In Vitro Biological Effects of E-Cigarette on the Cardiovascular System—Pro-Inflammatory Response Enhanced by the Presence of the Cinnamon Flavor
Abstract
1. Introduction
2. Materials and Methods
2.1. Cell Culture
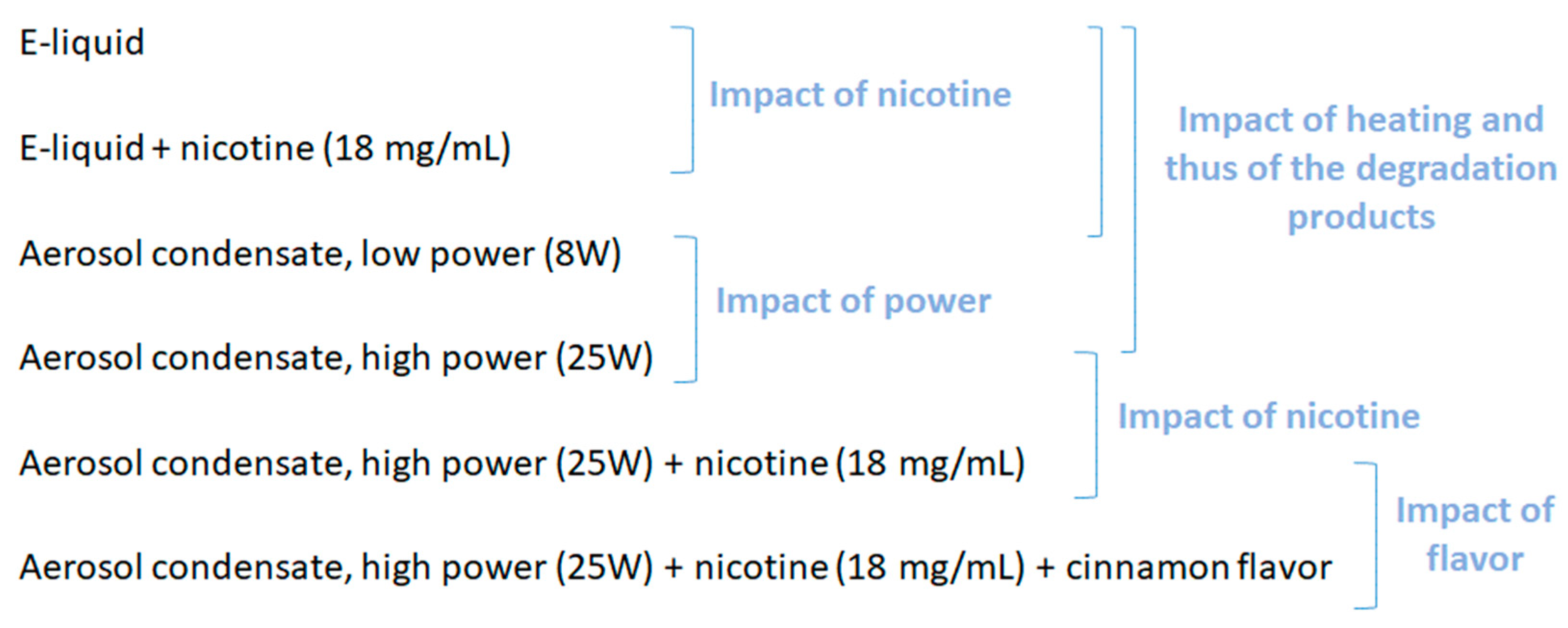
2.2. E-liquids and Aerosol Condensates Preparation
2.3. Toxicity Assessment
2.3.1. Cytotoxicity
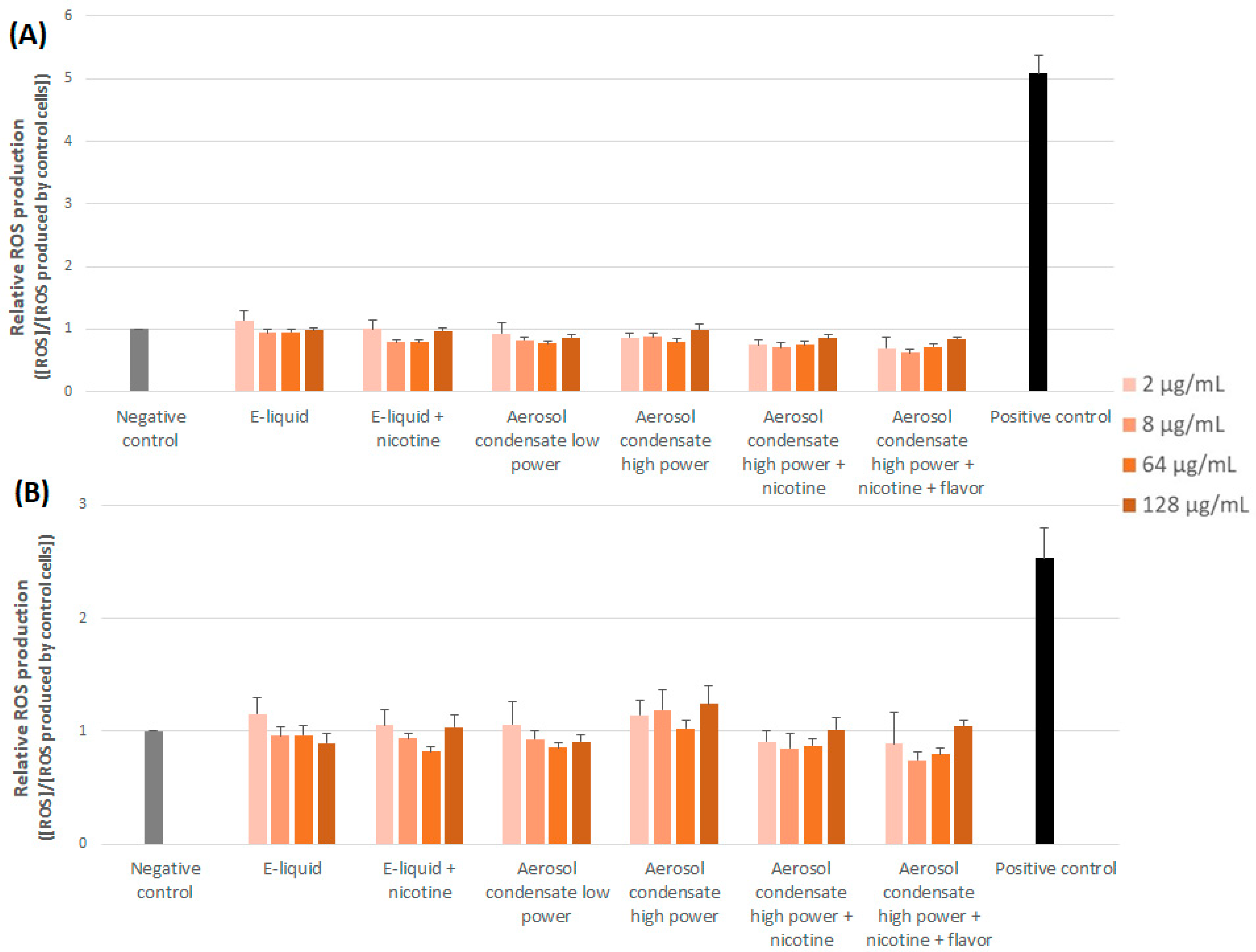
2.3.2. Production of Reactive Oxygen Species (ROS)
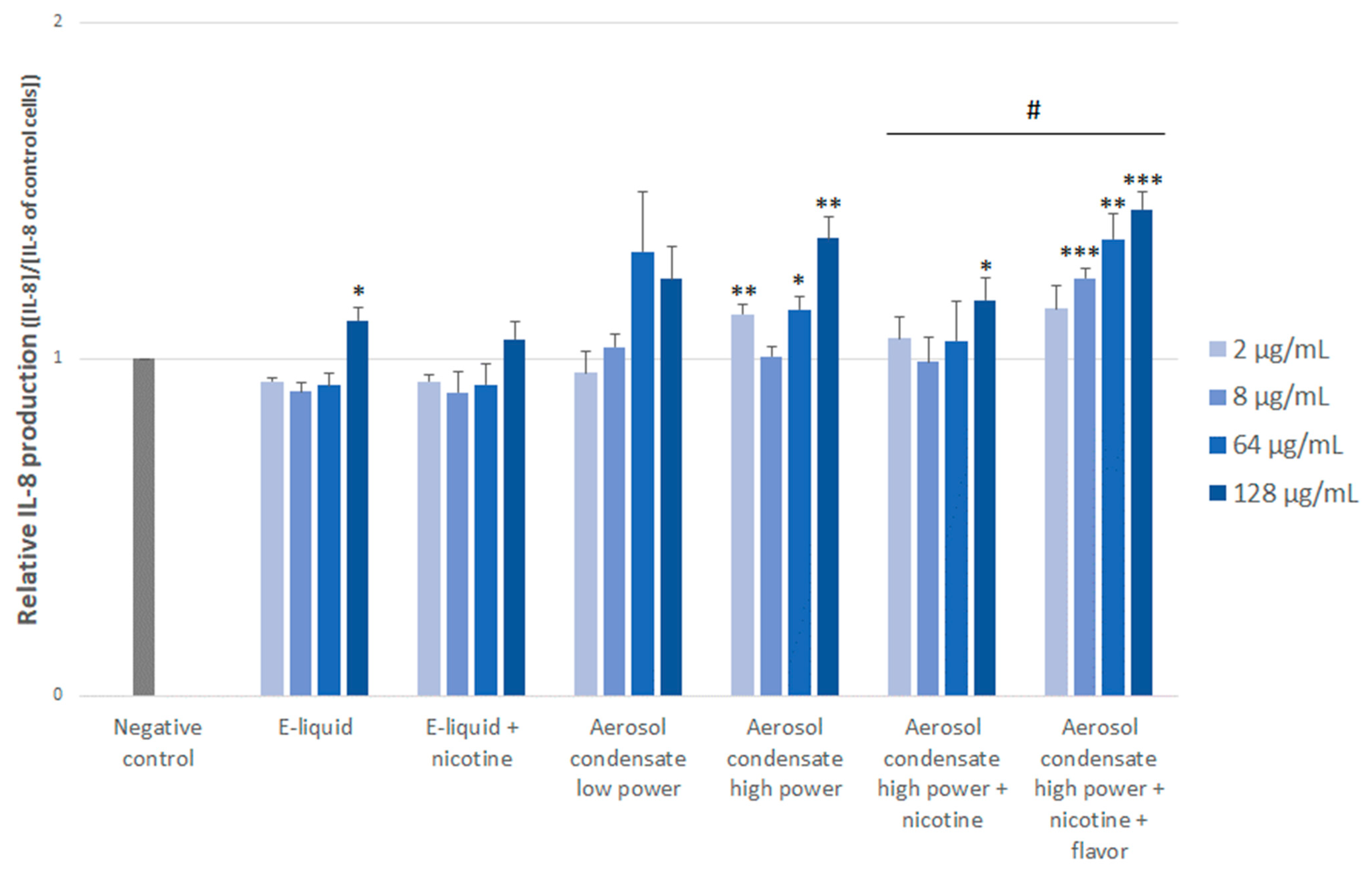
2.3.3. IL-8 Production
2.4. Statistical Analyses
3. Results
3.1. Cytotoxicity
3.2. ROS Production
3.3. IL-8 Production
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hajek, P.; Phillips-Waller, A.; Przulj, D.; Pesola, F.; Myers Smith, K.; Bisal, N.; Li, J.; Parrott, S.; Sasieni, P.; Dawkins, L.; et al. A Randomized Trial of E-Cigarettes versus Nicotine-Replacement Therapy. N. Engl. J. Med. 2019, 380, 629–637. [Google Scholar] [CrossRef]
- McNeill, A.; Brose, L.; Calder, R.; Simonavicius, E.; Robson, D. Vaping in England: An Evidence Update Including Vaping for Smoking Cessation, February 2021: A Report Commissioned by Public Health England; Public Health England: London, UK, 2021; p. 247. [Google Scholar]
- Marques, P.; Piqueras, L.; Sanz, M.-J. An Updated Overview of E-Cigarette Impact on Human Health. Respir. Res. 2021, 22, 151. [Google Scholar] [CrossRef]
- Dinakar, C.; O’Connor, G.T. The Health Effects of Electronic Cigarettes. N. Engl. J. Med. 2016, 375, 1372–1381. [Google Scholar] [CrossRef]
- Cao, Y.; Wu, D.; Ma, Y.; Ma, X.; Wang, S.; Li, F.; Li, M.; Zhang, T. Toxicity of Electronic Cigarettes: A General Review of the Origins, Health Hazards, and Toxicity Mechanisms. Sci. Total Environ. 2021, 772, 145475. [Google Scholar] [CrossRef]
- Buchanan, N.D.; Grimmer, J.A.; Tanwar, V.; Schwieterman, N.; Mohler, P.J.; Wold, L.E. Cardiovascular Risk of Electronic Cigarettes: A Review of Preclinical and Clinical Studies. Cardiovasc. Res. 2020, 116, 40–50. [Google Scholar] [CrossRef]
- Behar, R.Z.; Wang, Y.; Talbot, P. Comparing the Cytotoxicity of Electronic Cigarette Fluids, Aerosols and Solvents. Tob. Control 2018, 27, 325–333. [Google Scholar] [CrossRef]
- Wang, G.; Liu, W.; Song, W. Toxicity Assessment of Electronic Cigarettes. Inhal. Toxicol. 2019, 31, 259–273. [Google Scholar] [CrossRef]
- Vlachopoulos, C.; Ioakeimidis, N.; Abdelrasoul, M.; Terentes-Printzios, D.; Georgakopoulos, C.; Pietri, P.; Stefanadis, C.; Tousoulis, D. Electronic Cigarette Smoking Increases Aortic Stiffness and Blood Pressure in Young Smokers. J. Am. Coll. Cardiol. 2016, 67, 2802–2803. [Google Scholar] [CrossRef]
- Carnevale, R.; Sciarretta, S.; Violi, F.; Nocella, C.; Loffredo, L.; Perri, L.; Peruzzi, M.; Marullo, A.G.M.; De Falco, E.; Chimenti, I.; et al. Acute Impact of Tobacco vs Electronic Cigarette Smoking on Oxidative Stress and Vascular Function. Chest 2016, 150, 606–612. [Google Scholar] [CrossRef]
- Chaumont, M.; de Becker, B.; Zaher, W.; Culié, A.; Deprez, G.; Mélot, C.; Reyé, F.; Van Antwerpen, P.; Delporte, C.; Debbas, N.; et al. Differential Effects of E-Cigarette on Microvascular Endothelial Function, Arterial Stiffness and Oxidative Stress: A Randomized Crossover Trial. Sci. Rep. 2018, 8, 10378. [Google Scholar] [CrossRef]
- Franzen, K.F.; Willig, J.; Cayo Talavera, S.; Meusel, M.; Sayk, F.; Reppel, M.; Dalhoff, K.; Mortensen, K.; Droemann, D. E-Cigarettes and Cigarettes Worsen Peripheral and Central Hemodynamics as Well as Arterial Stiffness: A Randomized, Double-Blinded Pilot Study. Vasc. Med. 2018, 23, 419–425. [Google Scholar] [CrossRef]
- Skotsimara, G.; Antonopoulos, A.S.; Oikonomou, E.; Siasos, G.; Ioakeimidis, N.; Tsalamandris, S.; Charalambous, G.; Galiatsatos, N.; Vlachopoulos, C.; Tousoulis, D. Cardiovascular Effects of Electronic Cigarettes: A Systematic Review and Meta-Analysis. Eur. J. Prev. Cardiol. 2019, 26, 1219–1228. [Google Scholar] [CrossRef]
- Antoniewicz, L.; Brynedal, A.; Hedman, L.; Lundbäck, M.; Bosson, J.A. Acute Effects of Electronic Cigarette Inhalation on the Vasculature and the Conducting Airways. Cardiovasc. Toxicol. 2019, 19, 441–450. [Google Scholar] [CrossRef]
- Caporale, A.; Langham, M.C.; Guo, W.; Johncola, A.; Chatterjee, S.; Wehrli, F.W. Acute Effects of Electronic Cigarette Aerosol Inhalation on Vascular Function Detected at Quantitative MRI. Radiology 2019, 293, 97–106. [Google Scholar] [CrossRef]
- Keith, R.; Bhatnagar, A. Cardiorespiratory and Immunologic Effects of Electronic Cigarettes. Curr. Addict. Rep. 2021, 8, 336–346. [Google Scholar] [CrossRef]
- Kuntic, M.; Oelze, M.; Steven, S.; Kröller-Schön, S.; Stamm, P.; Kalinovic, S.; Frenis, K.; Vujacic-Mirski, K.; Bayo Jimenez, M.T.; Kvandova, M.; et al. Short-Term e-Cigarette Vapour Exposure Causes Vascular Oxidative Stress and Dysfunction: Evidence for a Close Connection to Brain Damage and a Key Role of the Phagocytic NADPH Oxidase (NOX-2). Eur. Heart J. 2020, 41, 2472–2483. [Google Scholar] [CrossRef]
- Higham, A.; Rattray, N.J.W.; Dewhurst, J.A.; Trivedi, D.K.; Fowler, S.J.; Goodacre, R.; Singh, D. Electronic Cigarette Exposure Triggers Neutrophil Inflammatory Responses. Respir. Res. 2016, 17, 56. [Google Scholar] [CrossRef]
- Landmesser, U.; Hornig, B.; Drexler, H. Endothelial Function: A Critical Determinant in Atherosclerosis? Circulation 2004, 109, II-27–II-33. [Google Scholar] [CrossRef]
- von Hundelshausen, P.; Schmitt, M.M.N. Platelets and Their Chemokines in Atherosclerosis-Clinical Applications. Front. Physiol. 2014, 5, 294. [Google Scholar] [CrossRef]
- Lacolley, P.; Regnault, V.; Segers, P.; Laurent, S. Vascular Smooth Muscle Cells and Arterial Stiffening: Relevance in Development, Aging, and Disease. Physiol. Rev. 2017, 97, 1555–1617. [Google Scholar] [CrossRef]
- Zhuge, Y.; Zhang, J.; Qian, F.; Wen, Z.; Niu, C.; Xu, K.; Ji, H.; Rong, X.; Chu, M.; Jia, C. Role of Smooth Muscle Cells in Cardiovascular Disease. Int. J. Biol. Sci. 2020, 16, 2741–2751. [Google Scholar] [CrossRef]
- Lee, W.H.; Ong, S.-G.; Zhou, Y.; Tian, L.; Bae, H.R.; Baker, N.; Whitlatch, A.; Mohammadi, L.; Guo, H.; Nadeau, K.C.; et al. Modeling Cardiovascular Risks of E-Cigarettes With Human-Induced Pluripotent Stem Cell–Derived Endothelial Cells. J. Am. Coll. Cardiol. 2019, 73, 2722–2737. [Google Scholar] [CrossRef]
- ANSES. RAPPORT de l’Anses Relatif à la Déclaration des Produits du Tabac et des Produits Connexes en France—Produits du Vapotage—Bilan 2016–2020; ANSES: Maisons-Alfort, France, 2020.
- AFNOR. Norme XP D90-300-3 Cigarettes Electroniques et e-Liquides—Exigences et Méthodes D’essai Relatives aux Emissions (Electronic Cigarettes and e-Liquids—Requirements and Test Methods for Emissions); AFNOR: Paris, France, 2021. [Google Scholar]
- Sassano, M.F.; Davis, E.S.; Keating, J.E.; Zorn, B.T.; Kochar, T.K.; Wolfgang, M.C.; Glish, G.L.; Tarran, R. Evaluation of E-Liquid Toxicity Using an Open-Source High-Throughput Screening Assay. PLoS Biol. 2018, 16, e2003904. [Google Scholar] [CrossRef]
- Gellatly, S.; Pavelka, N.; Crue, T.; Schweitzer, K.S.; Day, B.J.; Min, E.; Numata, M.; Voelker, D.R.; Scruggs, A.; Petrache, I.; et al. Nicotine-Free e-Cigarette Vapor Exposure Stimulates IL6 and Mucin Production in Human Primary Small Airway Epithelial Cells. JIR 2020, 13, 175–185. [Google Scholar] [CrossRef]
- Kalra, R.; Singh, S.P.; Pena-Philippides, J.C.; Langley, R.J.; Razani-Boroujerdi, S.; Sopori, M.L. Immunosuppressive and Anti-Inflammatory Effects of Nicotine Administered by Patch in an Animal Model. Clin. Vaccine Immunol. 2004, 11, 563–568. [Google Scholar] [CrossRef]
- Wu, Q.; Jiang, D.; Minor, M.; Chu, H.W. Electronic Cigarette Liquid Increases Inflammation and Virus Infection in Primary Human Airway Epithelial Cells. PLoS ONE 2014, 9, e108342. [Google Scholar] [CrossRef]
- Merecz-Sadowska, A.; Sitarek, P.; Zielinska-Blizniewska, H.; Malinowska, K.; Zajdel, K.; Zakonnik, L.; Zajdel, R. A Summary of In Vitro and In Vivo Studies Evaluating the Impact of E-Cigarette Exposure on Living Organisms and the Environment. Int. J. Mol. Sci. 2020, 21, 652. [Google Scholar] [CrossRef]
- Cervellati, F.; Muresan, X.M.; Sticozzi, C.; Gambari, R.; Montagner, G.; Forman, H.J.; Torricelli, C.; Maioli, E.; Valacchi, G. Comparative Effects between Electronic and Cigarette Smoke in Human Keratinocytes and Epithelial Lung Cells. Toxicol. In Vitro 2014, 28, 999–1005. [Google Scholar] [CrossRef]
- Scott, A.; Lugg, S.T.; Aldridge, K.; Lewis, K.E.; Bowden, A.; Mahida, R.Y.; Grudzinska, F.S.; Dosanjh, D.; Parekh, D.; Foronjy, R.; et al. Pro-Inflammatory Effects of e-Cigarette Vapour Condensate on Human Alveolar Macrophages. Thorax 2018, 73, 1161–1169. [Google Scholar] [CrossRef]
- Clapp, P.W.; Pawlak, E.A.; Lackey, J.T.; Keating, J.E.; Reeber, S.L.; Glish, G.L.; Jaspers, I. Flavored E-Cigarette Liquids and Cinnamaldehyde Impair Respiratory Innate Immune Cell Function. Am. J. Physiol. Lung. Cell. Mol. Physiol. 2017, 313, L278–L292. [Google Scholar] [CrossRef]
- Muthumalage, T.; Prinz, M.; Ansah, K.O.; Gerloff, J.; Sundar, I.K.; Rahman, I. Inflammatory and Oxidative Responses Induced by Exposure to Commonly Used E-Cigarette Flavoring Chemicals and Flavored e-Liquids without Nicotine. Front. Physiol. 2017, 8, 1130. [Google Scholar] [CrossRef]
- Fetterman, J.L.; Weisbrod, R.M.; Feng, B.; Bastin, R.; Tuttle, S.T.; Holbrook, M.; Baker, G.; Robertson, R.M.; Conklin, D.J.; Bhatnagar, A.; et al. Flavorings in Tobacco Products Induce Endothelial Cell Dysfunction. Arterioscler. Thromb. Vasc. Biol. 2018, 38, 1607–1615. [Google Scholar] [CrossRef]
- Wölkart, G.; Kollau, A.; Stessel, H.; Russwurm, M.; Koesling, D.; Schrammel, A.; Schmidt, K.; Mayer, B. Effects of Flavoring Compounds Used in Electronic Cigarette Refill Liquids on Endothelial and Vascular Function. PLoS ONE 2019, 14, e0222152. [Google Scholar] [CrossRef]
- Lerner, C.A.; Sundar, I.K.; Yao, H.; Gerloff, J.; Ossip, D.J.; McIntosh, S.; Robinson, R.; Rahman, I. Vapors Produced by Electronic Cigarettes and E-Juices with Flavorings Induce Toxicity, Oxidative Stress, and Inflammatory Response in Lung Epithelial Cells and in Mouse Lung. PLoS ONE 2015, 10, e0116732. [Google Scholar] [CrossRef]
- Gerloff, J.; Sundar, I.K.; Freter, R.; Sekera, E.R.; Friedman, A.E.; Robinson, R.; Pagano, T.; Rahman, I. Inflammatory Response and Barrier Dysfunction by Different E-Cigarette Flavoring Chemicals Identified by Gas Chromatography-Mass Spectrometry in e-Liquids and e-Vapors on Human Lung Epithelial Cells and Fibroblasts. Appl. In Vitro Toxicol. 2017, 3, 28–40. [Google Scholar] [CrossRef]
- Kaur, G.; Muthumalage, T.; Rahman, I. Mechanisms of Toxicity and Biomarkers of Flavoring and Flavor Enhancing Chemicals in Emerging Tobacco and Non-Tobacco Products. Toxicol. Lett. 2018, 288, 143–155. [Google Scholar] [CrossRef]
- Anderson, C.; Majeste, A.; Hanus, J.; Wang, S. E-Cigarette Aerosol Exposure Induces Reactive Oxygen Species, DNA Damage, and Cell Death in Vascular Endothelial Cells. Toxicol. Sci. 2016, 154, 332–340. [Google Scholar] [CrossRef]
- Su, L.; Zhao, M.; Ma, F.; An, Z.; Yue, Q.; Zhao, C.; Sun, X.; Zhang, S.; Xu, J.; Jiang, X.; et al. A Comparative Assessment of E-Cigarette Aerosol Extracts and Tobacco Cigarette Smoke Extracts on in Vitro Endothelial Cell Inflammation Response. Hum. Exp. Toxicol. 2022, 41, 9603271221088996. [Google Scholar] [CrossRef]
- De Martin, S.; Gabbia, D.; Bogialli, S.; Biasioli, F.; Boschetti, A.; Gstir, R.; Rainer, D.; Cappellin, L. Refill Liquids for Electronic Cigarettes Display Peculiar Toxicity on Human Endothelial Cells. Toxicol. Rep. 2021, 8, 456–462. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michon, M.; Mercier, C.; Petit, C.; Leclerc, L.; Bertoletti, L.; Pourchez, J.; Forest, V. In Vitro Biological Effects of E-Cigarette on the Cardiovascular System—Pro-Inflammatory Response Enhanced by the Presence of the Cinnamon Flavor. Toxics 2022, 10, 784. https://doi.org/10.3390/toxics10120784
Michon M, Mercier C, Petit C, Leclerc L, Bertoletti L, Pourchez J, Forest V. In Vitro Biological Effects of E-Cigarette on the Cardiovascular System—Pro-Inflammatory Response Enhanced by the Presence of the Cinnamon Flavor. Toxics. 2022; 10(12):784. https://doi.org/10.3390/toxics10120784
Chicago/Turabian StyleMichon, Marine, Clément Mercier, Claudie Petit, Lara Leclerc, Laurent Bertoletti, Jérémie Pourchez, and Valérie Forest. 2022. "In Vitro Biological Effects of E-Cigarette on the Cardiovascular System—Pro-Inflammatory Response Enhanced by the Presence of the Cinnamon Flavor" Toxics 10, no. 12: 784. https://doi.org/10.3390/toxics10120784
APA StyleMichon, M., Mercier, C., Petit, C., Leclerc, L., Bertoletti, L., Pourchez, J., & Forest, V. (2022). In Vitro Biological Effects of E-Cigarette on the Cardiovascular System—Pro-Inflammatory Response Enhanced by the Presence of the Cinnamon Flavor. Toxics, 10(12), 784. https://doi.org/10.3390/toxics10120784





