Airborne Dental Material Particulates and Occupational Exposure: Computational and Field Insights into Airflow Dynamics and Control Strategies
Abstract
1. Introduction
1.1. Computational Fluid Dynamics (CFD) Applications in Dental Settings
1.2. Engineering Controls and Mitigation Strategies
2. Materials and Methods
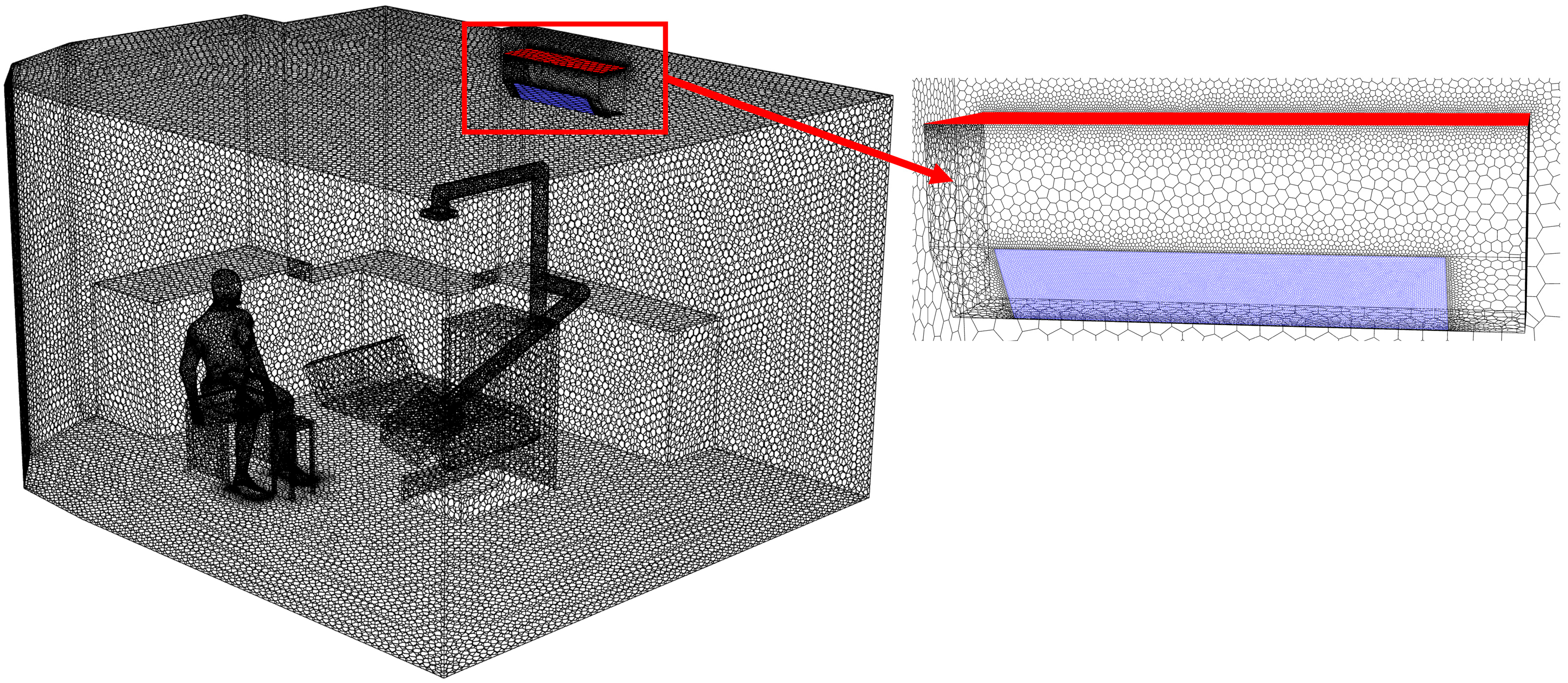
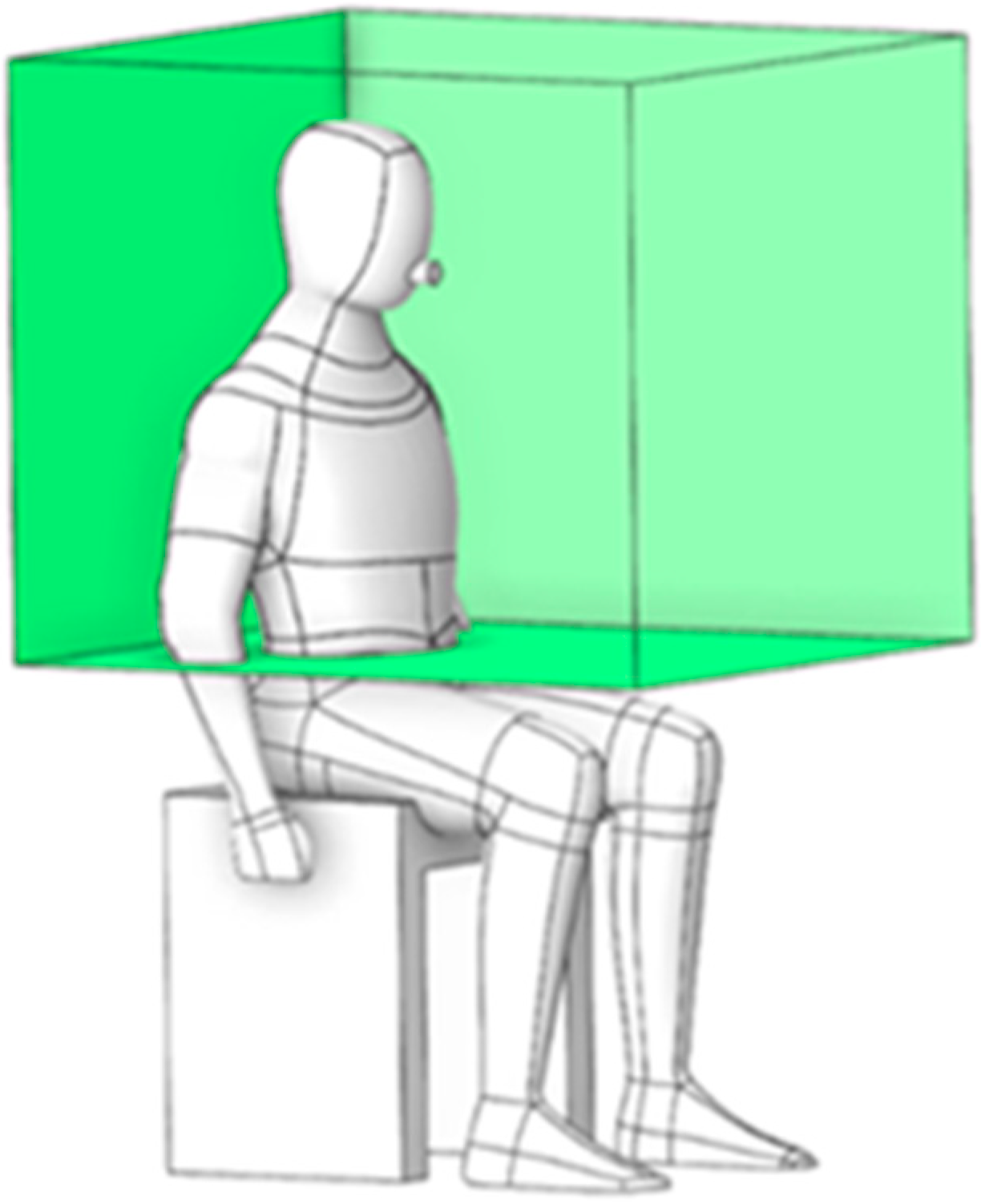
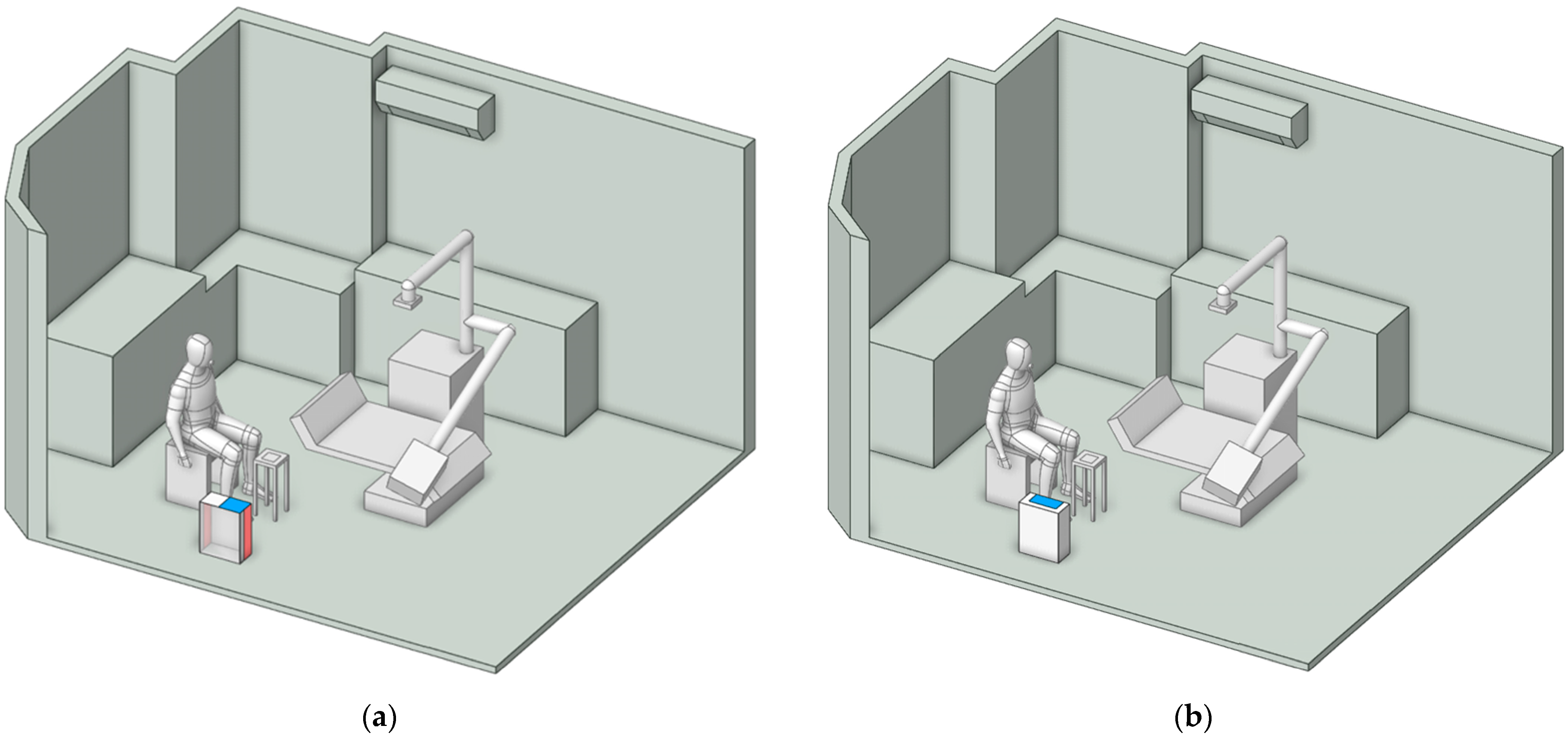
2.1. Physical Model and Boundary Conditions
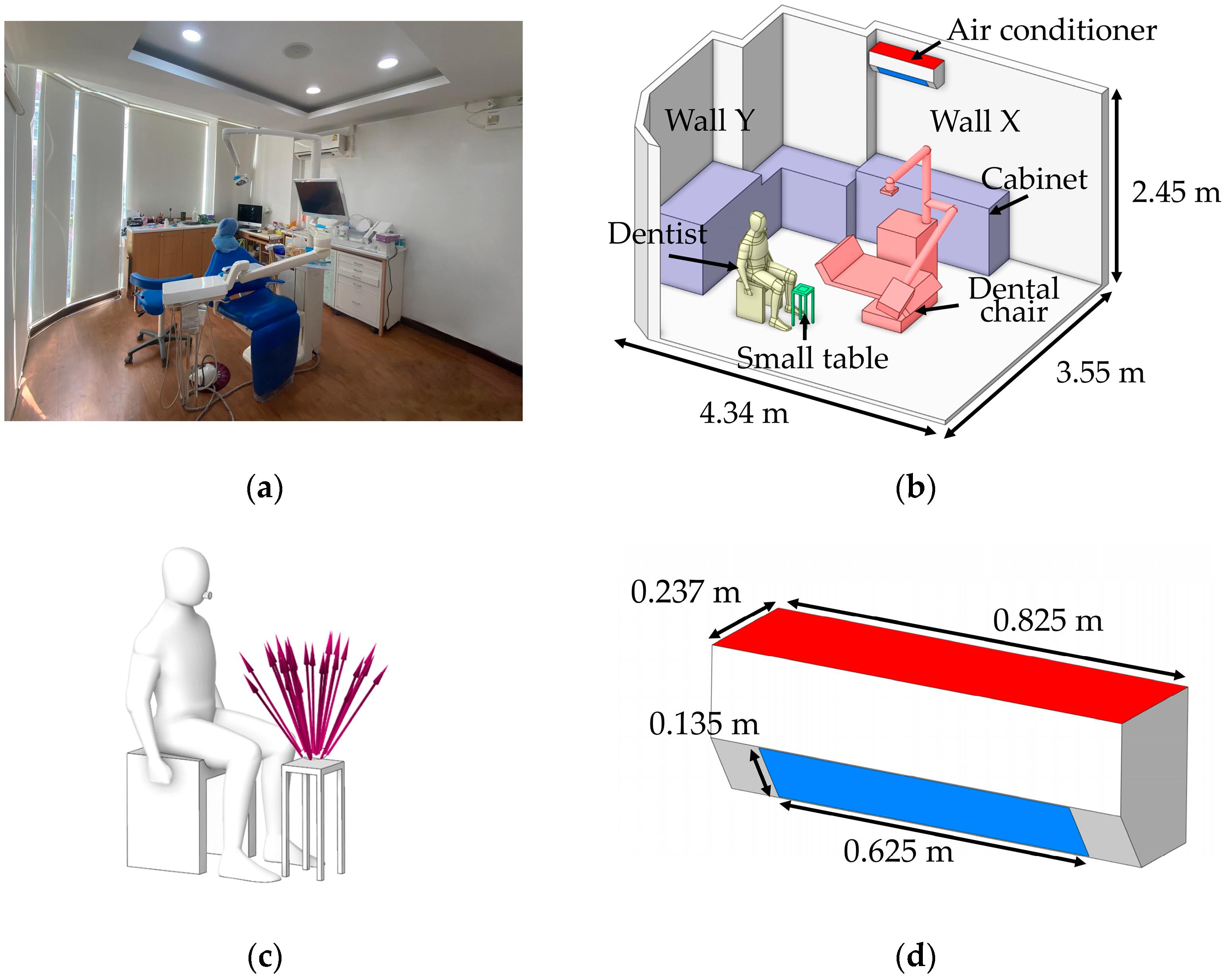
| Boundary Types | Boundary Conditions |
|---|---|
| Inlet | Velocity inlet 5.5 m/s, Temperature 24 °C |
| Outlet | Outflow |
| Human Surface | No-slip wall, Heat flux = 58.5 W/m2 |
| Wall and furniture | No-slip wall |
| Density of particle | |
| Number of particles | 850 pcs/s |
| Diameter of the particle | |
| Particle velocity | 10 m/s |
| Particle droplet | 30 s |
2.2. Meshing
2.3. Numerical Model
2.3.1. Airflow Phase Model
2.3.2. Particle Phase Model
2.4. Experimental Method
2.4.1. Measurement Devices
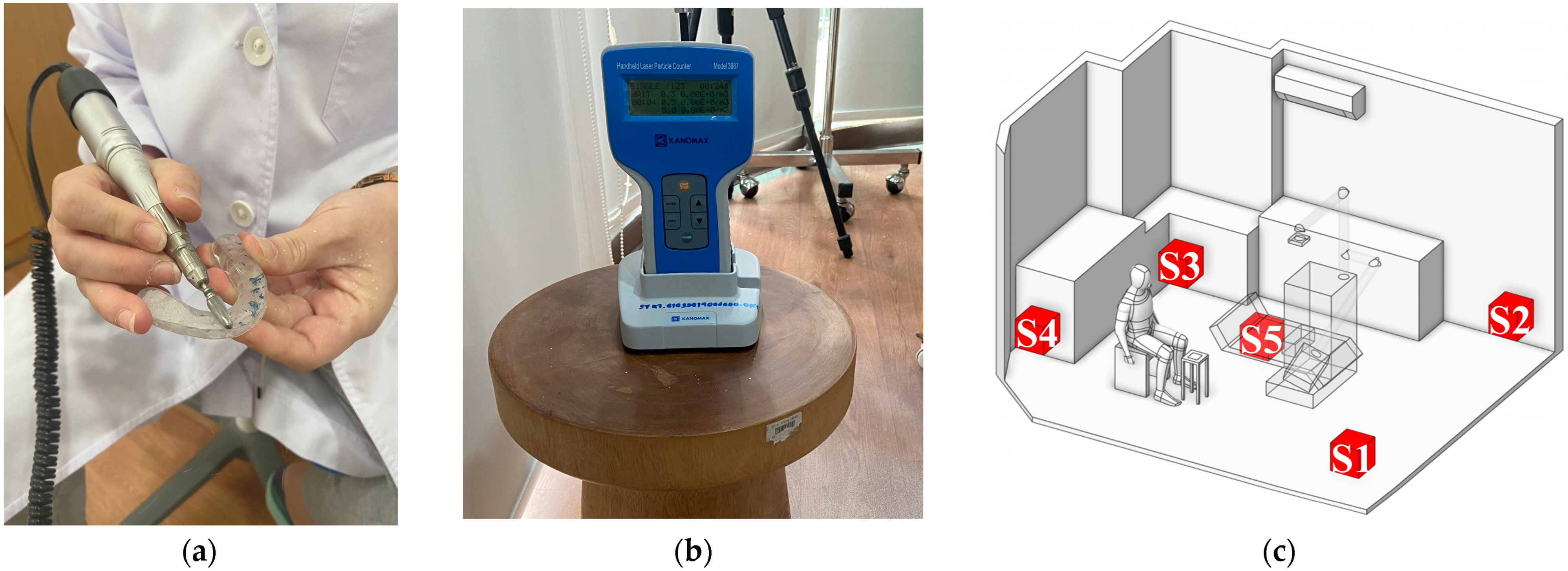
2.4.2. Field Measurement
Air Velocity Measurement
Quantifications of Particle Concentrations
- Particle Measurement at the Source: This step aimed to evaluate the quantity of particles generated during the dental procedure and to define the particle release boundary condition in the simulation. To minimize interference with the dentist’s workflow, the measuring device was placed as close as possible to the working area at a height of 0.45 m from the floor, corresponding to the typical operating height. Data collection was conducted over 30 s, based on the average time required to polish a single dental prosthesis by an experienced practitioner [60]. This duration also corresponds to the period during which the highest concentration of particles is typically released in dental procedures [61]. As shown in Table 4, the particle count measured at the source reached 25,000 particles.
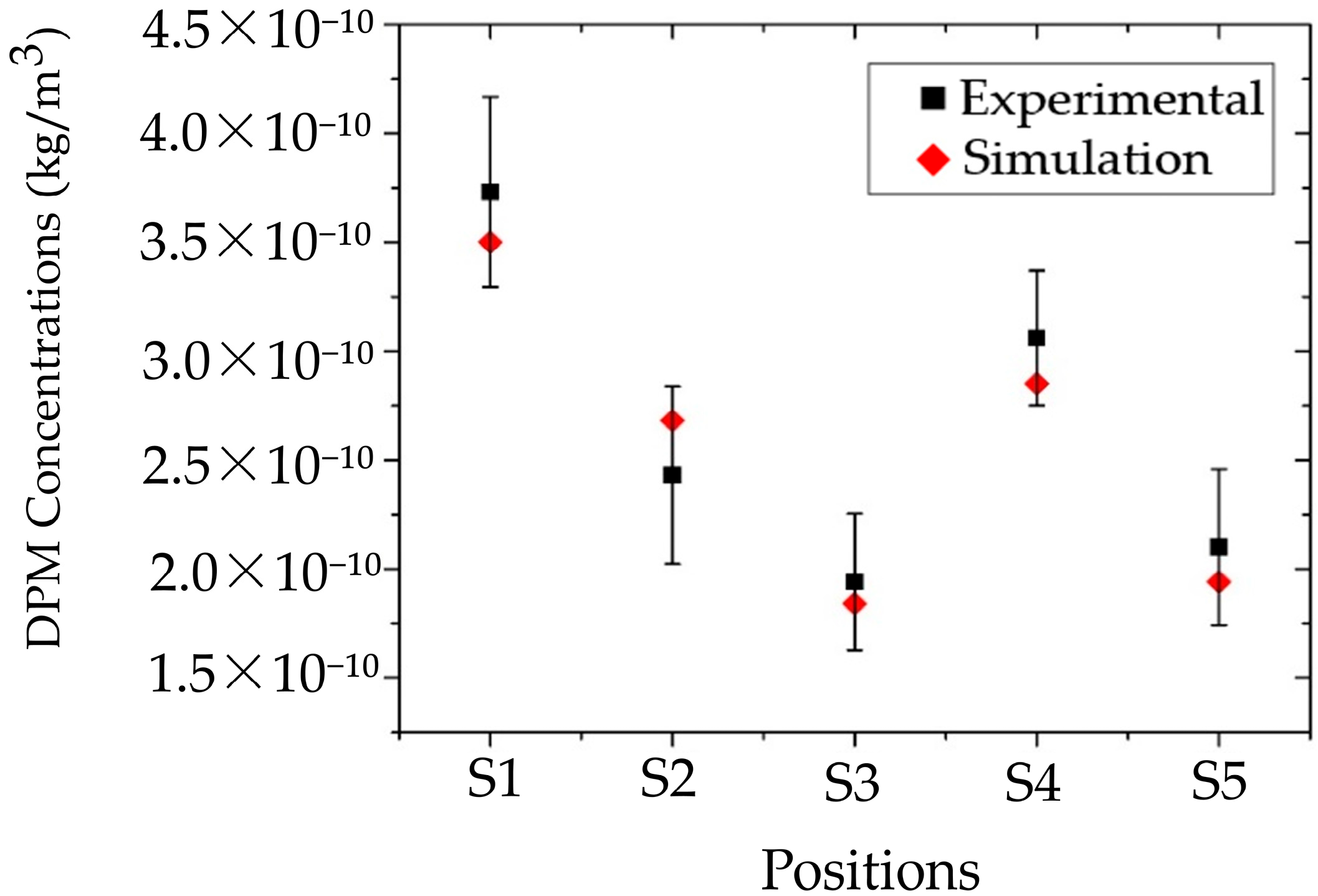
- Particle Concentration Measurement at Various Locations in the Room: To assess the particle concentration within the room, five measurement points were designated as S1–S5, which included the four corners of the room (S1, S2, S3, S4) and the other at the center of the room (S5), as shown in Figure 4c. These positions were selected because they are likely to generate recirculation and vortex zones, which can directly affect particle transport and result in significant accumulation [62]. Data collected from these positions were used to compare and validate the simulation results on particle concentration. During the experiment, the particle counter was placed 15 cm away from both adjacent walls and at a height of 0.45 m, consistent with the release height at the particle source. Each position was measured five times, with each measurement lasting 1 min. Owing to the limited number of particle counters, measurements were performed in a systematic sequence, with the clinic room undergoing basic cleaning for 45–60 min after each round to restore a safe baseline environment before the next measurement session. As shown in Table 4, the highest particle concentration was observed at S1, followed by S4, then S2, S3, and S5, in that order. These findings support the hypothesis that the corners of the room are prone to the formation of recirculation and vortex zones, resulting in higher particle accumulation compared to the center of the room. Additionally, the results help identify potential high-risk areas within the clinic, particularly at S1 and S4, where particles tend to accumulate or be carried by airflow in significant quantities.
| Positions | Starting Point at Particle Source (30 s) | S1 (60 s) | S2 (60 s) | S4 (60 s) | S4 (60 s) | S5 (60 s) |
|---|---|---|---|---|---|---|
| Particle concentration | 25,000 Particles |
2.5. Local Concentration Reduction
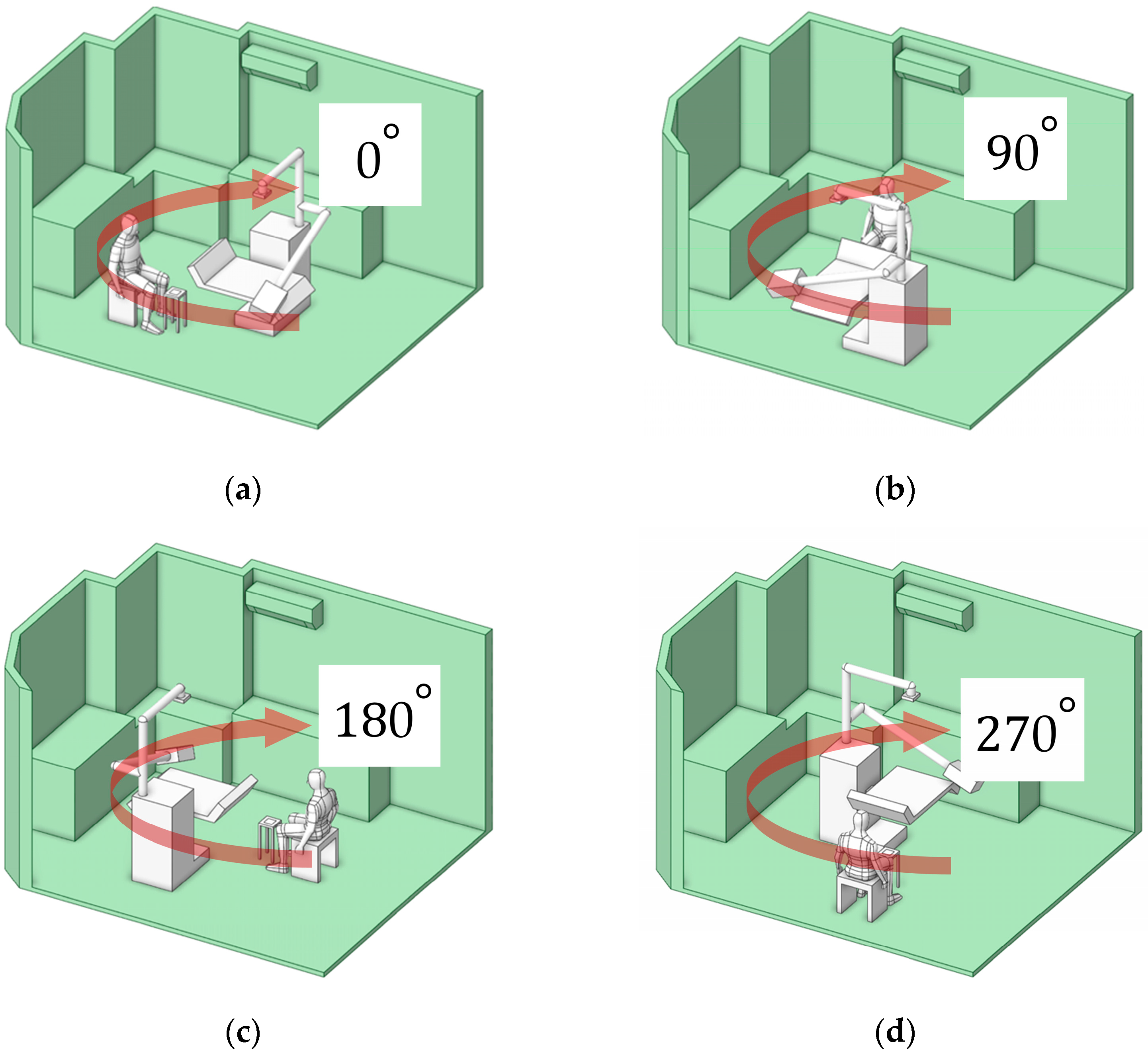
2.5.1. Working Zone Location
2.5.2. Impact of Portable Air Cleaner Intake Geometry on Mitigation
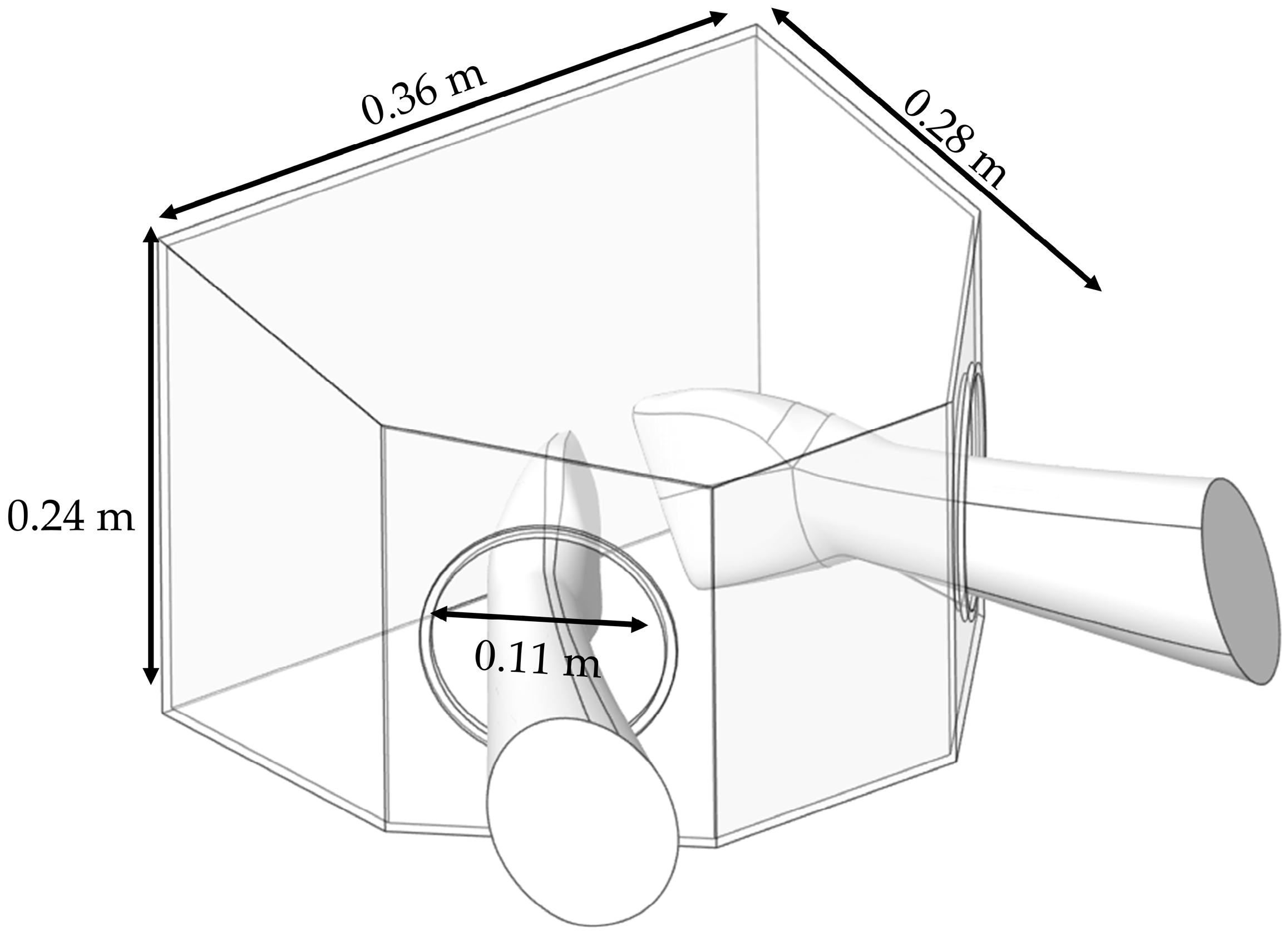
2.5.3. Box Dust Collector
3. Results and Discussions
3.1. Validation
3.1.1. Airflow Velocity and Grid Sensitivity
3.1.2. Particle Concentrations Validation
3.2. Investigation of Health Risks Location Within the Clinic
3.2.1. Airflow Field
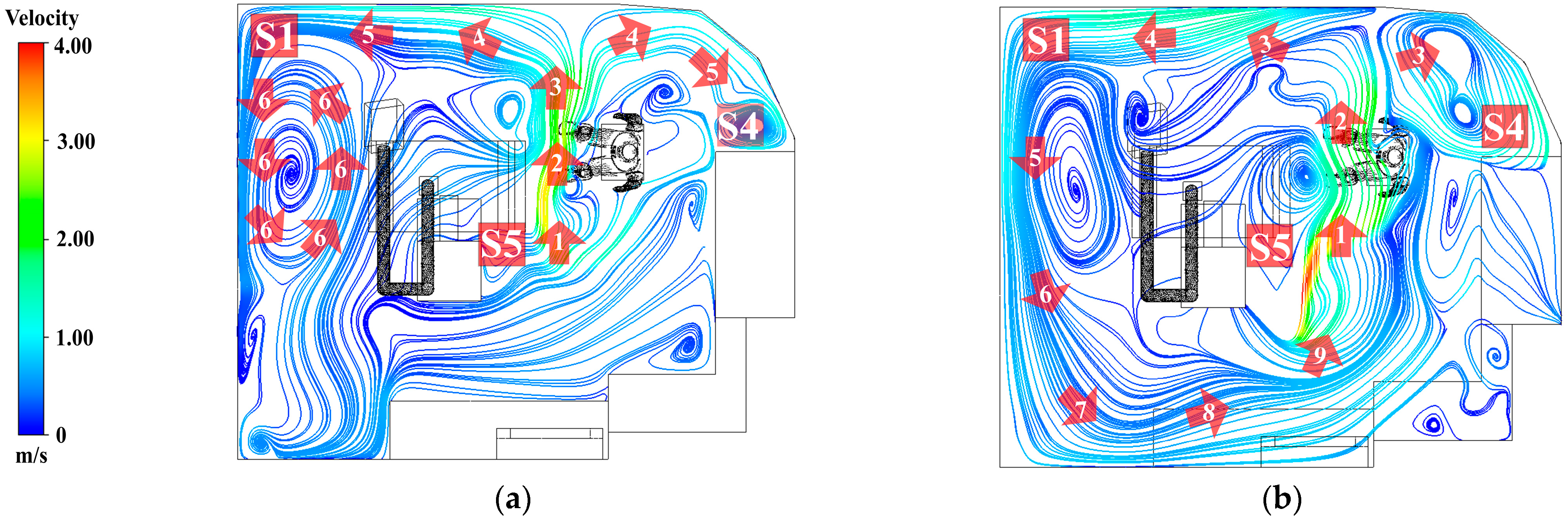
- At a height of 0.45 m, as shown in Figure 11a, sorting by number, the air released from the air conditioner flows according to the numbers 1, 2, 3, 4, 5, and 6. Most of the air released from the inlet flows directly toward the working zone. At number 2, airflow carries particles generated during dental material grinding and disperses them throughout the room, as shown in number 4. The airflow then impinges on the wall, resulting in a reduction in velocity reduction and separation into two streams. These separated flows subsequently collide with the room corners, forming recirculation zones, most prominently at positions S1 and S4. At these locations, repeated vortex-like circulations occur, which reduce airflow velocity and facilitate the accumulation of particles. By contrast, position S5, located at the center along the initial airflow path, demonstrates better ventilation than the other positions.
- At a height of 1.1 m, as shown in Figure 11b, sort by number, 1, 2, 3, 4, 5, 6, 7, 8, and 9. The airflow predominantly forms recirculating currents originating from the air conditioner outlet and extending into all corners of the room. At numbers 7, 8, and 9, the flow repeatedly returns toward the center of the room, reflecting inefficient ventilation. This pattern indicates that particles released into the air are likely to recirculate to their original positions, thereby increasing the dentist’s risk of exposure and inhalation.
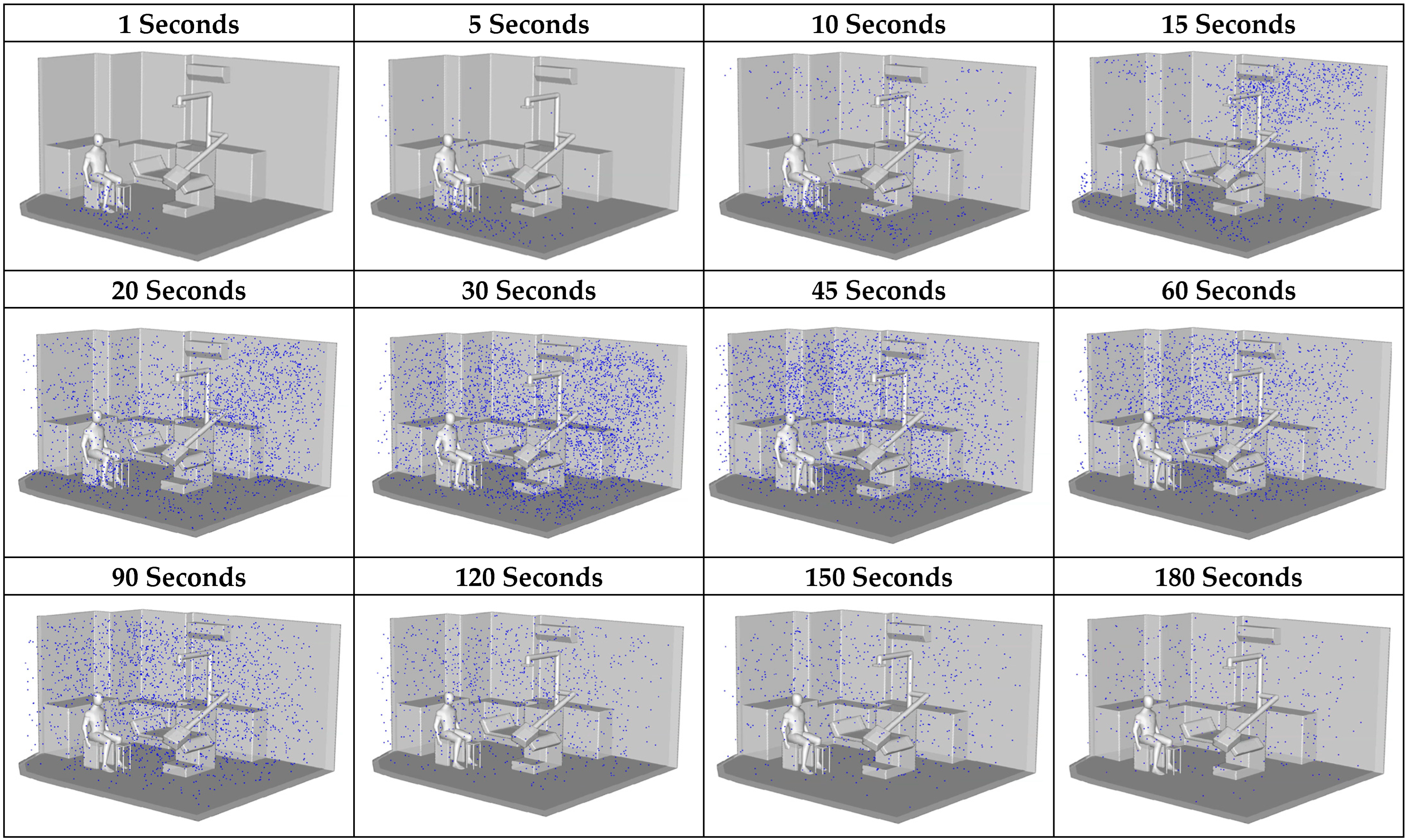
3.2.2. Particle Distribution
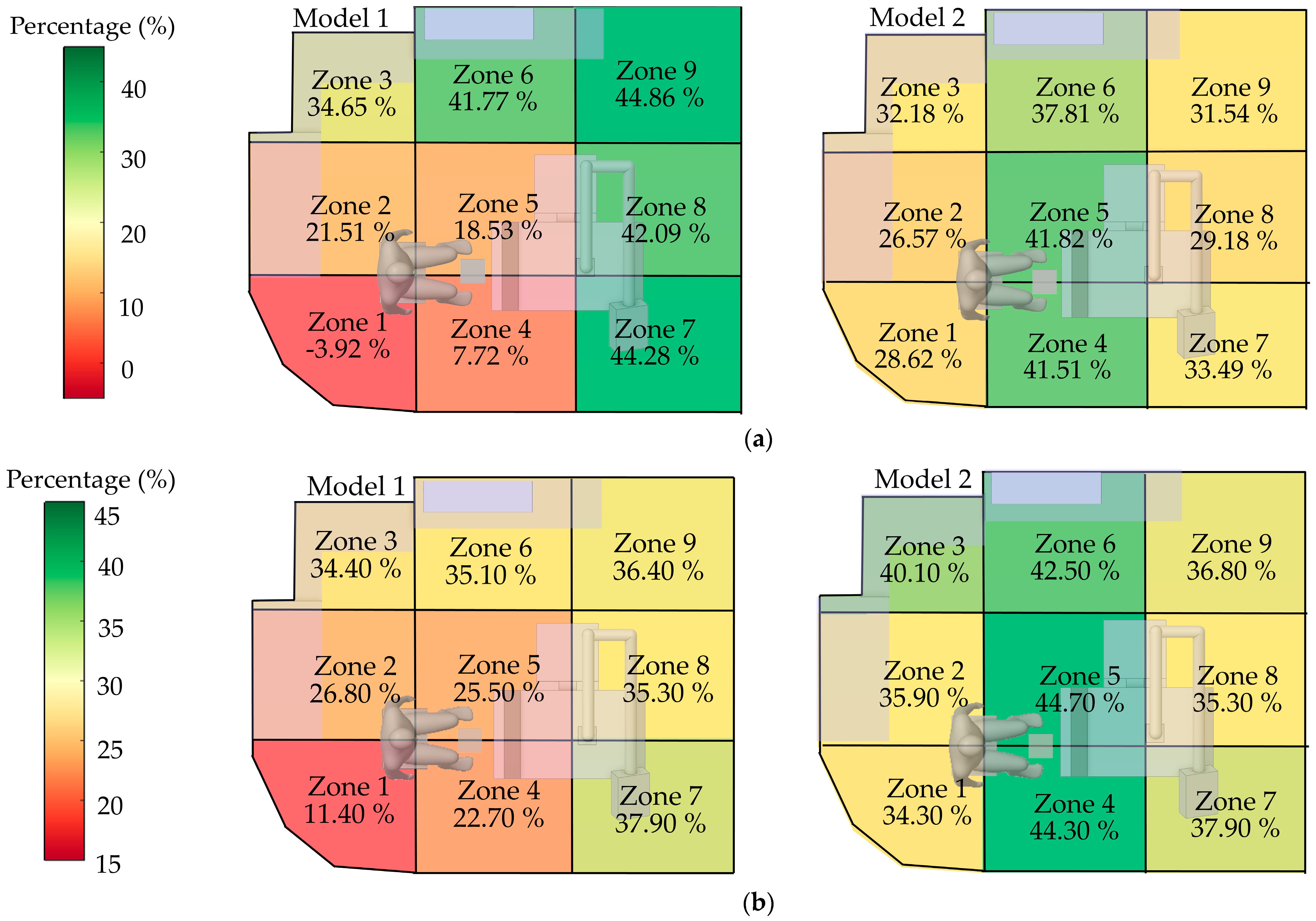
3.3. Spatial Concentration Reduction Measures
3.3.1. Optimal Working Position Assessment
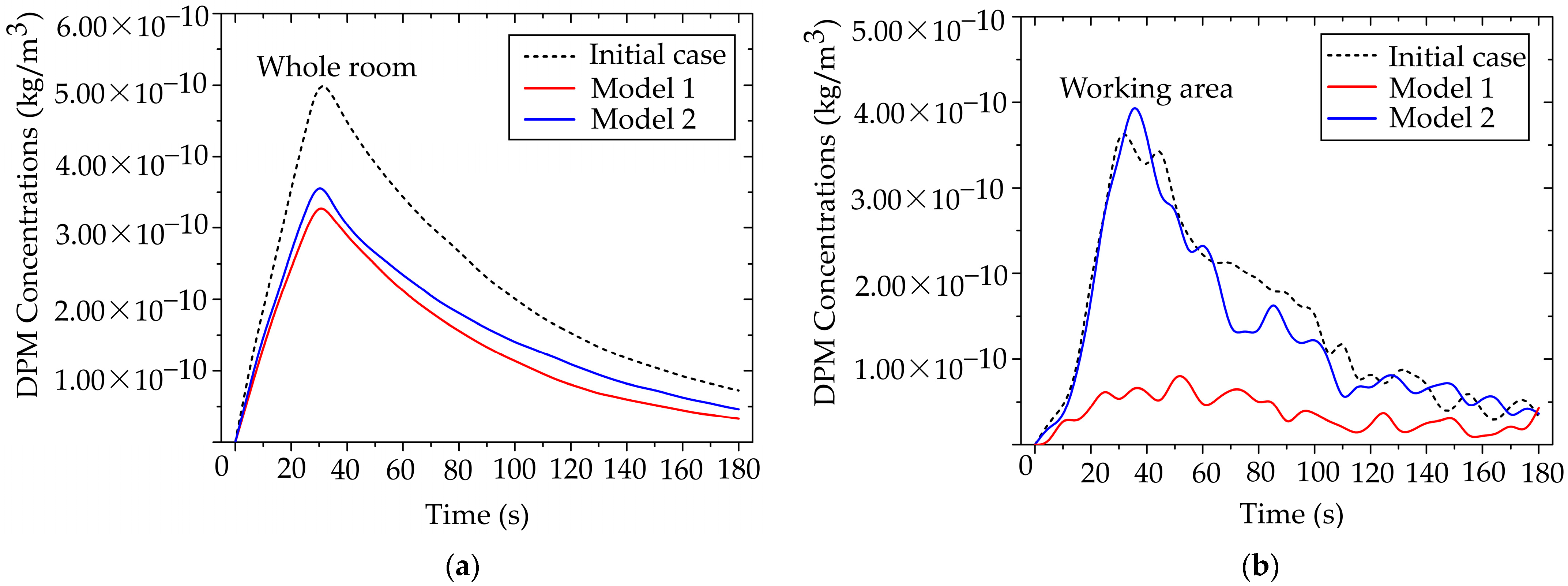
3.3.2. Effects of Air Purifiers on Particle Mitigation Improvement
3.3.3. Effectiveness Zones of Preventive Measures
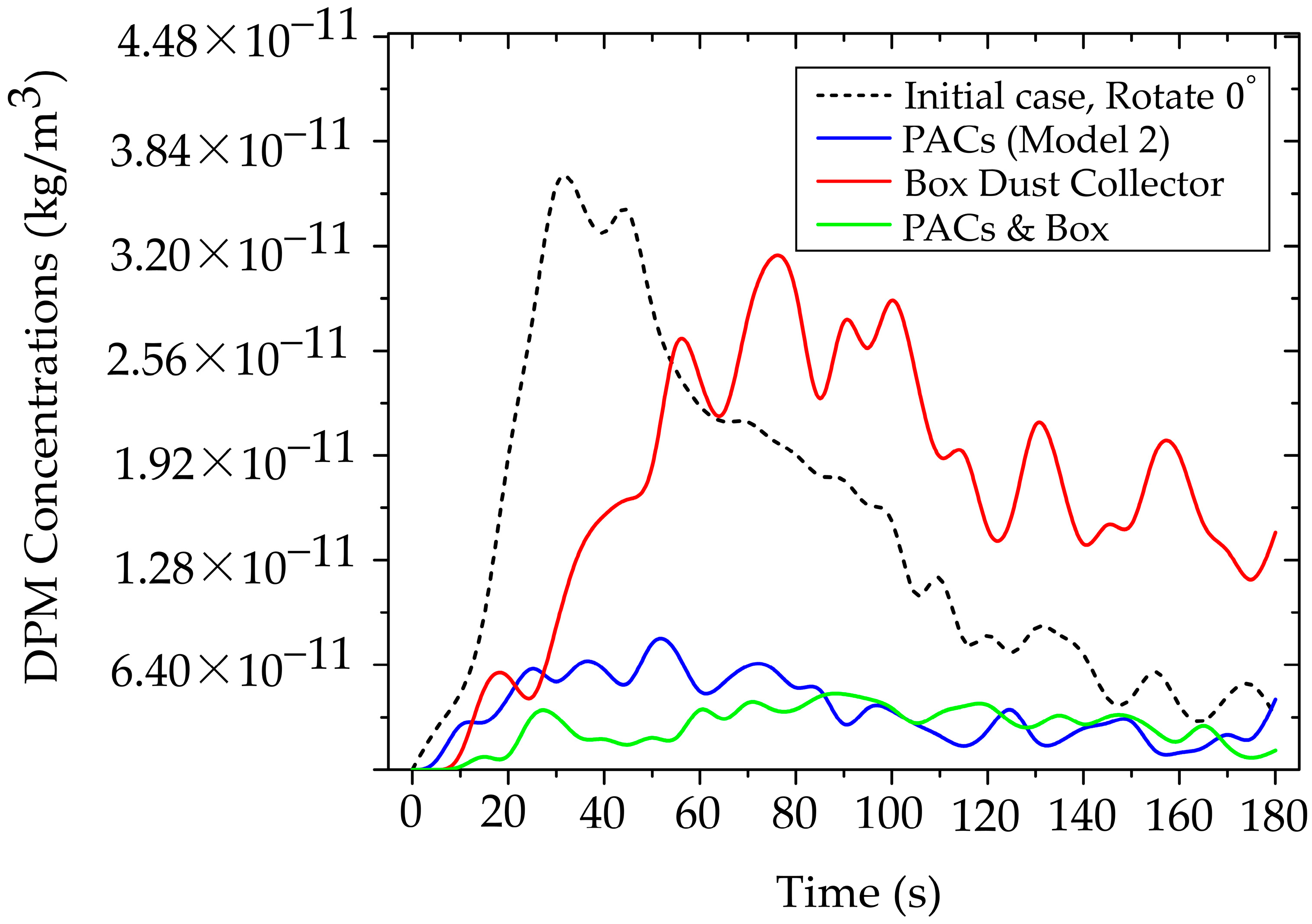
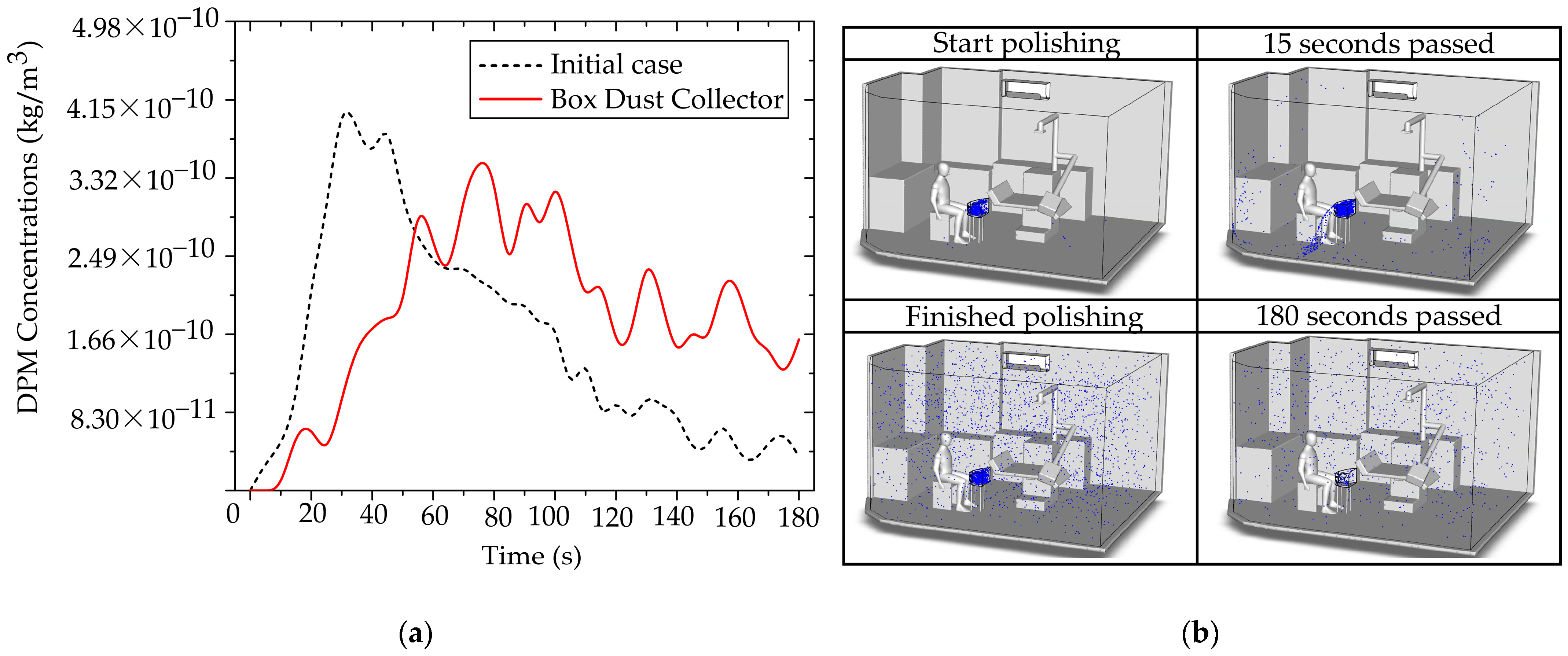
3.3.4. Investigation of Particle Mitigation Effects Using Box Dust Collector
3.3.5. Interoperability Between PACs and BC
3.4. Mandating a New Paradigm for Airborne Toxicant Control in Digital Dentistry
3.5. Integrating Toxicology and Dental Safety Narratives
| Mitigation Strategy | Mechanism of Action | Peak Particle Concentration Reduction | Breathing-Zone Concentration Reduction | Advantages | Limitations | Recommended Clinical Application |
|---|---|---|---|---|---|---|
| Baseline (No Control) | Natural room airflow only | — | — | Serves as control for CFD validation | High particle accumulation; prolonged airborne residence | Used for comparison and reference |
| Portable Air Cleaner (PACs Model 2) | Continuous air suction aligned with primary airflow direction | Up to 80% reduction | Up to 65% reduction | Effective at whole-room and local scales; portable and easy to install | Requires optimal placement; airflow alignment critical | General dental procedures, polishing, and prolonged tasks |
| Dust Box Collector (BC) | Localized source containment via frontal capture zone | Approx. 40–60 s delay in plume development | 35–45% transient reduction | Effective for early-stage containment; minimizes initial spread | Limited by particle leakage; efficiency decreases over time | High-emission short-duration tasks (e.g., grinding, trimming) |
| PACs Model 2 + BC | Synergistic combination of local containment and continuous extraction | Up to 85% total reduction in peak level | Sustained 75–80% reduction over 180 s | Strongest and most stable control; reduces residence time and exposure | Requires coordination of airflow directions and more spaces | Optimal for high-risk scenarios (3D-printing adjustments, chairside material grinding) |
3.6. Translating Risk into Control: Ergonomics, Material-Specific Considerations, and Future Research Mandates
- Multi-material and longevity studies: Future research must characterize particle profiles with distinct aerodynamic sizes, densities, and surface properties for the full spectrum of modern dental materials, including emerging 3D-printing resin-based and hybrid materials [71]. Crucially, studies must quantify the operational longevity (i.e., saturation time) of internal capture media for specific composites to prevent catastrophic particle breakthrough and ensure sustained occupational safety.
- Additive manufacturing trends: Future research should account for the unique challenges of 3D printing, specifically analyzing the potential for the release of volatile organic compounds (VOCs) during post-processing and exploring mitigation approaches [72].
- Refinement of CFD models: to maximize predictive power, future CFD models must integrate refined human factors (dentist/patient breathing patterns, thermal effects, and continuous room usage) and evaluate the sustained efficacy of control systems (PACs, BC) under diverse, continuous procedural conditions.
- The emission source was modeled as a steady surrogate with fixed release rate and initial jet velocity, and no formal sensitivity analysis was performed. Consequently, clinically relevant variability (tool type/speed, material removal rate, operator technique), transient bursts/duty cycles, and polydisperse size distributions were not parameterized. This simplification may bias estimates of short-term concentration peaks, plume intermittency, and local hot-spot magnitudes relative to conditions with time-resolved, case-specific emissions.
- Validation readings were acquired in quintuplicate (n = 5) and reported as mean ± SD. The handheld particle counter used for 0.3–5 µm channels has a stated accuracy of ±10% stated accuracy (2.83 L·min−1), and the hot-wire anemometer for air velocity has a stated accuracy of ±5%. Additional contributions arise from probe positioning/angle sensitivity in strong gradients as well as counting-statistics and coincidence at elevated concentrations. Replicate SDs were modest and remained within these specifications; consequently, the maximum CFD–measurement deviation (9.6%) falls within the instrument-limited uncertainty envelope and is not indicative of systematic model bias.
- Future work will extend to multiple dental materials (e.g., PMMA, resin composites, zirconia) with size-resolved, polydisperse emission spectra, and will assess long-term cumulative exposure by coupling transient CFD with time-activity schedules and maintained CADR/air-cleaning performance. Exposure will be summarized using shift-level occupational metrics (e.g., 8-h TWA, cumulative inhaled dose) to link engineering controls to health-relevant endpoints.
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pope, C.A.; Dockery, D.W. Health Effects of Fine Particulate Air Pollution: Lines that Connect. J. Air Waste Manag. Assoc. 2006, 56, 709–742. [Google Scholar] [CrossRef] [PubMed]
- Air Quality, Energy and Health (AQE). WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide, and Carbon Monoxide. Bulletin of the World Health Organization. Available online: https://www.who.int/publications/i/item/9789240034228 (accessed on 22 September 2021).
- Cohen, A.J.; Brauer, M.; Burnett, R.; Anderson, H.R.; Frostad, J.; Estep, K.; Balakrishnan, K.; Brunekreef, B.; Dandona, L.; Dandona, R.; et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the Global Burden of Diseases Study 2015. Lancet 2017, 389, 1907–1918. [Google Scholar] [CrossRef] [PubMed]
- Hoek, G.; Krishnan, R.M.; Beelen, R.; Peters, A.; Ostro, B.; Brunekreef, B.; Kaufman, J.D. Long-term Air Pollution Exposure and Cardio-Respiratory Mortality: A Review. Environ. Health 2013, 12, 43. [Google Scholar] [CrossRef]
- Xing, Y.F.; Xu, Y.H.; Shi, M.H.; Lian, Y.X. The Impact of PM2.5 on the Human Respiratory System. Int. J. Environ. Res. Public Health 2016, 8, E69–E74. [Google Scholar]
- Schraufnagel, D.E. The health effects of ultrafine particles. Exp. Mol. Med. 2020, 52, 311–317. [Google Scholar] [CrossRef]
- Nel, A.; Xia, T.; Mädler, L.; Li, N. Toxic Potential of Materials at the Nanolevel. Int. J. Environ. Res. Public Health 2006, 311, 622–627. [Google Scholar] [CrossRef]
- Kreyling, W.G.; Semmler-Behnke, M.; Möller, W. Ultrafine particle–lung interactions: Does size matter. J. Aerosol Med. Pulm. Drug Deliv. 2006, 19, 74–83. [Google Scholar] [CrossRef] [PubMed]
- Oberdörster, G.; Oberdörster, E.; Oberdörster, J. Nanotoxicology: An emerging discipline evolving from studies of ultrafine particles. Environ. Health Perspect. 2005, 113, 823–839. [Google Scholar] [CrossRef]
- Mannucci, P.M.; Franchini, M. Health effects of ambient air pollution in developing countries. Int. J. Environ. Res. Public Health 2017, 14, 1048. [Google Scholar]
- Harrel, S.K.; Molinari, J. Aerosols and splatter in dentistry: A brief review of the literature and infection control implications. J. Am. Dent. Assoc. 2004, 135, 429–437. [Google Scholar] [CrossRef]
- Geiser, M.; Kreyling, W.G. Deposition and Biokinetics of Inhaled Nanoparticles. Part. Fibre Toxicol. 2010, 7, 2. [Google Scholar] [CrossRef]
- Taira, M.; Sasaki, M.; Kimura, S.; Araki, Y. Characterization of Aerosols and Fine Particles Produced in Dentistry and Their Health Risk Assessments. Nano Biomed. Eng. 2009, 1, 9–15. [Google Scholar]
- Fernstrom, A.; Goldblatt, M. Aerobiology and Its Role in the Transmission of Infectious Diseases. J. Pathog. 2013, 2013, 493960. [Google Scholar] [CrossRef]
- Allison, J.R.; Tiede, S.; Holliday, R.; Durham, J.; Jakubovics, N.S. Bioaerosols and airborne transmission in the dental clinic. Int. Dent. J. 2024, 74, S418–S428. [Google Scholar] [CrossRef]
- Bennett, A.M.; Fulford, M.R.; Walker, J.T.; Bradshaw, D.J.; Martin, M.V.; Marsh, P.D. Microbial aerosols in general dental practice. Br. Dent. J. 2000, 189, 664–667. [Google Scholar] [CrossRef] [PubMed]
- Ding, S.; Lee, J.S.; Mohamed, M.A.; Ng, B.F. Infection Risk of SARS-CoV-2 in a Dining Setting: Deposited Droplets and Aerosols. Build. Environ. 2022, 213, 108888. [Google Scholar] [CrossRef] [PubMed]
- Innes, N.P.T.; Johnson, I.G.; Al-Yaseen, W.; Harris, R.; Jones, R.; KC, S.; McGregor, S.; Robertson, M.; Wade, W.G.; Gallagher, J.E. A Systematic Review of Droplet and Aerosol Generation in Dentistry. J. Dent. 2021, 105, 103556. [Google Scholar] [CrossRef] [PubMed]
- Zemouri, C.; de Soet, H.; Crielaard, W.; Laheij, A. A scoping review on bio-aerosols in healthcare and the dental environment. PLoS ONE 2017, 12, e0178007. [Google Scholar] [CrossRef]
- Barros, M.C.; Pedrinha, V.F.; Velásquez-Espedilla, E.G.; Cuellar, M.R.C.; De Andrade, F.B. Aerosols Generated by High-Speed Handpiece and Ultrasonic Unit during Endodontic Coronal Access, Alluding to the COVID-19 Pandemic. Sci. Rep. 2022, 12, 08739. [Google Scholar] [CrossRef]
- Han, P.; Li, H.; Walsh, L.J.; Ivanovski, S. Splatters and Aerosols Contamination in Dental Aerosol Generating Procedures. Appl. Sci. 2021, 11, 1914. [Google Scholar] [CrossRef]
- Yuan, C.; Yang, H.; Zheng, S.; Sun, X.; Chen, X.; Chen, Y.; Kang, J.; Liu, M.; Zheng, S. Spatiotemporal Distribution and Control Measure Evaluation of Droplets and Aerosol Clouds in Dental Procedures. Infect. Control Hosp. Epidemiol. 2022, 44, 514–516. [Google Scholar] [CrossRef]
- Pankhurst, C.L.; Coulter, W.; Philpott-Howard, J.N.; Surman-Lee, S.; Warburton, F.; Challacombe, S. Evaluation of the potential risk of occupational asthma in dentists exposed to contaminated dental unit waterlines. Prim. Dent. Care. 2005, 2, 53–60. [Google Scholar] [CrossRef]
- Quintal-Méndez, J.R.; Soledad, A.R.; López-Hernández, E.; Sánchez-Monroy, V. Pulmonary alterations among workers in a dental prosthesis laboratory: Exploring high dust concentrations and novel findings of bacterial genera in the workplace to achieve improved control. J. Occup. Environ. Med. 2020, 62, 930–936. [Google Scholar] [CrossRef]
- Pillai, S.; Upadhyay, A.; Khayambashi, P.; Farooq, I.; Sabri, H.; Tarar, M.; Lee, K.T.; Harb, I.; Zhou, S.; Wang, Y.; et al. Dental 3D-printing: Transferring art from the laboratories to the clinics. Polymers 2021, 13, 157. [Google Scholar] [CrossRef] [PubMed]
- Leeson, D. The digital factory in both the modern dental lab and clinic. Dent. Mater. J. 2020, 36, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Dawood, A.; Marti, B.M.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Cocârţă, D.M.; Prodana, M.; Demetrescu, I.; Lungu, P.E.M.; Didilescu, A.C. Indoor air pollution with fine particles and implications for workers’ health in dental offices: A brief review. Sustainability 2021, 13, 599. [Google Scholar] [CrossRef]
- Tang, F.; Qi, S.; Tang, X.; Wen, X.; Zhang, Y.; Peng, G.; Huang, G.; Shang, G.; Zhang, X.; Chen, F.; et al. Analysis of PM2. 5 Morphology, Composition and Health Risk in a Multi-Chair Dental Clinic. Environ. Toxicol. 2025, 40, 1207–1219. [Google Scholar] [CrossRef]
- Ding, J.; Li, J.; Qi, J.; Fu, L. Characterization of Dental Dust Particles and Their Pathogenicity to Respiratory System: A Narrative Review. Clin. Oral Investig. 2023, 27, 1815–1829. [Google Scholar] [CrossRef]
- Komarytsia, O.Y.; Paliy, A.V.; Krukovskiy, I.O.; Krupnyk, A.A.; Kordiyak, O.Y. Correlating Features Between Dental and Pulmonary Disease. Art Med. 2024, 80–83. [Google Scholar] [CrossRef]
- Du, L.; Wan, Z.; Guo, L.; Yang, C.; Zhu, Z. Aerosol dynamics in dental clinics: Effects of ventilation mode on the mitigation of airborne diseases transmission. Environ. Pollut. 2025, 367, 125645. [Google Scholar] [CrossRef]
- Tan, H.; Wong, K.Y.; Othman, M.H.D.; Kek, H.Y.; Wahab, R.A.; Ern, G.K.P.; Chong, W.T.; Lee, K.Q. Current and potential approaches on assessing airflow and particle dispersion in healthcare facilities: A systematic review. Environ. Sci. Pollut. Res. 2022, 29, 80137–80160. [Google Scholar] [CrossRef]
- Zhou, Y.; Ji, S. Experimental and Numerical Study on the Transport of Droplet Aerosols Generated by Occupants in a Fever Clinic. Build. Environ. 2020, 187, 107402. [Google Scholar] [PubMed]
- Liu, Z.; Zhang, P.; Li, Y.; Yang, W.; Guo, J.; Liu, J.; Yao, G. Assessment of Spatial Concentration Variation and Deposition of Bioaerosols in a Dental Clinic during Oral Cleaning. Build. Environ. 2021, 202, 108024. [Google Scholar] [CrossRef]
- Liu, Z.; Yao, G.; Li, Y.; Huang, Z.; Jiang, C.; He, J.; Wu, M.; Liu, J.; Liu, H. Bioaerosol Distribution Characteristics and Potential SARS-CoV-2 Infection Risk in a Multi-Compartment Dental Clinic. Build. Environ. 2022, 225, 109624. [Google Scholar] [CrossRef]
- Dey, S.; Tunio, M.; Boryc, L.C.; Hodgson, B.D.; Garcia, G.J. Quantifying strategies to minimize aerosol dispersion in dental clinics. Exp. Comput. Multiph. Flow 2023, 5, 290–303. [Google Scholar] [CrossRef] [PubMed]
- Lomardo, P.G.; Nunes, M.C.; Arriaga, P.; Antunes, L.A.; Machado, A.; Quinelato, V.; Aguiar, T.R.d.S.; Casado, P.L. Concern about the risk of aerosol contamination from ultrasonic scaler: A systematic review and meta-analysis. BMC Oral Health 2024, 24, 417. [Google Scholar] [CrossRef]
- Liu, P. Computational fluid dynamics optimization of an extraoral vacuum aerosol cup for airborne disease control in dental offices. Aerosol Sci. Eng. 2022, 6, 21–29. [Google Scholar] [CrossRef]
- Chen, L.; Zhou, X.; Xiao, F.; Deng, Y.; Mahadevan, S. Evidential Analytic Hierarchy Process Dependence Assessment Methodology in Human Reliability Analysis. Nucl. Eng. Technol. 2016, 49, 123–133. [Google Scholar] [CrossRef]
- Kashkooli, F.M.; Soltani, M.; Zargar, B.; Ijaz, M.K.; Taatizadeh, E.; Sattar, S.A. Analysis of an Indoor Air Decontamination Device Inside an Aerobiology Chamber: A Numerical-Experimental Study. Air Qual. Atmos. Health 2019, 13, 281–288. [Google Scholar] [CrossRef]
- Novoselac, A.; Siegel, J.A. Impact of Placement of Portable Air Cleaning Devices in Multizone Residential Environments. Build. Environ. 2009, 44, 2348–2356. [Google Scholar] [CrossRef]
- Dai, H.; Zhao, B. Reducing Airborne Infection Risk of COVID-19 by Locating Air Cleaners at Proper Positions Indoor: Analysis with a Simple Model. Build. Environ. 2022, 213, 108864. [Google Scholar] [CrossRef]
- Kajita, T.; Kikuchi, K.; Morishima, H.; Watanabe, J.; Iwamatsu-Kobayashi, Y.; Kanetaka, H.; Yashiro, W.; Yamauchi, K.; Egusa, H. Reduction of aerosol and droplet dispersions using intraoral and extraoral vacuums for dental treatments with face-up, diagonal and upright positions. BMC Oral Health 2024, 24, 1397. [Google Scholar] [CrossRef]
- Thongsri, J. A Successful CFD-Based Solution to a Water Condensation Problem in a Hard Disk Drive Factory. IEEE Access 2017, 5, 10795–10804. [Google Scholar] [CrossRef]
- ANSYS Fluent User’s Guide. Available online: https://www.ansys.com (accessed on 29 January 2019).
- Yang, X.; Ou, C.; Yang, H.; Liu, L.; Song, T.; Kang, M.; Lin, H.; Hang, J. Transmission of Pathogen-Laden Expiratory Droplets in a Coach Bus. J. Hazard. Mater. 2020, 397, 122609. [Google Scholar] [CrossRef]
- Pressing Dental Srl. Smile Cam (Discs in Various Shapes and Blocks for CAD/CAM Technology): Material Safety Data Sheet (Rev. No. 2); Pressing Dental Srl: Falciano, San Marino. Available online: https://www.pressing-dental.com (accessed on 16 July 2015).
- Matys, J.; Grzech-Leśniak, K. Dental Aerosol as a Hazard Risk for Dental Workers. Materials 2020, 13, 5109. [Google Scholar] [CrossRef]
- Miller, R.L. Characteristics of Blood-Containing Aerosols Generated by Common Powered Dental Instruments. Am. Ind. Hyg. Assoc. 1995, 56, 670–676. [Google Scholar]
- Yan, Y.; Li, X.; Shang, Y.; Tu, J. Evaluation of Airborne Disease Infection Risks in an Airliner Cabin Using the Lagrangian-Based Wells-Riley Approach. Build. Environ. 2017, 121, 79–92. [Google Scholar]
- Zhang, Z.; Zhang, W.; Zhai, Z.J.; Chen, Q.Y. Evaluation of Various Turbulence Models in Predicting Airflow and Turbulence in Enclosed Environments by CFD: Part 2—Comparison with Experimental Data from Literature. Hvac&R Res. 2007, 13, 871–886. [Google Scholar]
- Zhang, M.; Shrestha, P.; Liu, X.; Turnaoglu, T.; DeGraw, J.; Schafer, D.; Love, N. Computational Fluid Dynamics Simulation of SARS-CoV-2 Aerosol Dispersion Inside a Grocery Store. Build. Environ. 2021, 209, 108652. [Google Scholar] [CrossRef]
- Zhao, B.; Zhang, Y.; Li, X.; Yang, X.; Huang, D. Comparison of Indoor Aerosol Particle Concentration and Deposition in Different Ventilated Rooms by Numerical Method. Build. Environ. 2003, 39, 1–8. [Google Scholar] [CrossRef]
- Khongsin, J.; Thongsri, J. Numerical Investigation on the Performance of Suction Head in a Cleaning Process of Hard Disk Drive Factory. ECTI Trans. Electr. Eng. Electron. Commun. 2020, 18, 28–34. [Google Scholar] [CrossRef]
- Crowe, C.T.; Schwarzkopf, J.D.; Sommerfeld, M.; Tsuji, Y. Multiphase Flows with Droplets and Particles; eBooks; CRC Press: Boca Raton, FL, USA, 2011. [Google Scholar]
- Thongsri, J.; Tangsopa, W.; Khongsin, J. A Suitable Shape of the Suction Head for a Cleaning Process in a Factory Developed by Computational Fluid Dynamics. Processes 2021, 9, 1902. [Google Scholar] [CrossRef]
- Naosungnoen, J.; Thongsri, J. Airflow and Temperature Simulation in a Big Cleanroom to Reduce Contamination in an HDD Manufacturing Factory. IOP Conf. Ser. Mater. Sci. Eng. 2018, 361, 012025. [Google Scholar] [CrossRef]
- Doormaal, J.; Raithby, G. Enhancements of the SIMPLE Method for Predicting Incompressible Fluid Flows. Numer. Heat Transf. 1984, 7, 147–163. [Google Scholar] [CrossRef]
- Takanabe, Y.; Maruoka, Y.; Kondo, J.; Yagi, S.; Chikazu, D.; Okamoto, R.; Saitoh, M. Dispersion of Aerosols Generated during Dental Therapy. Int. J. Environ. Res. Public Health 2021, 18, 11279. [Google Scholar] [CrossRef]
- He, Z.; Gao, Q.; Henley, A.; Khatchadourian, Z.D.; Somerville, W.; Wiseman, M.; Mongeau, L.; Tamimi, F. Efficacy of Aerosol Reduction Measures for Dental Aerosol Generating Procedures. Aerosol Sci. Technol. 2022, 56, 413–424. [Google Scholar] [CrossRef] [PubMed]
- Morawska, L.; Ayoko, G.; Bae, G.; Buonanno, G.; Chao, C.; Clifford, S.; Fu, S.; Hänninen, O.; He, C.; Isaxon, C.; et al. Airborne Particles in Indoor Environment of Homes, Schools, Offices, and Aged Care Facilities: The Main Routes of Exposure. Environ. Int. 2017, 108, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Razavi, M.; Butt, Z.A.; Chen, H.; Tan, Z. In Situ Measurement of Airborne Particle Concentration in a Real Dental Office: Implications for Disease Transmission. Int. J. Environ. Res. Public Health 2021, 18, 8955. [Google Scholar] [CrossRef] [PubMed]
- Sotiriou, M.; Ferguson, S.F.; Davey, M.; Wolfson, J.M.; Demokritou, P.; Lawrence, J.; Sax, S.N.; Koutrakis, P. Measurement of Particle Concentrations in a Dental Office. Environ. Monit. Assess. 2007, 137, 351–361. [Google Scholar] [CrossRef]
- Mohamed, N.; Yusof, N.A.; Ali, W.N.S.W.; Ismail, N.A. The Effectiveness of the X-Dent Box (Dust Collector Box) in Collecting Trimming Dust from Different Types of Dental Prostheses Materials in Universiti Sains Islam Malaysia (USIM) Dental Laboratory. AIP Conf. Proc. 2018, 2030, 020299. [Google Scholar] [CrossRef]
- Oo, G.M.; Kotmool, K.; Mongkolwongrojn, M. Case Study on the Design Optimization of the Positive Pressure Operating Room. Sci. Rep. 2024, 14, 18671. [Google Scholar] [CrossRef]
- Yun, H.; Seo, J.H.; Yang, J. Development of Particle Filters for Portable Air Purifiers by Combining Melt-Blown and Polytetrafluoroethylene to Improve Durability and Performance. Indoor Air 2024, 2024, 5055615. [Google Scholar]
- Srivastava, A.; Andersen, M.R.; Alshehri, A.M.; Lara, B.; Bashiri, R.; Li, G.; Chambers, M.S. Effectiveness of a chairside acrylic adjustment cabinet in reducing dental acrylic debris and aerosols. J. Prosthodont. 2022, 31, 488–495. [Google Scholar] [CrossRef] [PubMed]
- Chan, F.L.; House, R.; Kudla, I.; Lipszyc, J.C.; Rajaram, N.; Tarlo, S.M. Health survey of employees regularly using 3D printers. J. Occup. Med. Toxicol. 2018, 68, 211–214. [Google Scholar] [CrossRef]
- Piirilä, P.; Hodgson, U.; Estlander, T.; Keskinen, H.; Saalo, A.; Voutilainen, R.; Kanerva, L. Occupational respiratory hypersensitivity in dental personnel. Int. Arch. Occup. Environ. Health 2002, 75, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Stefaniak, A.B.; Du Preez, S.; Du Plessis, J.L. Additive manufacturing for occupational hygiene: A comprehensive review of processes, emissions, & exposures. J. Toxicol. Environ. Health 2021, 24, 173–222. [Google Scholar]
- Mohammadian, Y.; Nasirzadeh, N. Toxicity risks of occupational exposure in 3D printing and bioprinting industries: A systematic review. Toxicol. Ind. Health 2021, 37, 573–584. [Google Scholar] [CrossRef]




| Instrument Name | Manufacturer | Model | Range | Flow Rate | Accuracy |
|---|---|---|---|---|---|
| Handheld Particle Counter | KANOMAX | 3887 | 0.3–5 | 0.1 cf/min 2.83 L/min | ±10% |
| Air velocity meter | Testo | 425 | 0 to +20 m/s | - | ±5% |
| Positions | P1 | P2 | P3 | P4 | P5 | P6 | P7 |
|---|---|---|---|---|---|---|---|
| Velocity of Air (m/s) | 5.5 m/s | 4.55 m/s | 3.42 m/s | 2.18 m/s | 1.9 m/s | 1.48 m/s | 1.31 m/s |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chanbandit, C.; Kanchanatawewat, K.; Oo, G.M.; Thongsri, J.; Tuntiwong, K. Airborne Dental Material Particulates and Occupational Exposure: Computational and Field Insights into Airflow Dynamics and Control Strategies. Toxics 2025, 13, 957. https://doi.org/10.3390/toxics13110957
Chanbandit C, Kanchanatawewat K, Oo GM, Thongsri J, Tuntiwong K. Airborne Dental Material Particulates and Occupational Exposure: Computational and Field Insights into Airflow Dynamics and Control Strategies. Toxics. 2025; 13(11):957. https://doi.org/10.3390/toxics13110957
Chicago/Turabian StyleChanbandit, Chanapat, Kanchana Kanchanatawewat, Ghaim Man Oo, Jatuporn Thongsri, and Kuson Tuntiwong. 2025. "Airborne Dental Material Particulates and Occupational Exposure: Computational and Field Insights into Airflow Dynamics and Control Strategies" Toxics 13, no. 11: 957. https://doi.org/10.3390/toxics13110957
APA StyleChanbandit, C., Kanchanatawewat, K., Oo, G. M., Thongsri, J., & Tuntiwong, K. (2025). Airborne Dental Material Particulates and Occupational Exposure: Computational and Field Insights into Airflow Dynamics and Control Strategies. Toxics, 13(11), 957. https://doi.org/10.3390/toxics13110957









