Machine Learning Big Data Analysis of the Impact of Air Pollutants on Rhinitis-Related Hospital Visits
Abstract
:1. Introduction
2. Materials and Methods
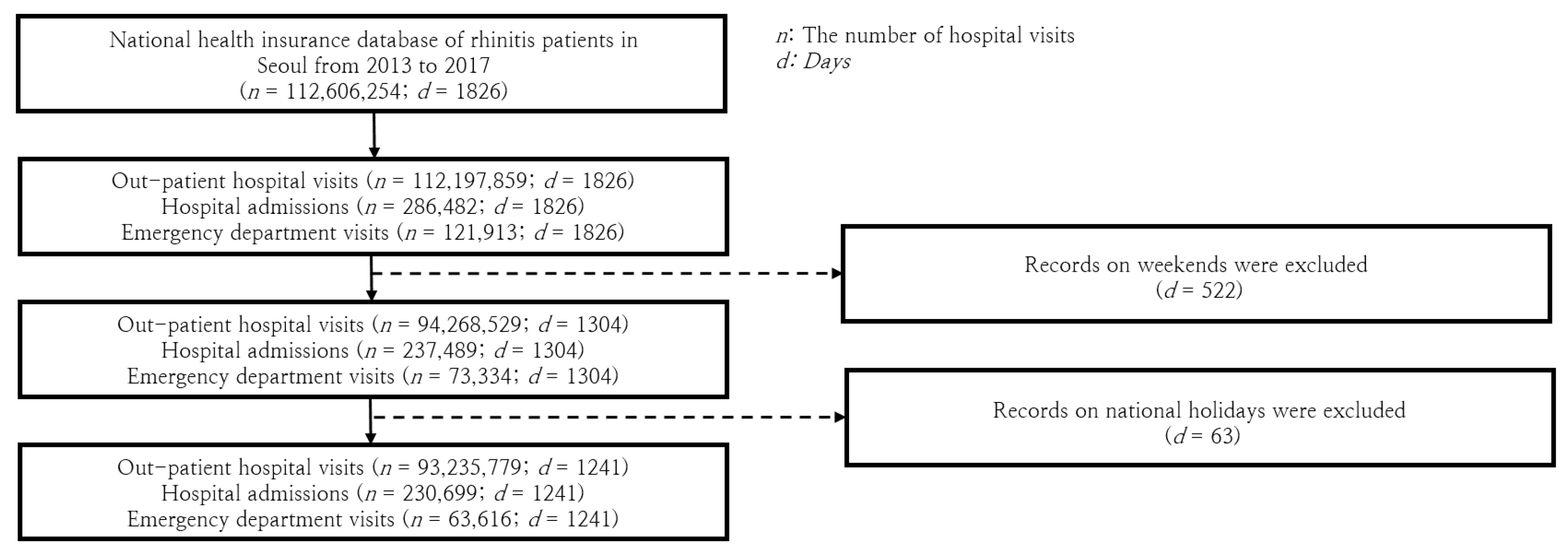
2.1. The Comprehensive Rhinitis Patient Visit Database in Seoul
2.2. Database of Daily Atmospheric Environmental Details
2.3. Analytical Approach: Combining Traditional Statistics and Machine Learning
2.3.1. Pearson and Spearman Correlations
2.3.2. Least Absolute Shrinkage and Selection Operator (LASSO)
2.3.3. Random Forest (RF)
2.3.4. Gradient Boosting Machine (GBM)
2.3.5. Interpreting Coefficients and Importance Measures
3. Results
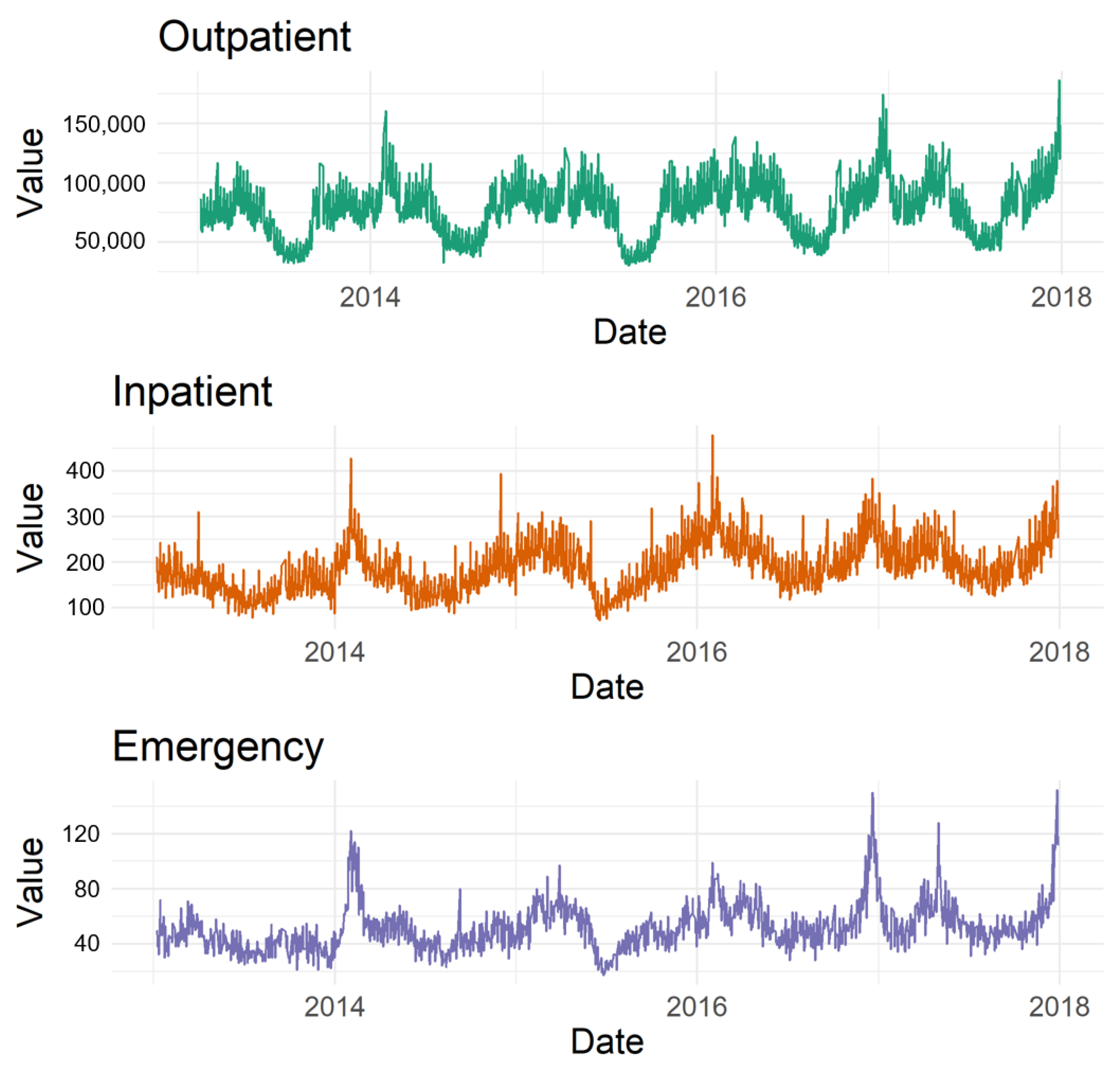
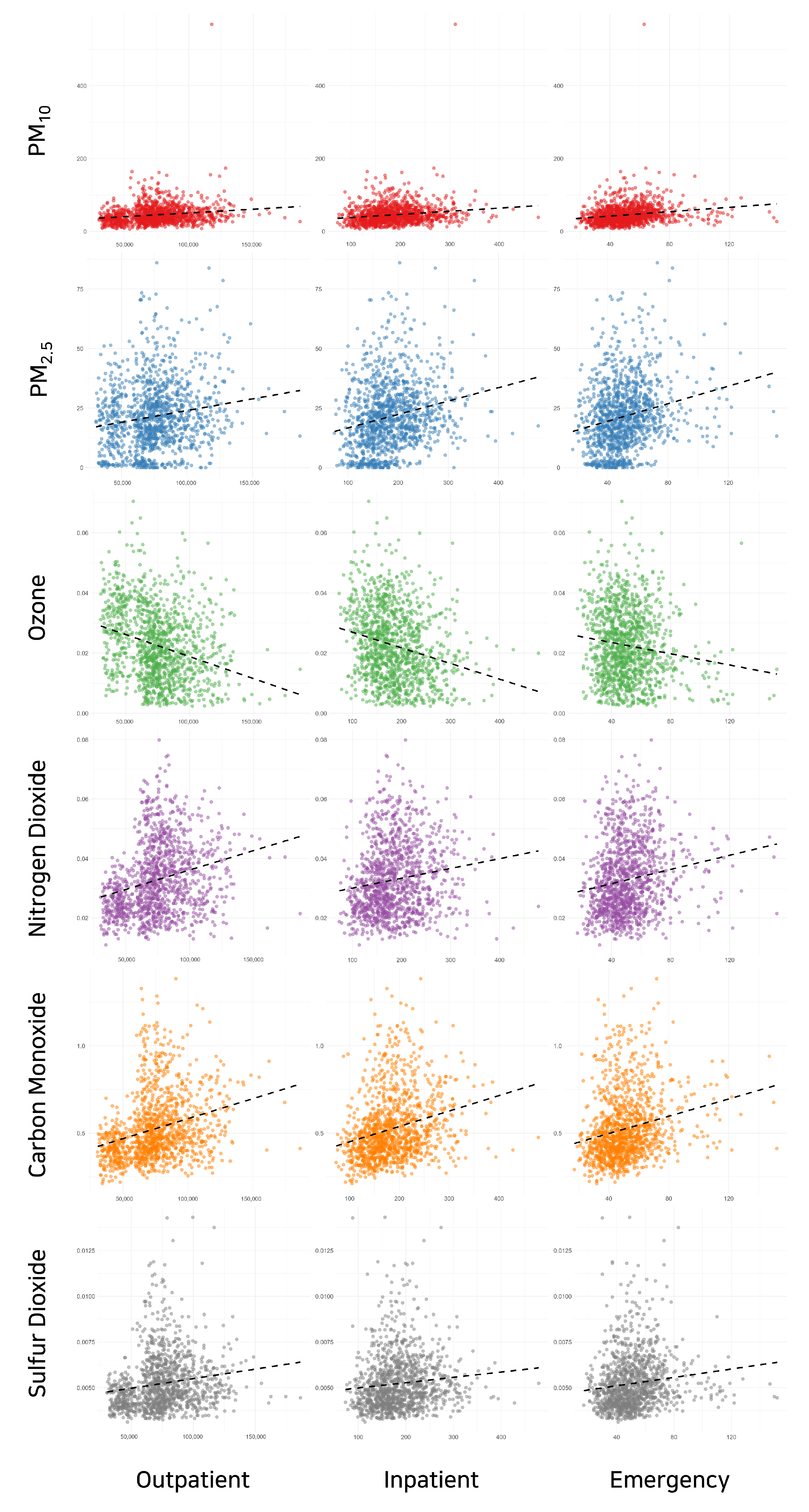
3.1. Exploratory Data Analysis
3.1.1. Air Pollutants Correlations
3.1.2. Hospital Visit Correlations
3.1.3. Pollutants and Patient Visits
3.2. Analysis of Hospital Visits and Air Pollutants Using Statistical Analysis
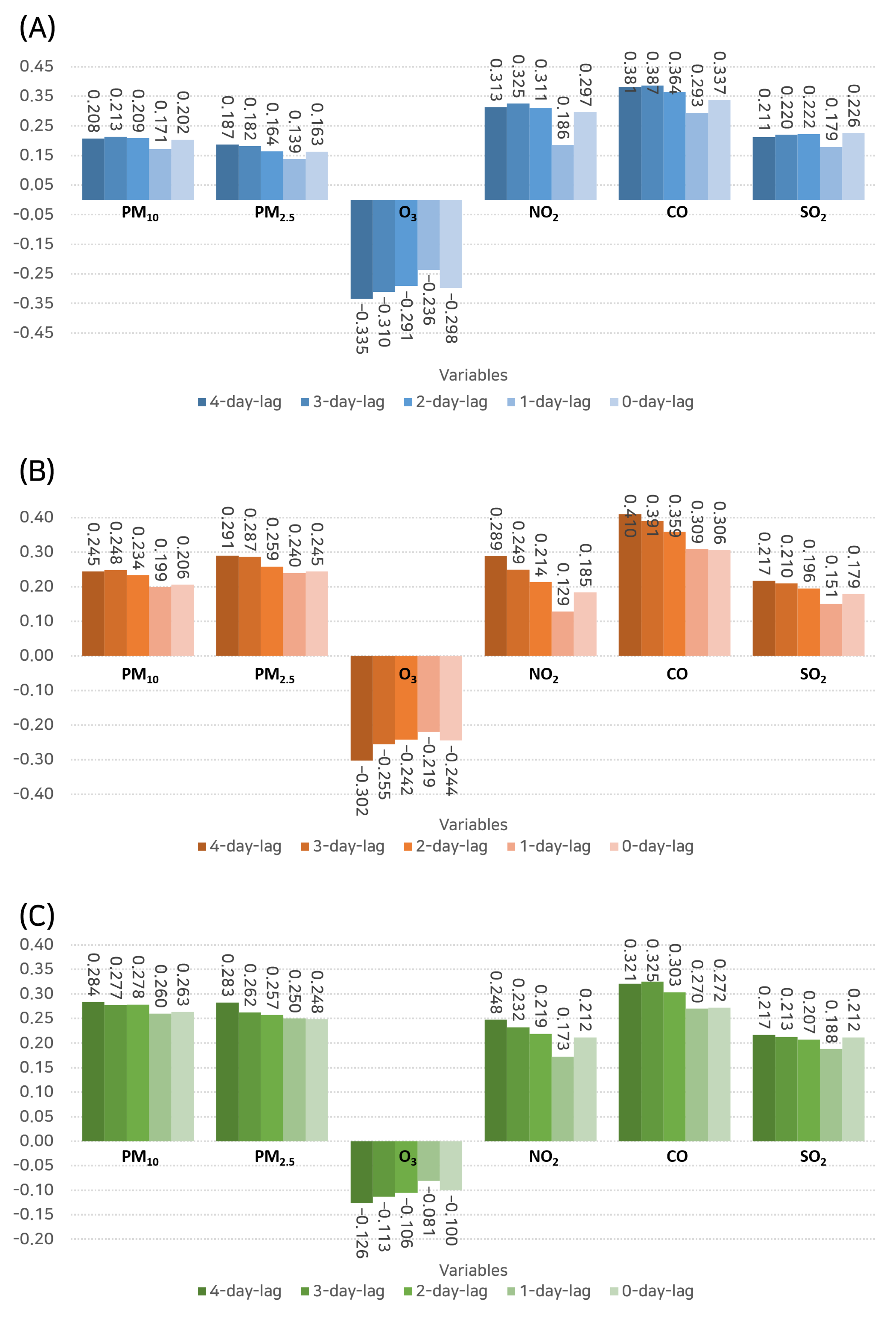
3.2.1. Pearson Correlation Analysis
3.2.2. Spearman Correlation Analysis
3.3. Analysis of Hospital Visits and Air Pollutants Using Machine Learning Analysis
3.3.1. LASSO Analysis
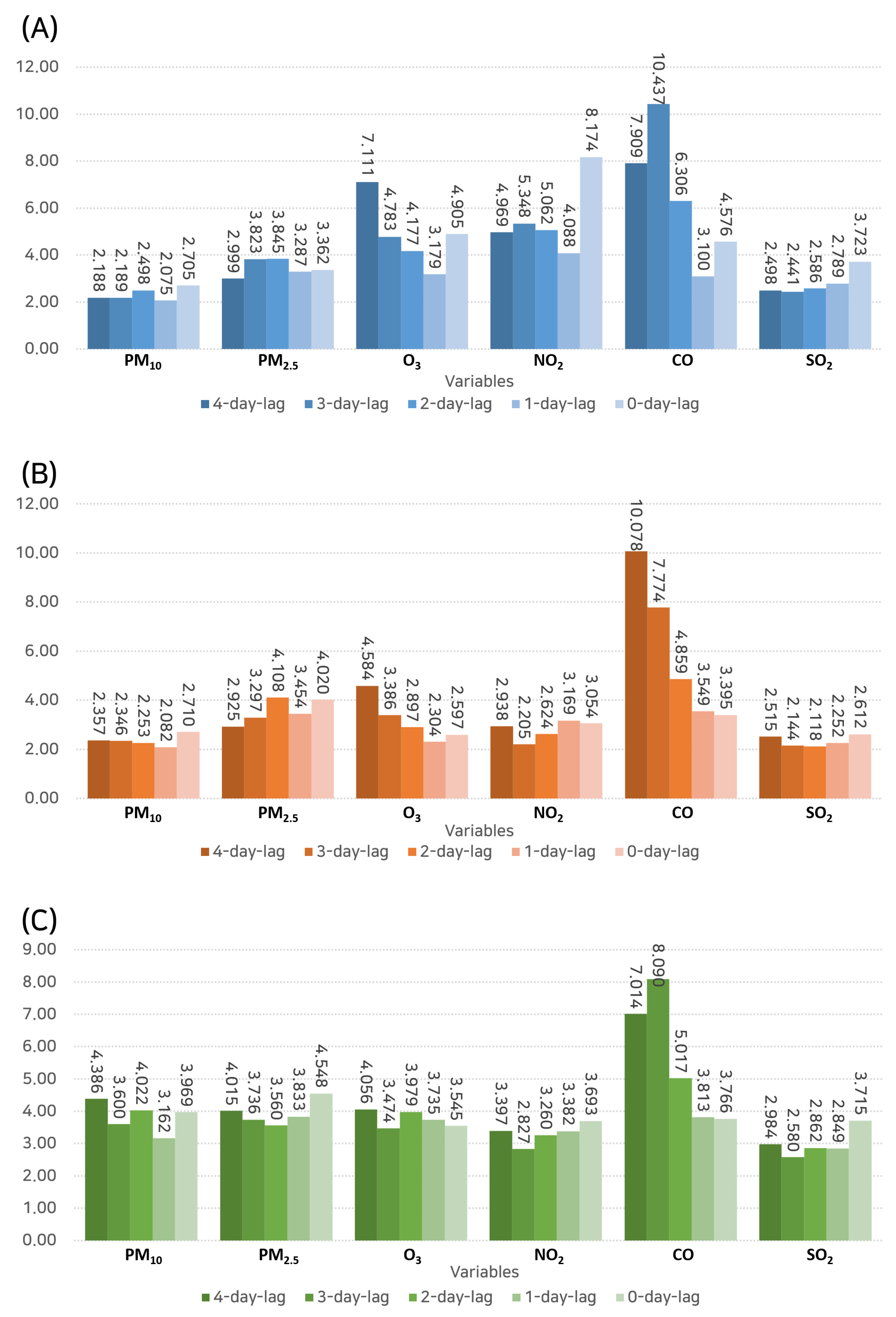
3.3.2. Random Forest Analysis
3.3.3. Gradient Boosting Machine Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Imbens, G.W.; Rubin, D.B. Causal Inference in Statistics, Social, and Biomedical Sciences; Cambridge University Press: Cambridge, UK, 2015. [Google Scholar]
- Yoo, I.; Alafaireet, P.; Marinov, M.; Pena-Hernandez, K.; Gopidi, R.; Chang, J.F.; Hua, L. Data mining in healthcare and biomedicine: A survey of the literature. J. Med. Syst. 2012, 36, 2431–2448. [Google Scholar] [CrossRef] [PubMed]
- Manzoni, C.; Kia, D.A.; Vandrovcova, J.; Hardy, J.; Wood, N.W.; Lewis, P.A.; Ferrari, R. Genome, transcriptome and proteome: The rise of omics data and their integration in biomedical sciences. Briefings Bioinform. 2018, 19, 286–302. [Google Scholar] [CrossRef]
- Greiner, A.N.; Hellings, P.W.; Rotiroti, G.; Scadding, G.K. Allergic rhinitis. Lancet 2011, 378, 2112–2122. [Google Scholar] [CrossRef] [PubMed]
- Varshney, J.; Varshney, H. Allergic rhinitis: An overview. Indian J. Otolaryngol. Head Neck Surg. 2015, 67, 143–149. [Google Scholar] [CrossRef]
- Bousquet, J.; Anto, J.M.; Bachert, C.; Baiardini, I.; Bosnic-Anticevich, S.; Walter Canonica, G.; Melén, E.; Palomares, O.; Scadding, G.K.; Togias, A.; et al. Allergic rhinitis. Nat. Rev. Dis. Prim. 2020, 6, 95. [Google Scholar] [CrossRef] [PubMed]
- Kelly, F.J.; Fussell, J.C. Air pollution and public health: Emerging hazards and improved understanding of risk. Environ. Geochem. Health 2015, 37, 631–649. [Google Scholar] [CrossRef]
- Klepac, P.; Locatelli, I.; Korošec, S.; Künzli, N.; Kukec, A. Ambient air pollution and pregnancy outcomes: A comprehensive review and identification of environmental public health challenges. Environ. Res. 2018, 167, 144–159. [Google Scholar] [CrossRef]
- Turner, M.C.; Andersen, Z.J.; Baccarelli, A.; Diver, W.R.; Gapstur, S.M.; Pope III, C.A.; Prada, D.; Samet, J.; Thurston, G.; Cohen, A. Outdoor air pollution and cancer: An overview of the current evidence and public health recommendations. CA Cancer J. Clin. 2020, 70, 460–479. [Google Scholar] [CrossRef]
- Lee, S.; Ku, H.; Hyun, C.; Lee, M. Machine Learning-Based Analyses of the Effects of Various Types of Air Pollutants on Hospital Visits by Asthma Patients. Toxics 2022, 10, 644. [Google Scholar] [CrossRef]
- Lee, S.; Lee, M. Low-to-moderate atmospheric ozone levels are negatively correlated with hospital visits by asthma patients. Medicine 2022, 101, e31737. [Google Scholar] [CrossRef]
- Syuhada, G.; Akbar, A.; Hardiawan, D.; Pun, V.; Darmawan, A.; Heryati, S.H.A.; Siregar, A.Y.M.; Kusuma, R.R.; Driejana, R.; Ingole, V.; et al. Impacts of Air Pollution on Health and Cost of Illness in Jakarta, Indonesia. Int. J. Environ. Res. Public Health 2023, 20, 2916. [Google Scholar] [CrossRef] [PubMed]
- Pinakana, S.D.; Mendez, E.; Ibrahim, I.; Majumder, M.S.; Raysoni, A.U. Air Pollution in South Texas: A Short Communication of Health Risks and Implications. Air 2023, 1, 94–103. [Google Scholar] [CrossRef]
- Zhu, J.; Lu, C. Air Quality, Pollution Perception, and Residents’ Health: Evidence from China. Toxics 2023, 11, 591. [Google Scholar] [CrossRef] [PubMed]
- Mlambo, C.; Ngonisa, P.; Ntshangase, B.; Ndlovu, N.; Mvuyana, B. Air Pollution and Health in Africa: The Burden Falls on Children. Economies 2023, 11, 196. [Google Scholar] [CrossRef]
- Eguiluz-Gracia, I.; Mathioudakis, A.G.; Bartel, S.; Vijverberg, S.J.; Fuertes, E.; Comberiati, P.; Cai, Y.S.; Tomazic, P.V.; Diamant, Z.; Vestbo, J.; et al. The need for clean air: The way air pollution and climate change affect allergic rhinitis and asthma. Allergy 2020, 75, 2170–2184. [Google Scholar] [CrossRef] [PubMed]
- Naclerio, R.; Ansotegui, I.J.; Bousquet, J.; Canonica, G.W.; d’Amato, G.; Rosario, N.; Pawankar, R.; Peden, D.; Bergmann, K.C.; Bielory, L.; et al. International expert consensus on the management of allergic rhinitis (AR) aggravated by air pollutants: Impact of air pollution on patients with AR: Current knowledge and future strategies. World Allergy Organ. J. 2020, 13, 100106. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Wu, W.; Wang, G.; Zhang, X.; Guo, Q.; Wang, B.; Cao, S.; Yan, M.; Pan, X.; Xue, T.; et al. Association between exposure to air pollution and risk of allergic rhinitis: A systematic review and meta-analysis. Environ. Res. 2022, 205, 112472. [Google Scholar] [CrossRef]
- Lee, M. Deep learning in CRISPR-Cas systems: A review of recent studies. Front. Bioeng. Biotechnol. 2023, 11, 1226182. [Google Scholar] [CrossRef]
- Samudra, S.; Barbosh, M.; Sadhu, A. Machine Learning-Assisted Improved Anomaly Detection for Structural Health Monitoring. Sensors 2023, 23, 3365. [Google Scholar] [CrossRef]
- Choi, S.R.; Lee, M. Transformer Architecture and Attention Mechanisms in Genome Data Analysis: A Comprehensive Review. Biology 2023, 12, 1033. [Google Scholar] [CrossRef]
- Lee, M. Machine Learning for Small Interfering RNAs: A Concise Review of Recent Developments. Front. Genet. 2023, 14, 1226336. [Google Scholar] [CrossRef] [PubMed]
- Benedum, C.M.; Sondhi, A.; Fidyk, E.; Cohen, A.B.; Nemeth, S.; Adamson, B.; Estévez, M.; Bozkurt, S. Replication of Real-World Evidence in Oncology Using Electronic Health Record Data Extracted by Machine Learning. Cancers 2023, 15, 1853. [Google Scholar] [CrossRef] [PubMed]
- Lee, M. Recent Advancements in Deep Learning Using Whole Slide Imaging for Cancer Prognosis. Bioengineering 2023, 10, 897. [Google Scholar] [CrossRef]
- Castelli, S.; Belleri, A. Framework for Identification and Prediction of Corrosion Degradation in a Steel Column through Machine Learning and Bayesian Updating. Appl. Sci. 2023, 13, 4646. [Google Scholar] [CrossRef]
- Lu, H.; Uddin, S. Disease Prediction Using Graph Machine Learning Based on Electronic Health Data: A Review of Approaches and Trends. Healthcare 2023, 11, 1031. [Google Scholar] [CrossRef] [PubMed]
- Reid, S.; Tibshirani, R.; Friedman, J. A study of error variance estimation in lasso regression. Stat. Sin. 2016, 26, 35–67. [Google Scholar] [CrossRef]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Friedman, J.H. Greedy function approximation: A gradient boosting machine. Ann. Stat. 2001, 29, 1189–1232. [Google Scholar] [CrossRef]
- Zhang, J.; Wei, Y.; Fang, Z. Ozone pollution: A major health hazard worldwide. Front. Immunol. 2019, 10, 2518. [Google Scholar] [CrossRef]
- Liu, H.; Liu, S.; Xue, B.; Lv, Z.; Meng, Z.; Yang, X.; Xue, T.; Yu, Q.; He, K. Ground-level ozone pollution and its health impacts in China. Atmos. Environ. 2018, 173, 223–230. [Google Scholar] [CrossRef]
- Nuvolone, D.; Petri, D.; Voller, F. The effects of ozone on human health. Environ. Sci. Pollut. Res. 2018, 25, 8074–8088. [Google Scholar] [CrossRef] [PubMed]
- Kyung, S.Y.; Jeong, S.H. Particulate-matter related respiratory diseases. Tuberc. Respir. Dis. 2020, 83, 116. [Google Scholar] [CrossRef] [PubMed]
- Jo, E.J.; Lee, W.S.; Jo, H.Y.; Kim, C.H.; Eom, J.S.; Mok, J.H.; Kim, M.H.; Lee, K.; Kim, K.U.; Lee, M.K.; et al. Effects of particulate matter on respiratory disease and the impact of meteorological factors in Busan, Korea. Respir. Med. 2017, 124, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.Z.; Ge, D.D.; Zhou, L.F.; Hou, L.Y.; Zhou, Y.; Li, Q.Y. Effects of particulate matter on allergic respiratory diseases. Chronic Dis. Transl. Med. 2018, 4, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Sadiq, A.A.; Khardi, S.; Lazar, A.N.; Bello, I.W.; Salam, S.P.; Faruk, A.; Alao, M.A.; Catinon, M.; Vincent, M.; Trunfio-Sfarghiu, A.M. A Characterization and Cell Toxicity Assessment of Particulate Pollutants from Road Traffic Sites in Kano State, Nigeria. Atmosphere 2022, 13, 80. [Google Scholar] [CrossRef]
- Fan, C.; Li, Y.; Guang, J.; Li, Z.; Elnashar, A.; Allam, M.; de Leeuw, G. The impact of the control measures during the COVID-19 outbreak on air pollution in China. Remote Sens. 2020, 12, 1613. [Google Scholar] [CrossRef]
- Mirri, S.; Delnevo, G.; Roccetti, M. Is a COVID-19 Second Wave Possible in Emilia-Romagna (Italy)? Forecasting a Future Outbreak with Particulate Pollution and Machine Learning. Computation 2020, 8, 74. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.; Hyun, C.; Lee, M. Machine Learning Big Data Analysis of the Impact of Air Pollutants on Rhinitis-Related Hospital Visits. Toxics 2023, 11, 719. https://doi.org/10.3390/toxics11080719
Lee S, Hyun C, Lee M. Machine Learning Big Data Analysis of the Impact of Air Pollutants on Rhinitis-Related Hospital Visits. Toxics. 2023; 11(8):719. https://doi.org/10.3390/toxics11080719
Chicago/Turabian StyleLee, Soyeon, Changwan Hyun, and Minhyeok Lee. 2023. "Machine Learning Big Data Analysis of the Impact of Air Pollutants on Rhinitis-Related Hospital Visits" Toxics 11, no. 8: 719. https://doi.org/10.3390/toxics11080719
APA StyleLee, S., Hyun, C., & Lee, M. (2023). Machine Learning Big Data Analysis of the Impact of Air Pollutants on Rhinitis-Related Hospital Visits. Toxics, 11(8), 719. https://doi.org/10.3390/toxics11080719





