Impact of Short-Term Exposure to Nitrogen Dioxide (NO2) and Ozone (O3) on Hospital Admissions for Non-ST-Segment Elevation Acute Coronary Syndrome
Abstract
1. Introduction
2. Materials and Methods
2.1. Hospital Admission Data
2.2. Air Pollution and Climatological Data
2.3. Statistical Analysis
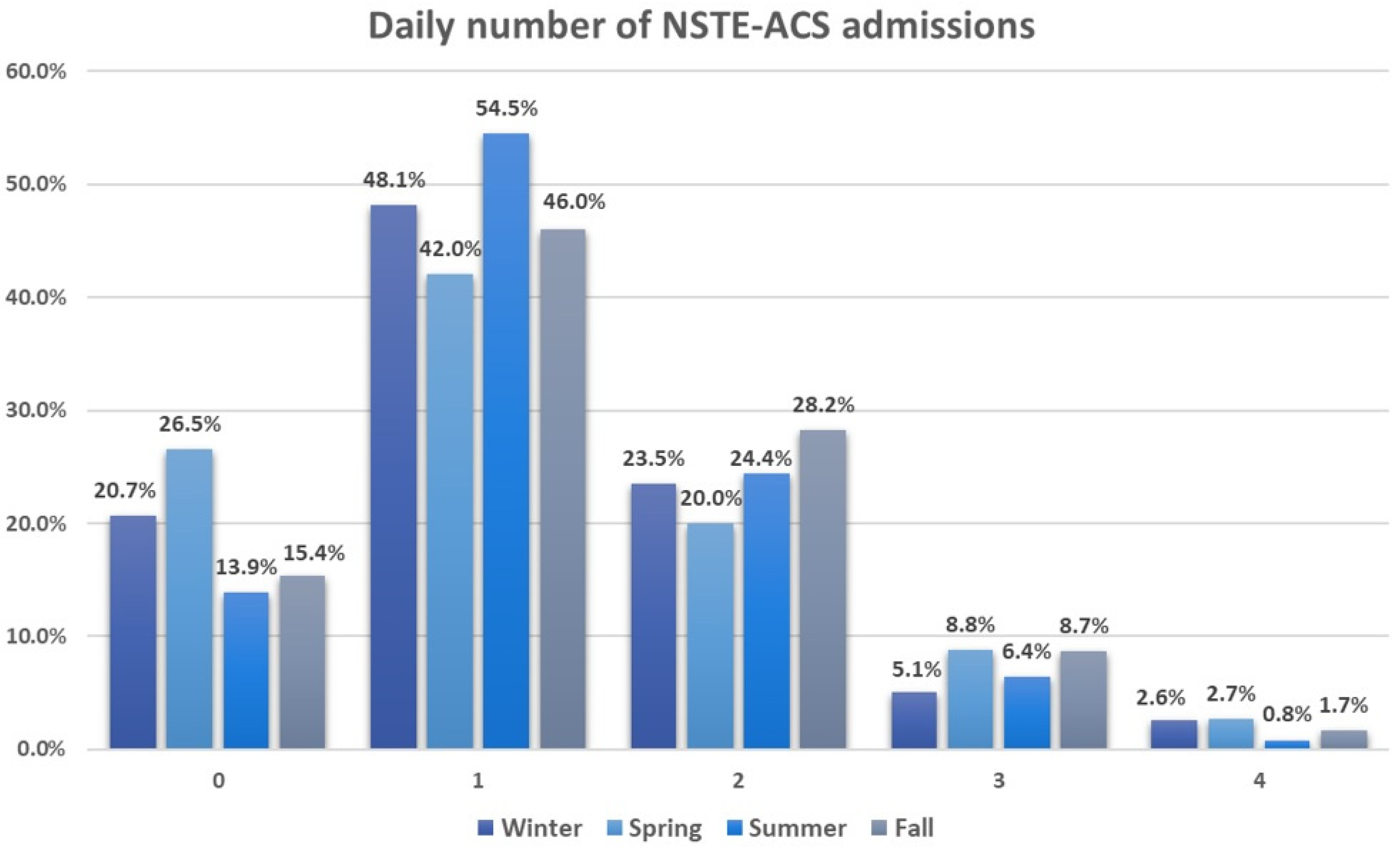
3. Results
3.1. Characteristics of Patients Hospitalized for Non-ST-Segment Elevation Acute Coronary Syndrome
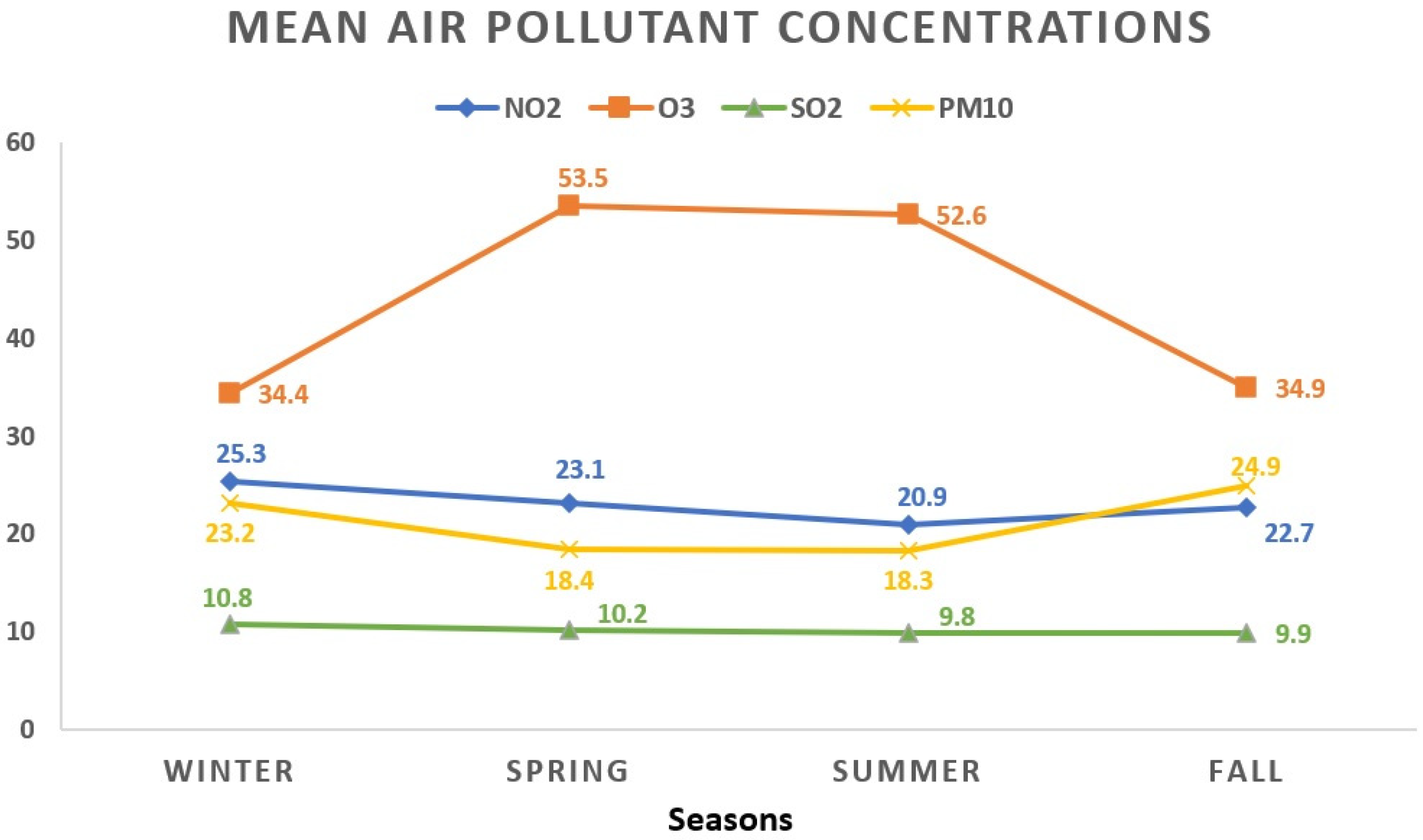
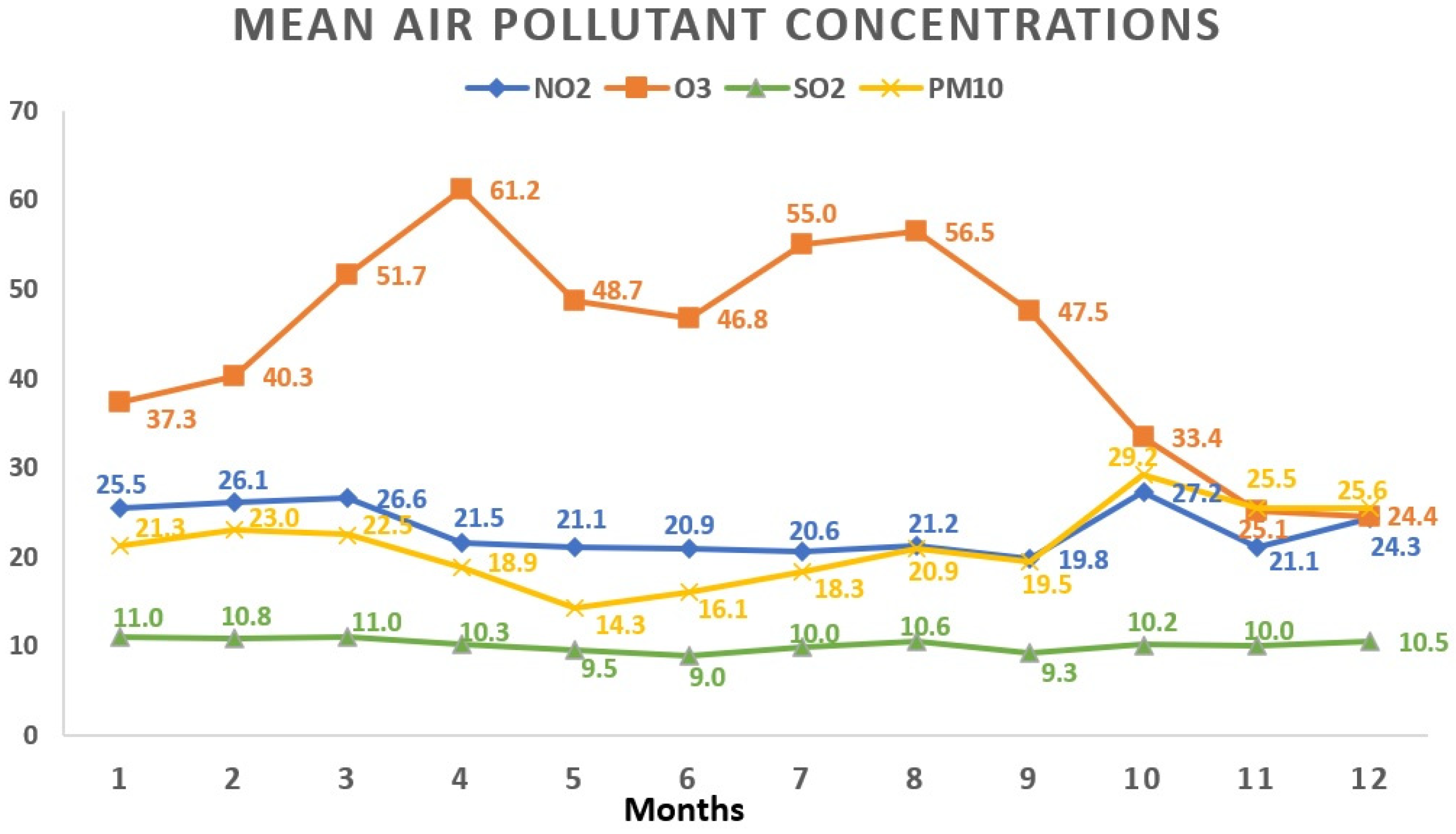
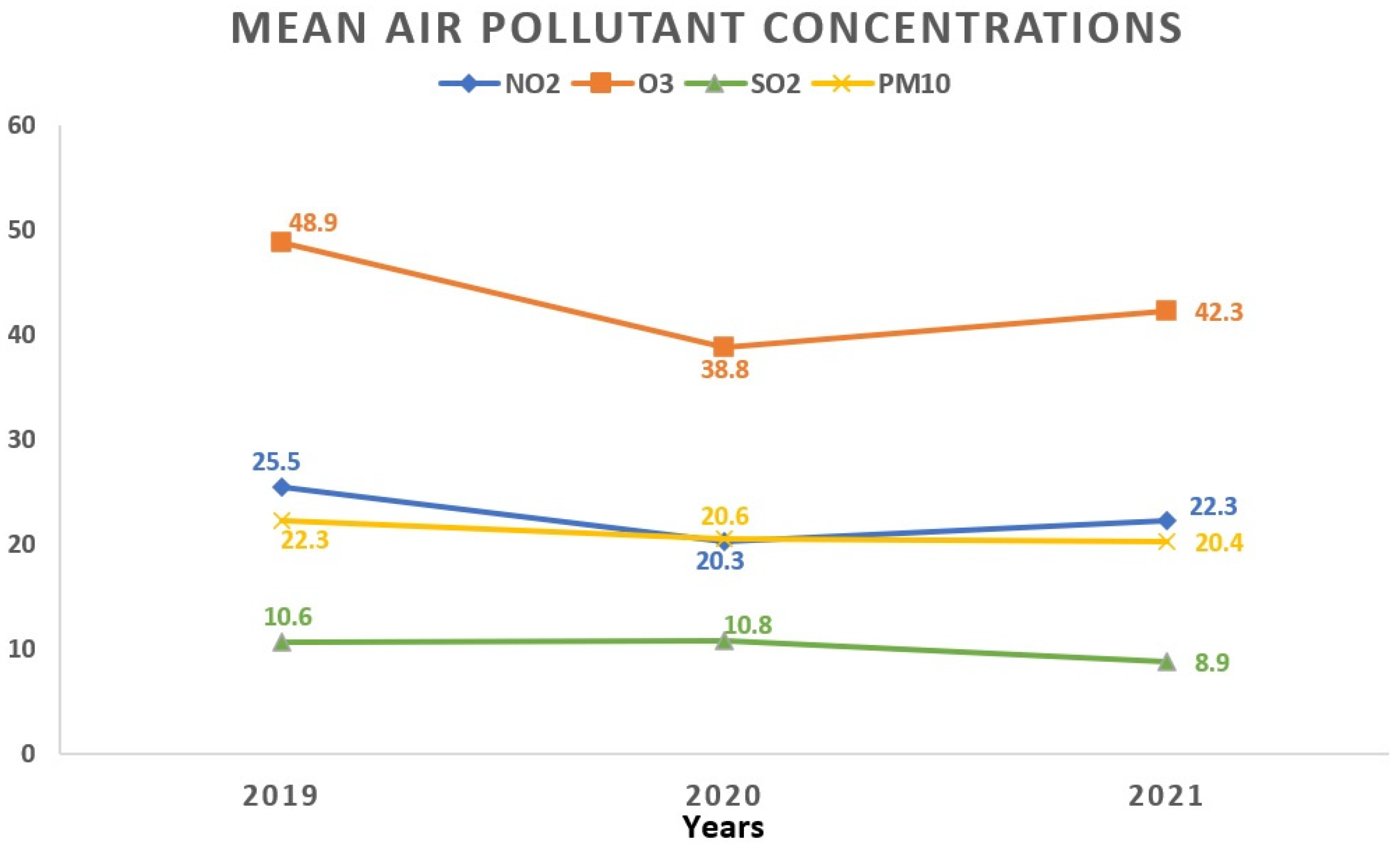
3.2. Daily Air Pollutants and Meteorological Variables Features
3.3. Evaluating the Influence of Elevated Atmospheric Pollutants Exceeding WHO Limits on Non-ST-Segment Elevation Acute Coronary Syndrome Hospital Admissions
3.4. Assessing the Influence of Brief Increases in Atmospheric Pollutant Concentrations (≥10 μg/m3) on Non-ST-segment Elevation Acute Coronary Syndrome Hospital Admissions
4. Discussion
5. Conclusions
Study Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Ambient (Outdoor) Air Pollution. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 30 November 2023).
- World Health Organization. Household Air Pollution. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/household-air-pollution-and-health (accessed on 30 November 2023).
- Markandya, A.; Sampedro, J.; Smith, S.J.; Van Dingenen, R.; Pizarro-Irizar, C.; Arto, I.; González-Eguino, M. Health co-benefits from air pollution and mitigation costs of the Paris Agreement: A modelling study. Lancet Planet Health 2018, 2, e126–e133. [Google Scholar] [CrossRef]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes: The Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC). Eur. Heart J. 2020, 41, 431. [Google Scholar] [CrossRef]
- Manisalidis, I.; Stavropoulou, E.; Stavropoulos, A.; Bezirtzoglou, E. Environmental and Health Impacts of Air Pollution: A Review. Front. Public Health 2020, 8, 14. [Google Scholar] [CrossRef] [PubMed]
- Brook, R.D.; Franklin, B.; Cascio, W.; Hong, Y.; Howard, G.; Lipsett, M.; Luepker, R.; Mittleman, M.; Samet, J.; Smith, S.C., Jr.; et al. Air Pollution and Cardiovascular Disease. Circulation 2004, 109, 2655–2671. [Google Scholar] [CrossRef]
- Libby, P. Current concepts of the pathogenesis of the acute coronary syndromes. Circulation 2001, 104, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Logan, W.P. Mortality in the London fog incident, 1952. Lancet 1953, 261, 336–338. [Google Scholar] [CrossRef] [PubMed]
- Nemery, B.; Hoet, P.H.; Nemmar, A. The Meuse Valley fog of 1930: An air pollution disaster. Lancet 2001, 357, 704–708. [Google Scholar] [CrossRef] [PubMed]
- Amsalu, E.; Wang, T.; Li, H.; Liu, Y.; Wang, A.; Liu, X.; Tao, L.; Luo, Y.; Zhang, F.; Yang, X.; et al. Acute effects of fine particulate matter (PM2.5) on hospital admissions for cardiovascular disease in Beijing, China: A time-series study. Environ. Health 2019, 18, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ruidavets, J.-B.; Cournot, M.; Cassadou, S.; Giroux, M.; Meybeck, M.; Ferrières, J. Ozone Air Pollution Is Associated with Acute Myocardial Infarction. Circulation 2005, 111, 563–569. [Google Scholar] [CrossRef]
- Jiang, Y.; Huang, J.; Li, G.; Wang, W.; Wang, K.; Wang, J.; Wei, C.; Li, Y.; Deng, F.; Baccarelli, A.A.; et al. Ozone pollution and hospital admissions for cardiovascular events. Eur. Heart J. 2023, 44, 1622–1632. [Google Scholar] [CrossRef]
- Gardner, B.; Ling, F.; Hopke, P.K.; Frampton, M.W.; Utell, M.J.; Zareba, W.; Cameron, S.J.; Chalupa, D.; Kane, C.; Kulandhaisamy, S.; et al. Ambient fine particulate air pollution triggers ST-elevation myocardial infarction, but not non-ST elevation myocardial infarction: A case-crossover study. Part Fibre Toxicol. 2014, 11, 1. [Google Scholar] [CrossRef] [PubMed]
- Tonne, C.; Wilkinson, P. Long-term exposure to air pollution is associated with survival following acute coronary syndrome. Eur. Heart J. 2013, 34, 1306–1311. [Google Scholar] [CrossRef] [PubMed]
- Pope, C.A., 3rd; Burnett, R.T.; Thun, M.J.; Calle, E.E.; Krewski, D.; Ito, K.; Thurston, G.D. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 2002, 287, 1132-41. [Google Scholar] [CrossRef]
- Bhaskaran, K.; Hajat, S.; Armstrong, B.; Haines, A.; Herrett, E.; Wilkinson, P.; Smeeth, L. The effects of hourly differences in air pollution on the risk of myocardial infarction: Case crossover analysis of the MINAP database. BMJ 2011, 343, d5531. [Google Scholar] [CrossRef] [PubMed]
- Vaudrey, B.; Mielcarek, M.; Sauleau, E.; Meyer, N.; Marchandot, B.; Moitry, M.; Robellet, P.; Reeb, T.; Jesel, L.; Ohlmann, P.; et al. Short-Term Effects of Air Pollution on Coronary Events in Strasbourg, France-Importance of Seasonal Variations. Med. Sci. 2020, 8, 31. [Google Scholar] [CrossRef] [PubMed]
- Belleudi, V.; Faustini, A.; Stafoggia, M.; Cattani, G.; Marconi, A.; Perucci, C.A.; Forastiere, F. Impact of fine and ultrafine particles on emergency hospital admissions for cardiac and respiratory diseases. Epidemiology 2010, 21, 414–423. [Google Scholar] [CrossRef] [PubMed]
- Kuźma, Ł.; Pogorzelski, S.; Struniawski, K.; Dobrzycki, S.; Bachórzewska-Gajewska, H. Effect of air pollution on the number of hospital admissions for acute coronary syndrome in elderly patients. Pol. Arch. Intern. Med. 2020, 130, 38–46. [Google Scholar] [CrossRef]
- Zou, L.; Zong, Q.; Fu, W.; Zhang, Z.; Xu, H.; Yan, S.; Mao, J.; Zhang, Y.; Cao, S.; Lv, C. Long-Term Exposure to Ambient Air Pollution and Myocardial Infarction: A Systematic Review and Meta-Analysis. Front. Med. 2021, 8, 616355. [Google Scholar] [CrossRef]
- Hanigan, I.C.; Rolfe, M.I.; Knibbs, L.D.; Salimi, F.; Cowie, C.T.; Heyworth, J.; Marks, G.B.; Guo, Y.; Cope, M.; Bauman, A.; et al. All-cause mortality and long-term exposure to low level air pollution in the ’45 and up study’ cohort, Sydney, Australia, 2006–2015. Environ. Int. 2019, 126, 762–770. [Google Scholar] [CrossRef]
- Huttunen, K.; Siponen, T.; Salonen, I.; Yli-Tuomi, T.; Aurela, M.; Dufva, H.; Hillamo, R.; Linkola, E.; Pekkanen, J.; Pennanen, A.; et al. Low-level exposure to ambient particulate matter is associated with systemic inflammation in ischemic heart disease patients. Environ. Res. 2012, 116, 44–51. [Google Scholar] [CrossRef]
- Rückerl, R.; Greven, S.; Ljungman, P.; Aalto, P.; Antoniades, C.; Bellander, T.; Berglind, N.; Chrysohoou, C.; Forastiere, F.; Jacquemin, B.; et al. AIRGENE Study Group. Air pollution and inflammation (interleukin-6, C-reactive protein, fibrinogen) in myocardial infarction survivors. Environ. Health Perspect. 2007, 115, 107280. [Google Scholar] [CrossRef]
- Mirowsky, J.E.; Carraway, M.S.; Dhingra, R.; Tong, H.; Neas, L.; Diaz-Sanchez, D.; Cascio, W.; Case, M.; Crooks, J.; Hauser, E.R.; et al. Ozone exposure is associated with acute changes in inflammation, fibrinolysis, and endothelial cell function in coronary artery disease patients. Environ. Health 2017, 16, 126. [Google Scholar] [CrossRef]
- Zhang, Y.; Shi, J.; Ma, Y.; Yu, N.; Zheng, P.; Chen, Z.; Wang, T.; Jia, G. Association between Air Pollution and Lipid Profiles. Toxics 2023, 11, 894. [Google Scholar] [CrossRef]
- Mills, N.L.; Törnqvist, H.; Gonzalez, M.C.; Vink, E.; Robinson, S.D.; Söderberg, S.; Boon, N.A.; Donaldson, K.; Sandström, T.; Blomberg, A.; et al. Ischemic and thrombotic effects of dilute diesel-exhaust inhalation in men with coronary heart disease. N. Engl. J. Med. 2007, 357, 1075–1082. [Google Scholar] [CrossRef] [PubMed]
- National Meteorological Administration. Available online: https://www.meteoromania.ro/clima/clima-romaniei/ (accessed on 29 November 2023).
- Mohammadian-Khoshnoud, M.; Habibi, H.; Manafi, B.; Safarpour, G.; Soltanian, A.R. Effects of Air Pollutant Exposure on Acute Myocardial Infarction. Heart Lung Circ. 2023, 32, 79–89. [Google Scholar] [CrossRef]
- Liang, L.; Cai, Y.; Lyu, B.; Zhang, D.; Chu, S.; Jing, H.; Rahimi, K.; Tong, Z. Air pollution and hospitalization of patients with idiopathic pulmonary fibrosis in Beijing: A time-series study. Respir. Res. 2022, 23, 81. [Google Scholar] [CrossRef] [PubMed]
- Milojevic, A.; Wilkinson, P.; Armstrong, B.; Bhaskaran, K.; Smeeth, L.; Hajat, S. Short-term effects of air pollution on a range of cardiovascular events in England and Wales: Case-crossover analysis of the MINAP database, hospital admissions and mortality. Heart 2014, 100, 1093–1098. [Google Scholar] [CrossRef]
- Wang, X.; Kindzierski, W.; Kaul, P. Air Pollution and Acute Myocardial Infarction Hospital Admission in Alberta, Canada: A Three-Step Procedure Case-Crossover Study. PLoS ONE 2015, 10, e0132769. [Google Scholar] [CrossRef] [PubMed]
- Kuźma, Ł.; Pogorzelski, S.; Struniawski, K.; Bachórzewska-Gajewska, H.; Dobrzycki, S. Exposure to air pollution-a trigger for myocardial infarction? A nine-year study in Bialystok-the capital of the Green Lungs of Poland (BIA-ACS registry). Int. J. Hyg. Environ. Health 2020, 229, 113578. [Google Scholar] [CrossRef]
- Mustafic, H.; Jabre, P.; Caussin, C.; Murad, M.H.; Escolano, S.; Tafflet, M.; Périer, M.C.; Marijon, E.; Vernerey, D.; Empana, J.P.; et al. Main air pollutants and myocardial infarction: A systematic review and meta-analysis. JAMA 2012, 307, 713–721. [Google Scholar] [CrossRef]
- Kuźma, Ł.; Wańha, W.; Kralisz, P.; Kazmierski, M.; Bachórzewska-Gajewska, H.; Wojakowski, W.; Dobrzycki, S. Impact of short-term air pollution exposure on acute coronary syndrome in two cohorts of industrial and non-industrial areas: A time series regression with 6,000,000 person-years of follow-up (ACS—Air Pollution Study). Environ. Res. 2021, 197, 111154. [Google Scholar] [CrossRef]
- Sahlén, A.; Ljungman, P.; Erlinge, D.; Chan, M.Y.; Yap, J.; Hausenloy, D.J.; Yeo, K.K.; Jernberg, T. Air pollution in relation to very short-term risk of ST-segment elevation myocardial infarction: Case-crossover analysis of SWEDEHEART. Int. J. Cardiol. 2019, 275, 26–30. [Google Scholar] [CrossRef]
- Butland, B.K.; Atkinson, R.W.; Milojevic, A.; Heal, M.R.; Doherty, R.M.; Armstrong, B.G.; MacKenzie, I.A.; Vieno, M.; Lin, C.; Wilkinson, P. Myocardial infarction, ST-elevation and non-ST-elevation myocardial infarction and modelled daily pollution concentrations: A case-crossover analysis of MINAP data. Open Heart 2016, 3, e000429. [Google Scholar] [CrossRef] [PubMed]
- Cesaroni, G.; Forastiere, F.; Stafoggia, M.; Andersen, Z.J.; Badaloni, C.; Beelen, R.; Caracciolo, B.; de Faire, U.; Erbel, R.; Eriksen, K.T.; et al. Long term exposure to ambient air pollution and incidence of acute coronary events: Prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. BMJ 2014, 348, f7412. [Google Scholar] [CrossRef]
- Guo, Y.; Tong, S.; Zhang, Y.; Barnett, A.G.; Jia, Y.; Pan, X. The relationship between particulate air pollution and emergency hospital visits for hypertension in Beijing, China. Sci. Total Environ. 2010, 408, 4446–4450. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.W.; Lau, T.S.; Yu, T.S.; Neller, A.; Wong, S.L.; Tam, W.; Pang, S.W. Air pollution and hospital admissions for respiratory and cardiovascular diseases in Hong Kong. Occup. Environ. Med. 1999, 56, 679–683. [Google Scholar] [CrossRef]
- Rodopoulou, S.; Chalbot, M.C.; Samoli, E.; Dubois, D.W.; San Filippo, B.D.; Kavouras, I.G. Air pollution and hospital emergency room and admissions for cardiovascular and respiratory diseases in Doña Ana County, New Mexico. Environ. Res. 2014, 129, 39–46. [Google Scholar] [CrossRef]
- Mantovani, K.C.; Nascimento, L.F.; Moreira, D.S.; Vieira, L.C.; Vargas, N.P. Air pollutants and hospital admissions due to cardiovascular diseases in São José do Rio Preto, Brazil. Cien Saude Colet. 2016, 21, 509–515. [Google Scholar] [CrossRef][Green Version]
- Newby, D.E.; Mannucci, P.M.; Tell, G.S.; Baccarelli, A.A.; Brook, R.D.; Donaldson, K.; Forastiere, F.; Franchini, M.; Franco, O.H.; Graham, I.; et al. ESC Working Group on Thrombosis, European Association for Cardiovascular Prevention and Rehabilitation; ESC Heart Failure Association. Expert position paper on air pollution and cardiovascular disease. Eur. Heart J. 2015, 36, 83b–93b. [Google Scholar] [CrossRef] [PubMed]
- Montone, R.A.; Camilli, M.; Russo, M.; Termite, C.; La Vecchia, G.; Iannaccone, G.; Rinaldi, R.; Gurgoglione, F.; Del Buono, M.G.; Sanna, T.; et al. Air Pollution and Coronary Plaque Vulnerability and Instability: An Optical Coherence Tomography Study. JACC Cardiovasc. Imaging. 2022, 15, 325–342. [Google Scholar] [CrossRef]
- Sun, L.; Liu, C.; Xu, X.; Ying, Z.; Maiseyeu, A.; Wang, A.; Allen, K.; Lewandowski, R.P.; Bramble, L.A.; Morishita, M.; et al. Ambient fine particulate matter and ozone exposures induce inflammation in epicardial and perirenal adipose tissues in rats fed a high fructose diet. Part Fibre Toxicol. 2013, 10, 43. [Google Scholar] [CrossRef] [PubMed]
- Devlin, R.B.; Duncan, K.E.; Jardim, M.; Schmitt, M.T.; Rappold, A.G.; Diaz-Sanchez, D. Controlled exposure of healthy young volunteers to ozone causes cardiovascular effects. Circulation 2012, 126, 104–411. [Google Scholar] [CrossRef] [PubMed]
| NSTE-ACS (n = 1547) | |
|---|---|
| Age (years) | 63.53 ± 10.0 |
| Gender (male) (female) | 1122 (72.5%) 425 (27.5%) |
| BMI (kg/m2) | 29.23 ± 5.1 |
| Clinical and paraclinical parameters at admission | |
| SBP (mmHg) | 138.95 ± 21.4 |
| DBP (mmHg) | 80.18 ± 12.0 |
| HR (bpm) | 72.52 ± 14.1 |
| Hemoglobin (mg/dL) | 13.96 ± 1.8 |
| Creatinine (mg/dL) | 1.19 ± 0.8 |
| Glucose (mg/dL) | 129.68 ± 52.6 |
| Total cholesterol (mg/dL) | 153.07 ± 44.8 |
| Triglycerides (mg/dL) | 151.43 ± 91.5 |
| LDL-cholesterol (mg/dL) | 94.08 ± 33.6 |
| HDL-cholesterol (mg/dL) | 34.756 ± 15.6 |
| Cardiovascular risk factors | |
| Smoking | 354 (22.9%) |
| Arterial hypertension | 1341 (86.7%) |
| Diabetes mellitus | 506 (32.7%) |
| Hypercholesterolemia | 588 (38%) |
| Coronary arteries lesions | |
| Single-vessel lesion | 436 (28.2%) |
| Two-vessel lesion | 542 (35%) |
| Three-vessel lesion | 569 (36.8%) |
| Treatment at admission | |
| PCI primary | 1306 (84.4%) |
| Balloon angioplasty | 19 (1.2%) |
| CABG | 88 (5.7%) |
| Conservative | 134 (8.7%) |
| Type of NSTE-ACS | |
| NSTEMI | 264 (17.1%) |
| UA | 1283 (82.9%) |
| Total Days (n = 1908) | Mean ± SD | Minimum | Percentiles | Maximum | ||
|---|---|---|---|---|---|---|
| 25th | 50th | 75th | ||||
| NO2 (μg/m3) | 23.0 ± 11.7 | 0.5 | 14.6 | 21.0 | 29.3 | 81.2 |
| O3 (μg/m3) | 43.9 ± 19.3 | 4.3 | 28.7 | 43.7 | 56.9 | 141.7 |
| SO2 (μg/m3) | 10.2 ± 3.6 | 3.7 | 8.0 | 9.3 | 11.2 | 43.3 |
| PM10 (μg/m3) | 21.2 ± 13.6 | 1.5 | 12.3 | 18.2 | 26.3 | 114.0 |
| Air temperature (°C) | 12.7 ± 8.5 | −8.3 | 5.7 | 12.5 | 19.7 | 30.4 |
| Relative humidity (%) | 72.4 ± 14.2 | 32.0 | 62 | 73 | 84 | 100.0 |
| NO2 | O3 | SO2 | PM10 | Temperature | Relative Humidity | |
|---|---|---|---|---|---|---|
| NO2 | 1 | −0.31 ** | −0.01 | 0.33 ** | −0.14 ** | 0.00 |
| O3 | −0.31 ** | 1 | 0.11 ** | −0.17 ** | 0.43 ** | −0.63 ** |
| SO2 | −0.01 | 0.11 ** | 1 | 0.16 ** | −0.08 ** | −0.05 * |
| PM10 | 0.33 ** | −0.17 ** | 0.16 ** | 1 | −0.08 ** | −0.03 |
| Temperature | −0.14 ** | 0.43 ** | −0.08 ** | −0.08 ** | 1 | −0.51 ** |
| Relative humidity | 0.00 | −0.63 ** | −0.05 * | −0.03 | −0.51 ** | 1 |
| Air Pollutants | NO2 ≥ 25 μg/m3 (WHO Guideline) | O3 ≥ 100 μg/m3 (WHO Guideline) * | SO2 ≥ 40 μg/m3 (WHO Guideline) * | PM10 ≥ 45 μg/m3 (WHO Guideline) | ||||
|---|---|---|---|---|---|---|---|---|
| Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | |
| Season | ||||||||
| All Seasons | 1.223 (1.125–1.330) | <0.001 | 0.652 (0.308–1.379) | 0.263 | 0.689 (0.172–2.759) | 0.598 | 0.896 (0.742–1.082) | 0.252 |
| 3 Winters | 1.077 (0.909–1.278) | 0.391 | 0.699 (0.097–5.036) | 0.722 | 0.843 (0.208–3.408) | 0.811 | 0.840 (0.606–1.163) | 0.293 |
| 3 Springs | 1.426 (1.196–1.701) | <0.001 | 0.728 (0.321–1.649) | 0.446 | - | - | 0.884 (0.470–1.664) | 0.703 |
| 3 Summers | 1.263 (1.072–1.487) | 0.005 | - | - | - | - | 1.274 (0.673–2.411) | 0.458 |
| 3 Falls | 1.143 (0.968–1.350) | 0.115 | - | - | - | - | 0.955 (0.718–1.272) | 0.754 |
| NO2 ≥ 25 μg/m3 (WHO Guideline) | O3 ≥ 100 μg/m3 (WHO Guideline) * | SO2 ≥ 40 μg/m3 (WHO Guideline) * | PM10 ≥ 45 μg/m3 (WHO Guideline) | |||||
|---|---|---|---|---|---|---|---|---|
| Subgroups | Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value |
| Gender | ||||||||
| Male (n = 1122) | 1.034 (0.934–1.143) | 0.521 | 0.676 (0.251–1.816) | 0.437 | 0.628 (0.157–2.519) | 0.512 | 0.853 (0.660–1.103) | 0.226 |
| Female (n = 425) | 1.114 (0.951–1.304) | 0.181 | 0.629 (0.154–2.572) | 0.519 | - | - | 0.942 (0.655–1.355) | 0.747 |
| Age | ||||||||
| <65 (n = 797) | 1.095 (0.972–1.234) | 0.134 | 0.655 (0.208–2.058) | 0.468 | 0.610 (0.152–2.448) | 0.486 | 0.873 (0.656–1.160) | 0.349 |
| ≥65 (n = 750) | 1.024 (0.907–1.156) | 0.700 | 0.667 (0.213–2.092) | 0.488 | - | - | 0.889 (0.652–1.211) | 0.456 |
| Patients with/without CVRF | ||||||||
| DM + (n = 506) | 0.998 (0.858–1.162) | 0.984 | 0.660 (0.242–1.800) | 0.417 | 0.609 (0.085–4.349) | 0.621 | 0.935 (0.641–1.363) | 0.726 |
| DM − (n = 1041) | 1.089 (0.982–1.208) | 0.105 | 0.667 (0.166–2.685) | 0.569 | 0.609 (0.086–4.334) | 0.621 | 0.859 (0.667–1.106) | 0.237 |
| HTN + (n = 1341) | 1.101 (1.007–1.204) | 0.035 | 0.660 (0.311–1.398) | 0.278 | 0.595 (0.148–2.383) | 0.463 | 0.858 (0.697–1.057) | 0.150 |
| HTN − (n = 206) | 0.982 (0.757–1.272) | 0.888 | - | - | - | - | 1.255 (0.791–1.992) | 0.334 |
| Coronary artery disease | ||||||||
| Single-vessel lesions (n = 436) | 1.009 (0.853–1.192) | 0.918 | 0.707 (0.224–2.232) | 0.554 | - | - | 0.880 (0.558–1.390) | 0.585 |
| Multi-vessel lesions (n = 1111) | 1.072 (0.971–1.183) | 0.167 | 0.643 (0.205–2.016) | 0.449 | 0.596 (0.149–2.387) | 0.464 | 0.878 (0.693–1.112) | 0.279 |
| Type of NSTE-ACS | ||||||||
| NSTEMI (n = 1283) | 0.997 (0.810–1.227) | 0.975 | 0.603 (0.258–1.412) | 0.244 | - | - | 0.829 (0.489–1.408) | 0.488 |
| UA (n = 264) | 1.107 (1.010–1.213) | 0.030 | 0.673 (0.095–4.792) | 0.693 | 0.602 (0.150–2.413) | 0.474 | 0.915 (0.748–1.120) | 0.390 |
| NO2 (μg/m3) | O3 (μg/m3) | SO2 (μg/m3) | PM10 (μg/m3) | |||||
|---|---|---|---|---|---|---|---|---|
| Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | |
| Lag 03 | ||||||||
| All Season | 1.005 (1.001–1.010) | 0.017 | 1.002 (0.998–1.005) | 0.288 | 0.987 (0.973–1.002) | 0.083 | 0.998 (0.994–1.001) | 0.213 |
| 3 Winters | 1.005 (0.997–1.014) | 0.179 | 1.007 (1.001–1.013) | 0.029 | 0.996 (0.971–1.022) | 0.770 | 0.994 (0.987–1.002) | 0.151 |
| 3 Springs | 1.013 (1.001–1.024) | 0.027 | 1.004 (0.996–1.011) | 0.309 | 0.972 (0.936–1.009) | 0.132 | 0.994 (0.982–1.006) | 0.301 |
| 3 Summers | 1.007 (0.999–1.016) | 0.085 | 1.002 (0.994–1.010) | 0.603 | 0.976 (0.949–1.004) | 0.095 | 0.998 (0.986–1.011) | 0.793 |
| 3 Falls | 0.997 (0.986–1.007) | 0.543 | 0.996 (0.988–1.055) | 0.424 | 0.998 (0.968–1.030) | 0.923 | 1.001 (0.993–1.008) | 0.881 |
| Lag 05 | ||||||||
| All Season | 1.005 (1.000–1.009) | 0.041 | 1.002 (0.999–1.006) | 0.220 | 0.983 (0.968–0.998) | 0.310 | 0.998 (0.994–1.002) | 0.333 |
| 3 Winters | 1.005 (0.997–1.013) | 0.258 | 1.007 (1.001–1.014) | 0.025 | 0.995 (0.969–1.022) | 0.717 | 0.994 (0.986–1.003) | 0.180 |
| 3 Springs | 1.010 (0.998–1.022) | 0.088 | 1.004 (0.996–1.011) | 0.365 | 0.958 (0.920–0.996) | 0.321 | 0.999 (0.986–1.012) | 0.853 |
| 3 Summers | 1.008 (0.999–1.017) | 0.090 | 1.002 (0.993–1.011) | 0.618 | 0.978 (0.951–1.006) | 0.130 | 1.001 (0.988–1.015) | 0.852 |
| 3 Falls | 0.996 (0.985–1.007) | 0.437 | 0.997 (0.988–1.006) | 0.524 | 0.991 (0.960–1.024) | 0.598 | 1.001 (0.993–1.009) | 0.795 |
| Lag 07 | ||||||||
| All Season | 1.006 (1.001–1.011) | 0.010 | 1.002 (0.998–1.005) | 0.364 | 0.983 (0.968–0.999) | 0.351 | 0.998 (0.994–1.002) | 0.384 |
| 3 Winters | 1.004 (0.996–1.013) | 0.300 | 1.006 (1.000–1.013) | 0.067 | 0.996 (0.970–1.023) | 0.764 | 0.996 (0.987–1.004) | 0.302 |
| 3 Springs | 1.013 (1.001–1.025) | 0.033 | 1.004 (0.996–1.012) | 0.346 | 0.950 (0.912–0.989) | 0.130 | 1.006 (0.992–1.020) | 0.386 |
| 3 Summers | 1.010 (1.001–1.019) | 0.032 | 1.002 (0.992–1.011) | 0.745 | 0.984 (0.957–1.012) | 0.255 | 1.004 (0.991–1.018) | 0.538 |
| 3 Falls | 0.997 (0.986–1.008) | 0.579 | 0.995 (0.986–1.005) | 0.317 | 0.993 (0.961–1.026) | 0.664 | 0.999 (0.991–1.007) | 0.812 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rus, A.-A.; Pescariu, S.-A.; Zus, A.-S.; Gaiţă, D.; Mornoş, C. Impact of Short-Term Exposure to Nitrogen Dioxide (NO2) and Ozone (O3) on Hospital Admissions for Non-ST-Segment Elevation Acute Coronary Syndrome. Toxics 2024, 12, 123. https://doi.org/10.3390/toxics12020123
Rus A-A, Pescariu S-A, Zus A-S, Gaiţă D, Mornoş C. Impact of Short-Term Exposure to Nitrogen Dioxide (NO2) and Ozone (O3) on Hospital Admissions for Non-ST-Segment Elevation Acute Coronary Syndrome. Toxics. 2024; 12(2):123. https://doi.org/10.3390/toxics12020123
Chicago/Turabian StyleRus, Andreea-Alexandra, Silvius-Alexandru Pescariu, Adrian-Sebastian Zus, Dan Gaiţă, and Cristian Mornoş. 2024. "Impact of Short-Term Exposure to Nitrogen Dioxide (NO2) and Ozone (O3) on Hospital Admissions for Non-ST-Segment Elevation Acute Coronary Syndrome" Toxics 12, no. 2: 123. https://doi.org/10.3390/toxics12020123
APA StyleRus, A.-A., Pescariu, S.-A., Zus, A.-S., Gaiţă, D., & Mornoş, C. (2024). Impact of Short-Term Exposure to Nitrogen Dioxide (NO2) and Ozone (O3) on Hospital Admissions for Non-ST-Segment Elevation Acute Coronary Syndrome. Toxics, 12(2), 123. https://doi.org/10.3390/toxics12020123







