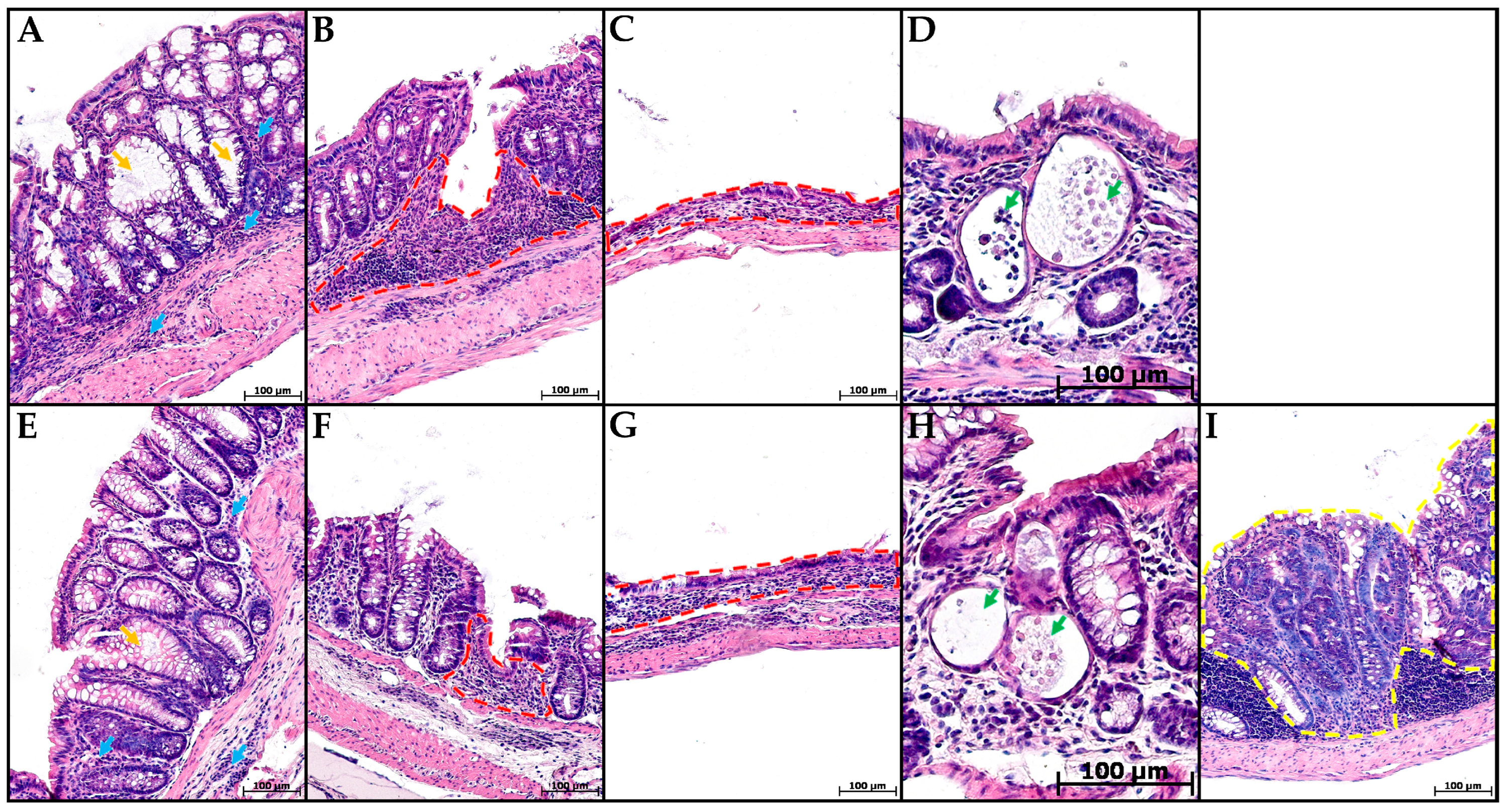
2.6.2. Prevalence of the Pathological Process
2.6.3. Severity of Inflammatory Infiltration
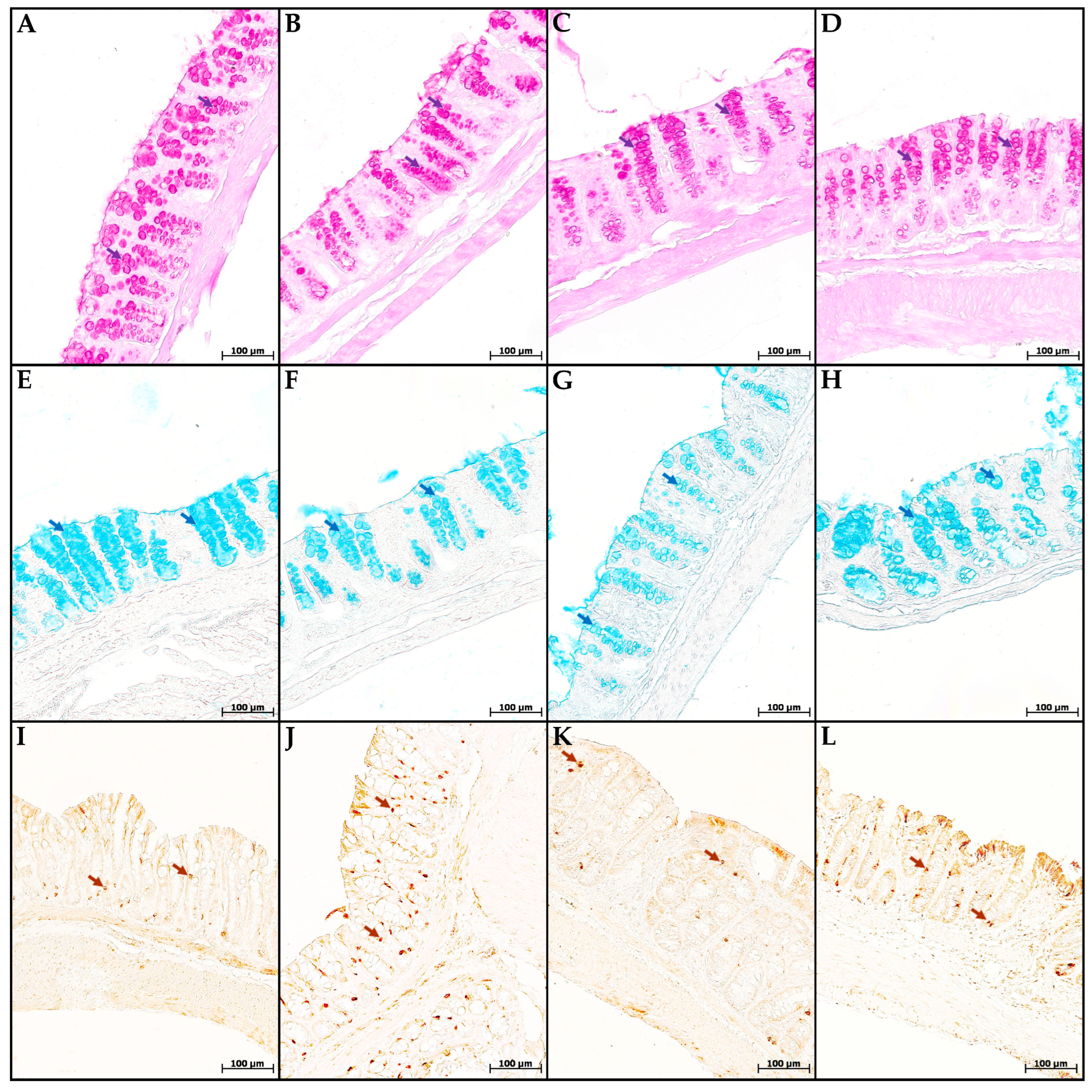
2.6.4. Goblet Cell Content and Mucus Properties
2.6.5. Enteroendocrine Cell Content
2.7. Real-Time PCR
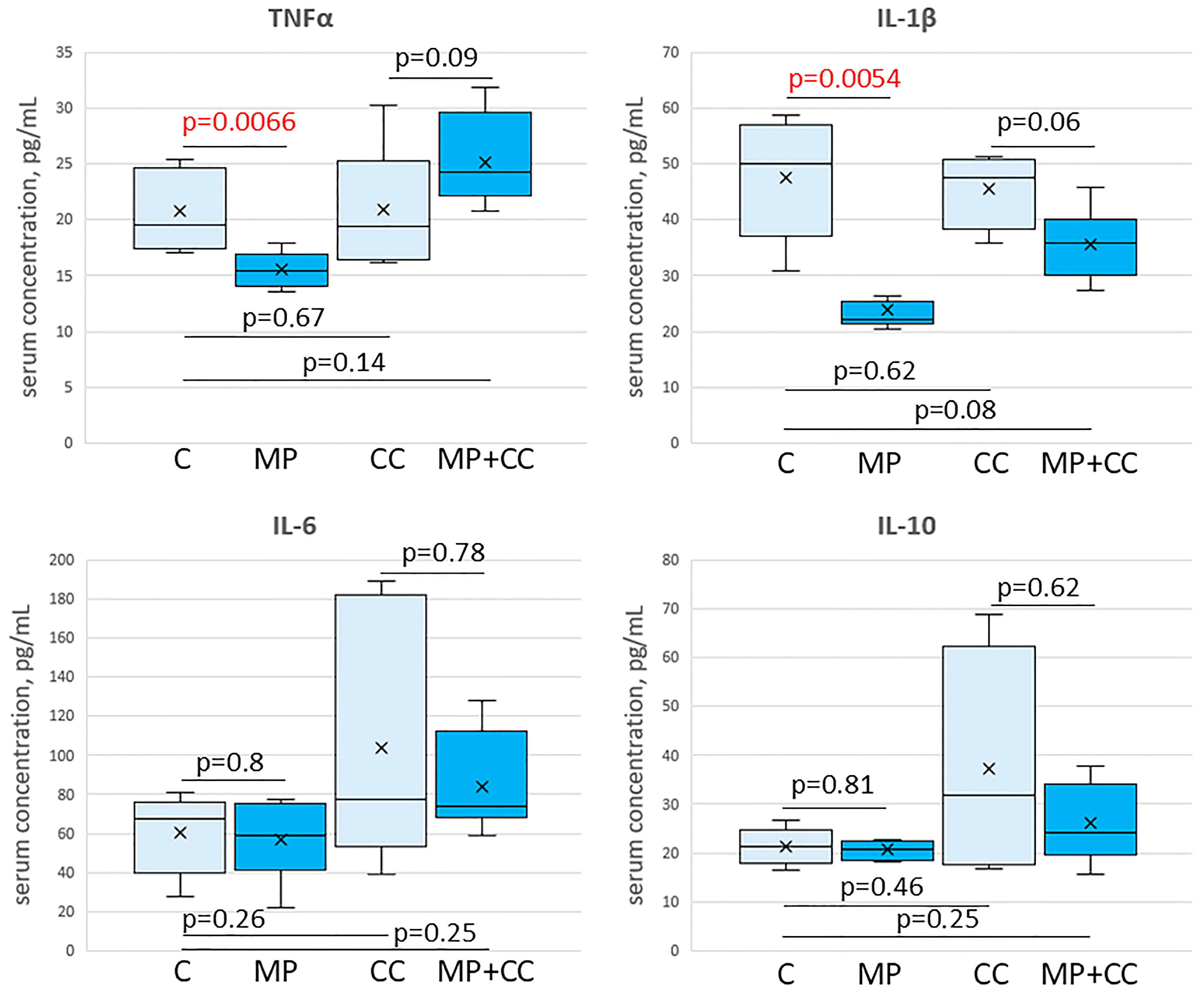
2.8. ELISA
2.9. Statistics
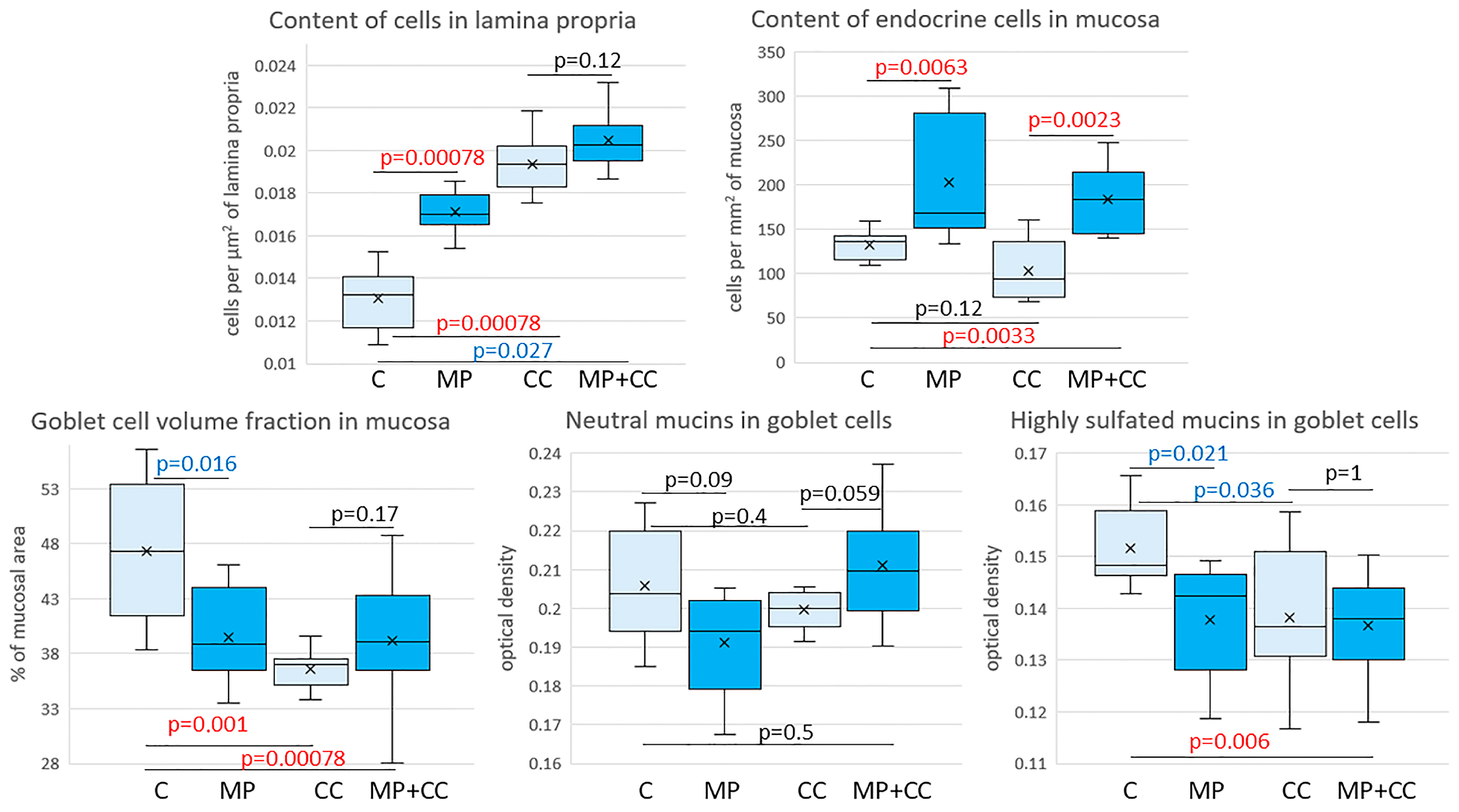
3. Results
4. Discussion
4.1. Microplastic Consumption
4.2. Effect of MP on the Colon of Healthy Mice
4.3. Chronic Colitis Model
4.4. Effect of MP on the Chronic Colitis Severity
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Actb | Actin beta |
| Bax | BCL2 associated X, apoptosis regulator |
| C | control |
| CC | chronic colitis |
| Cldn | claudin |
| DSS | Dextran sulfate sodium salt |
| IBD | Inflammatory bowel disease |
| IFNγ | interferon gamma |
| IL | interleukin |
| Mki67 | marker of proliferation Ki-67 |
| MP | microplastic |
| Muc | mucin |
| PAS | Periodic acid–Schiff |
| PE | polyethylene |
| PS | polystyrene |
| TNFα | tumor necrosis factor alpha |
| UC | Ulcerative colitis |
References
- Dube, E.; Okuthe, G.E. Plastics and Micro/Nano-Plastics (MNPs) in the Environment: Occurrence, Impact, and Toxicity. Int. J. Environ. Res. Public Health 2023, 20, 6667. [Google Scholar] [CrossRef]
- Kutralam-Muniasamy, G.; Shruti, V.C.; Pérez-Guevara, F.; Roy, P.D. Microplastic Diagnostics in Humans: “The 3Ps” Progress, Problems, and Prospects. Sci. Total Environ. 2023, 856, 159164. [Google Scholar] [CrossRef]
- Chen, X.; Wang, S.; Mao, X.; Xiang, X.; Ye, S.; Chen, J.; Zhu, A.; Meng, Y.; Yang, X.; Peng, S.; et al. Adverse Health Effects of Emerging Contaminants on Inflammatory Bowel Disease. Front. Public Health 2023, 11, 1140786. [Google Scholar] [CrossRef]
- Zhao, Y.; Liu, S.; Xu, H. Effects of Microplastic and Engineered Nanomaterials on Inflammatory Bowel Disease: A Review. Chemosphere 2023, 326, 138486. [Google Scholar] [CrossRef]
- Ji, J.; Wu, X.; Li, X.; Zhu, Y. Effects of Microplastics in Aquatic Environments on Inflammatory Bowel Disease. Environ. Res. 2023, 229, 115974. [Google Scholar] [CrossRef]
- Yan, Z.; Liu, Y.; Zhang, T.; Zhang, F.; Ren, H.; Zhang, Y. Analysis of Microplastics in Human Feces Reveals a Correlation between Fecal Microplastics and Inflammatory Bowel Disease Status. Environ. Sci. Technol. 2022, 56, 414–421. [Google Scholar] [CrossRef]
- Sokic-Milutinovic, A.; Milosavljevic, T. Inflammatory Bowel Disease: From Conventional Immunosuppression to Biologic Therapy. Dig. Dis. 2024, 42, 325–335. [Google Scholar] [CrossRef]
- Wang, R.; Li, Z.; Liu, S.; Zhang, D. Global, regional and national burden of inflammatory bowel disease in 204 countries and territories from 1990 to 2019: A systematic analysis based on the Global Burden of Disease Study 2019. BMJ Open 2023, 13, e065186. [Google Scholar] [CrossRef]
- Zolotova, N.; Dzhalilova, D.; Tsvetkov, I.; Silina, M.; Fokichev, N.; Makarova, O. Microplastic Effects on Mouse Colon in Normal and Colitis Conditions: A Literature Review. PeerJ 2025, 13, e18880. [Google Scholar] [CrossRef]
- Zolotova, N.; Dzhalilova, D.; Tsvetkov, I.; Makarova, O. Influence of Microplastics on Morphological Manifestations of Experimental Acute Colitis. Toxics 2023, 11, 730. [Google Scholar] [CrossRef]
- Zheng, H.; Wang, J.; Wei, X.; Chang, L.; Liu, S. Proinflammatory Properties and Lipid Disturbance of Polystyrene Microplastics in the Livers of Mice with Acute Colitis. Sci. Total Environ. 2021, 750, 143085. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Li, H.; Wang, J.; Wu, B.; Guo, X. Polystyrene Microplastics Aggravate Inflammatory Damage in Mice with Intestinal Immune Imbalance. Sci. Total Environ. 2022, 833, 155198. [Google Scholar] [CrossRef] [PubMed]
- Luo, T.; Wang, D.; Zhao, Y.; Li, X.; Yang, G.; Jin, Y. Polystyrene Microplastics Exacerbate Experimental Colitis in Mice Tightly Associated with the Occurrence of Hepatic Inflammation. Sci. Total Environ. 2022, 844, 156884. [Google Scholar] [CrossRef] [PubMed]
- Xie, S.; Zhang, R.; Li, Z.; Liu, C.; Chen, Y.; Yu, Q. Microplastics Perturb Colonic Epithelial Homeostasis Associated with Intestinal Overproliferation, Exacerbating the Severity of Colitis. Environ. Res. 2023, 217, 114861. [Google Scholar] [CrossRef]
- Ma, J.; Wan, Y.; Song, L.; Wang, L.; Wang, H.; Li, Y.; Huang, D. Polystyrene Nanobeads Exacerbate Chronic Colitis in Mice Involving in Oxidative Stress and Hepatic Lipid Metabolism. Part. Fibre Toxicol. 2023, 20, 49. [Google Scholar] [CrossRef]
- Schwarzfischer, M.; Niechcial, A.; Lee, S.S.; Sinnet, B.; Wawrzyniak, M.; Laimbacher, A.; Atrott, K.; Manzini, R.; Morsy, Y.; Häfliger, J.; et al. Ingested Nano- and Microsized Polystyrene Particles Surpass the Intestinal Barrier and Accumulate in the Body. NanoImpact 2022, 25, 100374. [Google Scholar] [CrossRef]
- Cross, E.; Saunders, B.; Farmer, A.D.; Prior, J.A. Diagnostic delay in adult inflammatory bowel disease: A systematic review. Indian. J. Gastroenterol. 2023, 42, 40–52. [Google Scholar] [CrossRef]
- Rosenberg, L.; Lawlor, G.O.; Zenlea, T.; Goldsmith, J.D.; Gifford, A.; Falchuk, K.R.; Wolf, J.L.; Cheifetz, A.S.; Robson, S.C.; Moss, A.C. Predictors of endoscopic inflammation in patients with ulcerative colitis in clinical remission. Inflamm. Bowel Dis. 2013, 19, 779–784. [Google Scholar] [CrossRef]
- Eichele, D.D.; Kharbanda, K.K. Dextran Sodium Sulfate Colitis Murine Model: An Indispensable Tool for Advancing Our Understanding of Inflammatory Bowel Diseases Pathogenesis. World J. Gastroenterol. 2017, 23, 6016–6029. [Google Scholar] [CrossRef]
- Perše, M.; Cerar, A. Dextran Sodium Sulphate Colitis Mouse Model: Traps and Tricks. J. Biomed. Biotechnol. 2012, 2012, 718617. [Google Scholar] [CrossRef]
- Pavel, C.; Diculescu, M.M.; Stepan, A.E.; Constantinescu, G.; Sandru, V.; Ţieranu, C.G.; Tomescu, L.; Constantinescu, A.; Patoni, C.; Plotogea, O.M.; et al. Considering Histologic Remission in Ulcerative Colitis as a Long-Term Target. J. Clin. Med. 2024, 13, 289. [Google Scholar] [CrossRef]
- Li, B.; Ding, Y.; Cheng, X.; Sheng, D.; Xu, Z.; Rong, Q.; Wu, Y.; Zhao, H.; Ji, X.; Zhang, Y. Polyethylene Microplastics Affect the Distribution of Gut Microbiota and Inflammation Development in Mice. Chemosphere 2020, 244, 125492. [Google Scholar] [CrossRef]
- Wen, S.; Zhao, Y.; Liu, S.; Chen, Y.; Yuan, H.; Xu, H. Polystyrene Microplastics Exacerbated Liver Injury from Cyclophosphamide in Mice: Insight into Gut Microbiota. Sci. Total Environ. 2022, 840, 156668. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Li, Q.; Shi, C.; Lv, J.; Xu, Y.; Yang, J.; Chua, S.L.; Jia, L.; Chen, H.; Liu, Q.; et al. Oligomer Nanoparticle Release from Polylactic Acid Plastics Catalysed by Gut Enzymes Triggers Acute Inflammation. Nat. Nanotechnol. 2023, 18, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Yang, B.; Zhu, X.; Li, Q.; Song, E.; Song, Y. Oral Exposure of Polystyrene Microplastics and Doxycycline Affects Mice Neurological Function via Gut Microbiota Disruption: The Orchestrating Role of Fecal Microbiota Transplantation. J. Hazard. Mater. 2024, 467, 133714. [Google Scholar] [CrossRef] [PubMed]
- Zolotova, N.A.; Akhrieva, K.M.; Zayratyants, O.V. Epithelial barrier of the colon in health and patients with ulcerative colitis. Exp. Clin. Gastroenterol. 2019, 2, 4–13. (In Russian) [Google Scholar] [CrossRef]
- Dunleavy, K.A.; Raffals, L.E.; Camilleri, M. Intestinal Barrier Dysfunction in Inflammatory Bowel Disease: Underpinning Pathogenesis and Therapeutics. Dig. Dis. Sci. 2023, 68, 4306–4320. [Google Scholar] [CrossRef]
- Neurath, M.F.; Artis, D.; Becker, C. The intestinal barrier: A pivotal role in health, inflammation, and cancer. Lancet Gastroenterol. Hepatol. 2025, 10, 573–592. [Google Scholar] [CrossRef]
- Hou, B.; Wang, F.; Liu, T.; Wang, Z. Reproductive Toxicity of Polystyrene Microplastics: In Vivo Experimental Study on Testicular Toxicity in Mice. J. Hazard. Mater. 2021, 405, 124028. [Google Scholar] [CrossRef]
- Zou, H.; Qu, H.; Bian, Y.; Sun, J.; Wang, T.; Ma, Y.; Yuan, Y.; Gu, J.; Bian, J.; Liu, Z. Polystyrene Microplastics Induce Oxidative Stress in Mouse Hepatocytes in Relation to Their Size. Int. J. Mol. Sci. 2023, 24, 7382. [Google Scholar] [CrossRef]
- Garcia-Hernandez, V.; Neumann, P.A.; Koch, S.; Lyons, R.; Nusrat, A.; Parkos, C.A. Systematic Scoring Analysis for Intestinal Inflammation in a Murine Dextran Sodium Sulfate-Induced Colitis Model. J. Vis. Exp. 2021, 168, e62135. [Google Scholar] [CrossRef] [PubMed]
- Senathirajah, K.; Attwood, S.; Bhagwat, G.; Carbery, M.; Wilson, S.; Palanisami, T. Estimation of the Mass of Microplastics Ingested—A Pivotal First Step towards Human Health Risk Assessment. J. Hazard. Mater. 2021, 404, 124004. [Google Scholar] [CrossRef]
- EFSA Panel on Contaminants in the Food Chain (CONTAM). Presence of microplastics and nanoplastics in food, with particular focus on seafood. EFSA J. 2016, 14, e04501. [Google Scholar] [CrossRef] [PubMed]
- Liang, B.; Zhong, Y.; Huang, Y.; Lin, X.; Liu, J.; Lin, L.; Hu, M.; Jiang, J.; Dai, M.; Wang, B.; et al. Underestimated Health Risks: Polystyrene Micro- and Nanoplastics Jointly Induce Intestinal Barrier Dysfunction by ROS-Mediated Epithelial Cell Apoptosis. Part. Fibre Toxicol. 2021, 18, 20. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Chen, N.; Yang, X.; Xia, Y.; Wu, D. Effects Induced by Polyethylene Microplastics Oral Exposure on Colon Mucin Release, Inflammation, Gut Microflora Composition and Metabolism in Mice. Ecotoxicol. Environ. Saf. 2021, 220, 112340. [Google Scholar] [CrossRef]
- Zha, H.; Tang, R.; Li, S.; Zhuge, A.; Xia, J.; Lv, J.; Wang, S.; Wang, K.; Zhang, H.; Li, L. Effects of Partial Reduction of Polystyrene Micro-Nanoplastics on the Immunity, Gut Microbiota and Metabolome of Mice. Chemosphere 2024, 349, 140940. [Google Scholar] [CrossRef]
- Choi, Y.J.; Park, J.W.; Kim, J.E.; Lee, S.J.; Gong, J.E.; Jung, Y.-S.; Seo, S.; Hwang, D.Y. Novel Characterization of Constipation Phenotypes in ICR Mice Orally Administrated with Polystyrene Microplastics. Int. J. Mol. Sci. 2021, 22, 5845. [Google Scholar] [CrossRef]
- Huang, J.; Sun, X.; Wang, Y.; Su, J.; Li, G.; Wang, X.; Yang, Y.; Zhang, Y.; Li, B.; Zhang, G.; et al. Biological Interactions of Polystyrene Nanoplastics: Their Cytotoxic and Immunotoxic Effects on the Hepatic and Enteric Systems. Ecotoxicol. Environ. Saf. 2023, 264, 115447. [Google Scholar] [CrossRef]
- Djouina, M.; Vignal, C.; Dehaut, A.; Caboche, S.; Hirt, N.; Waxin, C.; Himber, C.; Beury, D.; Hot, D.; Dubuquoy, L.; et al. Oral Exposure to Polyethylene Microplastics Alters Gut Morphology, Immune Response, and Microbiota Composition in Mice. Environ. Res. 2022, 212, 113230. [Google Scholar] [CrossRef]
- Xie, L.; Chen, T.; Liu, J.; Hou, Y.; Tan, Q.; Zhang, X.; Li, Z.; Farooq, T.H.; Yan, W.; Li, Y. Intestinal Flora Variation Reflects the Short-Term Damage of Microplastic to the Intestinal Tract in Mice. Ecotoxicol. Environ. Saf. 2022, 246, 114194. [Google Scholar] [CrossRef]
- Wang, J.; Tian, H.; Shi, Y.; Yang, Y.; Yu, F.; Cao, H.; Gao, L.; Liu, M. The Enhancement in Toxic Potency of Oxidized Functionalized Polyethylene-Microplastics in Mice Gut and Caco-2 Cells. Sci. Total Environ. 2023, 903, 166057. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.J.; Kim, J.E.; Lee, S.J.; Gong, J.E.; Jin, Y.J.; Seo, S.; Lee, J.H.; Hwang, D.Y. Inflammatory Response in the Mid Colon of ICR Mice Treated with Polystyrene Microplastics for Two Weeks. Lab. Anim. Res. 2021, 37, 31. [Google Scholar] [CrossRef] [PubMed]
- Shi, C.; Han, X.; Guo, W.; Wu, Q.; Yang, X.; Wang, Y.; Tang, G.; Wang, S.; Wang, Z.; Liu, Y.; et al. Disturbed Gut-Liver Axis Indicating Oral Exposure to Polystyrene Microplastic Potentially Increases the Risk of Insulin Resistance. Environ. Int. 2022, 164, 107273. [Google Scholar] [CrossRef] [PubMed]
- Jia, R.; Han, J.; Liu, X.; Li, K.; Lai, W.; Bian, L.; Yan, J.; Xi, Z. Exposure to Polypropylene Microplastics via Oral Ingestion Induces Colonic Apoptosis and Intestinal Barrier Damage through Oxidative Stress and Inflammation in Mice. Toxics 2023, 11, 127. [Google Scholar] [CrossRef]
- Wang, L.; Chen, J.; Zhang, X.; Xu, M.; Zhang, X.; Zhao, W.; Cui, J. Effects of Microplastics and Tetracycline on Intestinal Injury in Mice. Chemosphere 2023, 337, 139364. [Google Scholar] [CrossRef]
- Zeng, G.; Li, J.; Wang, Y.; Su, J.; Lu, Z.; Zhang, F.; Ding, W. Polystyrene Microplastic-Induced Oxidative Stress Triggers Intestinal Barrier Dysfunction via the NF-κB/NLRP3/IL-1β/MCLK Pathway. Environ. Pollut. 2024, 345, 123473. [Google Scholar] [CrossRef]
- Chen, X.; Zhuang, J.; Chen, Q.; Xu, L.; Yue, X.; Qiao, D. Polyvinyl Chloride Microplastics Induced Gut Barrier Dysfunction, Microbiota Dysbiosis and Metabolism Disorder in Adult Mice. Ecotoxicol. Environ. Saf. 2022, 241, 113809. [Google Scholar] [CrossRef]
- Shaoyong, W.; Jin, H.; Jiang, X.; Xu, B.; Liu, Y.; Wang, Y.; Jin, M. Benzo [a] Pyrene-Loaded Aged Polystyrene Microplastics Promote Colonic Barrier Injury via Oxidative Stress-Mediated Notch Signalling. J. Hazard. Mater. 2023, 457, 131820. [Google Scholar] [CrossRef]
- Pelaseyed, T.; Bergström, J.H.; Gustafsson, J.K.; Ermund, A.; Birchenough, G.M.H.; Schütte, A.; van der Post, S.; Svensson, F.; Rodríguez-Piñeiro, A.M.; Nyström, E.E.L.; et al. The Mucus and Mucins of the Goblet Cells and Enterocytes Provide the First Defense Line of the Gastrointestinal Tract and Interact with the Immune System. Immunol. Rev. 2014, 260, 8–20. [Google Scholar] [CrossRef]
- Fontaine, N.; Meslin, J.C.; Doré, J. Selective in Vitro Degradation of the Sialylated Fraction of Germ-Free Rat Mucins by the Caecal Flora of the Rat. Reprod. Nutr. Dev. 1998, 38, 289–296. [Google Scholar] [CrossRef]
- Robertson, A.M.; Wright, D.P. Bacterial Glycosulphatases and Sulphomucin Degradation. Can. J. Gastroenterol. 1997, 11, 361–366. [Google Scholar] [CrossRef]
- Park, S.B.; Jung, W.H.; Choi, K.J.; Koh, B.; Kim, K.Y. A Comparative Systematic Analysis of The Influence of Microplastics on Colon Cells, Mouse and Colon Organoids. Tissue Eng. Regen. Med. 2023, 20, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Johansson, M.E.V.; Sjövall, H.; Hansson, G.C. The Gastrointestinal Mucus System in Health and Disease. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 352–361. [Google Scholar] [CrossRef]
- Jonckheere, N.; Skrypek, N.; Frénois, F.; Van Seuningen, I. Membrane-Bound Mucin Modular Domains: From Structure to Function. Biochimie 2013, 95, 1077–1086. [Google Scholar] [CrossRef] [PubMed]
- Capaldo, C.T. Claudin Barriers on the Brink: How Conflicting Tissue and Cellular Priorities Drive IBD Pathogenesis. Int. J. Mol. Sci. 2023, 24, 8562. [Google Scholar] [CrossRef] [PubMed]
- Serigado, J.M.; Foulke-Abel, J.; Hines, W.C.; Hanson, J.A.; In, J.; Kovbasnjuk, O. Ulcerative Colitis: Novel Epithelial Insights Provided by Single Cell RNA Sequencing. Front. Med. 2022, 9, 868508. [Google Scholar] [CrossRef]
- Nishida, M.; Yoshida, M.; Nishiumi, S.; Furuse, M.; Azuma, T. Claudin-2 Regulates Colorectal Inflammation via Myosin Light Chain Kinase-Dependent Signaling. Dig. Dis. Sci. 2013, 58, 1546–1559. [Google Scholar] [CrossRef]
- Ahmad, R.; Chaturvedi, R.; Olivares-Villagómez, D.; Habib, T.; Asim, M.; Shivesh, P.; Polk, D.B.; Wilson, K.T.; Washington, M.K.; Van Kaer, L.; et al. Targeted Colonic Claudin-2 Expression Renders Resistance to Epithelial Injury, Induces Immune Suppression, and Protects from Colitis. Mucosal Immunol. 2014, 7, 1340–1353. [Google Scholar] [CrossRef]
- Gunawardene, A.R.; Corfe, B.M.; Staton, C.A. Classification and Functions of Enteroendocrine Cells of the Lower Gastrointestinal Tract. Int. J. Exp. Pathol. 2011, 92, 219–231. [Google Scholar] [CrossRef]
- Shajib, M.S.; Khan, W.I. The Role of Serotonin and Its Receptors in Activation of Immune Responses and Inflammation. Acta Physiol. 2015, 213, 561–574. [Google Scholar] [CrossRef]
- Liang, Y.; Liu, D.; Zhan, J.; Liu, X.; Li, P.; Ma, X.; Hou, H.; Wang, P. Polystyrene Microplastics Induce Kidney Injury via Gut Barrier Dysfunction and C5a/C5aR Pathway Activation. Environ. Pollut. 2024, 342, 122909. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Ye, Y.; Han, Y.; Wang, Q.; Lu, H.; Li, J.; Qian, W.; Zeng, X.; Zhang, Z.; Zhao, Y.; et al. Microplastics Dampen the Self-Renewal of Hematopoietic Stem Cells by Disrupting the Gut Microbiota-Hypoxanthine-Wnt Axis. Cell Discov. 2024, 10, 35. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Wang, Z.; Xiang, Q.; Wu, B.; Lv, W.; Xu, S. A Comparative Study in Healthy and Diabetic Mice Followed the Exposure of Polystyrene Microplastics: Differential Lipid Metabolism and Inflammation Reaction. Ecotoxicol. Environ. Saf. 2022, 244, 114031. [Google Scholar] [CrossRef] [PubMed]
- DeRoche, T.C.; Xiao, S.-Y.; Liu, X. Histological Evaluation in Ulcerative Colitis. Gastroenterol. Rep. 2014, 2, 178–192. [Google Scholar] [CrossRef]
- Chassaing, B.; Aitken, J.D.; Malleshappa, M.; Vijay-Kumar, M. Dextran Sulfate Sodium (DSS)-Induced Colitis in Mice. Curr. Protoc. Immunol. 2014, 104, 15–25. [Google Scholar] [CrossRef]
- Corfield, A.P.; Carroll, D.; Myerscough, N.; Probert, C.S. Mucins in the Gastrointestinal Tract in Health and Disease. Front. Biosci. 2001, 6, D1321–D1357. [Google Scholar] [CrossRef]
- Clapper, M.L.; Cooper, H.S.; Chang, W.-C.L. Dextran Sulfate Sodium-Induced Colitis-Associated Neoplasia: A Promising Model for the Development of Chemopreventive Interventions. Acta Pharmacol. Sin. 2007, 28, 1450–1459. [Google Scholar] [CrossRef]
- Bopanna, S.; Ananthakrishnan, A.N.; Kedia, S.; Yajnik, V.; Ahuja, V. Risk of Colorectal Cancer in Asian Patients with Ulcerative Colitis: A Systematic Review and Meta-Analysis. Lancet Gastroenterol. Hepatol. 2017, 2, 269–276. [Google Scholar] [CrossRef]
- Longman, R.J.; Poulsom, R.; Corfield, A.P.; Warren, B.F.; Wright, N.A.; Thomas, M.G. Alterations in the Composition of the Supramucosal Defense Barrier in Relation to Disease Severity of Ulcerative Colitis. J. Histochem. Cytochem. 2006, 54, 1335–1348. [Google Scholar] [CrossRef]
- Petersson, J.; Schreiber, O.; Hansson, G.C.; Gendler, S.J.; Velcich, A.; Lundberg, J.O.; Roos, S.; Holm, L.; Phillipson, M. Importance and Regulation of the Colonic Mucus Barrier in a Mouse Model of Colitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2011, 300, G327–G333. [Google Scholar] [CrossRef]
- Zolotova, N.A.; Polikarpova, A.V.; Khochanskii, D.N.; Makarova, O.V.; Mikhailova, L.P. Expression of Mucins and Claudins in the Colon during Acute and Chronic Experimental Colitis. Bull. Exp. Biol. Med. 2018, 165, 434–437. [Google Scholar] [CrossRef]
- Zolotova, N.A.; Khochansky, D.N.; Polikarpova, A.V.; Dobrynina, M.T.; Makarova, O.V. Cytophysiological characteristics of epithelial secretory cells of different parts of the colon in experimental ulcerative colitis. Clin. Exp. Morphol. 2016, 2, 29–37. (In Russian) [Google Scholar]
- Ahmad, T.; Marshall, S.-E.; Jewell, D. Genetics of Inflammatory Bowel Disease: The Role of the HLA Complex. World J. Gastroenterol. 2006, 12, 3628–3635. [Google Scholar] [CrossRef]
- Ding, L.; Lu, Z.; Foreman, O.; Tatum, R.; Lu, Q.; Renegar, R.; Cao, J.; Chen, Y.-H. Inflammation and Disruption of the Mucosal Architecture in Claudin-7-Deficient Mice. Gastroenterology 2012, 142, 305–315. [Google Scholar] [CrossRef]

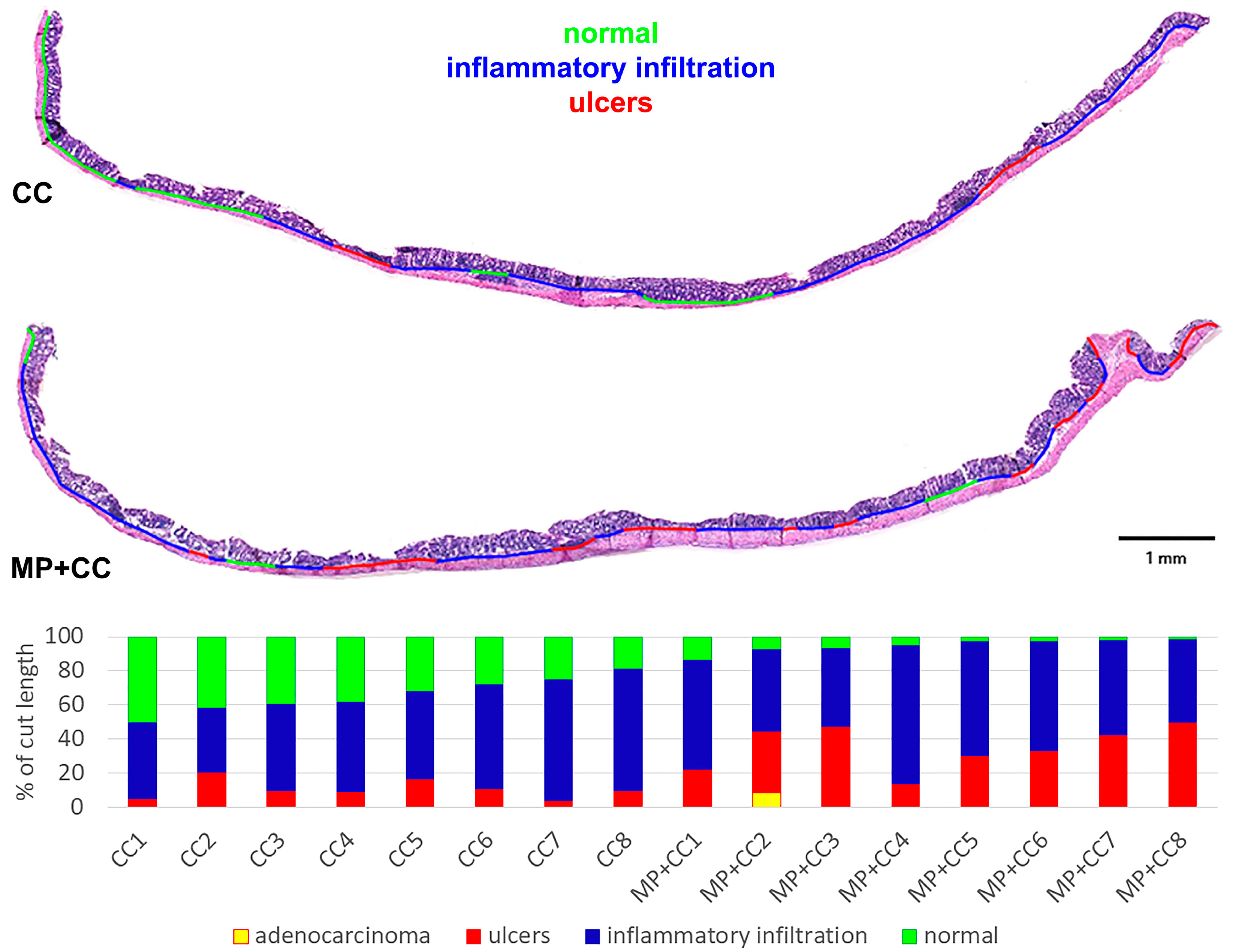
| Group | Prevalence of All Pathological Changes, % | Prevalence of Ulcers, % | Prevalence of Inflammatory Infiltration, % | Number of Crypt Abscesses per Section |
|---|---|---|---|---|
| CC | 65.2 (60.1; 72.9) | 9.7 (8.1; 12.4) | 53.0 (51.3; 66.1) | 0 (0; 1) |
| MP+CC | 96.2 (93.3; 97.8) | 34.8 (28.3; 43.7) | 55.7 (48.4; 65.6) | 1.5 (1; 2) |
| p | 0.00078 | 0.0016 | 0.6 | 0.021 |
| Groups | ||||
|---|---|---|---|---|
| Genes | C | MP | CC | MP+CC |
| Muc1 | 0.28 (0.11; 0.48) | 0.14 (0; 0.18) P(MP/C) = 0.39 | 0 (0; 0) P(CC/C) = 0.007 ↓↓ | 0 (0; 0) P(MP+CC/C) = 0.012 ↓ P(MP+CC/C) = 1 |
| Muc3 | 130 (11; 1610) | 31 (10; 735) P(MP/C) = 0.87 | 485 (122; 2594) P(CC/C) = 0.13 | 574 (502; 2771) P(MP+CC/C) = 0.17 P(MP+CC/C) = 0.53 |
| Muc13 | 1.36 (0.07; 19.15) | 0.47 (0.01; 16.08) P(MP/C) = 0.71 | 2.53 (1.90; 11.64) P(CC/C) = 0.052 | 6.32 (1.82; 13.92) P(MP+CC/C) = 0.42 P(MP+CC/C) = 0.36 |
| Cldn2 | 0.18 (0.08; 0.27) | 0.63 (0.22; 1.74) P(MP/C) = 0.040 ↑ | 0.26 (0; 0.51) P(CC/C) = 0.71 | 0 (0; 0.04) P(MP+CC/C) = 0.036 ↓ P(MP+CC/C) = 0.044 ↓ |
| Cldn4 | 1.15 (0.30; 15.02) | 0.87 (0.02; 5.42) P(MP/C) = 0.32 | 2.19 (0.06; 10.54) P(CC/C) = 0.53 | 10.9 (2.66; 12.74) P(MP+CC/C) = 0.33 P(MP+CC/C) = 0.076 |
| Cldn7 | 0.48 (0.14; 18.00) | 0.06 (0; 4.21) P(MP/C) = 0.13 | 1.92 (0.20; 6.36) P(CC/C) = 0.55 | 12.52 (5.25; 25.67) P(MP+CC/C) = 0.27 P(MP+CC/C) = 0.026 ↑ |
| Bax | 1.95 (0.5; 9.09) | 1.07 (0.58; 1.07) P(MP/C) = 0.44 | 3.04 (0; 8.92) P(CC/C) = 0.72 | 5.63 (0; 12.6) P(MP+CC/C) = 0.95 P(MP+CC/C) = 0.74 |
| Mki67 | 0.22 (0.01; 3.24) | 0.3 (0.15; 1.27) P(MP/C) = 0.72 | 1.54 (0.12; 6.63) P(CC/C) = 0.47 | 0.14 (0; 5.74) P(MP+CC/C) = 0.75 P(MP+CC/C) = 0.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zolotova, N.; Silina, M.; Dzhalilova, D.; Tsvetkov, I.; Fokichev, N.; Makarova, O. Influence of Microplastics on Manifestations of Experimental Chronic Colitis. Toxics 2025, 13, 701. https://doi.org/10.3390/toxics13080701
Zolotova N, Silina M, Dzhalilova D, Tsvetkov I, Fokichev N, Makarova O. Influence of Microplastics on Manifestations of Experimental Chronic Colitis. Toxics. 2025; 13(8):701. https://doi.org/10.3390/toxics13080701
Chicago/Turabian StyleZolotova, Natalia, Maria Silina, Dzhuliia Dzhalilova, Ivan Tsvetkov, Nikolai Fokichev, and Olga Makarova. 2025. "Influence of Microplastics on Manifestations of Experimental Chronic Colitis" Toxics 13, no. 8: 701. https://doi.org/10.3390/toxics13080701
APA StyleZolotova, N., Silina, M., Dzhalilova, D., Tsvetkov, I., Fokichev, N., & Makarova, O. (2025). Influence of Microplastics on Manifestations of Experimental Chronic Colitis. Toxics, 13(8), 701. https://doi.org/10.3390/toxics13080701







