Reliability of Heterochromatic Flicker Photometry in Measuring Macular Pigment Optical Density among Preadolescent Children
Abstract
:1. Introduction
2. Experimental Section
2.1. Participants
2.2. MPOD Measurement
2.3. Training of Examiners
2.4. Statistical Analysis
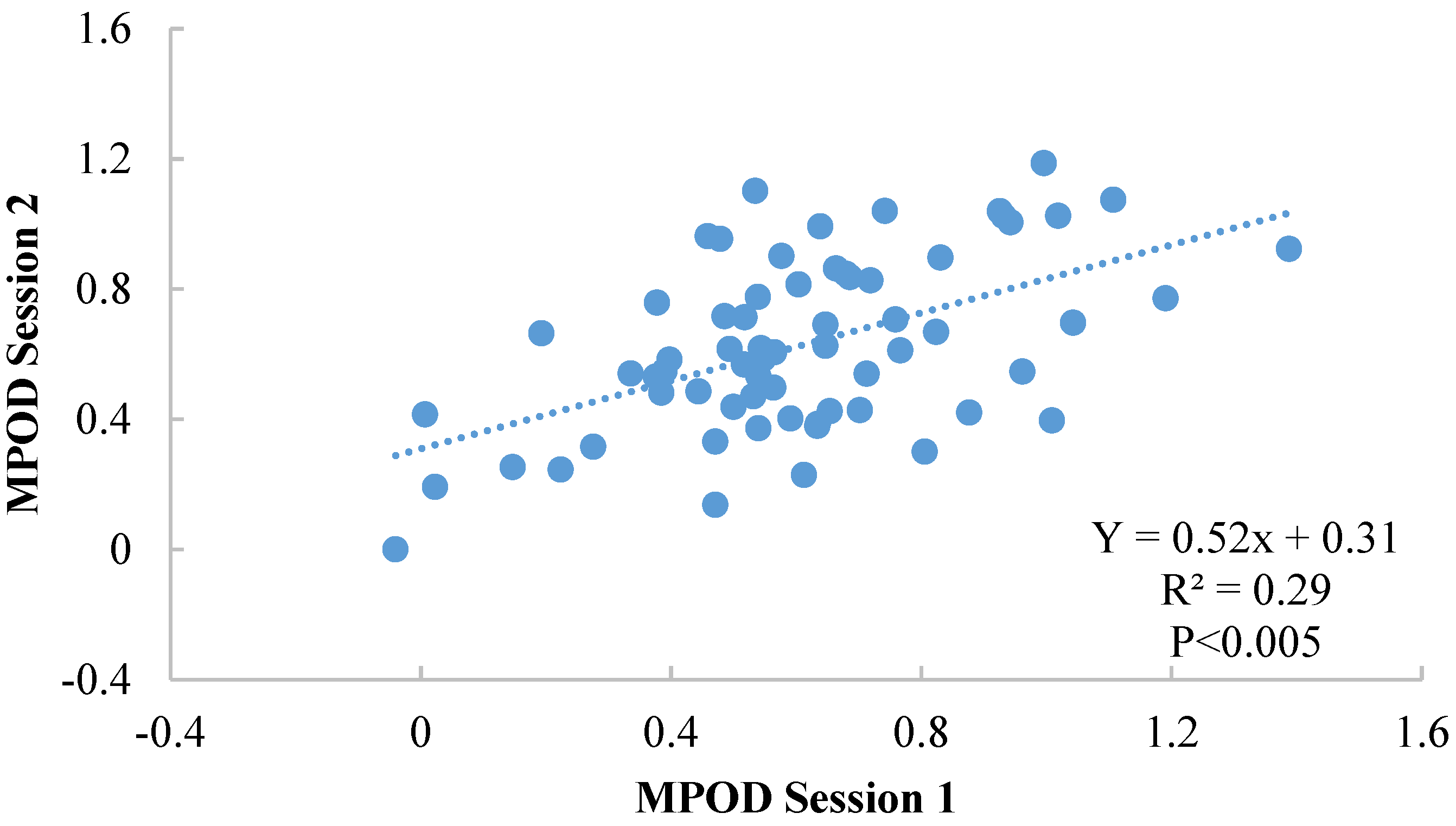
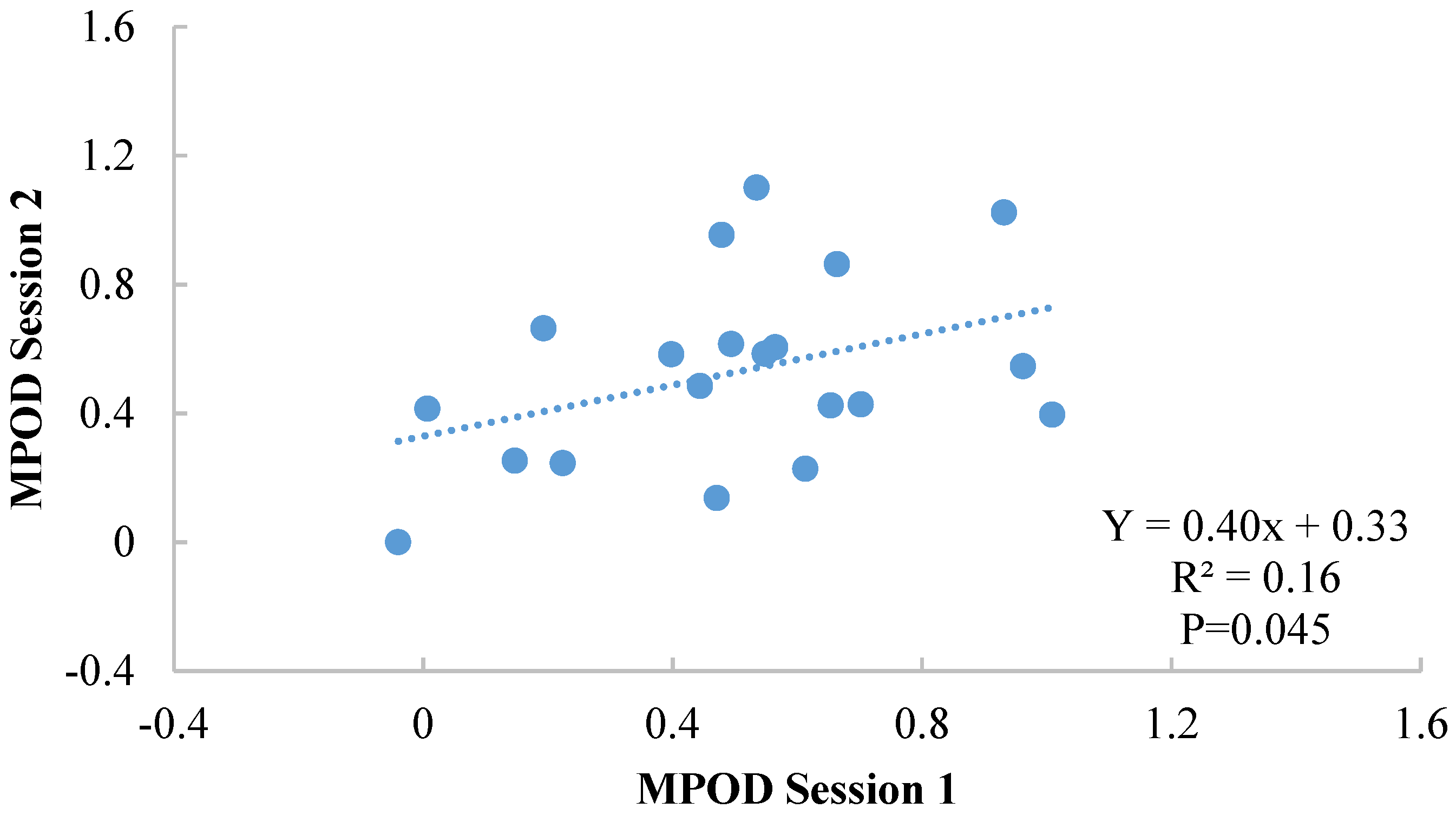
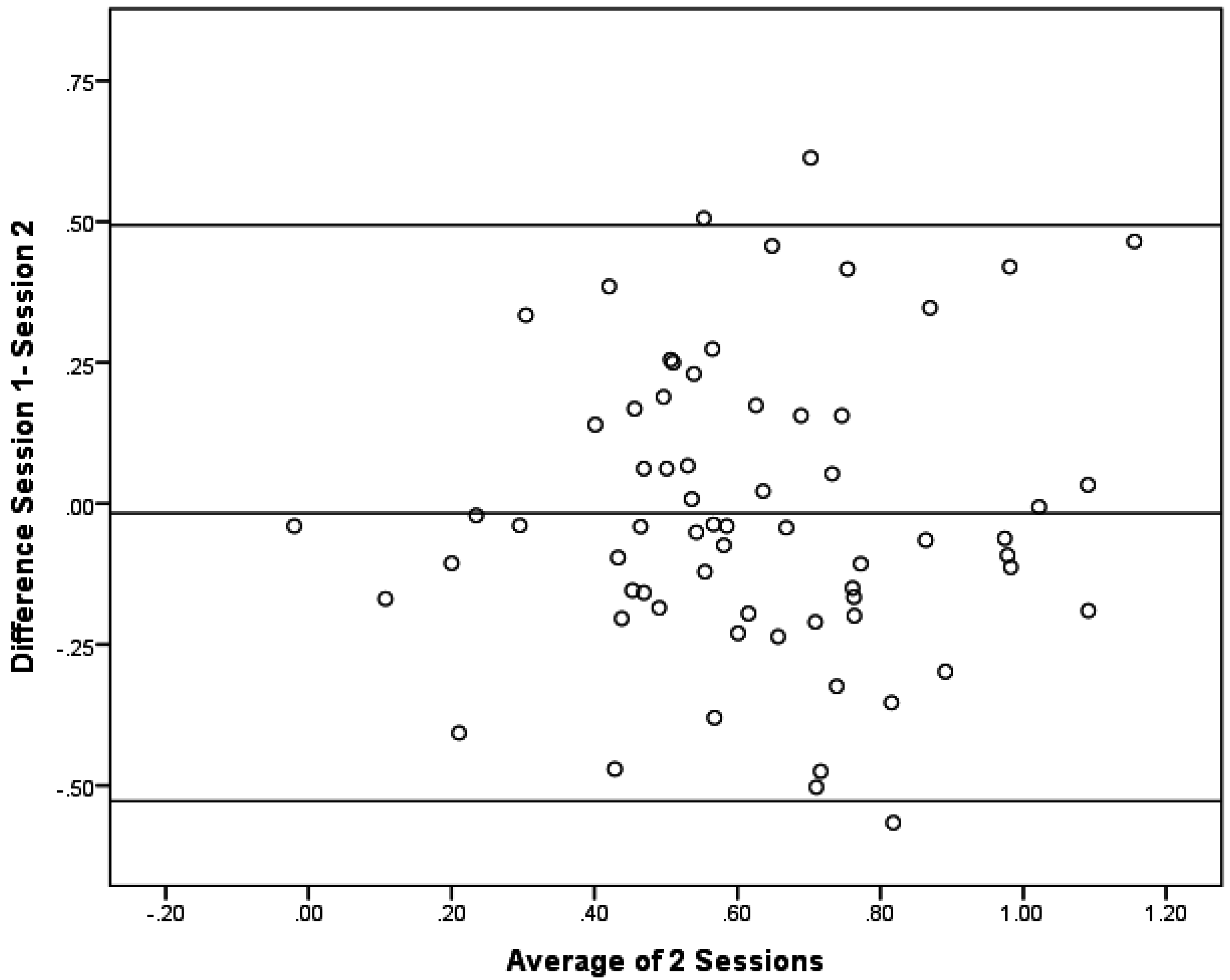
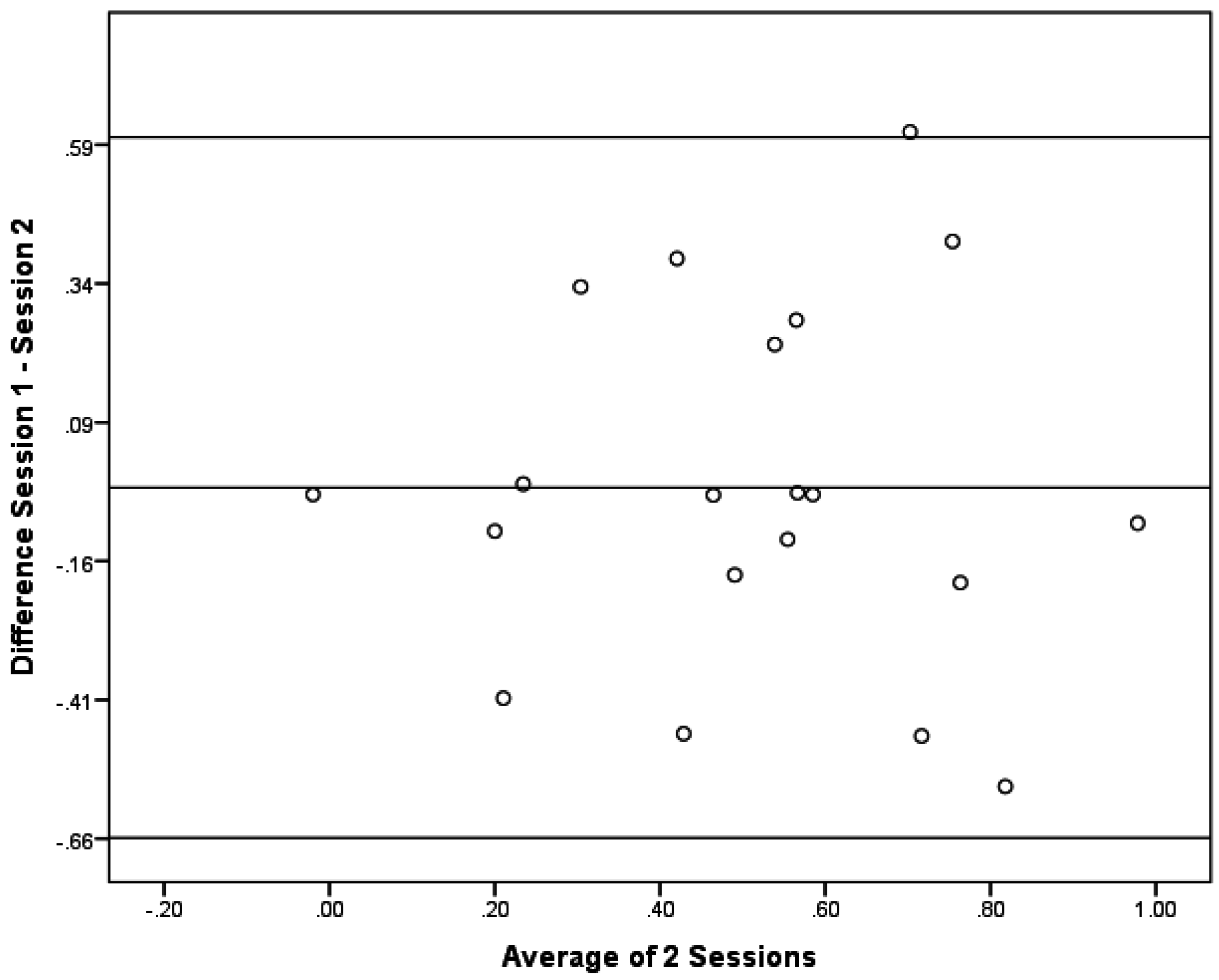
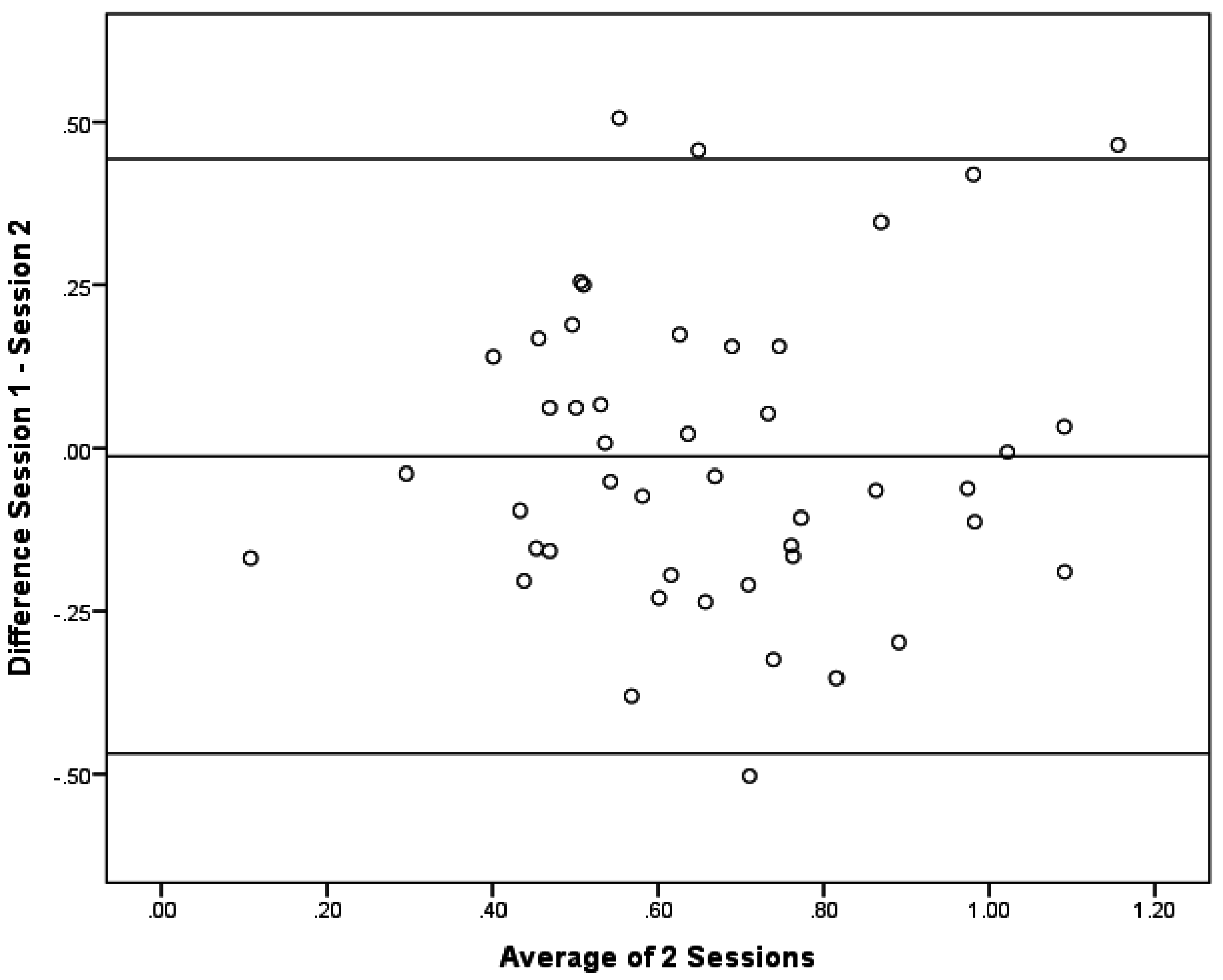
3. Results
| Characteristic | Full Sample (n = 66) | Subgroup 1 (n = 20) | Subgroup 2 (n = 46) |
|---|---|---|---|
| Sex [n (%)] | |||
| Male | 26 (39) | 14 (70) | 12 (26) |
| Female | 40 (60) | 6 (30) | 34 (74) |
| Age (years) | 8.8 ± 0.08 | 8.7 ± 0.13 | 8.8 ± 0.11 |

4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Vishwanathan, R.; Kuchan, M.J.; Sen, S.; Johnson, E.J. Lutein and preterm infants with decreased concentration of brain carotenoids. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 659–665. [Google Scholar] [CrossRef] [PubMed]
- Johnson, E.J.; Vishwanathan, R.; Johnson, MA.; Hausman, D.B.; Davey, A.; Scott, T.M.; Green, R.C.; Miller, L.S.; Gearing, M.; Woodard, J.; et al. Relationship between Serum and Brain Carotenoids, alpha-Tocopherol, and Retinol Concentrations and Cognitive Performance in the Oldest Old from the Georgia Centenarian Study. J. Aging Res. 2013, 2013, 13. [Google Scholar] [CrossRef] [PubMed]
- Sabour-Pickett, S.; Nolan, J.M.; Loughman, J.; Beatty, S. A review of the evidence germane to the putative protective role of the macular carotenoids for age-related macular degeneration. Mol. Nutr. Food Res. 2012, 56, 270–286. [Google Scholar] [CrossRef] [PubMed]
- Vishwanathan, R.; Iannaccone, A.; Scott, T.M.; Kritchevsky, S.B.; Jennings, B.J.; Carboni, G.; Forma, G.; Satterfield, S.; Harris, T.; Johnson, K.C.; et al. Macular pigment optical density is related to cognitive function in older people. Age Ageing 2014, 43, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Feeney, J.; Finucane, C.; Savva, G.M.; Cronin, H.; Beatty, S.; Nolan, J.M.; Kenny, R.A. Low macular pigment optical density is associated with lower cognitive performance in a large, population-based sample of older adults. Neurobiol. Aging 2013, 34, 2449–2456. [Google Scholar] [CrossRef] [PubMed]
- Vishwanathan, R.; Neuringer, M.; Snodderly, D.M.; Schalch, W.; Johnson, E.J. Macular lutein and zeaxanthin are related to brain lutein and zeaxanthin in primates. Nutr. Neurosci. 2013, 16, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Hammond, B.R.; Wooten, B.R. CFF thresholds: Relation to macular pigment optical density. Ophthalmic Physiol. Opt. 2005, 25, 315–319. [Google Scholar] [CrossRef] [PubMed]
- Johnson, E.J.; McDonald, K.; Caldarella, S.M.; Chung, H.; Troen, A.M.; Snodderly, D.M. Cognitive findings of an exploratory trial of docosahexaenoic acid and lutein supplementation in older women. Nutr. Neurosci. 2008, 11, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Renzi, L.M.; Dengler, M.J.; Puente, A.; Miller, L.S.; Hammond, B.R., Jr. Relationships between macular pigment optical density and cognitive function in unimpaired and mildly cognitively impaired older adults. Neurobiol. Aging 2014, 35, 1695–1699. [Google Scholar] [CrossRef] [PubMed]
- Mulder, K.A.; Innis, S.M.; Rasmussen, B.F.; Wu, B.T.; Richardson, K.J.; Hasman, D. Plasma lutein concentrations are related to dietary intake, but unrelated to dietary saturated fat or cognition in young children. J. Nutr. Sci. 2014, 3, e11. [Google Scholar] [CrossRef] [PubMed]
- Hammond, B.R. Lutein and cognition in children. J. Nutr. Sci. 2014, 3, e53. [Google Scholar] [CrossRef] [PubMed]
- Beatty, S.; Nolan, J.; Kavanagh, H.; O’Donovan, O. Macular pigment optical density and its relationship with serum and dietary levels of lutein and zeaxanthin. Arch. Biochem. Biophys. 2004, 430, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Howells, O.; Eperjesi, F.; Bartlett, H. Measuring macular pigment optical density in vivo: A review of techniques. Graefes Arch. Clin. Exp. Ophthalmol. 2011, 249, 315–347. [Google Scholar] [CrossRef] [PubMed]
- Lam, R.F.; Rao, S.K.; Fan, D.S.; Lau, F.T.; Lam, D.S. Macular pigment optical density in a Chinese sample. Curr Eye Res. 2005, 30, 729–35. [Google Scholar] [CrossRef] [PubMed]
- Van Der Veen, R.L.P.; Berendschot, T.T.; Hendrikse, F.; Carden, D.; Makridaki, M.; Murray, I.J. A new desktop instrument for measuring macular pigment optical density based on a novel technique for setting flicker thresholds. Ophthalmic Physiol. Opt. 2009, 29, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Ciulla, T.A.; Hammond, B.R.; Yung, C.W.; Pratt, L.M. Macular pigment optical density before and after cataract extraction. Investig. Ophthalmol. Vis. Sci. 2001, 42, 1338–1341. [Google Scholar]
- Hammond, B.R., Jr.; Curran-Celantano, J.; Judd, S.; Fuld, K.; Krinsky, N.I.; Wooten, B.R.; Snodderly, D.M. Sex Differences in Macular Pigment Optical Density: Relation to Plasma Carotenoid Concentrations and Dietary Patterns. Vis. Res. 1996, 36, 2001–2012. [Google Scholar] [CrossRef]
- Raman, R.; Rajan, R.; Biswas, S.; Vaitheeswaran, K.; Sharma, T. Macular pigment optical density in a South Indian population. Investig. Ophthalmol. Vis. Sci. 2011, 52, 7910–7916. [Google Scholar] [CrossRef] [PubMed]
- Iannaccone, A.; Mura, M.; Gallaher, K.T.; Johnson, E.J.; Todd, W.A.; Kenyon, E.; Harris, T.L.; Harris, T.; Satterfield, S.; Johnson, K.C.; et al. Macular pigment optical density in the elderly: Findings in a large biracial Midsouth population sample. Investig. Ophthalmol. Vis. Sci. 2007, 48, 1458–1465. [Google Scholar] [CrossRef] [PubMed]
- Tang, C.; Yip, H.; Poon, M.; Yau, W.; Yap, M.K. Macular pigment optical density in young Chinese adults. Ophthalmic Physiol. Opt. 2004, 24, 586–593. [Google Scholar] [CrossRef] [PubMed]
- Wooten, B.R.; Hammond, B.R.; Land, R.I.; Snodderly, D.M. A Practical Method for Measuring Macular Pigment Optical Density. Investig. Ophthalmol. Vis. Sci. 1999, 40, 2481–2489. [Google Scholar]
- Stringham, J.M.; Hammond, B.R.; Nolan, J.M.; Wooten, B.R.; Mammen, A.; Smollon, W.; Snodderly, D.M. The utility of using customized heterochromatic flicker photometry (cHFP) to measure macular pigment in patients with age-related macular degeneration. Exp. Eye Res. 2008, 87, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Hammond, B.R., Jr.; Fuld, K.; Curran-Celentano, J. Macular pigment density in monozygotic twins. Investig. Ophthalmol. Vis. Sci. 1995, 36, 2531–2541. [Google Scholar] [CrossRef]
- Hammond, B.R., Jr.; Caruso-Avery, M. Macular pigment optical density in a Southwestern sample. Investig. Ophthalmol. Vis. Sci. 2000, 41, 1492–1497. [Google Scholar]
- Zheng, W.; Zhang, Z.; Jiang, K.; Zhu, J.; He, G.; Ke, B. Macular pigment optical density and its relationship with refractive status and foveal thickness in Chinese school-aged children. Curr. Eye Res. 2013, 38, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Ciulla, T.A.; Curran-Celantano, J.; Cooper, D.A.; Hammond, B.R., Jr.; Danis, R.P.; Pratt, L.M.; Riccardi, K.A.; Filloon, T.G. Macular pigment optical density in a midwestern sample. Ophthalmology 2001, 108, 730–737. [Google Scholar] [CrossRef]
- Johnson, E.J.; Maras, J.E.; Rasmussen, H.M.; Tucker, K.L. Intake of Lutein and Zeaxanthin Differ with Age, Sex, and Ethnicity. J. Am. Diet. Assoc. 2010, 110, 1357–1362. [Google Scholar] [CrossRef] [PubMed]
- Forman, M.R.; Beecher, G.R.; Muesing, R.; Lanza, E.; Olson, B.; Campbell, W.S.; McAdam, P.; Raymond, E.; Schulman, J.D.; Graubard, B.I. The fluctuation of plasma carotenoid concentrations by phase of the menstrual cycle: A controlled diet study. Am. J. Clin. Nutr. 1996, 64, 559–565. [Google Scholar] [PubMed]
- Hammond, B.R.; Fuld, K. Interocular differences in macular pigment density. Investig. Ophthalmol. Vis. Sci. 1992, 33, 350–355. [Google Scholar]
- Richer, S.; Devenport, J.; Lang, J.C. LAST II: Differential temporal responses of macular pigment optical density in patients with atrophic age-related macular degeneration to dietary supplementation with xanthophylls. Optom. J. Am. Optom. Assoc. 2007, 78, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Hammond, B.R., Jr.; Johnson, E.J.; Russell, R.M.; Krinsky, N.I.; Yeum, K.; Edwards, R.B.; Snodderly, D.M. Dietary modification of human macular pigment density. Investig. Ophthalmol. Vis. Sci. 1997, 38, 1795–1801. [Google Scholar]
- Bone, R.A.; Landrum, J.T.; Tarsis, S.L. Preliminary identification of the human macular pigment. Vis. Res. 1985, 25, 1531–1535. [Google Scholar] [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
McCorkle, S.M.; Raine, L.B.; Hammond, B.R., Jr.; Renzi-Hammond, L.; Hillman, C.H.; Khan, N.A. Reliability of Heterochromatic Flicker Photometry in Measuring Macular Pigment Optical Density among Preadolescent Children. Foods 2015, 4, 594-604. https://doi.org/10.3390/foods4040594
McCorkle SM, Raine LB, Hammond BR Jr., Renzi-Hammond L, Hillman CH, Khan NA. Reliability of Heterochromatic Flicker Photometry in Measuring Macular Pigment Optical Density among Preadolescent Children. Foods. 2015; 4(4):594-604. https://doi.org/10.3390/foods4040594
Chicago/Turabian StyleMcCorkle, Sasha M., Lauren B. Raine, Billy R. Hammond, Jr., Lisa Renzi-Hammond, Charles H. Hillman, and Naiman A. Khan. 2015. "Reliability of Heterochromatic Flicker Photometry in Measuring Macular Pigment Optical Density among Preadolescent Children" Foods 4, no. 4: 594-604. https://doi.org/10.3390/foods4040594
APA StyleMcCorkle, S. M., Raine, L. B., Hammond, B. R., Jr., Renzi-Hammond, L., Hillman, C. H., & Khan, N. A. (2015). Reliability of Heterochromatic Flicker Photometry in Measuring Macular Pigment Optical Density among Preadolescent Children. Foods, 4(4), 594-604. https://doi.org/10.3390/foods4040594







